Chapter 8 Infant Nutrition Through the Life Cycle



















- Slides: 65
Chapter 8 Infant Nutrition Through the Life Cycle Judith E. Brown
Assessing Newborn Health • Birthweight as an Outcome – Full-term infant (37 to 42 wks) • Typical weight 2500 -3800 g (5. 5 to 8. 5 lbs) • Typical length 47 -54 cm (18. 5 to 21. 5 in) • 88% of U. S. infants are born full-term
Infant Mortality • Infant mortality defined as death that occurs within the first year • Major cause is low birthweight (< 2500 g) • Other leading causes inlcude: – 1) congenital malformations, – 2) preterm births, and – 3) SIDS

Combating Infant Mortality • Factors associated with mortality: • • • Social and economic status Access to health care Medical interventions Teenage pregnancy Availability of abortion services Failure to prevent preterm & LBW births
Resources to Combat Infant Mortality – Resources and prevention programs to combat infant mortality • Medicaid • Child Health Initiatives Program (CHP) • Early Periodic Screening, Detection, and Treatment Program (EPSDT) • WIC and CDC (Nutrition Surveillance Program) • Bright Futures
Assessing Newborn Health • Standard Newborn Growth Assessment – “Appropriate for gestational age” (AGA) – “Small for gestational age” (SGA) and “intrauterine growth retardation” (IUGR) mean newborn was <10 th % wt/age – “Large for gestational age” (LGA) means newborn was >90 th % wt/age

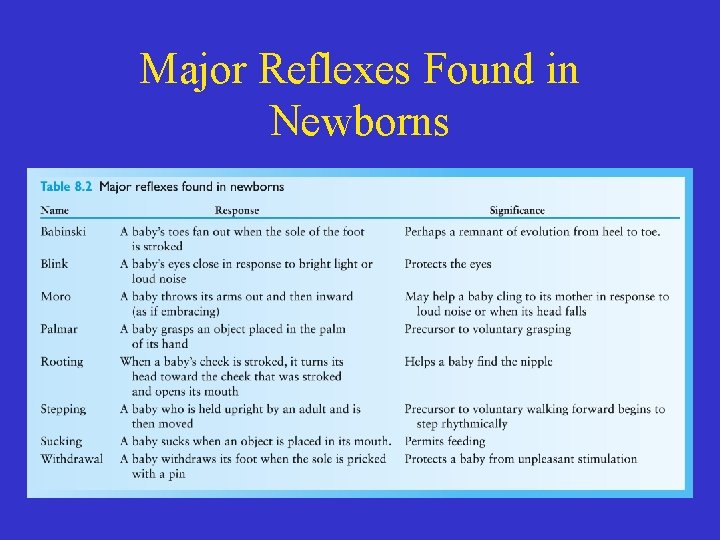
Infant Development • Newborns: – Hear and move in response to familiar voice – CNS is immature resulting in inconsistent cues for hunger and satiety – Strong reflexes, especially suckle and root (reflexes are protective for newborns)

Infant Development • Terms Related to Development: – Reflex—automatic response triggered by specific stimulus – Rooting reflex—infant turns head toward the cheek that is touched – Suckle—reflex causing tongue to move forward and backward – http: //www. youtube. com/watch? v=ULno 8 FAm t 0 c
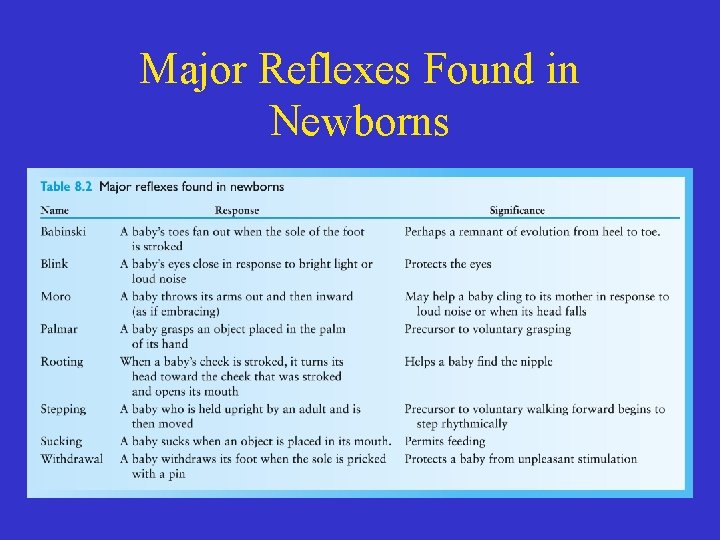
Major Reflexes Found in Newborns
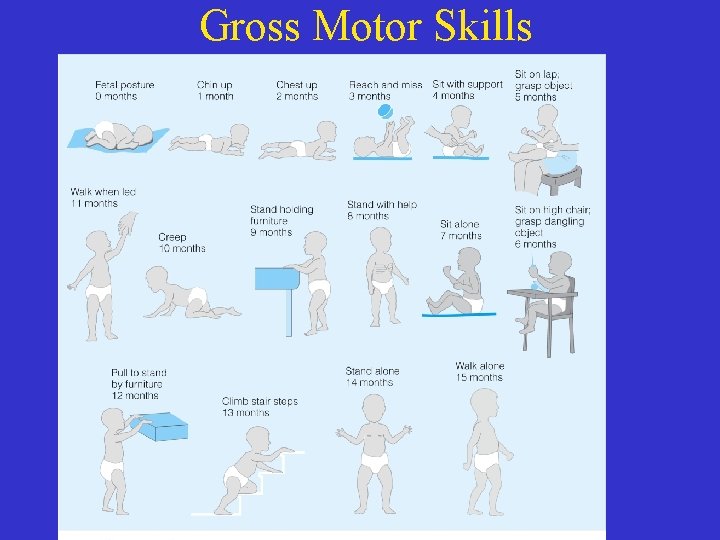
Motor development • Motor development: ability to control voluntary muscles • Motor development is top down— controls head first and lower legs last • Muscle development from central to peripheral • Influences ability to feed self & the amount of energy expended
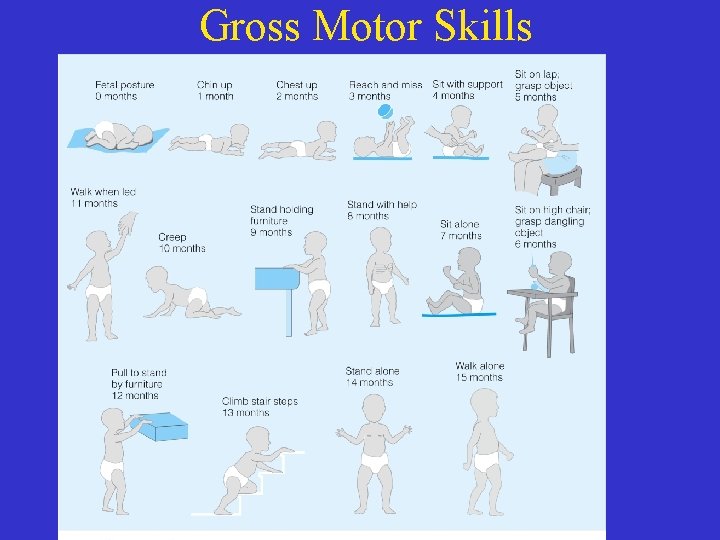
Gross Motor Skills
Critical Periods of Infant Development • A fixed period of time in which certain behaviors or developments emerge • Necessary for sequential behaviors or developments • If the critical period is missed, there may be difficulty later on
Cognitive Development of Infants • Factors that impact cognition – Sensorimotor development – Adequate nutrient intake – Positive social and emotional interactions – Genetics
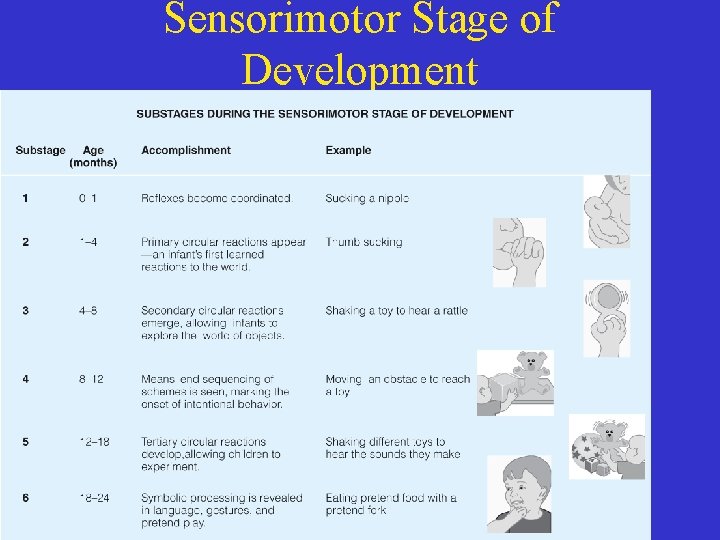
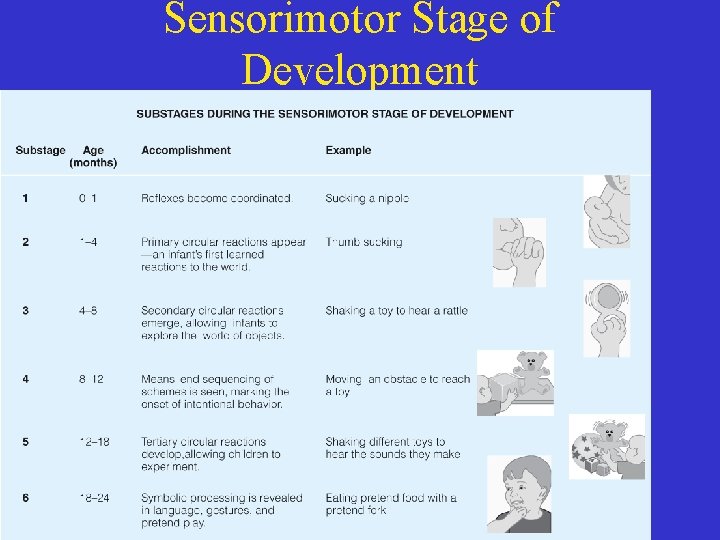
Sensorimotor Stage of Development
Digestive System Development of Infants • Fetus swallows amniotic fluid which stimulates intestinal maturation and growth • At birth the healthy newborn can digest fats, protein and simple sugars. • Common problems include gastroesophageal reflux (GER), diarrhea, and constipation
Digestive System Development of Infants • Factors that impact rate of food passage in GI – Osmolarity of foods or liquids – Colon bacterial flora – Water and fluid balance in the body
Parenting • New parents must learn: – Infant’s cues of hunger and satiety – Temperament of infant – How to respond to infant cues
Energy and Nutrient Needs • The recommendations for infants are from the Dietary Reference Intakes (DRI), National Academy of Medicine, AAP and the ADA – Caloric needs – Protein needs – Fats – Metabolic rate, calories, fats and protein—how do they all tie together?
Energy Needs • Energy (Calories): – 108 kcal/kg/day from birth to 6 months (range from 80 to 120) – 98 kcal/kg/day from 6 to 12 months • Factors that influence calorie needs – Weight and growth rate – Sleep/wake cycle – Temperature and climate – Physical activity – Metabolic response to food – Health status

Protein Needs • Protein Needs – 2. 2 g/kg/day from birth to 6 months – 1. 6 g/kg/day from 6 to 12 months • How much is that? – Newborn weighing 4 kg (8. 8 lbs) needs 2. 2 X 4 = 8. 8 g protein – 6 -month-old weighing 8 kg (17. 6 lbs) needs 1. 6 X 8 = 12. 8 g protein • Protein needs are similar to that of energy but are also influenced by body composition
Fat Needs • Breastmilk contains about 55% calories from fat • Infants need cholesterol for gonad and brain development • Breast milk contains short-chain and mediumchain fatty acids (in addition to the long-chain) – Easier to digest and utilize than long-chain fatty acids
Metabolic Rate, Calories, Fats and Protein • Metabolic rate of infants is highest of any time after birth – The higher rate is related to rapid growth and high proportion of muscle – Low carbohydrate and/or energy intake results in protein catabolism impacting growth

Other Nutrients and Nonnutrients – Fluoride— 0. 1 - 0. 5 mg/d depending on age (too much may cause tooth discoloration) – Vitamin D— 400 IU/day – Sodium— 120 mg/day – Fiber—no recommendations – Lead—None—may be toxic

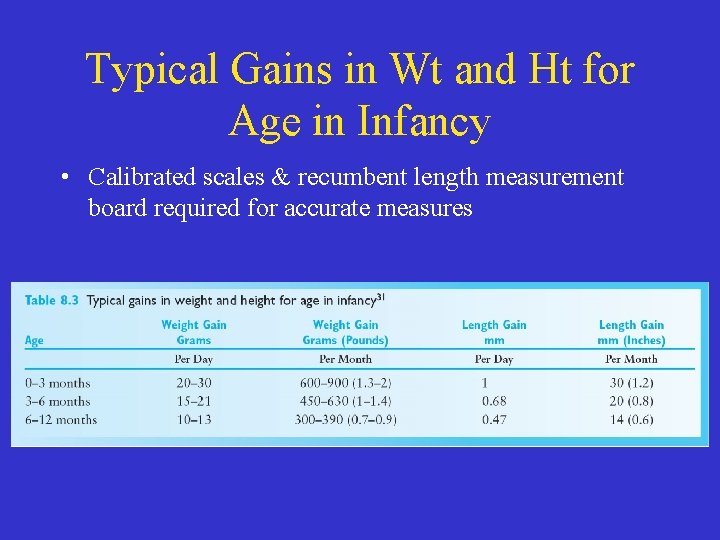
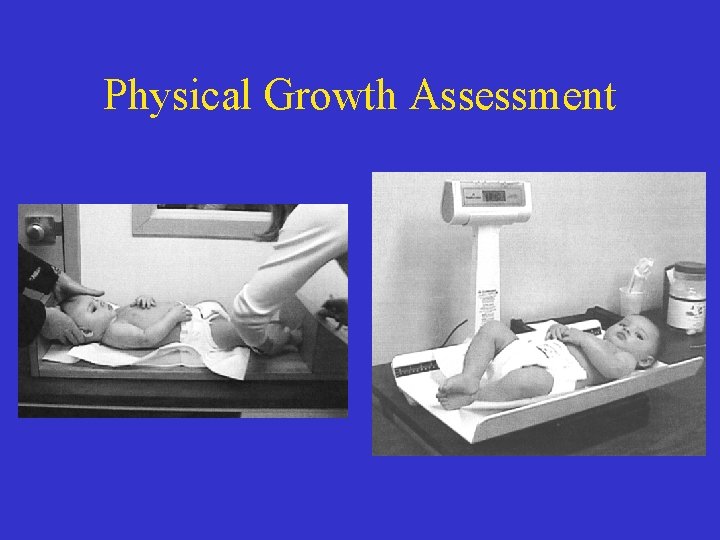
Physical Growth Assessment • Newborns double birthweight by 4 -6 mos and triple it by 1 yr • Growth reflects: – Nutritional adequacy – Health status – Economic & environmental adequacy • There is a wide range of growth =normal • Calibrated scales & recumbent length measurement board required for accurate measures
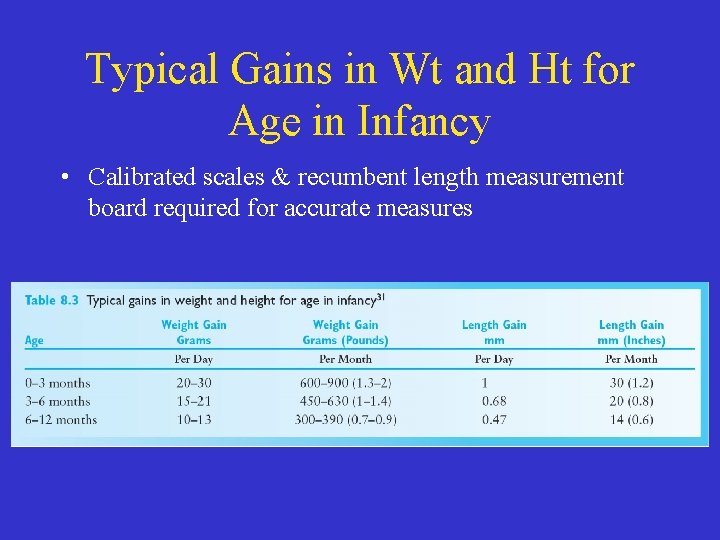
Typical Gains in Wt and Ht for Age in Infancy • Calibrated scales & recumbent length measurement board required for accurate measures
Physical Growth Assessment

Measuring Growth in Infants

Interpretation of Growth Data • Measures over time identify change in growth rate and need for intervention • Warning signs: – Lack of Wt or Lt gain – Plateau in Wt, Lt or HC for > 1 month – Drop in Wt without regain in a few weeks
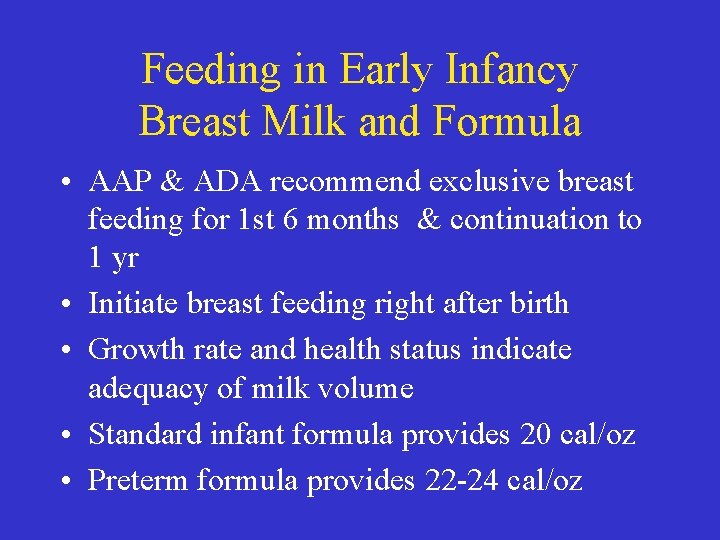
Feeding in Early Infancy Breast Milk and Formula • AAP & ADA recommend exclusive breast feeding for 1 st 6 months & continuation to 1 yr • Initiate breast feeding right after birth • Growth rate and health status indicate adequacy of milk volume • Standard infant formula provides 20 cal/oz • Preterm formula provides 22 -24 cal/oz
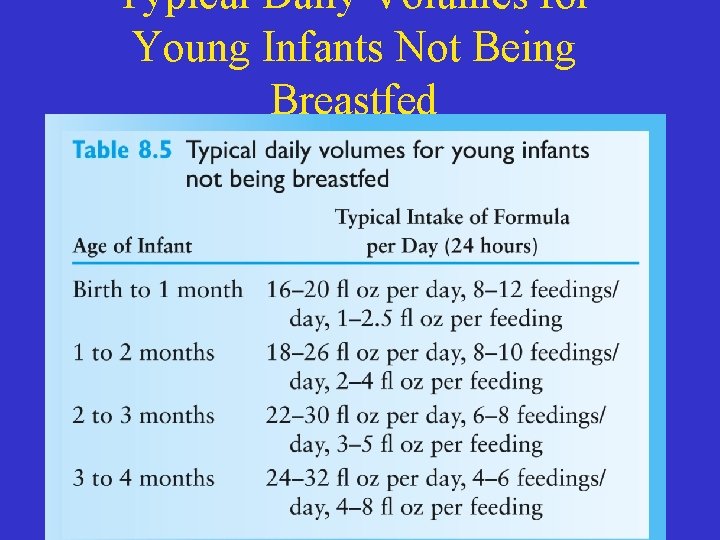
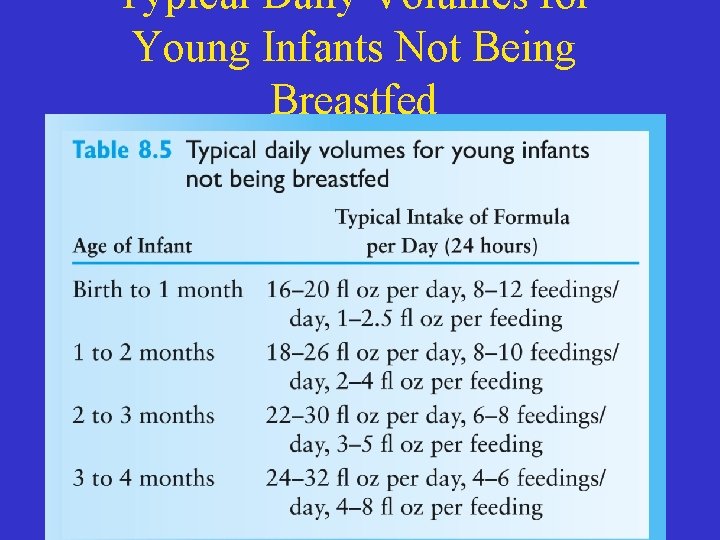
Typical Daily Volumes for Young Infants Not Being Breastfed
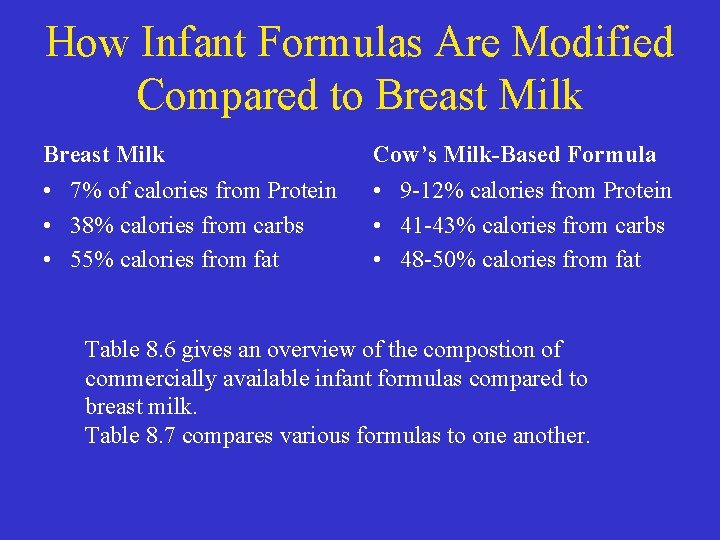
How Infant Formulas Are Modified Compared to Breast Milk Cow’s Milk-Based Formula • 7% of calories from Protein • 38% calories from carbs • 55% calories from fat • 9 -12% calories from Protein • 41 -43% calories from carbs • 48 -50% calories from fat Table 8. 6 gives an overview of the compostion of commercially available infant formulas compared to breast milk. Table 8. 7 compares various formulas to one another.

Cow’s Milk during Infancy • Whole, reduced-fat or skim cow’s milk should not be used in infancy • Iron-deficiency anemia linked to early introduction of cow’s milk • Anemia linked to: – GI blood loss – Calcium & phosphorus – Displacement of iron-rich foods
Soy Protein-Based Forumla during Infancy • Soy protein in place of milk protein should be limited in its use • There is little scientific evidence for benefit of increase soy over milk-based • The use of soy formula is not recommended – For managing infantile colic – Or as an advantage of cow’s milk formula for preventing allergy in healthy at-risk infants

Development of Infant Feeding Skills • Infants born with reflexes & food intake regulatory mechanism • Inherent preference for sweet taste • At 4 -6 wks, reflexes fade; infant begins to purposely signal wants & needs • Table 8. 8 shows infant developmental milestones and readiness for feeding skills
Development of Infant Feeding Skills • Cues infants may give for feeding readiness include: – Watching the food being opened in anticipation of eating – Tight fists or reaching for spoon – Irritation if feeding too slow or stops temp. – Playing with food or spoon – Slowing intake or turning away when full – Stop eating or spit out food when full
Introduction of Solid Foods • Food offered from spoon stimulates muscle development • At 4 -6 months, offer small portions of semisoft food on a spoon once or twice each day
Recommendations for Introduction of Solid Foods • • Infant should not be overly tired or hungry Use small spoon with shallow bowl Allow infant to open mouth & extend tongue Place spoon on front of tongue with gentle pressure Avoid scraping spoon on infant’s gums Pace feeding to allow infant to swallow First meals may be 5 -6 spoons over 10 minutes

The Importance of Infant Feeding Position • Improper positioning may cause choking, discomfort, and ear infections • Position young bottle-fed infants in a semiupright • Spoon-feeding should be with infant seated with back and feet supported • Adults feeding infants should be directly in front of infant making eye contact
Preparing for Drinking from a Cup • • Offer water or juice from cup after 6 months Wean to a cup at 12 to 24 months First portion from cup is 1 -2 oz Early weaning may result in plateau in weight (due to reduced calories) and/or constipation (from low fluid intake)

Preparing for Drinking from a Cup • Changing from a bottle to a covered “sippy” cup with a small spout is not the same developmental step as weaning to an open cup • Open cup drinking skills also encourage speech development
Food Texture and Development “They say fingers were made before forks and hands before knives. ” − Jonathan Swift
Food Texture and Development • Can swallow pureed foods at 4 -6 months • Early introduction of lumpy foods may cause choking • Can swallow very soft, lumpy foods at 6 -8 months • By 8 -10 months, can eat soft mashed foods

First Foods • 6 months—iron-fortified baby cereal – Rice cereal is hypoallergenic • 6 months—fruits and vegetables • Only one new food over 2 -3 days • Commercial baby foods are not necessary but do provide sanitary and convenient choices • 9 -12 months soft table foods

Inappropriate and Unsafe Food Choices • Foods that choke infants – – – Popcorn Peanuts Raisins, whole grapes Stringy meats Gum & gummy-textured candy, hard candy or jelly beans – Hot dogs – Hard fruits or vegetables
Water • Breast milk or formula provide adquate water for healthy infants up to 6 months. • All forms of fluids contribute to water intake • Additional plain water needed in hot, humid climates • Dehydration is common in infants
Water • Pedialyte or sports drinks provide electrolytes but lower in calories than formula or breast milk • Limit juice – AAP recommends juice is not needed to meet the fluid needs before the age of 6 months • Avoid colas and tea
How Much Food is Enough for Infants? • Infants vary in temperament • Crying or fussiness may be interpreted as hunger resulting in overfeeding • First foods may appear to be rejected due to immature tongue movement
How Infants Learn Food Preferences • Infants learn food preferences • Flavor of breast milk influenced by mother’s diet • Genetic predisposition to sweet taste • Food preference from infancy sets stage for lifelong food habits
Nutrition Guidance • Guidance materials are available – WIC program – Bright Future in Practice • Infant feeding recommendations from nutrition education materials are sampled in Table 8. 9
Nutrition Guidance • Infants and exercise – Adult exercise and fitness do not apply to infants • Stimulating environment is recommended to allow infants to explore and move as a part of their developmental milestones
Nutrition Guidance • Supplements for infants – Fluoride—for breastfed infants or if in any area with no fluoridated water – Iron—if mother was anemic – Vitamin B 12—for vegans – Vitamin D—needed if low sun exposure or exclusively breastfed
Common Nutritional Problems and Concerns • • • Failure to thrive (FTT) Colic Iron-deficiency anemia Constipation Dental caries Food allergies
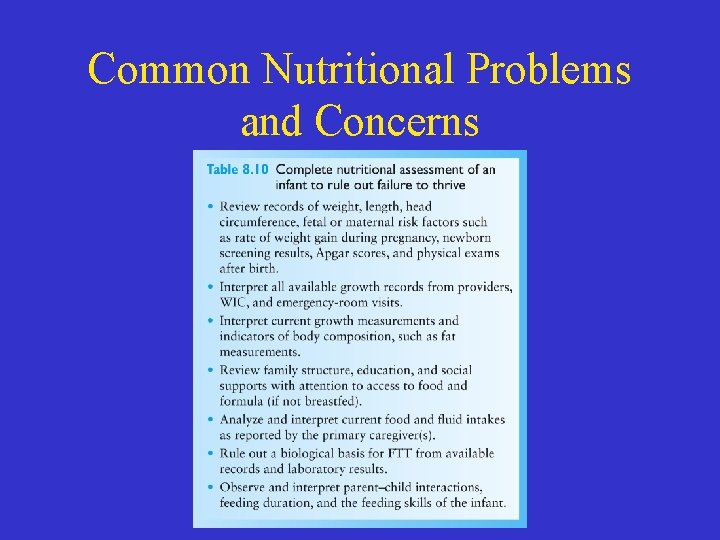
Common Nutritional Problems and Concerns • Failure to thrive (FTT) – Inadequate wt or lt gain – Organic—diagnosed medical illness – Nonorganic—not based on medical diagnosis • Intervention for FTT – May be complex and involve a team approach including the registered dietitian
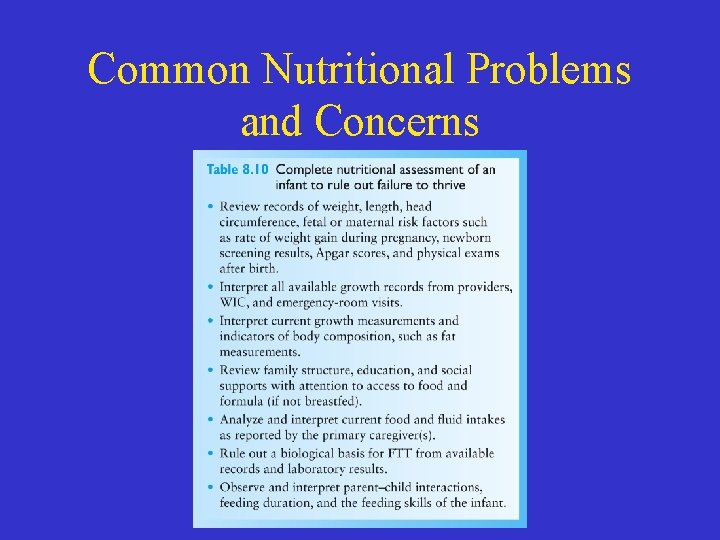
Common Nutritional Problems and Concerns
Colic • The sudden onset of irritability, fussiness or crying • Episodes may appear at the same time each day • Disappear at 3 rd or 4 th • Cause unknown but associated with GI upset, infant feeding practices

Iron-deficiency Anemia • Less common in infants than in toddlers • Irons stores in the infant reflect the iron stores of the mother • More common in low-income families • Breastfed infants may be given iron supplements and iron-fortified cereals at 4 -6 months • Iron-fortified versus “Low-iron” formula
Diarrhea and Constipation • Infants typically have 2 -6 stools per day • Causes of diarrhea & constipation: – Viral and bacterial infections – Food intolerance – Changes in fluid intake

Diarrhea and Constipation • To avoid constipation assure adequate fluids • Diarrhea may be a serious problem-continue to feed the usual diet during diarrhea
Prevention of Baby Bottle Caries and Ear Infections • Caries and ear infections linked to feeding practices • Feeding techniques to reduce caries and ear infections – Limit use of bedtime bottle – Offer juice in cup – Only give water bottles at bedtime – Examine and clean emerging teeth
Food Allergies and Intolerances • About 6 -8% of children < 4 yrs have allergies • Absorption of intact proteins causes allergic reactions • Common symptoms are wheezing or skin rashes • Treatment may consist of formula with hydrolyzed proteins
Lactose Intolerance • Inability to digest the disaccharide lactose • Characterized by cramps, nausea and pain and alternating diarrhea and constipation • Lactose intolerance in uncommon and tends to be overestimated • Many infants “outgrow” lactose intolerance

Cross-Cultural Considerations • Baby foods do not reflect ethnic diversity • Some cultural practices are harmful; others are harmless or helpful • Cultural considerations may impact willingness to participate in assistance programs

Vegetarian Diets • Infants receiving well-planned vegetarian diets grow normally • Breastfed vegan infants need supplements – Vitamin D – Vitamin B 12 – Possibly iron and zinc

Nutrition Intervention for Risk Reduction • Early Head Start Program – Works with families at risk such as drug abuse, infants with disabilities, or teenage mothers • Model program: newborn screening – Phenylketonuria, galactosemia, hypothyroidism, or sickle-cell anemia