Implementation of an InfantDriven Feeding Algorithm Brooke Welker
Implementation of an Infant-Driven Feeding Algorithm Brooke Welker, BSN, RN
Objectives • Describe implementation of an infant-driven feeding tool in the NICU • Identify barriers to implementation of an infant feeding readiness tool
Introduction • Oral feedings: most prevalent developmental challenge preterm infants face • Feeding difficulties increase LOS & cost of healthcare • Former premature infants: 40% referred to feeding disorder clinics • Growth and discharge
Background • Volume-driven (medical order) • Set intervals • Often the infant’s behavioral and physiological readiness is not taken into consideration
Significance • Stress to infant during feeding negative desire and capability to feed in the NICU and at home • >50% of parents with former NICU babies reveal feeding difficulties in their infant at the age of 1824 months • Infant-driven feeding • Reduces the time it takes to reach full feedings compared to volume-driven feedings reducing LOS and NICU costs
Significance • National Association of Neonatal Nurses (NANN) recommends infant-driven and patient-specific feedings to assure safety • To improve the chances for successful feeding outcomes for both the short and longterm transition to an infant-driven feeding approach
Local Problem • 24 -bed Midwestern level II-III NICU • Volume-driven approach • No infant feeding readiness tool • Inconsistencies in feeding practices among caregivers & parents • Force feed vs. gavage feed
Purpose Statement • The purpose of this quality improvement project was to implement an infant-driven feeding tool in an effort to transition to a uniform infant-driven feeding culture in the Neonatal Intensive Care Unit.
Literature Review • Preterm Infant Feeding Challenges • Physiologic complications • Immature gastrointestinal system • Immature neurologic system • Enteral and Oral Feeding Practices • • Variances among nurses Inconsistencies in clinical practice Infant-driven feeding practices Volume-driven feeding
Literature Review • Infant Feeding Readiness Scales • • Infant-Driven Feeding Scale (IDFS) Neonatal Oral Motor Assessment Scale (NOMAS) Early Feeding Skills (EFS) Supporting Oral Feeding in Fragile Infants (SOFFI) Method
Theoretical Framework • The Synactive Theory of Development • Premise: Infant must learn to self-regulate and balance the environment • Promotes idea that caregivers can assess the infant determine oral feeding readiness
Implementation • Initial Survey • Questionnaire: collect basic demographic information, in addition to questions considering the nurses’ perception regarding attitudes towards current enteral feeding practices within our NICU (Fall/Winter of 2015) • Results: Unsure about feeding readiness tool, diverse responses from participants • The physicians and NNPs were most involved in the decision to oral feed the infants • GA and respiratory status were primary criteria for initiation of oral feeds • Success: Able to consume entire volume (50%)
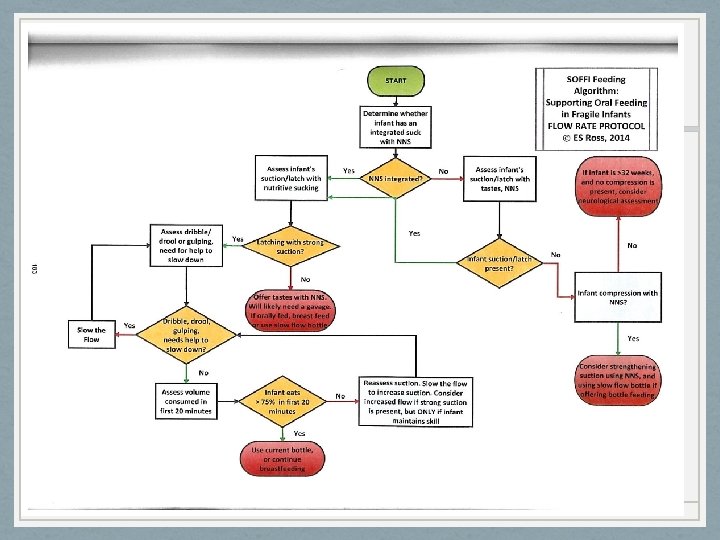
Implementation • Selection of Feeding Tools/Method • SOFFI Method • EFS documentation • Decision made to utilize SOFFI Method and documentation within EFS • EFS used to illustrate cues and infant states prior to, during, and after feedings (EFS closely aligns with SOFFI, checklist vs. algorithm)
Implementation • Education of Staff • Healthcare system hosted Dr. Erin Ross, creator of the SOFFI Method, to provide education on the method • I attended Dr. Ross’s lecture and used this information to provide education to the NICU staff • The education was provided to all NICU nursing staff at the monthly staff meetings • EFS education at nursing skills lab following SOFFI education • EFS flowsheet was placed on each nurse’s documentation layout (in EPIC) to assure access to flowsheet
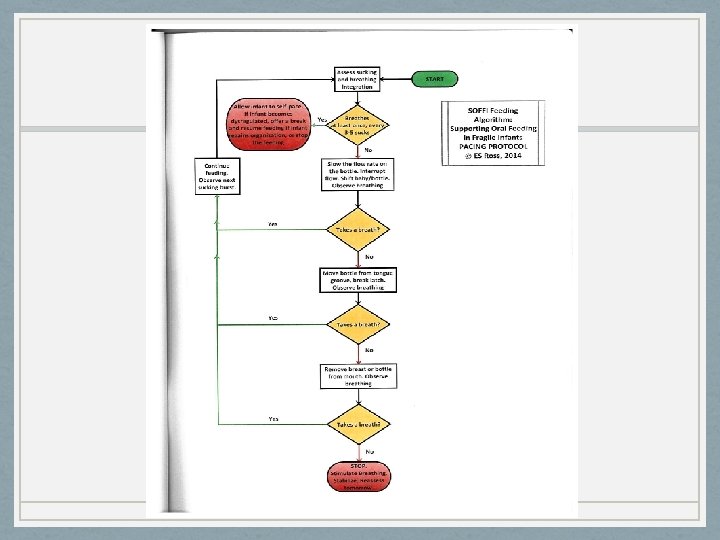
Implementation & Documentation Audit • SOFFI algorithm, Pacing Protocol, and Flow Rate Protocol placed at the each bedside • Detailed SOFFI algorithm on main unit computers • Go Live for SOFFI Method and EFS documentation 12/1/16 • Weekly chart audits in December

Follow-up Survey • To reevaluate current enteral feeding practices in the NICU • Illustrate how nursing perceptions regarding feeding practices have changed following SOFFI implementation • Similar survey as pre-implementation
Results • Chart audits- adequate documentation? • Weekly x 6 weeks • Reviewed charts on infants currently in the NICU (n=29) • Compliance 16 -27%
Results • Survey: N=15 • Demographics • • • All RNs 57% <6 years experience as NICU RN 43% >7 years experience as NICU RN 73% NICU RN for same time as NICU RN at this facility Shifts worked: 47% day shifts, 47% rotating shifts, <1% night shift • 46% participated in previous survey, 23% did not; 31% unsure
Results • Oral feeding practices • 93% state unit used feeding tool
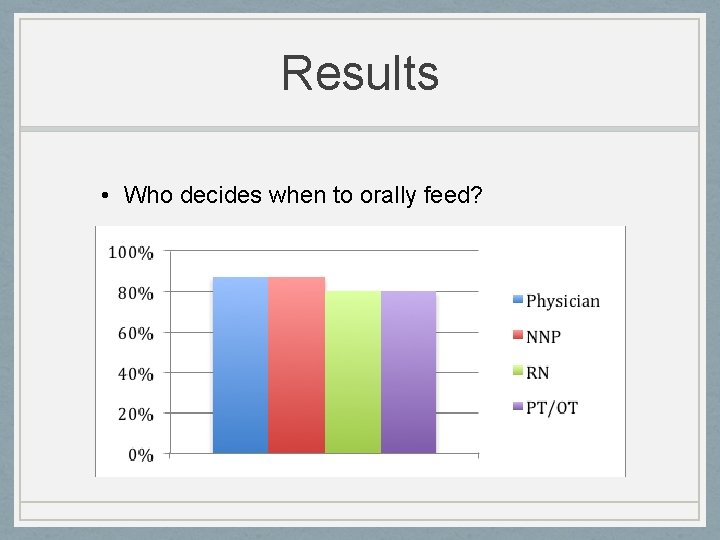
Results • Who decides when to orally feed?
Results • Criteria to initiate oral feedings • • Gestational age (85%) Respiratory status (92%) Infant displaying cues (100%) Infant successfully sucking on pacifier (85%)
Results • Oral feeding advancement • Volume (increased volume every few days) (92%) • Feeding orders • 54% stated their orders limit feeding volume • 62% stated their orders limit oral feeding frequency • 46% stated their orders limit feeding duration
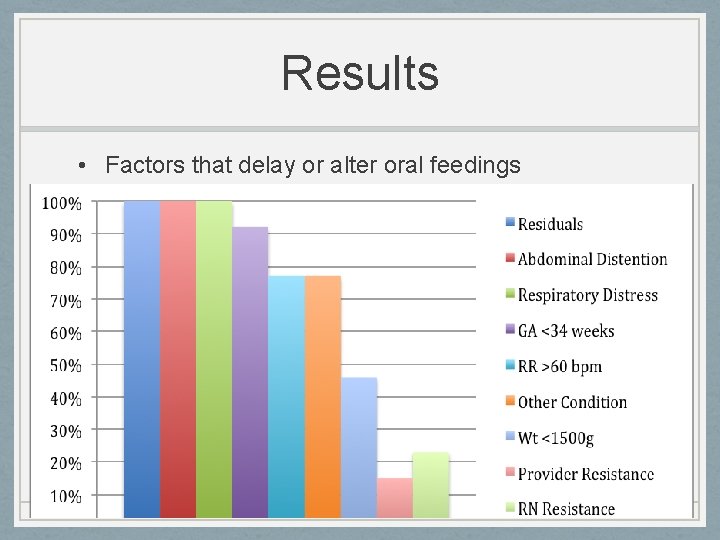
Results • Factors that delay or alter oral feedings
Results • Factors to stop an oral feeding and switch to gavage • Infant appears disinterested (100%) • Infant choking (92%) • Infant experiences apnea/bradycardia during feeding (92%) • Infant desaturates (92%) • Infant appears sleepy (92%)
Results • Nurses measure feeding success by • Infant nipples with a strong, coordinated suck (100%) • Infant does not experience desaturation during feeding (92%) • Infant does not experience apnea/bradycardia during feeding (92%) • Infant consumes entire volume of feeding (46%)
Results • Feeding techniques to support bottling success • • • Chin support (58%) External pacing (83%) Modified side-lying (100%) Cheek support (58%) Oxygen modification (67%)
Discussion • Barriers with implementation • Nurses did not comply (low compliance rate) • Despite education, some respondents still unaware of infant-driven feeding tool • RNs still measure feeding success by volume consumed (poor infant-driven feeding culture) • Management turnover (less buy-in)
Discussion • Barriers with implementation • Majority identified working in this NICU for the same amount of time as they have been RNs • No experience of other NICU feeding cultures • Resistant to change • Non-NICU staff/Travelers/Float Pool • Mainly care for low acuity infants (feeders) • No education on SOFFI or EFS documentation • Follow-up emails only went to NICU staff
References • Bertoncelli, N. , Cuomo, G. , Cattani, S. , Mazzi, C. , Pugliese, M. , Coccolini, E. , Zagni, P. , Mordini, B. , & Ferrari, F. (2012). Oral feeding competences of healthy preterm infants: A review. International Journal of Pediatrics, 1 -5. doi: 10. 1155/2012/896257 • Centers for Disease Control and Prevention. (2014). Preterm birth. Retrieved from http: //www. cdc. gov/reproductivehealth/Maternal. Infant. Health/Preterm. Birth. htm • Cormack, B. , Sinn, J. , Lui, K. , & Tudehope, D. (2013). Australasian neonatal intensive care enteral nutrition survey: Implications for practice. Journal of Pediatrics and Child Health, 49, E 340 -E 347. doi: 10. 111/jpc. 122016 • Costa, S. P. , & Schans, C. P. (2008). The reliability of the neonatal oral-motor assessment scale. Acta Paediatrica, 97(1), 21 -26. Doi: 10. 1111/j. 1651 -2227. 2007. 00577. x • Gennattasio, A. , Perri, E. A. , Baranek, D. , & Rohan, A. (2015). Oral feeding readiness assessment in premature infants. The American Journal of Maternal Child Nursing, 40(2), 96 -104. doi: 10. 1097/NMC. 0000000115 • Gregory, K. E. , & Connolly, T. C. (2012). Enteral feeding practices in the NICU: Results from a 2009 neonatal enteral feeding survey. Advances in Neonatal Care, 12(1), 46 -55. doi: 10. 1097/anc. 0 b 013 e 3182425 aab • Kirk, A. T. , Alder, S. C. , & King, J. D. (2007). Cue-based oral feeding clinical pathway results in earlier attainment of full oral feeding in premature infants. Journal of Perinatology, 27(9), 572 -578. doi: 10. 1038/sj. jp. 7211791
References • Laptook, A. R. (2013). Neurologic and metabolic issues in moderately preterm, late preterm, and early term infants. Clinics in Perinatology, 40(4), 723 -738. doi: 10. 1016/j. clp. 2013. 07. 005 • Ludwig, S. M. , & Waitzman, K. A. (2007). Changing feeding documentation to reflect infant-driven feeding practice. Newborn and Infant Nursing Reviews, 7(3), 155 -160. Doi: 10. 1053/j. nainr. 2007. 06. 007 • National Association of Neonatal Nurses. (2011). Age-appropriate care of the premature and critically ill hospitalized infant: Guideline for practice. Retrieved from http: //www. nann. org/uploads/Age-Appropriate_Care. FINAL_11 -01 -11. pdf • National Institute of Nursing Research. (2012). Fiscal year 2013 budget request. Retrieved from https: //www. ninr. nih. gov/sites/www. ninr. nih. gov/files/NINRFY 2013 Opening. Statement. FINALfor. Web. pdf • Newland, L. , L’Huillier, M. W. , & Petrey, B. (2013). Implementation of cue-based feeding in a level III NICU. Neonatal Network, 32(2), 132 -137. doi: 10. 1891/0730 -0832. 2. 132 • Pickler, R. H. (2004). A model of feeding readiness for preterm infants. Neonatal Intensive Care: The Journal of Perinatology - Neonatology, 17(4), 31 -36. Retrieved from http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 1317102/ • Puckett, B. , Grover, V. K. , Holt, T. , & Sankaran, K. (2008). Cue-based feeding for preterm infants: A prospective trial. American Journal of Perinatology, 25(10), 623 -628. doi: 10. 1055/s-0028 -1090583
References • Ross, E. S. , & Philbin, M. K. (2011). The SOFFI Reference Guide: Text, Algorithms, and Appendices: A Manualized Method for Quality Bottle-Feedings. Journal Of Perinatal & Neonatal Nursing, 25(4), 349 -357. • Shaker, C. S. (2012 a). Cue-based feeding in your NICU: Food for thought. Retrieved from http: //www. nann. org/enews/November-2012/feature. html • Shaker, C. S. (2012 b). Feed me only when I’m cueing: Moving away from a volume-driven culture in the NICU. Retrieved from https: //shaker 4 swallowingandfeeding. files. wordpress. com/2013/02/shaker-cue-based-feeding 2012. pdf • Shaker, C. S. (2013). Cue-based feeding in the NICU: Using the infant’s communication as a guide. Neonatal Network, 32(6), 404 -408. Doi: 10. 1891/0730 -0832. 6. 404 • Thoyre, S. M. , Shaker, C. S. , & Pridham, K. F. (2005). The early feeding skills assessment for preterm infants. Neonatal Network, 24(3), 7 -16. doi: 10. 1891/0730 -0832. 24. 3. 7 • United States Department of Health and Human Services, Healthy People 2020. (2015). Maternal, infant, and child health. Retrieved from http: //www. healthypeople. gov/2020/leading-health-indicators/2020 -lhitopics/Maternal-Infant-and-Child-Health • Waitzman, K. A. , Ludwig, S. M. , & Nelson, C. L. (2014). Contributing to content validity of the infant-driven feeding scales through Delphi surveys. Newborn and Infant Nursing Reviews, 14(3), 88 -91. doi: 10. 1053/j. naiinr. 2014. 06. 010
References • Wellingtown, A. , & Perlman, J. M. (2015). Infantdriven feeding in premature infants: A quality improvement project. Archives of Diseases in Childhood, Fetal and Neonatal Edition, F 1 -F 6. doi: 10. 1136/archdischild-2015 -308296 • World Health Organization. (2013). What health challenges do preterm babies face? Retrieved from http: //www. who. int/features/qa/preterm_health_ch allenges/en/
- Slides: 35