Clinical Trials Scientific Aspects AND Legal Procedural Aspects
![Clinical Trials Scientific Aspects AND Legal & Procedural Aspects M K Unnikrishnan [Aug 2006] Clinical Trials Scientific Aspects AND Legal & Procedural Aspects M K Unnikrishnan [Aug 2006]](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-1.jpg)
![Phase II • First in patient [ different from healthy volunteer] • Early phase Phase II • First in patient [ different from healthy volunteer] • Early phase](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-5.jpg)

![Functions of participating parties – [1] Patient / Healthy volunteer : Subject of the Functions of participating parties – [1] Patient / Healthy volunteer : Subject of the](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-11.jpg)
![Functions of parties contd. – [4] Ethical Review Board or Institutional Ethical Committee: – Functions of parties contd. – [4] Ethical Review Board or Institutional Ethical Committee: –](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-12.jpg)
- Slides: 18
![Clinical Trials Scientific Aspects AND Legal Procedural Aspects M K Unnikrishnan Aug 2006 Clinical Trials Scientific Aspects AND Legal & Procedural Aspects M K Unnikrishnan [Aug 2006]](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-1.jpg)
Clinical Trials Scientific Aspects AND Legal & Procedural Aspects M K Unnikrishnan [Aug 2006]
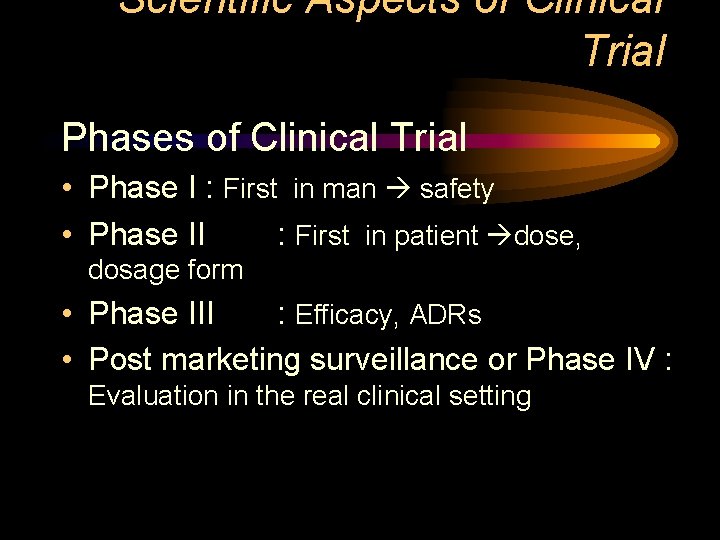
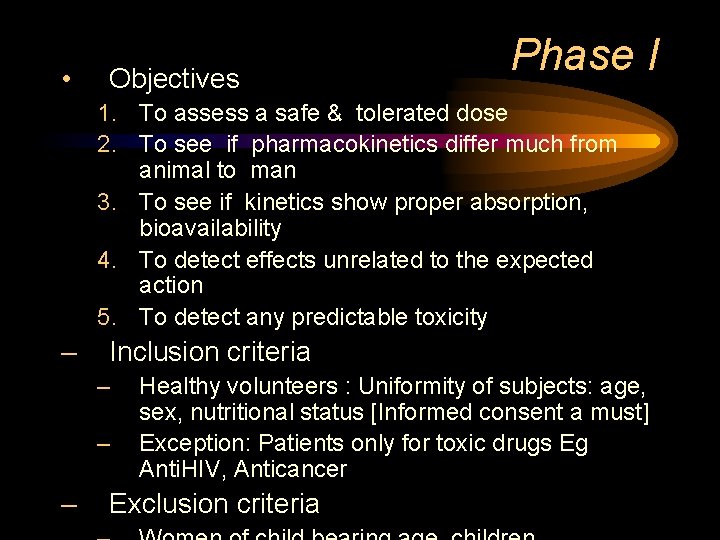
Scientific Aspects of Clinical Trial Phases of Clinical Trial • Phase I : First in man safety • Phase II : First in patient dose, dosage form • Phase III : Efficacy, ADRs • Post marketing surveillance or Phase IV : Evaluation in the real clinical setting
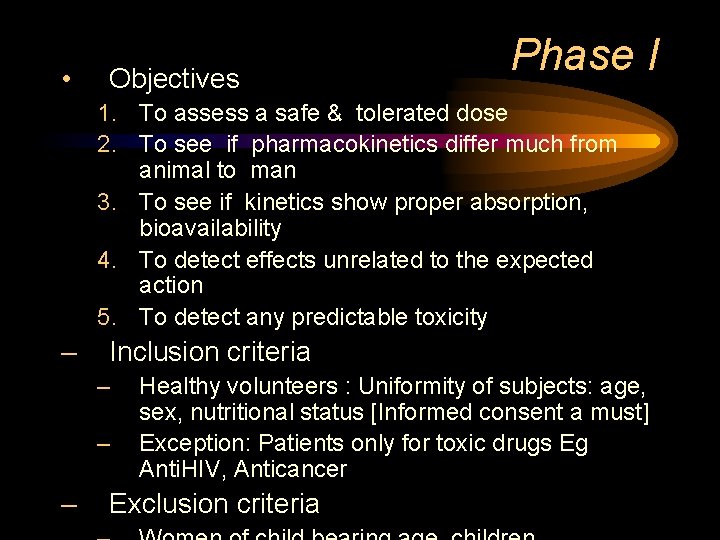
• Objectives Phase I 1. To assess a safe & tolerated dose 2. To see if pharmacokinetics differ much from animal to man 3. To see if kinetics show proper absorption, bioavailability 4. To detect effects unrelated to the expected action 5. To detect any predictable toxicity – Inclusion criteria – – – Healthy volunteers : Uniformity of subjects: age, sex, nutritional status [Informed consent a must] Exception: Patients only for toxic drugs Eg Anti. HIV, Anticancer Exclusion criteria
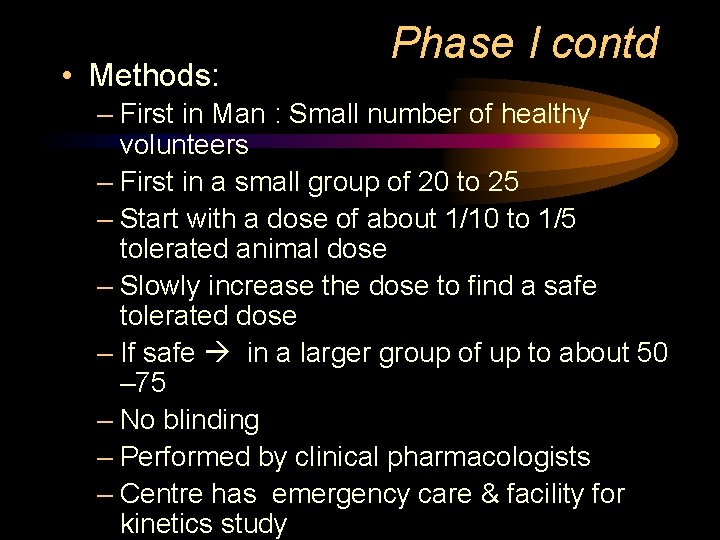
• Methods: Phase I contd – First in Man : Small number of healthy volunteers – First in a small group of 20 to 25 – Start with a dose of about 1/10 to 1/5 tolerated animal dose – Slowly increase the dose to find a safe tolerated dose – If safe in a larger group of up to about 50 – 75 – No blinding – Performed by clinical pharmacologists – Centre has emergency care & facility for kinetics study
![Phase II First in patient different from healthy volunteer Early phase Phase II • First in patient [ different from healthy volunteer] • Early phase](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-5.jpg)
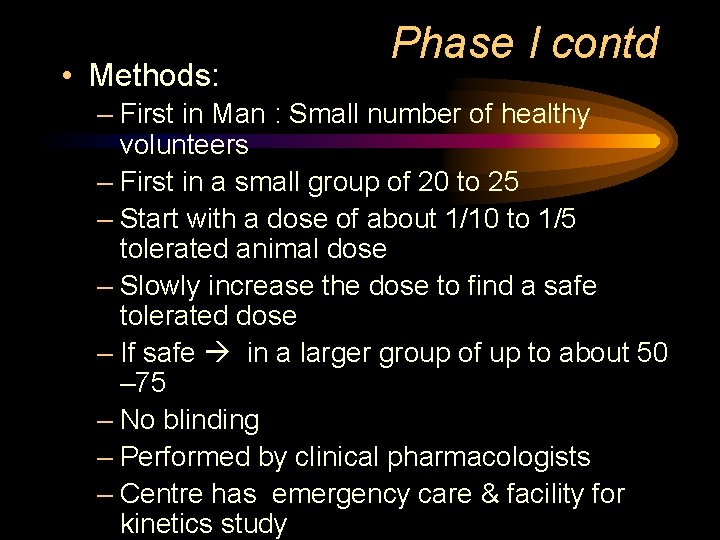
Phase II • First in patient [ different from healthy volunteer] • Early phase [20 – 200 patients with relevant disease] – Therapeutic benefits & ADRs evaluated – Establish a dose range to be used in late phase – Single blind [Only patient knows] comparison with standard drug • Late phase [ 50 – 500] – Double blind – Compared with a placebo or standard drug • Outcomes – Assesses efficacy against a defined therapeutic endpoint – Detailed P. kinetic & P. dynamic data
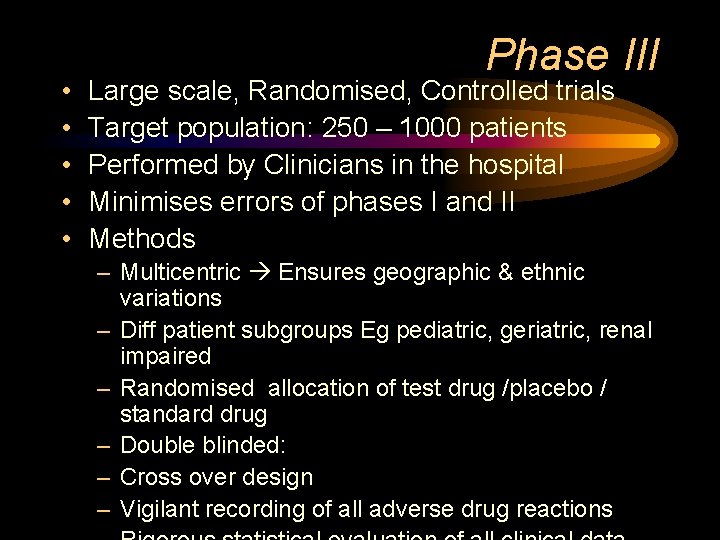
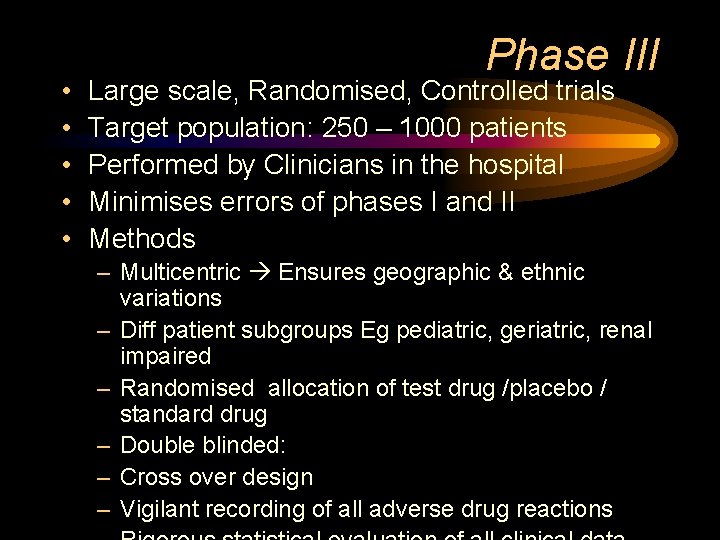
• • • Phase III Large scale, Randomised, Controlled trials Target population: 250 – 1000 patients Performed by Clinicians in the hospital Minimises errors of phases I and II Methods – Multicentric Ensures geographic & ethnic variations – Diff patient subgroups Eg pediatric, geriatric, renal impaired – Randomised allocation of test drug /placebo / standard drug – Double blinded: – Cross over design – Vigilant recording of all adverse drug reactions

Cross over design Group I II III Week 1 Standard Placebo Test Week 2 Placebo Test Standard Week 3 Test Standard Placebo * A wash out period of a week between two weeks of therapy
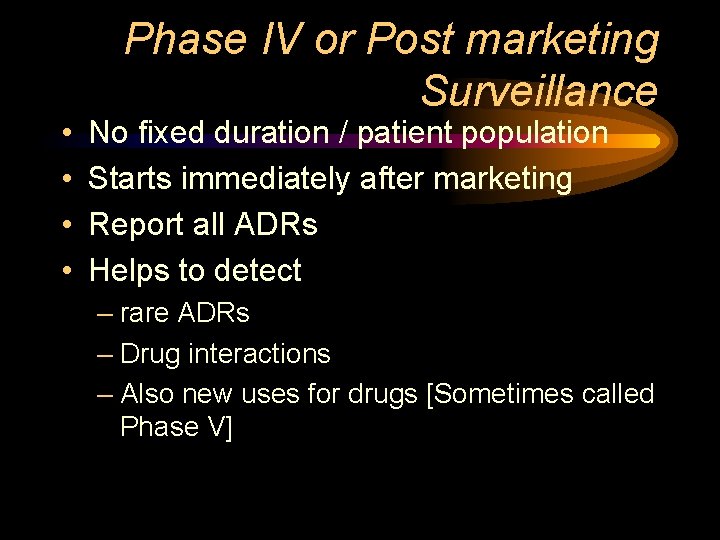
• • Phase IV or Post marketing Surveillance No fixed duration / patient population Starts immediately after marketing Report all ADRs Helps to detect – rare ADRs – Drug interactions – Also new uses for drugs [Sometimes called Phase V]
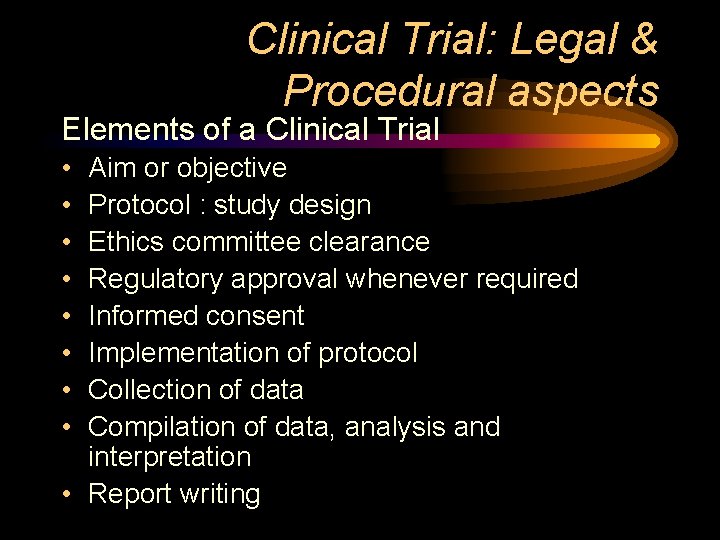
Clinical Trial: Legal & Procedural aspects Elements of a Clinical Trial • • Aim or objective Protocol : study design Ethics committee clearance Regulatory approval whenever required Informed consent Implementation of protocol Collection of data Compilation of data, analysis and interpretation • Report writing
Participating Parties in Clinical Trial 1. Patient / Healthy volunteer 2. Clinical Pharmacologist, Clinical Investigator & team: [Qualified and competent] 3. Institution where trials are held : [Approval required] 4. Ethical Review Board or Institutional Ethical Committee: 5. Sponsor 6. Regulatory Authorities:
![Functions of participating parties 1 Patient Healthy volunteer Subject of the Functions of participating parties – [1] Patient / Healthy volunteer : Subject of the](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-11.jpg)
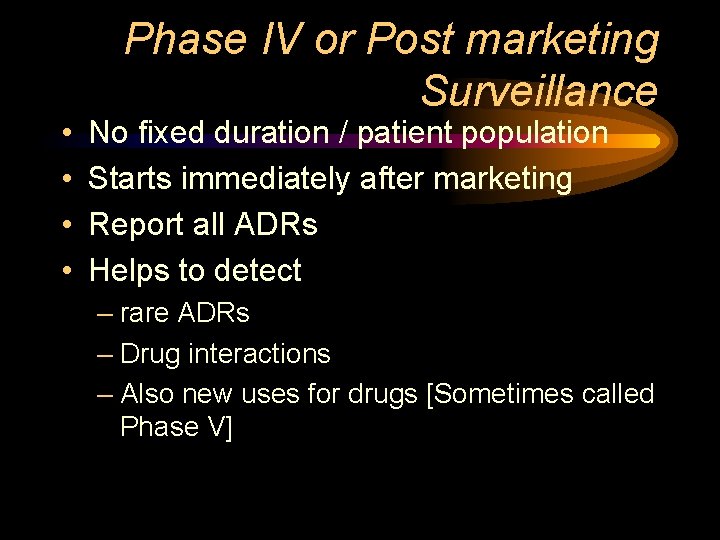
Functions of participating parties – [1] Patient / Healthy volunteer : Subject of the trial – [2] Clinical Pharmacologist, Clinical Investigator & team: – Conducts the clinical trial; reports all adverse events – [3] Institution where trials are held : – Provides all facilities [Approval required]
![Functions of parties contd 4 Ethical Review Board or Institutional Ethical Committee Functions of parties contd. – [4] Ethical Review Board or Institutional Ethical Committee: –](https://slidetodoc.com/presentation_image_h/b5239a81b5cbe6e7b5f061fbab53b71d/image-12.jpg)
Functions of parties contd. – [4] Ethical Review Board or Institutional Ethical Committee: – Supervises and monitors every step; – Safeguard the welfare and the rights of the participants – [5] Sponsor : – – Pays for all expenses; Appoints competent investigators, Ships all drugs for the trial, Files all papers to legal / regulatory authorities, – [6] Regulatory Authorities:
Clinical Trial Protocol • Title & Abstract • Introduction – – General statement of purpose Complete Preclinical results on animal study Clinical data if available Time frame • Goals: Primary & secondary objectives • Study Design: – – Type of study Recruitment criteria : Exclusion & Inclusion criteria Randomisation criteria and Sample size Duration of study • Data Analysis: – Case report forms, Statistical Analysis, Bibliography
Informed Consent • Informed consent form: – Voluntary – Explained in simple nontechnical language – Translated in the native language of the subject – Comprehensive information regarding the trials • Benefit of new therapy over existing ones • Alternative treatments available – All possible adverse reactions – Freedom to withdraw from the trial • at any time,
Institutional Ethical Committee – Independent – Competent – 5 – 7 members; 5 required for quorum. – Member Sec from same Institution – Others: A mix of medical nonmedical, scientific & non-scientific including lay public – Multidisciplinary & Multisectorial
Responsibilities of IEC 1. To protect the dignity, rights & well being of patients / volunteers 2. Ensure a competent review of the protocol 3. Advise on all aspects of welfare & safety 4. Ensure scientific soundness of the proposal
The composition of IEC 1. 2. 3. 4. 5. 6. 7. 8. Chairperson 1 -2 basic medical scientists. 1 -2 clinicians from various Institutes One legal expert or retired judge One social scientist / representative of NGO One philosopher / ethicist / theologian One lay person from the community Member Secretary – Individuals from other institutions if required – Adequate representation of age, gender, community,
Problem areas • Compensation in drug related injuries – Mild and Severe • Patient Rights – Confidentiality of data – Right to withdraw • Collection procedures & amount of biological material taken • Compensation & Insurance claims • Sending bio-material abroad • Selection of Patients
 Phs human subjects and clinical trials information
Phs human subjects and clinical trials information Difference between inspection and audit
Difference between inspection and audit Nida clinical trials network
Nida clinical trials network Site initiation visit powerpoint presentation
Site initiation visit powerpoint presentation Clinical trials.gov api
Clinical trials.gov api Role of statistician in clinical trials
Role of statistician in clinical trials Mrc clinical trials unit
Mrc clinical trials unit Randomization
Randomization Mpn clinical trials
Mpn clinical trials Prs registration
Prs registration Clinical trials
Clinical trials Clinical trials quality by design
Clinical trials quality by design Mpn clinical trials
Mpn clinical trials Lej hub customs dhl
Lej hub customs dhl Clinical hysteria salem witch trials
Clinical hysteria salem witch trials Ohsu clinical trials office
Ohsu clinical trials office Protocol registration system
Protocol registration system Clinical trials.gov login
Clinical trials.gov login Iwr ivr clinical
Iwr ivr clinical