Chronic liver disease Waleed Alhamoudi Gastroentrology and hepatology




- Slides: 47
Chronic liver disease Waleed Al-hamoudi Gastroentrology and hepatology unit
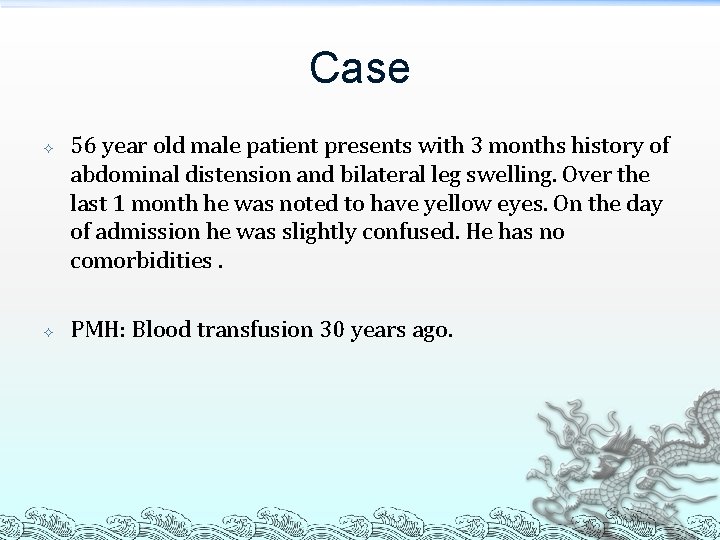
Case 56 year old male patient presents with 3 months history of abdominal distension and bilateral leg swelling. Over the last 1 month he was noted to have yellow eyes. On the day of admission he was slightly confused. He has no comorbidities. PMH: Blood transfusion 30 years ago.
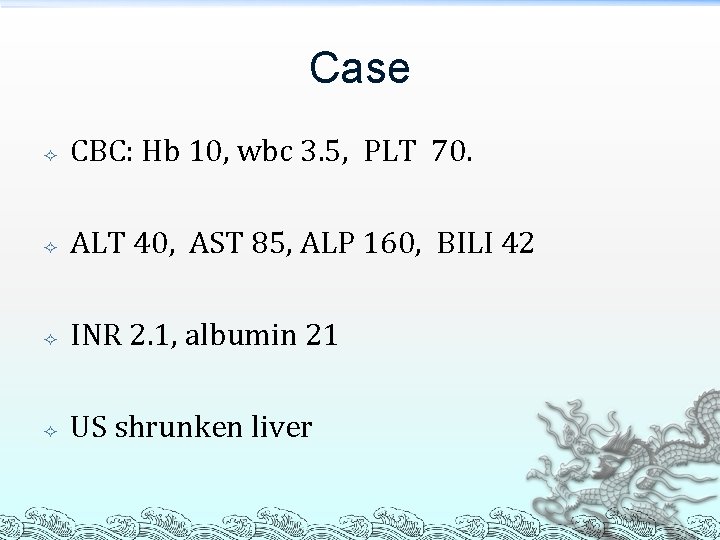
Case CBC: Hb 10, wbc 3. 5, PLT 70. ALT 40, AST 85, ALP 160, BILI 42 INR 2. 1, albumin 21 US shrunken liver
Cause of chronic liver disease Viral ³ ³ Chronic hepatic disease § hepatitis B(Hbsag) , C (hcv ab), D Acute, self-limited viruses § hepatitis A, E, G, CMV, EBV
Causes of chronic liver disease Autoimmune ANA, ASMA, Immunoglobulins (Ig. G, Ig. M, Ig. A) Cholestatic liver disease Primary billiary cirrhosis : AMA Primary sclerosing cholangitis : ERCP, MRCP
Causes of chronic liver disease Metabolic liver disease *Hemochromatosis: iron studies *Wilson disease: 24 hour urinary copper, ceruloplasmin, K-F RINGS. *α-1 antitrypsin: enzyme level
Causes of chronic liver disease Alcoholic liver disease: history Nafld: exclude other etiology. Budd-chiari syndrome: doppler us Drugs: methotrexate
Causes of chronic liver disease Congenital liver disease Bilharziasis: serology Cryptogenic cirrhosis
History& examination Hepatatic and cholestatic symptoms. Risk factors for viral hepatitis. Alcohol, risk factors for NAFLD. Complications of portal HTN: abdominal distension, edema, confusion, gi bleed Family history Drugs Examination: stigmat for CLD.
Investigations Cbc (pancytopenia, thrombocytopenia) Liver enzymes ast>alt INR, Bilirubin, Albumin (child class) Liver imaging Kidney function and electrolytes Liver biopsy and fibroscan

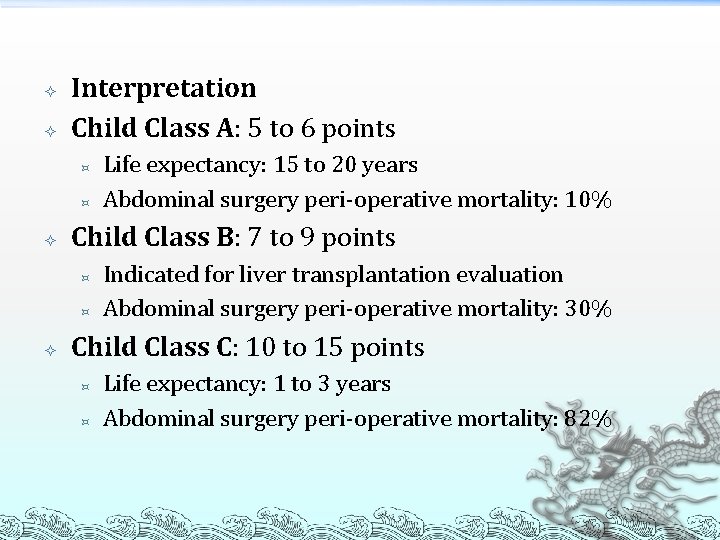
Interpretation Child Class A: 5 to 6 points ³ ³ Child Class B: 7 to 9 points ³ ³ Life expectancy: 15 to 20 years Abdominal surgery peri-operative mortality: 10% Indicated for liver transplantation evaluation Abdominal surgery peri-operative mortality: 30% Child Class C: 10 to 15 points ³ ³ Life expectancy: 1 to 3 years Abdominal surgery peri-operative mortality: 82%
Portal hypertension Hepatic blood flow is normally about 1500 m. L/minute. Normal, uncorrected pressure in the portal vein ranges from 5 to 10 mm Hg. Gradient of 2 -6. Portal HPN present when gradient > 12 mm. Hg. Approximately 2/3 of the hepatic blood supply is provided by portal venous blood. The high-pressure, well-oxygenated hepatic arterial blood mixes completely with the low-pressure, low-oxygencontaining, nutrient-rich portal venous blood within the hepatic sinusoids.
Complications Ascites Variceal bleed Encephalopathy HCC
Ascites Ascites is of Greek derivation ("askos") and refers to a bag or sack describes pathologic fluid accumulation within the peritoneal cavity. Most patients (80%) with ascites have cirrhosis. The three most common causes of cirrhosis at the present time are alcohol, chronic hepatitis B, C, and nonalcoholic steatohepatitis (NASH) related to obesity.


Serum-Ascites Albumin Gradient (SAAG): Measuring the albumin concentration of serum and ascitic fluid specimens and simply subtracting the ascitic fluid value from the serum value. The gradient is calculated by subtraction and is not a ratio. If the SAAG is greater than or equal to 1. 1 g/d. L (11 g/L), the patient can be diagnosed with portal hypertension with an accuracy of approximately 97%. Conversely, if the SAAG is less than 1. 1 g/d. L (11 g/L), the patient does not have portal hypertension with an accuracy of approximately 97%.
COMPLICATIONS Infection Tense Ascites Pleural Effusions Abdominal Wall Hernias
Spontaneous Bacterial Peritonitis (SBP) (1) Positive ascitic fluid culture. (2) An elevated ascitic fluid absolute PMN count (i. e. at least 250 cells/mm 3 or wbc >500 cells/mm 3 (3) without evidence of an intra-abdominal surgically treatable source of infection.
The spontaneous bacterial peritonitis occur only in the setting of severe liver disease. chronic (cirrhosis), but may be acute (fulminant hepatic failure) or subacute (alcoholic hepatitis). Cirrhosis of all causes can be complicated by spontaneous ascitic fluid infection. Essentially all patients with SBP have Child-Pugh class B or C cirrhosis, ascites a prerequisite to the development of SBP.
currently available evidence suggests that the spontaneous forms of ascitic fluid infection are the result of overgrowth of a specific organism in the gut, "translocation" of that microbe from the gut to mesenteric lymph nodes, and resulting spontaneous bacteremia and subsequent colonization of susceptible ascitic fluid. Low-protein ascitic fluid (e. g. , <1 g/d. L [10 g/L]) is particularly susceptible to SBP are symptomatic at the time the infection is diagnosed, the symptoms and signs of infection are often subtle, such as a slight change in mental status.
Fully 98% of causative organisms were susceptible to cefotaxime, which did not result in superinfection or nephrotoxicity. Cefotaxime or a similar third-generation cephalosporin appears to be the treatment of choice for suspected SBP. IV albumin (1. 5 g/kg body weight at the time the infection is detected and 1. 0 g/kg on day 3) in combination with cefotaxime has been shown in a large randomized trial to reduce the risk of renal failure and improve survival.
Paracentesis should be repeated after 48 hours of treatment if the course is atypical. < 5% of patients die of infection if appropriate antibiotics are administered. Norfloxacin 400 mg/day orally has been reported to reduce the risk of SBP in inpatients with low-protein ascites and patients with prior SBP. Norfloxacin 400 mg orally twice daily for 7 days helps prevent infection in patients with variceal hemorrhage, however, oral antibiotics do not prolong survival and do select for resistant organisms in the gut flora, which can subsequently cause spontaneous ascitic infection.
Tense Ascites Requires urgent therapeutic paracentesis. Total paracentesis, " even more than 20 L, has recently been demonstrated to be safe, improves venous return and hemodynamics. The myth of paracentesis-related hemodynamic disasters was based on observations in small numbers of patients.
Pleural Effusions: Unilateral and right-sided but occasionally may be bilateral and larger on the right side than the left. A large effusion in a patient with cirrhotic ascites is referred to as hepatic hydrothorax. Hepatic hydrothorax have been shown to have a small defect in the right hemidiaphragm, With large diaphragmatic defects, ascites may be undetectable. The most common symptom is shortness of breath
The analysis of uncomplicated hepatic hydrothorax fluid is similar to that of ascites. Rx of hepatic hydrothorax has been difficult until the availability of transjugular intrahepatic portosystemic stent shunts (TIPS) Chest tube insertion and sclerosis of the pleurae with tetracycline. Sodium restriction and use of diuretics constitute the safest and most effective first-line therapy of hepatic hydrothorax. TIPS has been reported to be successful and is reasonable second-line treatment.
Determine the precipitating cause of ascites formation (e. g. , dietary indiscretion or noncompliance with diuretics or saline iv). The dietary Na restriction for inpatients and outpatients is 2 grams (88 mmol) per day. No fluid restriction unless low Na Although it is traditional to order bed rest, there are no controlled trials to support this practice, strict bed rest is unnecessary and may lead to decubitus ulcers in these emaciated pts.
Diuretics : spironolactone and furosemide together on the first hospital day in initial doses of 100 mg and 40 mg, respectively, each taken once in the morning. If the combination of spironolactone 100 mg/day (or 10 mg/day of amiloride) and furosemide 40 mg/day orally is ineffective in increasing urinary sodium or decreasing body weight, the doses of both drugs should be increased simultaneously.
The ratio of spironolactone and furosemide can be adjusted to correct abnormal serum potassium levels. Occasionally. When combined with a sodium-restricted diet in a study of almost 4000 patients, the regimen of spironolactone and furosemide has been demonstrated to achieve successful diuresis in more than 90% of cirrhotic patients. IV diuretics cause acute decreases in the GFR in cirrhotic patients with ascites and should be avoided.
Once the edema has resolved, a reasonable maximum weight loss is probably 0. 5 kg/day. Encephalopathy, a serum sodium concentration less than 120 mmol/L despite fluid restriction, or a serum creatinine level greater than 2. 0 mg/d. L (180 μmol/L) should result in cessation of diuretics and reassessment of the situation. NSAID should be avoided in cirrhotic ascites as they inhibit diuresis, may promote renal failure, and cause gastrointestinal bleeding.
Refractory Ascites : ascites unresponsive to a Na-restricted diet and high-dose diuretic treatment, which may be manifested by minimal or no wt. loss despite diuretics or the development of complications of diuretics. < 10% of patients with cirrhotic ascites are refractory to standard medical therapy. Viable options for patients refractory to routine medical therapy include liver transplantation, serial therapeutic paracenteses, TIPS, and peritoneovenous shunts.

Varices
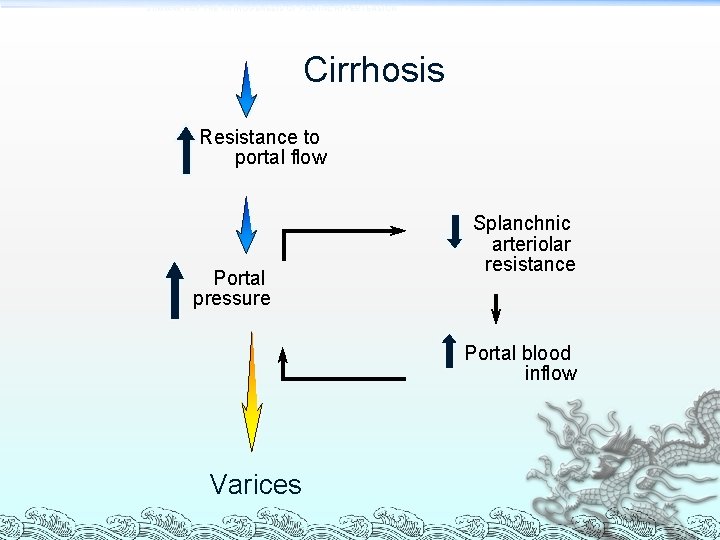
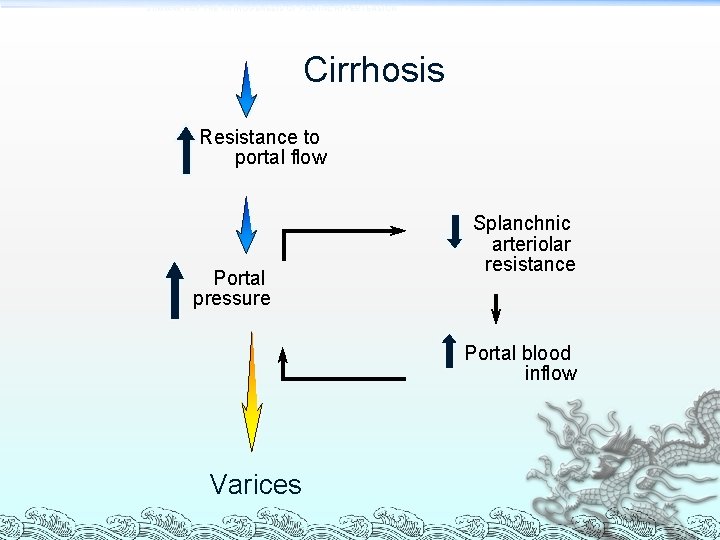
SUMMARY OF THE PATHOGENESIS OF PORTAL HYPERTENSION Cirrhosis Resistance to portal flow Portal pressure Splanchnic arteriolar resistance Portal blood inflow Varices
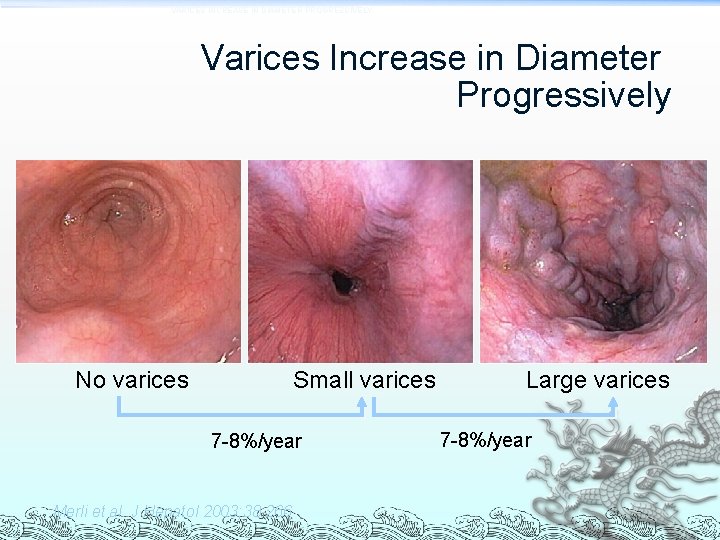
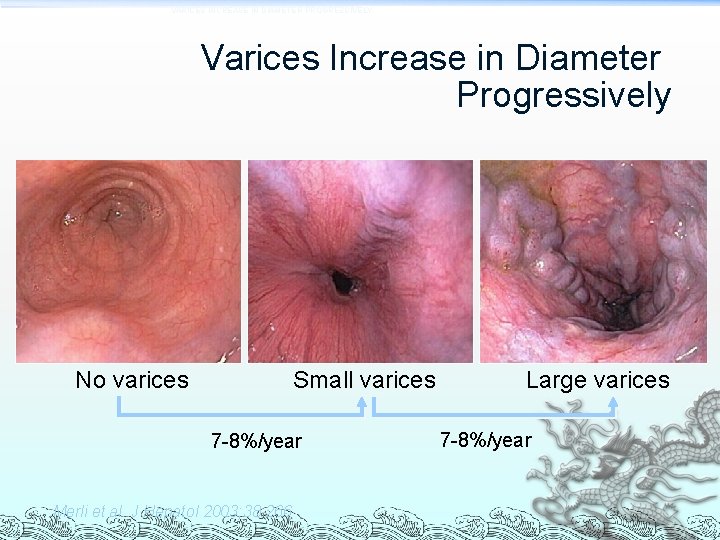
VARICES INCREASE IN DIAMETER PROGRESSIVELY Varices Increase in Diameter Progressively No varices Small varices 7 -8%/year Merli et al. J Hepatol 2003; 38: 266 Large varices 7 -8%/year
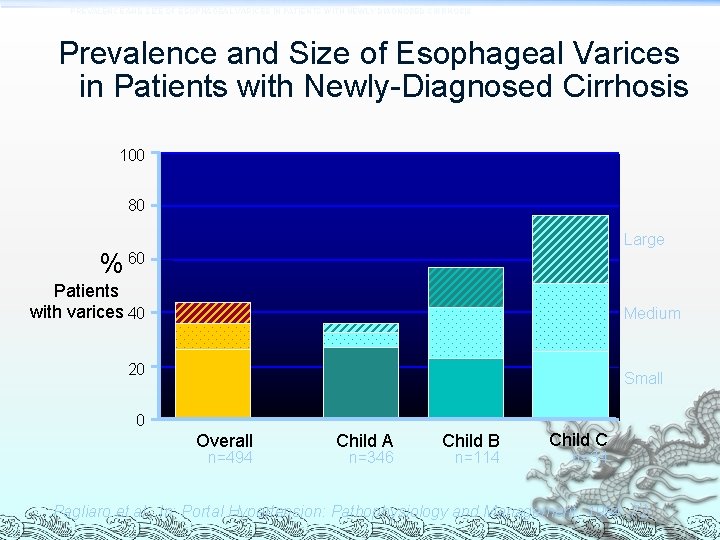
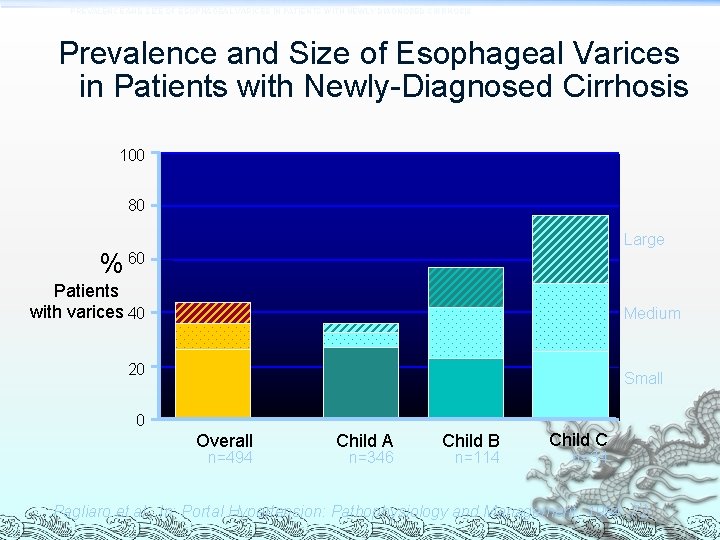
PREVALENCE AND SIZE OF ESOPHAGEAL VARICES IN PATIENTS WITH NEWLY DIAGNOSED CIRRHOSIS Prevalence and Size of Esophageal Varices in Patients with Newly-Diagnosed Cirrhosis 100 80 Large % 60 Patients with varices 40 Medium 20 Small 0 Overall n=494 Child A n=346 Child B n=114 Child C n=34 Pagliaro et al. , In: Portal Hypertension: Pathophysiology and Management, 1994: 72
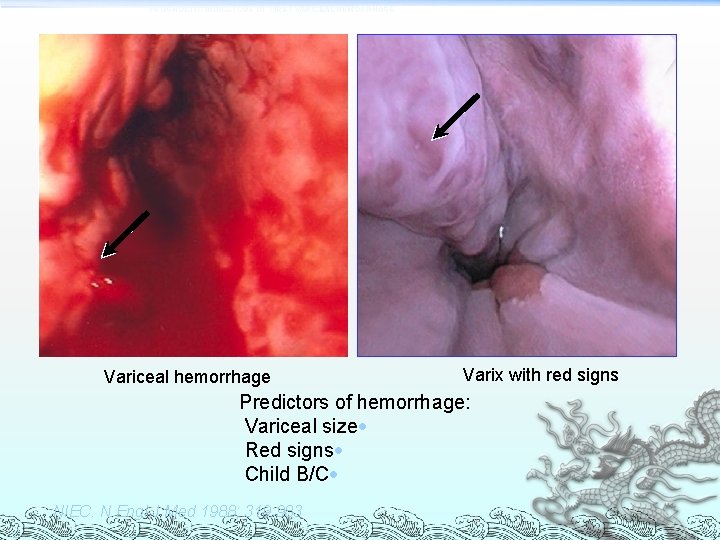
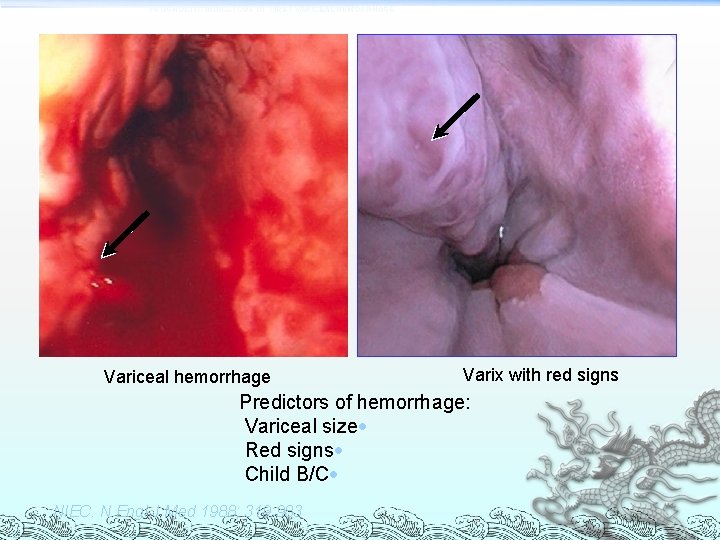
PROGNOSTIC INDICATORS OF FIRST VARICEAL HEMORRHAGE Variceal hemorrhage Varix with red signs Predictors of hemorrhage: Variceal size· Red signs· Child B/C· NIEC. N Engl J Med 1988; 319: 983
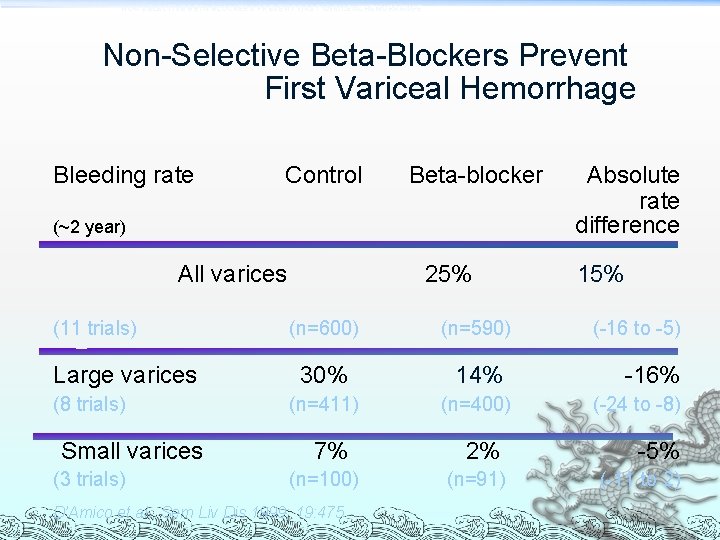
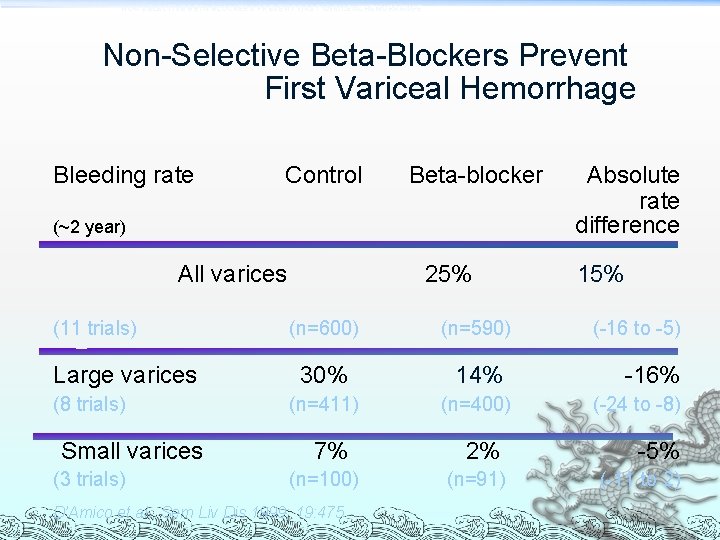
NON-SELECTIVE BETA-BLOCKERS PREVENT FIRST VARICEAL HEMORRHAGE Non-Selective Beta-Blockers Prevent First Variceal Hemorrhage Bleeding rate Control Beta-blocker (~2 year) All varices (11 trials) Large varices (8 trials) Small varices (3 trials) 25% (n=600) (n=590) 30% 14% (n=411) (n=400) 7% (n=100) D’Amico et al. , Sem Liv Dis 1999; 19: 475 Absolute rate difference 15% (-16 to -5) -16% (-24 to -8) 2% -5% (n=91) (-11 to 2)
Other treatment options Band ligation Sclerotherapy TIPPS insertion Shunt surgery Transplantation
Acute Variceal Bleed ABC!!! Octreotide PPI *** Antibiotics *** ³ Cefotaxime or Norfloxacin Keep Hb 80 -100 g/L
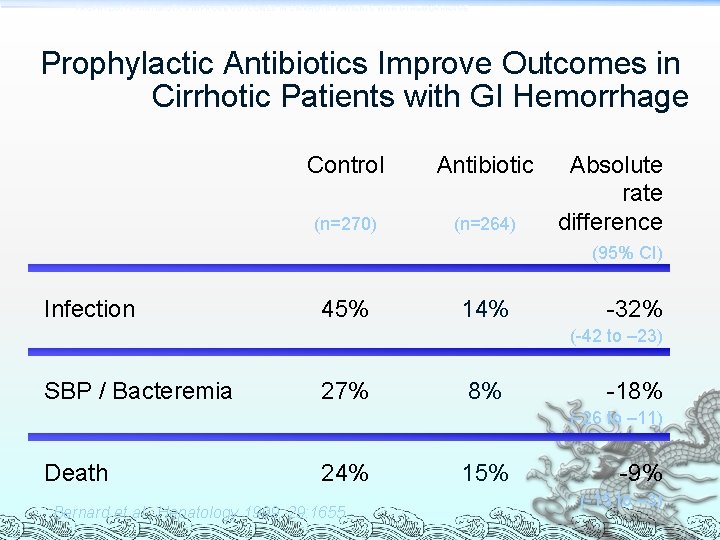
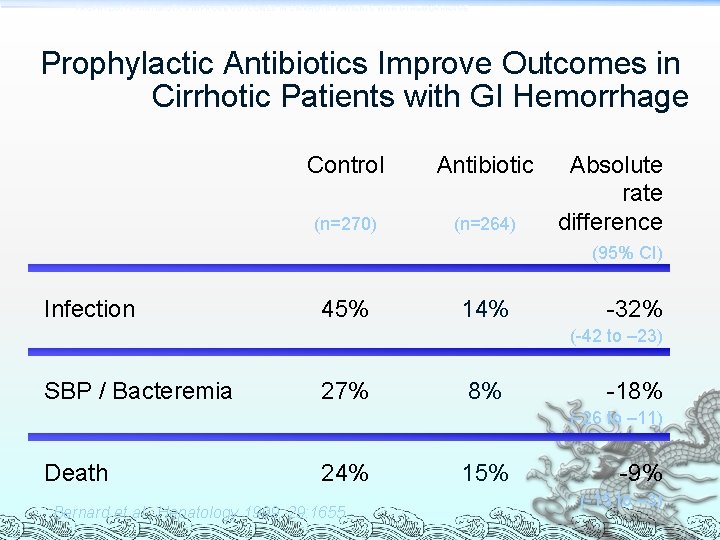
PROPHYLACTIC ANTIBIOTICS IMPROVE OUTCOMES IN CIRRHOTIC PATIENTS WITH GI HEMORRHAGE Prophylactic Antibiotics Improve Outcomes in Cirrhotic Patients with GI Hemorrhage Control Antibiotic (n=270) (n=264) Absolute rate difference (95% CI) Infection 45% 14% -32% (-42 to – 23) SBP / Bacteremia 27% 8% -18% (-26 to – 11) Death 24% Bernard et al. , Hepatology 1999; 29: 1655 15% -9% (-15 to – 3)
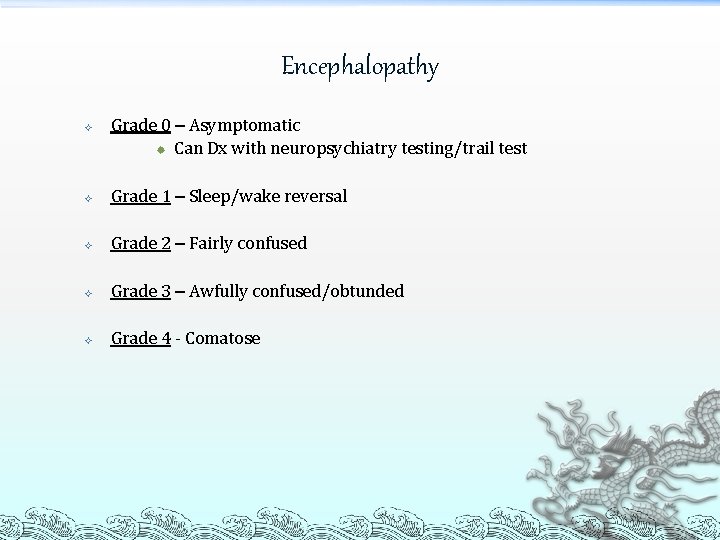
Encephalopathy Grade 0 – Asymptomatic ® Can Dx with neuropsychiatry testing/trail test Grade 1 – Sleep/wake reversal Grade 2 – Fairly confused Grade 3 – Awfully confused/obtunded Grade 4 - Comatose
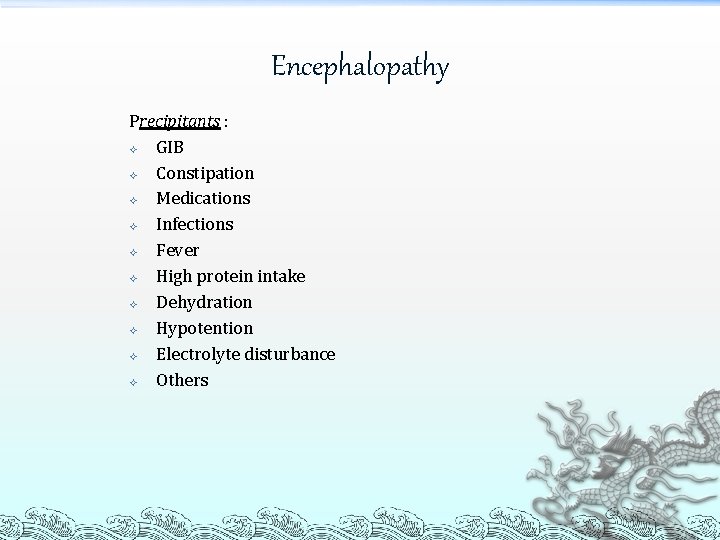
Encephalopathy Precipitants : GIB Constipation Medications Infections Fever High protein intake Dehydration Hypotention Electrolyte disturbance Others
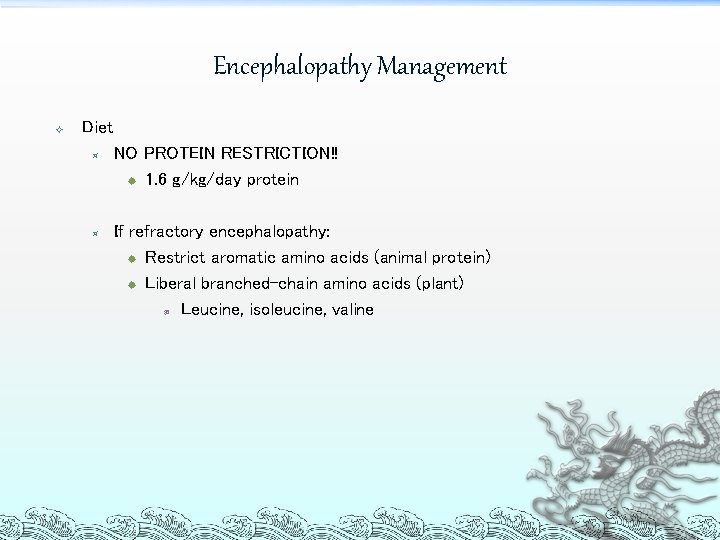
Encephalopathy Management Diet ³ ³ NO PROTEIN RESTRICTION!! ® 1. 6 g/kg/day protein If refractory encephalopathy: ® Restrict aromatic amino acids (animal protein) ® Liberal branched-chain amino acids (plant) ¯ Leucine, isoleucine, valine
Encephalopathy Management Lactulose ³ Titrate to 2 -4 BM/day Antibiotics ³ Flagyl, Neomycin
Hepatocellular Carcinoma recommendations U/S abdomen, alpha-fetoprotein q 6 months All cirrhotic patients Early detection is associated with better outcome
Questions. . .
 Stigmata of chronic liver disease
Stigmata of chronic liver disease Dcld vs cld
Dcld vs cld Stigmata of chronic liver disease
Stigmata of chronic liver disease Stigmata of chronic liver disease
Stigmata of chronic liver disease Nursing management of liver cirrhosis
Nursing management of liver cirrhosis Hepatology
Hepatology Biliary system
Biliary system Addenbrookes hepatology
Addenbrookes hepatology Renal bruit auscultation
Renal bruit auscultation Chronic liver desease
Chronic liver desease Circulatory disturbances pathology
Circulatory disturbances pathology Waleed elsafoury
Waleed elsafoury Waleed huwio
Waleed huwio Hydrometer soil test
Hydrometer soil test Waleed majeed
Waleed majeed Kevin gimpel
Kevin gimpel Historty
Historty Chronic granulomatous disease
Chronic granulomatous disease Jewish chronic disease study
Jewish chronic disease study Chronic kidney disease near atwater
Chronic kidney disease near atwater Nih score
Nih score Kate lorig chronic disease self-management
Kate lorig chronic disease self-management Who developed the chronic care model
Who developed the chronic care model Chronic disease
Chronic disease Chronic disease
Chronic disease Bullous emphysema
Bullous emphysema Chronic rheumatic heart disease
Chronic rheumatic heart disease Decompensated liver disease
Decompensated liver disease Complication of liver cirrhosis
Complication of liver cirrhosis Elisabetta bugianesi
Elisabetta bugianesi Portal hypertension symptoms and signs
Portal hypertension symptoms and signs Gennifer shafer liver disease
Gennifer shafer liver disease Cirrhosis
Cirrhosis Infiltrative liver disease
Infiltrative liver disease Bharathi viswanathan
Bharathi viswanathan Cardinal sign of inflammation
Cardinal sign of inflammation Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Morphological patterns of chronic inflammation
Morphological patterns of chronic inflammation Leukemia death rate
Leukemia death rate Periradicular disease definition
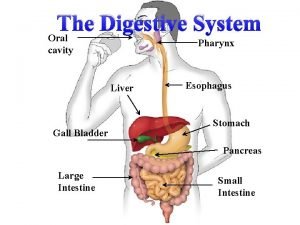
Periradicular disease definition Location of pancrease
Location of pancrease Liver and pancreas function
Liver and pancreas function Difference between spleen and gallbladder
Difference between spleen and gallbladder Liver hilus
Liver hilus Function of liver and pancreas in digestion
Function of liver and pancreas in digestion Psyhomotor
Psyhomotor Pancreasitis
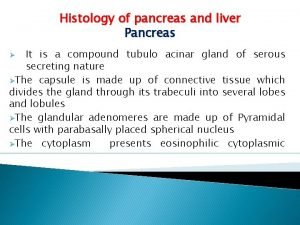
Pancreasitis Liver lobules
Liver lobules