NIDA CLINICAL TRIALS NETWORK EXAMPLES OF COMMUNITY PROGRAM
- Slides: 1
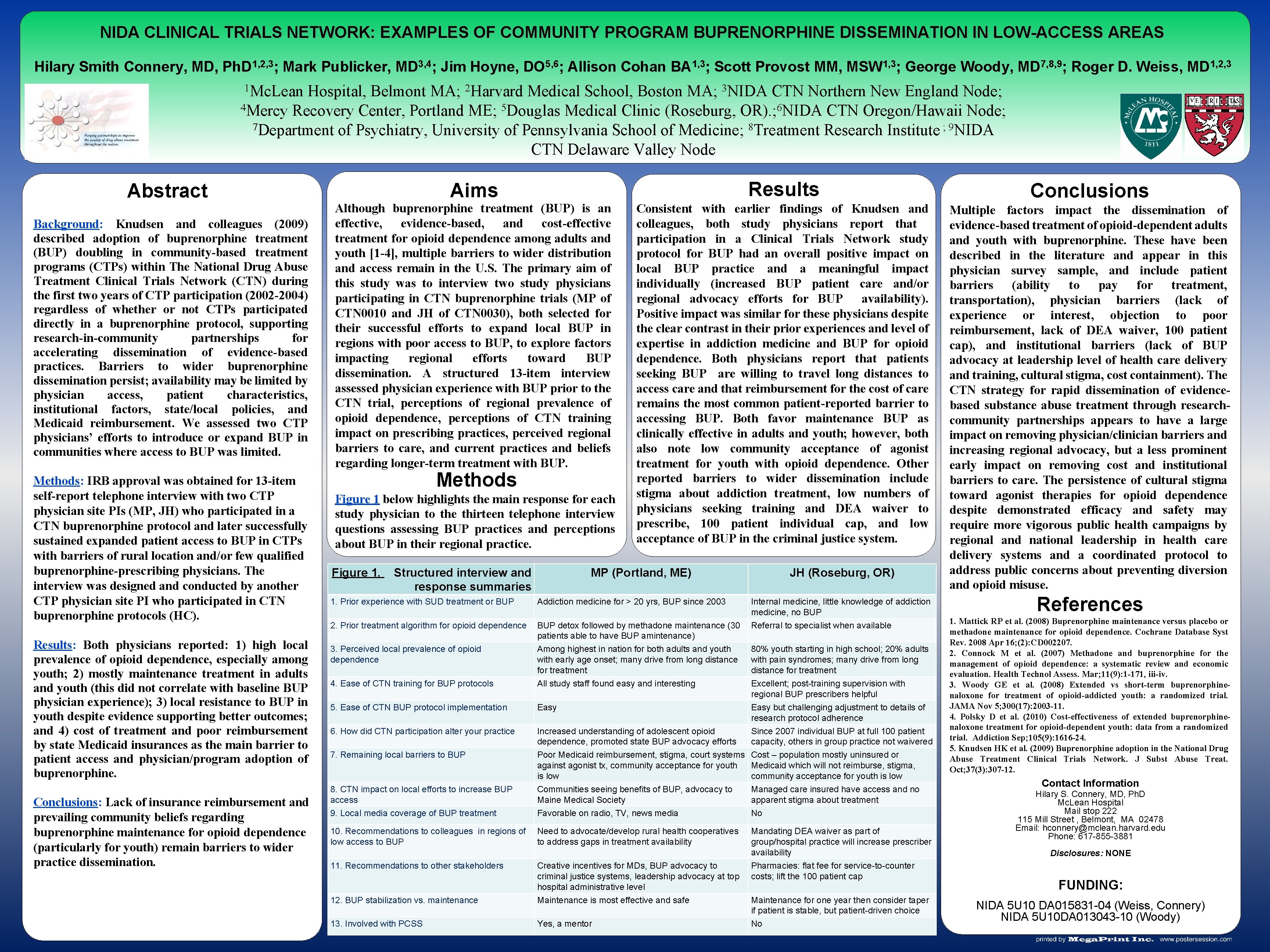
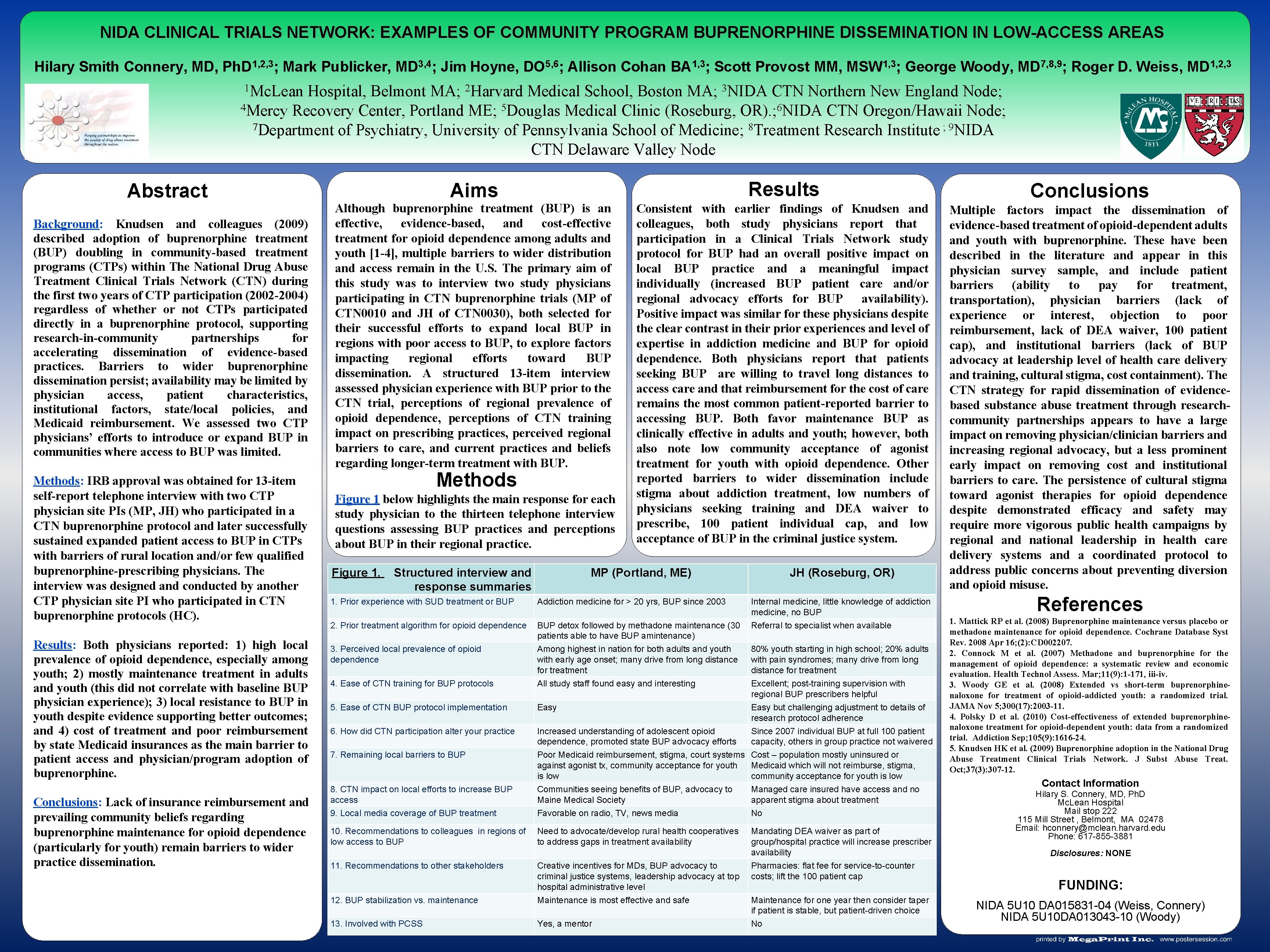
NIDA CLINICAL TRIALS NETWORK: EXAMPLES OF COMMUNITY PROGRAM BUPRENORPHINE DISSEMINATION IN LOW-ACCESS AREAS Hilary Smith Connery, MD, Ph. D 1, 2, 3; Mark Publicker, MD 3, 4; Jim Hoyne, DO 5, 6; Allison Cohan BA 1, 3; Scott Provost MM, MSW 1, 3; George Woody, MD 7, 8, 9; Roger D. Weiss, MD 1, 2, 3 1 Mc. Lean Hospital, Belmont MA; 2 Harvard Medical School, Boston MA; 3 NIDA CTN Northern New England Node; 4 Mercy Recovery Center, Portland ME; 5 Douglas Medical Clinic (Roseburg, OR). ; 6 NIDA CTN Oregon/Hawaii Node; 7 Department of Psychiatry, University of Pennsylvania School of Medicine; 8 Treatment Research Institute ; 9 NIDA CTN Delaware Valley Node Abstract Background: Knudsen and colleagues (2009) described adoption of buprenorphine treatment (BUP) doubling in community-based treatment programs (CTPs) within The National Drug Abuse Treatment Clinical Trials Network (CTN) during the first two years of CTP participation (2002 -2004) regardless of whether or not CTPs participated directly in a buprenorphine protocol, supporting research-in-community partnerships for accelerating dissemination of evidence-based practices. Barriers to wider buprenorphine dissemination persist; availability may be limited by physician access, patient characteristics, institutional factors, state/local policies, and Medicaid reimbursement. We assessed two CTP physicians’ efforts to introduce or expand BUP in communities where access to BUP was limited. Methods: IRB approval was obtained for 13 -item self-report telephone interview with two CTP physician site PIs (MP, JH) who participated in a CTN buprenorphine protocol and later successfully sustained expanded patient access to BUP in CTPs with barriers of rural location and/or few qualified buprenorphine-prescribing physicians. The interview was designed and conducted by another CTP physician site PI who participated in CTN buprenorphine protocols (HC). Results: Both physicians reported: 1) high local prevalence of opioid dependence, especially among youth; 2) mostly maintenance treatment in adults and youth (this did not correlate with baseline BUP physician experience); 3) local resistance to BUP in youth despite evidence supporting better outcomes; and 4) cost of treatment and poor reimbursement by state Medicaid insurances as the main barrier to patient access and physician/program adoption of buprenorphine. Conclusions: Lack of insurance reimbursement and prevailing community beliefs regarding buprenorphine maintenance for opioid dependence (particularly for youth) remain barriers to wider practice dissemination. Results Aims Although buprenorphine treatment (BUP) is an effective, evidence-based, and cost-effective treatment for opioid dependence among adults and youth [1 -4], multiple barriers to wider distribution and access remain in the U. S. The primary aim of this study was to interview two study physicians participating in CTN buprenorphine trials (MP of CTN 0010 and JH of CTN 0030), both selected for their successful efforts to expand local BUP in regions with poor access to BUP, to explore factors impacting regional efforts toward BUP dissemination. A structured 13 -item interview assessed physician experience with BUP prior to the CTN trial, perceptions of regional prevalence of opioid dependence, perceptions of CTN training impact on prescribing practices, perceived regional barriers to care, and current practices and beliefs regarding longer-term treatment with BUP. Methods Figure 1 below highlights the main response for each study physician to the thirteen telephone interview questions assessing BUP practices and perceptions about BUP in their regional practice. Figure 1. Structured interview and response summaries Consistent with earlier findings of Knudsen and colleagues, both study physicians report that participation in a Clinical Trials Network study protocol for BUP had an overall positive impact on local BUP practice and a meaningful impact individually (increased BUP patient care and/or regional advocacy efforts for BUP availability). Positive impact was similar for these physicians despite the clear contrast in their prior experiences and level of expertise in addiction medicine and BUP for opioid dependence. Both physicians report that patients seeking BUP are willing to travel long distances to access care and that reimbursement for the cost of care remains the most common patient-reported barrier to accessing BUP. Both favor maintenance BUP as clinically effective in adults and youth; however, both also note low community acceptance of agonist treatment for youth with opioid dependence. Other reported barriers to wider dissemination include stigma about addiction treatment, low numbers of physicians seeking training and DEA waiver to prescribe, 100 patient individual cap, and low acceptance of BUP in the criminal justice system. MP (Portland, ME) JH (Roseburg, OR) 1. Prior experience with SUD treatment or BUP Addiction medicine for > 20 yrs, BUP since 2003 2. Prior treatment algorithm for opioid dependence BUP detox followed by methadone maintenance (30 patients able to have BUP amintenance) 3. Perceived local prevalence of opioid dependence 4. Ease of CTN training for BUP protocols Among highest in nation for both adults and youth with early age onset; many drive from long distance for treatment All study staff found easy and interesting 80% youth starting in high school; 20% adults with pain syndromes; many drive from long distance for treatment Excellent; post-training supervision with regional BUP prescribers helpful 5. Ease of CTN BUP protocol implementation Easy 6. How did CTN participation alter your practice Increased understanding of adolescent opioid dependence, promoted state BUP advocacy efforts Easy but challenging adjustment to details of research protocol adherence Since 2007 individual BUP at full 100 patient capacity, others in group practice not waivered 7. Remaining local barriers to BUP 8. CTN impact on local efforts to increase BUP access Poor Medicaid reimbursement, stigma, court systems against agonist tx, community acceptance for youth is low Communities seeing benefits of BUP, advocacy to Maine Medical Society Cost – population mostly uninsured or Medicaid which will not reimburse, stigma, community acceptance for youth is low Managed care insured have access and no apparent stigma about treatment 9. Local media coverage of BUP treatment Favorable on radio, TV, news media No 10. Recommendations to colleagues in regions of low access to BUP Need to advocate/develop rural health cooperatives to address gaps in treatment availability Mandating DEA waiver as part of group/hospital practice will increase prescriber availability 11. Recommendations to other stakeholders Internal medicine, little knowledge of addiction medicine, no BUP Referral to specialist when available Pharmacies: flat fee for service-to-counter costs; lift the 100 patient cap 12. BUP stabilization vs. maintenance Creative incentives for MDs, BUP advocacy to criminal justice systems, leadership advocacy at top hospital administrative level Maintenance is most effective and safe 13. Involved with PCSS Yes, a mentor No Maintenance for one year then consider taper if patient is stable, but patient-driven choice Conclusions Multiple factors impact the dissemination of evidence-based treatment of opioid-dependent adults and youth with buprenorphine. These have been described in the literature and appear in this physician survey sample, and include patient barriers (ability to pay for treatment, transportation), physician barriers (lack of experience or interest, objection to poor reimbursement, lack of DEA waiver, 100 patient cap), and institutional barriers (lack of BUP advocacy at leadership level of health care delivery and training, cultural stigma, cost containment). The CTN strategy for rapid dissemination of evidencebased substance abuse treatment through researchcommunity partnerships appears to have a large impact on removing physician/clinician barriers and increasing regional advocacy, but a less prominent early impact on removing cost and institutional barriers to care. The persistence of cultural stigma toward agonist therapies for opioid dependence despite demonstrated efficacy and safety may require more vigorous public health campaigns by regional and national leadership in health care delivery systems and a coordinated protocol to address public concerns about preventing diversion and opioid misuse. References 1. Mattick RP et al. (2008) Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2008 Apr 16; (2): CD 002207. 2. Connock M et al. (2007) Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess. Mar; 11(9): 1 -171, iii-iv. 3. Woody GE et al. (2008) Extended vs short-term buprenorphinenaloxone for treatment of opioid-addicted youth: a randomized trial. JAMA Nov 5; 300(17): 2003 -11. 4. Polsky D et al. (2010) Cost-effectiveness of extended buprenorphinenaloxone treatment for opioid-dependent youth: data from a randomized trial. Addiction Sep; 105(9): 1616 -24. 5. Knudsen HK et al. (2009) Buprenorphine adoption in the National Drug Abuse Treatment Clinical Trials Network. J Subst Abuse Treat. Oct; 37(3): 307 -12. Contact Information Hilary S. Connery, MD, Ph. D Mc. Lean Hospital Mail stop 222 115 Mill Street , Belmont, MA 02478 Email: hconnery@mclean. harvard. edu Phone: 617 -855 -3881 Disclosures: NONE FUNDING: NIDA 5 U 10 DA 015831 -04 (Weiss, Connery) NIDA 5 U 10 DA 013043 -10 (Woody)