Case presentation Tania Jain Chief medical resident Detroit













- Slides: 64
Case presentation Tania Jain Chief medical resident Detroit Receiving Hospital

Idea of an M and M conference • Learn (that’s why we are in a training program ; ) • Improve the system (we owe it to the hospital !)
Idea of an M and M conference • Learn (that’s why we are in a training program ; ) • Improve the system (we owe it to the hospital !) • Have fun
At admission • 68 yo man with h/o CAD (s/p MI and PCI in 2006) • 2 weeks of generalized abdominal pain, constipation (8 days) and weight loss (15 -20 lbs) • ROS – cough
Other histories…. • PMHx: CAD (patient reports he doesn't take any medications, currently) • PSHx: Cardiac stent 2006 • Family Hx: Mother - MI, Father - TB • Social Hx: 1 PPD x 20 years (quit 2006); 1 fifth/day (quit 2006); remote IV heroin (60's and 70's) • Allergies: NKDA

Physical exam • HR 117 • Vital signs including RR and O 2 Sat. were normal range (12 -18/ 96 -100%) • Respiratory: Positive egophony on left lung. • Gastrointestinal: Diffusely tender to palpation without rebound/ guarding, no masses
ER work-up • Abdominal XR = No obstruction/ air fluid level Atelectasis with central bronchial obstruction


More about the cough ? • Cough productive of thick, white phlegm. • Dyspnea at rest as well as fatigue, generalized weakness and inability to walk • No fever, night sweats, hemoptysis • Only exposure in distant past (father; died many years ago)




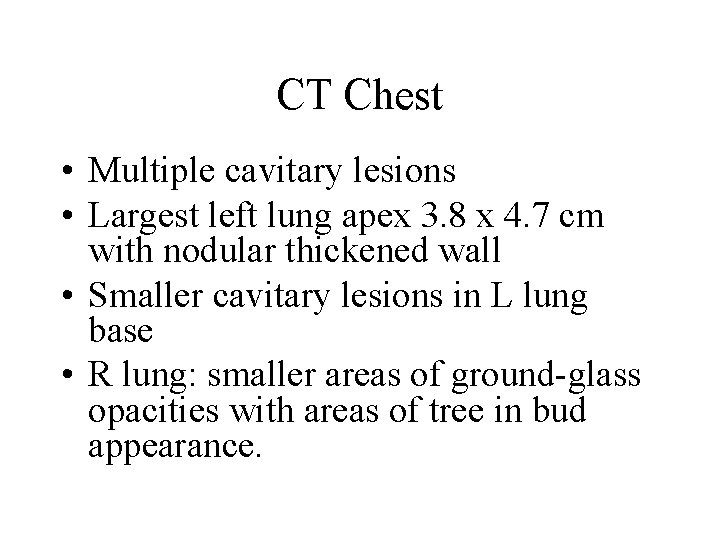
CT Chest • Multiple cavitary lesions • Largest left lung apex 3. 8 x 4. 7 cm with nodular thickened wall • Smaller cavitary lesions in L lung base • R lung: smaller areas of ground-glass opacities with areas of tree in bud appearance.
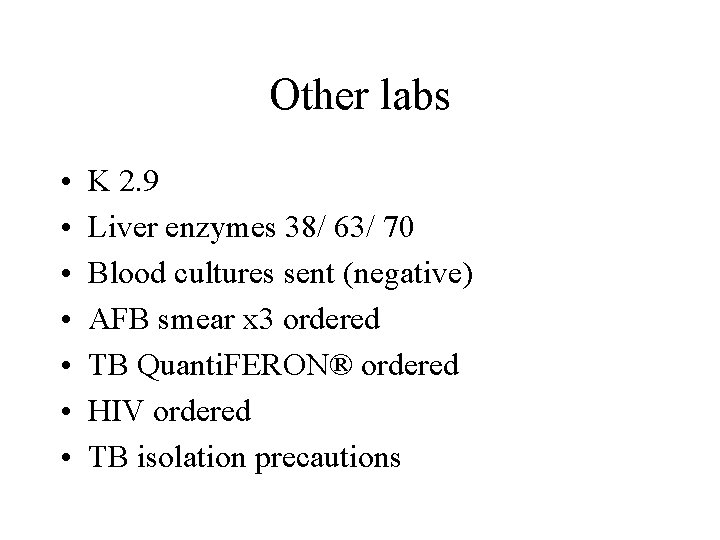
Other labs • • K 2. 9 Liver enzymes 38/ 63/ 70 Blood cultures sent (negative) AFB smear x 3 ordered TB Quanti. FERON® ordered HIV ordered TB isolation precautions
Day 2 • With Pulmonary consulted, plan is to pursue a bronchoscopy if AFB x 3 negative (concern infections vs malignancy)
By Day 5 • 3 x AFB sputum smear reported negative * producing very little sputum * one sample was induced sputum by RT * One morning sample
Oh BTW…. • The morning of day 5 (which is the day patient scheduled for bronchoscopy), TB Quanti. FERON® reported positive
What do you do now ? ? Discontinue isolation ? Bronchoscopy ? Nucleic acid amplification ? Treat active TB ? Treat latent TB
What actually happened ? • AFB isolation discontinued • Patient underwent bronchoscopy
A few hours post-bronchoscopy… • • Tachypneic with RR 30 s Tachycardic to HR 150 s Hypoxic w/ SPO 2 92 on 4 L NC Accessory muscle use. Crackles, most prominent over left upper lung field. Decreased breath sounds, more prominent on left side • ABG 7. 5 / 22 / 65 / 20 / 93, lact 3. 4 • Transferred to MICU for new sepsis secondary to HCAP ; Rx vancomycin and cefepime

Day 6 & 7 • • BAL smear : 4+ AFB isolation re-initiated Started on RIPE Blood and respiratory fungal cultures negative
Back on floors • • Repeat 3 AFP sputum - negative BAL sent for susceptibility testing Continued RIPE and AFB isolation Discharged after 2 weeks inpatient RIPE; Detroit/ Michigan dept of health informed; TB clinic follow up
• Day 30, sputum cultures (from day 2, 3) are reported positive for Mycobacterium tuberculosis

Aim • To understand the following about TB diagnosis and prevention : ? CDC guidelines to prevent transmission ? Testing for TB diagnosis ? Role of bronchoscopy ? When in doubt
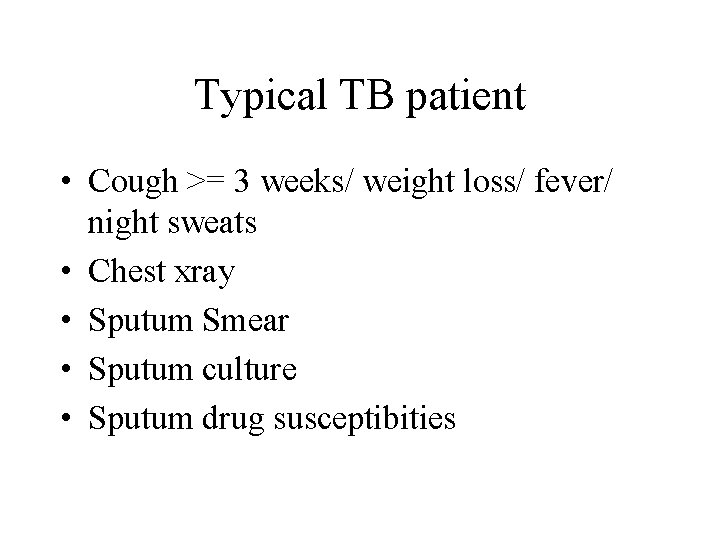
Typical TB patient • Cough >= 3 weeks/ weight loss/ fever/ night sweats • Chest xray • Sputum Smear • Sputum culture • Sputum drug susceptibities
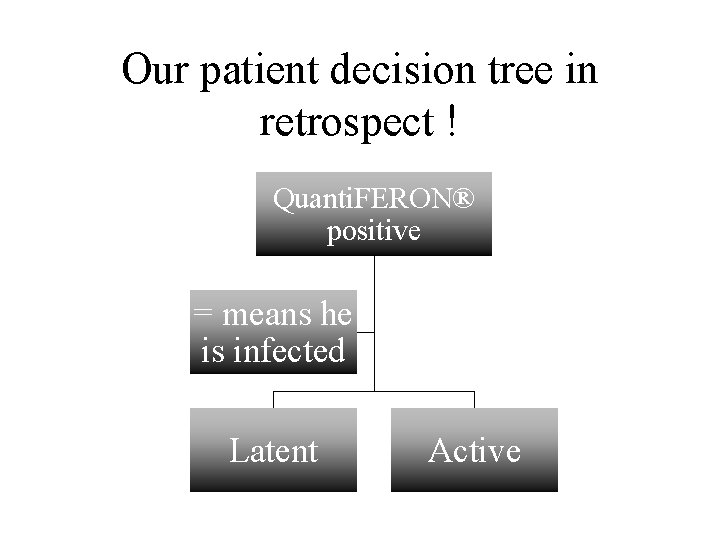
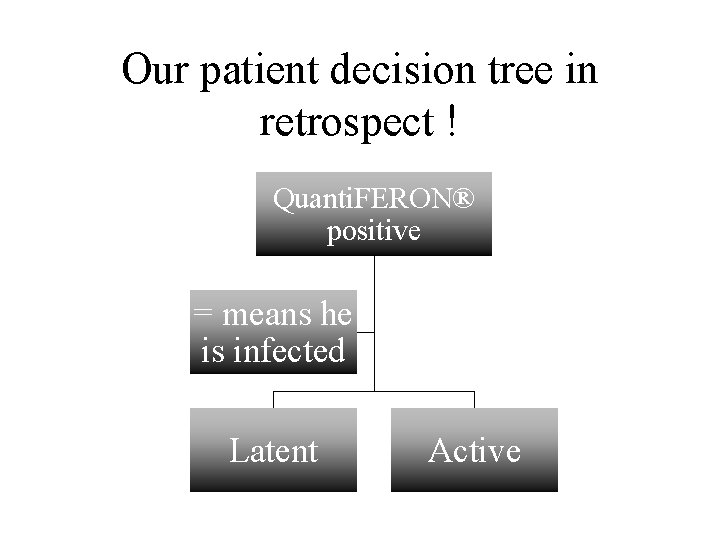
Our patient decision tree in retrospect ! Quanti. FERON® positive = means he is infected Latent Active
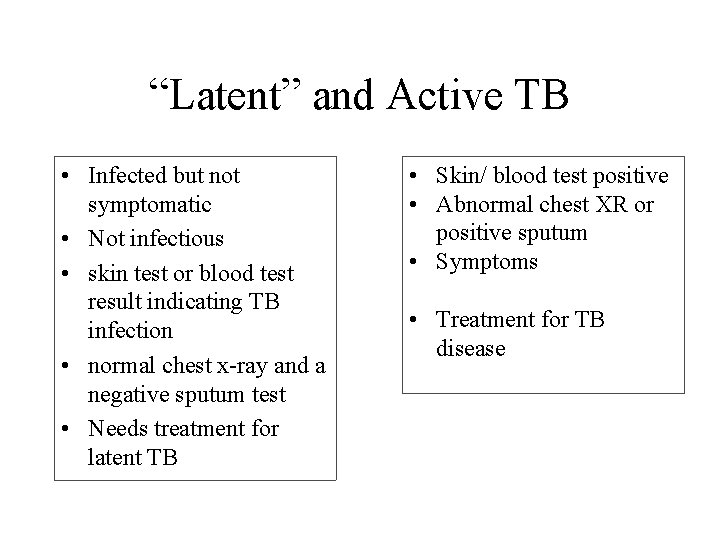
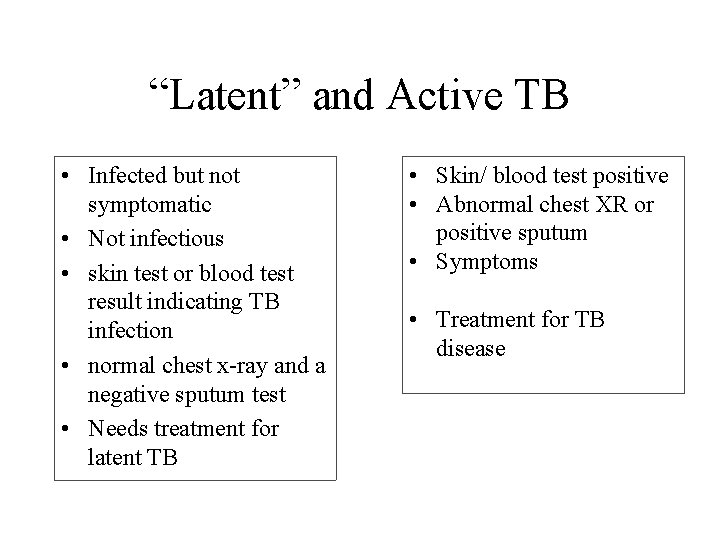
“Latent” and Active TB • Infected but not symptomatic • Not infectious • skin test or blood test result indicating TB infection • normal chest x-ray and a negative sputum test • Needs treatment for latent TB • Skin/ blood test positive • Abnormal chest XR or positive sputum • Symptoms • Treatment for TB disease
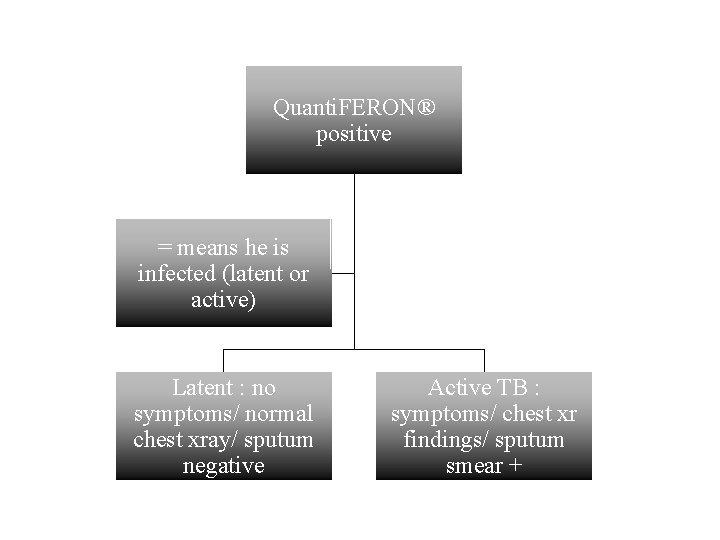
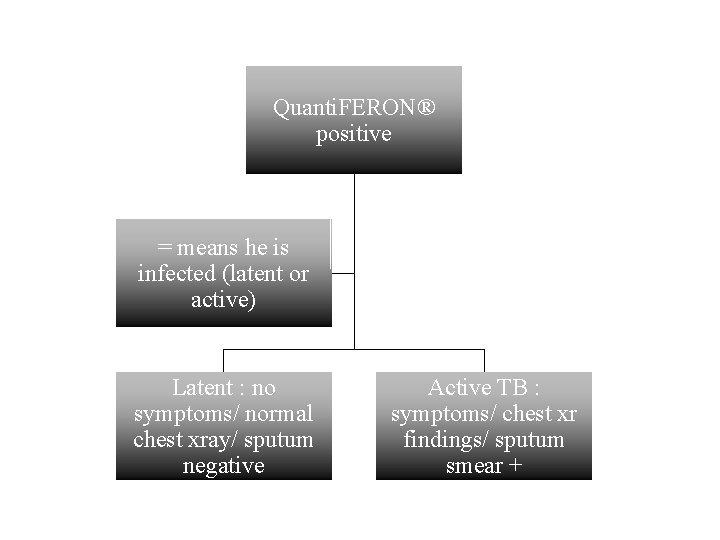
Quanti. FERON® positive = means he is infected (latent or active) Latent : no symptoms/ normal chest xray/ sputum negative Active TB : symptoms/ chest xr findings/ sputum smear +
Preventing transmission • Who to isolate ? “Anyone suspected to have TB disease OR has known TB disease and has not had enough treatment”
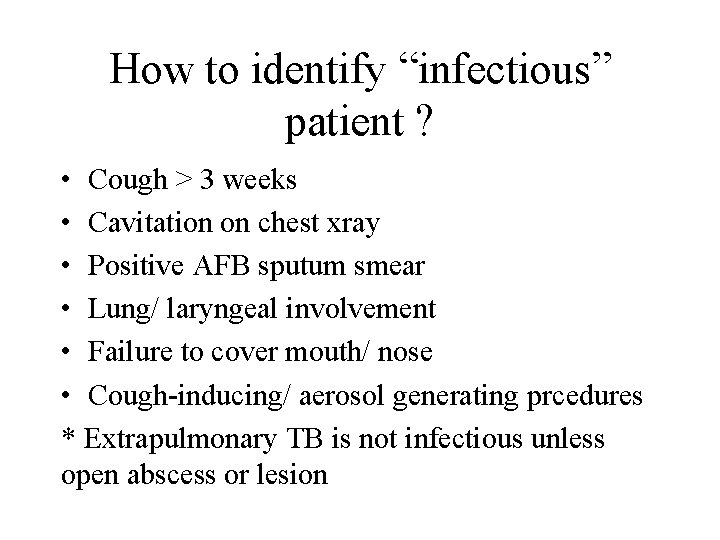
How to identify “infectious” patient ? • Cough > 3 weeks • Cavitation on chest xray • Positive AFB sputum smear • Lung/ laryngeal involvement • Failure to cover mouth/ nose • Cough-inducing/ aerosol generating prcedures * Extrapulmonary TB is not infectious unless open abscess or lesion
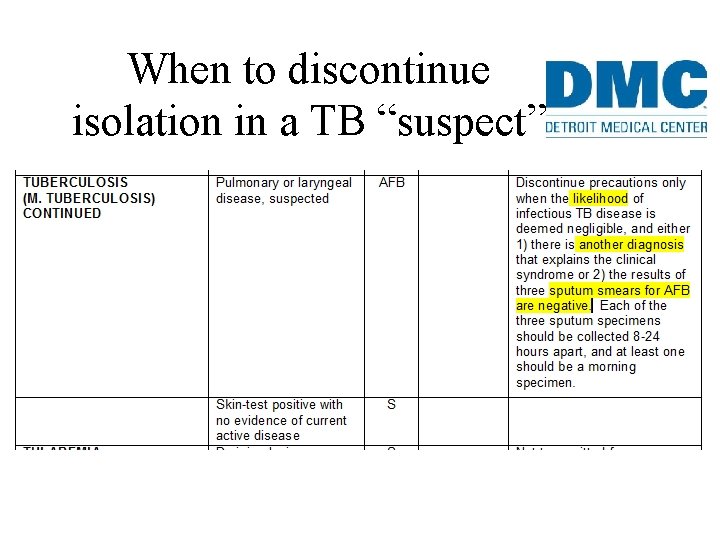
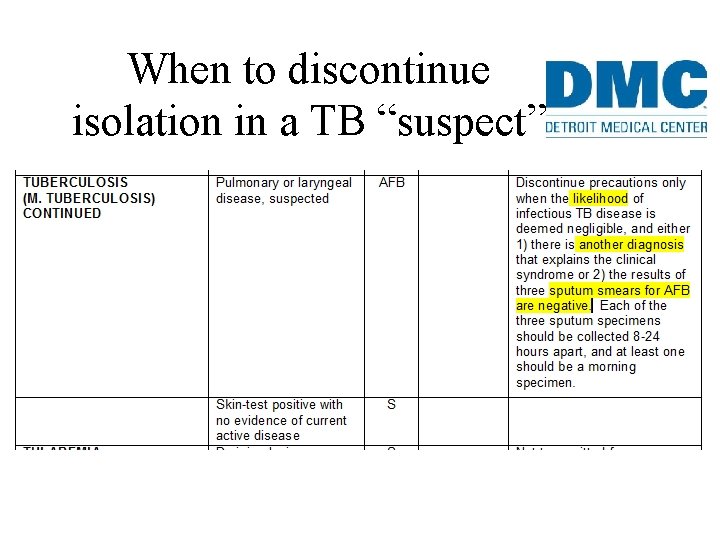
When to discontinue isolation in a TB “suspect”
• Likelihood of TB AND Another possible diagnosis OR AFB smears negative x 3
Excerpts from CDC : • Hospitalized patients for whom suspicion of TB remains after 3 negative AFB sputum smear should not be released from airborne precautions until they are on standard multidrug antituberculosis treatment and are clinically improving.
Fun fact • In one study, 17% of transmission occurred from person with negative AFB smear results. Behr MA etal. Transmission of mycobacterium tuberculosis from patients smearnegative for acid-fast bacilli. Lancet 1999; 353: 444 -9
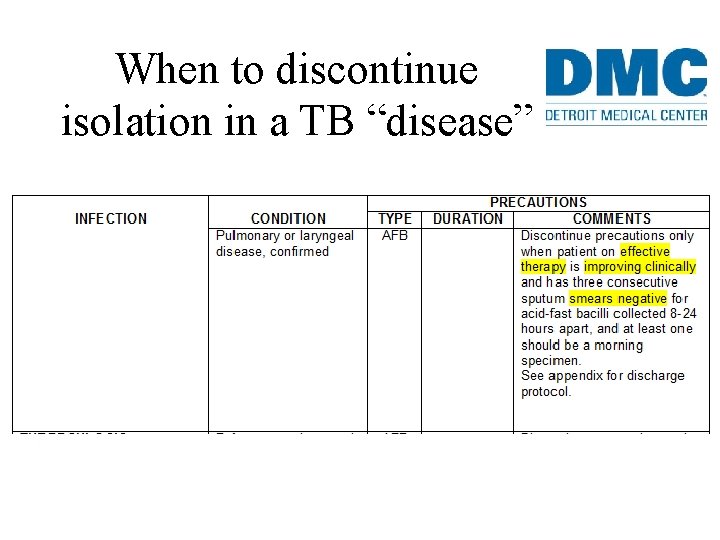
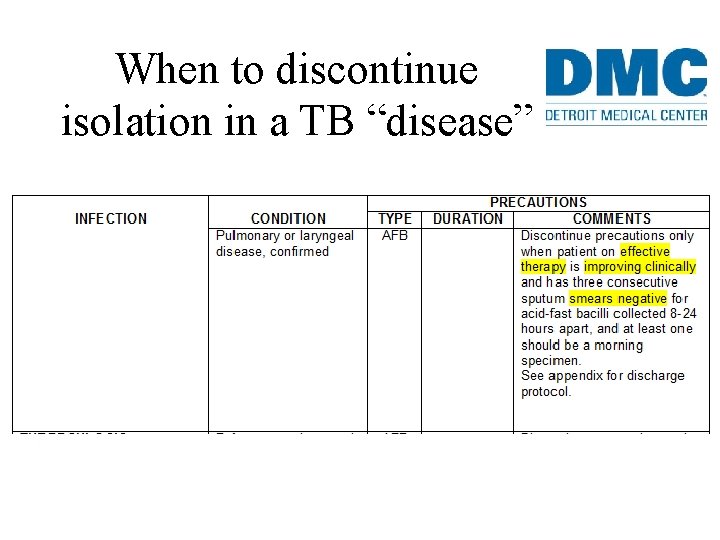
When to discontinue isolation in a TB “disease”
• Effective therapy for 2 weeks • Clinical improvement • AFB smears negative x 3
How about discharge home ? • Specific plan for follow up • Standard multidrug TB Rx and DOT • No infants/ children < 4 yrs or immunosuppressed • Immunocompetent members have been exposed
Diagnostic procedures for TB
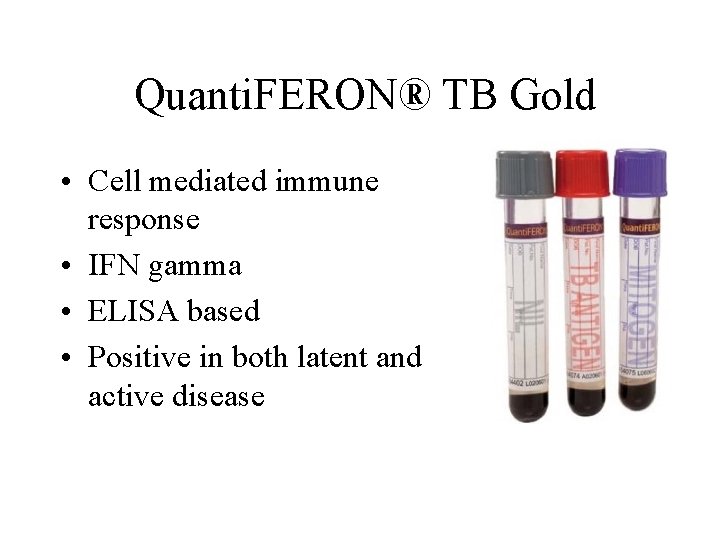
Quanti. FERON® TB Gold • Cell mediated immune response • IFN gamma • ELISA based • Positive in both latent and active disease
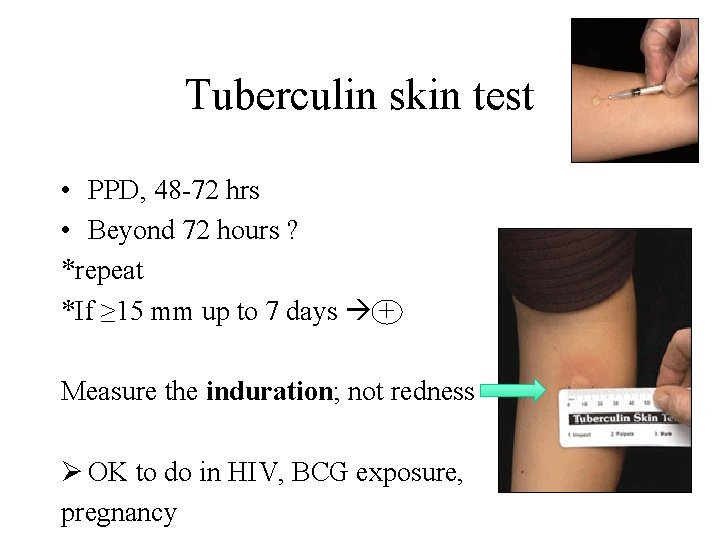
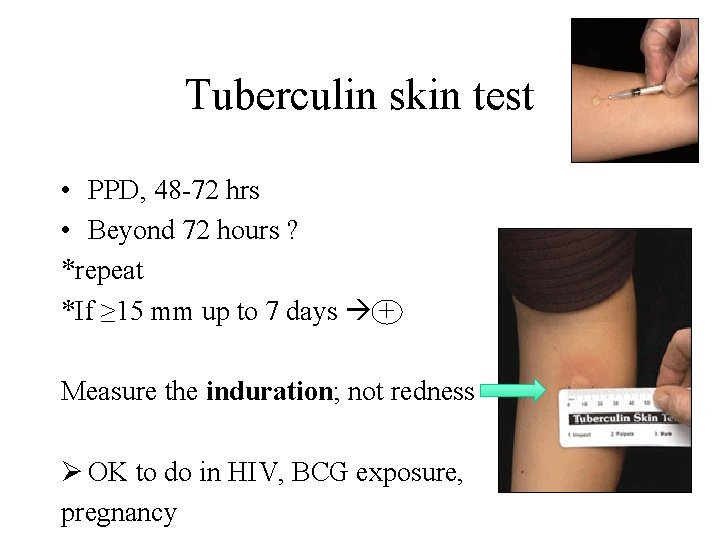
Tuberculin skin test • PPD, 48 -72 hrs • Beyond 72 hours ? *repeat *If ≥ 15 mm up to 7 days + Measure the induration; not redness Ø OK to do in HIV, BCG exposure, pregnancy

Interpreting the TST Size of induration: >5 mm highest risk, HIV, known exposure >10 mm other risk factors >15 mm no known risk factors
Chest radiography • Active disease: upper lobe infiltration/ cavity/ effusion • Healed: nodules, fibrotic scars, calcified granulomas or basal pleural effusion • Normal in latent TB • HIV: infiltrate in any lung zone, mediastinal or hilar LAD, normal
Sputum samples • 3 samples, 8 – 24 hours apart, atleast 1 morning • Type: Spontaneous expectoration Induced sputum Gastric aspirate (esp children) Bronchoscopy sample
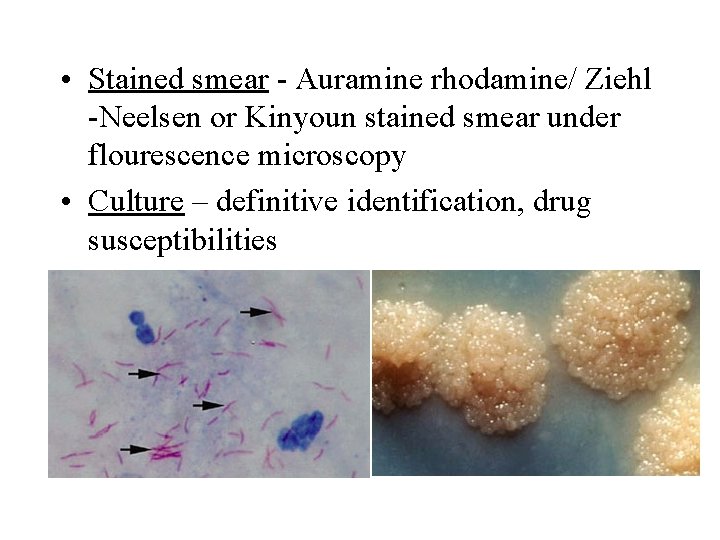
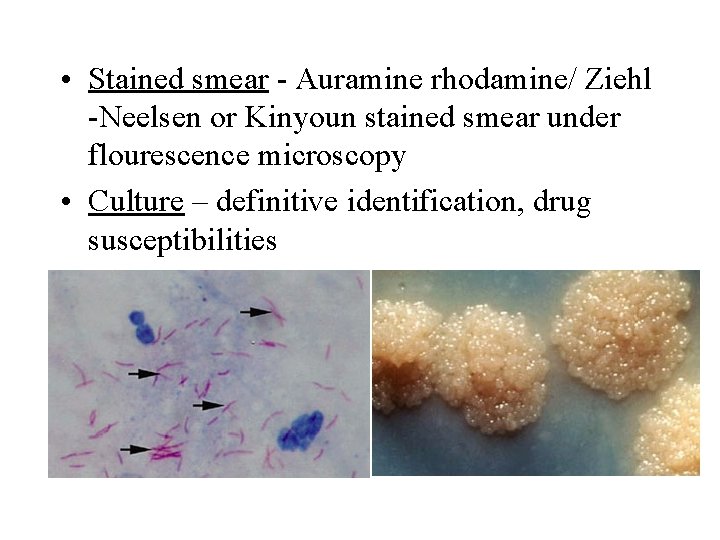
• Stained smear - Auramine rhodamine/ Ziehl -Neelsen or Kinyoun stained smear under flourescence microscopy • Culture – definitive identification, drug susceptibilities
Nucleic acid amplification • 70% sensitivity in smear negative • Utilize a lot of amount of specimen, which could be used for culture/ drug susceptibilities • Should not replace culture and drugsusceptibility testing in suspected TB.
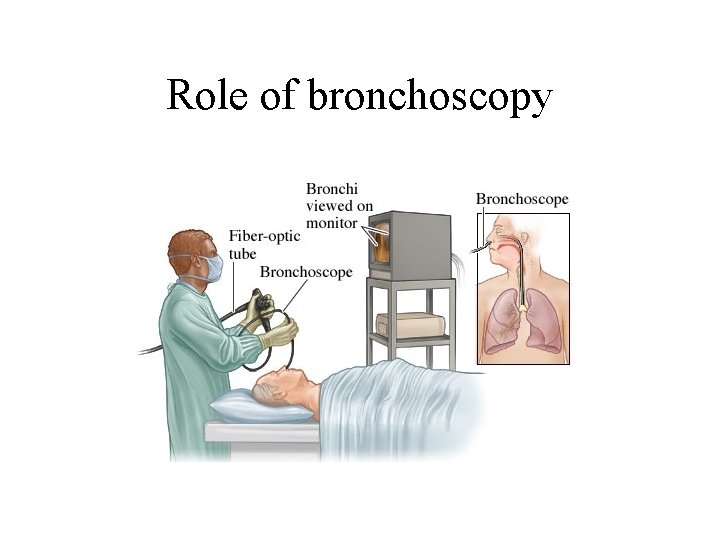
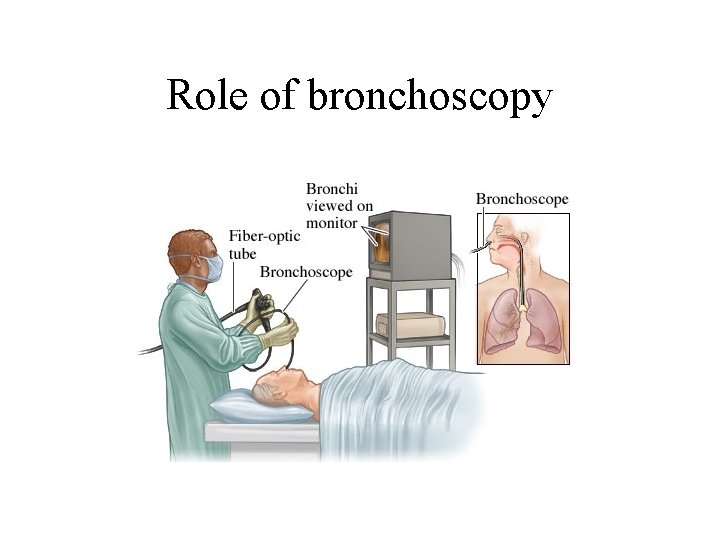
Role of bronchoscopy

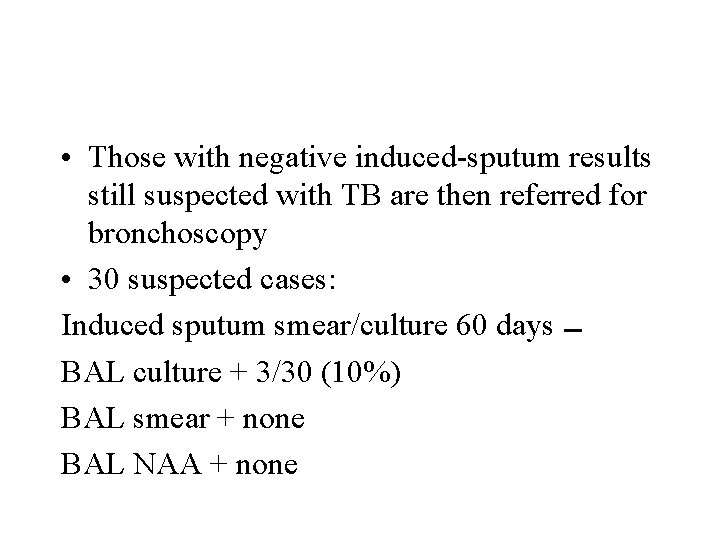
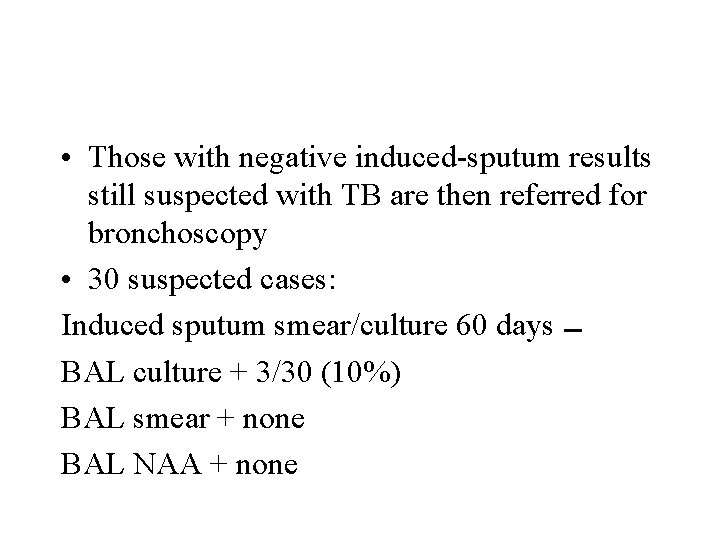
• Those with negative induced-sputum results still suspected with TB are then referred for bronchoscopy • 30 suspected cases: Induced sputum smear/culture 60 days BAL culture + 3/30 (10%) BAL smear + none BAL NAA + none
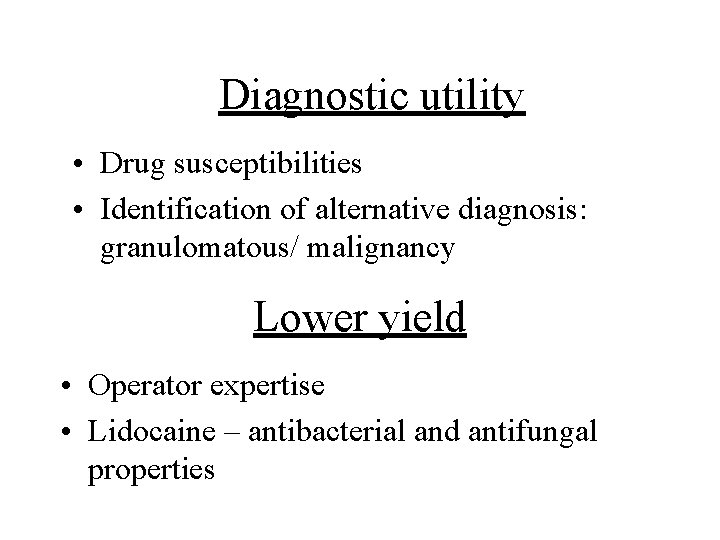
Diagnostic utility • Drug susceptibilities • Identification of alternative diagnosis: granulomatous/ malignancy Lower yield • Operator expertise • Lidocaine – antibacterial and antifungal properties

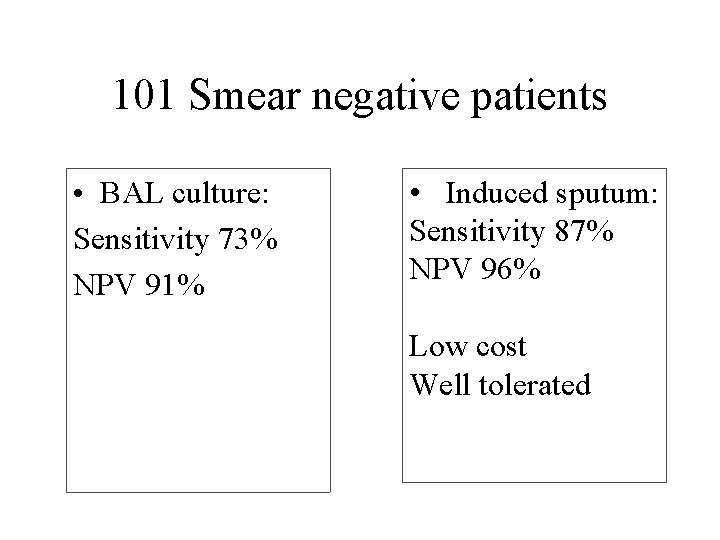
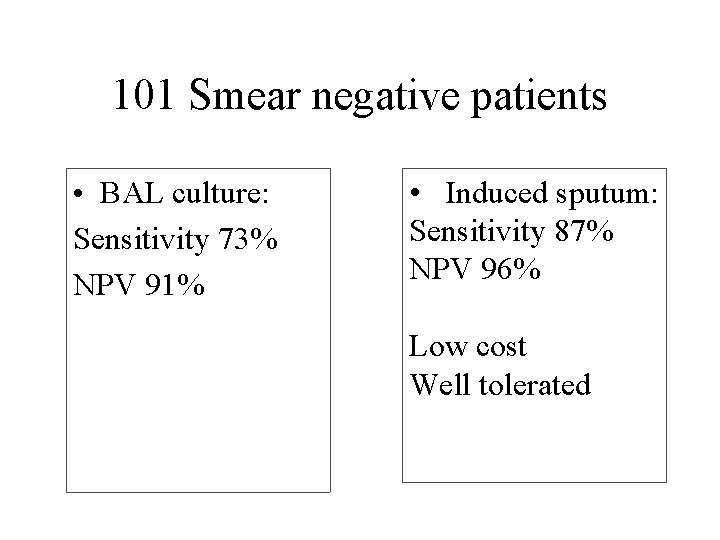
101 Smear negative patients • BAL culture: Sensitivity 73% NPV 91% • Induced sputum: Sensitivity 87% NPV 96% Low cost Well tolerated
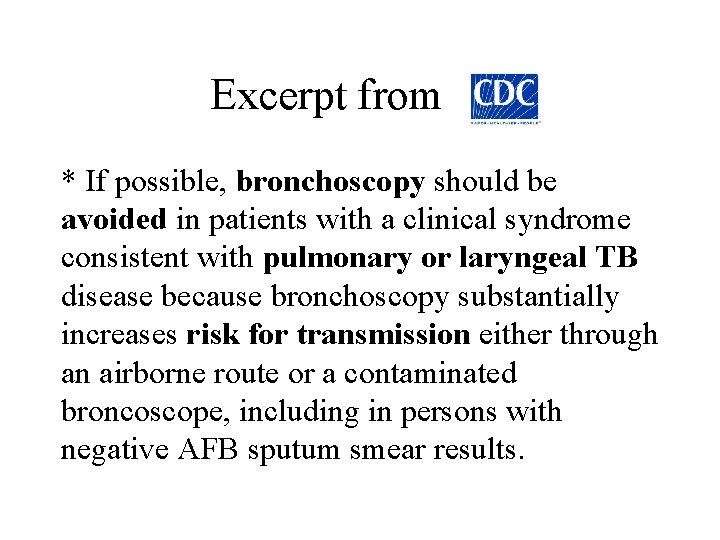
Excerpt from * If possible, bronchoscopy should be avoided in patients with a clinical syndrome consistent with pulmonary or laryngeal TB disease because bronchoscopy substantially increases risk for transmission either through an airborne route or a contaminated broncoscope, including in persons with negative AFB sputum smear results.
Excerpt from • If the underlying cause of radiographic abnormality remains unknown, additional evaluation with bronchoscopy might be indicated; however, in case where TB disease remains a diagnostic possibility, initiation of a standard TB regimen for a period before bronchoscopy might reduce the risk for transmission.
Excerpt from • If bronchoscopy is performed, because it is a cough-inducing procedure, additional sputum samples for AFB smear and culture should be collected after the procedure to increase the diagnostic yield.
HIV Testing u Who to test for HIV ? Every patient with latent or active TB u Why ? Progression from latent to active TB. Rapid progression/ fatal. Rapid expansion of outbreaks. u What test ? Rapid HIV/ Standard labs assays
Hot off the press from MMWR. .
DMC does not have this test available ! • Automated nucleic acid amplification test that can simultaneously identify M. tuberculosis and rifampin resistance within 2 hours. • 98 percent of patients with smear-positive tuberculosis and 72 percent of patients with smear-negative/culture-positive tuberculosis
This recent newsletter says… • To aid in decision of whether continued airborne isolation is warranted for pts with suspected pulmonary TB. • Per the data presented at Conference on Retroviruses and Opportunistic Infections in Seattle in Feb 2015, negative Xpert MTB/RIF assay results form either one or two sputum samples are highly predictive of results of two or three negative AFB sputum smears. • Single negative Xpert assay NPV 99. 7% (99. 6% in USA and 100% outside) • Two serial negative NPV 100%
Take home ! • • High suspicion “Intraweb” / DMC resources Take you own history It’s ok to seek help when in doubt
Acknowledgments Dr D. Kissner Dr R. Roxas Dr S. Dhar CDC
 Tarrytown chief resident conference
Tarrytown chief resident conference Chapter 9 lesson 3 commander in chief and chief diplomat
Chapter 9 lesson 3 commander in chief and chief diplomat Vidya jain case
Vidya jain case Case study conclusion
Case study conclusion Best worst and average case
Best worst and average case Chief medical officers physical activity guidelines
Chief medical officers physical activity guidelines Tania stathaki
Tania stathaki Pabellon areilza basurto
Pabellon areilza basurto Tania mattiuzzo psicologa
Tania mattiuzzo psicologa Tania sabugal
Tania sabugal Moodle logopedia unipd
Moodle logopedia unipd Tania wolfgramm
Tania wolfgramm Dr tania brasse
Dr tania brasse Liceo scientifico ferro
Liceo scientifico ferro Tania dennison
Tania dennison Tania alfaro
Tania alfaro Tania amelie leblond
Tania amelie leblond Tania tomasi
Tania tomasi Tania tomasi
Tania tomasi Tania tomasi
Tania tomasi Dr tania tillett
Dr tania tillett Tania naanous
Tania naanous Nacac step by step
Nacac step by step Tania barry
Tania barry Tania manrique gómez
Tania manrique gómez Tania bruguera
Tania bruguera Tania stathaki
Tania stathaki Tania otero
Tania otero Tania tomasi
Tania tomasi Resident set management
Resident set management Resident retention
Resident retention Resident set management
Resident set management Resident and citizen
Resident and citizen Divine intervention 143
Divine intervention 143 Resident lifecycle
Resident lifecycle Chapter 2 foundations of resident care
Chapter 2 foundations of resident care Attending vs resident
Attending vs resident Misappropriation of resident property
Misappropriation of resident property Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease When ambulating a resident should be wearing
When ambulating a resident should be wearing Partially resident textures
Partially resident textures Acgme resident survey
Acgme resident survey Employment of non-resident aliens in the philippines
Employment of non-resident aliens in the philippines Orientation and resident rights quiz
Orientation and resident rights quiz Customer service conflict resolution
Customer service conflict resolution Define resident flora
Define resident flora Resident subnet
Resident subnet Resident assessment instrument definition
Resident assessment instrument definition Resident alien telluride
Resident alien telluride Resident and family engagement
Resident and family engagement Resident and family engagement
Resident and family engagement Ota core curriculum
Ota core curriculum Acgme survey
Acgme survey Ota core curriculum
Ota core curriculum Detroit shock initiative
Detroit shock initiative Prsa detroit
Prsa detroit Pelvimetrie interne
Pelvimetrie interne Detroit atd
Detroit atd Detroit development fund
Detroit development fund Detroit shock initiative
Detroit shock initiative Detroit sister city
Detroit sister city Cpa building
Cpa building Detroit convention bureau
Detroit convention bureau Building the engine of community development in detroit
Building the engine of community development in detroit Segment de tore
Segment de tore