CCRNPCCN Certification Review Hematology CCRN and PCCN Test
- Slides: 47
CCRN-PCCN Certification Review Hematology
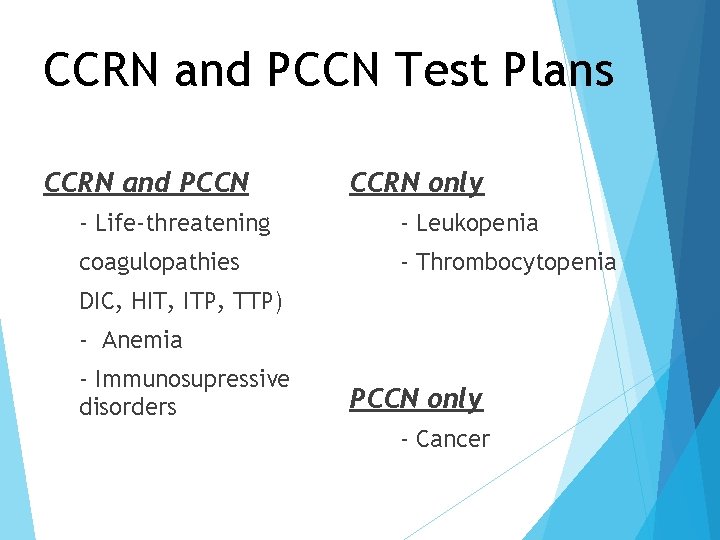
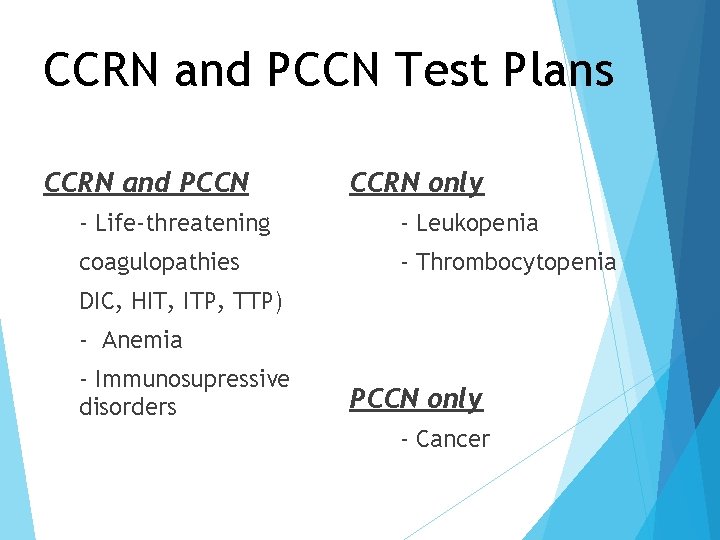
CCRN and PCCN Test Plans CCRN and PCCN CCRN only - Life-threatening - Leukopenia coagulopathies - Thrombocytopenia DIC, HIT, ITP, TTP) - Anemia - Immunosupressive disorders PCCN only - Cancer
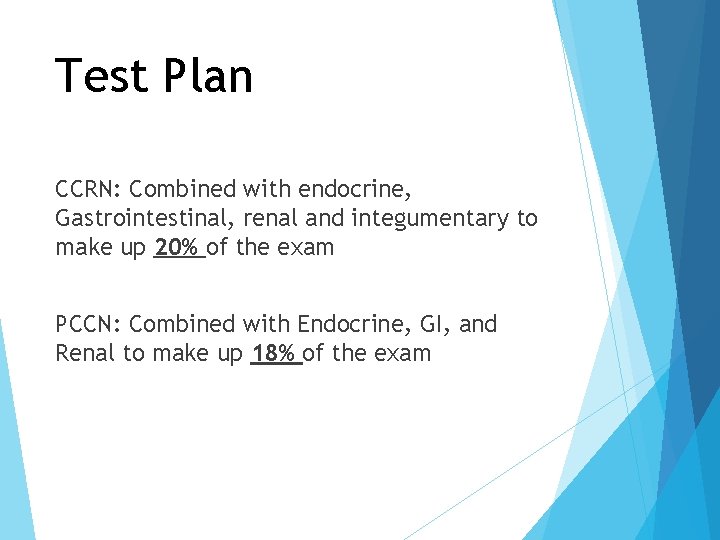
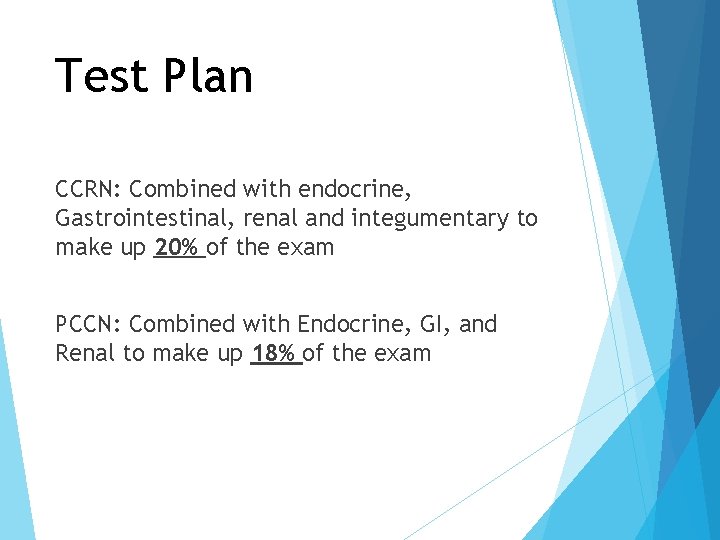
Test Plan CCRN: Combined with endocrine, Gastrointestinal, renal and integumentary to make up 20% of the exam PCCN: Combined with Endocrine, GI, and Renal to make up 18% of the exam
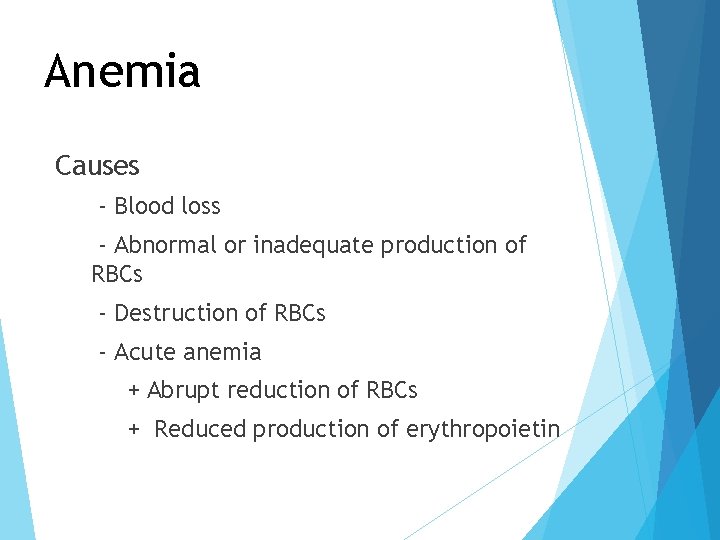
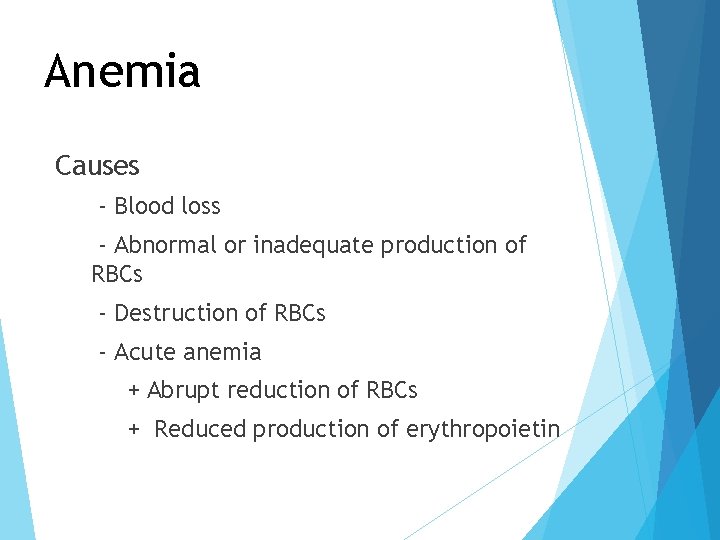
Anemia Causes - Blood loss - Abnormal or inadequate production of RBCs - Destruction of RBCs - Acute anemia + Abrupt reduction of RBCs + Reduced production of erythropoietin
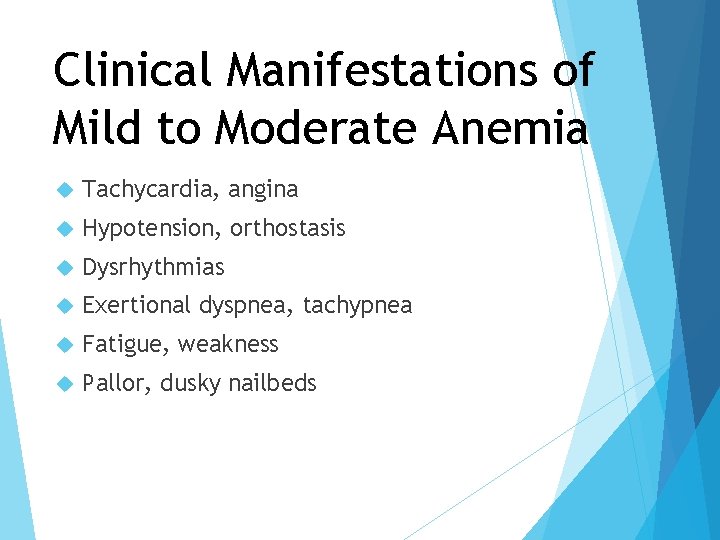
Clinical Manifestations of Mild to Moderate Anemia Tachycardia, angina Hypotension, orthostasis Dysrhythmias Exertional dyspnea, tachypnea Fatigue, weakness Pallor, dusky nailbeds
Clinical Manifestations of Severe Anemia Decreased oxygen delivery to tissues Anaerobic metabolism Lactate production Myocardial infarction Ischemic stroke
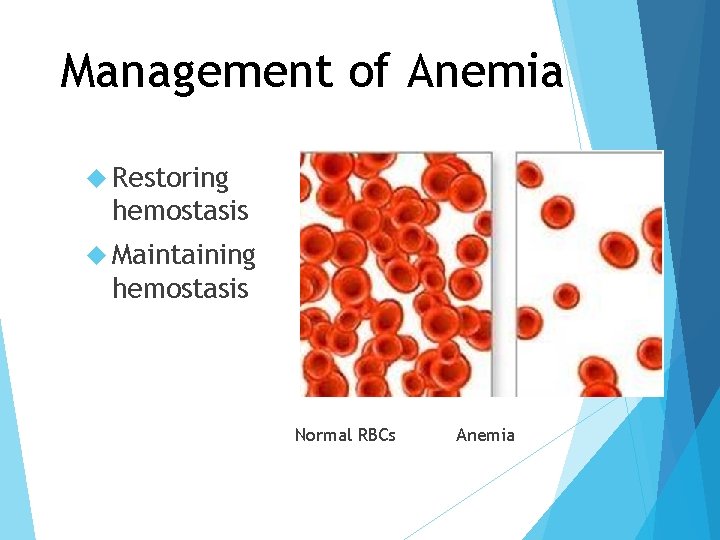
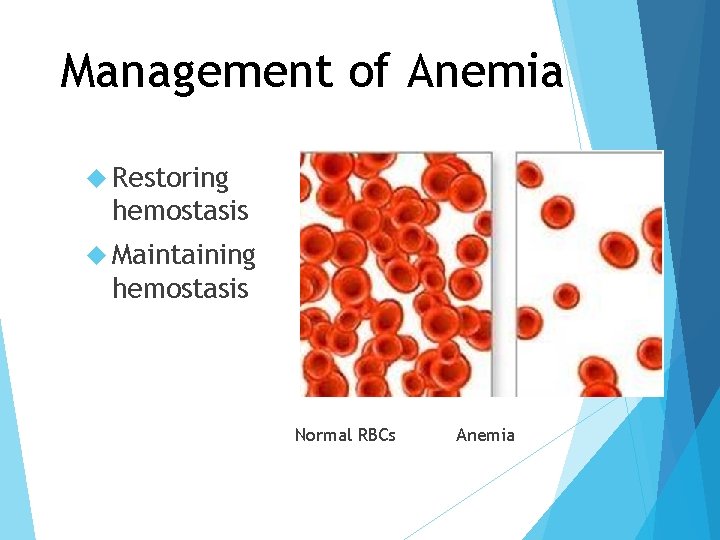
Management of Anemia Restoring hemostasis Maintaining hemostasis Normal RBCs Anemia
Management of Anemia Improve oxygen delivery Supplemental RBC oxygen transfusion to replete hemoglobin Other volume replacement Monitor patient vital signs, response to therapy Minimize activity
Management of Anemia Identifying & treating underlying disease states Diagnostic tests (labs, radiologic, endoscopic) Erythropoietin to increase marrow production in chronic anemia Iron preparation Vitamin B 12 & folic acid
Management of Anemia Minimize blood loss/reduce transfusions Small volume blood collection tubes Daily assessment of routine blood draws Autologous blood donation Prophylaxis against GI bleeding
Who Should be Transfused? Controversial & varying practices Optimal hemoglobin & hematocrit level for acutely ill adults has not been determined Transfusion triggers: Controversial Restrictive transfusion thresholds now common H/H of 7/21 to 8/24 Avoidance of unnecessary transfusion
Whole Blood Indication Symptomatic anemia with large volume deficit Benefit Increases oxygen-carrying capacity Increases blood volume
Packed Red Blood Cells Indication: Symptomatic anemia Benefit Increases oxygen- carrying capacity Increases hbg by 1 gm/dl and hct by 2 -3%
Leukocyte Reduction Indications: Preventing non-hemolytic febrile transfusion reactions Preventing CMV transmission by cellular blood components Preventing or delaying alloimmunization to leukocyte antigens in selected patients who are chronic transfusion candidates
Irradiated Blood Products Prevention of Transfusion Associated Graft versus Host Disease Transplant patients Bone marrow recipients Cancer patients such as Lymphoma Neonates Persons with congenital immune deficiency syndromes
Platelets Indication Bleeding due to thrombocytopenia or platelet function abnormality Benefit Corrects Aids low platelet levels in clotting
Fresh Frozen Plasma Indication Deficiency of labile and stable plasma coagulation factors TTP Benefit Source of deficient of defective plasma proteins
Cryoprecipitate Indications Hemophilia von A Willebrand’s disease Replaces clotting factors, including factors VIII and XIII Benefits Improves hemostasis
Albumin Indications Volume expansion Benefit Hypertonic solution draws fluid from interstitium into vascular space Developed Does from plasma not require crossmatching
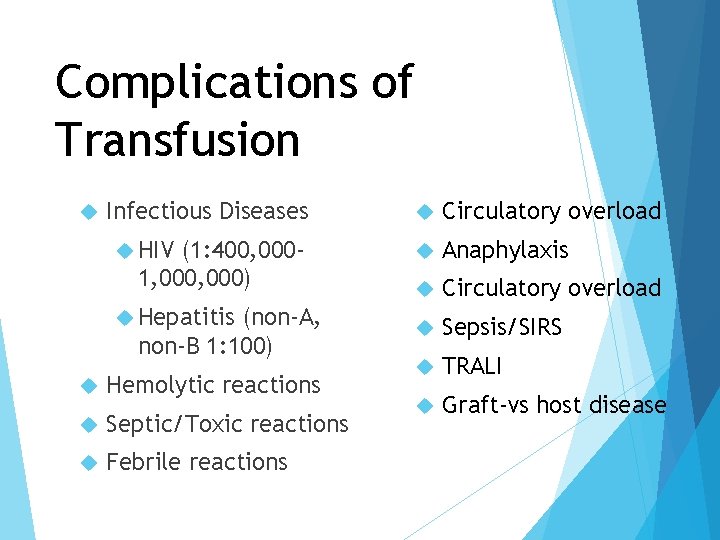
Complications of Transfusion Infectious Diseases HIV (1: 400, 0001, 000) Hepatitis (non-A, non-B 1: 100) Hemolytic reactions Septic/Toxic reactions Febrile reactions Circulatory overload Anaphylaxis Circulatory overload Sepsis/SIRS TRALI Graft-vs host disease
Care of the Patient with Coagulopathies Acutely ill hospitalized adults develop coagulopathies due to abnormalities in: Platelets Hemostasis Fibrinolysis Combination of all factors
Disseminated Intravascular Coagulation (DIC) Accelerated activation of clotting cascade Depletion of clotting factors Bleeding Secondary problem
Pathophysiology Initiating event: procoagulants Stimulation of intrinsic or extrinsic pathway Clots in microvasculature Consumption of clotting factors Fibrinolysis FDPs: potent anticoagulants
Etiology Infection Trauma (e. g. burns, crush) Obstetric conditions (e. g. abruptio, amniotic fluid embolus, retained dead fetus) Hematologic disorders Oncologic disorders Other: shock or sepsis, acute respiratory distress syndrome
Clinical Manifestations of DIC Hemorrhage- predominant clinical finding Sites of injury Surgical incisions Venipuncture Gastric ulcers sites
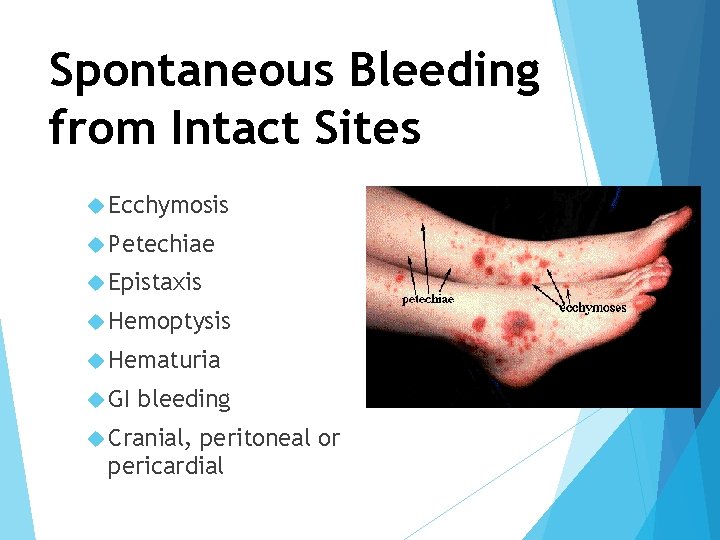
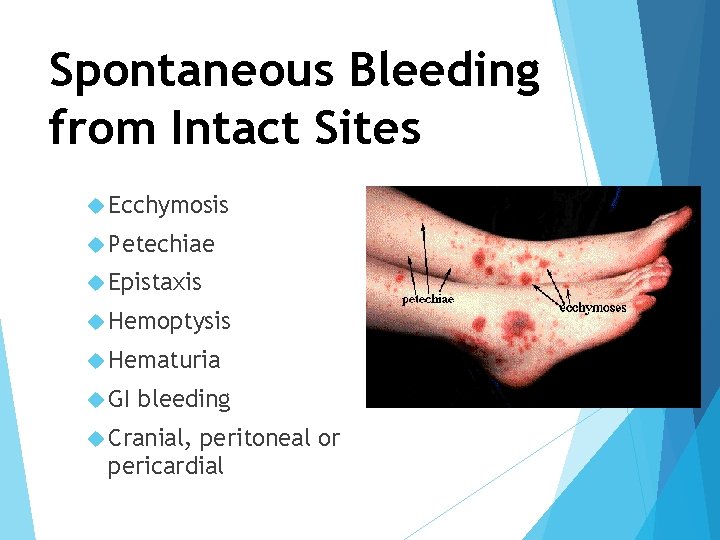
Spontaneous Bleeding from Intact Sites Ecchymosis Petechiae Epistaxis Hemoptysis Hematuria GI bleeding Cranial, peritoneal or pericardial
Thrombotic Manifestations of DIC Result in obstruction of blood flow to multiple organ systems and multiple system failure Ischemia to end organs Major cause of morbidity, mortality in DIC Overt Bleeding or oozing Decreased perfusion to organs Changes in mental status Infarction of tissue in digits and nose
Laboratory Diagnosis Decreased platelets Decreased fibrinogen Prolonged PT, a. PTT, thrombin time Elevated FDP or FSP Increased D-Dimer Decrease in coagulating factors Decrease in hemoglobin and hematocrit
Treatment Correct the underlying cause Administer blood and components Platelets Fresh frozen plasma Cryoprecipitate Packed RBCs Stop abnormal coagulation Heparin
Nursing Management Assess and Prevent Frequent Laboratory analysis Administration of Blood products Assess circulation Relieve Pain Assess of complications: shock, multisystem organ failure, impaired circulation
Heparin Induced Thrombocytopenia (HIT)
Type II HIT Serious immune-mediated syndrome in which the administration of heparin is associated with Thrombocytopenia Generation of heparin dependent antibodies Thrombosis caused by formation of heparinantibody complexes Adhere to platelet and endothelial surfaces Release thrombin Formation of platelet clumps
Clinical Presentation Following the initiation of heparin thrombocytopenia observed 5 -14 days later or may occur sooner with previous exposure Platelet count <100, 000 or Platelet count 50% of baseline (preheparin value)
Laboratory Tests for HIT Platelet Key count indicator Drop of 30 -50% or less than 50, 000/mm 3 Enzyme-linked immunosorbent assay (ELISA) Identifies antigen presence of HIT
Complications of HIT Due to clumping of platelets, plateletantibody complexes, and thrombin Deep vein thrombosis Pulmonary embolism Myocardial infarction Occlusion of limb arteries (possibly resulting in amputation) Cerebrovascular accidents Skin necrosis End-organ damage (eg, adrenal, bowel, spleen, gallbladder or hepatic infarction; renal failure) Death
Treatment Discontinue all heparin containing Unfractionated heparin Low molecular weight heparin Heparin flush Heparin-coated catheter Administer products medications that inhibit thrombin formation, or cause direct thrombin inhibition Lepirudin (Refludan) Bivalirudin (Angiomax) Argatroban
Idiopathic Thrombocytopenia Purpura (ITP) Autoimmune destruction of platelets Primary disorder or due to AIDS, SLE, drugs Results in petechiae, purpura, epistaxis Management Steroids IVIG Splenectomy
Thrombotic Thrombocytopenia Purpura (TTP) Viral or associated with toxin in E. coli Hemolytic anemia, fever, renal failure, widespread vascular occlusion, bleeding Management with plasmapheresis
Etiology of Immunosupression Chronically ill Sepsis Genetic Disorders Viral infections such as HIV Radiation therapy Immunosupressive treatments such as chemo or antirejection drugs Autoimmune disorders Diseases (Diabetes) Neutropenia
Nursing Care Meticulous personal hygiene Aseptic technique Minimize invasive procedures Manipulate environment to minimize exposure to organisms Restrict exposure to persons with infection Adequate nutrition Alleviation of stress
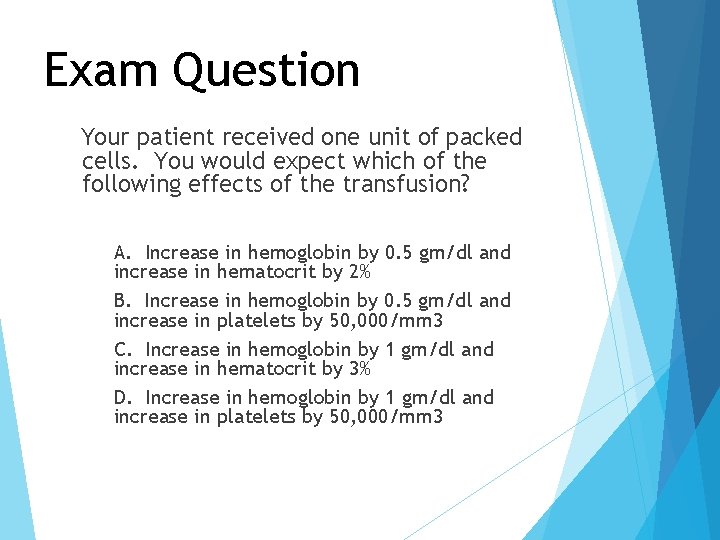
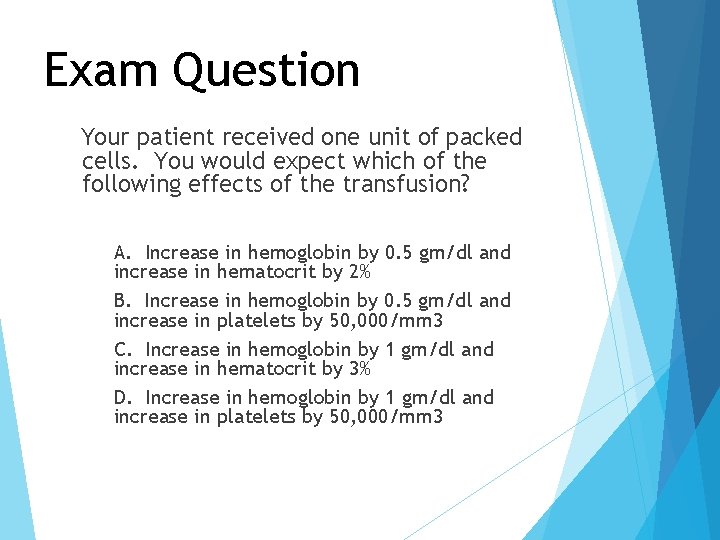
Exam Question Your patient received one unit of packed cells. You would expect which of the following effects of the transfusion? A. Increase in hemoglobin by 0. 5 gm/dl and increase in hematocrit by 2% B. Increase in hemoglobin by 0. 5 gm/dl and increase in platelets by 50, 000/mm 3 C. Increase in hemoglobin by 1 gm/dl and increase in hematocrit by 3% D. Increase in hemoglobin by 1 gm/dl and increase in platelets by 50, 000/mm 3
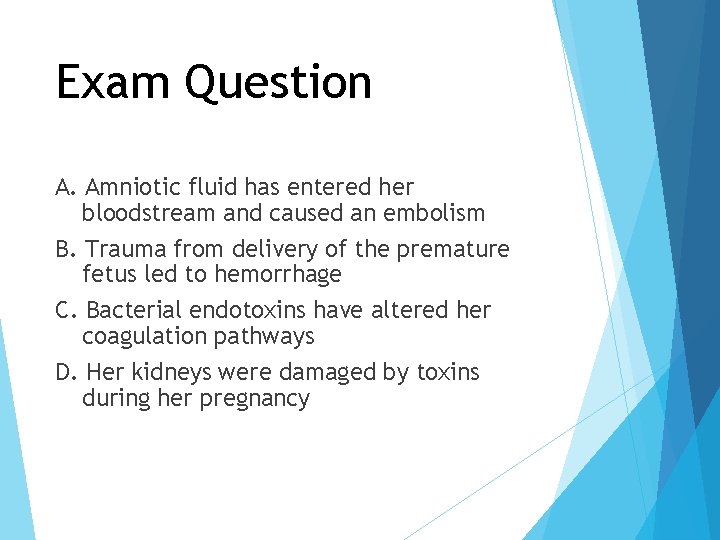
Exam Question (I) A young woman did not seek medical care during her brief, unwanted pregnancy owing to her cultural beliefs as well as to economic challenges. One week ago, the patient’s grandmother helped her to end the pregnancy, using traditional methods.
Exam Question (II) Today the woman collapsed at school and was transported to the hospital exhibiting petechiae on her skin and difficulty breathing. Which of the following best explains the pathophysiology underlying this patient’s condition?
Exam Question A. Amniotic fluid has entered her bloodstream and caused an embolism B. Trauma from delivery of the premature fetus led to hemorrhage C. Bacterial endotoxins have altered her coagulation pathways D. Her kidneys were damaged by toxins during her pregnancy
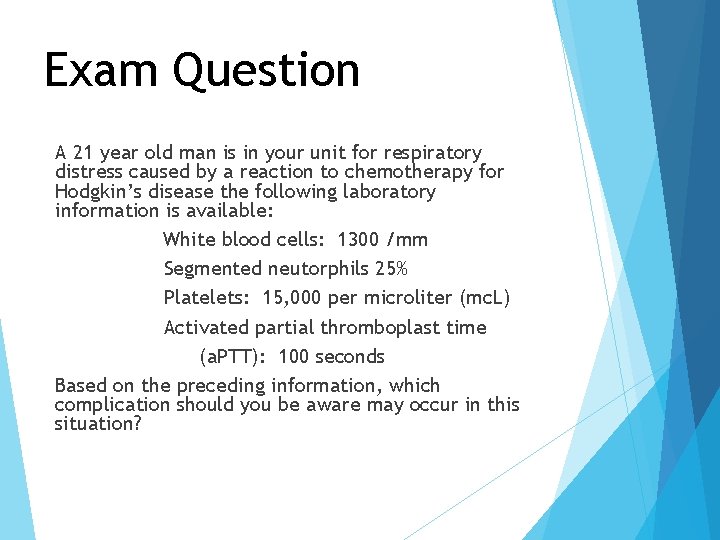
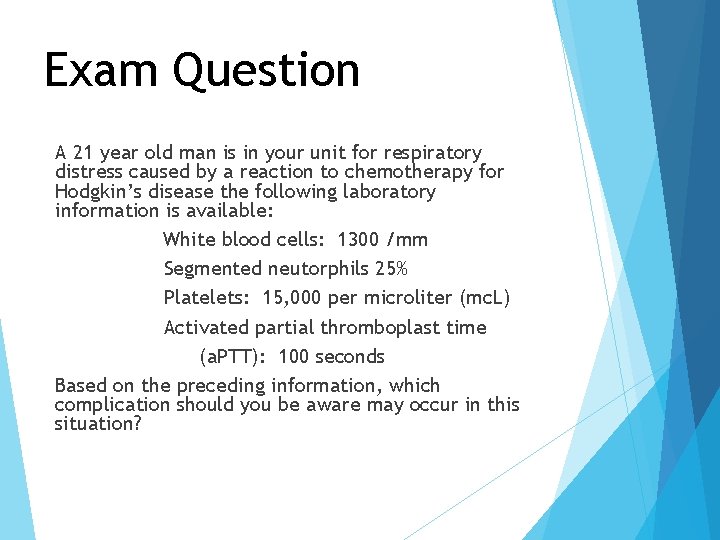
Exam Question A 21 year old man is in your unit for respiratory distress caused by a reaction to chemotherapy for Hodgkin’s disease the following laboratory information is available: White blood cells: 1300 /mm Segmented neutorphils 25% Platelets: 15, 000 per microliter (mc. L) Activated partial thromboplast time (a. PTT): 100 seconds Based on the preceding information, which complication should you be aware may occur in this situation?
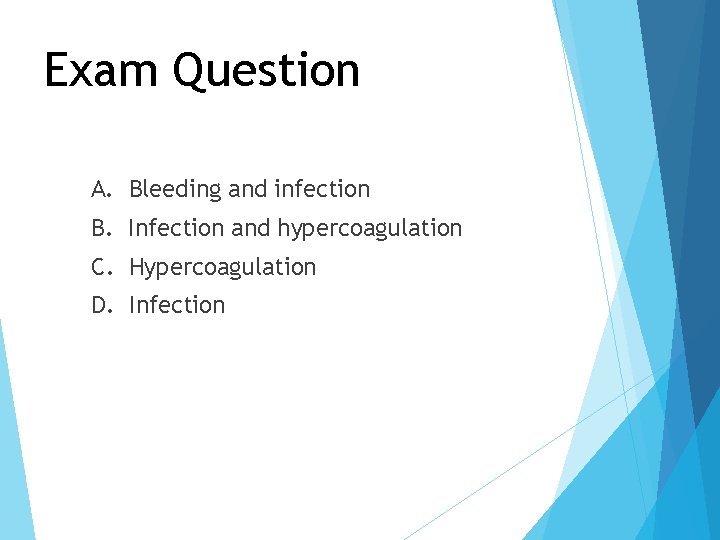
Exam Question A. Bleeding and infection B. Infection and hypercoagulation C. Hypercoagulation D. Infection
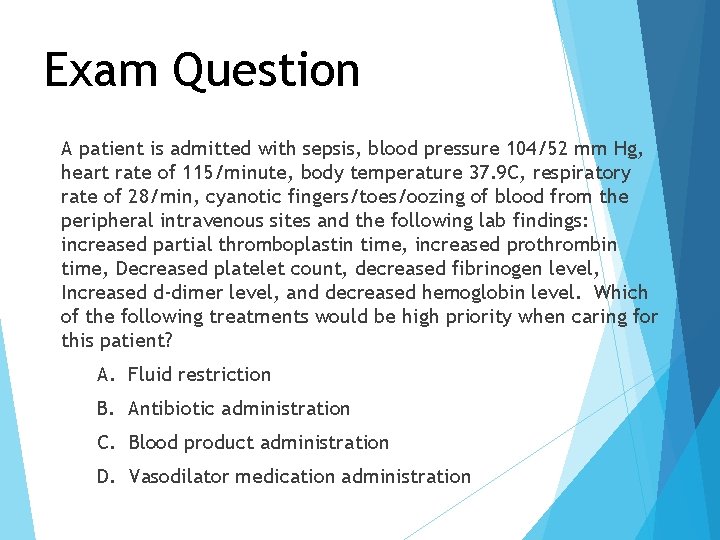
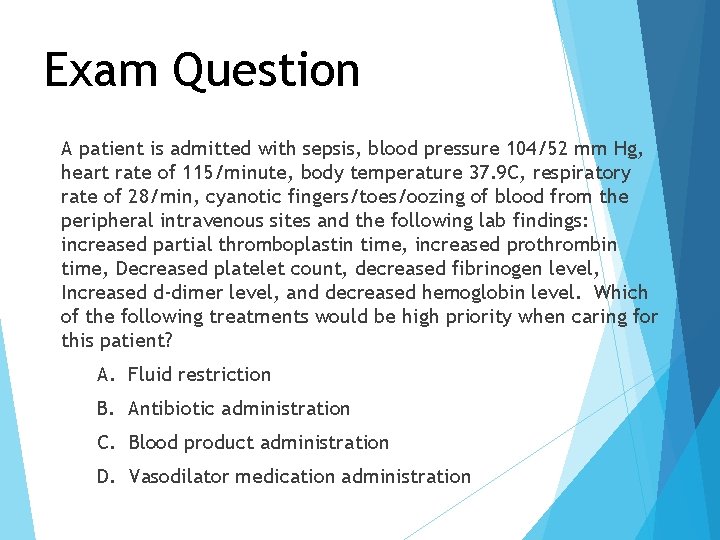
Exam Question A patient is admitted with sepsis, blood pressure 104/52 mm Hg, heart rate of 115/minute, body temperature 37. 9 C, respiratory rate of 28/min, cyanotic fingers/toes/oozing of blood from the peripheral intravenous sites and the following lab findings: increased partial thromboplastin time, increased prothrombin time, Decreased platelet count, decreased fibrinogen level, Increased d-dimer level, and decreased hemoglobin level. Which of the following treatments would be high priority when caring for this patient? A. Fluid restriction B. Antibiotic administration C. Blood product administration D. Vasodilator medication administration