MULTIPLE ENDOCRINE NEOPLASIA SYNDROMES DEFINITION A case or

- Slides: 24
MULTIPLE ENDOCRINE NEOPLASIA SYNDROMES DEFINITION • A case or a family with hormone-secreting or hormone producing neoplasia in multiple tissue types • It encompasses several types of etiology, varying from two coincidental tumors to complex patterns of tumor types.
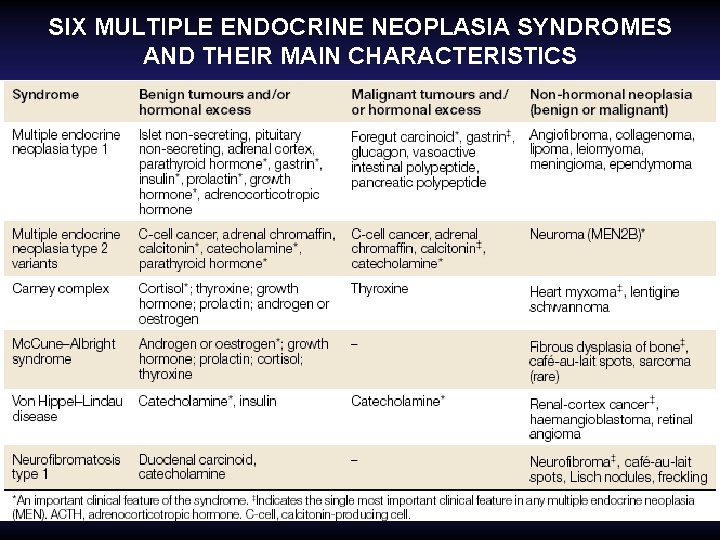
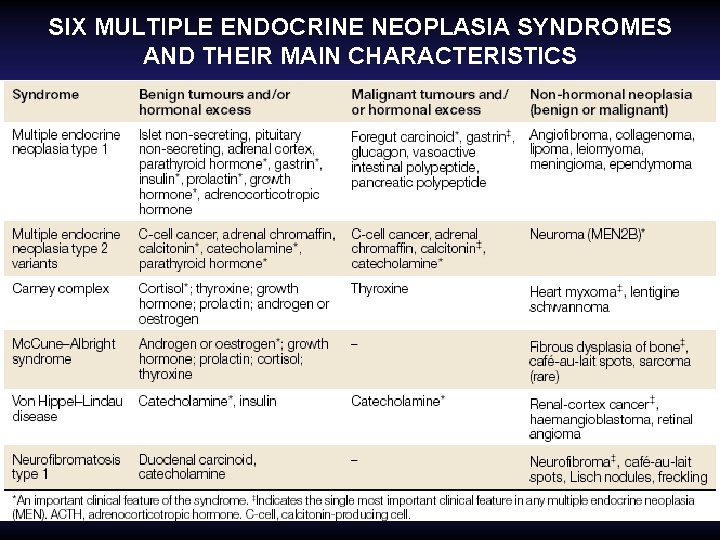
SIX MULTIPLE ENDOCRINE NEOPLASIA SYNDROMES AND THEIR MAIN CHARACTERISTICS
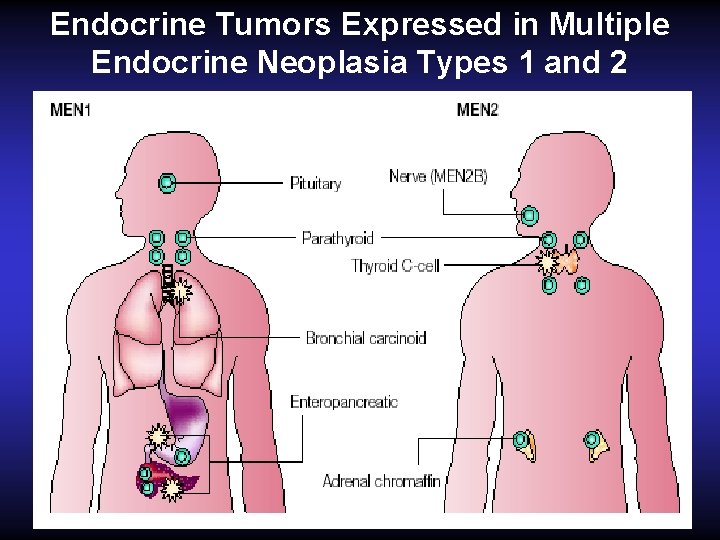
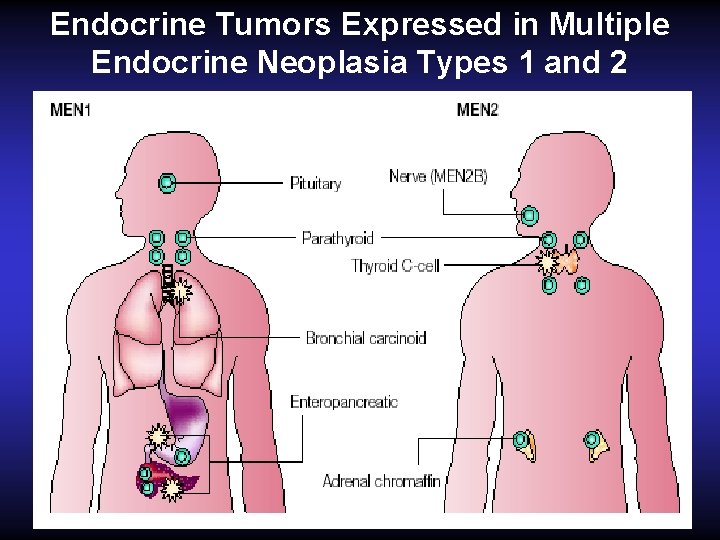
Endocrine Tumors Expressed in Multiple Endocrine Neoplasia Types 1 and 2
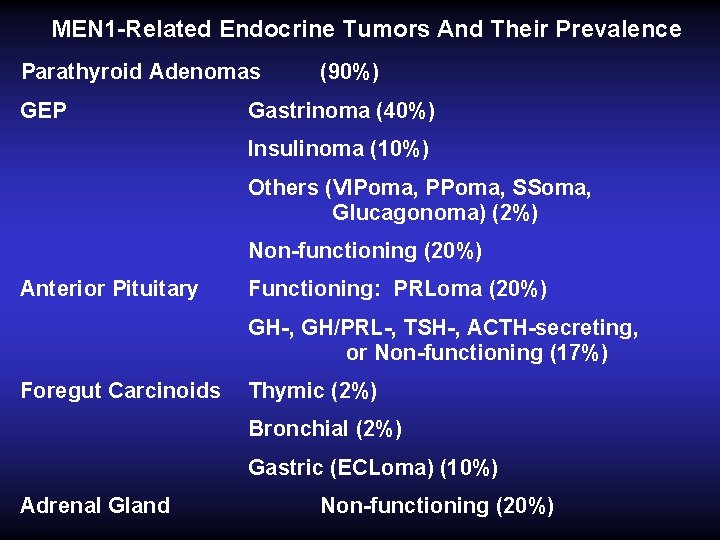
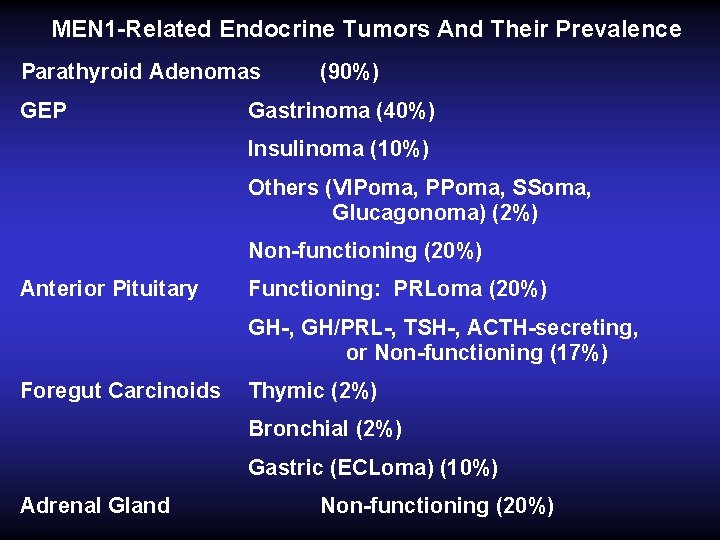
MEN 1 -Related Endocrine Tumors And Their Prevalence Parathyroid Adenomas GEP (90%) Gastrinoma (40%) Insulinoma (10%) Others (VIPoma, PPoma, SSoma, Glucagonoma) (2%) Non-functioning (20%) Anterior Pituitary Functioning: PRLoma (20%) GH-, GH/PRL-, TSH-, ACTH-secreting, or Non-functioning (17%) Foregut Carcinoids Thymic (2%) Bronchial (2%) Gastric (ECLoma) (10%) Adrenal Gland Non-functioning (20%)
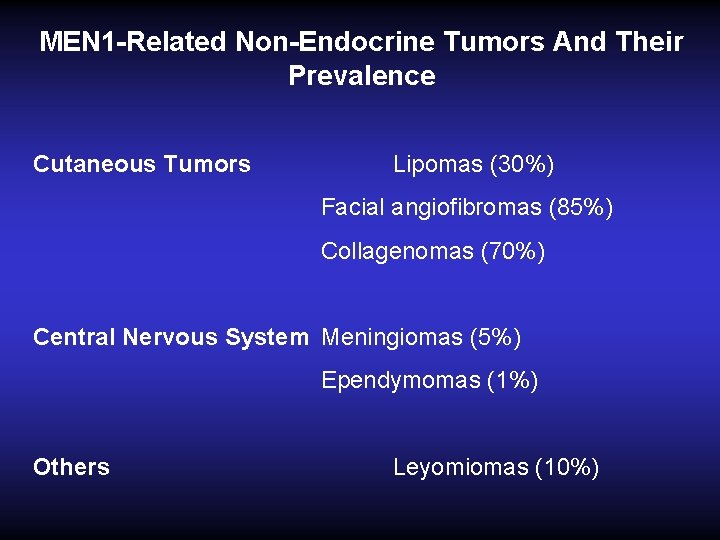
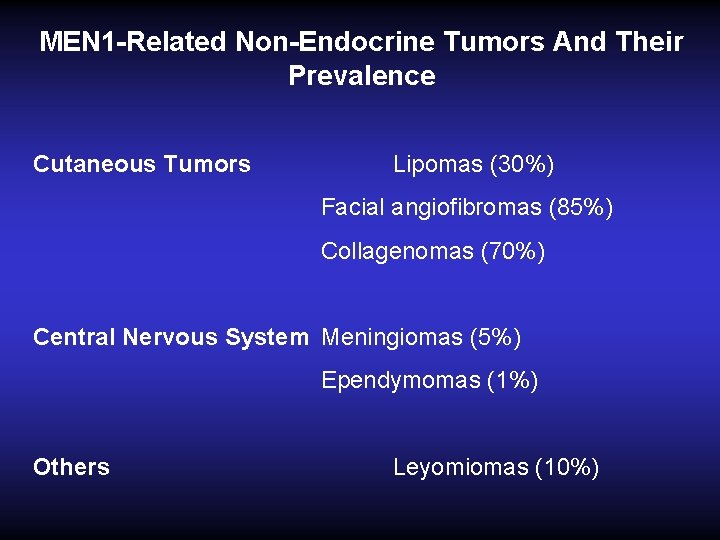
MEN 1 -Related Non-Endocrine Tumors And Their Prevalence Cutaneous Tumors Lipomas (30%) Facial angiofibromas (85%) Collagenomas (70%) Central Nervous System Meningiomas (5%) Ependymomas (1%) Others Leyomiomas (10%)
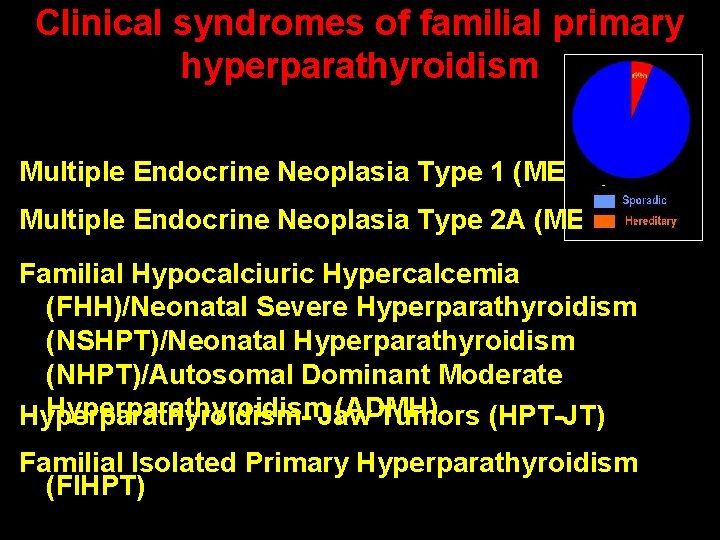
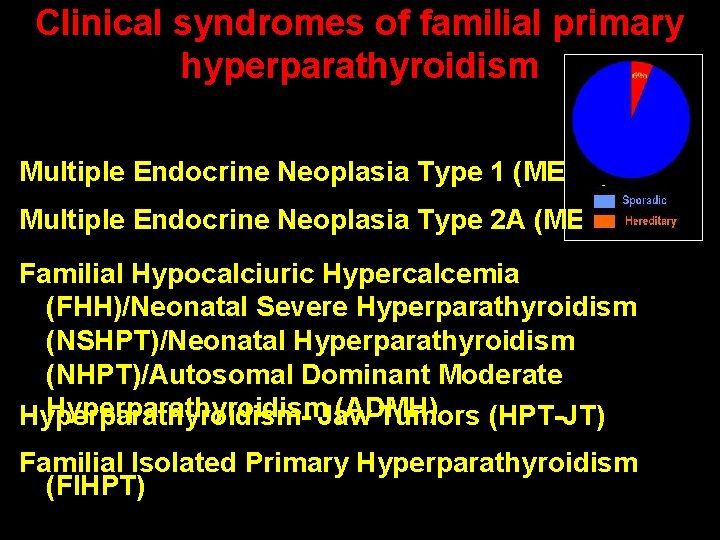
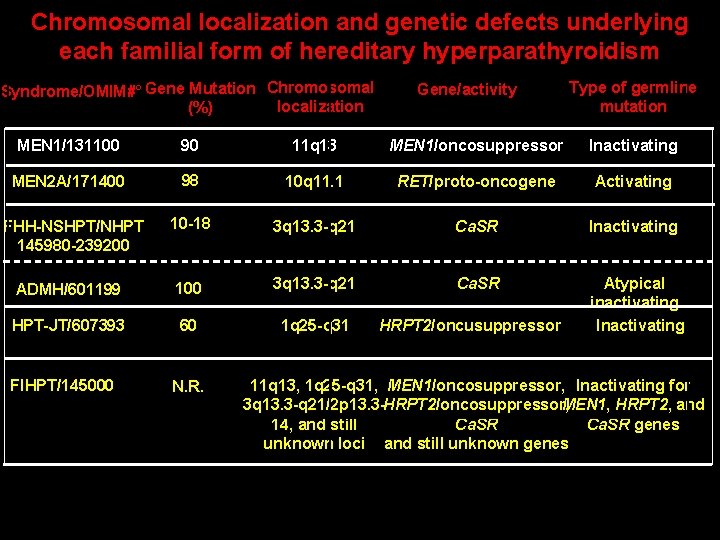
Clinical syndromes of familial primary hyperparathyroidism Multiple Endocrine Neoplasia Type 1 (MEN 1) Multiple Endocrine Neoplasia Type 2 A (MEN 2 A) Familial Hypocalciuric Hypercalcemia (FHH)/Neonatal Severe Hyperparathyroidism (NSHPT)/Neonatal Hyperparathyroidism (NHPT)/Autosomal Dominant Moderate Hyperparathyroidism (ADMH) Hyperparathyroidism- Jaw Tumors (HPT-JT) Familial Isolated Primary Hyperparathyroidism (FIHPT)
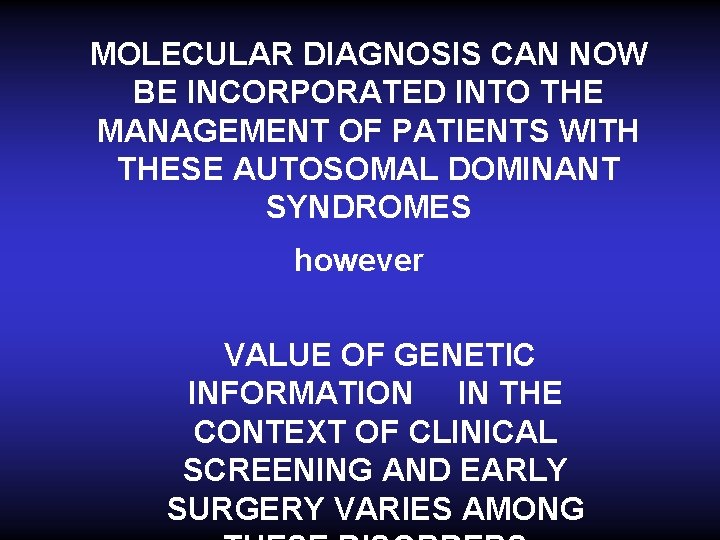
MOLECULAR DIAGNOSIS CAN NOW BE INCORPORATED INTO THE MANAGEMENT OF PATIENTS WITH THESE AUTOSOMAL DOMINANT SYNDROMES however VALUE OF GENETIC INFORMATION IN THE CONTEXT OF CLINICAL SCREENING AND EARLY SURGERY VARIES AMONG
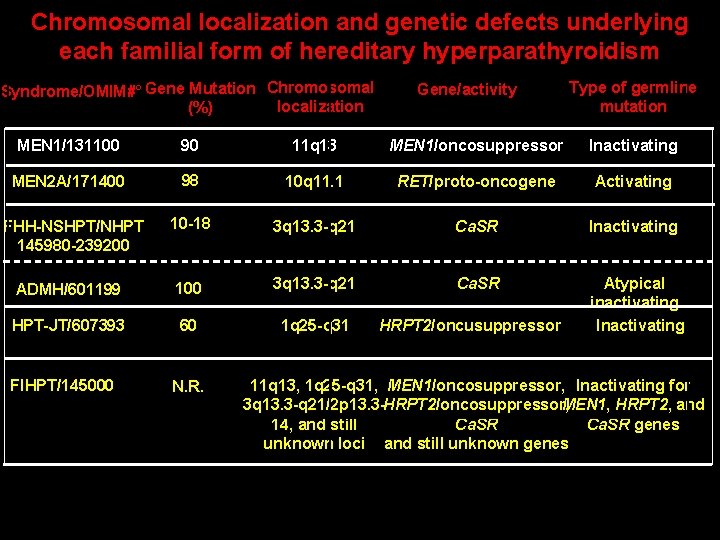
Chromosomal localization and genetic defects underlying each familial form of hereditary hyperparathyroidism Syndrome/OMIM#° Gene Mutation Chromosomal localization (%) Gene/activity Type of germline mutation MEN 1/131100 90 11 q 13 MEN 1/oncosuppressor Inactivating MEN 2 A/171400 98 10 q 11. 1 RET/proto-oncogene Activating 10 -18 3 q 13. 3 -q 21 Ca. SR Inactivating ADMH/601199 100 3 q 13. 3 -q 21 Ca. SR HPT-JT/607393 60 1 q 25 -q 31 Atypical inactivating Inactivating FHH-NSHPT/NHPT 145980 -239200 FIHPT/145000 N. R. HRPT 2/oncusuppressor 11 q 13, 1 q 25 -q 31, MEN 1/oncosuppressor, Inactivating for 3 q 13. 3 -q 21/2 p 13. 3 -HRPT 2/oncosuppressor, MEN 1, HRPT 2, and 14, and still Ca. SR genes unknown loci and still unknown genes
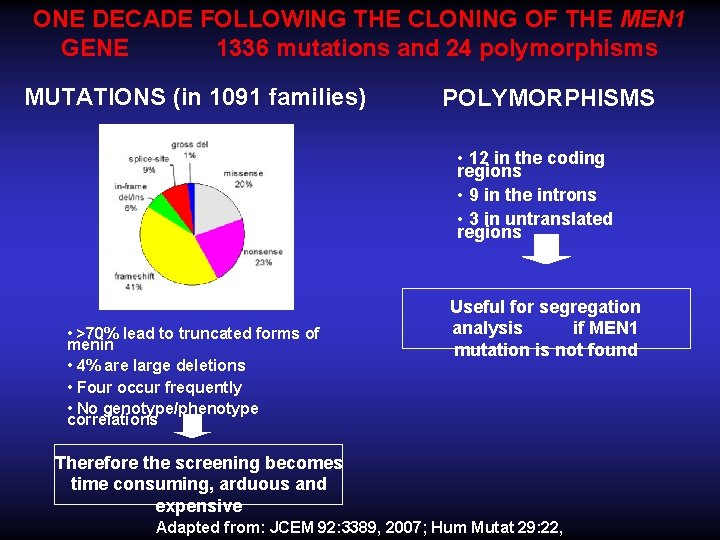
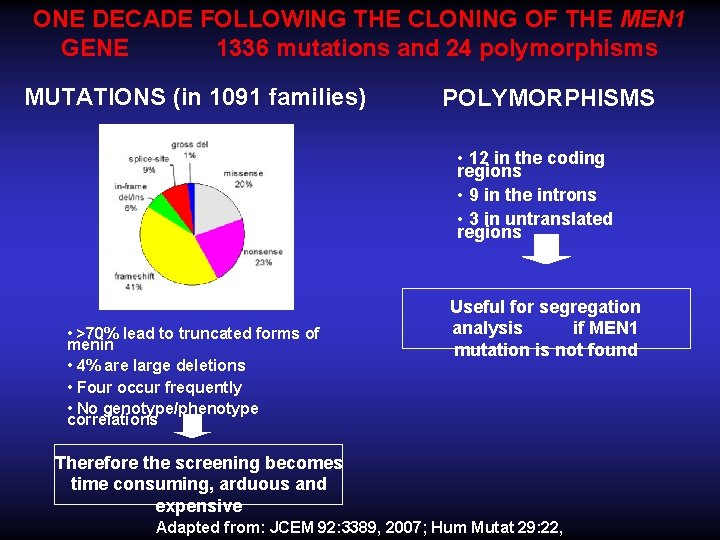
ONE DECADE FOLLOWING THE CLONING OF THE MEN 1 GENE 1336 mutations and 24 polymorphisms MUTATIONS (in 1091 families) POLYMORPHISMS • 12 in the coding regions • 9 in the introns • 3 in untranslated regions • >70% lead to truncated forms of menin • 4% are large deletions • Four occur frequently • No genotype/phenotype correlations Useful for segregation analysis if MEN 1 mutation is not found Therefore the screening becomes time consuming, arduous and expensive Adapted from: JCEM 92: 3389, 2007; Hum Mutat 29: 22,
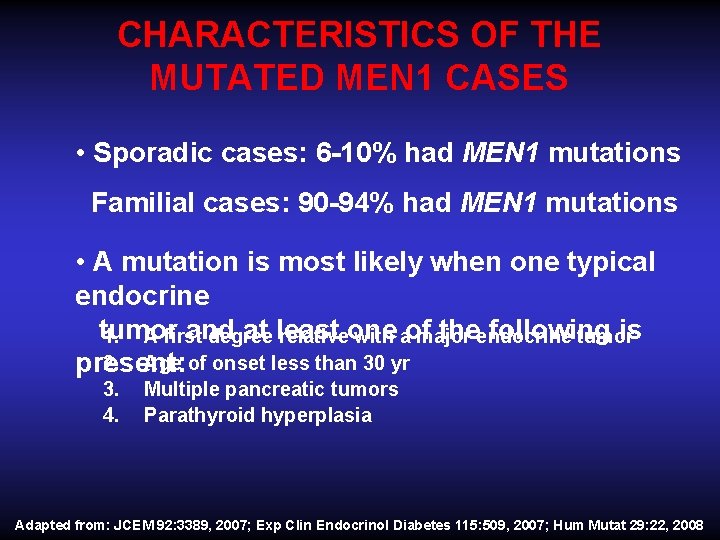
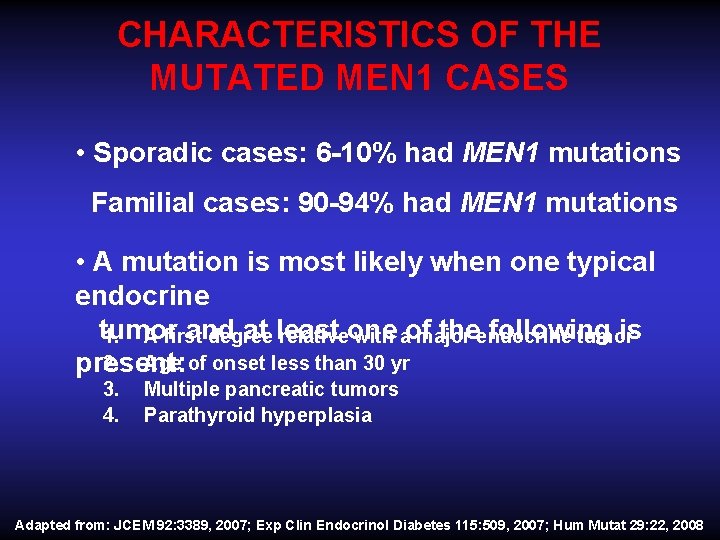
CHARACTERISTICS OF THE MUTATED MEN 1 CASES • Sporadic cases: 6 -10% had MEN 1 mutations Familial cases: 90 -94% had MEN 1 mutations • A mutation is most likely when one typical endocrine tumor and at least one of the following is 1. A first degree relative with a major endocrine tumor 2. Age of onset less than 30 yr present: 3. Multiple pancreatic tumors 4. Parathyroid hyperplasia Adapted from: JCEM 92: 3389, 2007; Exp Clin Endocrinol Diabetes 115: 509, 2007; Hum Mutat 29: 22, 2008
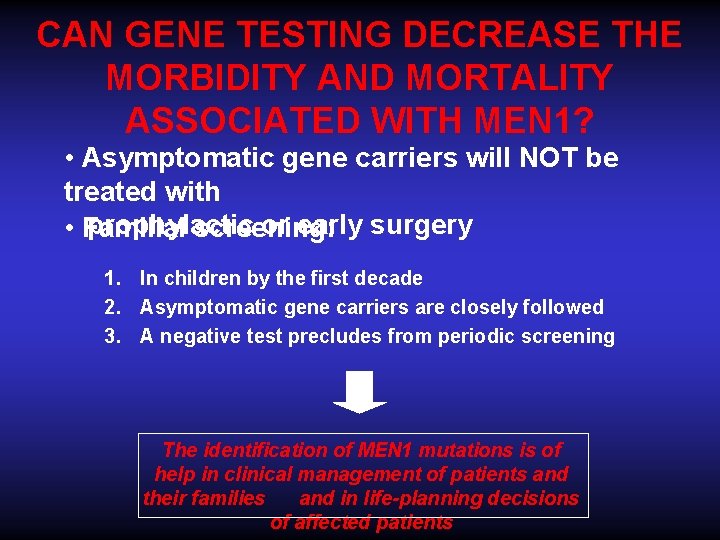
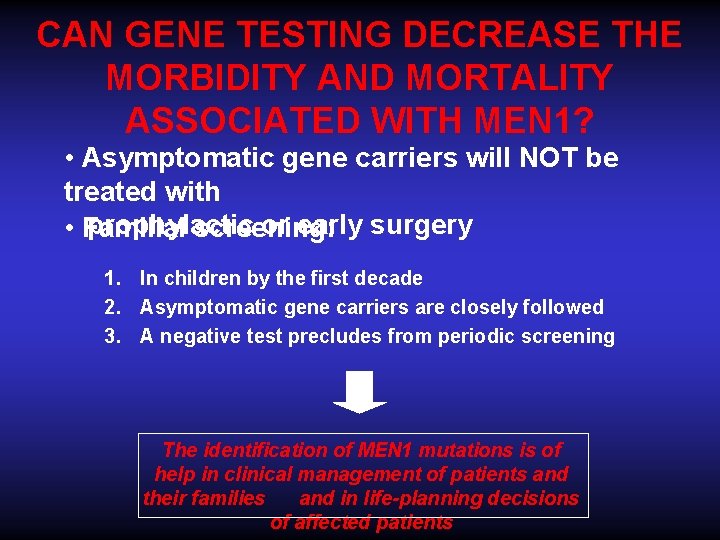
CAN GENE TESTING DECREASE THE MORBIDITY AND MORTALITY ASSOCIATED WITH MEN 1? • Asymptomatic gene carriers will NOT be treated with • prophylactic or early surgery Familial screening: 1. In children by the first decade 2. Asymptomatic gene carriers are closely followed 3. A negative test precludes from periodic screening The identification of MEN 1 mutations is of help in clinical management of patients and their families and in life-planning decisions of affected patients
J Clin Endocrinol Metab, September 2012, 97(9): 2990– 3011
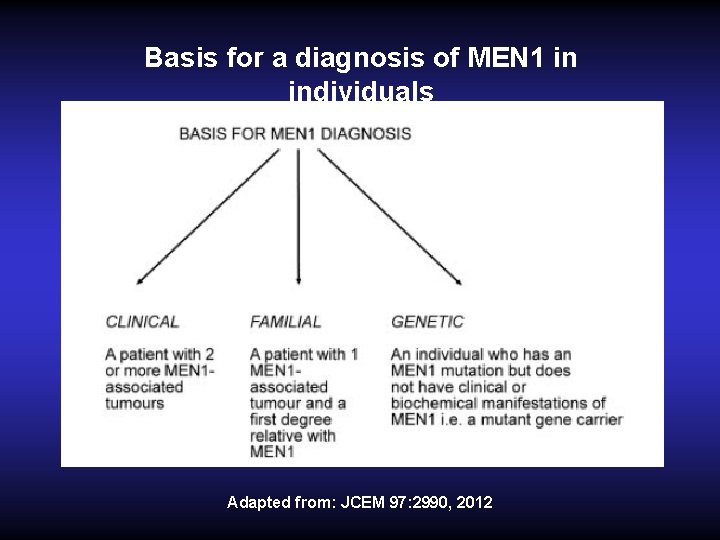
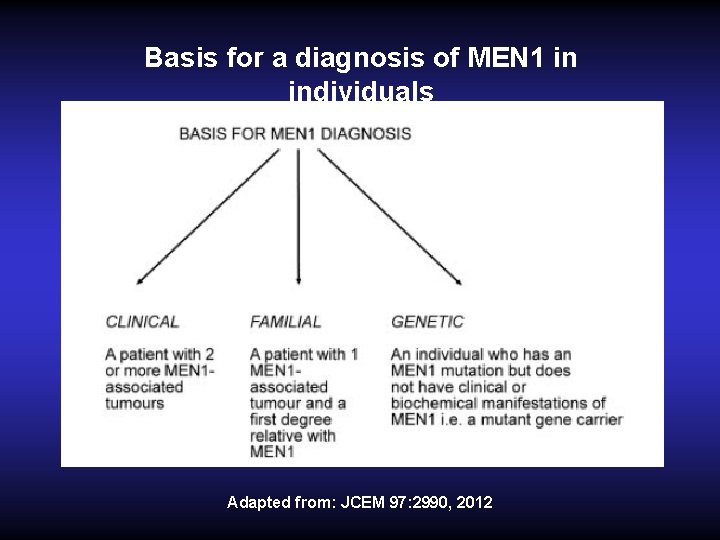
Basis for a diagnosis of MEN 1 in individuals Adapted from: JCEM 97: 2990, 2012
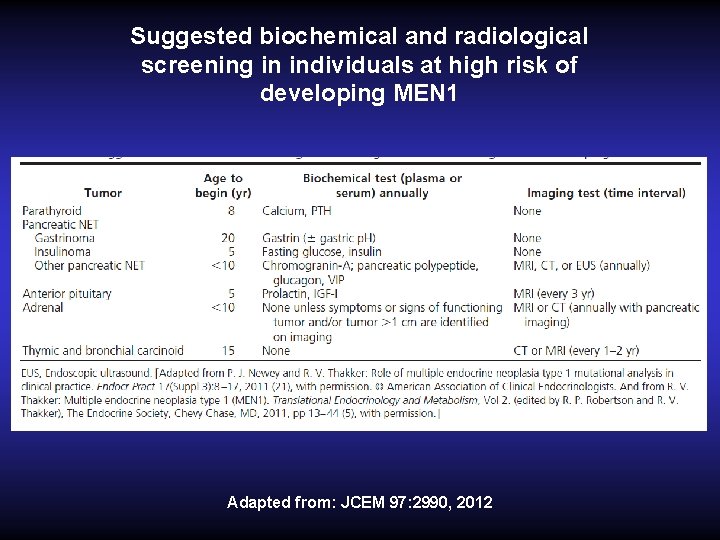
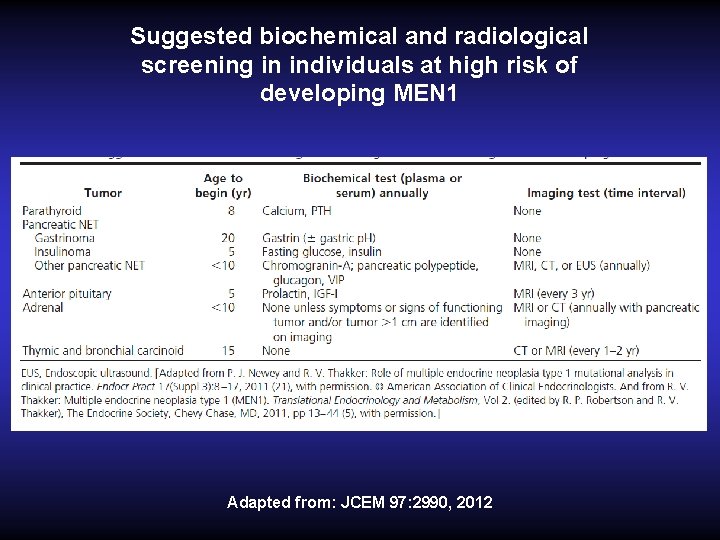
Suggested biochemical and radiological screening in individuals at high risk of developing MEN 1 Adapted from: JCEM 97: 2990, 2012
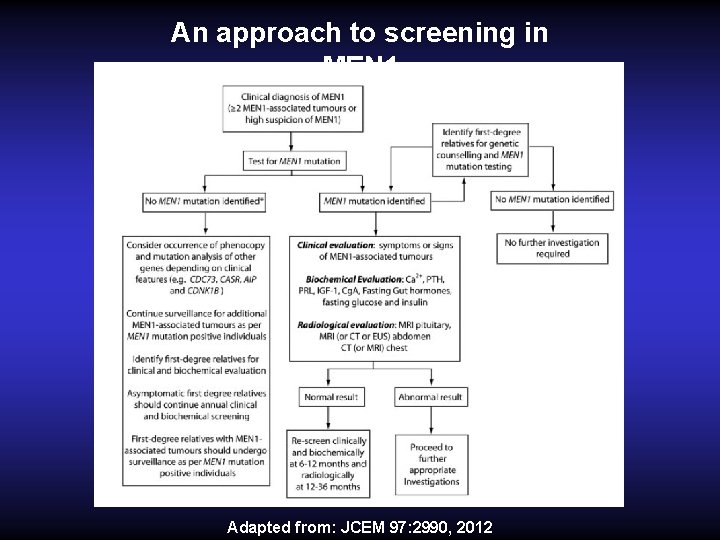
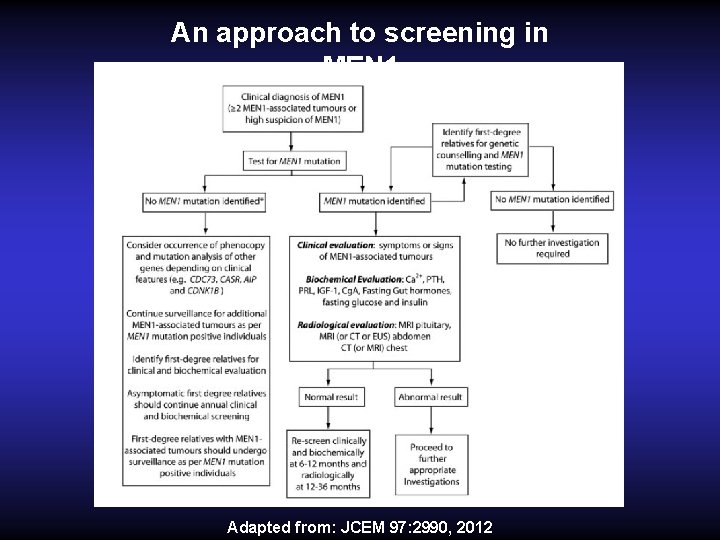
An approach to screening in MEN 1 Adapted from: JCEM 97: 2990, 2012
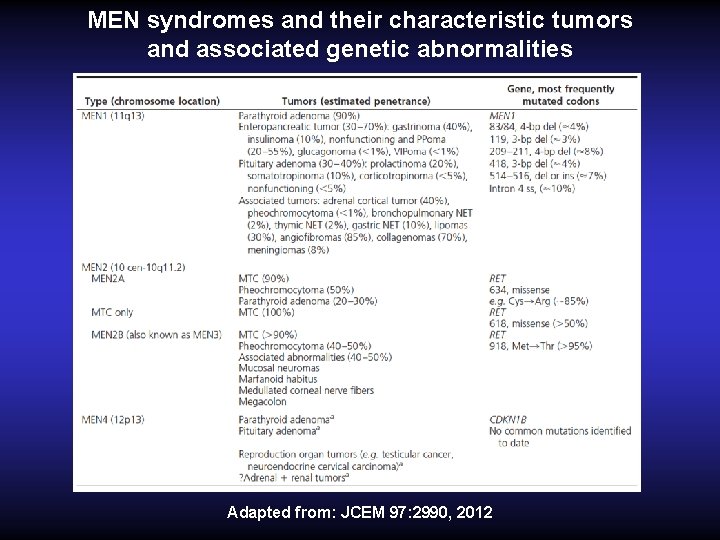
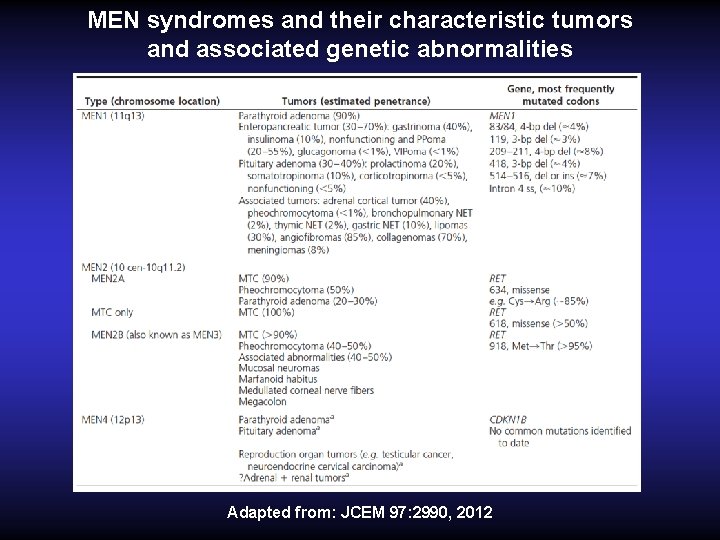
MEN syndromes and their characteristic tumors and associated genetic abnormalities Adapted from: JCEM 97: 2990, 2012
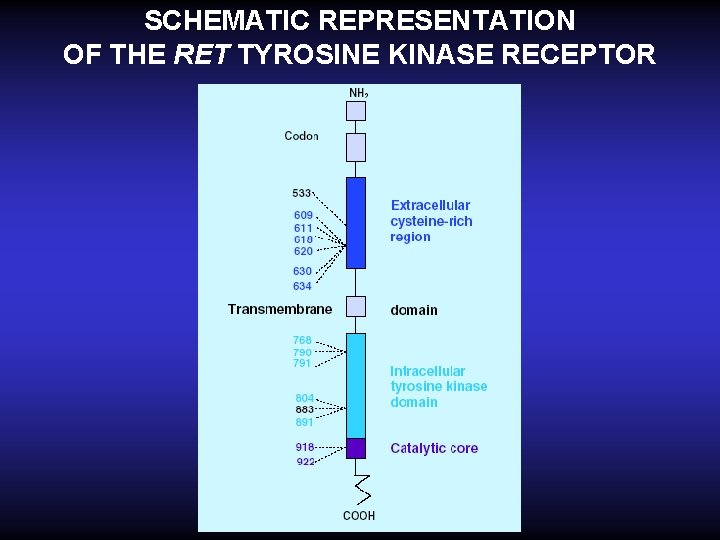
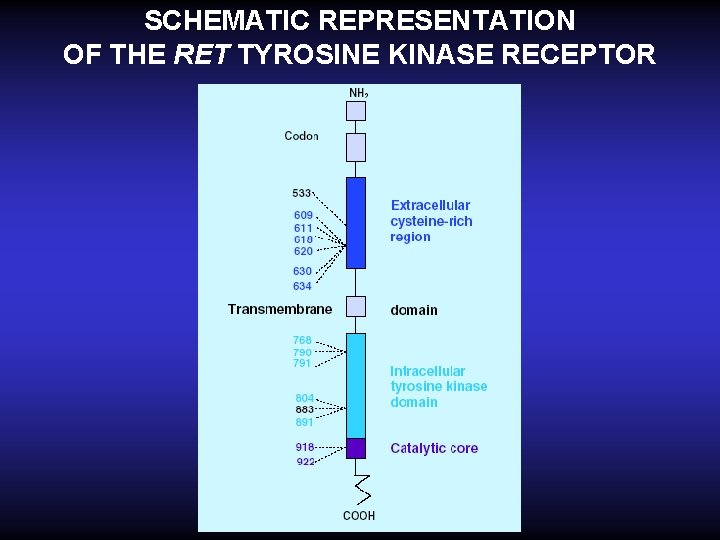
SCHEMATIC REPRESENTATION OF THE RET TYROSINE KINASE RECEPTOR

ALL THE MEN 2 VARIANTS ARE CAUSED BY RET GERMLINE MUTATION Stratification risk according to RET mutation • codons 883, 918, 922 (exons 15, 16) MEN 2 B highest risk for aggressive MTC; operated on within the first 6 months • codons 611, 618, 620, 634 (exons 10, 11) MEN 2 A/FMTC intermediate risk; thyroidectomy performed before the age of 5 yr. • codons 609, 768, 790, 791 804, 891 (exons 10, 13, 14, 15) MEN 2 A/FMTC lower risk; operated on at a later stage
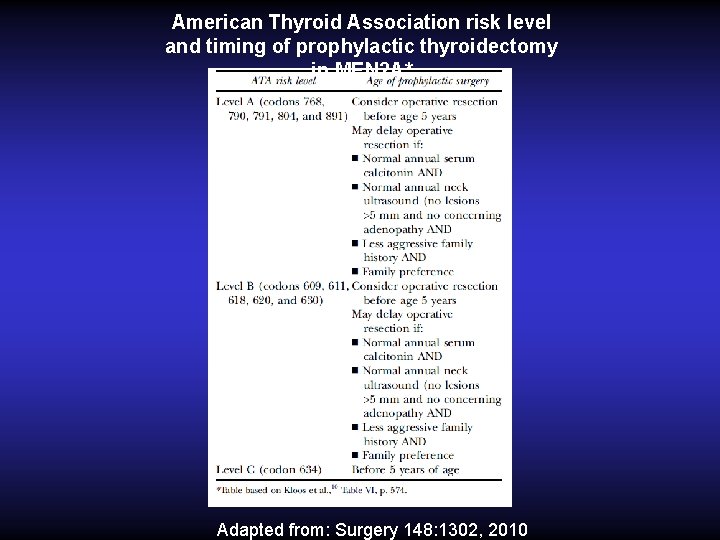
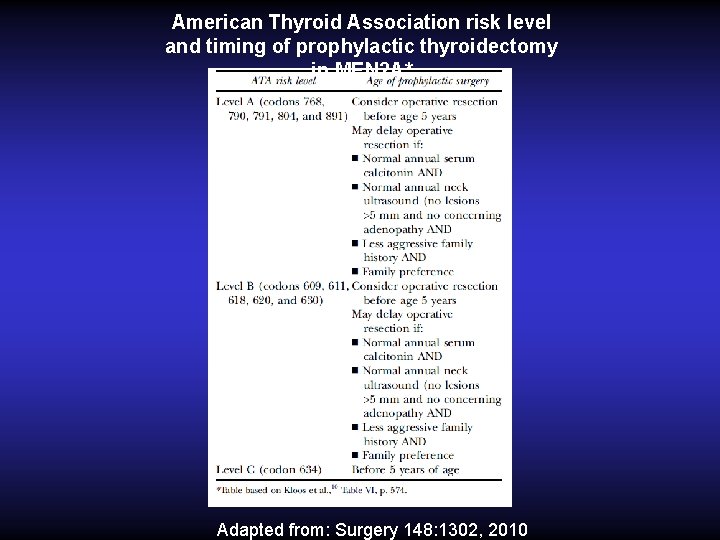
American Thyroid Association risk level and timing of prophylactic thyroidectomy in MEN 2 A* Adapted from: Surgery 148: 1302, 2010
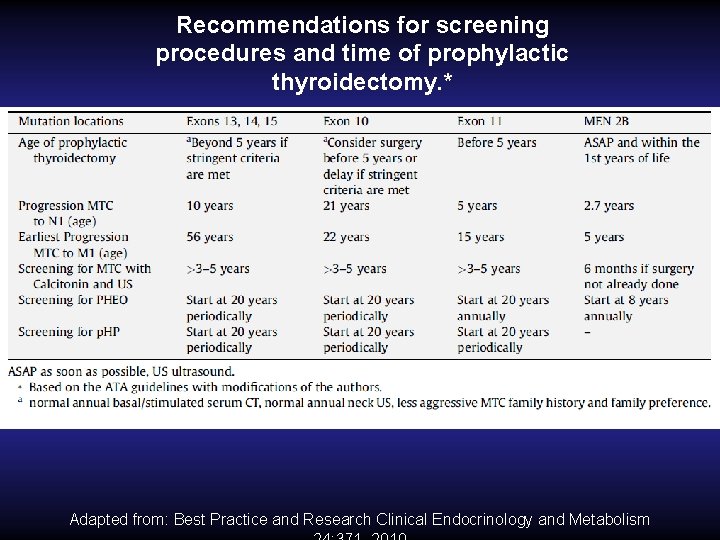
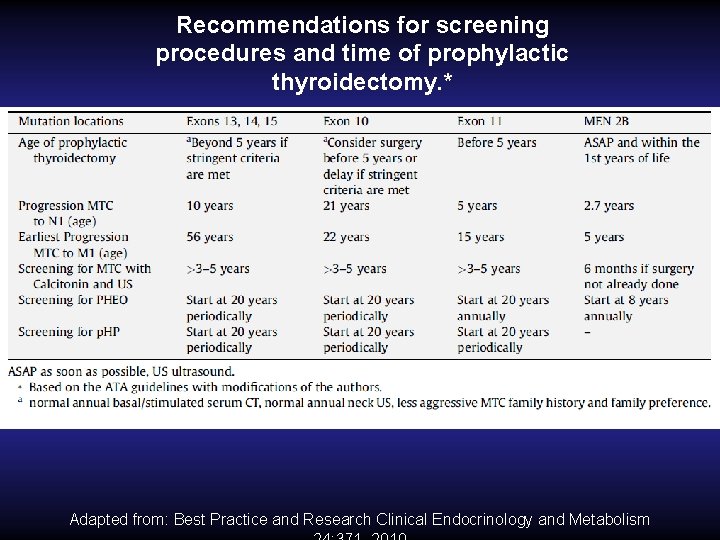
Recommendations for screening procedures and time of prophylactic thyroidectomy. * Adapted from: Best Practice and Research Clinical Endocrinology and Metabolism
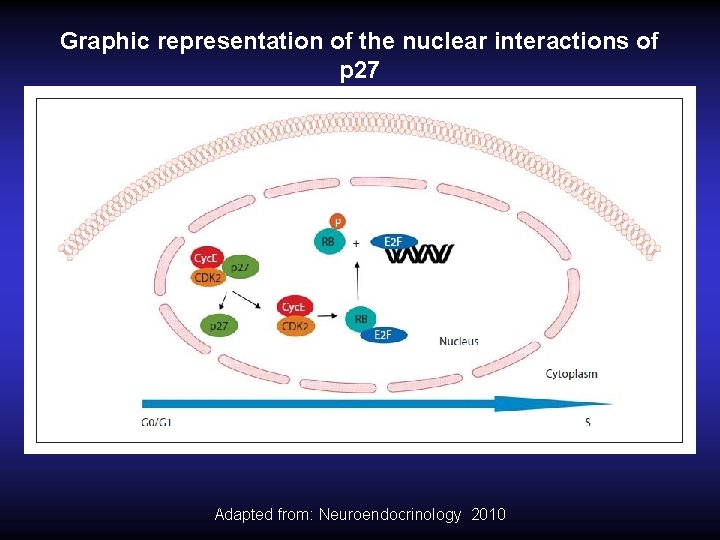
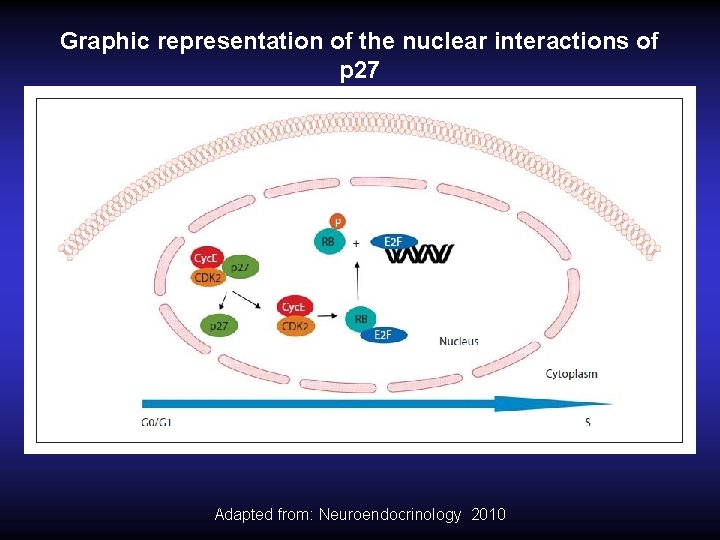
Graphic representation of the nuclear interactions of p 27 Adapted from: Neuroendocrinology 2010
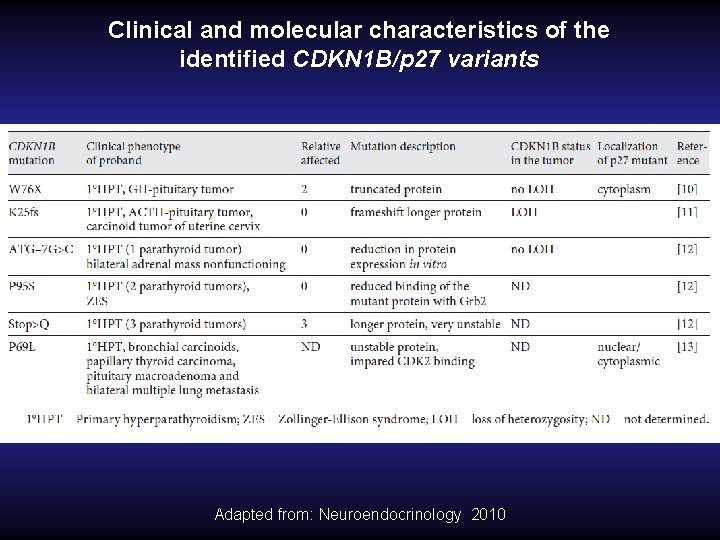
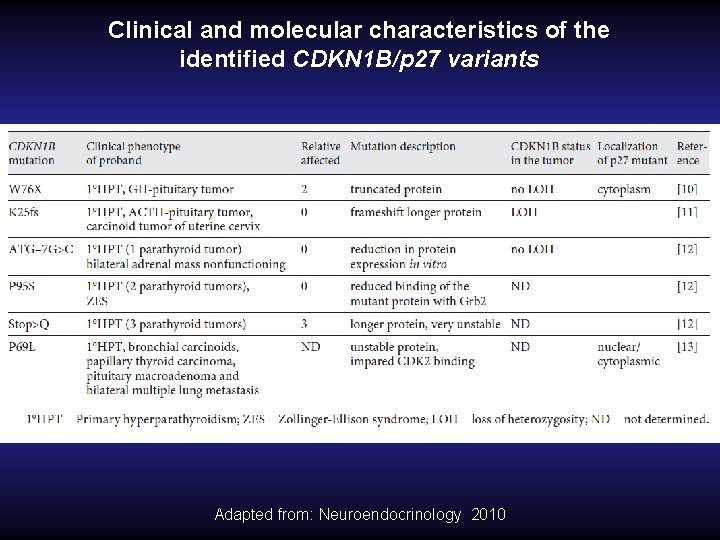
Clinical and molecular characteristics of the identified CDKN 1 B/p 27 variants Adapted from: Neuroendocrinology 2010
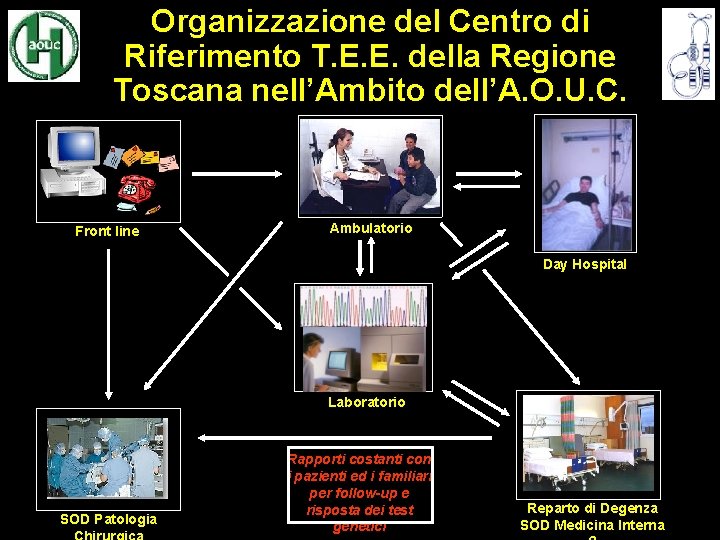
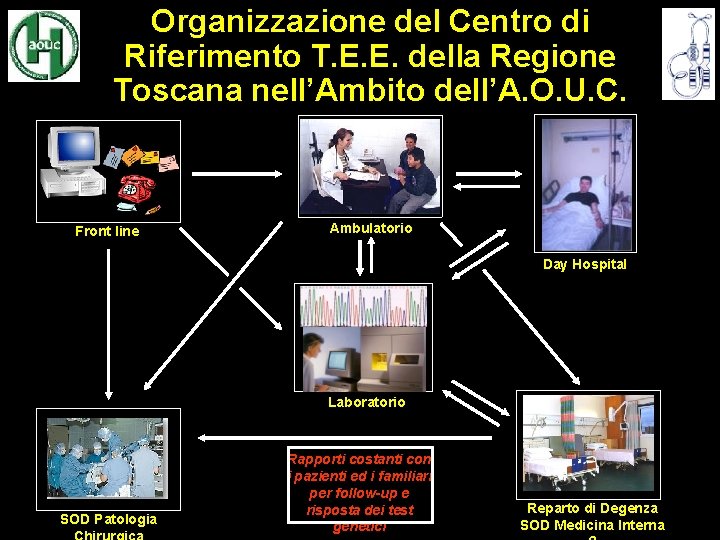
Organizzazione del Centro di Riferimento T. E. E. della Regione Toscana nell’Ambito dell’A. O. U. C. Front line Ambulatorio Day Hospital Laboratorio SOD Patologia Rapporti costanti con i pazienti ed i familiari per follow-up e risposta dei test genetici Reparto di Degenza SOD Medicina Interna
 Multiple endocrine neoplasia type 2
Multiple endocrine neoplasia type 2 Willis definition of neoplasia
Willis definition of neoplasia Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology What is geriatric syndromes
What is geriatric syndromes Neuroendocrine syndromes in gynecology
Neuroendocrine syndromes in gynecology Brainstem stroke syndromes
Brainstem stroke syndromes Anatonomina
Anatonomina Cerebellar syndromes
Cerebellar syndromes Clinical features of neoplasia
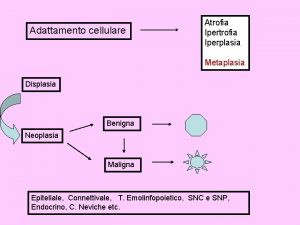
Clinical features of neoplasia Neoplasia
Neoplasia Neoplasia
Neoplasia Malignancy
Malignancy Malignant neoplasm
Malignant neoplasm Cin
Cin Malacoplachia
Malacoplachia Glandula mamária
Glandula mamária Enfermedades de la vulva
Enfermedades de la vulva Adenocarcinoma
Adenocarcinoma Que es una neoplasia
Que es una neoplasia Neoplasia literally means
Neoplasia literally means Valsava
Valsava Vaginal neoplasia
Vaginal neoplasia Best case worst case average case
Best case worst case average case Multiple baseline vs multiple probe design
Multiple baseline vs multiple probe design Multiple instruction multiple data
Multiple instruction multiple data