CASE S London Syncope 2018 Dr Nick Gall

- Slides: 32
CASE S London Syncope 2018 Dr. Nick Gall King’s College Hospital London, UK
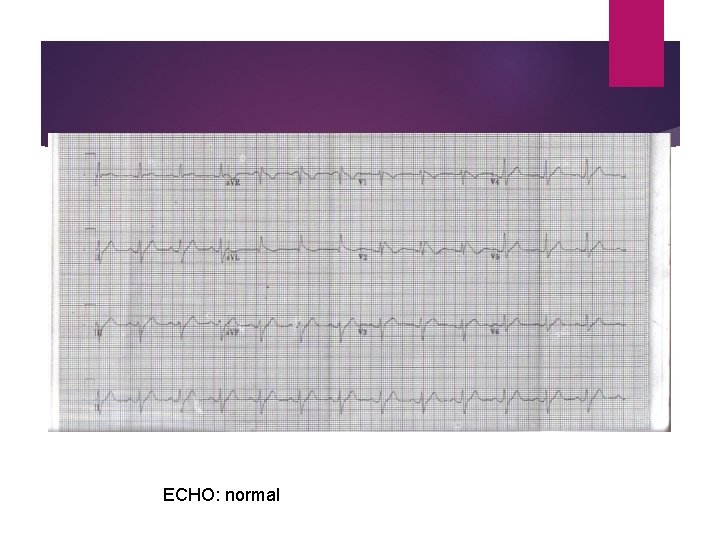
CASE 1 27 year old man 6 year history of T-LOC Initially thought to be epilepsy but no positive evidence after neurological review. Referred to cardiology PMH: Significant asthma with recurrent chest infections FH: Nil DH: Nil
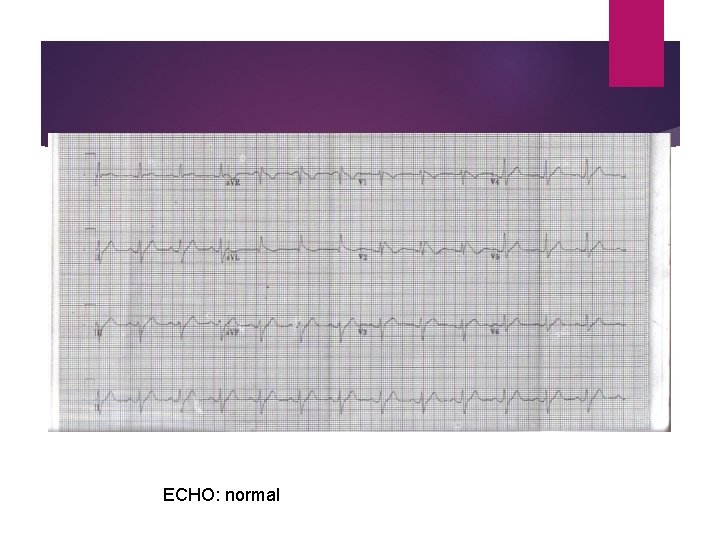
ECHO: normal
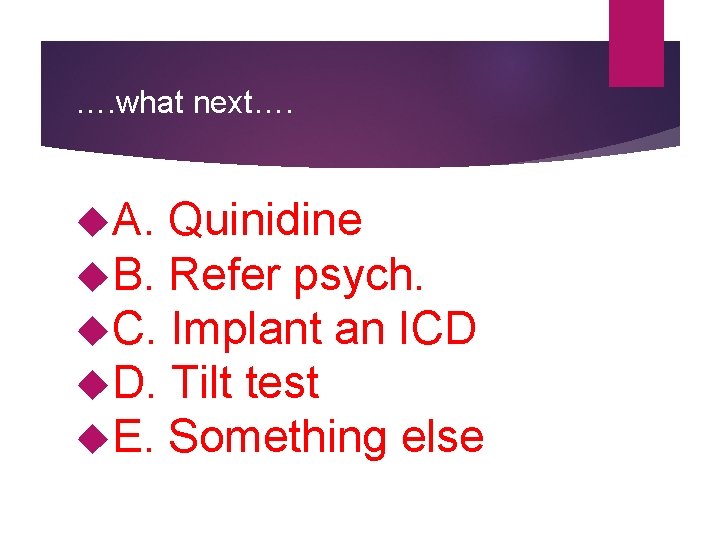
…. what next…. A. Quinidine B. Refer psych. C. Implant an ICD D. Tilt test E. Something else
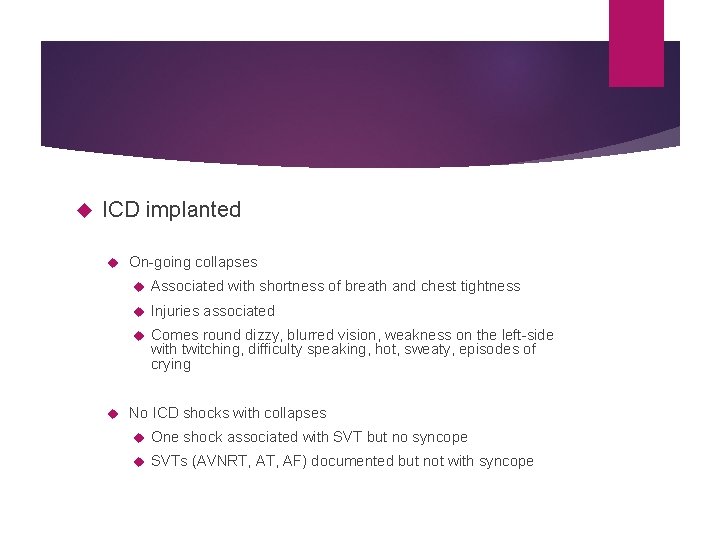
ICD implanted On-going collapses Associated with shortness of breath and chest tightness Injuries associated Comes round dizzy, blurred vision, weakness on the left-side with twitching, difficulty speaking, hot, sweaty, episodes of crying No ICD shocks with collapses One shock associated with SVT but no syncope SVTs (AVNRT, AF) documented but not with syncope
…. what next…. A. Refer neurology B. Refer psych. C. Tilt D. EPS E. Quinidine
…in fact we did everything… Further neuro’ review with more EEGs – nil abnormal TILT – negative EPS – dual AVN physiology only Chest review – advice on asthma (not that bad) Exercise echo / CT cors / angiogram Autonomic function tests MDT with ICC team (GSTT and the Heart) Psychological review
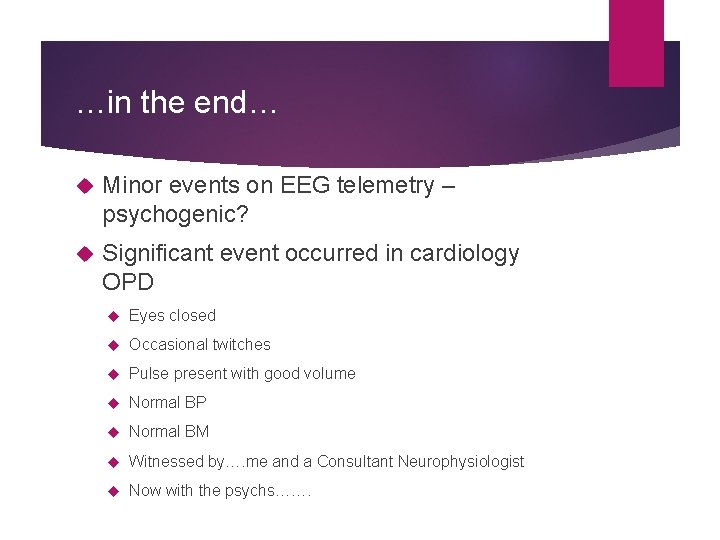
…in the end… Minor events on EEG telemetry – psychogenic? Significant event occurred in cardiology OPD Eyes closed Occasional twitches Pulse present with good volume Normal BP Normal BM Witnessed by…. me and a Consultant Neurophysiologist Now with the psychs…….
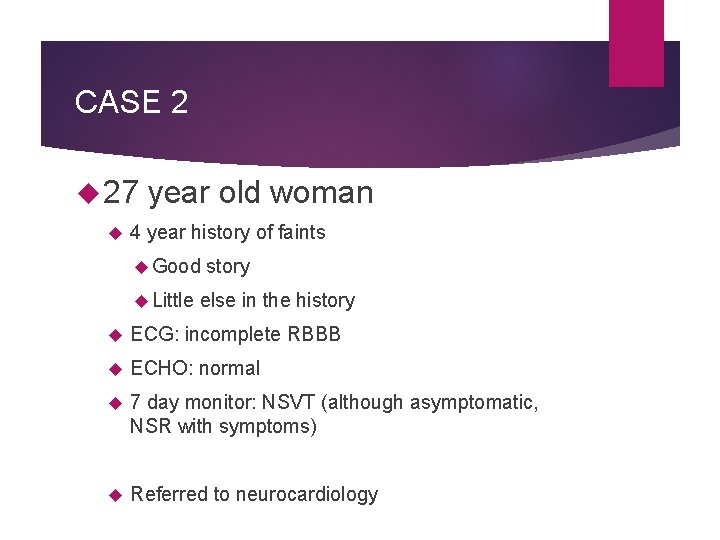
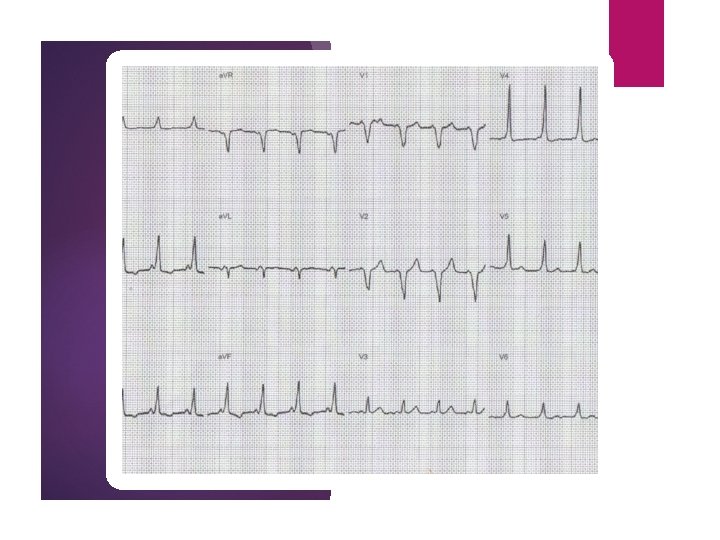
CASE 2 27 year old woman 4 year history of faints Good Little story else in the history ECG: incomplete RBBB ECHO: normal 7 day monitor: NSVT (although asymptomatic, NSR with symptoms) Referred to neurocardiology
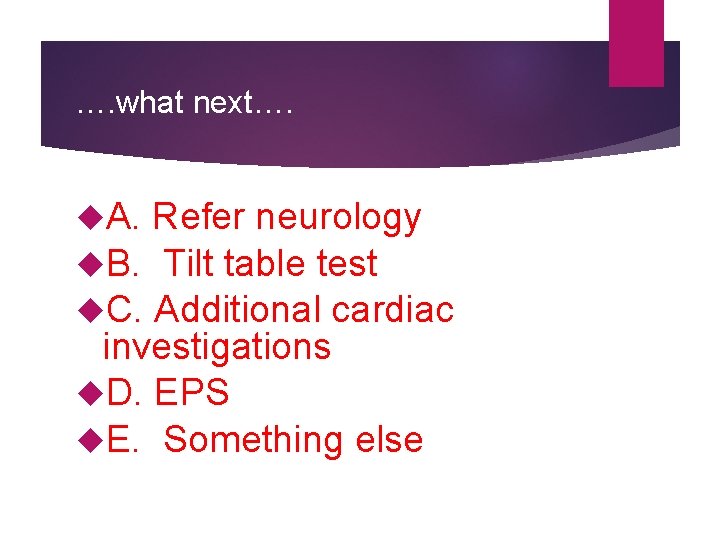
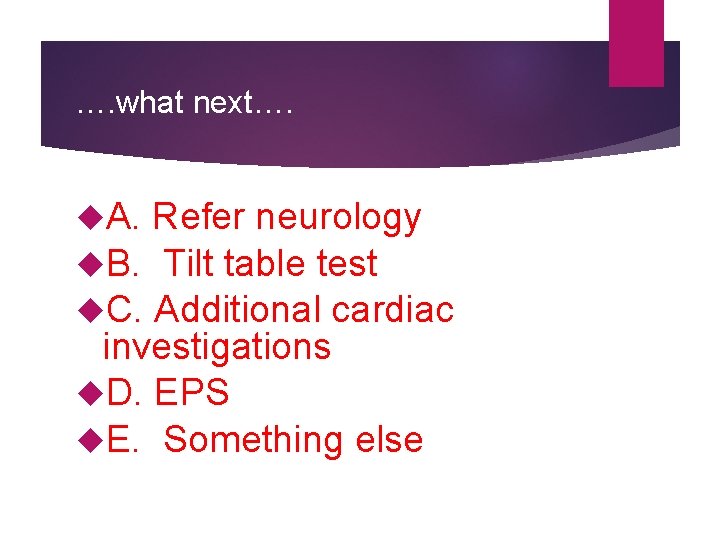
…. what next…. A. Refer neurology B. Tilt table test C. Additional cardiac investigations D. EPS E. Something else
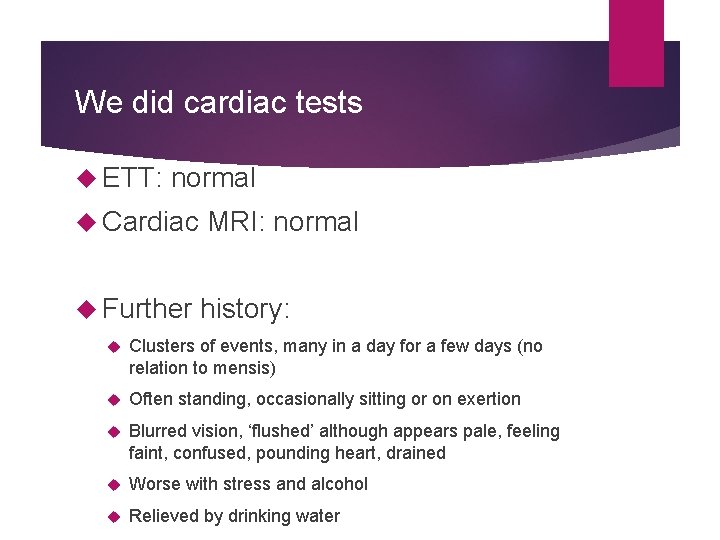
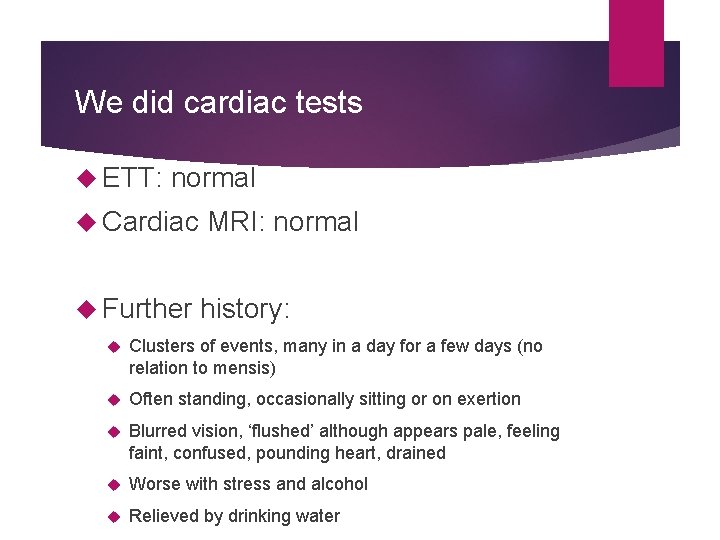
We did cardiac tests ETT: normal Cardiac MRI: normal Further history: Clusters of events, many in a day for a few days (no relation to mensis) Often standing, occasionally sitting or on exertion Blurred vision, ‘flushed’ although appears pale, feeling faint, confused, pounding heart, drained Worse with stress and alcohol Relieved by drinking water
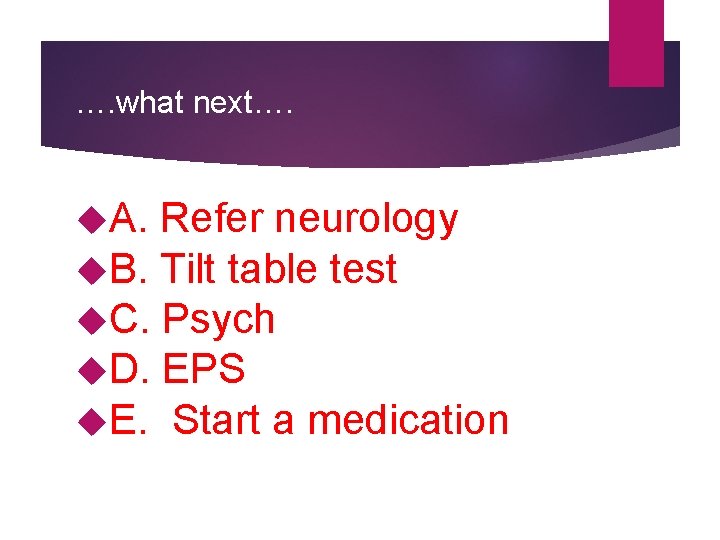
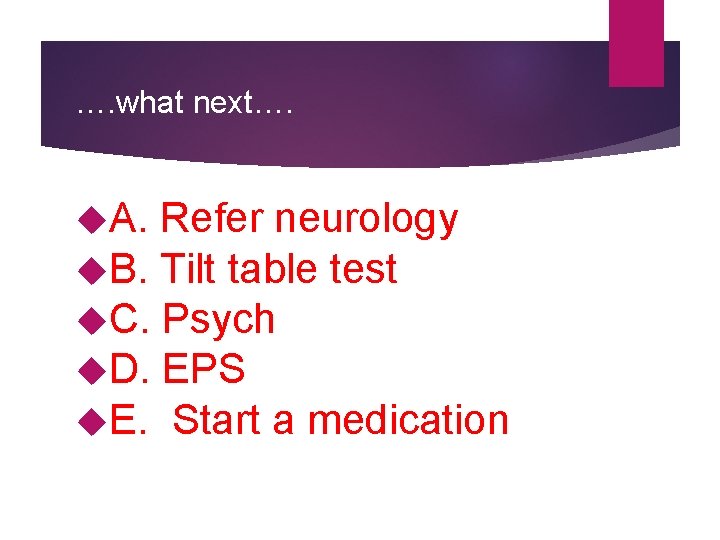
…. what next…. A. Refer neurology B. Tilt table test C. Psych D. EPS E. Start a medication
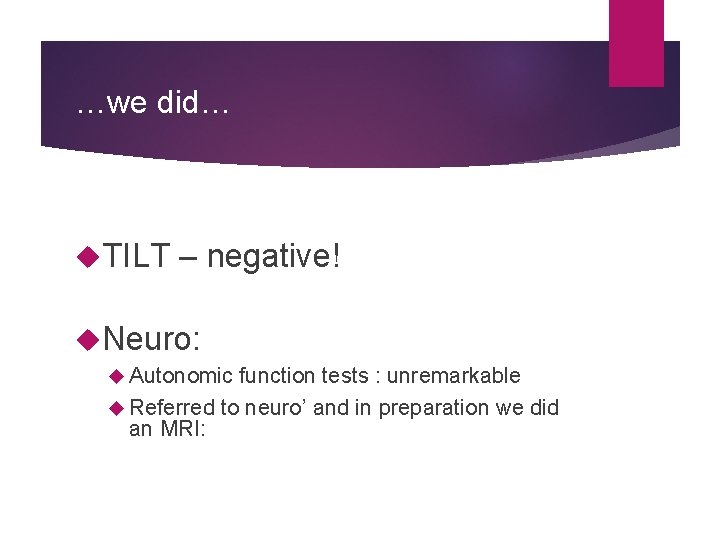
…we did… TILT – negative! Neuro: Autonomic function tests : unremarkable Referred to neuro’ and in preparation we did an MRI:
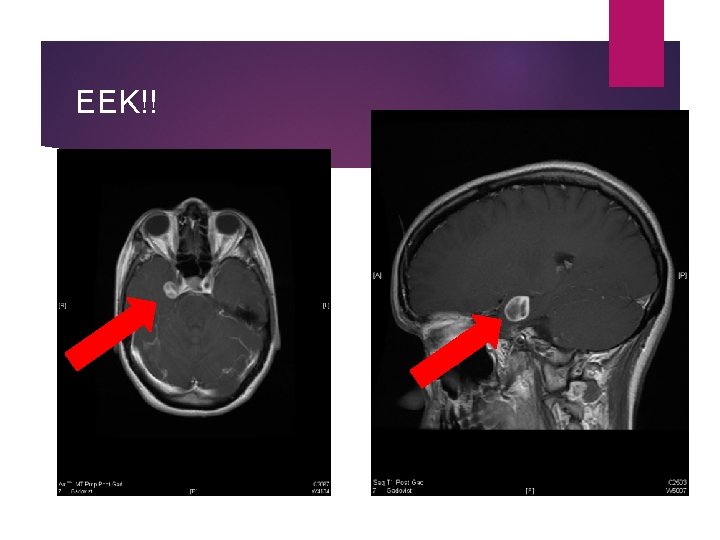
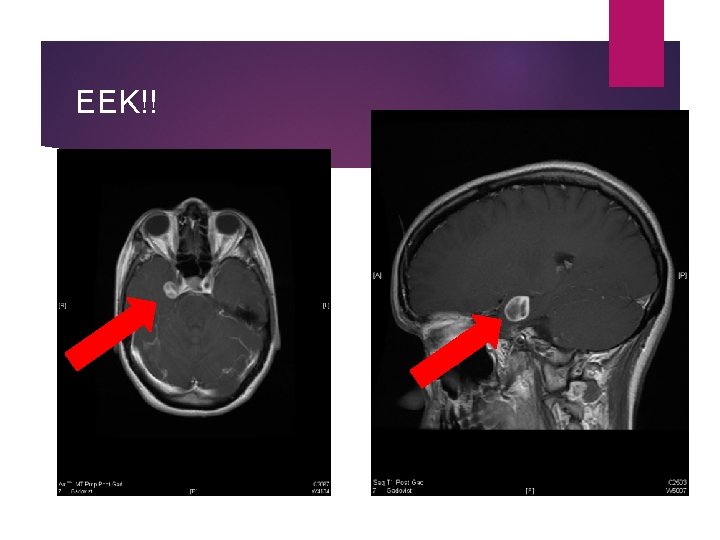
EEK!!
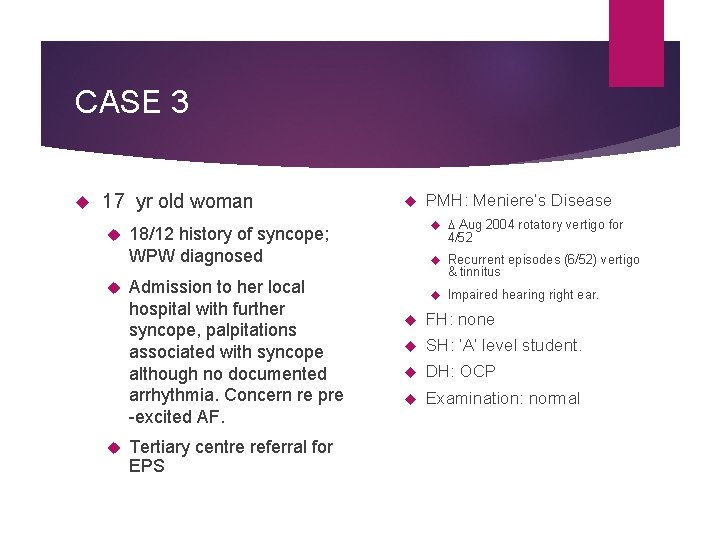
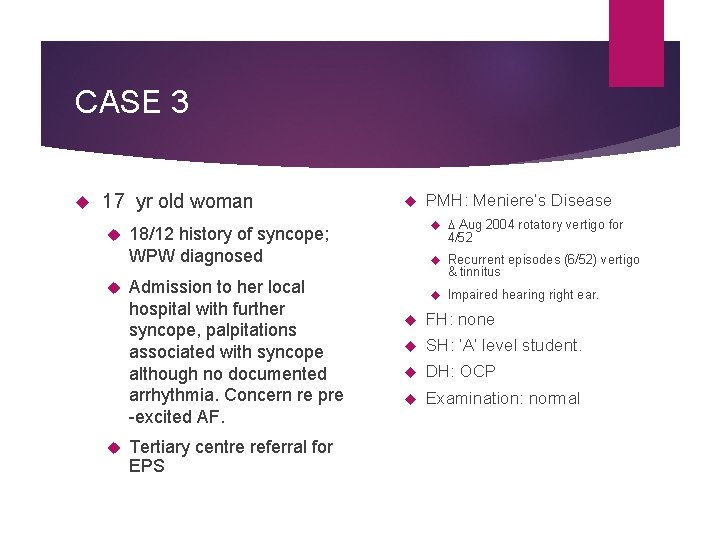
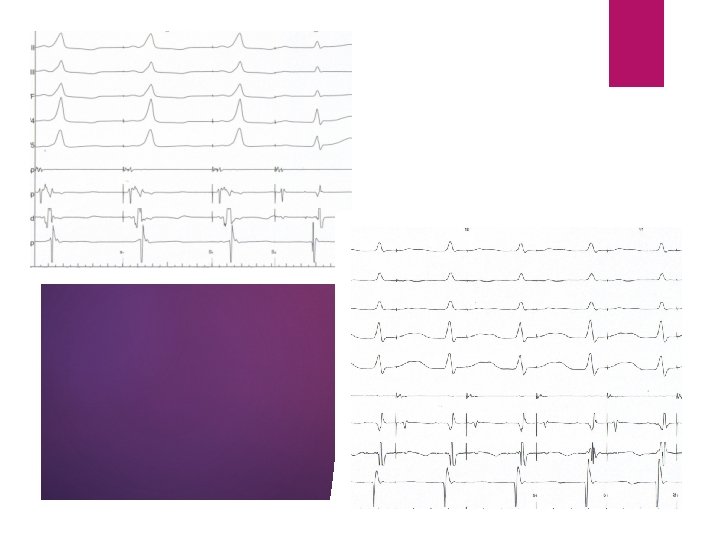
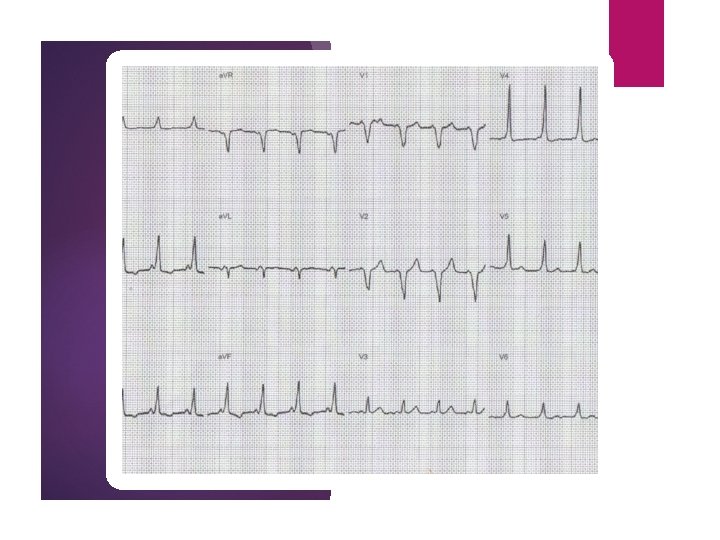
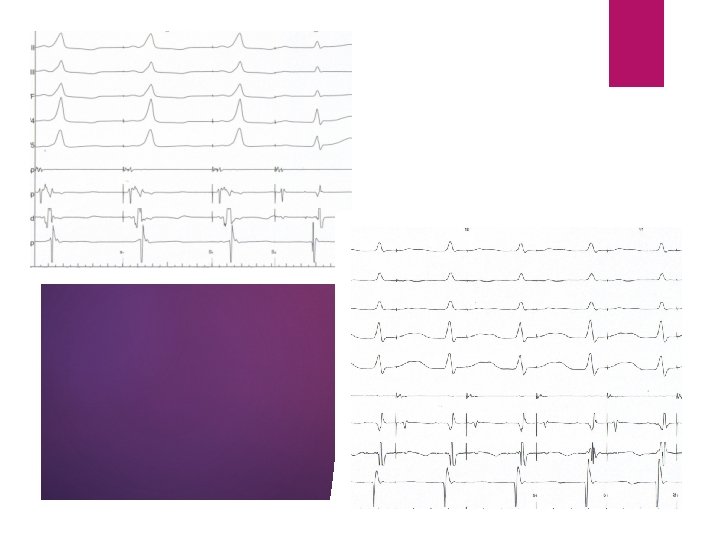
CASE 3 17 yr old woman Aug 2004 rotatory vertigo for 18/12 history of syncope; WPW diagnosed Admission to her local hospital with further syncope, palpitations associated with syncope although no documented arrhythmia. Concern re pre -excited AF. Tertiary centre referral for EPS PMH: Meniere’s Disease 4/52 Recurrent episodes (6/52) vertigo & tinnitus Impaired hearing right ear. FH: none SH: ‘A’ level student. DH: OCP Examination: normal
…. what next…. A. Refer neurology B. Refer psych. C. Implant an ILR D. EPS E. Something else
Syncope and SVT Fainting in SVT can relate to Rate Pre-excited AF In WPW can indicate risk but not necessarily Vaso-vagal reaction to the arrhythmia
…. what next…. A. Refer psych B. Medication C. Implant an ILR D. Ablation E. Refer Neuro
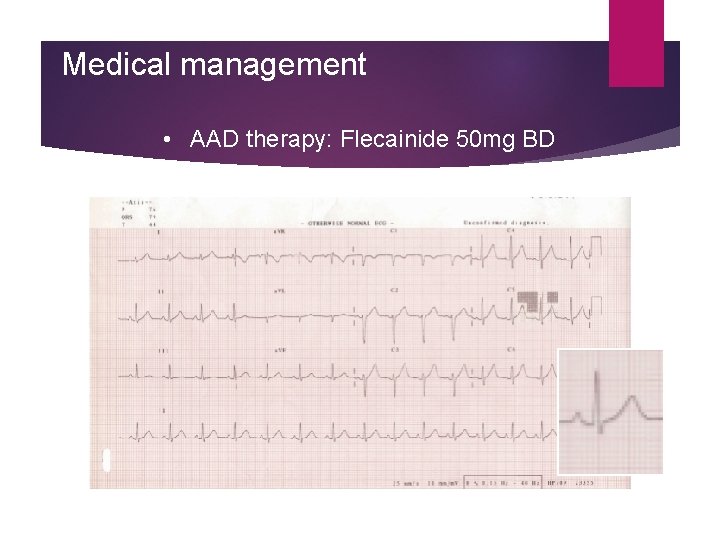
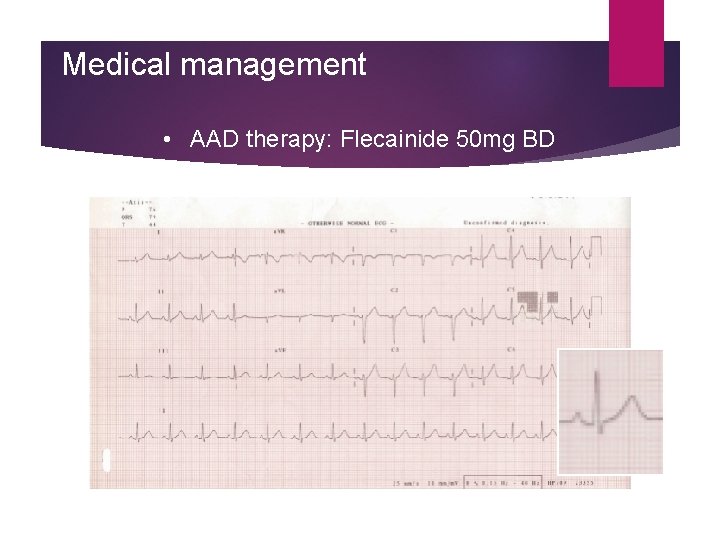
Medical management • AAD therapy: Flecainide 50 mg BD
Ablation Continued episodes of syncope In A&E weekly; Disrupting A level work Admitted for further evaluation: Cryoablation Pathway mapped to the mid-septal territory Ablated for 1 hour then returned! Subsequent long discussion with patient and her mother
…. what next…. A. Phone a friend B. Medication C. Implant an ILR D. Re-do ablation E. Something else

. . even more detailed history. . Recurrent syncope Slurred speech, dropping things Occipital headache Transient amnesia Hearing change Collapse for up to 40 minutes Floppy, ‘asleep’ Satisfactory HR and BP if assessed Poor relationship with mother’s new boyfriend Disruptive at school Poor relationships with teachers / GP
…. what next…. A. Phone a friend B. Medication C. Implant an ILR D. Re-do ablation E. Refer psych.
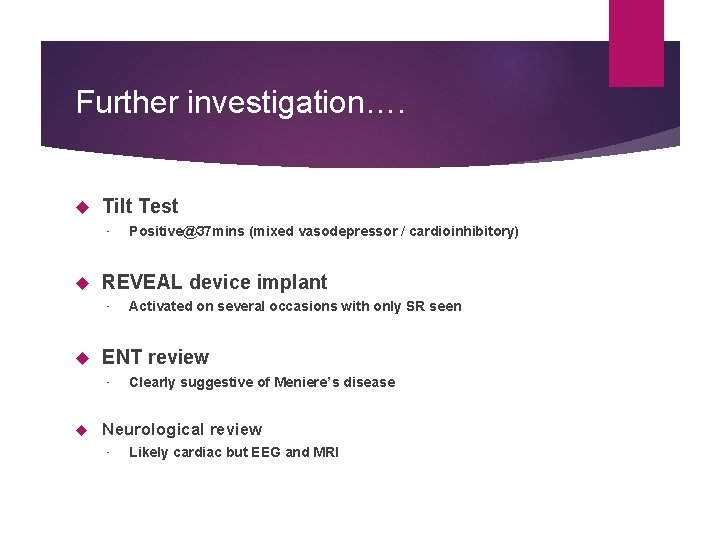
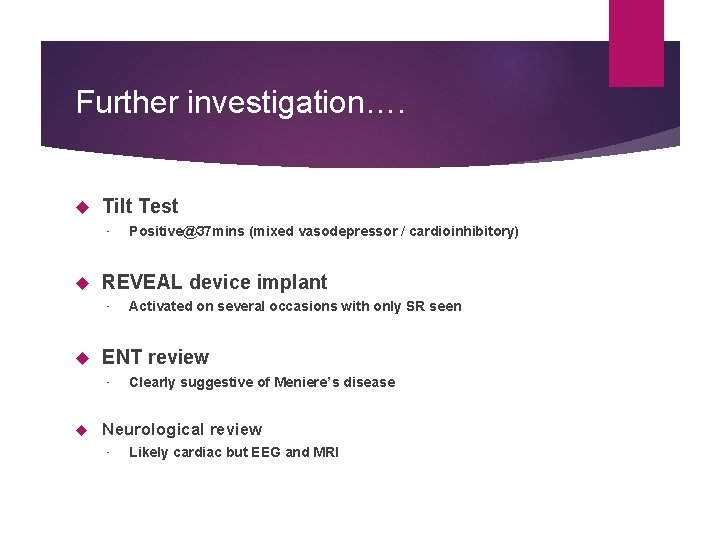
Further investigation…. Tilt Test • REVEAL device implant • Activated on several occasions with only SR seen ENT review • Positive@37 mins (mixed vasodepressor / cardioinhibitory) Clearly suggestive of Meniere’s disease Neurological review • Likely cardiac but EEG and MRI
…you know what’s coming…
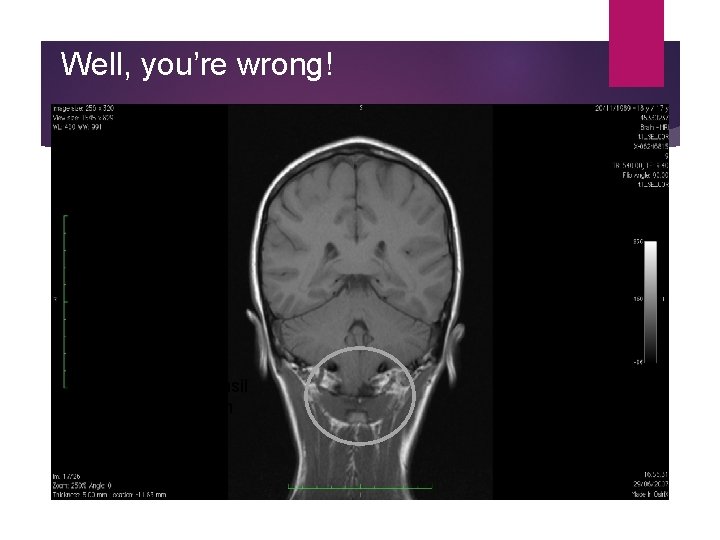
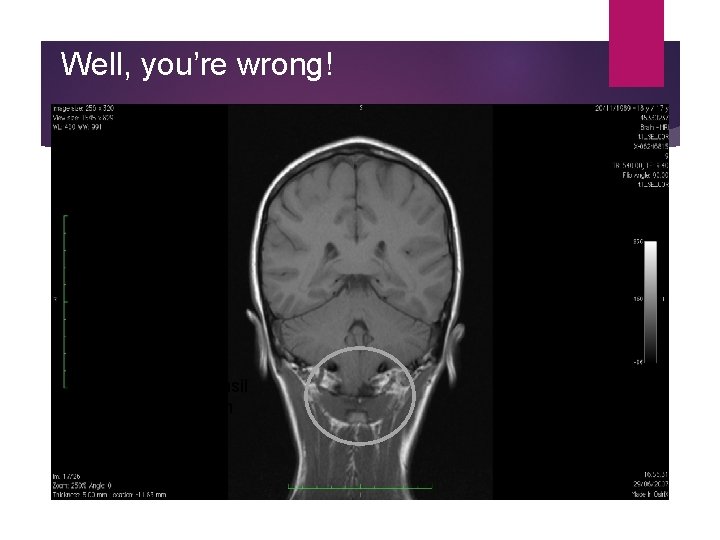
Well, you’re wrong! Right cerebellar tonsil herniation ~16 mm
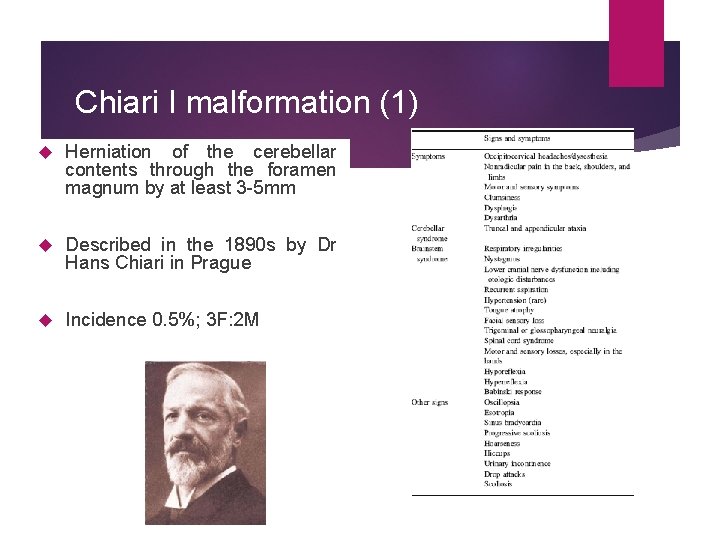
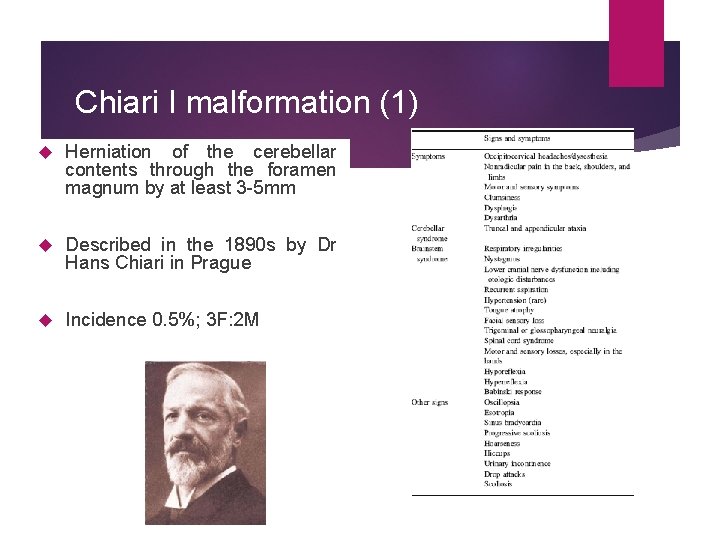
Chiari I malformation (1) Herniation of the cerebellar contents through the foramen magnum by at least 3 -5 mm Described in the 1890 s by Dr Hans Chiari in Prague Incidence 0. 5%; 3 F: 2 M
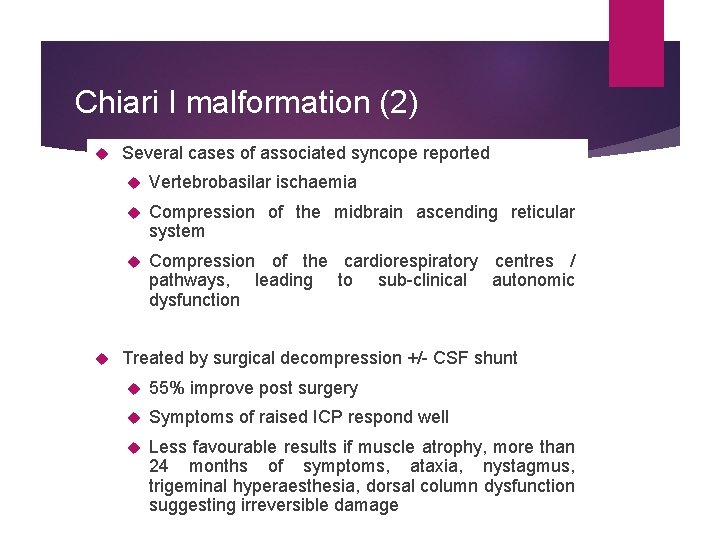
Chiari I malformation (2) Several cases of associated syncope reported Vertebrobasilar ischaemia Compression of the midbrain ascending reticular system Compression of the cardiorespiratory centres / pathways, leading to sub-clinical autonomic dysfunction Treated by surgical decompression +/- CSF shunt 55% improve post surgery Symptoms of raised ICP respond well Less favourable results if muscle atrophy, more than 24 months of symptoms, ataxia, nystagmus, trigeminal hyperaesthesia, dorsal column dysfunction suggesting irreversible damage
…since then… Surgical decompression performed early 2008 Chiari events resolved Neurocardiogenic / stress-related events better since left school and life settled down! Still hasn’t had an ablation!
…AND NOW. . . LUNCH