CASES Dr Harsha K J 2 nd yr




- Slides: 61
CASES Dr. Harsha K J 2 nd yr resident, Department of Radiodiagnosis, Baroda Medical College, Baroda. 1
CASE 1 2
• Young adult woman with anorexia, and progressive confusion following fever with upper respiratory infection. • The patient also developed multifocal motor and sensory deficits. • CSF studies showed • increased white cell counts with lymphocyte predominance, • elevated protein & decreased glucose levels. • Cultures, however, were negative. 3
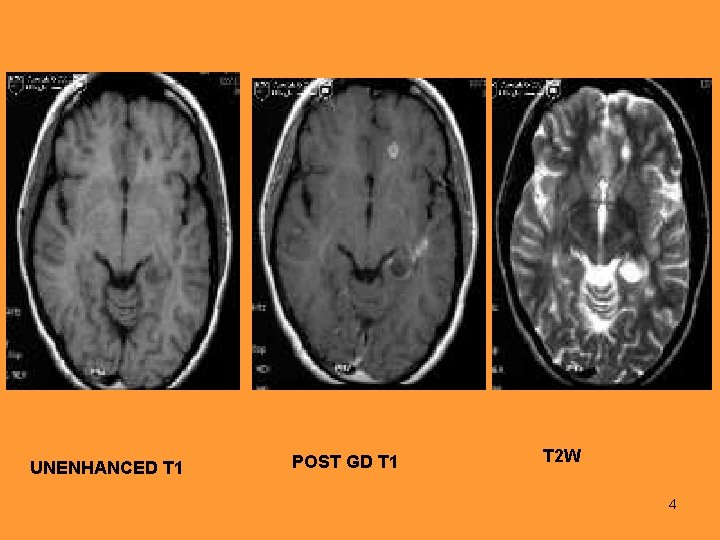
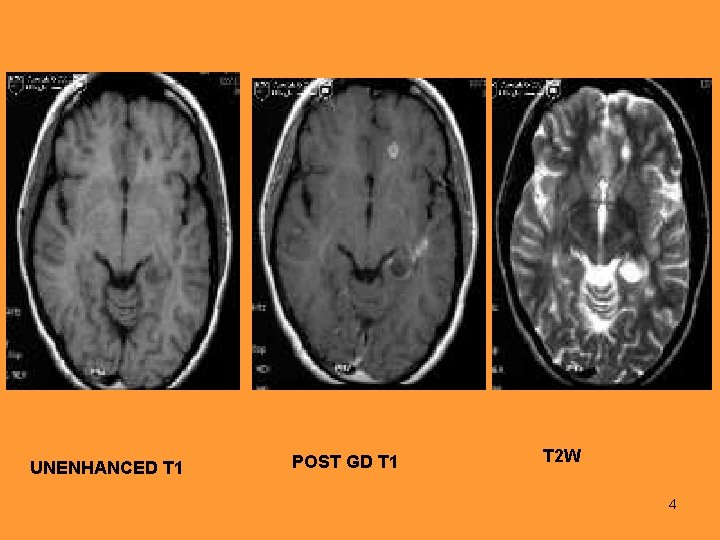
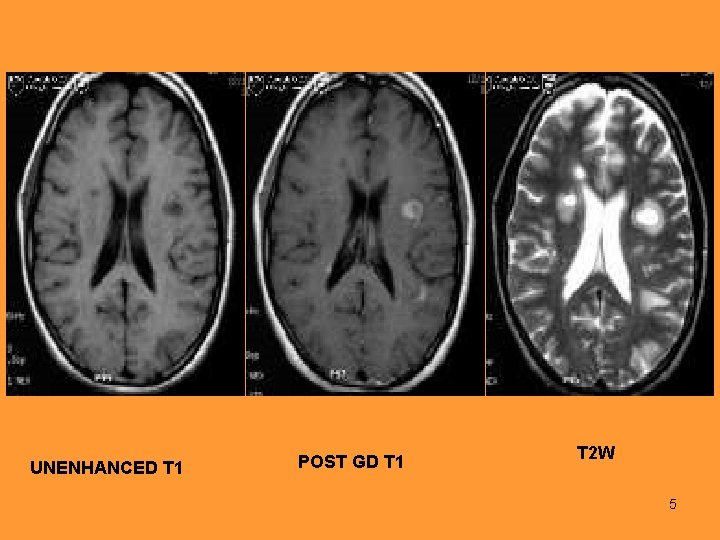
UNENHANCED T 1 POST GD T 1 T 2 W 4
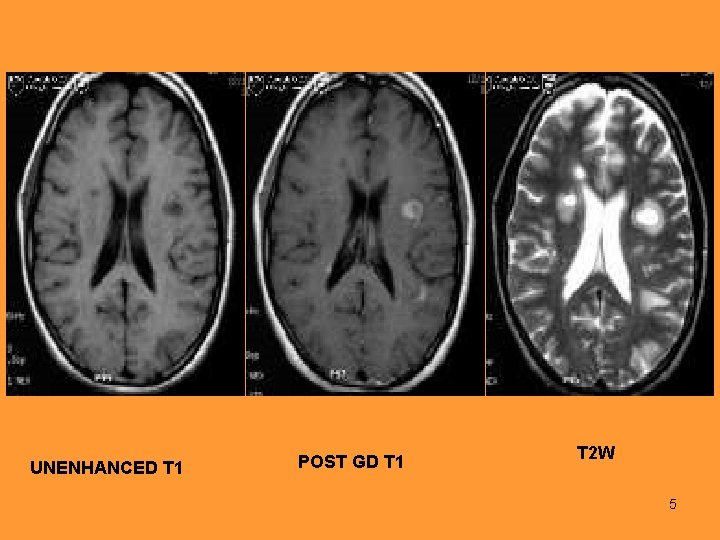
UNENHANCED T 1 POST GD T 1 T 2 W 5
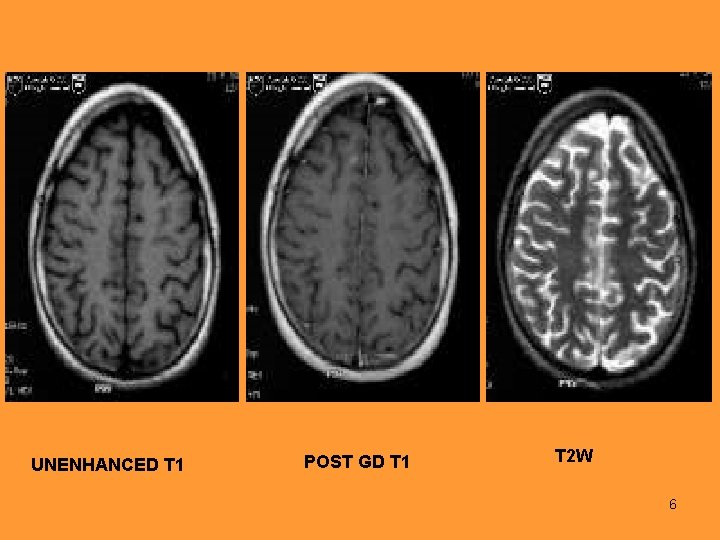
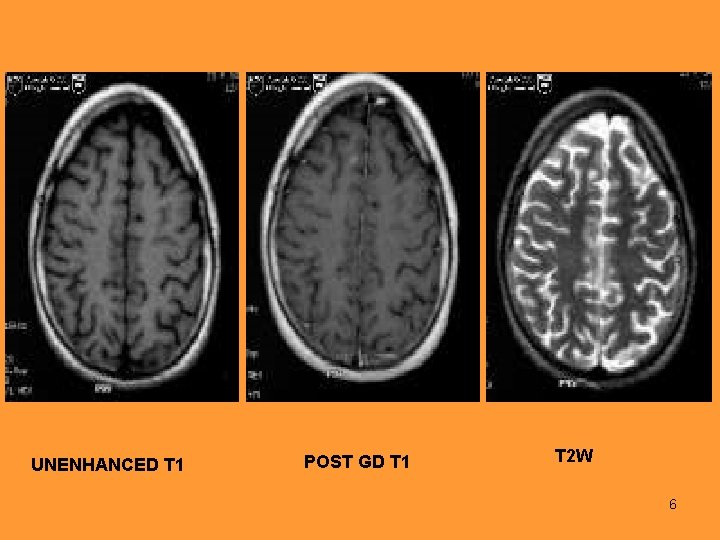
UNENHANCED T 1 POST GD T 1 T 2 W 6
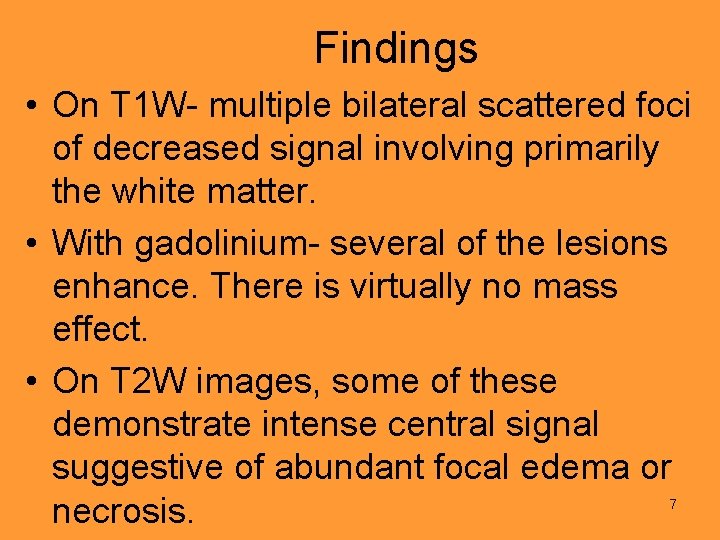
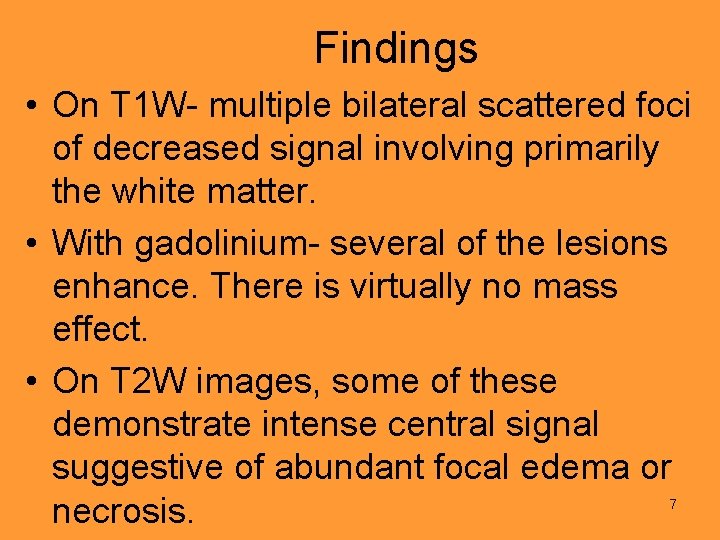
Findings • On T 1 W- multiple bilateral scattered foci of decreased signal involving primarily the white matter. • With gadolinium- several of the lesions enhance. There is virtually no mass effect. • On T 2 W images, some of these demonstrate intense central signal suggestive of abundant focal edema or necrosis. 7
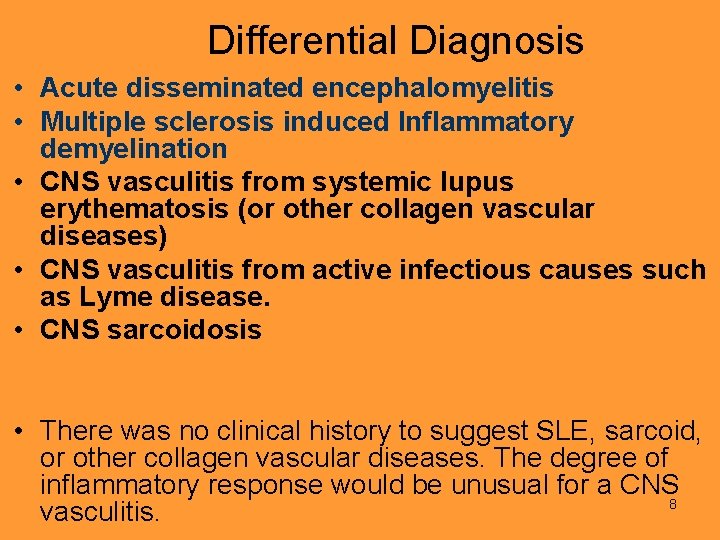
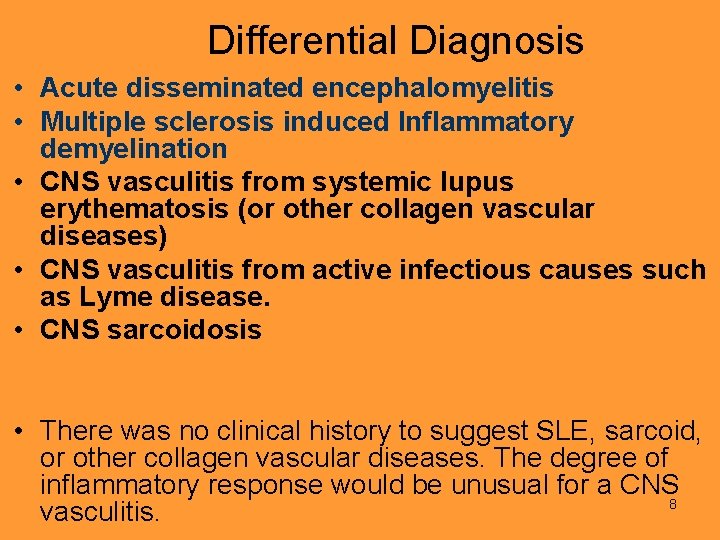
Differential Diagnosis • Acute disseminated encephalomyelitis • Multiple sclerosis induced Inflammatory demyelination • CNS vasculitis from systemic lupus erythematosis (or other collagen vascular diseases) • CNS vasculitis from active infectious causes such as Lyme disease. • CNS sarcoidosis • There was no clinical history to suggest SLE, sarcoid, or other collagen vascular diseases. The degree of inflammatory response would be unusual for a CNS 8 vasculitis.
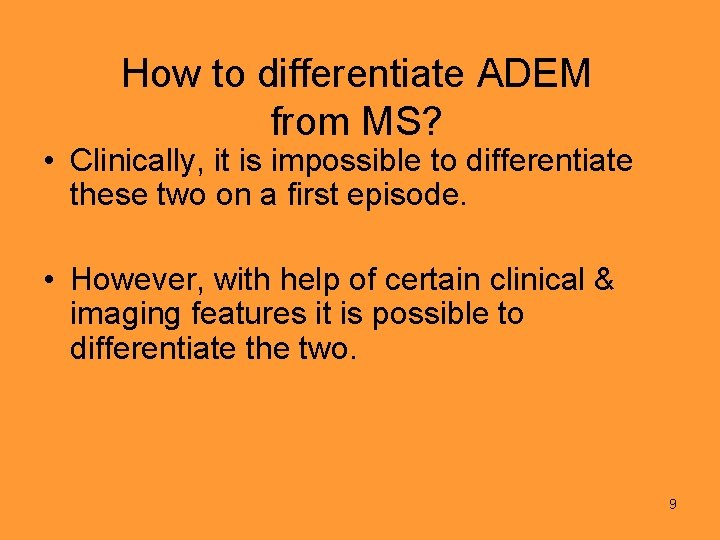
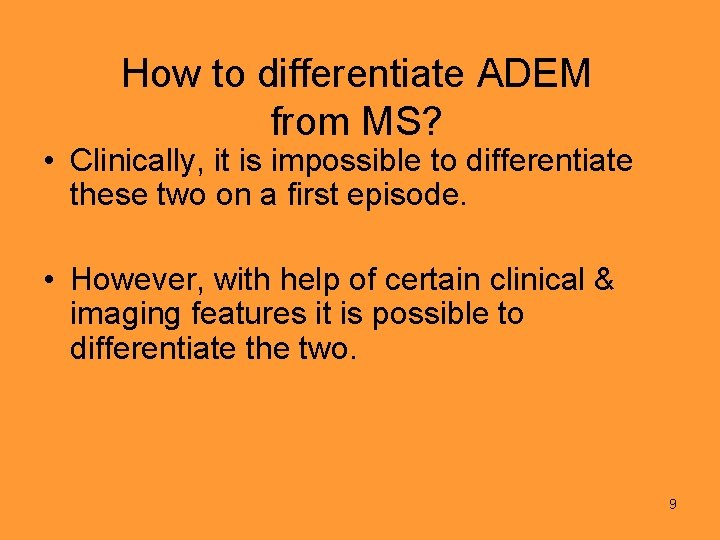
How to differentiate ADEM from MS? • Clinically, it is impossible to differentiate these two on a first episode. • However, with help of certain clinical & imaging features it is possible to differentiate the two. 9
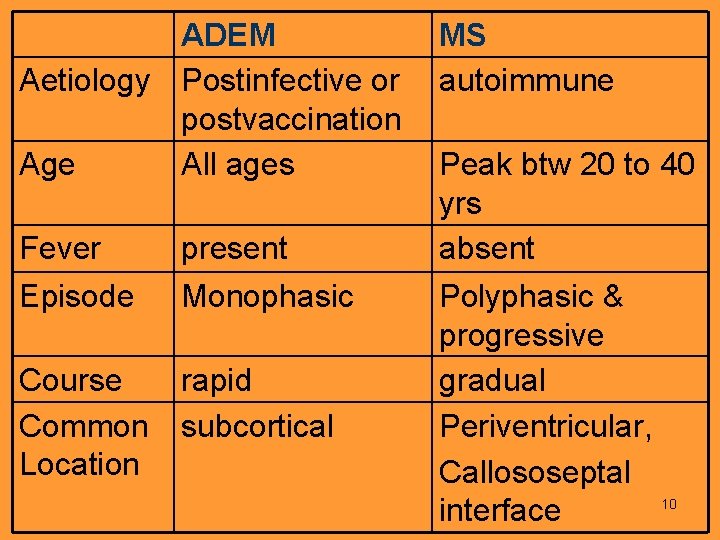
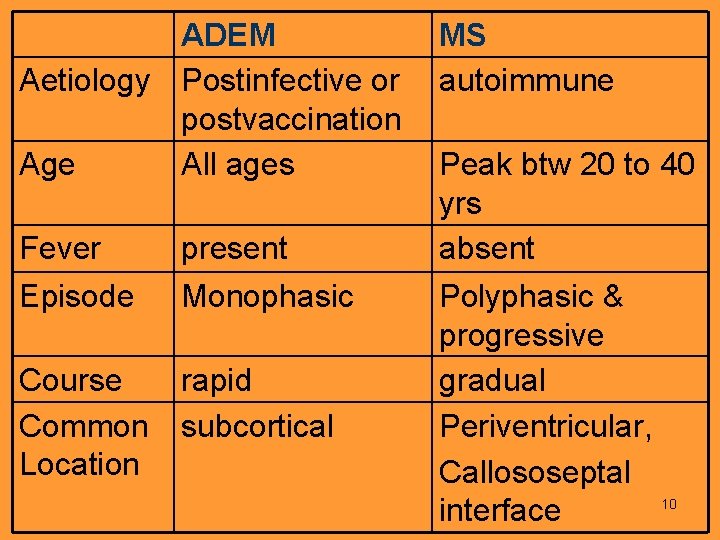
ADEM MS Aetiology Postinfective or autoimmune postvaccination Age All ages Peak btw 20 to 40 yrs Fever present absent Episode Monophasic Polyphasic & progressive Course rapid gradual Common subcortical Periventricular, Location Callososeptal 10 interface
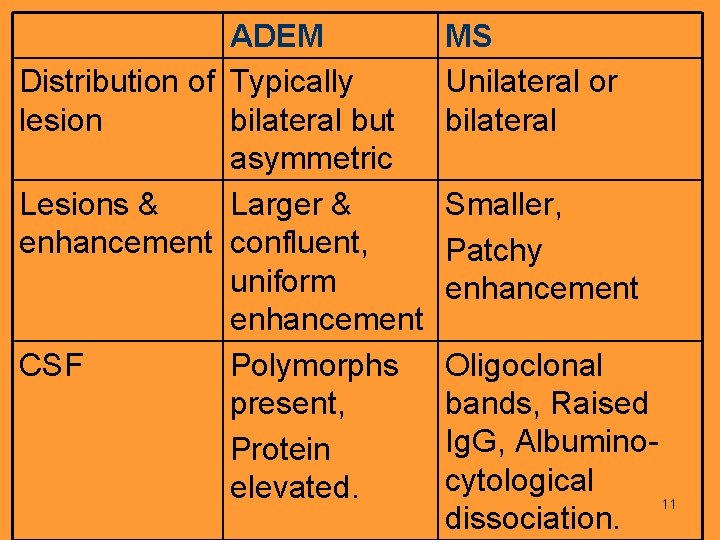
ADEM Distribution of Typically lesion bilateral but asymmetric Lesions & Larger & enhancement confluent, uniform enhancement CSF Polymorphs present, Protein elevated. MS Unilateral or bilateral Smaller, Patchy enhancement Oligoclonal bands, Raised Ig. G, Albuminocytological 11 dissociation.
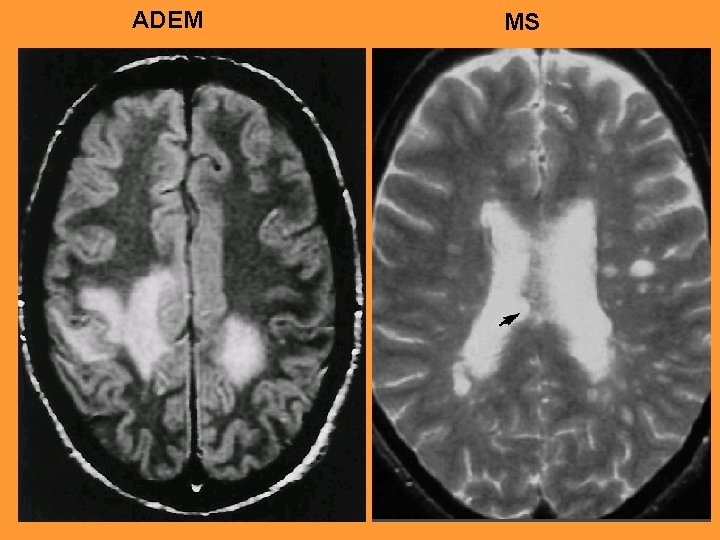
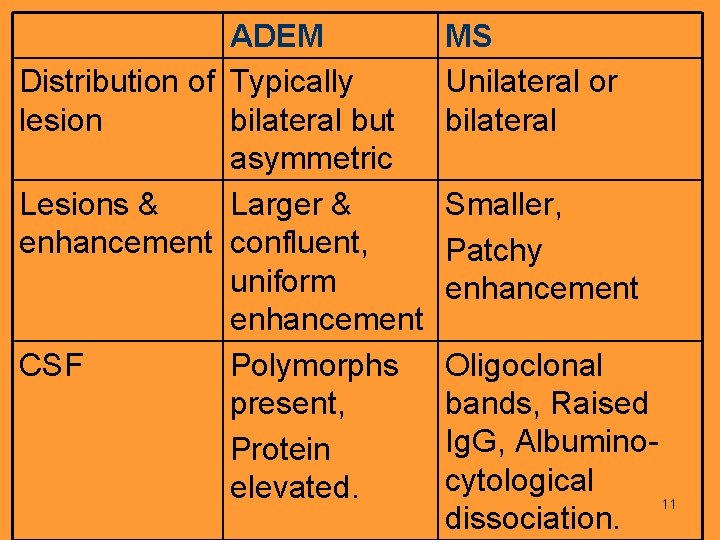
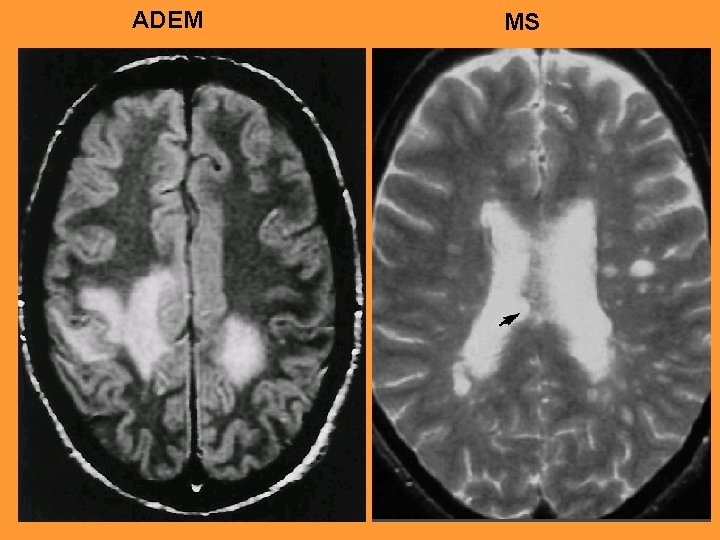
ADEM MS 12
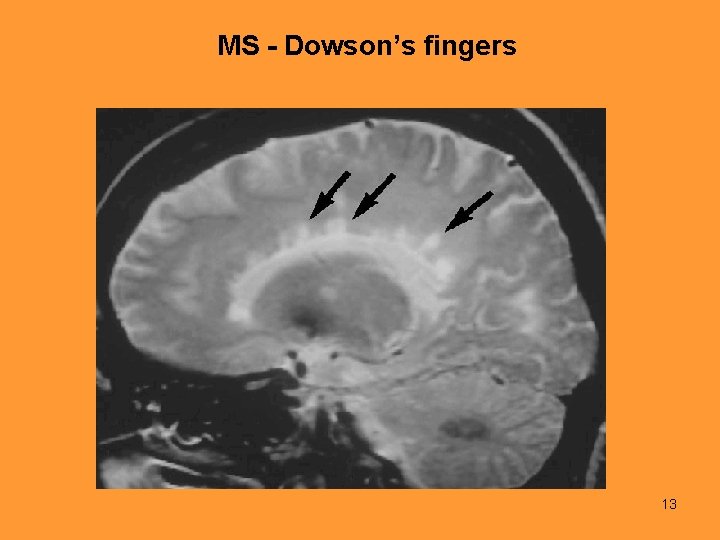
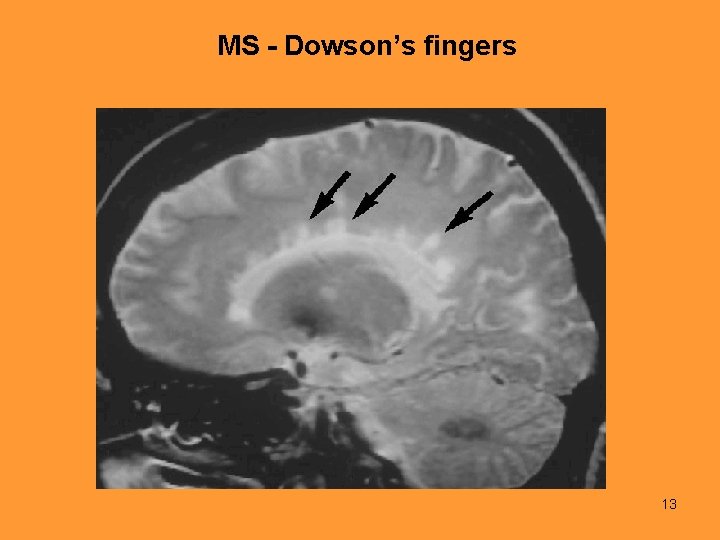
MS - Dowson’s fingers 13
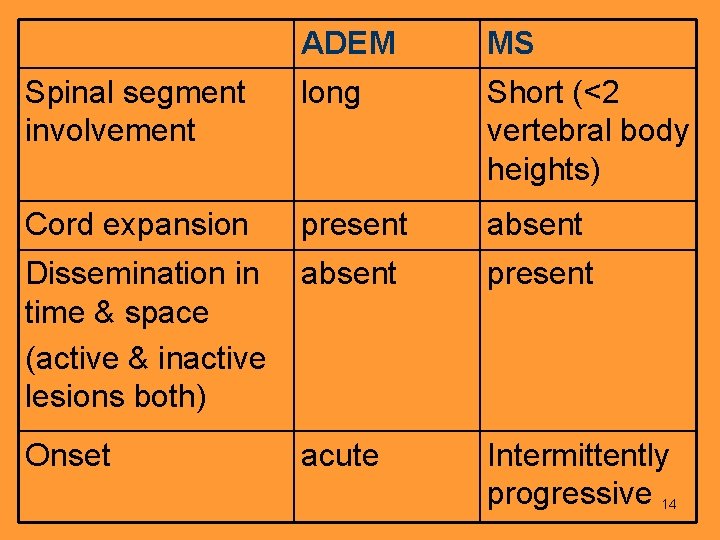
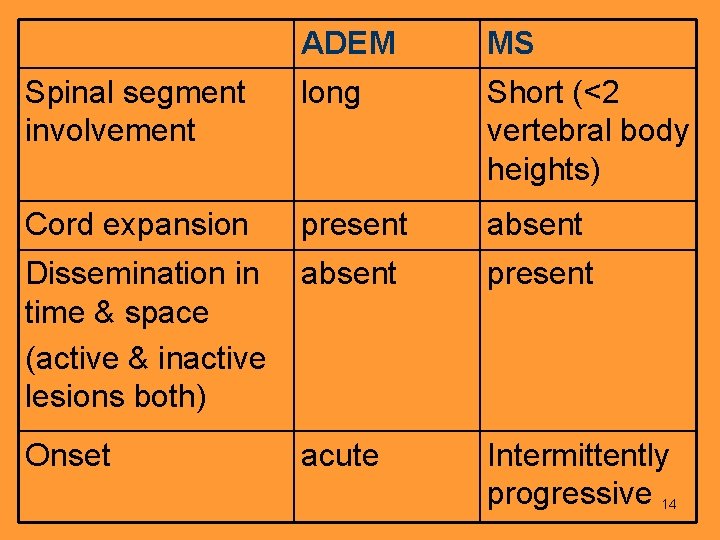
ADEM MS Spinal segment involvement long Short (<2 vertebral body heights) Cord expansion present absent Dissemination in absent time & space (active & inactive lesions both) present Onset Intermittently progressive 14 acute
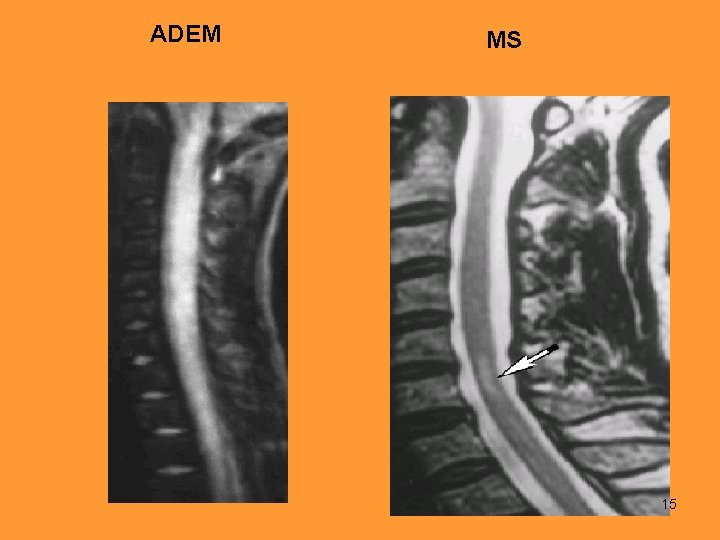
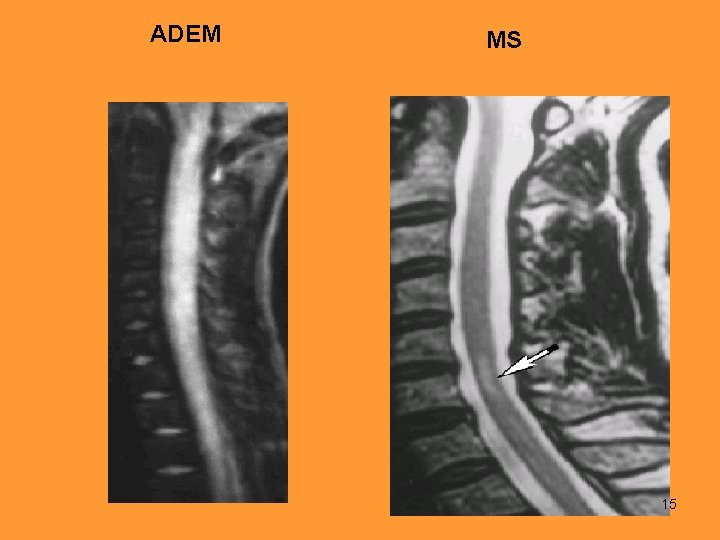
ADEM MS 15
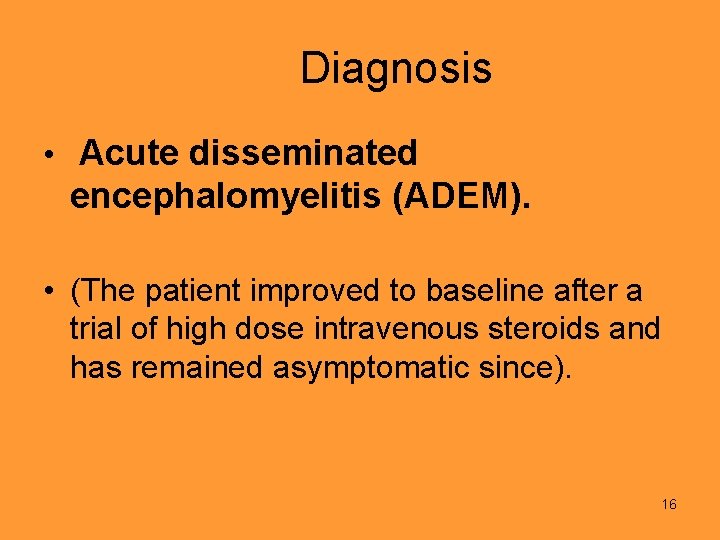
Diagnosis • Acute disseminated encephalomyelitis (ADEM). • (The patient improved to baseline after a trial of high dose intravenous steroids and has remained asymptomatic since). 16
Acute Disseminated Encephalomyelitis • ADEM is an autoimmune demyelinating disease generally associated with preceding viral infection or vaccination or occur spontaneously. • Affects all ages mainly children & young adults. • Typically abrupt onset. Neurologic symptoms begin 1 to 3 weeks after infection. 17
• Fever, Headache, and altered mental status with confusion progressing to lethargy and coma are common accompaniments. • The clinical course is rapid. • Evidence of upper motor neuron dysfunction is the rule. • Sensory findings are almost always present. • Cranial nerve involvement is common, particularly optic neuritis. 18
• Often there is evidence of transverse myelitis. Cerebellar dysfunction is common and initially may be the only finding. • Typically shows a CSF pleocytosis with up to 150 -200 WBCs, generally with a lymphocytic predominance. The protein level is usually elevated. • MRI images show multiple white matter hyperintense lesions on T 2 & flair sequences with gadolinium enhancement on T 1. • Commonly subcortical location & bilateral but asymmetric distribution. 19
CASE 2 20
21
22
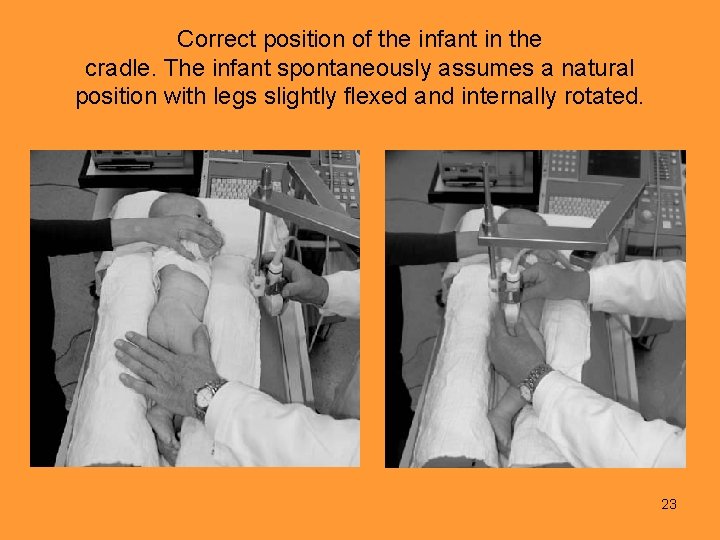
Correct position of the infant in the cradle. The infant spontaneously assumes a natural position with legs slightly flexed and internally rotated. 23

24
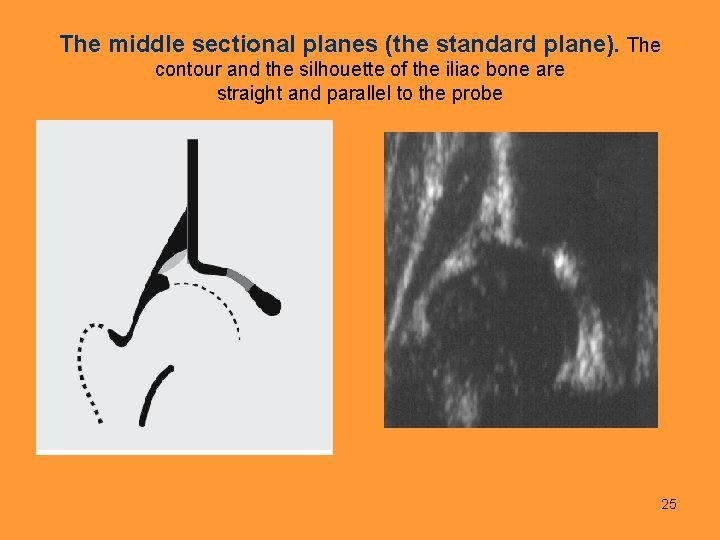
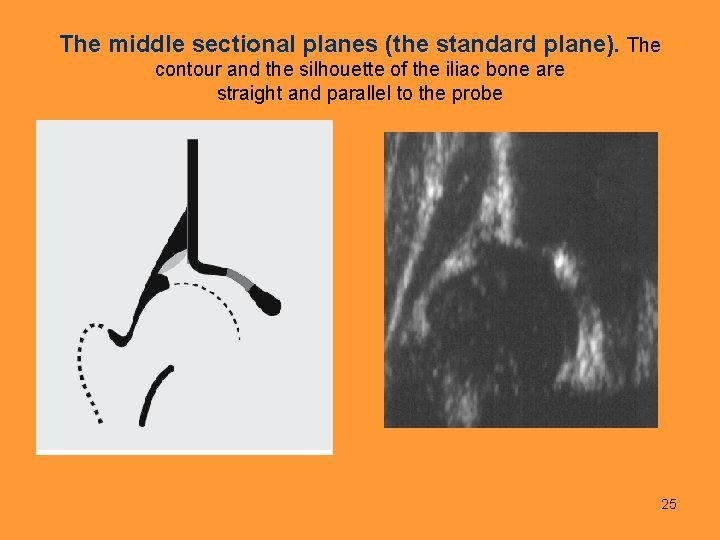
The middle sectional planes (the standard plane). The contour and the silhouette of the iliac bone are straight and parallel to the probe 25
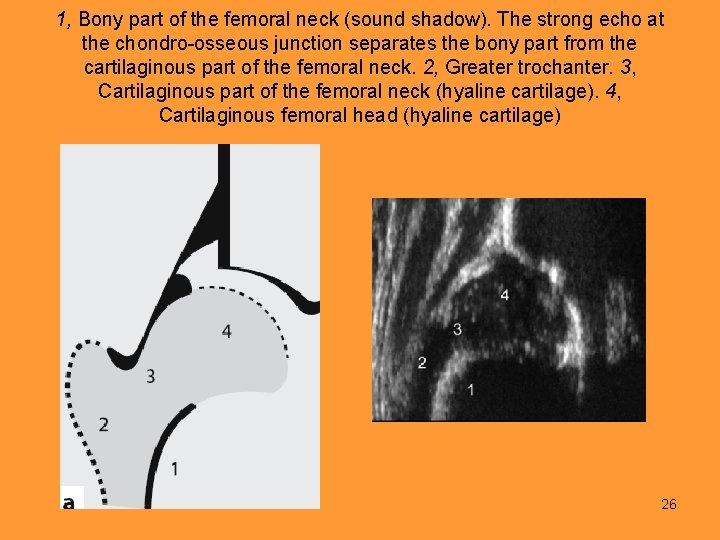
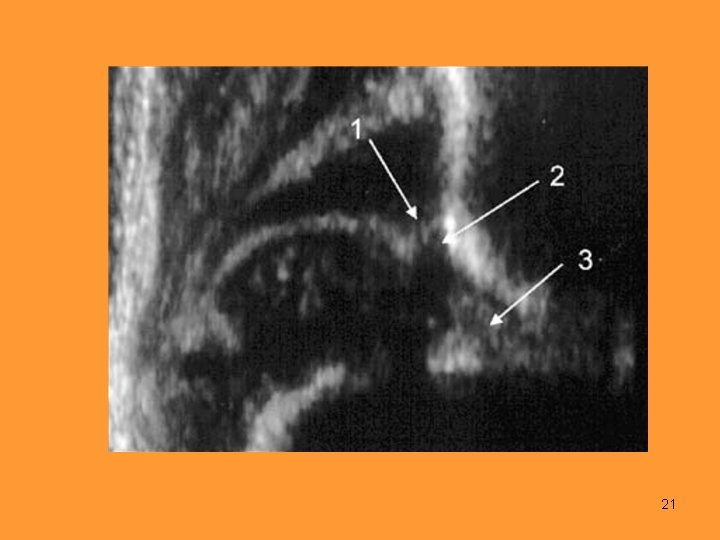
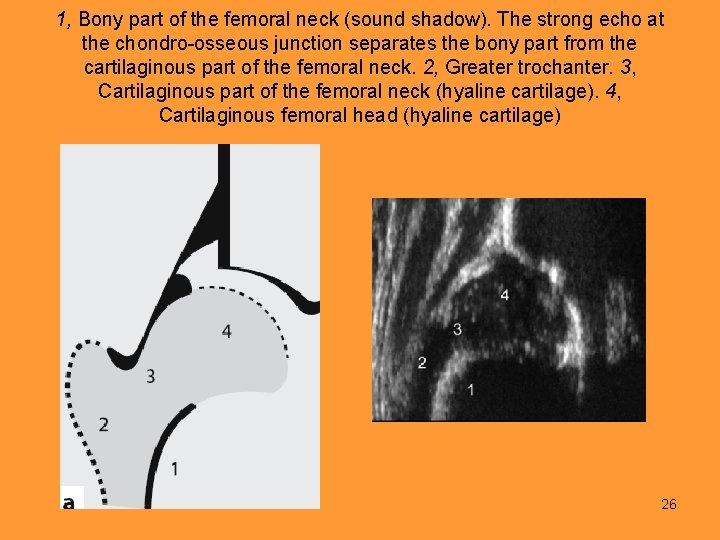
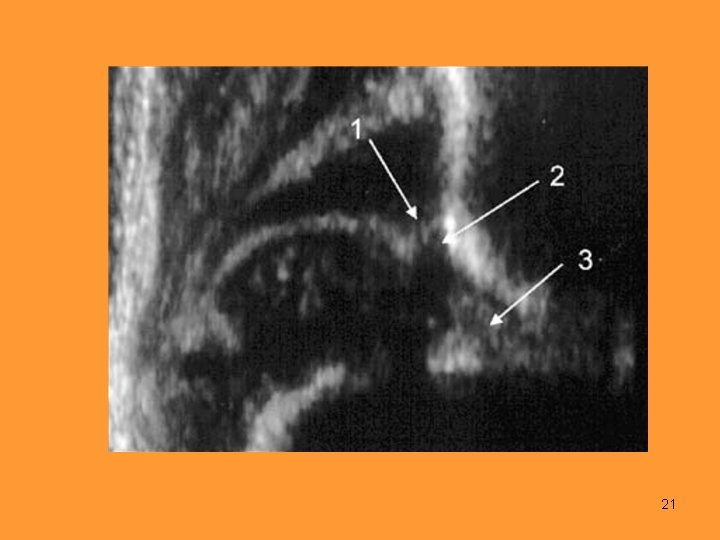
1, Bony part of the femoral neck (sound shadow). The strong echo at the chondro-osseous junction separates the bony part from the cartilaginous part of the femoral neck. 2, Greater trochanter. 3, Cartilaginous part of the femoral neck (hyaline cartilage). 4, Cartilaginous femoral head (hyaline cartilage) 26
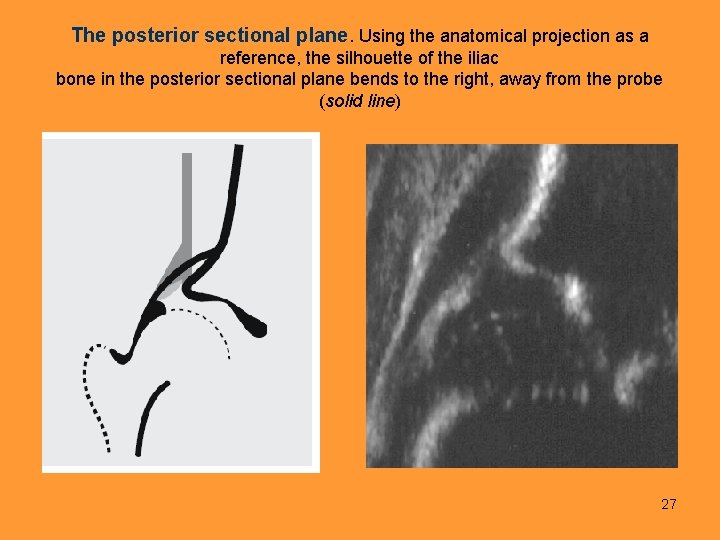
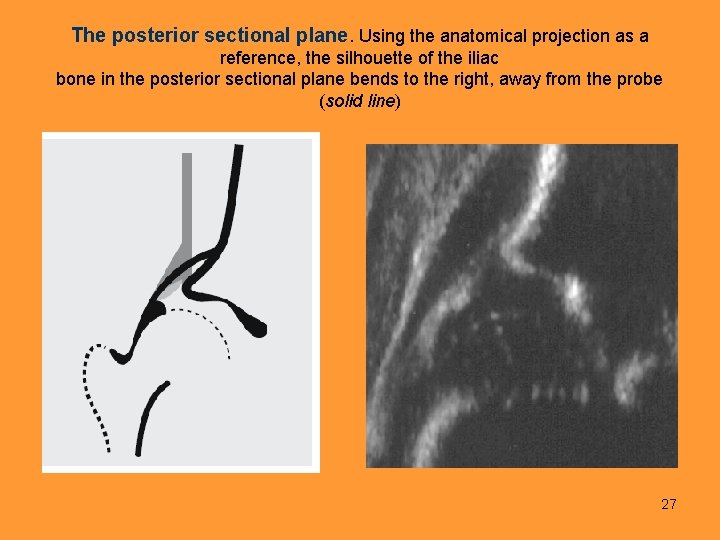
The posterior sectional plane. Using the anatomical projection as a reference, the silhouette of the iliac bone in the posterior sectional plane bends to the right, away from the probe (solid line) 27
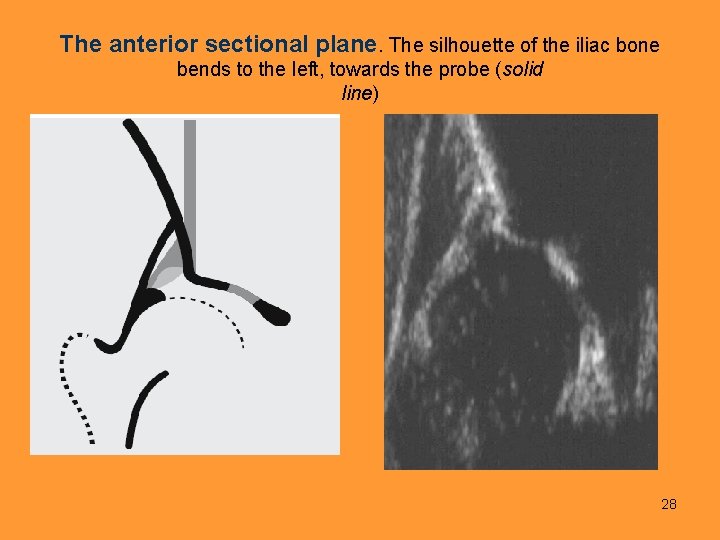
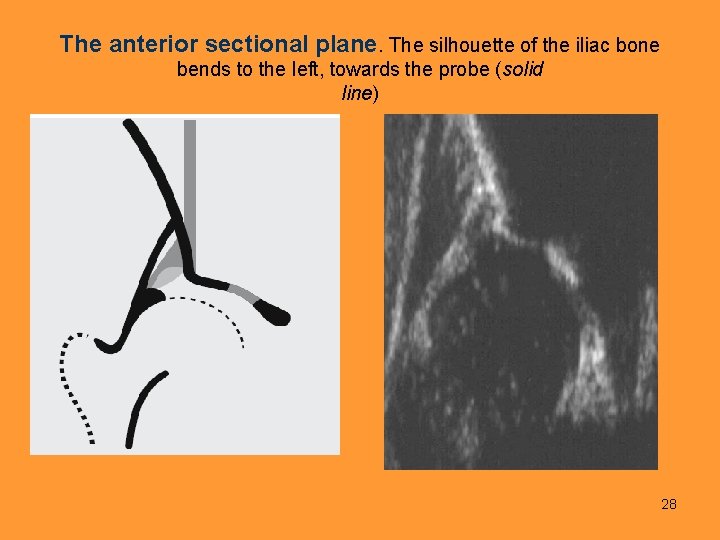
The anterior sectional plane. The silhouette of the iliac bone bends to the left, towards the probe (solid line) 28
ANGLES 29
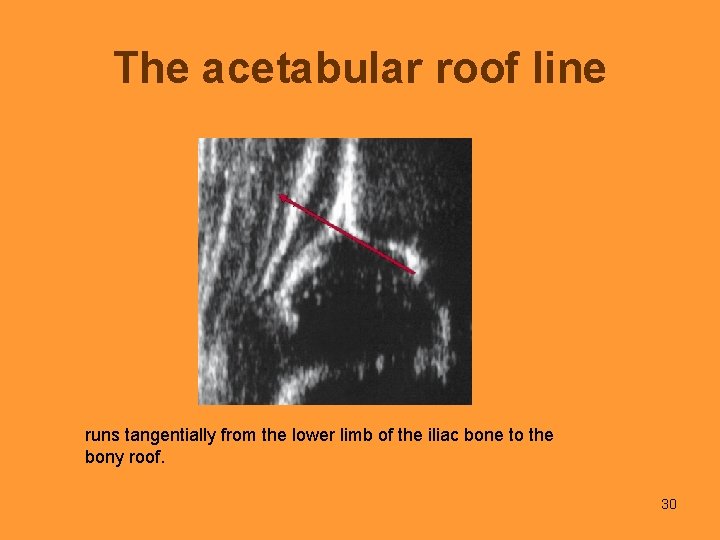
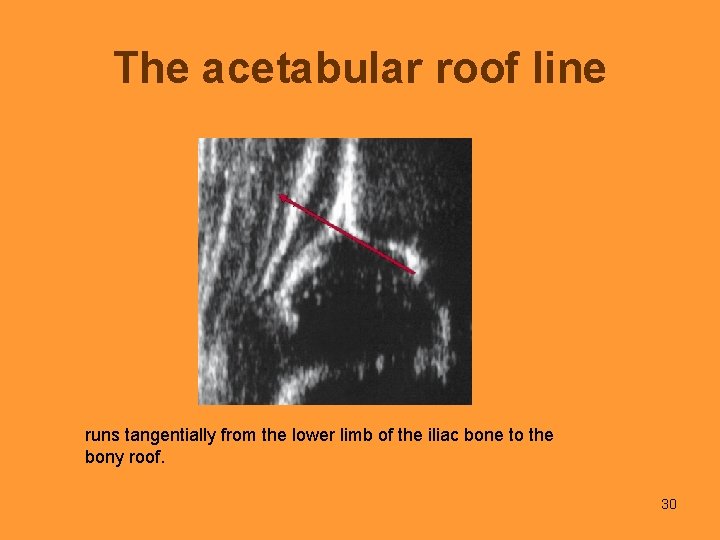
The acetabular roof line runs tangentially from the lower limb of the iliac bone to the bony roof. 30
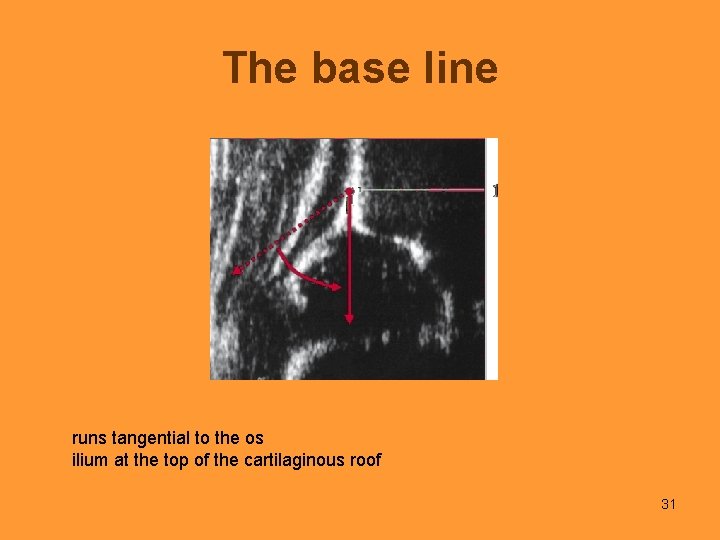
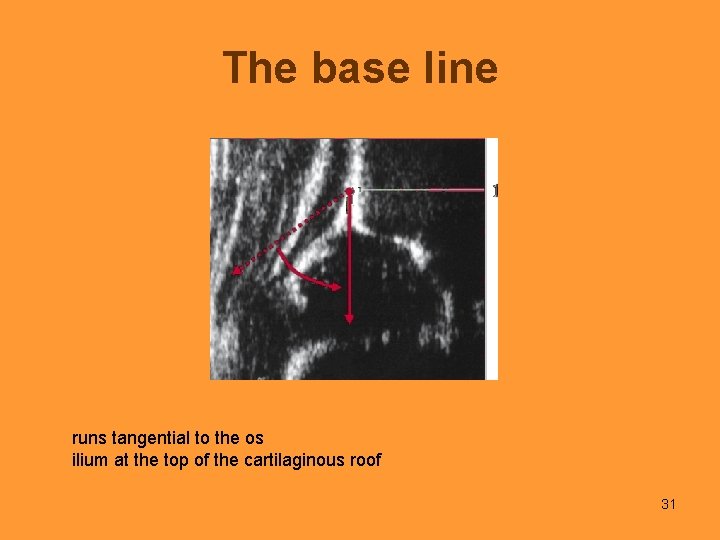
The base line runs tangential to the os ilium at the top of the cartilaginous roof 31
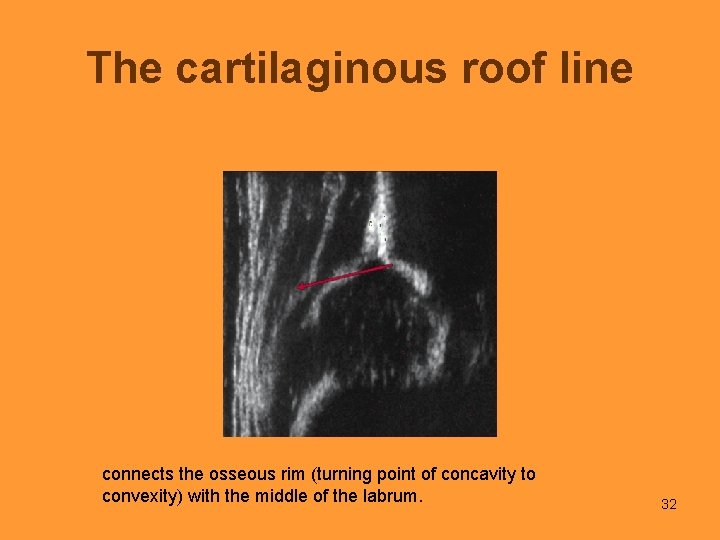
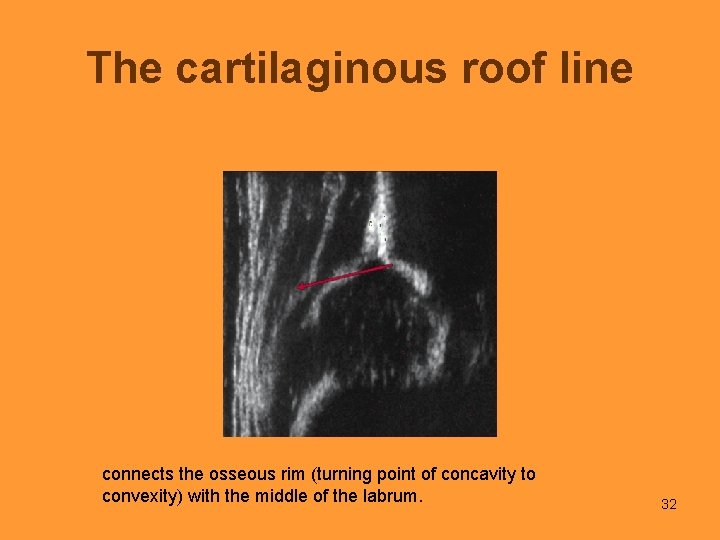
The cartilaginous roof line connects the osseous rim (turning point of concavity to convexity) with the middle of the labrum. 32

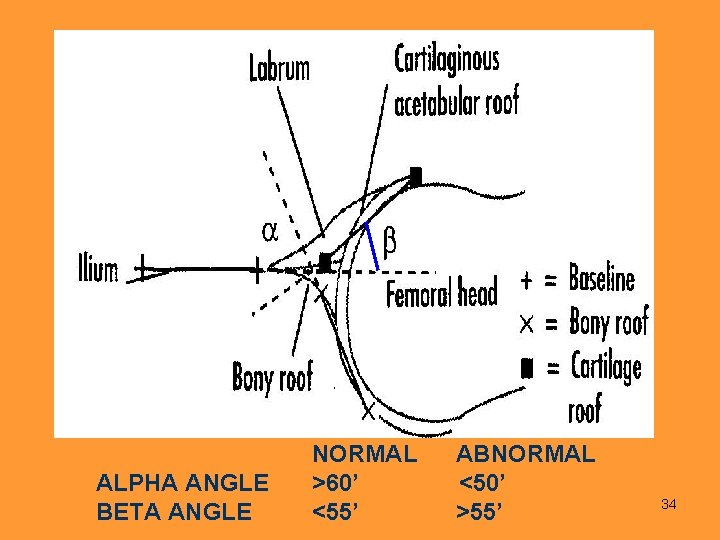
BETA ANGLE ALPHA ANGLE 33
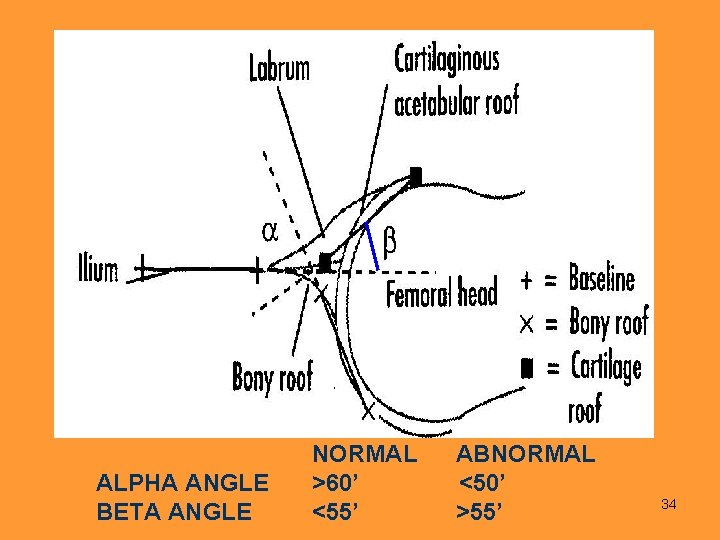
ALPHA ANGLE BETA ANGLE NORMAL ABNORMAL >60’ <50’ <55’ >55’ 34
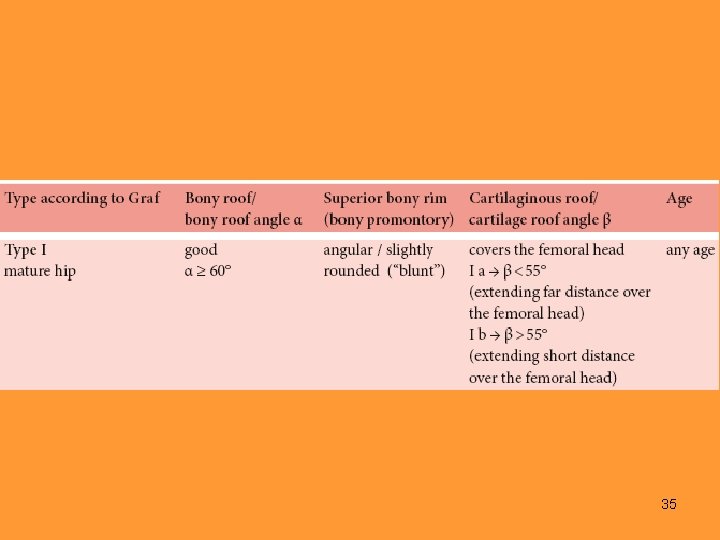
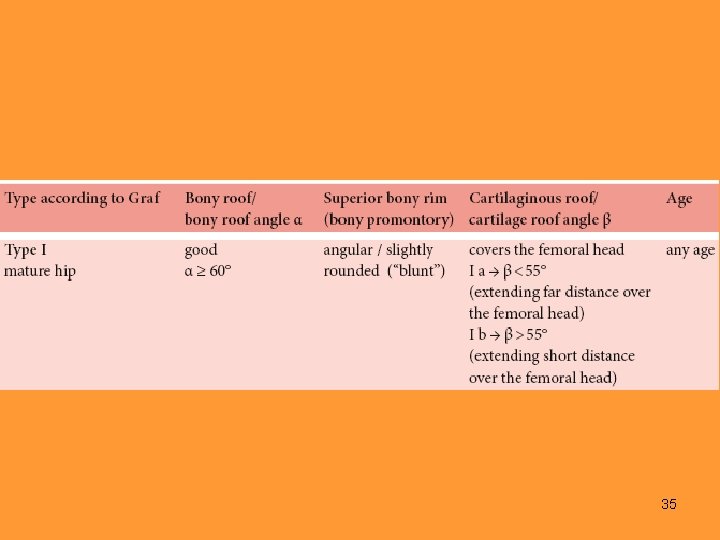
35
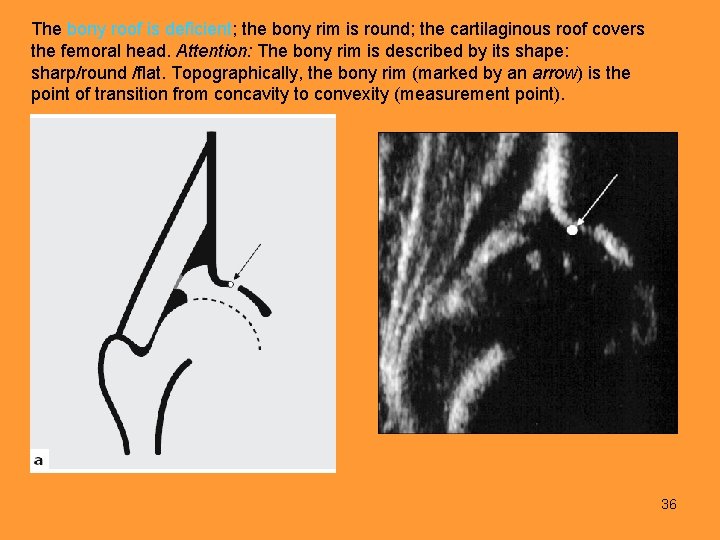
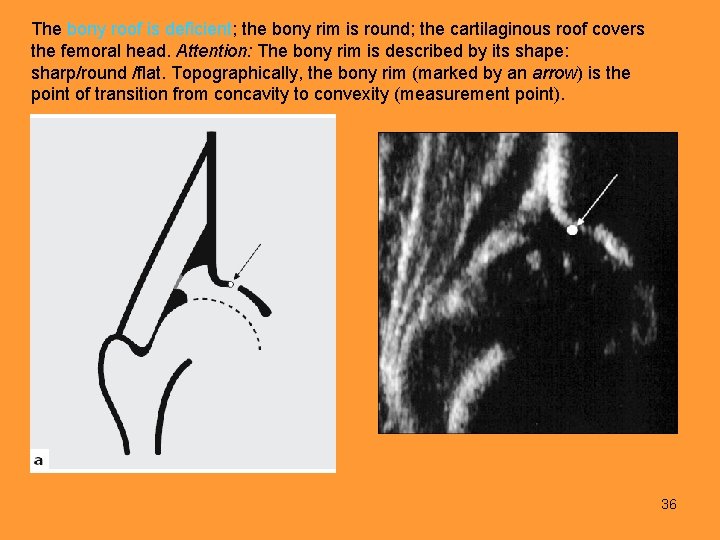
The bony roof is deficient; the bony rim is round; the cartilaginous roof covers the femoral head. Attention: The bony rim is described by its shape: sharp/round /flat. Topographically, the bony rim (marked by an arrow) is the point of transition from concavity to convexity (measurement point). 36
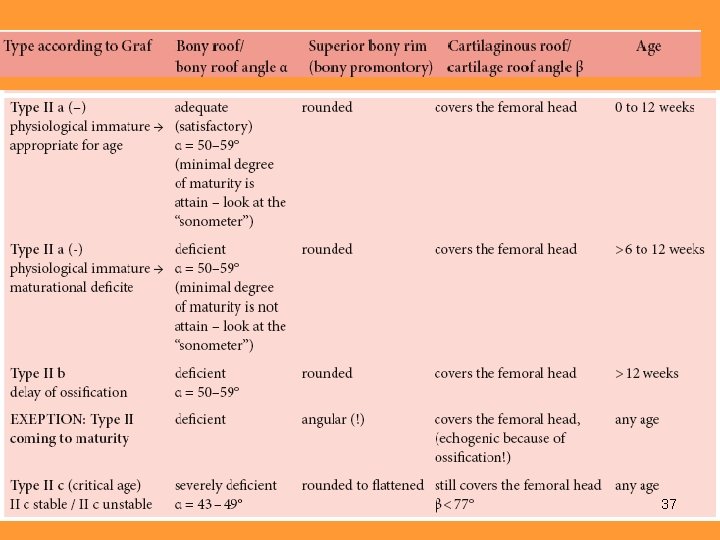
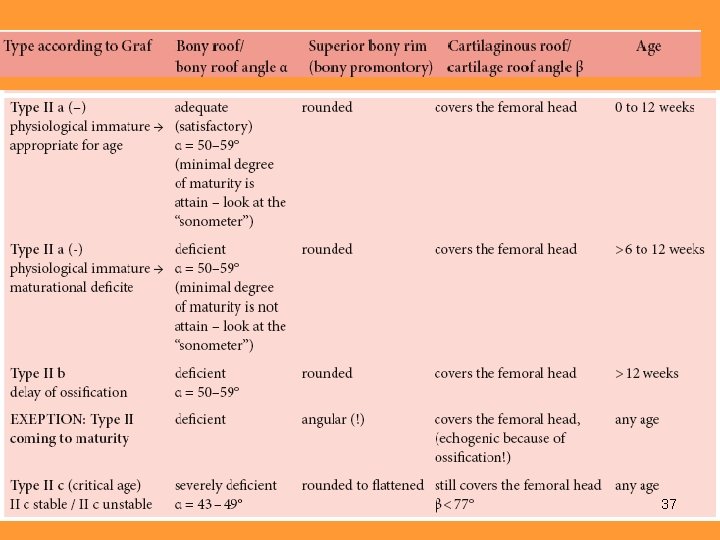
37
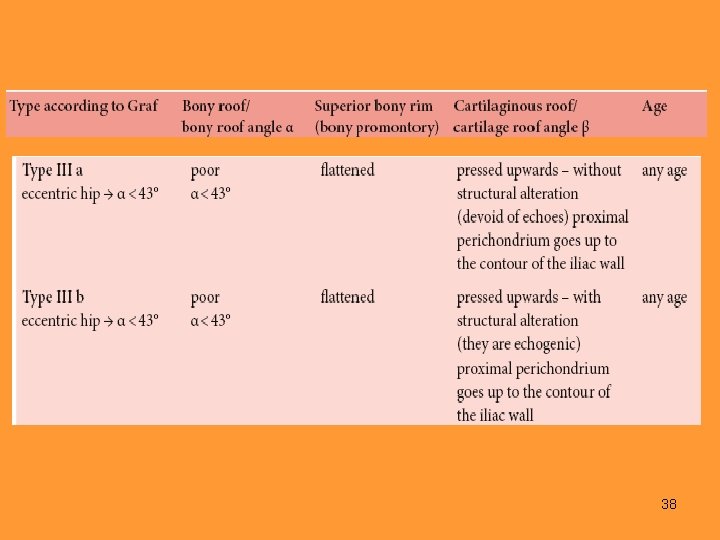
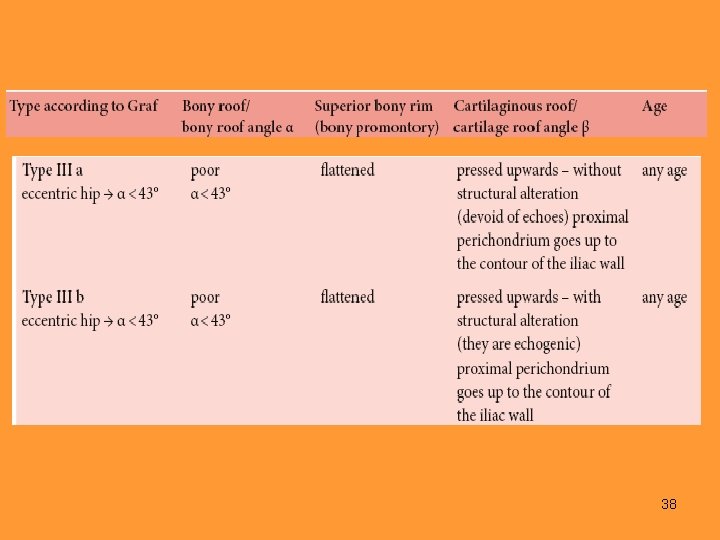
38
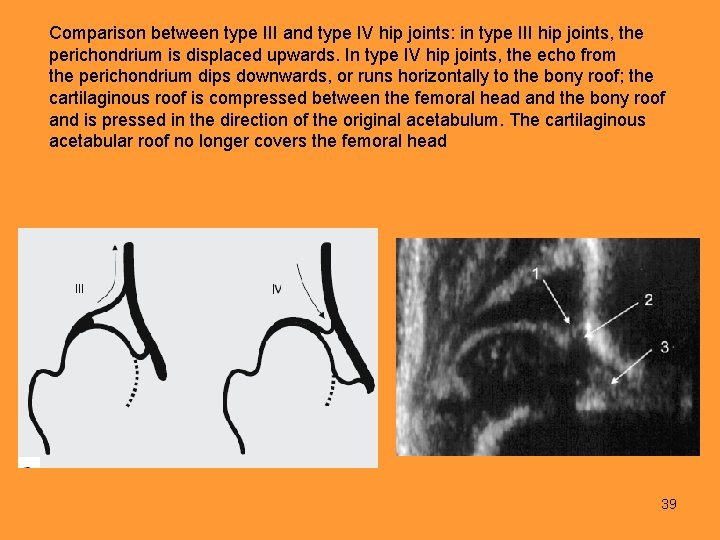
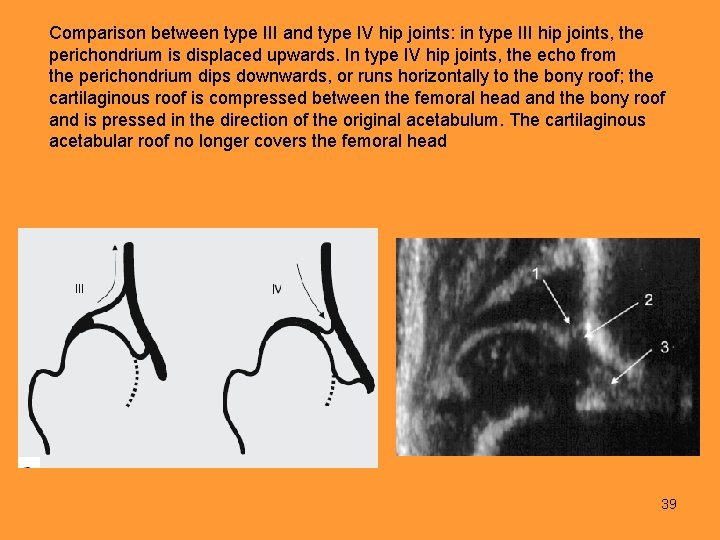
Comparison between type III and type IV hip joints: in type III hip joints, the perichondrium is displaced upwards. In type IV hip joints, the echo from the perichondrium dips downwards, or runs horizontally to the bony roof; the cartilaginous roof is compressed between the femoral head and the bony roof and is pressed in the direction of the original acetabulum. The cartilaginous acetabular roof no longer covers the femoral head 39
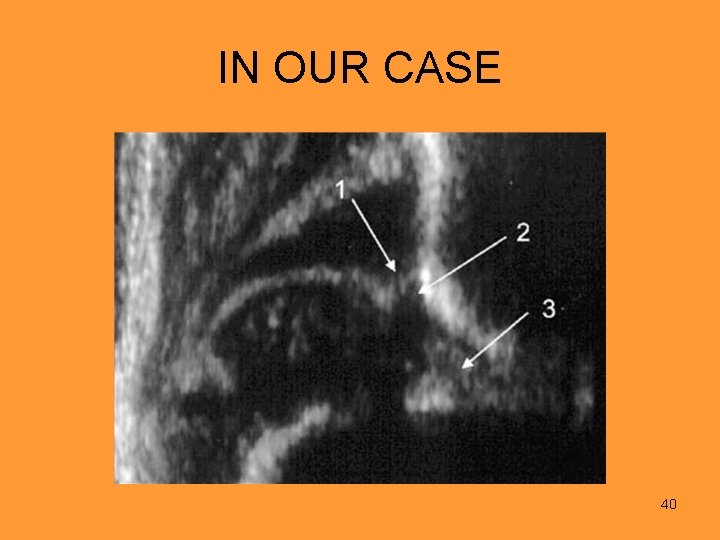
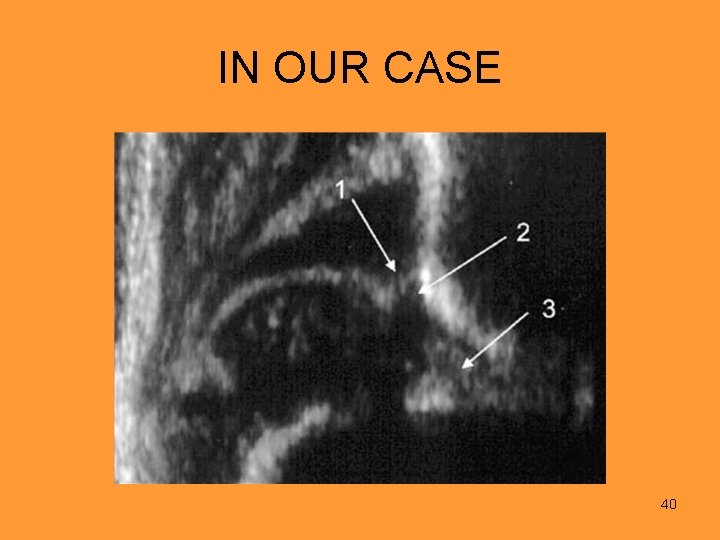
IN OUR CASE 40
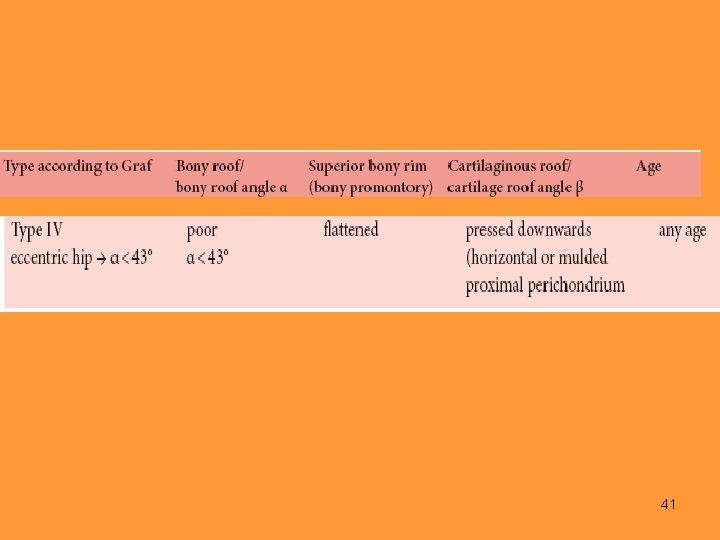
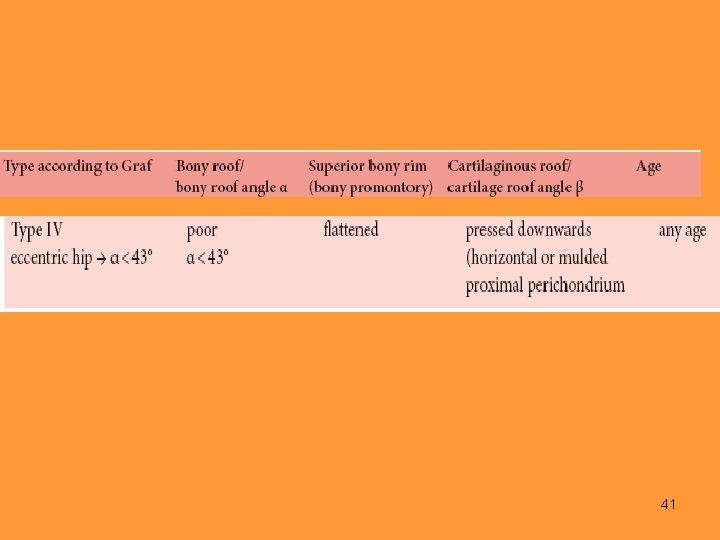
41
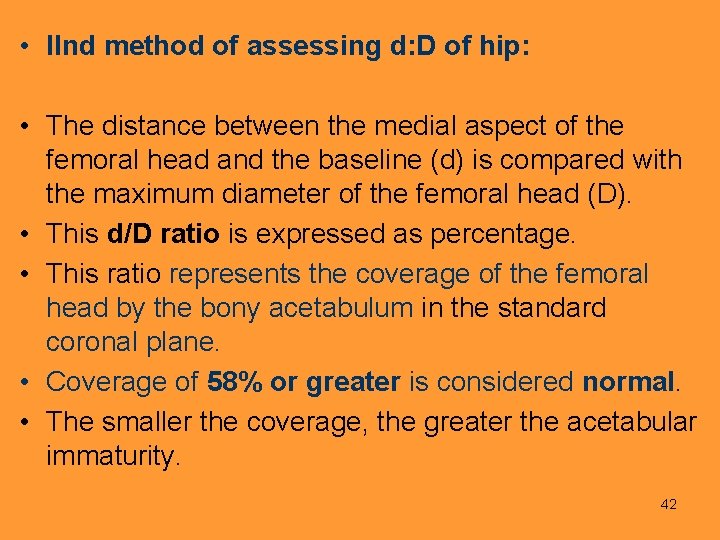
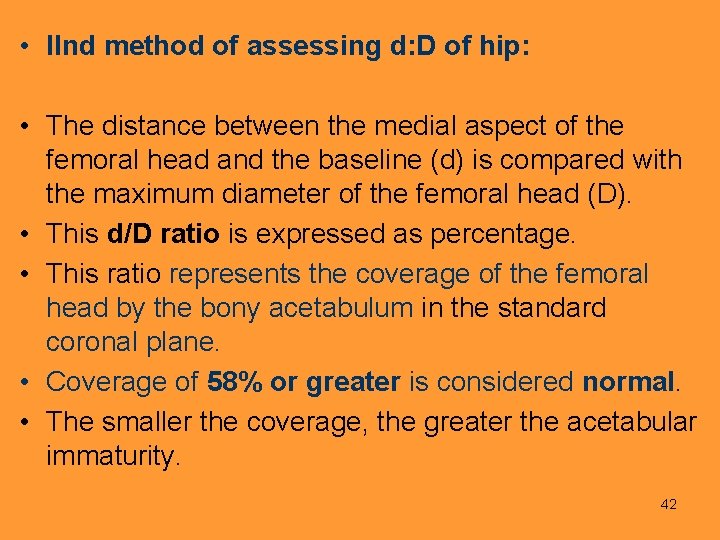
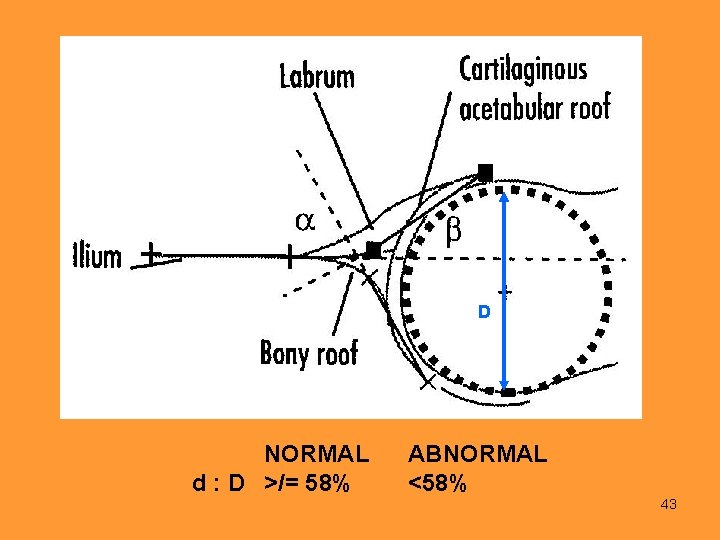
• IInd method of assessing d: D of hip: • The distance between the medial aspect of the femoral head and the baseline (d) is compared with the maximum diameter of the femoral head (D). • This d/D ratio is expressed as percentage. • This ratio represents the coverage of the femoral head by the bony acetabulum in the standard coronal plane. • Coverage of 58% or greater is considered normal. • The smaller the coverage, the greater the acetabular immaturity. 42
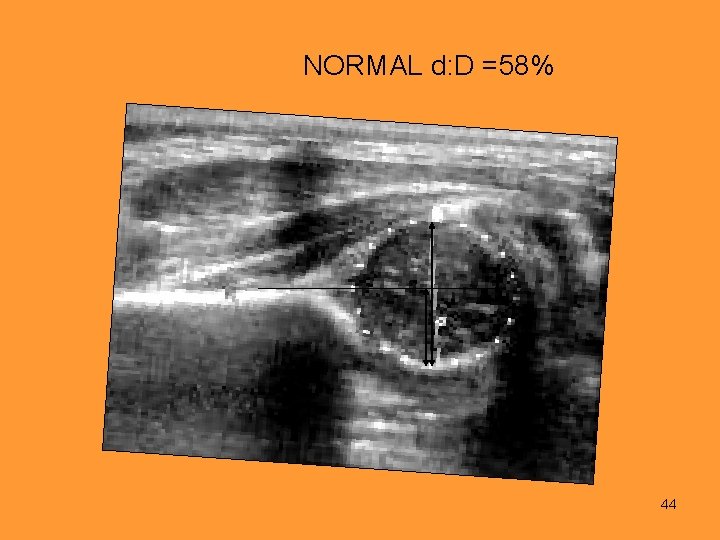
D NORMAL d : D >/= 58% d ABNORMAL <58% 43
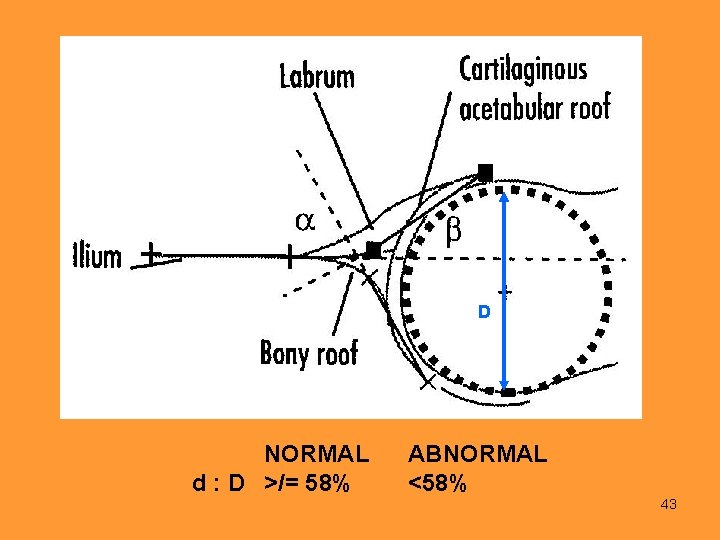
NORMAL d: D =58% 44
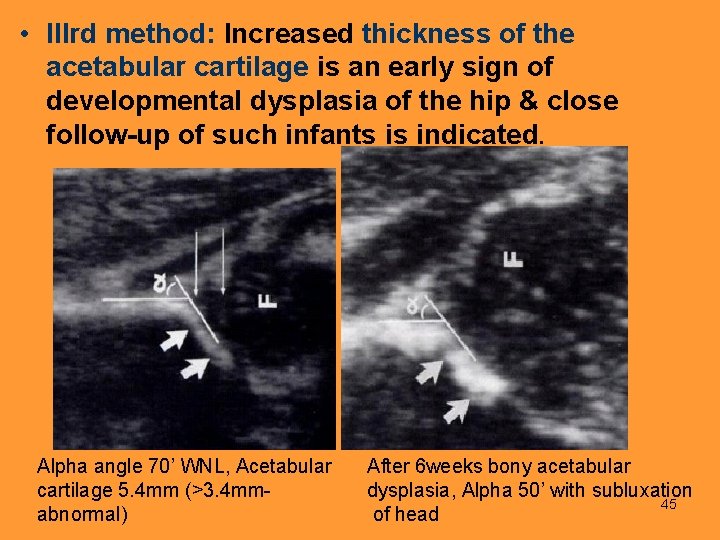
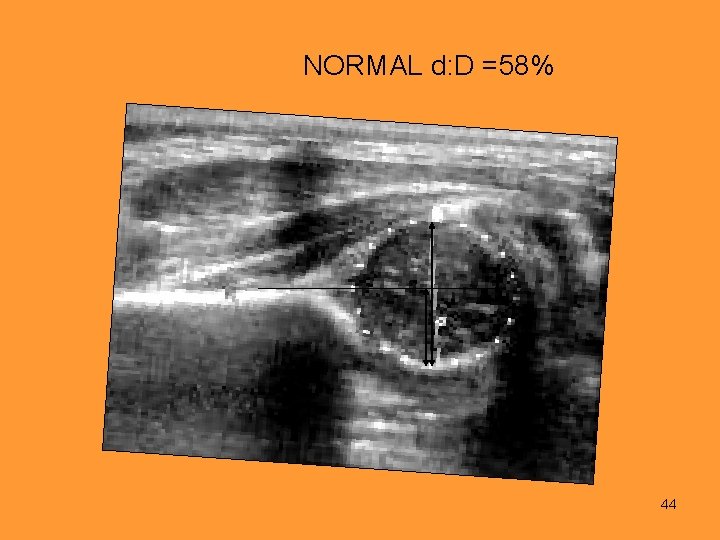
• IIIrd method: Increased thickness of the acetabular cartilage is an early sign of developmental dysplasia of the hip & close follow-up of such infants is indicated. Alpha angle 70’ WNL, Acetabular cartilage 5. 4 mm (>3. 4 mm- abnormal) After 6 weeks bony acetabular dysplasia, Alpha 50’ with subluxation 45 of head
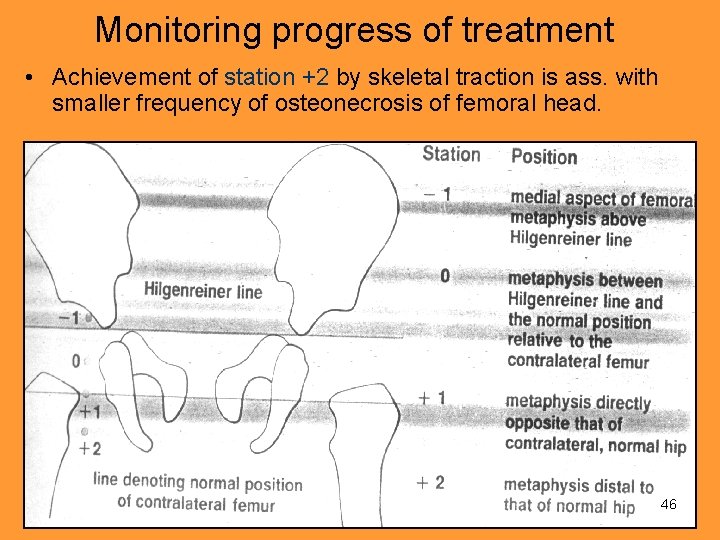
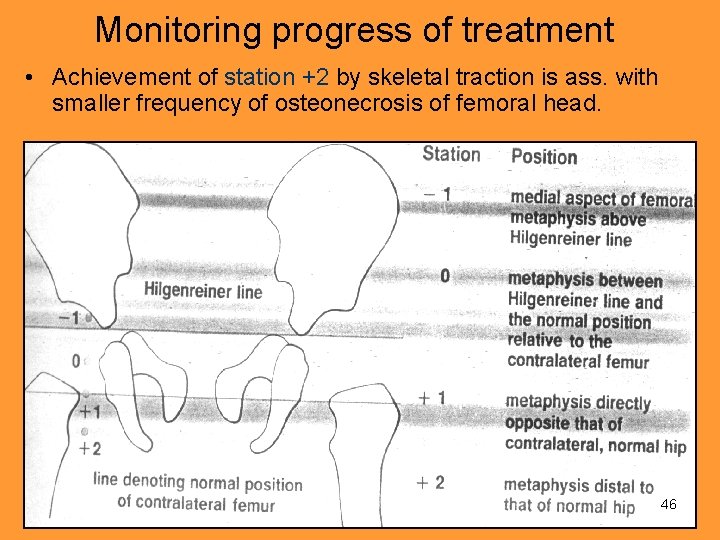
Monitoring progress of treatment • Achievement of station +2 by skeletal traction is ass. with smaller frequency of osteonecrosis of femoral head. 46
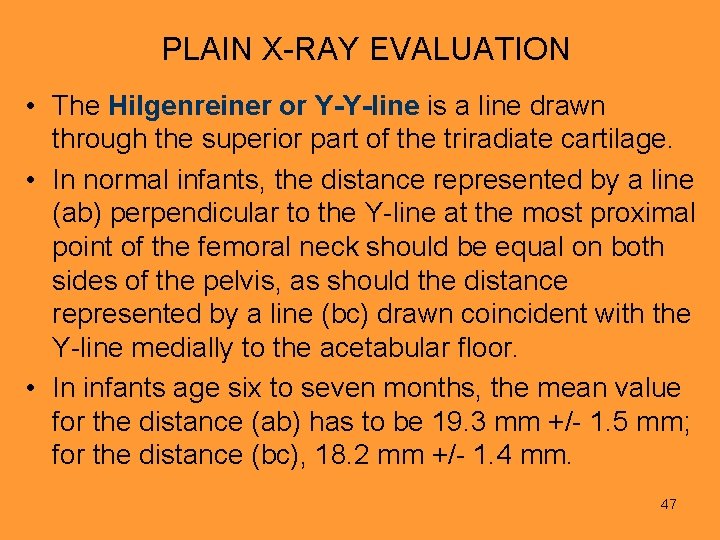
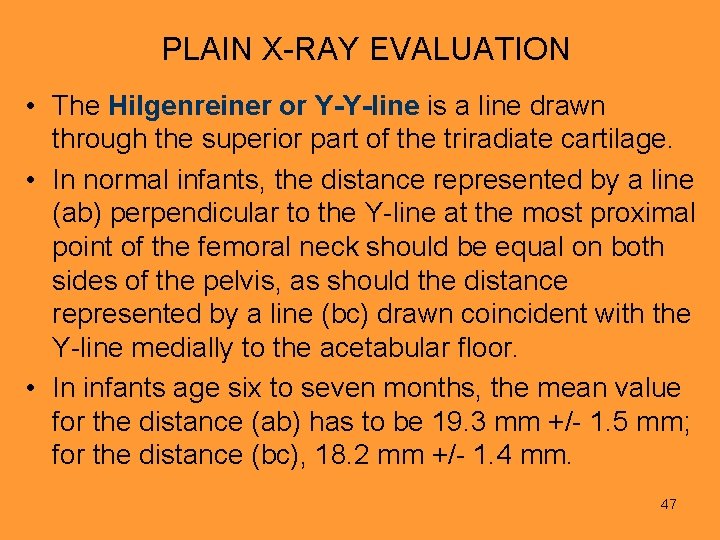
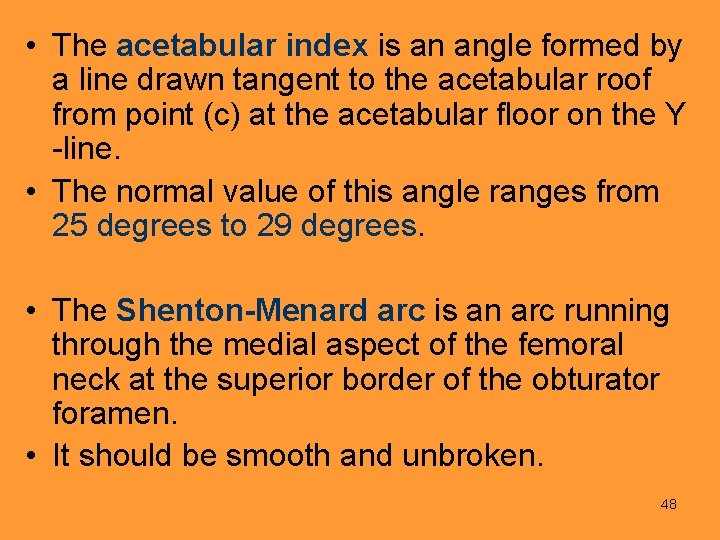
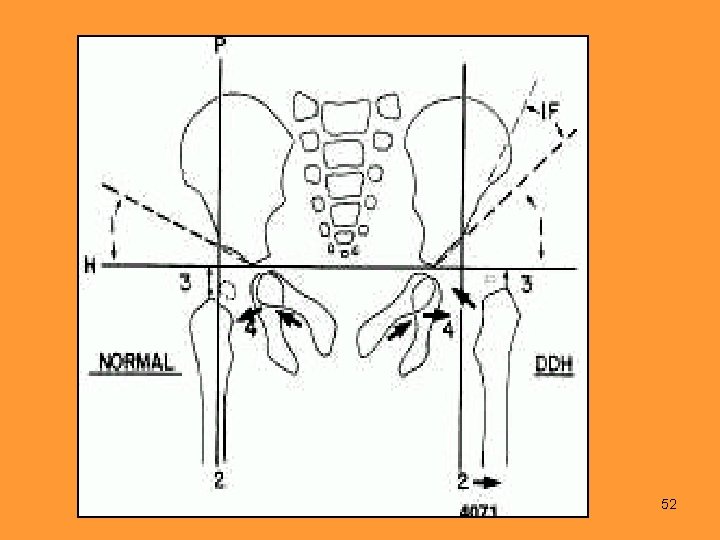
PLAIN X-RAY EVALUATION • The Hilgenreiner or Y-Y-line is a line drawn through the superior part of the triradiate cartilage. • In normal infants, the distance represented by a line (ab) perpendicular to the Y-line at the most proximal point of the femoral neck should be equal on both sides of the pelvis, as should the distance represented by a line (bc) drawn coincident with the Y-line medially to the acetabular floor. • In infants age six to seven months, the mean value for the distance (ab) has to be 19. 3 mm +/- 1. 5 mm; for the distance (bc), 18. 2 mm +/- 1. 4 mm. 47
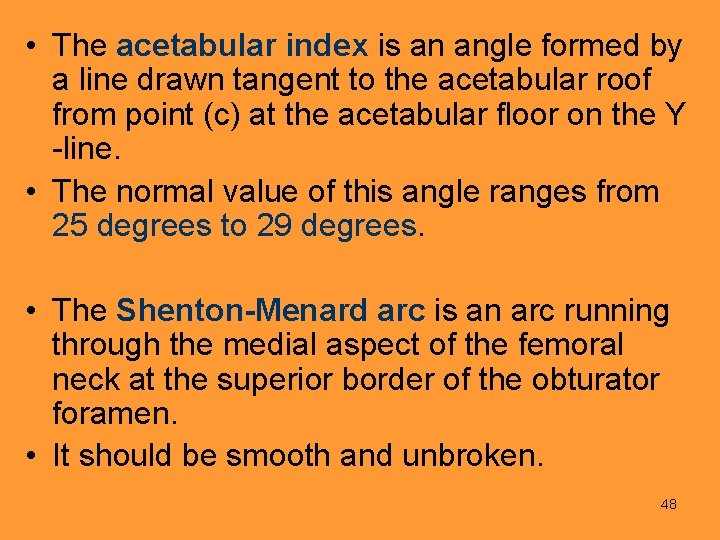
• The acetabular index is an angle formed by a line drawn tangent to the acetabular roof from point (c) at the acetabular floor on the Y -line. • The normal value of this angle ranges from 25 degrees to 29 degrees. • The Shenton-Menard arc is an arc running through the medial aspect of the femoral neck at the superior border of the obturator foramen. • It should be smooth and unbroken. 48
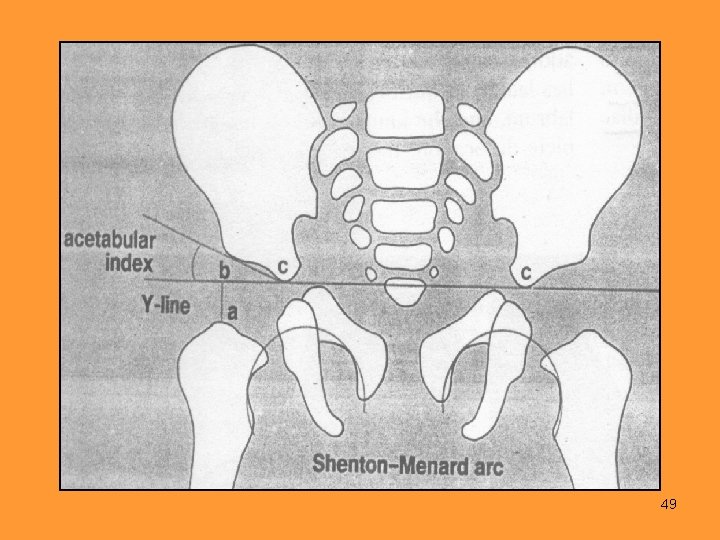
49
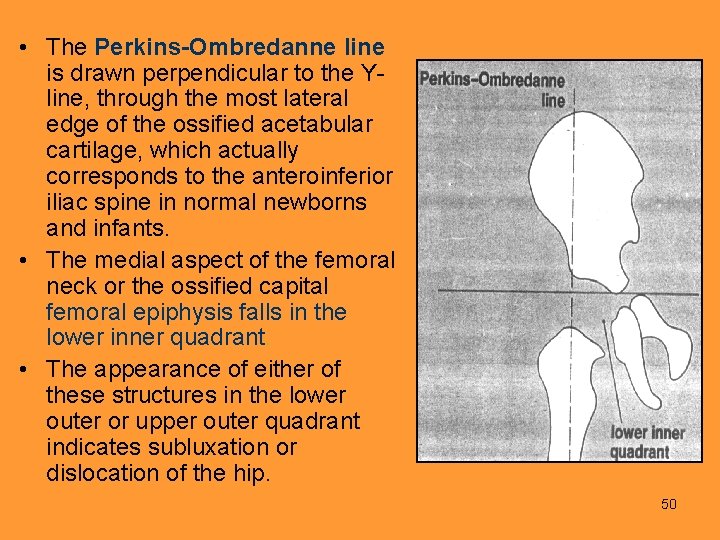
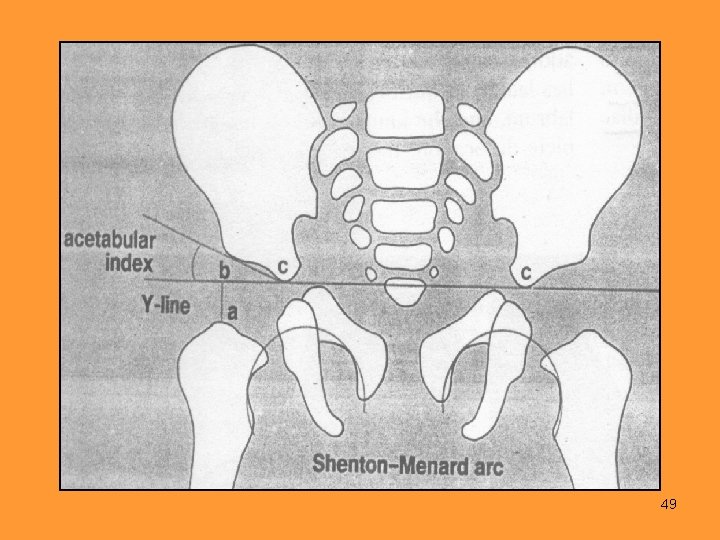
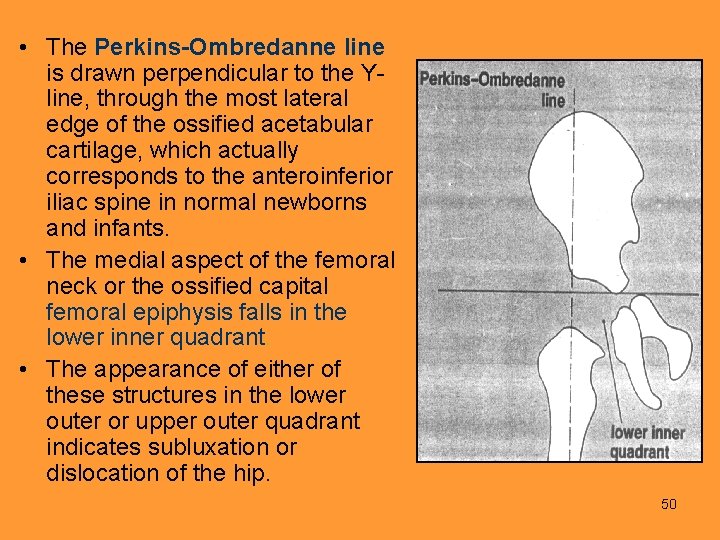
• The Perkins-Ombredanne line is drawn perpendicular to the Yline, through the most lateral edge of the ossified acetabular cartilage, which actually corresponds to the anteroinferior iliac spine in normal newborns and infants. • The medial aspect of the femoral neck or the ossified capital femoral epiphysis falls in the lower inner quadrant. • The appearance of either of these structures in the lower outer or upper outer quadrant indicates subluxation or dislocation of the hip. 50

51
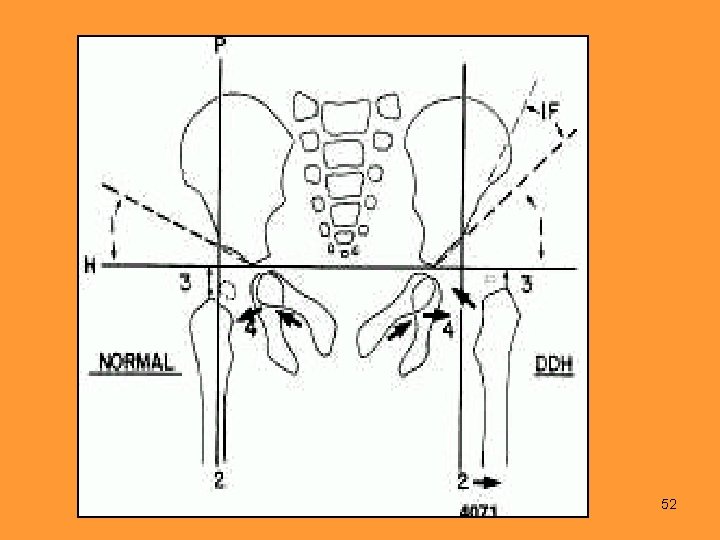
52
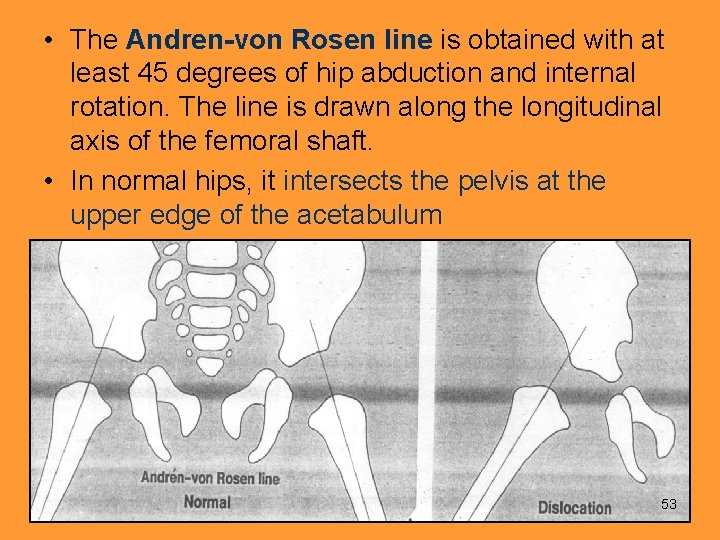
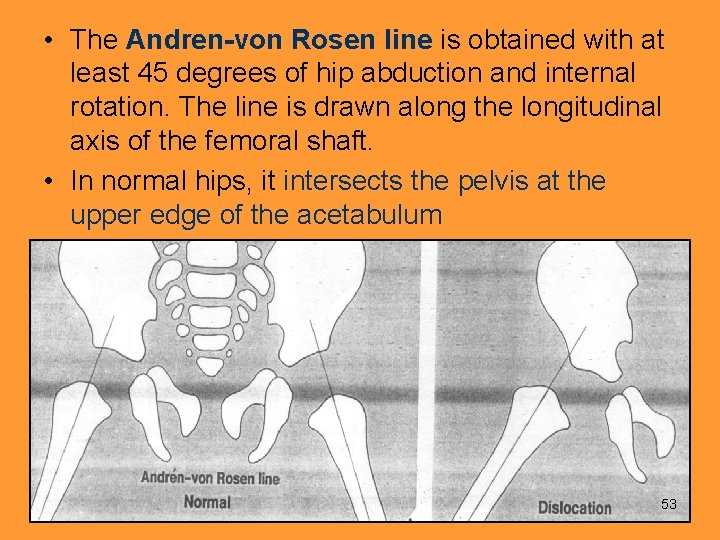
• The Andren-von Rosen line is obtained with at least 45 degrees of hip abduction and internal rotation. The line is drawn along the longitudinal axis of the femoral shaft. • In normal hips, it intersects the pelvis at the upper edge of the acetabulum. 53
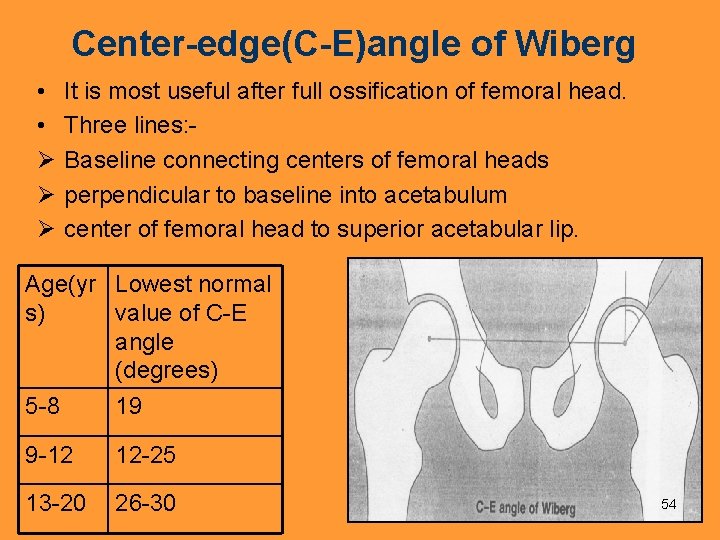
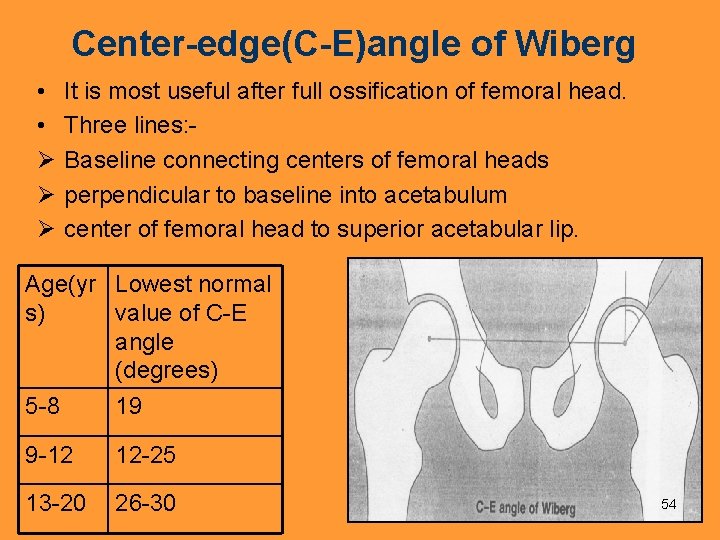
Center-edge(C-E)angle of Wiberg • • Ø Ø Ø It is most useful after full ossification of femoral head. Three lines: Baseline connecting centers of femoral heads perpendicular to baseline into acetabulum center of femoral head to superior acetabular lip. Age(yr Lowest normal s) value of C-E angle (degrees) 5 -8 19 9 -12 12 -25 13 -20 26 -30 54
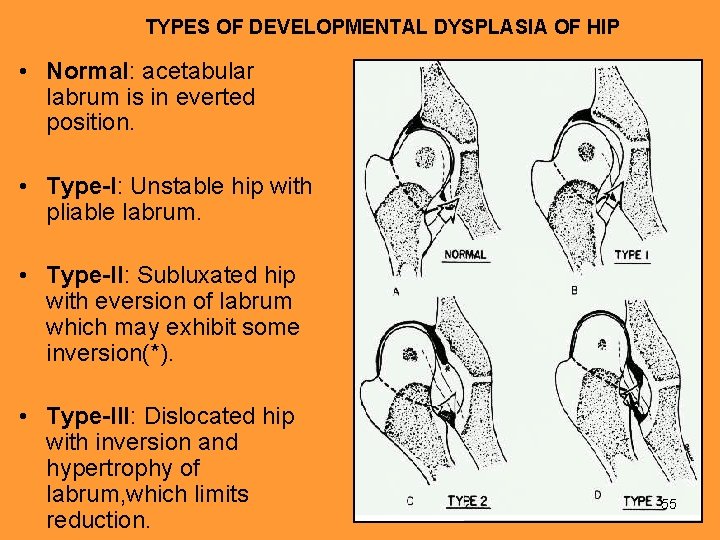
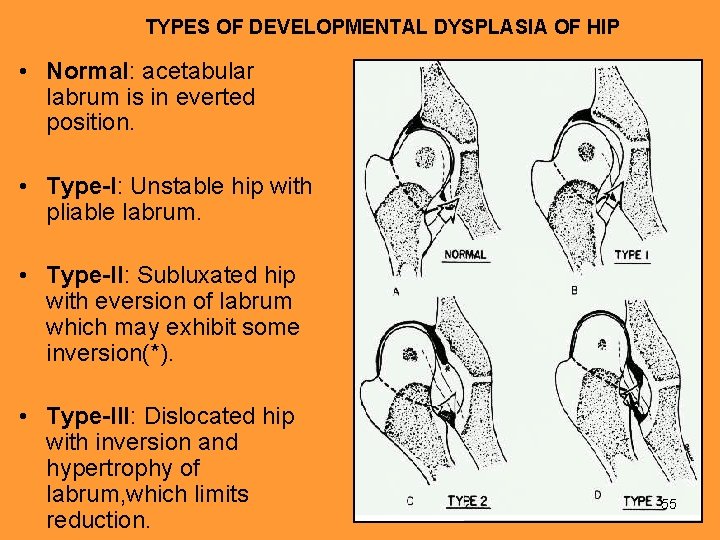
TYPES OF DEVELOPMENTAL DYSPLASIA OF HIP • Normal: acetabular labrum is in everted position. • Type-I: Unstable hip with pliable labrum. • Type-II: Subluxated hip with eversion of labrum which may exhibit some inversion(*). • Type-III: Dislocated hip with inversion and hypertrophy of labrum, which limits reduction. 55

SIGN 56
• Dripping Candle Wax Sign 57
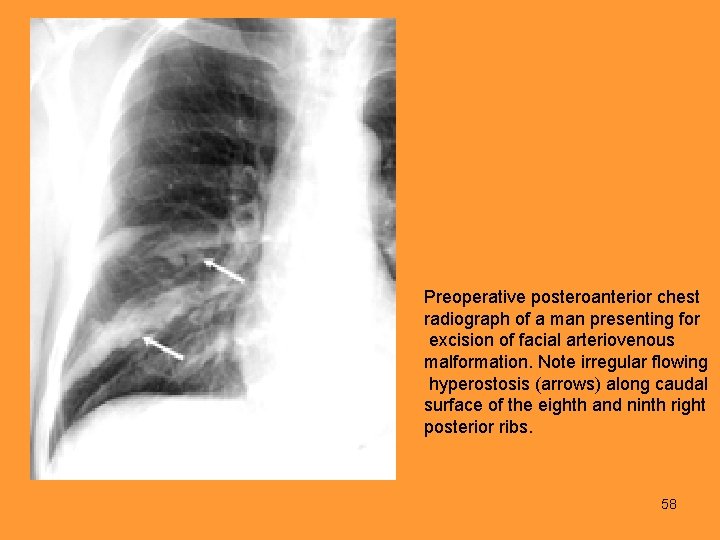
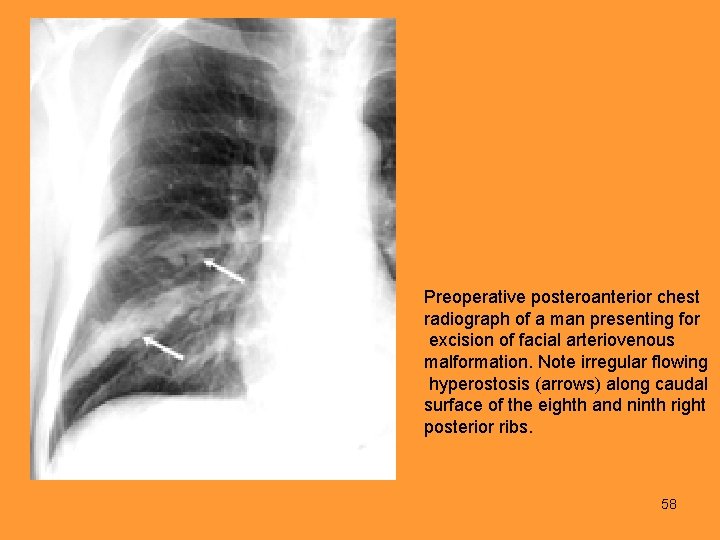
Preoperative posteroanterior chest radiograph of a man presenting for excision of facial arteriovenous malformation. Note irregular flowing hyperostosis (arrows) along caudal surface of the eighth and ninth right posterior ribs. 58
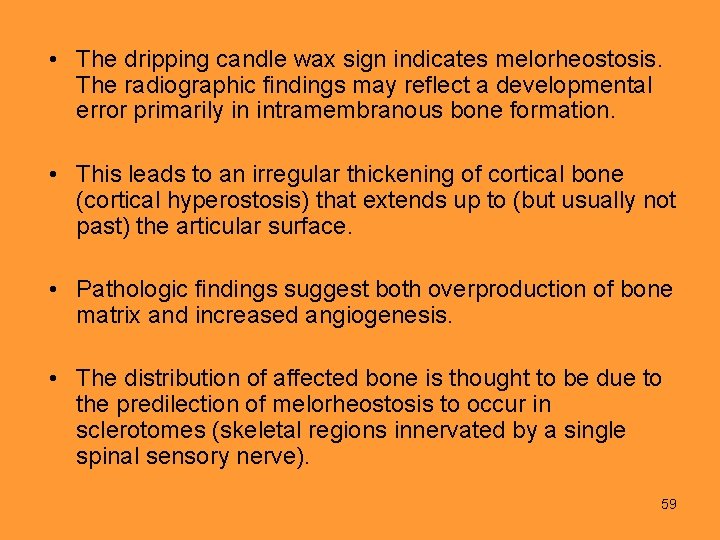
• The dripping candle wax sign indicates melorheostosis. The radiographic findings may reflect a developmental error primarily in intramembranous bone formation. • This leads to an irregular thickening of cortical bone (cortical hyperostosis) that extends up to (but usually not past) the articular surface. • Pathologic findings suggest both overproduction of bone matrix and increased angiogenesis. • The distribution of affected bone is thought to be due to the predilection of melorheostosis to occur in sclerotomes (skeletal regions innervated by a single spinal sensory nerve). 59
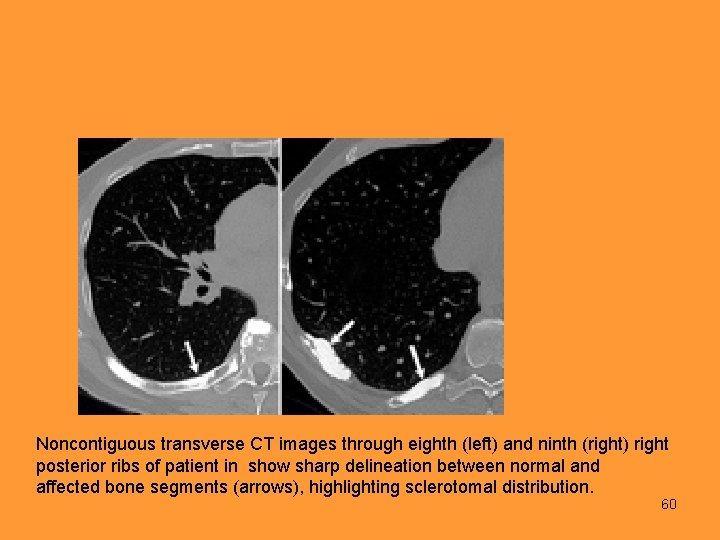
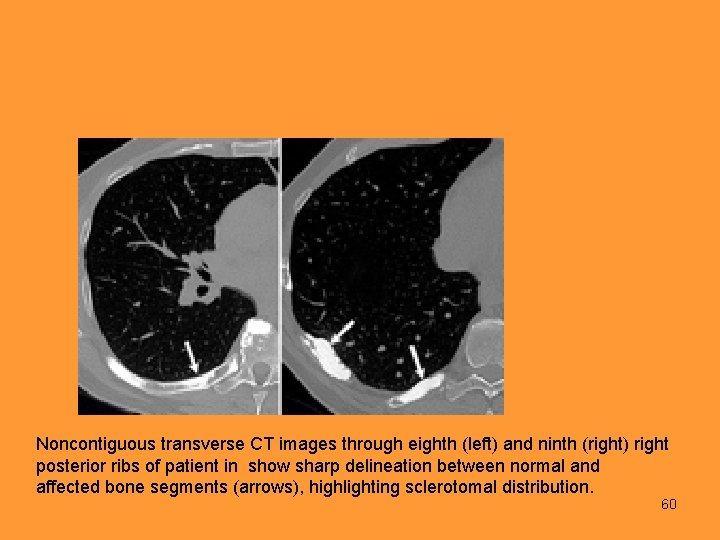
Noncontiguous transverse CT images through eighth (left) and ninth (right) right posterior ribs of patient in show sharp delineation between normal and affected bone segments (arrows), highlighting sclerotomal distribution. 60
K T A N H U Y O 61