Cardiovascular outcomes trials with GLP1 receptor agonists EDUCATIONAL

- Slides: 42
Cardiovascular outcomes trials with GLP-1 receptor agonists EDUCATIONAL SLIDE MODULE Date of preparation: January 2020 Version 4. 0 SC-CRP-03320
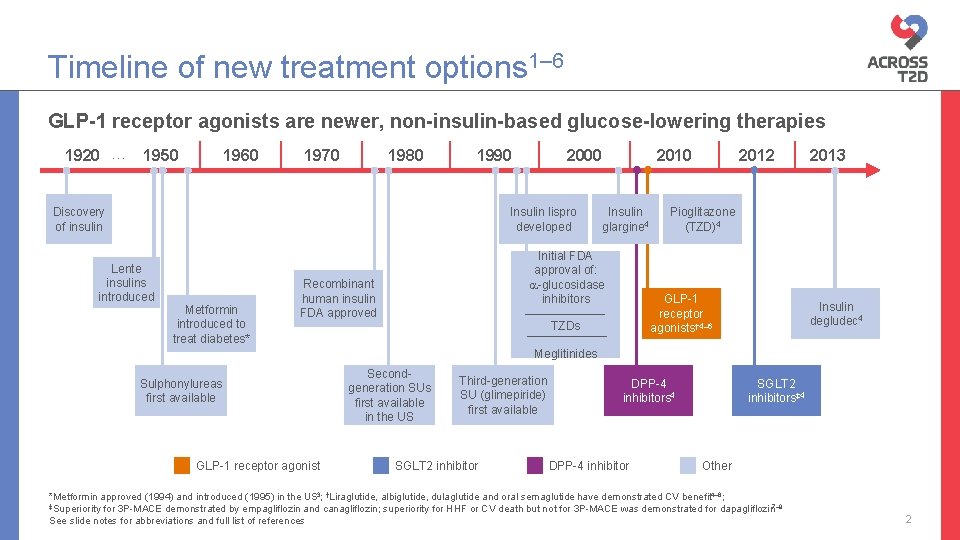
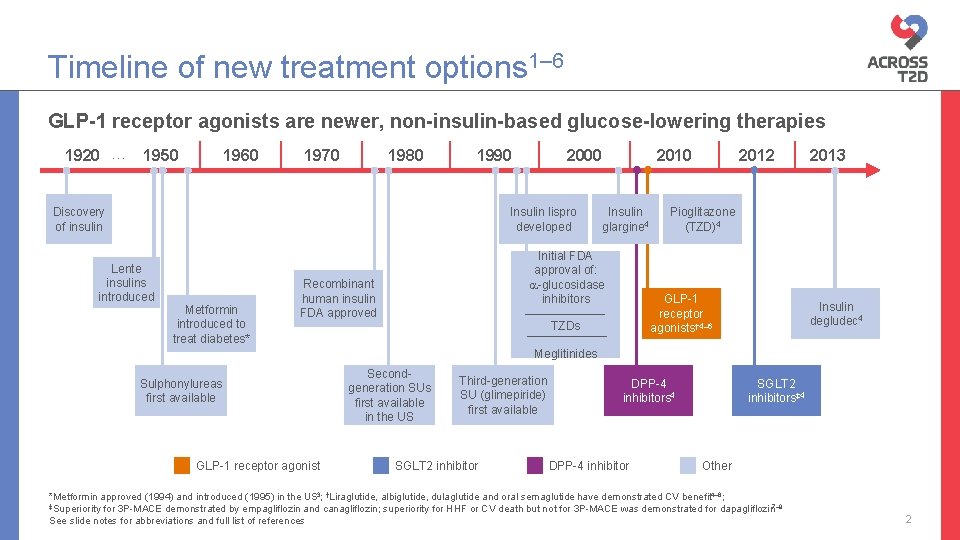
Timeline of new treatment options 1– 6 GLP-1 receptor agonists are newer, non-insulin-based glucose-lowering therapies 1920 … 1950 1960 1970 1980 1990 Discovery of insulin 2000 Insulin lispro developed Lente insulins introduced Metformin introduced to treat diabetes* 2010 Insulin glargine 4 Initial FDA approval of: -glucosidase inhibitors Recombinant human insulin FDA approved 2012 Pioglitazone (TZD)4 GLP-1 receptor agonists† 4– 6 TZDs 2013 Insulin degludec 4 Meglitinides Sulphonylureas first available GLP-1 receptor agonist Secondgeneration SUs first available in the US Third-generation SU (glimepiride) first available SGLT 2 inhibitor DPP-4 inhibitors 4 DPP-4 inhibitor SGLT 2 inhibitors‡ 4 Other *Metformin approved (1994) and introduced (1995) in the US 3; †Liraglutide, albiglutide, dulaglutide and oral semaglutide have demonstrated CV benefit 4– 6; ‡Superiority for 3 P-MACE demonstrated by empagliflozin and canagliflozin; superiority for HHF or CV death but not for 3 P-MACE was demonstrated for dapagliflozin 7– 9 See slide notes for abbreviations and full list of references 2
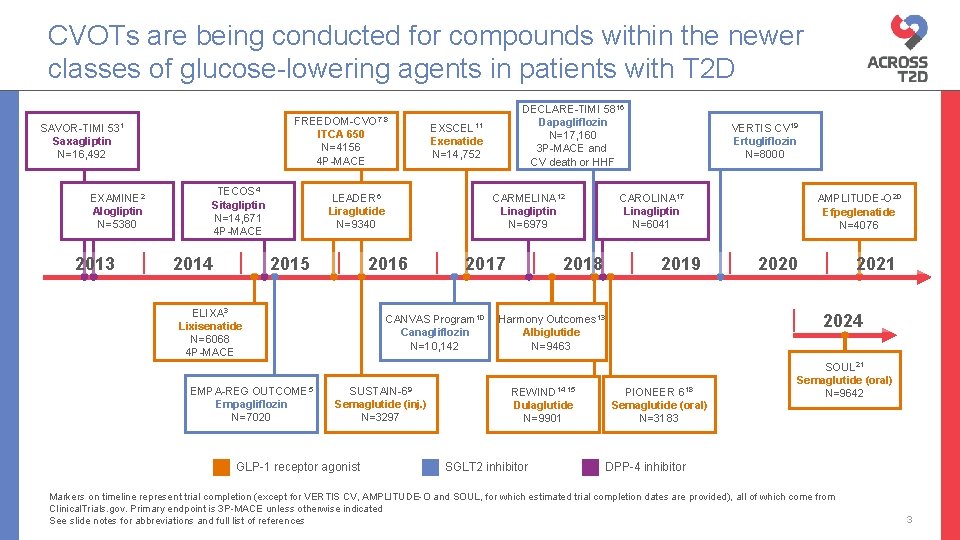
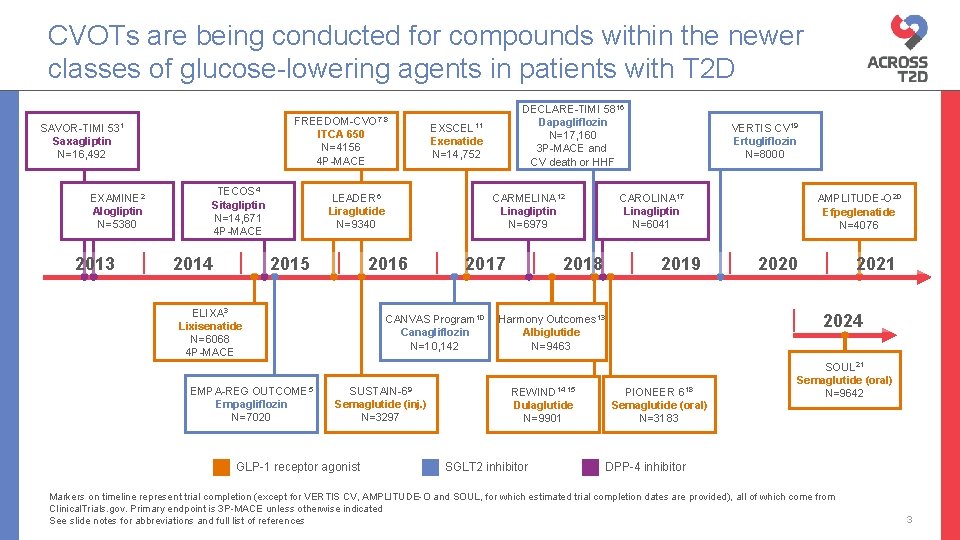
CVOTs are being conducted for compounds within the newer classes of glucose-lowering agents in patients with T 2 D FREEDOM-CVO 7, 8 SAVOR-TIMI 531 Saxagliptin N=16, 492 EXAMINE 2 Alogliptin N=5380 2013 ITCA 650 N=4156 4 P-MACE TECOS 4 Sitagliptin N=14, 671 4 P-MACE 2014 EXSCEL 11 Exenatide N=14, 752 LEADER 6 Liraglutide N=9340 2015 EMPA-REG OUTCOME 5 Empagliflozin N=7020 CARMELINA 12 Linagliptin N=6979 2016 ELIXA 3 Lixisenatide N=6068 4 P-MACE 2017 CANVAS Program 10 Canagliflozin N=10, 142 SUSTAIN-69 Semaglutide (inj. ) N=3297 GLP-1 receptor agonist DECLARE-TIMI 5816 Dapagliflozin N=17, 160 3 P-MACE and CV death or HHF 2018 VERTIS CV 19 Ertugliflozin N=8000 CAROLINA 17 Linagliptin N=6041 2019 SGLT 2 inhibitor 2020 2021 2024 Harmony Outcomes 13 Albiglutide N=9463 REWIND 14, 15 Dulaglutide N=9901 AMPLITUDE-O 20 Efpeglenatide N=4076 PIONEER 618 Semaglutide (oral) N=3183 SOUL 21 Semaglutide (oral) N=9642 DPP-4 inhibitor Markers on timeline represent trial completion (except for VERTIS CV, AMPLITUDE-O and SOUL, for which estimated trial completion dates are provided), all of which come from Clinical. Trials. gov. Primary endpoint is 3 P-MACE unless otherwise indicated See slide notes for abbreviations and full list of references 3
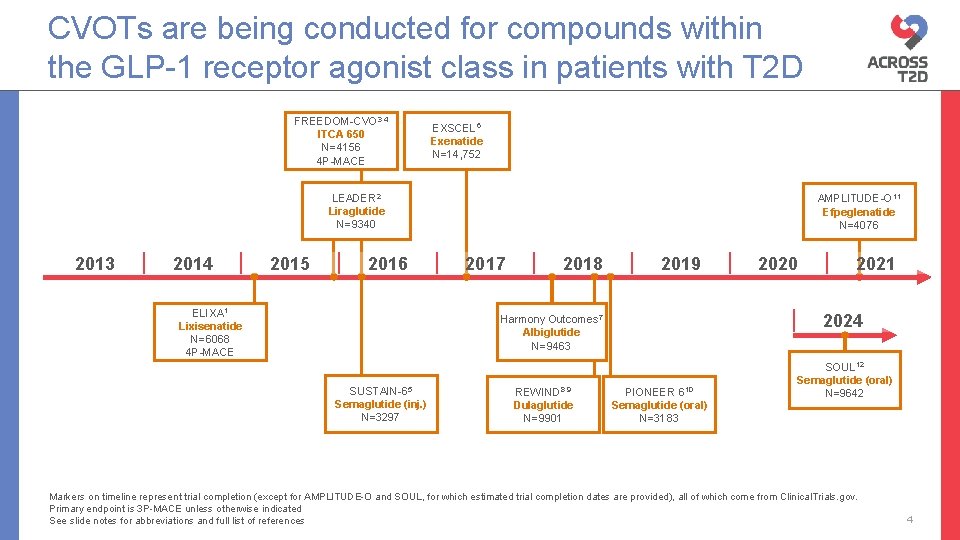
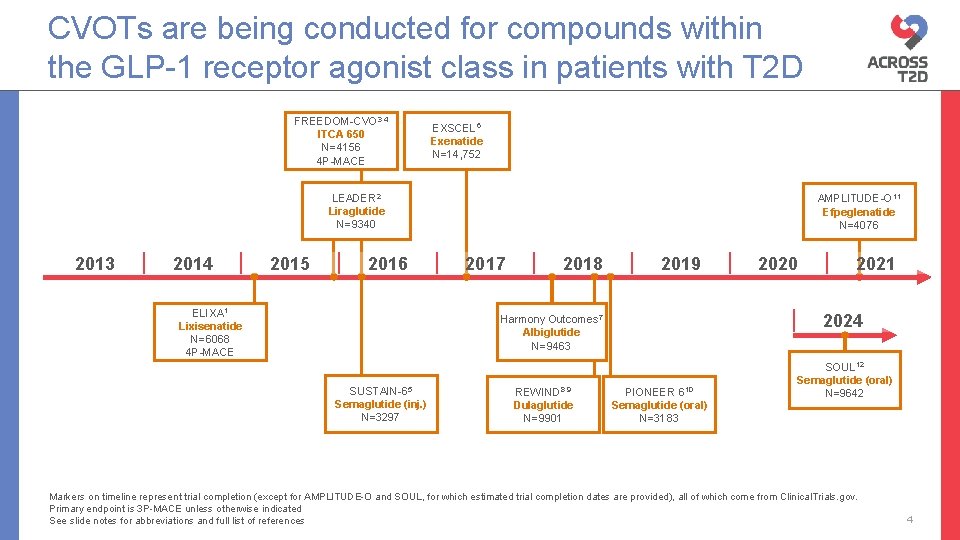
CVOTs are being conducted for compounds within the GLP-1 receptor agonist class in patients with T 2 D FREEDOM-CVO 3, 4 ITCA 650 N=4156 4 P-MACE EXSCEL 6 Exenatide N=14, 752 LEADER 2 Liraglutide N=9340 2013 2014 2015 2016 ELIXA 1 Lixisenatide N=6068 4 P-MACE AMPLITUDE-O 11 Efpeglenatide N=4076 2017 2018 2019 REWIND 8, 9 Dulaglutide N=9901 2024 Harmony Outcomes 7 Albiglutide N=9463 SUSTAIN-65 Semaglutide (inj. ) N=3297 2020 PIONEER 610 Semaglutide (oral) N=3183 SOUL 12 Semaglutide (oral) N=9642 Markers on timeline represent trial completion (except for AMPLITUDE-O and SOUL, for which estimated trial completion dates are provided), all of which come from Clinical. Trials. gov. Primary endpoint is 3 P-MACE unless otherwise indicated See slide notes for abbreviations and full list of references 4
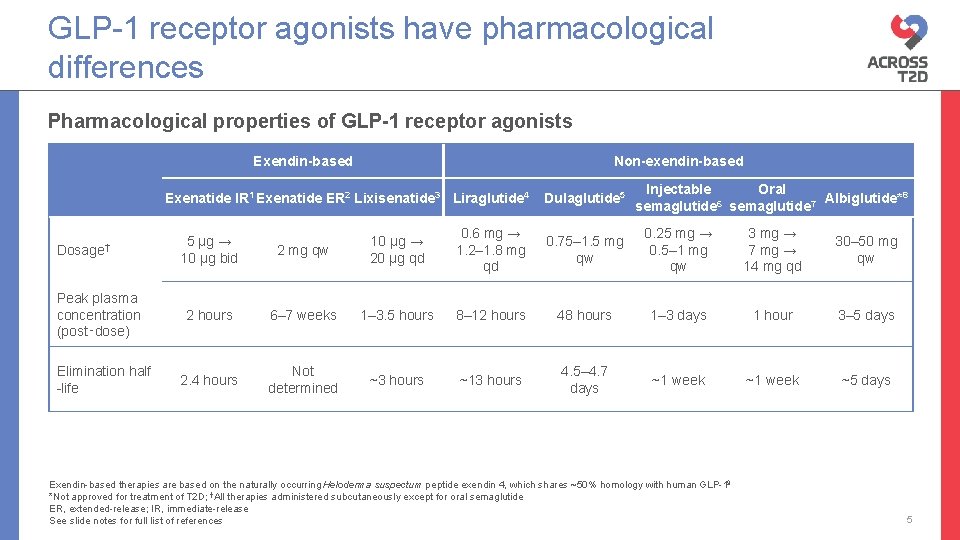
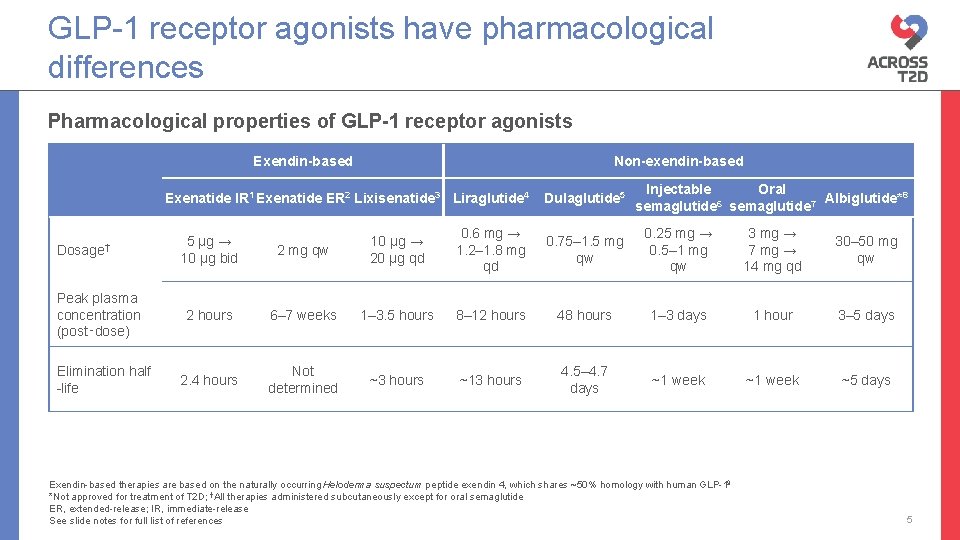
GLP-1 receptor agonists have pharmacological differences Pharmacological properties of GLP-1 receptor agonists Exendin-based Dosage† Peak plasma concentration (post‑dose) Elimination half -life Non-exendin-based Injectable Oral Albiglutide*8 6 semaglutide 7 Exenatide IR 1 Exenatide ER 2 Lixisenatide 3 Liraglutide 4 Dulaglutide 5 0. 6 mg → 1. 2– 1. 8 mg qd 0. 75– 1. 5 mg qw 0. 25 mg → 0. 5– 1 mg qw 3 mg → 7 mg → 14 mg qd 30– 50 mg qw 5 µg → 10 µg bid 2 mg qw 10 µg → 20 µg qd 2 hours 6– 7 weeks 1– 3. 5 hours 8– 12 hours 48 hours 1– 3 days 1 hour 3– 5 days 2. 4 hours Not determined ~3 hours ~13 hours 4. 5– 4. 7 days ~1 week ~5 days Exendin-based therapies are based on the naturally occurring Heloderma suspectum peptide exendin 4, which shares ~50% homology with human GLP-19 *Not approved for treatment of T 2 D; †All therapies administered subcutaneously except for oral semaglutide ER, extended-release; IR, immediate-release See slide notes for full list of references 5
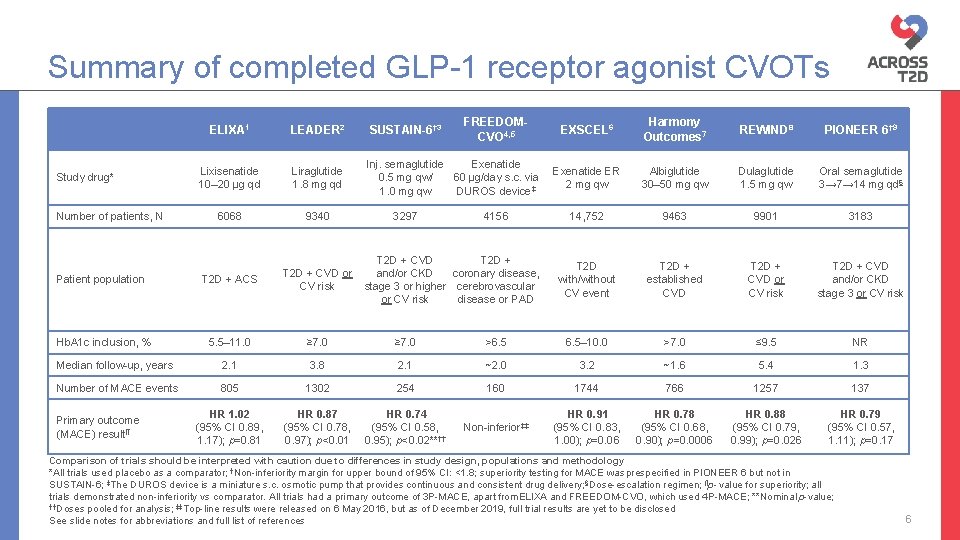
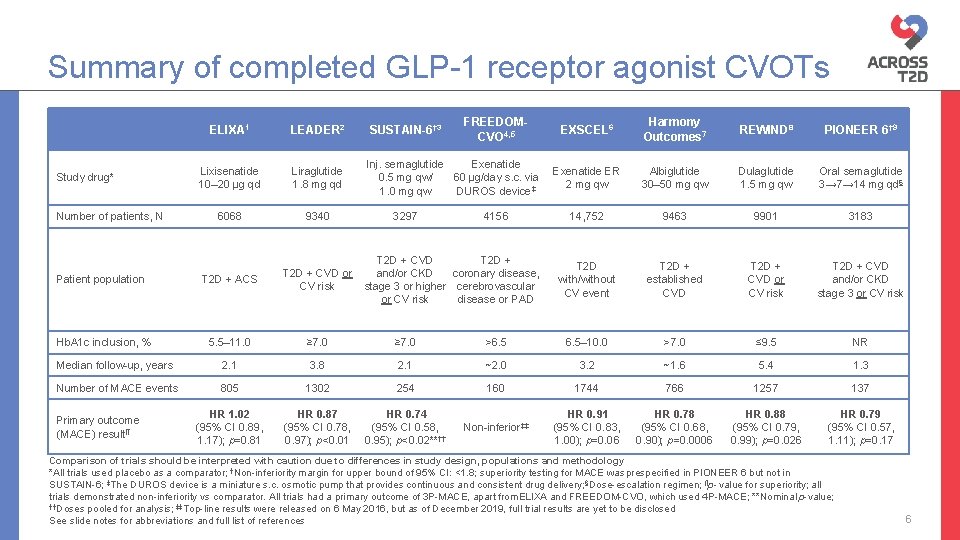
Summary of completed GLP-1 receptor agonist CVOTs Study drug* Number of patients, N FREEDOMCVO 4, 5 ELIXA 1 LEADER 2 SUSTAIN-6† 3 Lixisenatide 10– 20 µg qd Liraglutide 1. 8 mg qd Inj. semaglutide Exenatide 0. 5 mg qw/ 60 µg/day s. c. via 1. 0 mg qw DUROS device‡ 6068 9340 3297 4156 T 2 D + CVD T 2 D + and/or CKD coronary disease, stage 3 or higher cerebrovascular or CV risk disease or PAD EXSCEL 6 Harmony Outcomes 7 REWIND 8 PIONEER 6† 9 Exenatide ER 2 mg qw Albiglutide 30– 50 mg qw Dulaglutide 1. 5 mg qw Oral semaglutide 3→ 7→ 14 mg qd§ 14, 752 9463 9901 3183 T 2 D with/without CV event T 2 D + established CVD T 2 D + CVD or CV risk T 2 D + CVD and/or CKD stage 3 or CV risk T 2 D + ACS T 2 D + CVD or CV risk 5. 5– 11. 0 ≥ 7. 0 >6. 5– 10. 0 >7. 0 ≤ 9. 5 NR Median follow-up, years 2. 1 3. 8 2. 1 ~2. 0 3. 2 ~1. 6 5. 4 1. 3 Number of MACE events 805 1302 254 160 1744 766 1257 137 HR 1. 02 (95% CI 0. 89, 1. 17); p=0. 81 HR 0. 87 (95% CI 0. 78, 0. 97); p<0. 01 HR 0. 74 (95% CI 0. 58, 0. 95); p<0. 02**†† Non-inferior‡‡ HR 0. 91 (95% CI 0. 83, 1. 00); p=0. 06 HR 0. 78 (95% CI 0. 68, 0. 90); p=0. 0006 HR 0. 88 (95% CI 0. 79, 0. 99); p=0. 026 HR 0. 79 (95% CI 0. 57, 1. 11); p=0. 17 Patient population Hb. A 1 c inclusion, % Primary outcome (MACE) result¶ Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *All trials used placebo as a comparator; †Non-inferiority margin for upper bound of 95% CI: <1. 8; superiority testing for MACE was prespecified in PIONEER 6 but not in SUSTAIN-6; ‡The DUROS device is a miniature s. c. osmotic pump that provides continuous and consistent drug delivery; §Dose-escalation regimen; ¶p- value for superiority; all trials demonstrated non-inferiority vs comparator. All trials had a primary outcome of 3 P-MACE, apart from. ELIXA and FREEDOM-CVO, which used 4 P-MACE; **Nominal p-value; ††Doses pooled for analysis; ‡‡Top-line results were released on 6 May 2016, but as of December 2019, full trial results are yet to be disclosed See slide notes for abbreviations and full list of references 6
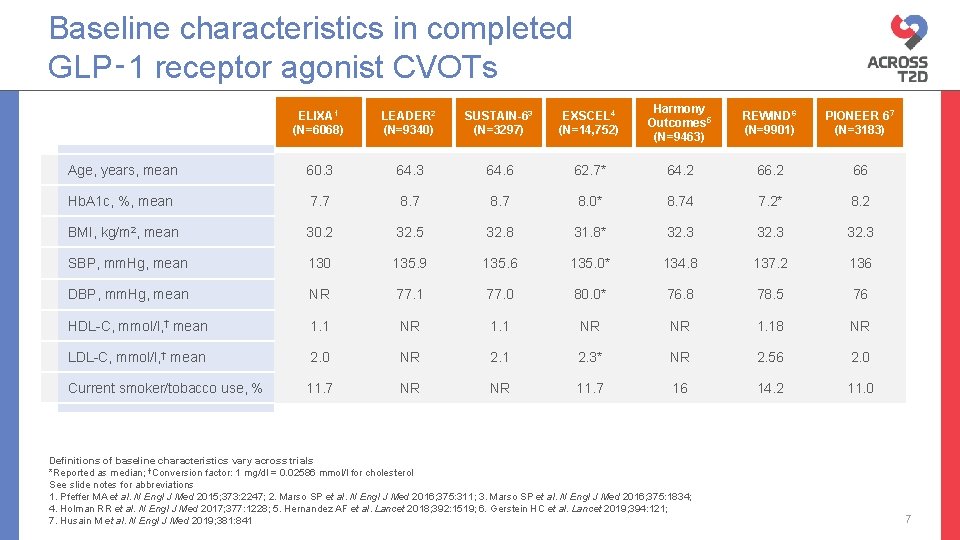
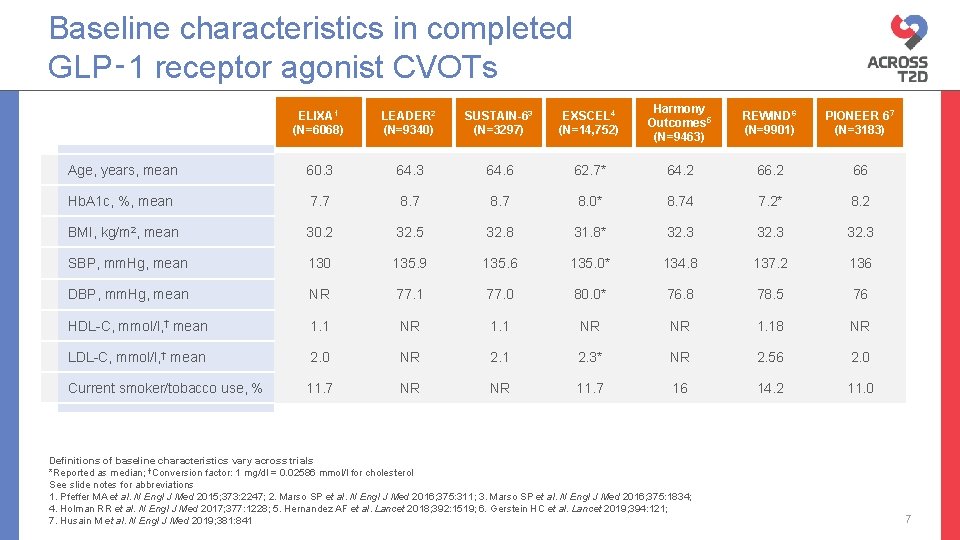
Baseline characteristics in completed GLP‑ 1 receptor agonist CVOTs ELIXA 1 (N=6068) LEADER 2 (N=9340) SUSTAIN-63 (N=3297) EXSCEL 4 (N=14, 752) Harmony Outcomes 5 (N=9463) REWIND 6 (N=9901) PIONEER 67 (N=3183) Age, years, mean 60. 3 64. 6 62. 7* 64. 2 66 Hb. A 1 c, %, mean 7. 7 8. 0* 8. 74 7. 2* 8. 2 BMI, kg/m 2, mean 30. 2 32. 5 32. 8 31. 8* 32. 3 SBP, mm. Hg, mean 130 135. 9 135. 6 135. 0* 134. 8 137. 2 136 DBP, mm. Hg, mean NR 77. 1 77. 0 80. 0* 76. 8 78. 5 76 HDL-C, mmol/l, † mean 1. 1 NR NR 1. 18 NR LDL-C, mmol/l, † mean 2. 0 NR 2. 1 2. 3* NR 2. 56 2. 0 Current smoker/tobacco use, % 11. 7 NR NR 11. 7 16 14. 2 11. 0 Definitions of baseline characteristics vary across trials *Reported as median; †Conversion factor: 1 mg/dl = 0. 02586 mmol/l for cholesterol See slide notes for abbreviations 1. Pfeffer MA et al. N Engl J Med 2015; 373: 2247; 2. Marso SP et al. N Engl J Med 2016; 375: 311; 3. Marso SP et al. N Engl J Med 2016; 375: 1834; 4. Holman RR et al. N Engl J Med 2017; 377: 1228; 5. Hernandez AF et al. Lancet 2018; 392: 1519; 6. Gerstein HC et al. Lancet 2019; 394: 121; 7. Husain M et al. N Engl J Med 2019; 381: 841 7
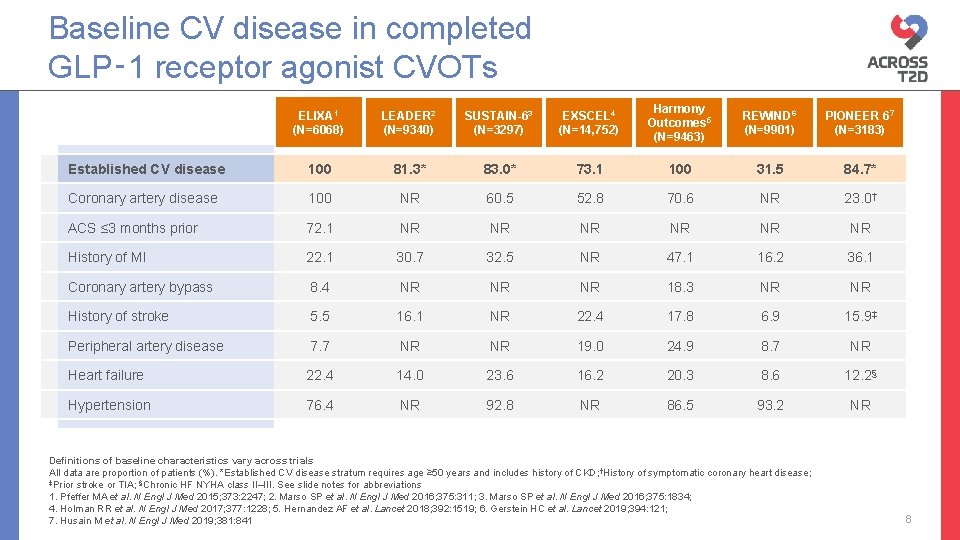
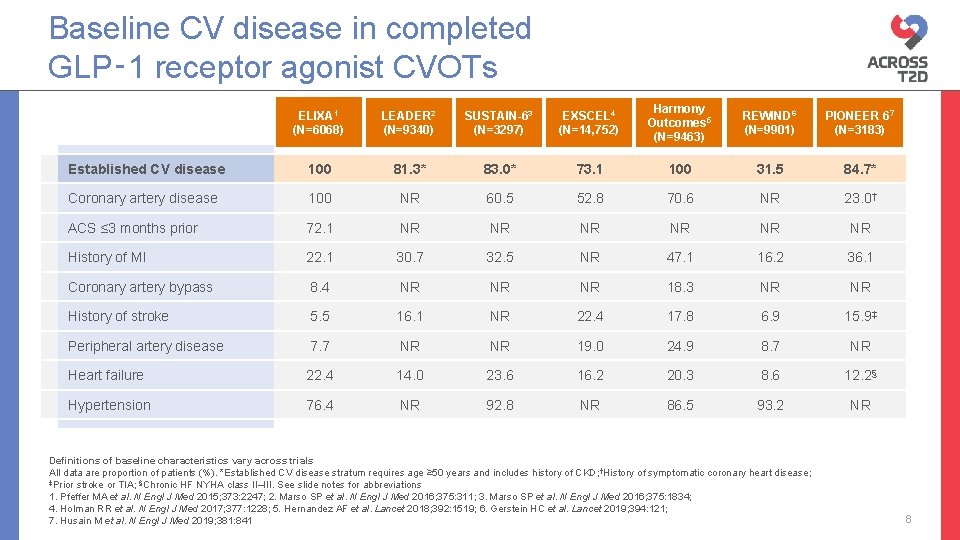
Baseline CV disease in completed GLP‑ 1 receptor agonist CVOTs ELIXA 1 (N=6068) LEADER 2 (N=9340) SUSTAIN-63 (N=3297) EXSCEL 4 (N=14, 752) Harmony Outcomes 5 (N=9463) REWIND 6 (N=9901) PIONEER 67 (N=3183) Established CV disease 100 81. 3* 83. 0* 73. 1 100 31. 5 84. 7* Coronary artery disease 100 NR 60. 5 52. 8 70. 6 NR 23. 0† ACS ≤ 3 months prior 72. 1 NR NR NR History of MI 22. 1 30. 7 32. 5 NR 47. 1 16. 2 36. 1 Coronary artery bypass 8. 4 NR NR NR 18. 3 NR NR History of stroke 5. 5 16. 1 NR 22. 4 17. 8 6. 9 15. 9‡ Peripheral artery disease 7. 7 NR NR 19. 0 24. 9 8. 7 NR Heart failure 22. 4 14. 0 23. 6 16. 2 20. 3 8. 6 12. 2§ Hypertension 76. 4 NR 92. 8 NR 86. 5 93. 2 NR Definitions of baseline characteristics vary across trials All data are proportion of patients (%). *Established CV disease stratum requires age ≥ 50 years and includes history of CKD; †History of symptomatic coronary heart disease; ‡Prior stroke or TIA; §Chronic HF NYHA class II–III. See slide notes for abbreviations 1. Pfeffer MA et al. N Engl J Med 2015; 373: 2247; 2. Marso SP et al. N Engl J Med 2016; 375: 311; 3. Marso SP et al. N Engl J Med 2016; 375: 1834; 4. Holman RR et al. N Engl J Med 2017; 377: 1228; 5. Hernandez AF et al. Lancet 2018; 392: 1519; 6. Gerstein HC et al. Lancet 2019; 394: 121; 7. Husain M et al. N Engl J Med 2019; 381: 841 8
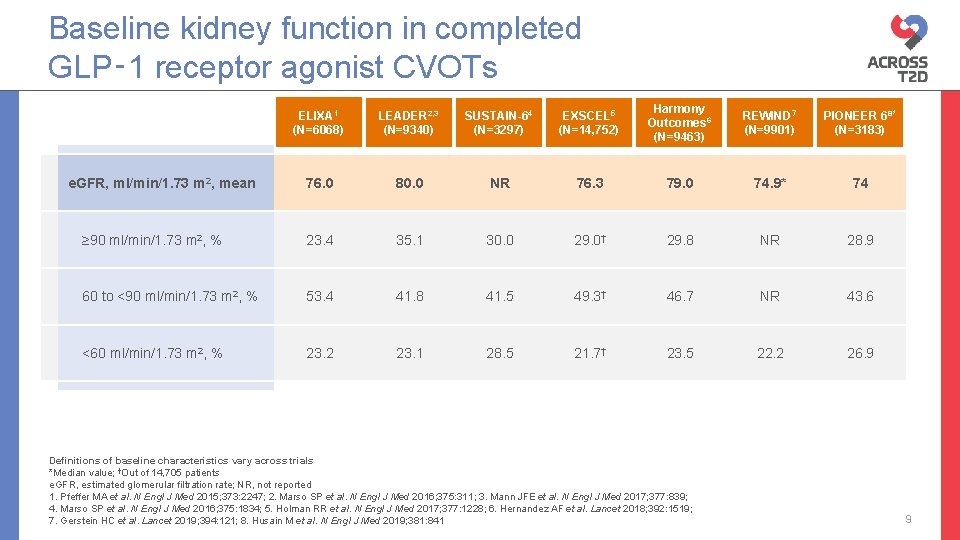
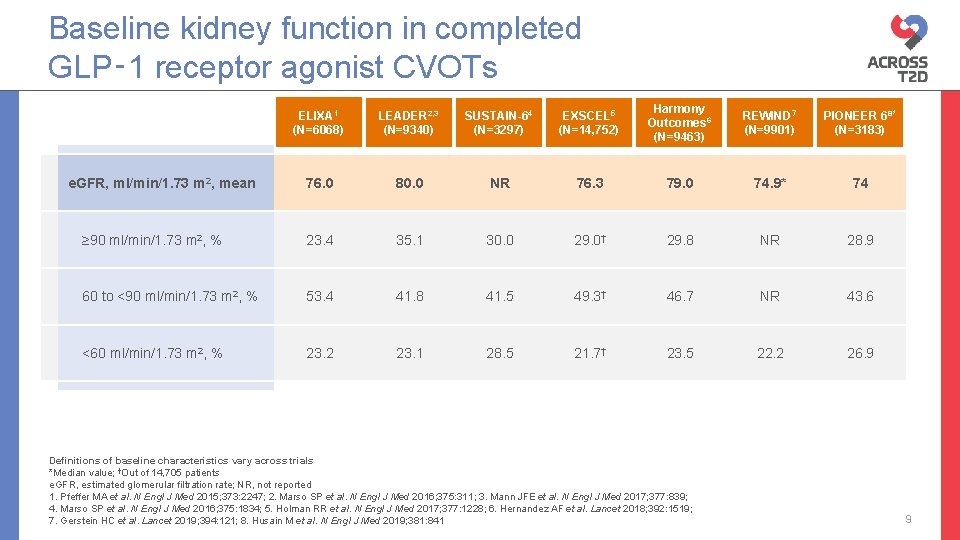
Baseline kidney function in completed GLP‑ 1 receptor agonist CVOTs ELIXA 1 (N=6068) LEADER 2, 3 (N=9340) SUSTAIN-64 (N=3297) EXSCEL 5 (N=14, 752) Harmony Outcomes 6 (N=9463) REWIND 7 (N=9901) PIONEER 68* (N=3183) 76. 0 80. 0 NR 76. 3 79. 0 74. 9* 74 ≥ 90 ml/min/1. 73 m 2, % 23. 4 35. 1 30. 0 29. 0† 29. 8 NR 28. 9 60 to <90 ml/min/1. 73 m 2, % 53. 4 41. 8 41. 5 49. 3† 46. 7 NR 43. 6 <60 ml/min/1. 73 m 2, % 23. 2 23. 1 28. 5 21. 7† 23. 5 22. 2 26. 9 e. GFR, ml/min/1. 73 m 2, mean Definitions of baseline characteristics vary across trials *Median value; †Out of 14, 705 patients e. GFR, estimated glomerular filtration rate; NR, not reported 1. Pfeffer MA et al. N Engl J Med 2015; 373: 2247; 2. Marso SP et al. N Engl J Med 2016; 375: 311; 3. Mann JFE et al. N Engl J Med 2017; 377: 839; 4. Marso SP et al. N Engl J Med 2016; 375: 1834; 5. Holman RR et al. N Engl J Med 2017; 377: 1228; 6. Hernandez AF et al. Lancet 2018; 392: 1519; 7. Gerstein HC et al. Lancet 2019; 394: 121; 8. Husain M et al. N Engl J Med 2019; 381: 841 9
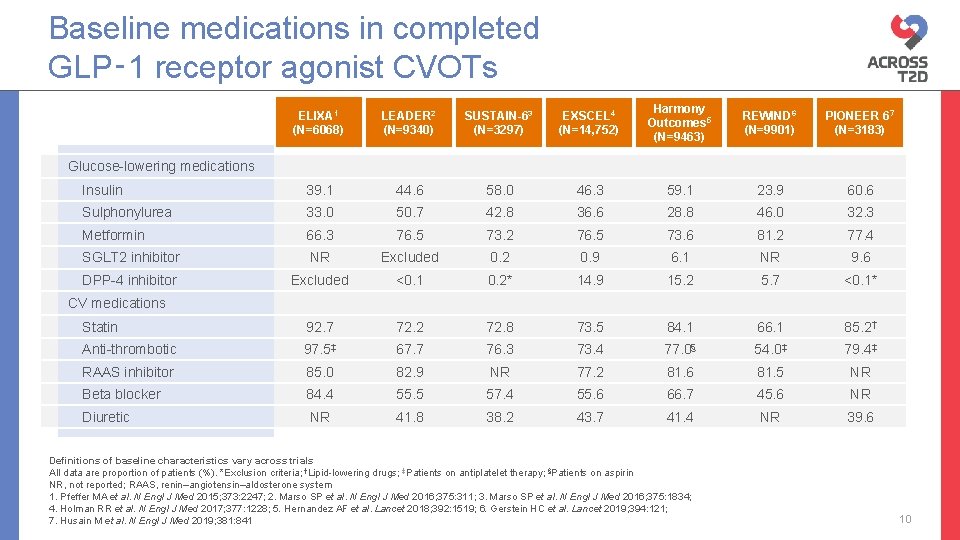
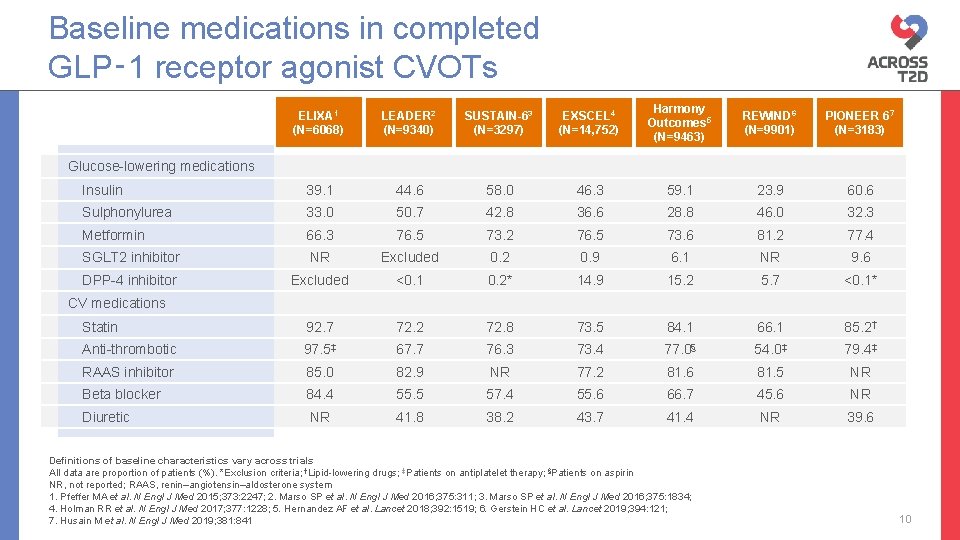
Baseline medications in completed GLP‑ 1 receptor agonist CVOTs ELIXA 1 (N=6068) LEADER 2 (N=9340) SUSTAIN-63 (N=3297) EXSCEL 4 (N=14, 752) Harmony Outcomes 5 (N=9463) REWIND 6 (N=9901) PIONEER 67 (N=3183) Insulin 39. 1 44. 6 58. 0 46. 3 59. 1 23. 9 60. 6 Sulphonylurea 33. 0 50. 7 42. 8 36. 6 28. 8 46. 0 32. 3 Metformin 66. 3 76. 5 73. 2 76. 5 73. 6 81. 2 77. 4 SGLT 2 inhibitor NR Excluded 0. 2 0. 9 6. 1 NR 9. 6 DPP-4 inhibitor Excluded <0. 1 0. 2* 14. 9 15. 2 5. 7 <0. 1* Statin 92. 7 72. 2 72. 8 73. 5 84. 1 66. 1 85. 2† Anti-thrombotic 97. 5‡ 67. 7 76. 3 73. 4 77. 0§ 54. 0‡ 79. 4‡ RAAS inhibitor 85. 0 82. 9 NR 77. 2 81. 6 81. 5 NR Beta blocker 84. 4 55. 5 57. 4 55. 6 66. 7 45. 6 NR Diuretic NR 41. 8 38. 2 43. 7 41. 4 NR 39. 6 Glucose-lowering medications CV medications Definitions of baseline characteristics vary across trials All data are proportion of patients (%). *Exclusion criteria; †Lipid-lowering drugs; ‡Patients on antiplatelet therapy; §Patients on aspirin NR, not reported; RAAS, renin–angiotensin–aldosterone system 1. Pfeffer MA et al. N Engl J Med 2015; 373: 2247; 2. Marso SP et al. N Engl J Med 2016; 375: 311; 3. Marso SP et al. N Engl J Med 2016; 375: 1834; 4. Holman RR et al. N Engl J Med 2017; 377: 1228; 5. Hernandez AF et al. Lancet 2018; 392: 1519; 6. Gerstein HC et al. Lancet 2019; 394: 121; 7. Husain M et al. N Engl J Med 2019; 381: 841 10
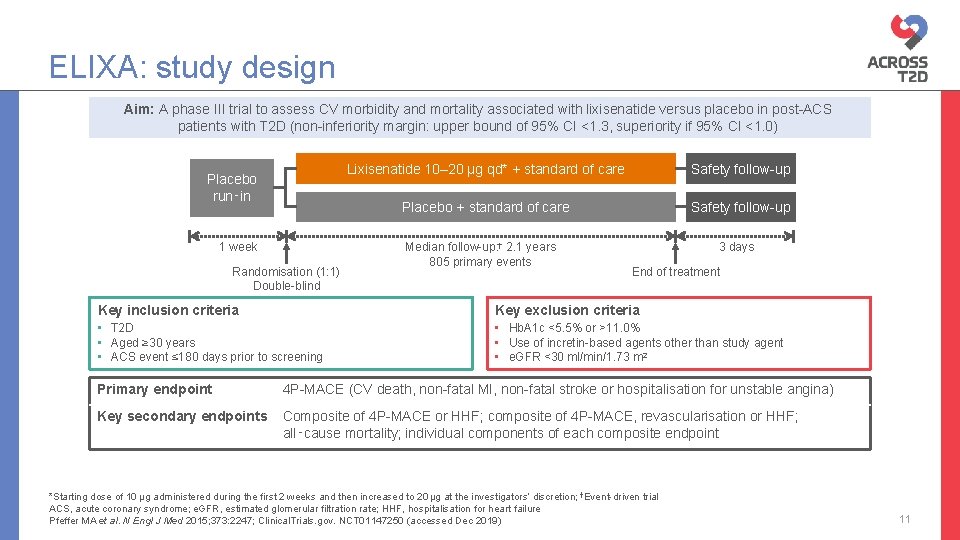
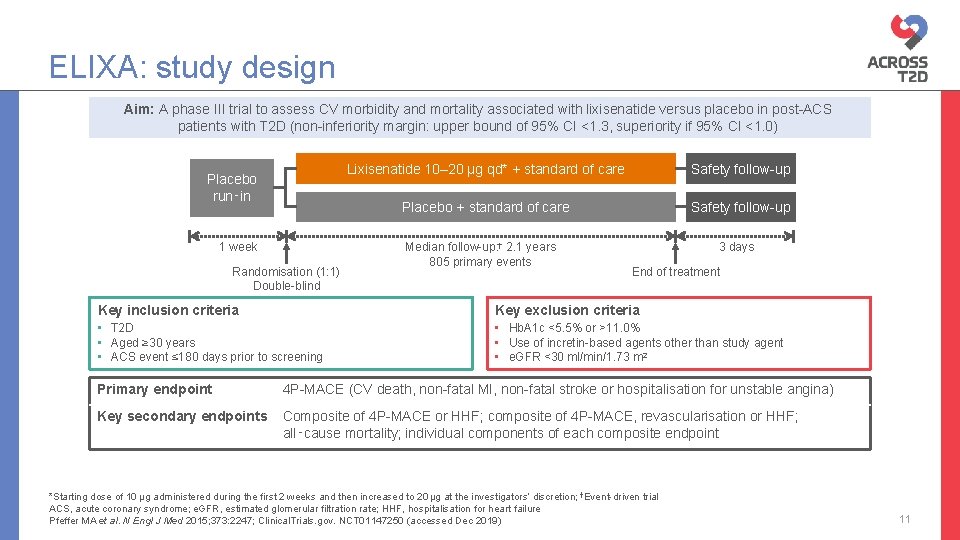
ELIXA: study design Aim: A phase III trial to assess CV morbidity and mortality associated with lixisenatide versus placebo in post-ACS patients with T 2 D (non-inferiority margin: upper bound of 95% CI <1. 3, superiority if 95% CI <1. 0) Placebo run‑in 1 week Randomisation (1: 1) Double-blind Lixisenatide 10– 20 µg qd* + standard of care Safety follow-up Placebo + standard of care Safety follow-up Median follow-up: † 2. 1 years 805 primary events 3 days End of treatment Key inclusion criteria Key exclusion criteria • T 2 D • Aged ≥ 30 years • ACS event ≤ 180 days prior to screening • Hb. A 1 c <5. 5% or >11. 0% • Use of incretin-based agents other than study agent • e. GFR <30 ml/min/1. 73 m 2 Primary endpoint 4 P-MACE (CV death, non-fatal MI, non-fatal stroke or hospitalisation for unstable angina) Key secondary endpoints Composite of 4 P-MACE or HHF; composite of 4 P-MACE, revascularisation or HHF; all‑cause mortality; individual components of each composite endpoint *Starting dose of 10 μg administered during the first 2 weeks and then increased to 20 μg at the investigators’ discretion; †Event-driven trial ACS, acute coronary syndrome; e. GFR, estimated glomerular filtration rate; HHF, hospitalisation for heart failure Pfeffer MA et al. N Engl J Med 2015; 373: 2247; Clinical. Trials. gov. NCT 01147250 (accessed Dec 2019) 11
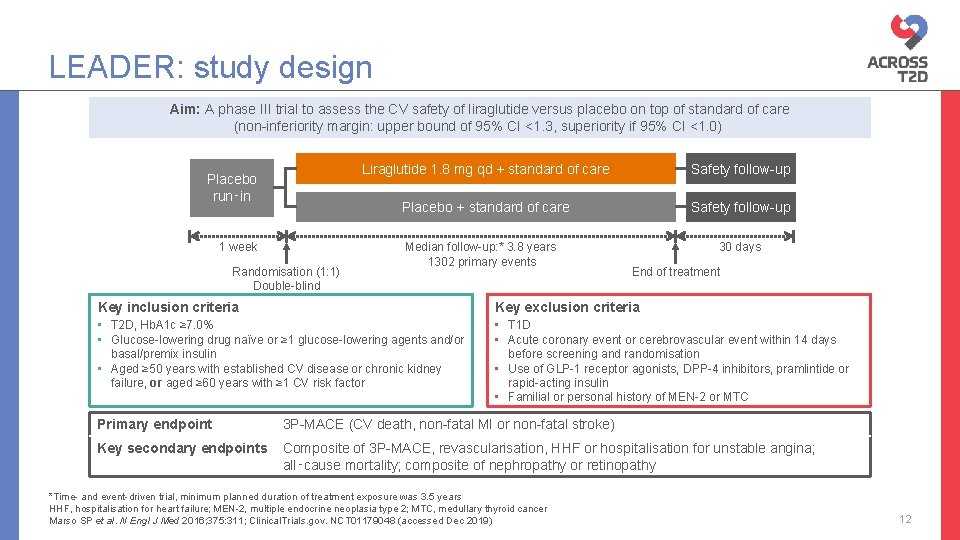
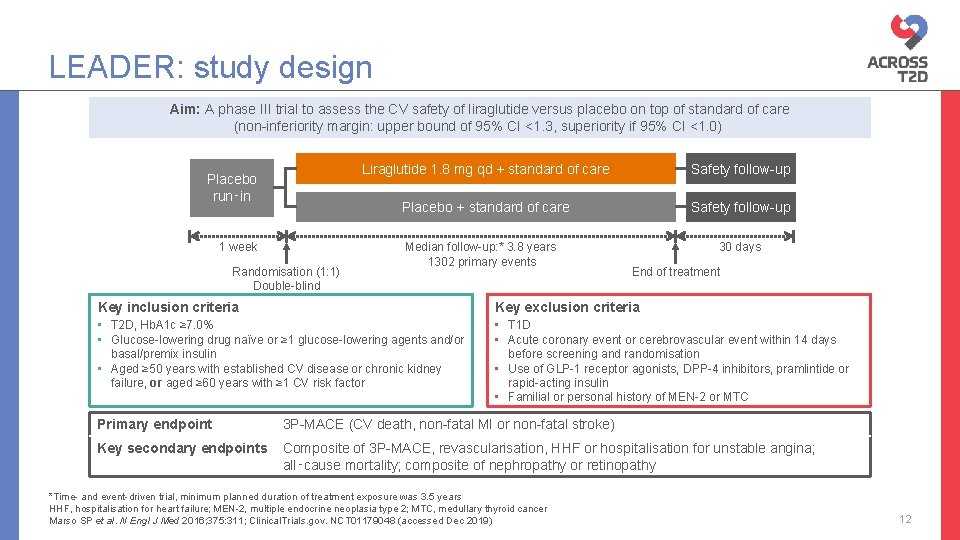
LEADER: study design Aim: A phase III trial to assess the CV safety of liraglutide versus placebo on top of standard of care (non-inferiority margin: upper bound of 95% CI <1. 3, superiority if 95% CI <1. 0) Placebo run‑in 1 week Randomisation (1: 1) Double-blind Liraglutide 1. 8 mg qd + standard of care Safety follow-up Placebo + standard of care Safety follow-up Median follow-up: * 3. 8 years 1302 primary events 30 days End of treatment Key inclusion criteria Key exclusion criteria • T 2 D, Hb. A 1 c ≥ 7. 0% • Glucose-lowering drug naïve or ≥ 1 glucose-lowering agents and/or basal/premix insulin • Aged ≥ 50 years with established CV disease or chronic kidney failure, or aged ≥ 60 years with ≥ 1 CV risk factor • T 1 D • Acute coronary event or cerebrovascular event within 14 days before screening and randomisation • Use of GLP-1 receptor agonists, DPP-4 inhibitors, pramlintide or rapid-acting insulin • Familial or personal history of MEN-2 or MTC Primary endpoint 3 P-MACE (CV death, non-fatal MI or non-fatal stroke) Key secondary endpoints Composite of 3 P-MACE, revascularisation, HHF or hospitalisation for unstable angina; all‑cause mortality; composite of nephropathy or retinopathy *Time- and event-driven trial, minimum planned duration of treatment exposure was 3. 5 years HHF, hospitalisation for heart failure; MEN-2, multiple endocrine neoplasia type 2; MTC, medullary thyroid cancer Marso SP et al. N Engl J Med 2016; 375: 311; Clinical. Trials. gov. NCT 01179048 (accessed Dec 2019) 12
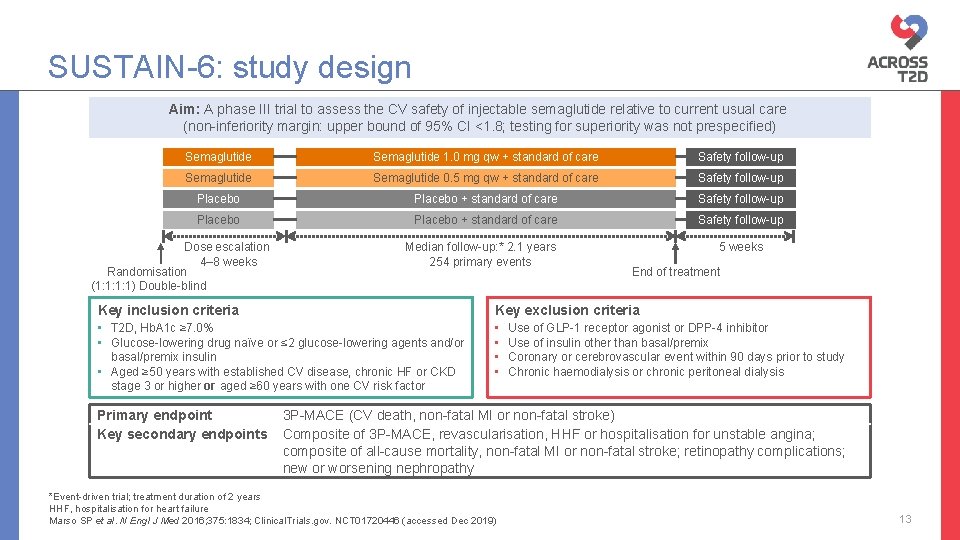
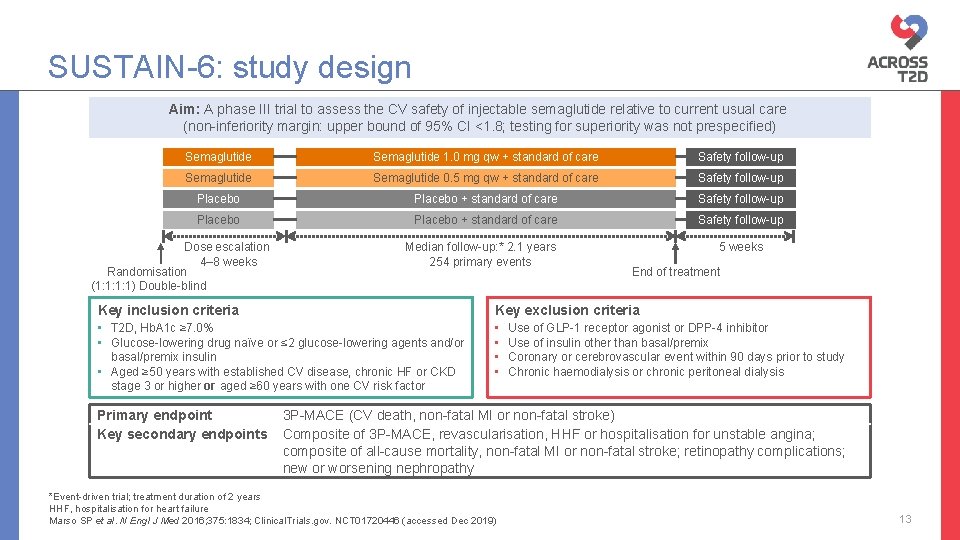
SUSTAIN-6: study design Aim: A phase III trial to assess the CV safety of injectable semaglutide relative to current usual care (non-inferiority margin: upper bound of 95% CI <1. 8; testing for superiority was not prespecified) Semaglutide 1. 0 mg qw + standard of care Safety follow-up Semaglutide 0. 5 mg qw + standard of care Safety follow-up Placebo + standard of care Safety follow-up Dose escalation 4– 8 weeks Randomisation (1: 1: 1: 1) Double-blind Median follow-up: * 2. 1 years 254 primary events 5 weeks End of treatment Key inclusion criteria Key exclusion criteria • T 2 D, Hb. A 1 c ≥ 7. 0% • Glucose-lowering drug naïve or ≤ 2 glucose-lowering agents and/or basal/premix insulin • Aged ≥ 50 years with established CV disease, chronic HF or CKD stage 3 or higher or aged ≥ 60 years with one CV risk factor • • Primary endpoint Key secondary endpoints Use of GLP-1 receptor agonist or DPP-4 inhibitor Use of insulin other than basal/premix Coronary or cerebrovascular event within 90 days prior to study Chronic haemodialysis or chronic peritoneal dialysis 3 P-MACE (CV death, non-fatal MI or non-fatal stroke) Composite of 3 P-MACE, revascularisation, HHF or hospitalisation for unstable angina; composite of all-cause mortality, non-fatal MI or non-fatal stroke; retinopathy complications; new or worsening nephropathy *Event-driven trial; treatment duration of 2 years HHF, hospitalisation for heart failure Marso SP et al. N Engl J Med 2016; 375: 1834; Clinical. Trials. gov. NCT 01720446 (accessed Dec 2019) 13
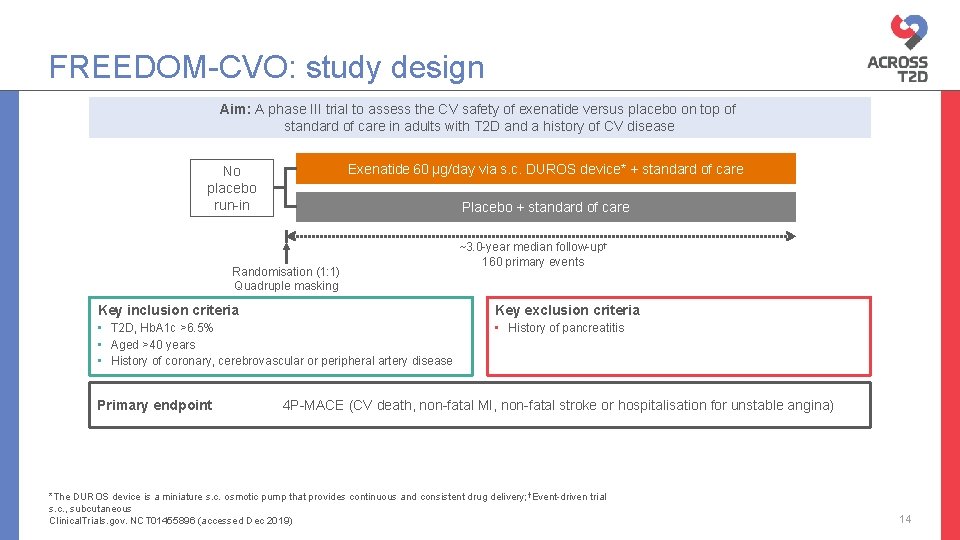
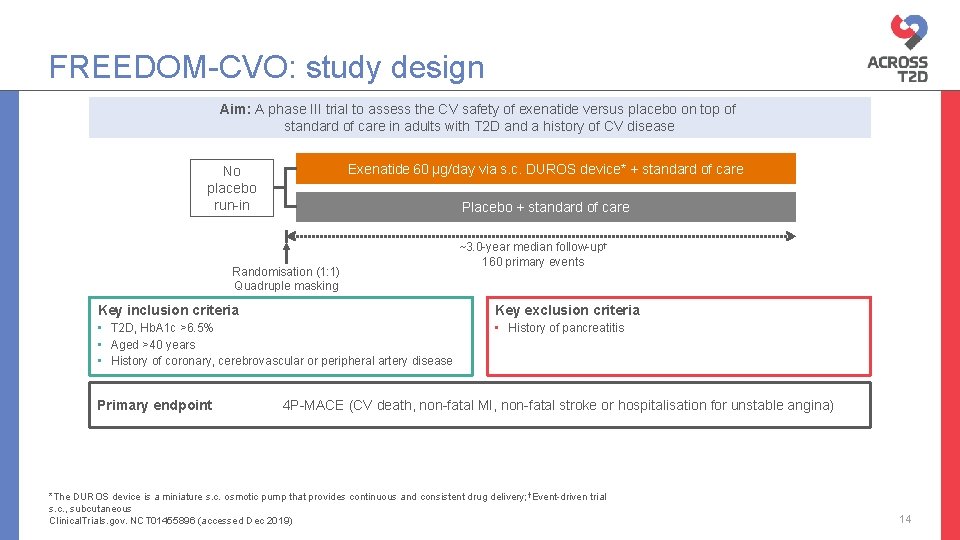
FREEDOM-CVO: study design Aim: A phase III trial to assess the CV safety of exenatide versus placebo on top of standard of care in adults with T 2 D and a history of CV disease Exenatide 60 µg/day via s. c. DUROS device* + standard of care No placebo run-in Placebo + standard of care Randomisation (1: 1) Quadruple masking ~3. 0 -year median follow-up† 160 primary events Key inclusion criteria Key exclusion criteria • T 2 D, Hb. A 1 c >6. 5% • Aged >40 years • History of coronary, cerebrovascular or peripheral artery disease • History of pancreatitis Primary endpoint 4 P-MACE (CV death, non-fatal MI, non-fatal stroke or hospitalisation for unstable angina) *The DUROS device is a miniature s. c. osmotic pump that provides continuous and consistent drug delivery; †Event-driven trial s. c. , subcutaneous Clinical. Trials. gov. NCT 01455896 (accessed Dec 2019) 14
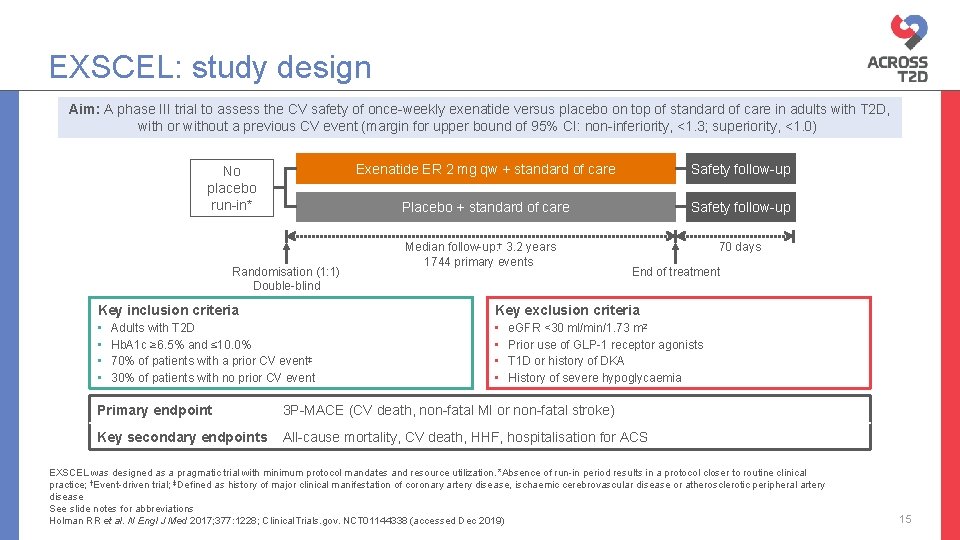
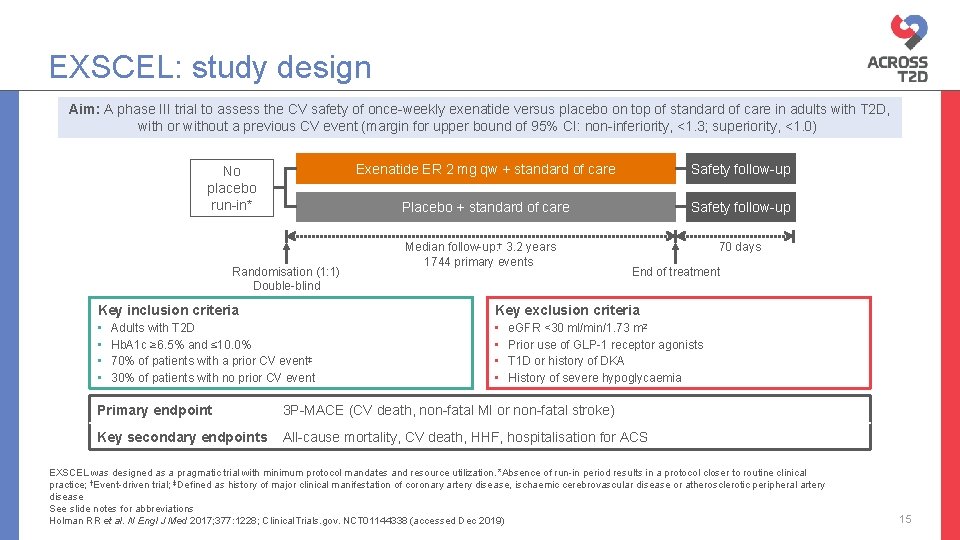
EXSCEL: study design Aim: A phase III trial to assess the CV safety of once-weekly exenatide versus placebo on top of standard of care in adults with T 2 D, with or without a previous CV event (margin for upper bound of 95% CI: non-inferiority, <1. 3; superiority, <1. 0) No placebo run-in* Randomisation (1: 1) Double-blind Exenatide ER 2 mg qw + standard of care Safety follow-up Placebo + standard of care Safety follow-up Median follow-up: † 3. 2 years 1744 primary events 70 days End of treatment Key inclusion criteria Key exclusion criteria • • Adults with T 2 D Hb. A 1 c ≥ 6. 5% and ≤ 10. 0% 70% of patients with a prior CV event‡ 30% of patients with no prior CV event e. GFR <30 ml/min/1. 73 m 2 Prior use of GLP-1 receptor agonists T 1 D or history of DKA History of severe hypoglycaemia Primary endpoint 3 P-MACE (CV death, non-fatal MI or non-fatal stroke) Key secondary endpoints All-cause mortality, CV death, HHF, hospitalisation for ACS EXSCEL was designed as a pragmatic trial with minimum protocol mandates and resource utilization. *Absence of run-in period results in a protocol closer to routine clinical practice; †Event-driven trial; ‡Defined as history of major clinical manifestation of coronary artery disease, ischaemic cerebrovascular disease or atherosclerotic peripheral artery disease See slide notes for abbreviations Holman RR et al. N Engl J Med 2017; 377: 1228; Clinical. Trials. gov. NCT 01144338 (accessed Dec 2019) 15
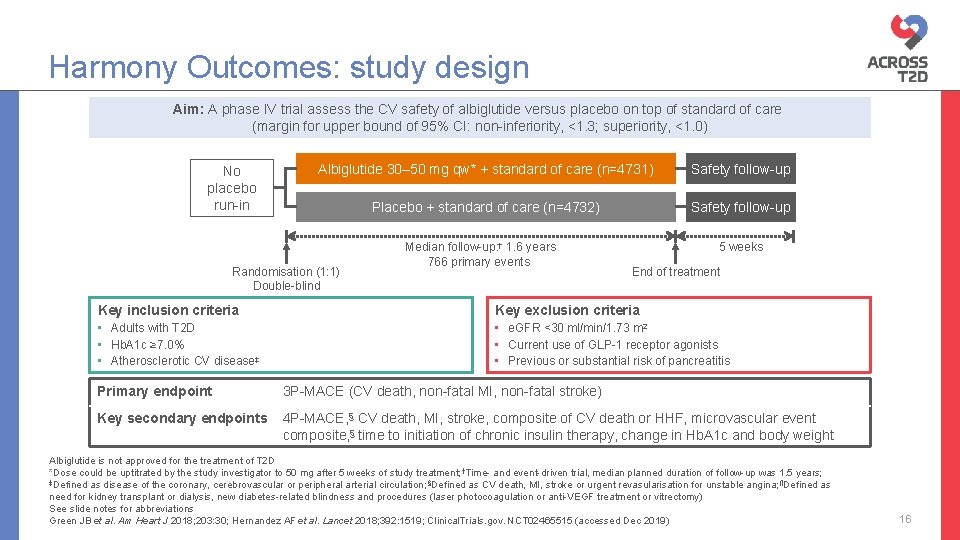
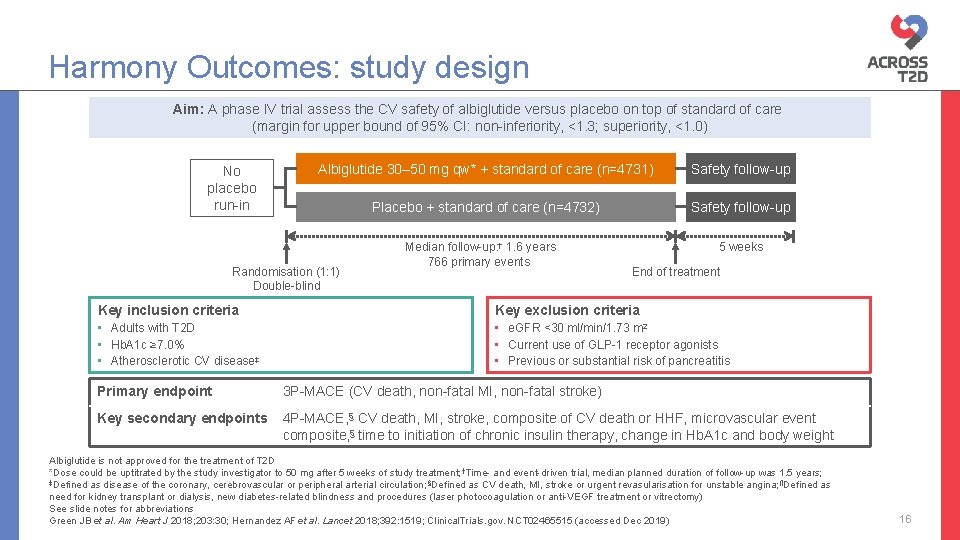
Harmony Outcomes: study design Aim: A phase IV trial assess the CV safety of albiglutide versus placebo on top of standard of care (margin for upper bound of 95% CI: non-inferiority, <1. 3; superiority, <1. 0) No placebo run-in Albiglutide 30– 50 mg qw* + standard of care (n=4731) Safety follow-up Placebo + standard of care (n=4732) Safety follow-up Randomisation (1: 1) Double-blind Median follow-up: † 1. 6 years 766 primary events 5 weeks End of treatment Key inclusion criteria Key exclusion criteria • Adults with T 2 D • Hb. A 1 c ≥ 7. 0% • Atherosclerotic CV disease‡ • e. GFR <30 ml/min/1. 73 m 2 • Current use of GLP-1 receptor agonists • Previous or substantial risk of pancreatitis Primary endpoint 3 P-MACE (CV death, non-fatal MI, non-fatal stroke) Key secondary endpoints 4 P-MACE, § CV death, MI, stroke, composite of CV death or HHF, microvascular event composite, § time to initiation of chronic insulin therapy, change in Hb. A 1 c and body weight Albiglutide is not approved for the treatment of T 2 D *Dose could be uptitrated by the study investigator to 50 mg after 5 weeks of study treatment; †Time- and event-driven trial, median planned duration of follow-up was 1. 5 years; ‡Defined as disease of the coronary, cerebrovascular or peripheral arterial circulation; §Defined as CV death, MI, stroke or urgent revasularisation for unstable angina; ¶Defined as need for kidney transplant or dialysis, new diabetes-related blindness and procedures (laser photocoagulation or anti-VEGF treatment or vitrectomy) See slide notes for abbreviations Green JB et al. Am Heart J 2018; 203: 30; Hernandez AF et al. Lancet 2018; 392: 1519; Clinical. Trials. gov. NCT 02465515 (accessed Dec 2019) 16
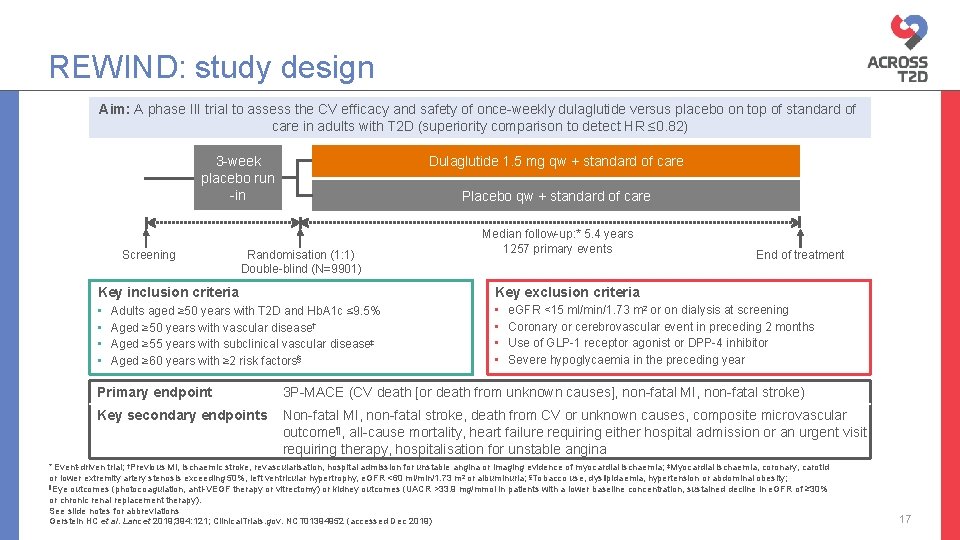
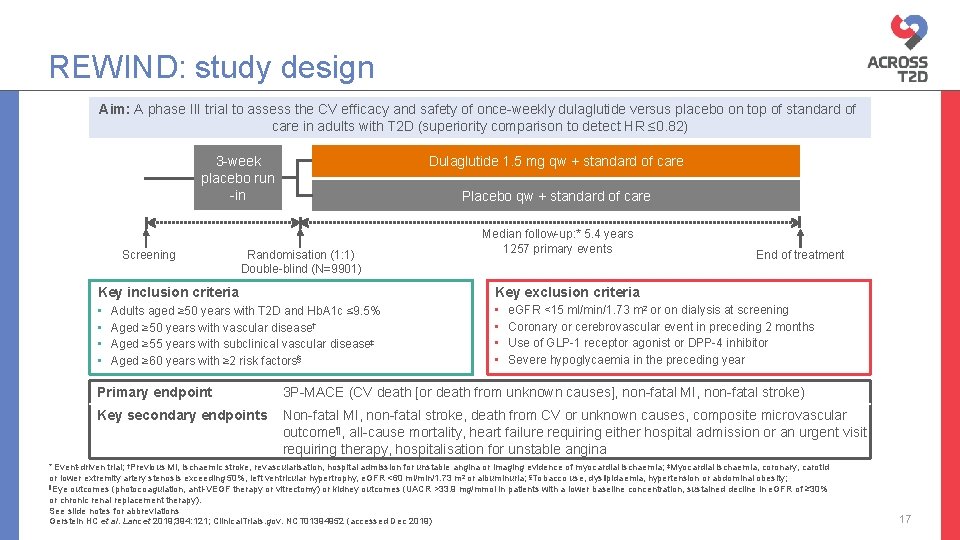
REWIND: study design Aim: A phase III trial to assess the CV efficacy and safety of once-weekly dulaglutide versus placebo on top of standard of care in adults with T 2 D (superiority comparison to detect HR ≤ 0. 82) Dulaglutide 1. 5 mg qw + standard of care 3 -week placebo run -in Screening Placebo qw + standard of care Randomisation (1: 1) Double-blind (N=9901) Median follow-up: * 5. 4 years 1257 primary events Key inclusion criteria Key exclusion criteria • • Adults aged ≥ 50 years with T 2 D and Hb. A 1 c ≤ 9. 5% Aged ≥ 50 years with vascular disease† Aged ≥ 55 years with subclinical vascular disease‡ Aged ≥ 60 years with ≥ 2 risk factors§ End of treatment e. GFR <15 ml/min/1. 73 m 2 or on dialysis at screening Coronary or cerebrovascular event in preceding 2 months Use of GLP-1 receptor agonist or DPP-4 inhibitor Severe hypoglycaemia in the preceding year Primary endpoint 3 P-MACE (CV death [or death from unknown causes], non-fatal MI, non-fatal stroke) Key secondary endpoints Non-fatal MI, non-fatal stroke, death from CV or unknown causes, composite microvascular outcome¶, all-cause mortality, heart failure requiring either hospital admission or an urgent visit requiring therapy, hospitalisation for unstable angina * Event-driven trial; †Previous MI, ischaemic stroke, revascularisation, hospital admission for unstable angina or imaging evidence of myocardial ischaemia; ‡Myocardial ischaemia, coronary, carotid or lower extremity artery stenosis exceeding 50%, left ventricular hypertrophy, e. GFR <60 ml/min/1. 73 m 2 or albuminuria; §Tobacco use, dyslipidaemia, hypertension or abdominal obesity; ¶Eye outcomes (photocoagulation, anti-VEGF therapy or vitrectomy) or kidney outcomes (UACR >33. 9 mg/mmol in patients with a lower baseline concentration, sustained decline in e. GFR of ≥ 30% or chronic renal replacement therapy). See slide notes for abbreviations Gerstein HC et al. Lancet 2019; 394: 121; Clinical. Trials. gov. NCT 01394952 (accessed Dec 2019) 17
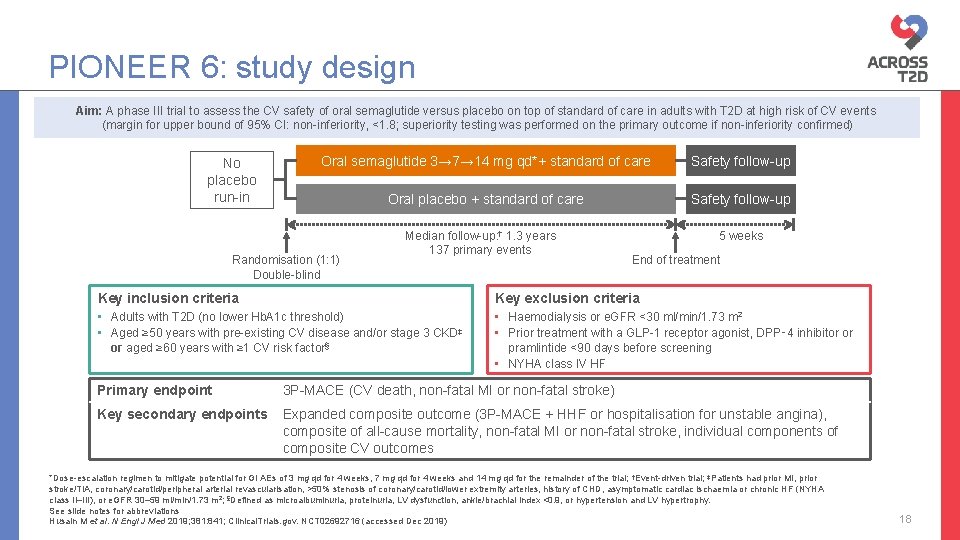
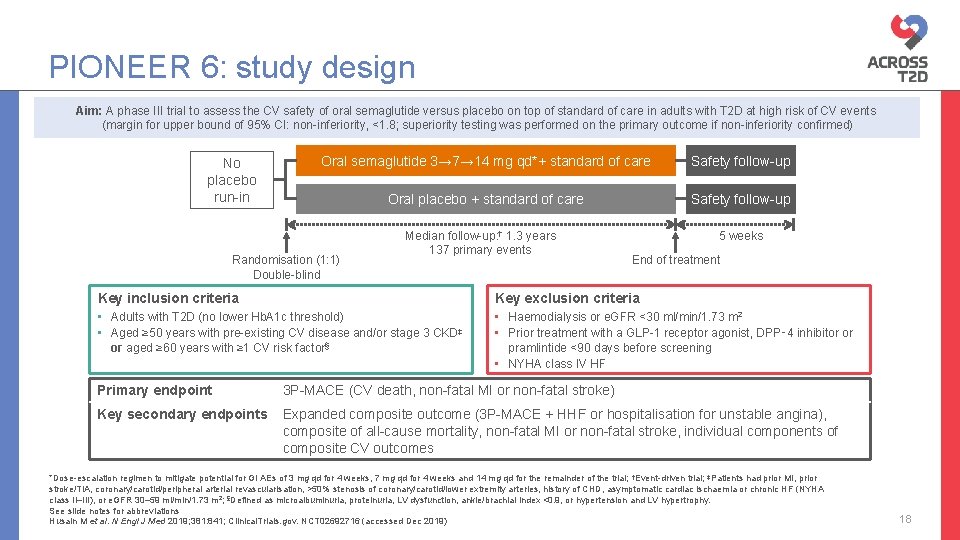
PIONEER 6: study design Aim: A phase III trial to assess the CV safety of oral semaglutide versus placebo on top of standard of care in adults with T 2 D at high risk of CV events (margin for upper bound of 95% CI: non-inferiority, <1. 8; superiority testing was performed on the primary outcome if non-inferiority confirmed) No placebo run-in Oral semaglutide 3→ 7→ 14 mg qd*+ standard of care Safety follow-up Oral placebo + standard of care Safety follow-up Randomisation (1: 1) Double-blind Median follow-up: † 1. 3 years 137 primary events 5 weeks End of treatment Key inclusion criteria Key exclusion criteria • Adults with T 2 D (no lower Hb. A 1 c threshold) • Aged ≥ 50 years with pre-existing CV disease and/or stage 3 CKD‡ or aged ≥ 60 years with ≥ 1 CV risk factor§ • Haemodialysis or e. GFR <30 ml/min/1. 73 m 2 • Prior treatment with a GLP-1 receptor agonist, DPP‑ 4 inhibitor or pramlintide <90 days before screening • NYHA class IV HF Primary endpoint 3 P-MACE (CV death, non-fatal MI or non-fatal stroke) Key secondary endpoints Expanded composite outcome (3 P-MACE + HHF or hospitalisation for unstable angina), composite of all-cause mortality, non-fatal MI or non-fatal stroke, individual components of composite CV outcomes *Dose-escalation regimen to mitigate potential for GI AEs of 3 mg qd for 4 weeks, 7 mg qd for 4 weeks and 14 mg qd for the remainder of the trial; †Event-driven trial; ‡Patients had prior MI, prior stroke/TIA, coronary/carotid/peripheral arterial revascularisation, >50% stenosis of coronary/carotid/lower extremity arteries, history of CHD, asymptomatic cardiac ischaemia or chronic HF (NYHA class II–III), or e. GFR 30– 59 ml/min/1. 73 m 2; §Defined as microalbuminuria, proteinuria, LV dysfunction, ankle/brachial index <0. 9, or hypertension and LV hypertrophy. See slide notes for abbreviations Husain M et al. N Engl J Med 2019; 381: 841; Clinical. Trials. gov. NCT 02692716 (accessed Dec 2019) 18
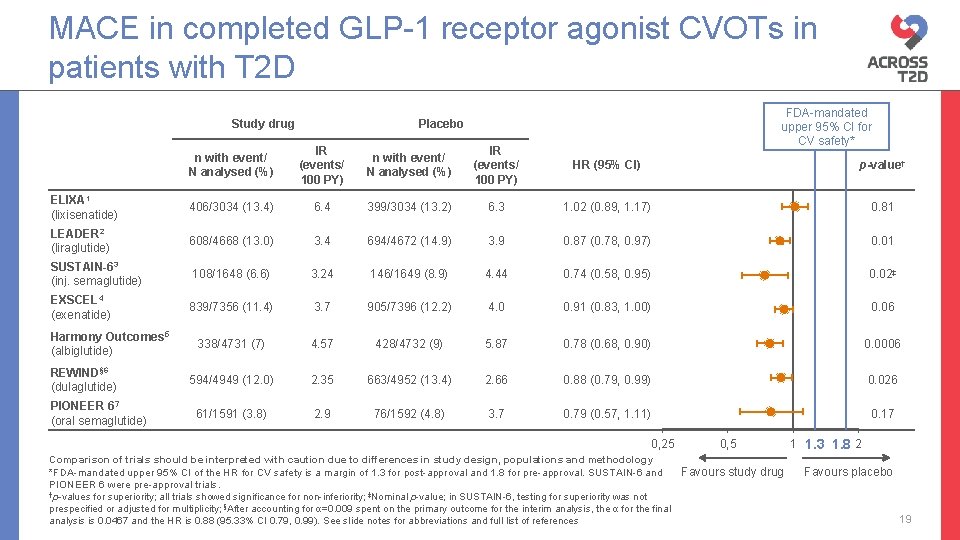
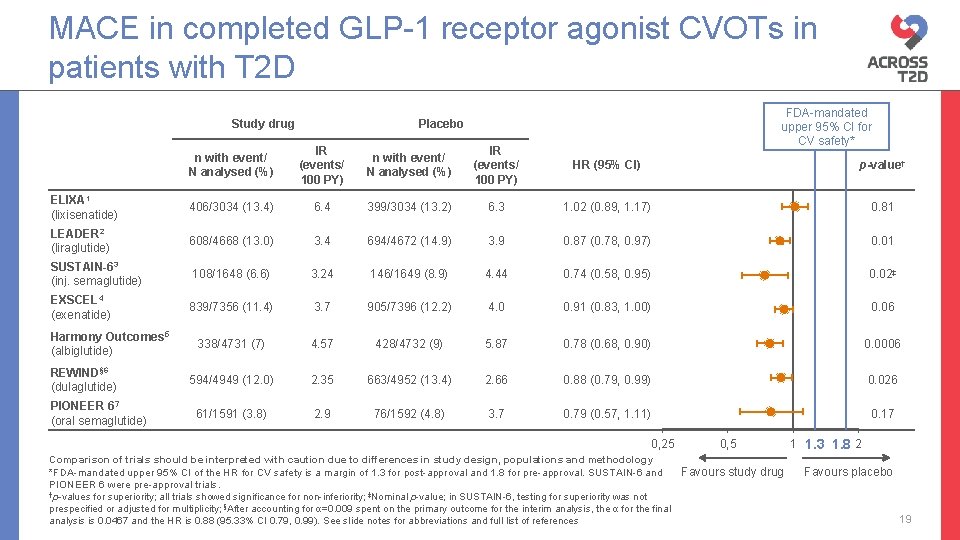
MACE in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug FDA-mandated upper 95% CI for CV safety* Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value† ELIXA 1 (lixisenatide) 406/3034 (13. 4) 6. 4 399/3034 (13. 2) 6. 3 1. 02 (0. 89, 1. 17) 0. 81 LEADER 2 (liraglutide) 608/4668 (13. 0) 3. 4 694/4672 (14. 9) 3. 9 0. 87 (0. 78, 0. 97) 0. 01 SUSTAIN-63 (inj. semaglutide) 108/1648 (6. 6) 3. 24 146/1649 (8. 9) 4. 44 0. 74 (0. 58, 0. 95) 0. 02‡ EXSCEL 4 (exenatide) 839/7356 (11. 4) 3. 7 905/7396 (12. 2) 4. 0 0. 91 (0. 83, 1. 00) 0. 06 338/4731 (7) 4. 57 428/4732 (9) 5. 87 0. 78 (0. 68, 0. 90) 0. 0006 594/4949 (12. 0) 2. 35 663/4952 (13. 4) 2. 66 0. 88 (0. 79, 0. 99) 0. 026 61/1591 (3. 8) 2. 9 76/1592 (4. 8) 3. 7 0. 79 (0. 57, 1. 11) 0. 17 Harmony Outcomes 5 (albiglutide) REWIND§ 6 (dulaglutide) PIONEER 67 (oral semaglutide) 0, 25 0, 5 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *FDA-mandated upper 95% CI of the HR for CV safety is a margin of 1. 3 for post-approval and 1. 8 for pre-approval. SUSTAIN-6 and Favours study drug PIONEER 6 were pre-approval trials. †p-values for superiority; all trials showed significance for non-inferiority; ‡Nominal p-value; in SUSTAIN-6, testing for superiority was not prespecified or adjusted for multiplicity; §After accounting for α=0. 009 spent on the primary outcome for the interim analysis, the α for the final analysis is 0. 0467 and the HR is 0. 88 (95. 33% CI 0. 79, 0. 99). See slide notes for abbreviations and full list of references 1 1. 3 1. 8 2 Favours placebo 19
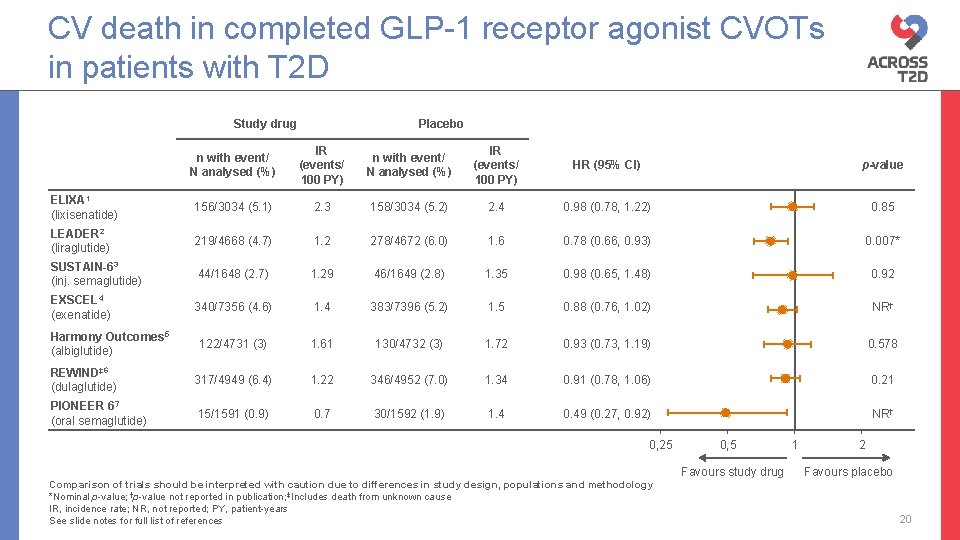
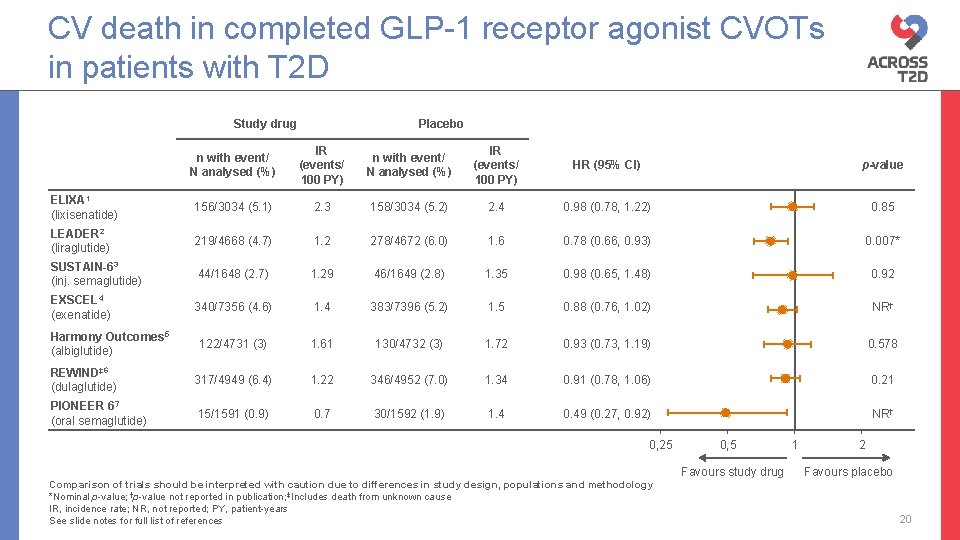
CV death in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value ELIXA 1 (lixisenatide) 156/3034 (5. 1) 2. 3 158/3034 (5. 2) 2. 4 0. 98 (0. 78, 1. 22) 0. 85 LEADER 2 (liraglutide) 219/4668 (4. 7) 1. 2 278/4672 (6. 0) 1. 6 0. 78 (0. 66, 0. 93) 0. 007* SUSTAIN-63 (inj. semaglutide) 44/1648 (2. 7) 1. 29 46/1649 (2. 8) 1. 35 0. 98 (0. 65, 1. 48) 0. 92 EXSCEL 4 (exenatide) 340/7356 (4. 6) 1. 4 383/7396 (5. 2) 1. 5 0. 88 (0. 76, 1. 02) NR† 122/4731 (3) 1. 61 130/4732 (3) 1. 72 0. 93 (0. 73, 1. 19) 0. 578 REWIND‡ 6 (dulaglutide) 317/4949 (6. 4) 1. 22 346/4952 (7. 0) 1. 34 0. 91 (0. 78, 1. 06) 0. 21 PIONEER 67 (oral semaglutide) 15/1591 (0. 9) 0. 7 30/1592 (1. 9) 1. 4 0. 49 (0. 27, 0. 92) NR† Harmony Outcomes 5 (albiglutide) 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Nominal p-value; †p-value not reported in publication; ‡Includes death from unknown cause IR, incidence rate; NR, not reported; PY, patient-years See slide notes for full list of references 0, 5 Favours study drug 1 2 Favours placebo 20
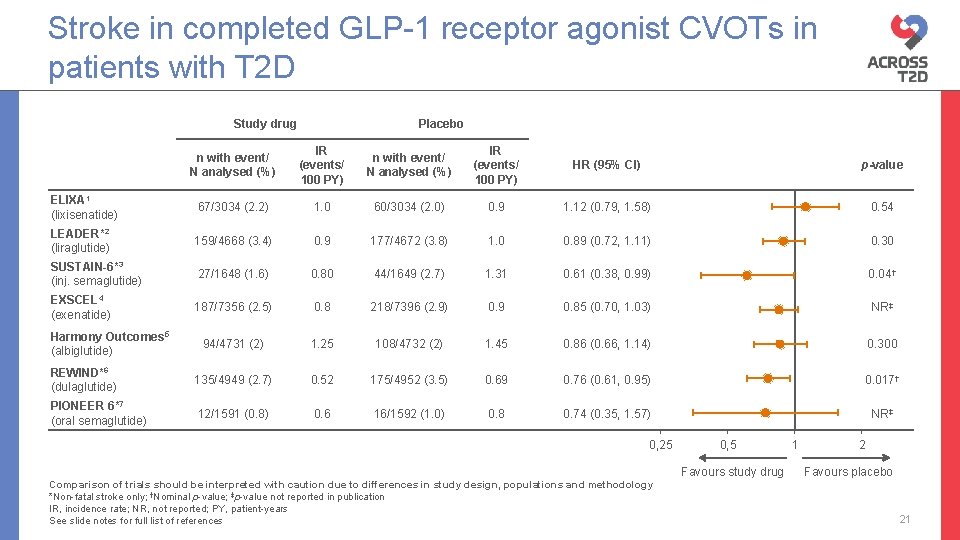
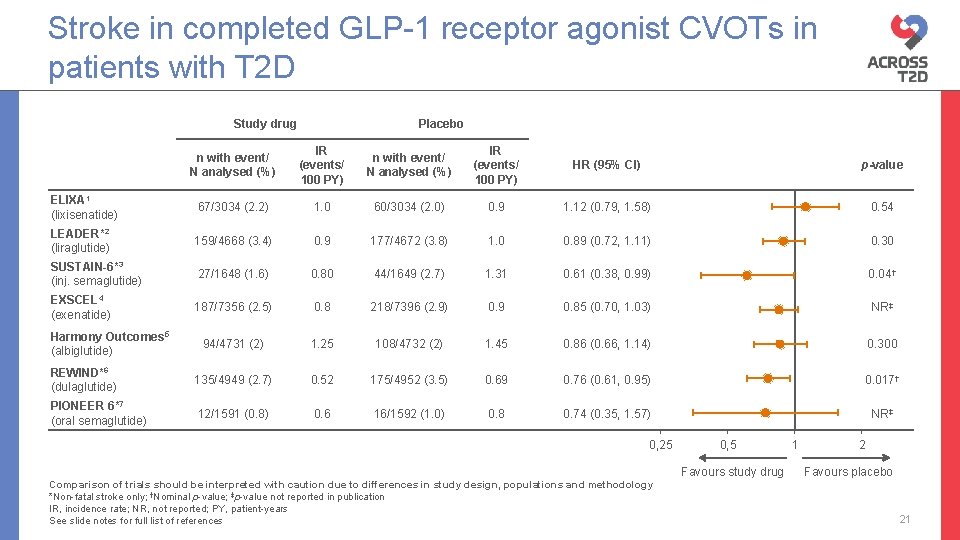
Stroke in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value ELIXA 1 (lixisenatide) 67/3034 (2. 2) 1. 0 60/3034 (2. 0) 0. 9 1. 12 (0. 79, 1. 58) 0. 54 LEADER*2 (liraglutide) 159/4668 (3. 4) 0. 9 177/4672 (3. 8) 1. 0 0. 89 (0. 72, 1. 11) 0. 30 SUSTAIN-6*3 (inj. semaglutide) 27/1648 (1. 6) 0. 80 44/1649 (2. 7) 1. 31 0. 61 (0. 38, 0. 99) 0. 04† EXSCEL 4 (exenatide) 187/7356 (2. 5) 0. 8 218/7396 (2. 9) 0. 9 0. 85 (0. 70, 1. 03) NR‡ 94/4731 (2) 1. 25 108/4732 (2) 1. 45 0. 86 (0. 66, 1. 14) 0. 300 REWIND*6 (dulaglutide) 135/4949 (2. 7) 0. 52 175/4952 (3. 5) 0. 69 0. 76 (0. 61, 0. 95) 0. 017† PIONEER 6*7 (oral semaglutide) 12/1591 (0. 8) 0. 6 16/1592 (1. 0) 0. 8 0. 74 (0. 35, 1. 57) NR‡ Harmony Outcomes 5 (albiglutide) 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Non-fatal stroke only; †Nominal p-value; ‡p-value not reported in publication IR, incidence rate; NR, not reported; PY, patient-years See slide notes for full list of references 0, 5 Favours study drug 1 2 Favours placebo 21
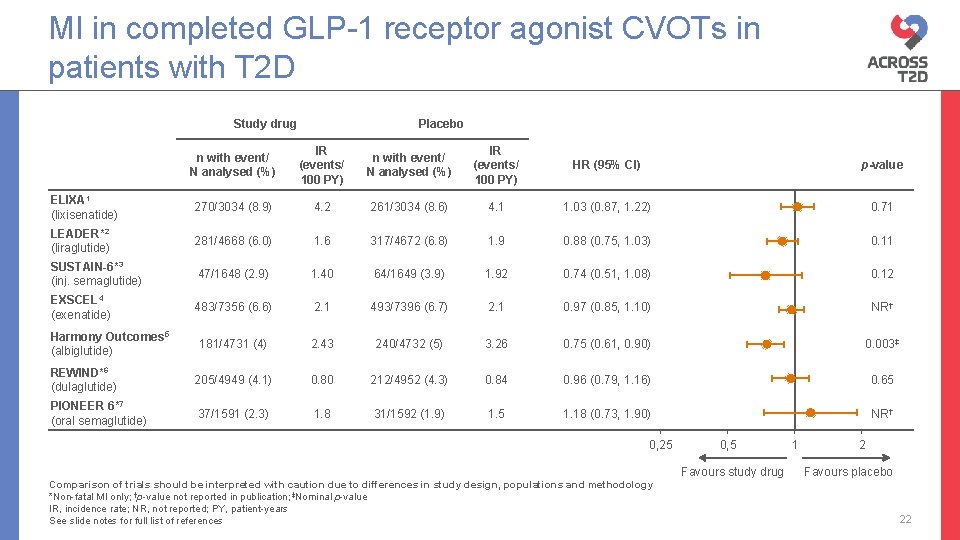
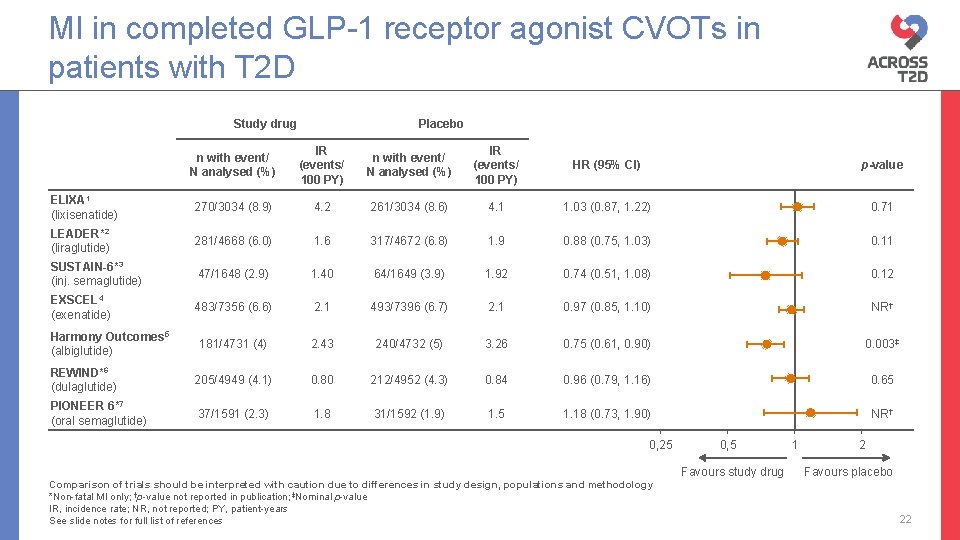
MI in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value ELIXA 1 (lixisenatide) 270/3034 (8. 9) 4. 2 261/3034 (8. 6) 4. 1 1. 03 (0. 87, 1. 22) 0. 71 LEADER*2 (liraglutide) 281/4668 (6. 0) 1. 6 317/4672 (6. 8) 1. 9 0. 88 (0. 75, 1. 03) 0. 11 SUSTAIN-6*3 (inj. semaglutide) 47/1648 (2. 9) 1. 40 64/1649 (3. 9) 1. 92 0. 74 (0. 51, 1. 08) 0. 12 EXSCEL 4 (exenatide) 483/7356 (6. 6) 2. 1 493/7396 (6. 7) 2. 1 0. 97 (0. 85, 1. 10) NR† 181/4731 (4) 2. 43 240/4732 (5) 3. 26 0. 75 (0. 61, 0. 90) 0. 003‡ REWIND*6 (dulaglutide) 205/4949 (4. 1) 0. 80 212/4952 (4. 3) 0. 84 0. 96 (0. 79, 1. 16) 0. 65 PIONEER 6*7 (oral semaglutide) 37/1591 (2. 3) 1. 8 31/1592 (1. 9) 1. 5 1. 18 (0. 73, 1. 90) NR† Harmony Outcomes 5 (albiglutide) 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Non-fatal MI only; †p-value not reported in publication; ‡Nominal p-value IR, incidence rate; NR, not reported; PY, patient-years See slide notes for full list of references 0, 5 Favours study drug 1 2 Favours placebo 22
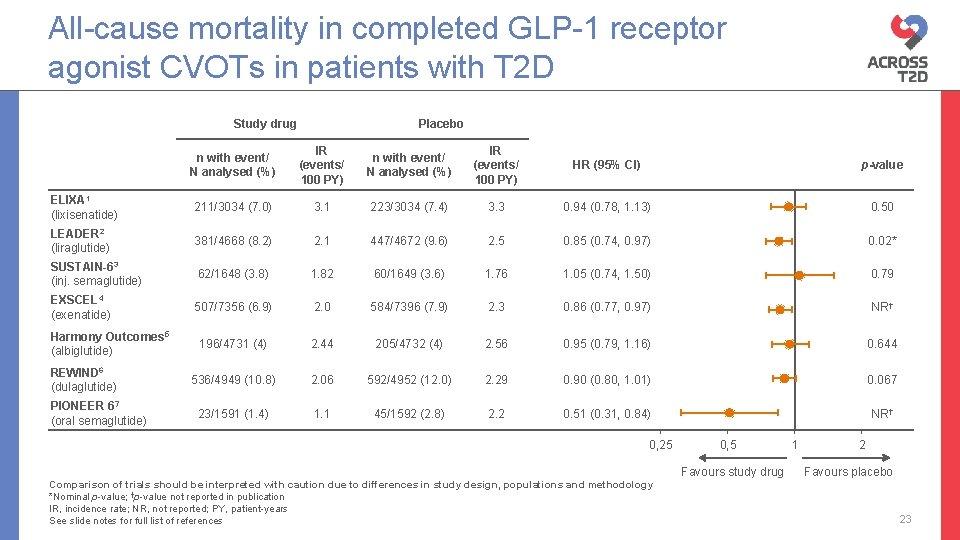
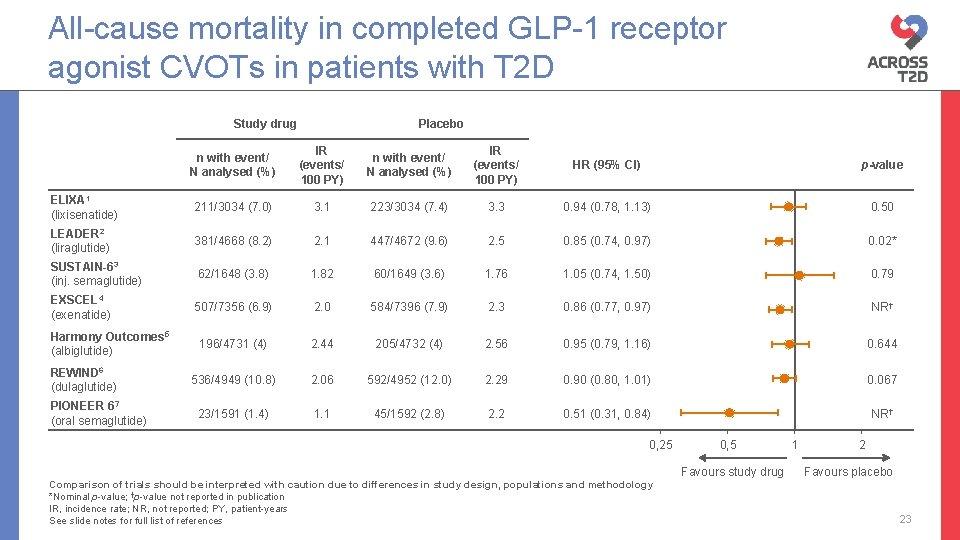
All-cause mortality in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value ELIXA 1 (lixisenatide) 211/3034 (7. 0) 3. 1 223/3034 (7. 4) 3. 3 0. 94 (0. 78, 1. 13) 0. 50 LEADER 2 (liraglutide) 381/4668 (8. 2) 2. 1 447/4672 (9. 6) 2. 5 0. 85 (0. 74, 0. 97) 0. 02* SUSTAIN-63 (inj. semaglutide) 62/1648 (3. 8) 1. 82 60/1649 (3. 6) 1. 76 1. 05 (0. 74, 1. 50) 0. 79 EXSCEL 4 (exenatide) 507/7356 (6. 9) 2. 0 584/7396 (7. 9) 2. 3 0. 86 (0. 77, 0. 97) NR† 196/4731 (4) 2. 44 205/4732 (4) 2. 56 0. 95 (0. 79, 1. 16) 0. 644 536/4949 (10. 8) 2. 06 592/4952 (12. 0) 2. 29 0. 90 (0. 80, 1. 01) 0. 067 23/1591 (1. 4) 1. 1 45/1592 (2. 8) 2. 2 0. 51 (0. 31, 0. 84) NR† Harmony Outcomes 5 (albiglutide) REWIND 6 (dulaglutide) PIONEER 67 (oral semaglutide) 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Nominal p-value; †p-value not reported in publication IR, incidence rate; NR, not reported; PY, patient-years See slide notes for full list of references 0, 5 Favours study drug 1 2 Favours placebo 23
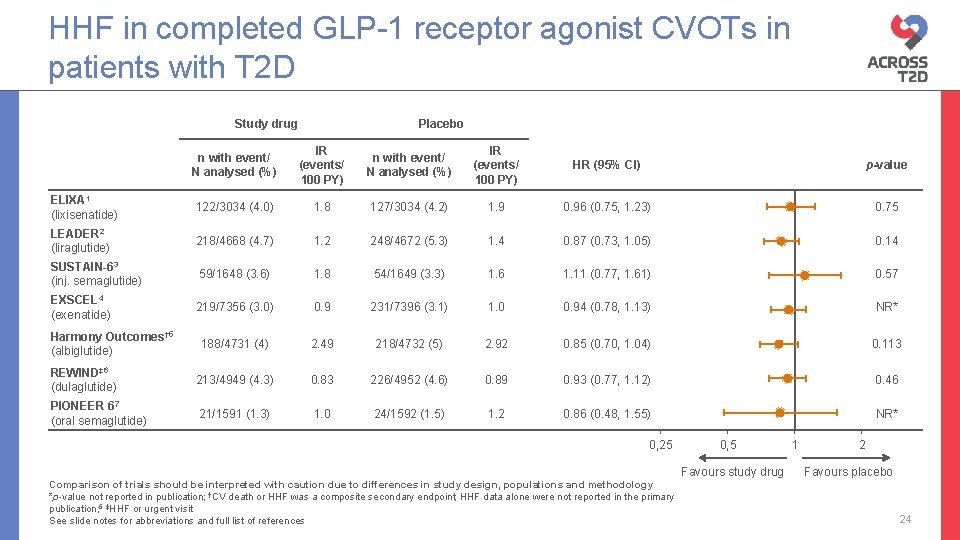
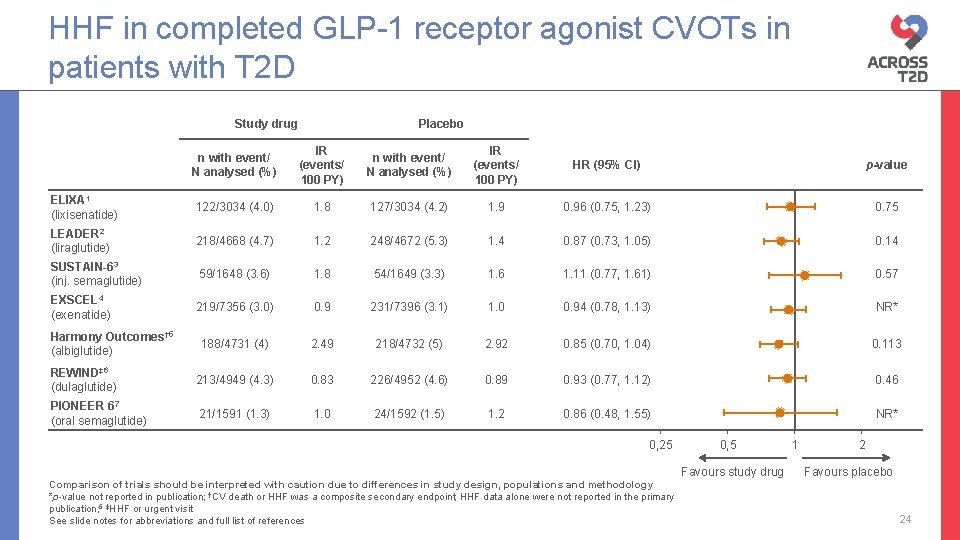
HHF in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value ELIXA 1 (lixisenatide) 122/3034 (4. 0) 1. 8 127/3034 (4. 2) 1. 9 0. 96 (0. 75, 1. 23) 0. 75 LEADER 2 (liraglutide) 218/4668 (4. 7) 1. 2 248/4672 (5. 3) 1. 4 0. 87 (0. 73, 1. 05) 0. 14 SUSTAIN-63 (inj. semaglutide) 59/1648 (3. 6) 1. 8 54/1649 (3. 3) 1. 6 1. 11 (0. 77, 1. 61) 0. 57 EXSCEL 4 (exenatide) 219/7356 (3. 0) 0. 9 231/7396 (3. 1) 1. 0 0. 94 (0. 78, 1. 13) NR* 188/4731 (4) 2. 49 218/4732 (5) 2. 92 0. 85 (0. 70, 1. 04) 0. 113 REWIND‡ 6 (dulaglutide) 213/4949 (4. 3) 0. 83 226/4952 (4. 6) 0. 89 0. 93 (0. 77, 1. 12) 0. 46 PIONEER 67 (oral semaglutide) 21/1591 (1. 3) 1. 0 24/1592 (1. 5) 1. 2 0. 86 (0. 48, 1. 55) NR* Harmony Outcomes† 5 (albiglutide) 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *p-value not reported in publication; †CV death or HHF was a composite secondary endpoint; HHF data alone were not reported in the primary publication; 5 ‡HHF or urgent visit See slide notes for abbreviations and full list of references 0, 5 Favours study drug 1 2 Favours placebo 24
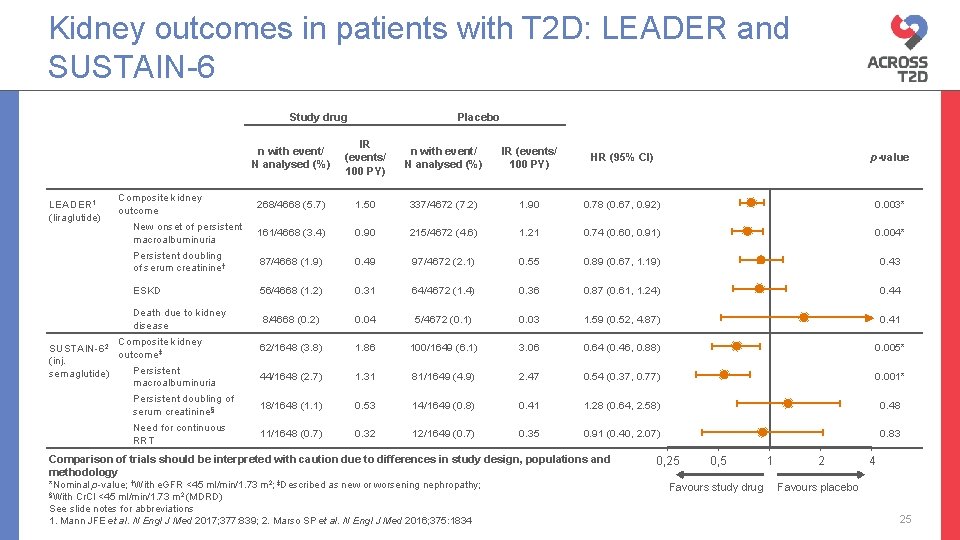
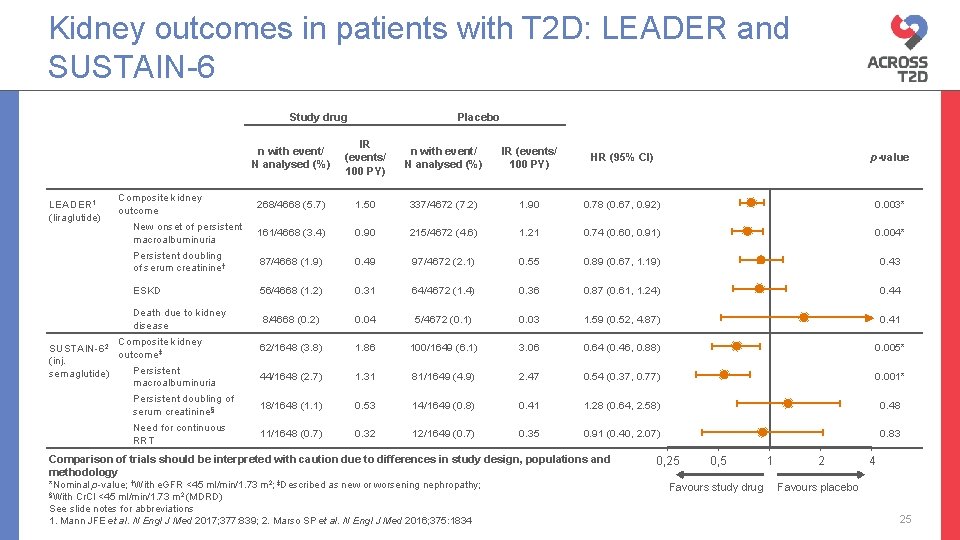
Kidney outcomes in patients with T 2 D: LEADER and SUSTAIN-6 Study drug LEADER 1 (liraglutide) Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value 268/4668 (5. 7) 1. 50 337/4672 (7. 2) 1. 90 0. 78 (0. 67, 0. 92) 0. 003* New onset of persistent macroalbuminuria 161/4668 (3. 4) 0. 90 215/4672 (4. 6) 1. 21 0. 74 (0. 60, 0. 91) 0. 004* Persistent doubling of serum creatinine† 87/4668 (1. 9) 0. 49 97/4672 (2. 1) 0. 55 0. 89 (0. 67, 1. 19) 0. 43 ESKD 56/4668 (1. 2) 0. 31 64/4672 (1. 4) 0. 36 0. 87 (0. 61, 1. 24) 0. 44 Death due to kidney disease 8/4668 (0. 2) 0. 04 5/4672 (0. 1) 0. 03 1. 59 (0. 52, 4. 87) 0. 41 62/1648 (3. 8) 1. 86 100/1649 (6. 1) 3. 06 0. 64 (0. 46, 0. 88) 0. 005* 44/1648 (2. 7) 1. 31 81/1649 (4. 9) 2. 47 0. 54 (0. 37, 0. 77) 0. 001* Persistent doubling of serum creatinine§ 18/1648 (1. 1) 0. 53 14/1649 (0. 8) 0. 41 1. 28 (0. 64, 2. 58) 0. 48 Need for continuous RRT 11/1648 (0. 7) 0. 32 12/1649 (0. 7) 0. 35 0. 91 (0. 40, 2. 07) 0. 83 Composite kidney outcome Composite kidney SUSTAIN-62 outcome‡ (inj. Persistent semaglutide) macroalbuminuria Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Nominal p-value; †With e. GFR <45 ml/min/1. 73 m 2; ‡Described as new or worsening nephropathy; §With Cr. Cl <45 ml/min/1. 73 m 2 (MDRD) See slide notes for abbreviations 1. Mann JFE et al. N Engl J Med 2017; 377: 839; 2. Marso SP et al. N Engl J Med 2016; 375: 1834 0, 25 0, 5 Favours study drug 1 2 4 Favours placebo 25
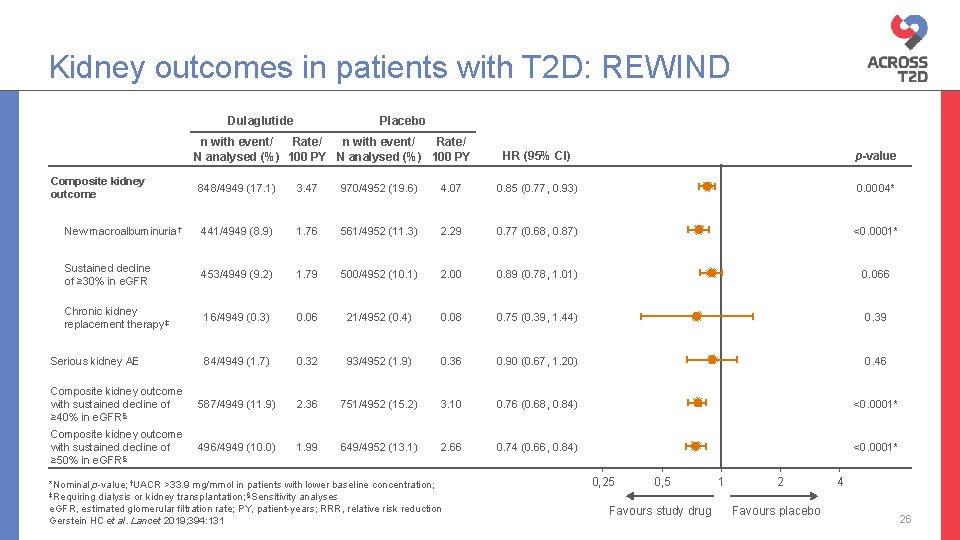
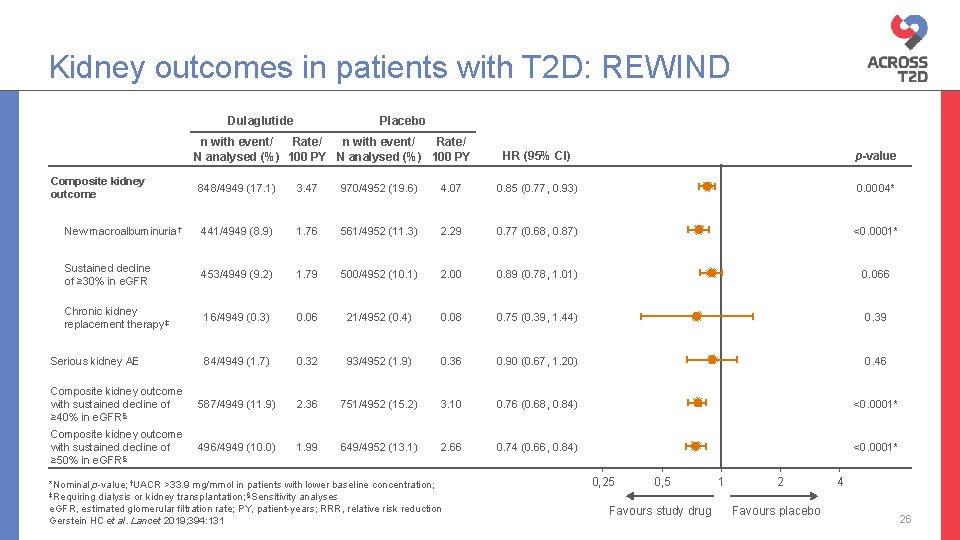
Kidney outcomes in patients with T 2 D: REWIND Dulaglutide Placebo n with event/ Rate/ N analysed (%) 100 PY Composite kidney outcome HR (95% CI) p-value 848/4949 (17. 1) 3. 47 970/4952 (19. 6) 4. 07 0. 85 (0. 77, 0. 93) 0. 0004* New macroalbuminuria† 441/4949 (8. 9) 1. 76 561/4952 (11. 3) 2. 29 0. 77 (0. 68, 0. 87) <0. 0001* Sustained decline of ≥ 30% in e. GFR 453/4949 (9. 2) 1. 79 500/4952 (10. 1) 2. 00 0. 89 (0. 78, 1. 01) 0. 066 Chronic kidney replacement therapy‡ 16/4949 (0. 3) 0. 06 21/4952 (0. 4) 0. 08 0. 75 (0. 39, 1. 44) 0. 39 84/4949 (1. 7) 0. 32 93/4952 (1. 9) 0. 36 0. 90 (0. 67, 1. 20) 0. 46 Composite kidney outcome with sustained decline of ≥ 40% in e. GFR§ 587/4949 (11. 9) 2. 36 751/4952 (15. 2) 3. 10 0. 76 (0. 68, 0. 84) <0. 0001* Composite kidney outcome with sustained decline of ≥ 50% in e. GFR§ 496/4949 (10. 0) 1. 99 649/4952 (13. 1) 2. 66 0. 74 (0. 66, 0. 84) <0. 0001* Serious kidney AE *Nominal p-value; †UACR >33. 9 mg/mmol in patients with lower baseline concentration; ‡Requiring dialysis or kidney transplantation; §Sensitivity analyses e. GFR, estimated glomerular filtration rate; PY, patient-years; RRR, relative risk reduction Gerstein HC et al. Lancet 2019; 394: 131 0, 25 0, 5 Favours study drug 1 2 Favours placebo 4 26
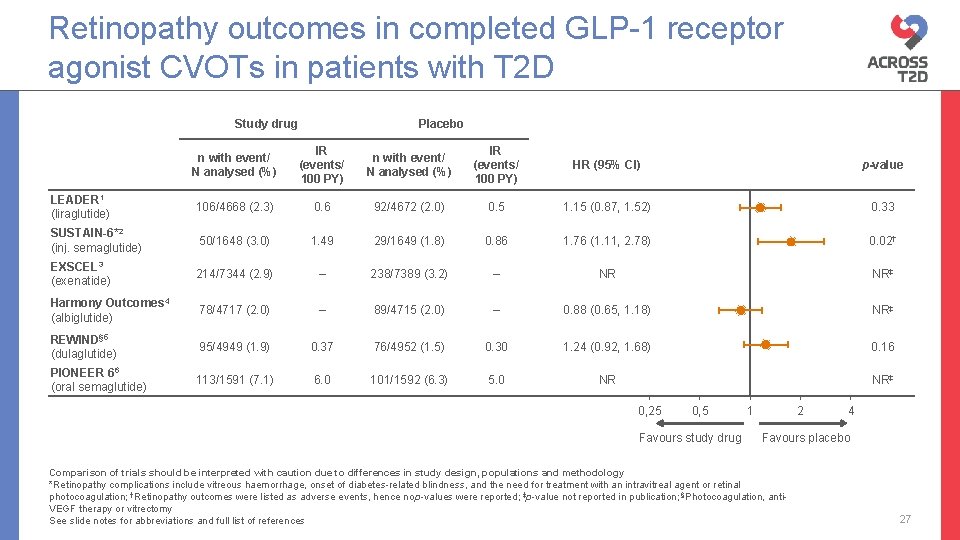
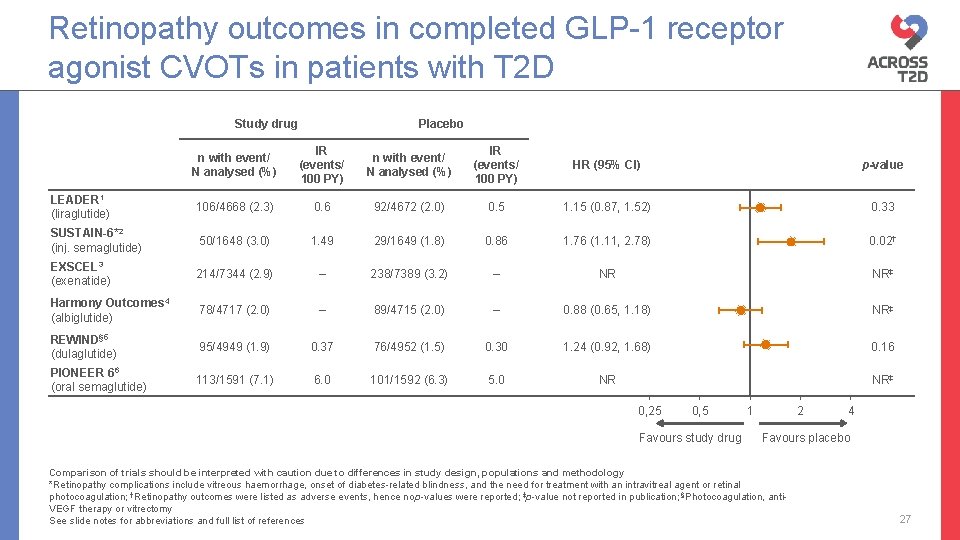
Retinopathy outcomes in completed GLP-1 receptor agonist CVOTs in patients with T 2 D Study drug Placebo n with event/ N analysed (%) IR (events/ 100 PY) HR (95% CI) p-value LEADER 1 (liraglutide) 106/4668 (2. 3) 0. 6 92/4672 (2. 0) 0. 5 1. 15 (0. 87, 1. 52) 0. 33 SUSTAIN-6*2 (inj. semaglutide) 50/1648 (3. 0) 1. 49 29/1649 (1. 8) 0. 86 1. 76 (1. 11, 2. 78) 0. 02† EXSCEL 3 (exenatide) 214/7344 (2. 9) – 238/7389 (3. 2) – NR NR‡ Harmony Outcomes 4 (albiglutide) 78/4717 (2. 0) – 89/4715 (2. 0) – 0. 88 (0. 65, 1. 18) NR‡ REWIND§ 5 (dulaglutide) 95/4949 (1. 9) 0. 37 76/4952 (1. 5) 0. 30 1. 24 (0. 92, 1. 68) 0. 16 PIONEER 66 (oral semaglutide) 113/1591 (7. 1) 6. 0 101/1592 (6. 3) 5. 0 NR NR‡ 0, 25 0, 5 Favours study drug 1 2 4 Favours placebo Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Retinopathy complications include vitreous haemorrhage, onset of diabetes-related blindness, and the need for treatment with an intravitreal agent or retinal photocoagulation; †Retinopathy outcomes were listed as adverse events, hence no p-values were reported; ‡p-value not reported in publication; §Photocoagulation, anti. VEGF therapy or vitrectomy See slide notes for abbreviations and full list of references 27
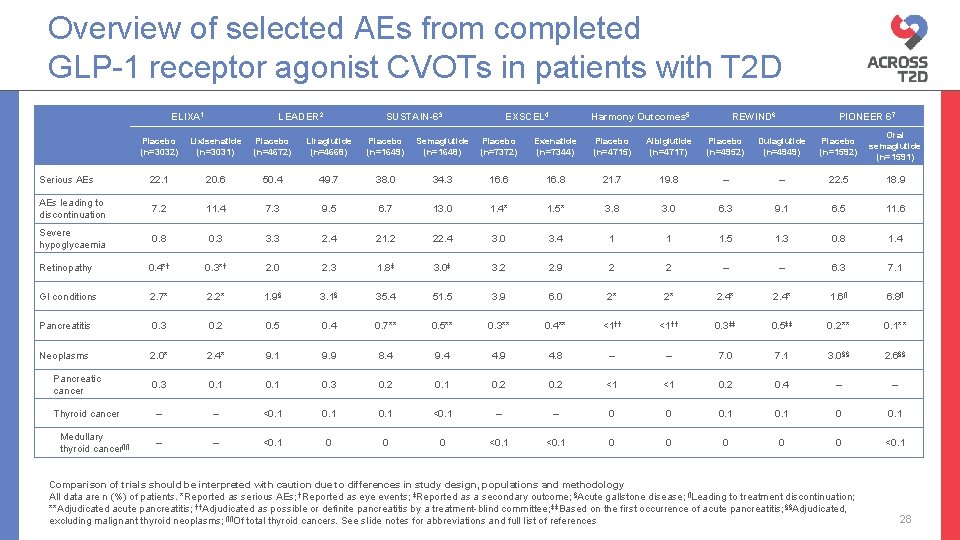
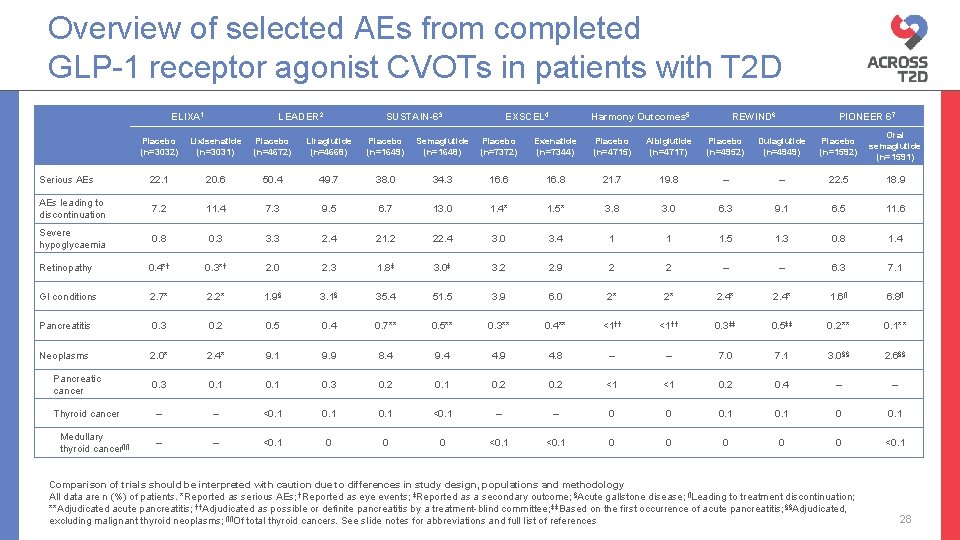
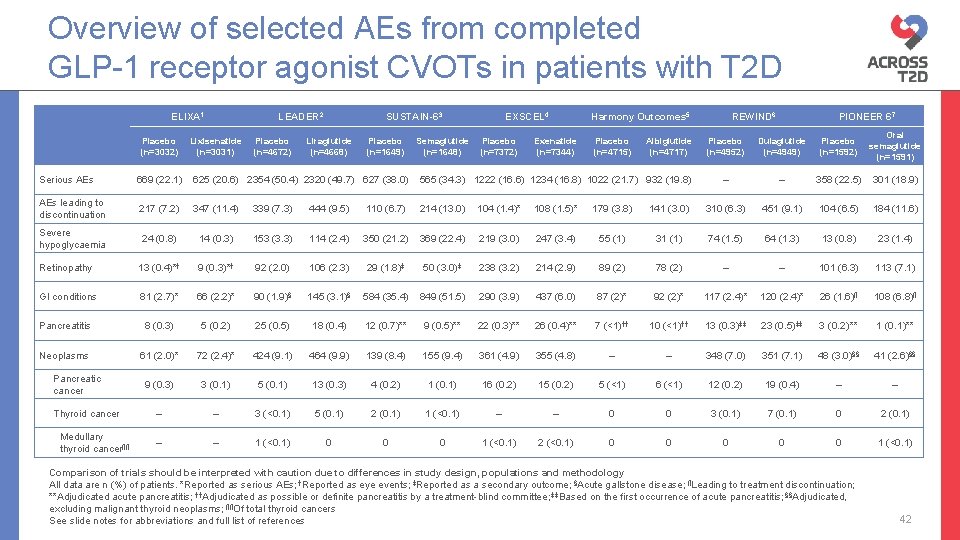
Overview of selected AEs from completed GLP-1 receptor agonist CVOTs in patients with T 2 D ELIXA 1 LEADER 2 SUSTAIN-63 EXSCEL 4 Harmony Outcomes 5 REWIND 6 PIONEER 67 Placebo (n=3032) Lixisenatide (n=3031) Placebo (n=4672) Liraglutide (n=4668) Placebo (n=1649) Semaglutide (n=1648) Placebo (n=7372) Exenatide (n=7344) Placebo (n=4715) Albiglutide (n=4717) Placebo (n=4952) Dulaglutide (n=4949) Placebo (n=1592) Oral semaglutide (n=1591) Serious AEs 22. 1 20. 6 50. 4 49. 7 38. 0 34. 3 16. 6 16. 8 21. 7 19. 8 – – 22. 5 18. 9 AEs leading to discontinuation 7. 2 11. 4 7. 3 9. 5 6. 7 13. 0 1. 4* 1. 5* 3. 8 3. 0 6. 3 9. 1 6. 5 11. 6 Severe hypoglycaemia 0. 8 0. 3 3. 3 2. 4 21. 2 22. 4 3. 0 3. 4 1 1 1. 5 1. 3 0. 8 1. 4 Retinopathy 0. 4*† 0. 3*† 2. 0 2. 3 1. 8‡ 3. 0‡ 3. 2 2. 9 2 2 – – 6. 3 7. 1 GI conditions 2. 7* 2. 2* 1. 9§ 3. 1§ 35. 4 51. 5 3. 9 6. 0 2* 2* 2. 4* 1. 6¶ 6. 8¶ Pancreatitis 0. 3 0. 2 0. 5 0. 4 0. 7** 0. 5** 0. 3** 0. 4** <1†† 0. 3‡‡ 0. 5‡‡ 0. 2** 0. 1** Neoplasms 2. 0* 2. 4* 9. 1 9. 9 8. 4 9. 4 4. 9 4. 8 – – 7. 0 7. 1 3. 0§§ 2. 6§§ 0. 3 0. 1 0. 3 0. 2 0. 1 0. 2 <1 <1 0. 2 0. 4 – – <0. 1 <0. 1 – – 0 0 0. 1 – – <0. 1 0 0 0 <0. 1 Pancreatic cancer Thyroid cancer Medullary thyroid cancer¶¶ Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology All data are n (%) of patients. *Reported as serious AEs; †Reported as eye events; ‡Reported as a secondary outcome; §Acute gallstone disease; ¶Leading to treatment discontinuation; **Adjudicated acute pancreatitis; ††Adjudicated as possible or definite pancreatitis by a treatment-blind committee; ‡‡Based on the first occurrence of acute pancreatitis; §§Adjudicated, excluding malignant thyroid neoplasms; ¶¶Of total thyroid cancers. See slide notes for abbreviations and full list of references 28
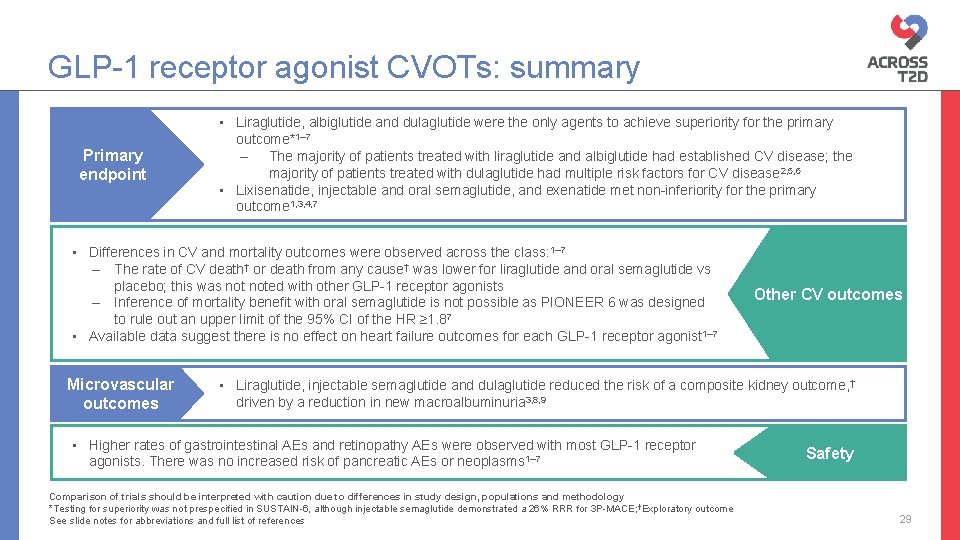
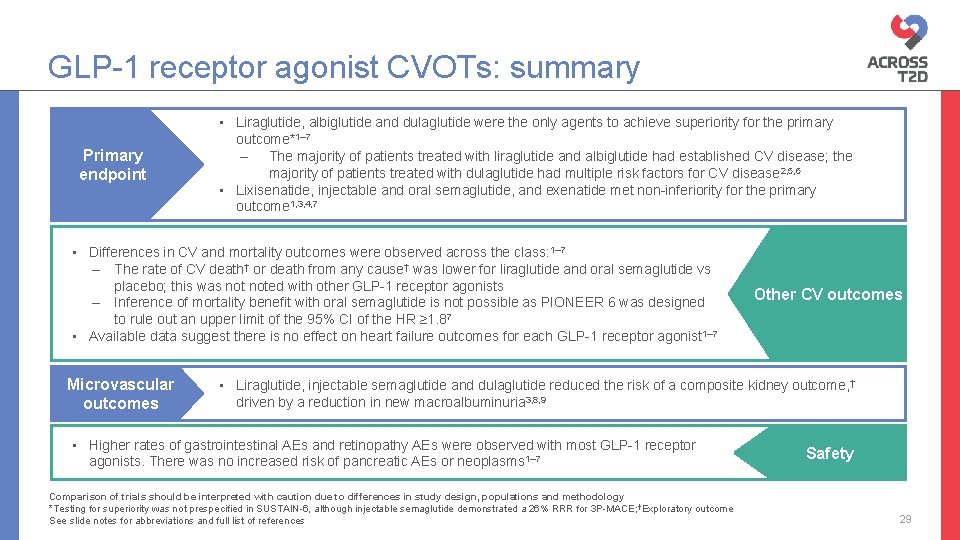
GLP-1 receptor agonist CVOTs: summary Primary endpoint • Liraglutide, albiglutide and dulaglutide were the only agents to achieve superiority for the primary outcome*1– 7 – The majority of patients treated with liraglutide and albiglutide had established CV disease; the majority of patients treated with dulaglutide had multiple risk factors for CV disease 2, 5, 6 • Lixisenatide, injectable and oral semaglutide, and exenatide met non-inferiority for the primary outcome 1, 3, 4, 7 • Differences in CV and mortality outcomes were observed across the class: 1– 7 – The rate of CV death† or death from any cause† was lower for liraglutide and oral semaglutide vs placebo; this was noted with other GLP-1 receptor agonists – Inference of mortality benefit with oral semaglutide is not possible as PIONEER 6 was designed to rule out an upper limit of the 95% CI of the HR ≥ 1. 87 • Available data suggest there is no effect on heart failure outcomes for each GLP-1 receptor agonist 1– 7 Microvascular outcomes Other CV outcomes • Liraglutide, injectable semaglutide and dulaglutide reduced the risk of a composite kidney outcome, † driven by a reduction in new macroalbuminuria 3, 8, 9 • Higher rates of gastrointestinal AEs and retinopathy AEs were observed with most GLP-1 receptor agonists. There was no increased risk of pancreatic AEs or neoplasms 1– 7 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Testing for superiority was not prespecified in SUSTAIN-6, although injectable semaglutide demonstrated a 26% RRR for 3 P-MACE; †Exploratory outcome See slide notes for abbreviations and full list of references Safety 29

Back-up slides
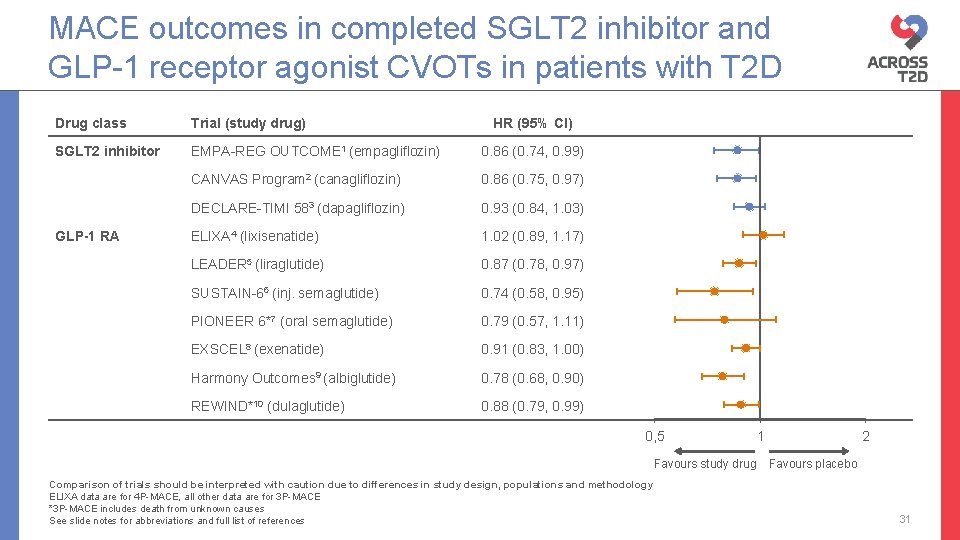
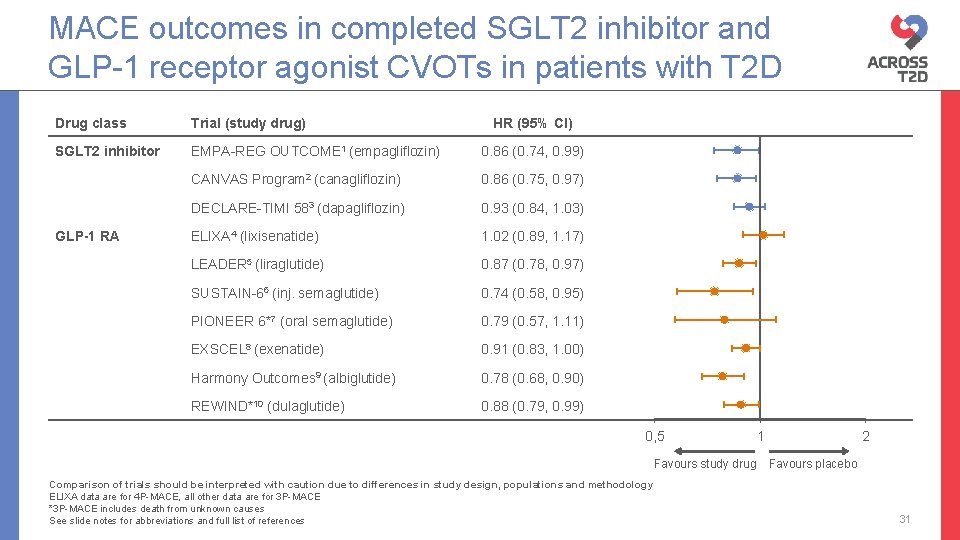
MACE outcomes in completed SGLT 2 inhibitor and GLP-1 receptor agonist CVOTs in patients with T 2 D Drug class Trial (study drug) SGLT 2 inhibitor EMPA-REG OUTCOME 1 (empagliflozin) 0. 86 (0. 74, 0. 99) CANVAS Program 2 (canagliflozin) 0. 86 (0. 75, 0. 97) DECLARE-TIMI 583 (dapagliflozin) 0. 93 (0. 84, 1. 03) ELIXA 4 (lixisenatide) 1. 02 (0. 89, 1. 17) LEADER 5 (liraglutide) 0. 87 (0. 78, 0. 97) SUSTAIN-66 (inj. semaglutide) 0. 74 (0. 58, 0. 95) PIONEER 6*7 (oral semaglutide) 0. 79 (0. 57, 1. 11) EXSCEL 8 (exenatide) 0. 91 (0. 83, 1. 00) Harmony Outcomes 9 (albiglutide) 0. 78 (0. 68, 0. 90) REWIND*10 (dulaglutide) 0. 88 (0. 79, 0. 99) GLP-1 RA HR (95% CI) 0, 5 Favours study drug Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology ELIXA data are for 4 P-MACE, all other data are for 3 P-MACE *3 P-MACE includes death from unknown causes See slide notes for abbreviations and full list of references 1 2 Favours placebo 31
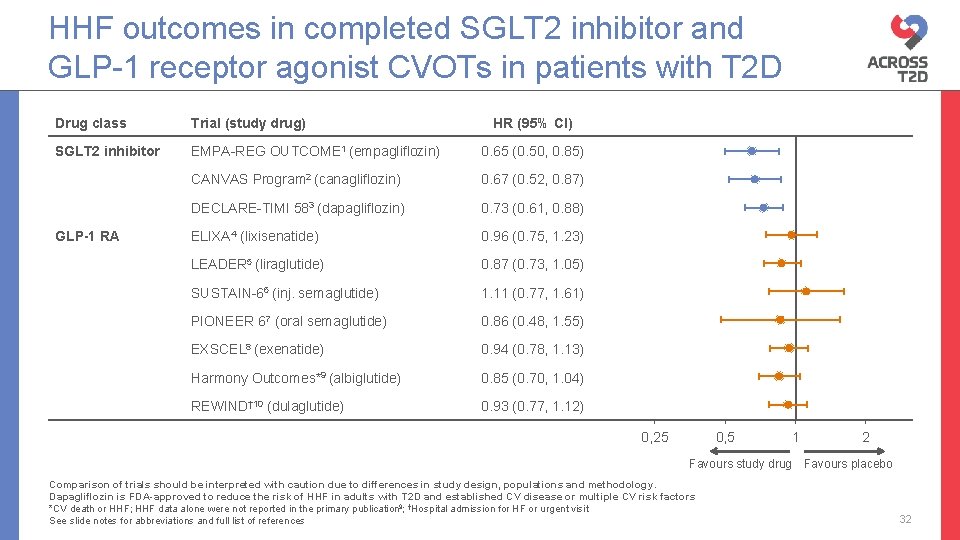
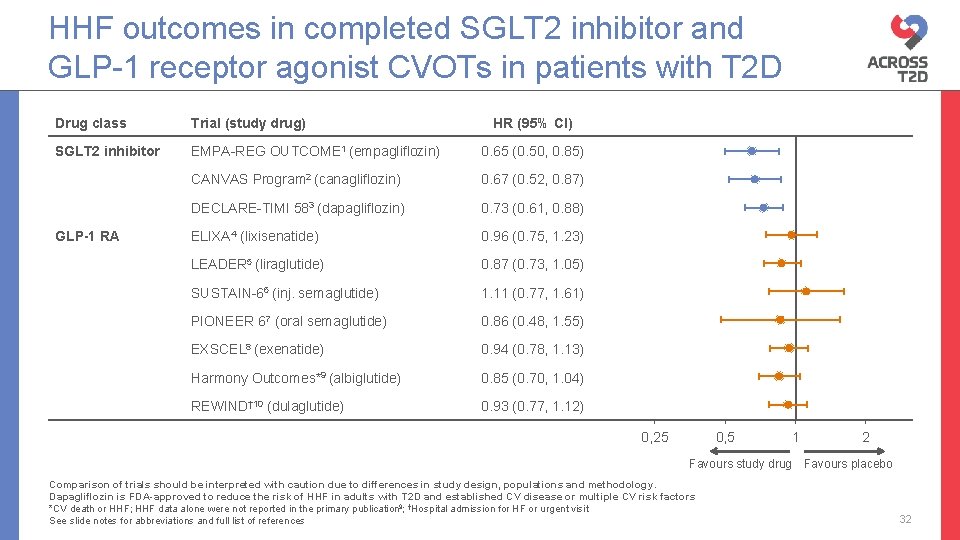
HHF outcomes in completed SGLT 2 inhibitor and GLP-1 receptor agonist CVOTs in patients with T 2 D Drug class Trial (study drug) SGLT 2 inhibitor EMPA-REG OUTCOME 1 (empagliflozin) 0. 65 (0. 50, 0. 85) CANVAS Program 2 (canagliflozin) 0. 67 (0. 52, 0. 87) DECLARE-TIMI 583 (dapagliflozin) 0. 73 (0. 61, 0. 88) ELIXA 4 (lixisenatide) 0. 96 (0. 75, 1. 23) LEADER 5 (liraglutide) 0. 87 (0. 73, 1. 05) SUSTAIN-66 (inj. semaglutide) 1. 11 (0. 77, 1. 61) PIONEER 67 (oral semaglutide) 0. 86 (0. 48, 1. 55) EXSCEL 8 (exenatide) 0. 94 (0. 78, 1. 13) Harmony Outcomes*9 (albiglutide) 0. 85 (0. 70, 1. 04) REWIND† 10 (dulaglutide) 0. 93 (0. 77, 1. 12) GLP-1 RA HR (95% CI) 0, 25 0, 5 1 Favours study drug Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology. Dapagliflozin is FDA-approved to reduce the risk of HHF in adults with T 2 D and established CV disease or multiple CV risk factors *CV death or HHF; HHF data alone were not reported in the primary publication 9; †Hospital admission for HF or urgent visit See slide notes for abbreviations and full list of references 2 Favours placebo 32
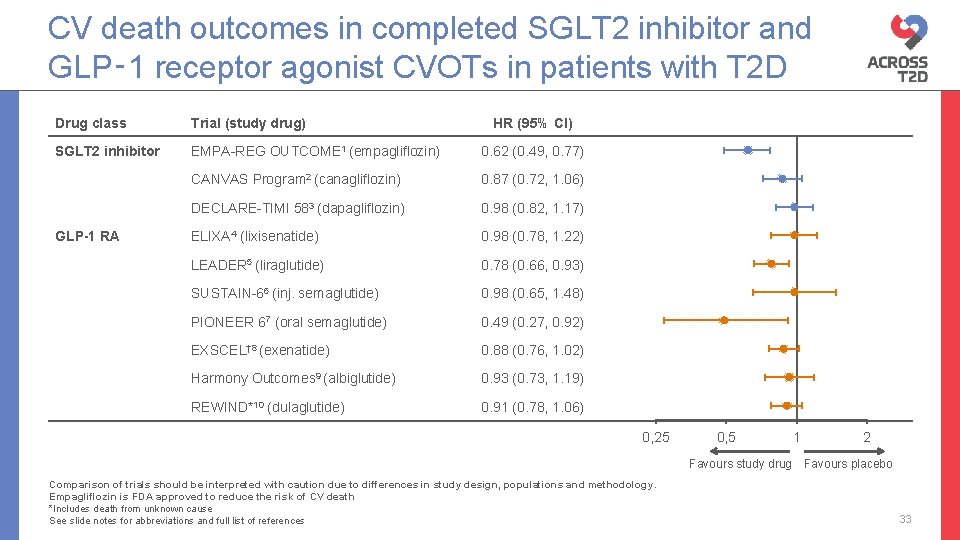
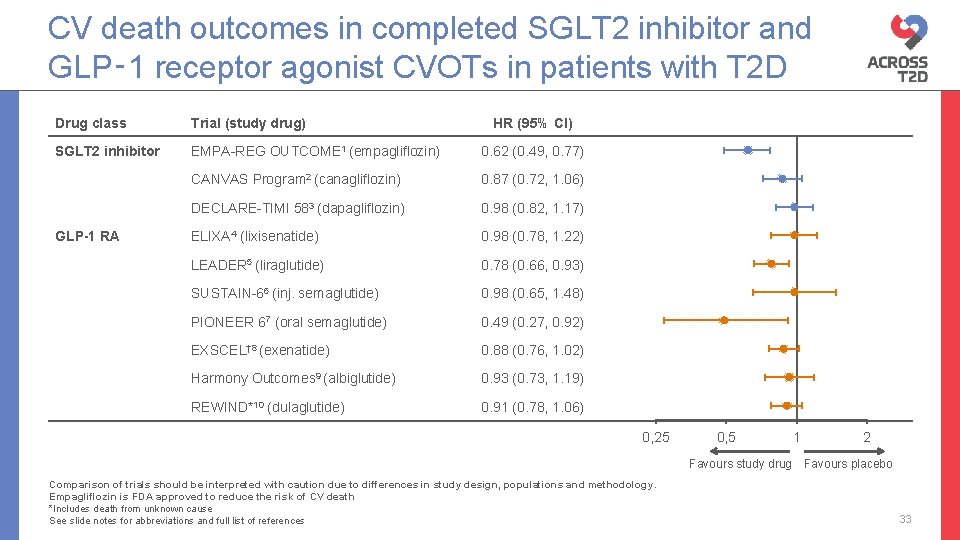
CV death outcomes in completed SGLT 2 inhibitor and GLP‑ 1 receptor agonist CVOTs in patients with T 2 D Drug class Trial (study drug) SGLT 2 inhibitor EMPA-REG OUTCOME 1 (empagliflozin) 0. 62 (0. 49, 0. 77) CANVAS Program 2 (canagliflozin) 0. 87 (0. 72, 1. 06) DECLARE-TIMI 583 (dapagliflozin) 0. 98 (0. 82, 1. 17) ELIXA 4 (lixisenatide) 0. 98 (0. 78, 1. 22) LEADER 5 (liraglutide) 0. 78 (0. 66, 0. 93) SUSTAIN-66 (inj. semaglutide) 0. 98 (0. 65, 1. 48) PIONEER 67 (oral semaglutide) 0. 49 (0. 27, 0. 92) EXSCEL† 8 (exenatide) 0. 88 (0. 76, 1. 02) Harmony Outcomes 9 (albiglutide) 0. 93 (0. 73, 1. 19) REWIND*10 (dulaglutide) 0. 91 (0. 78, 1. 06) GLP-1 RA HR (95% CI) 0, 25 0, 5 Favours study drug Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology. Empagliflozin is FDA approved to reduce the risk of CV death *Includes death from unknown cause See slide notes for abbreviations and full list of references 1 2 Favours placebo 33
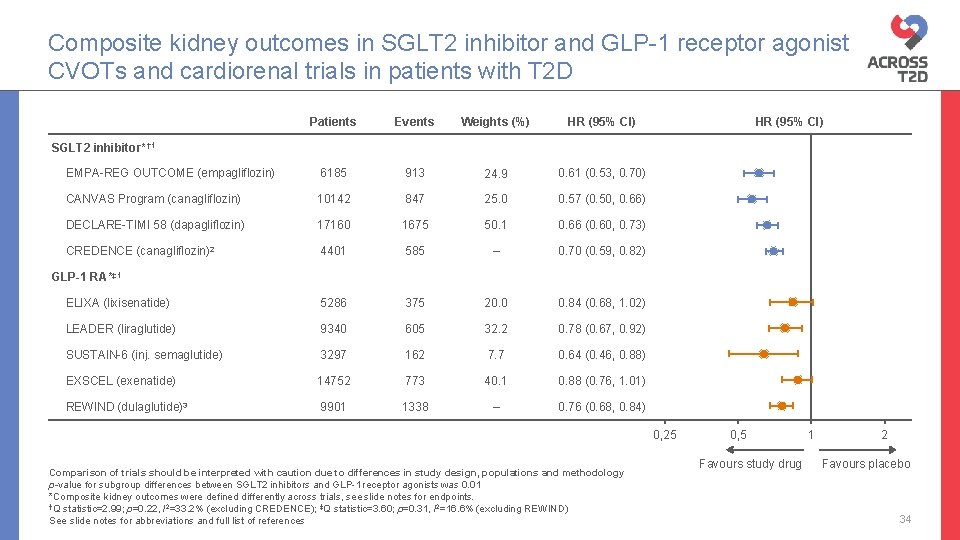
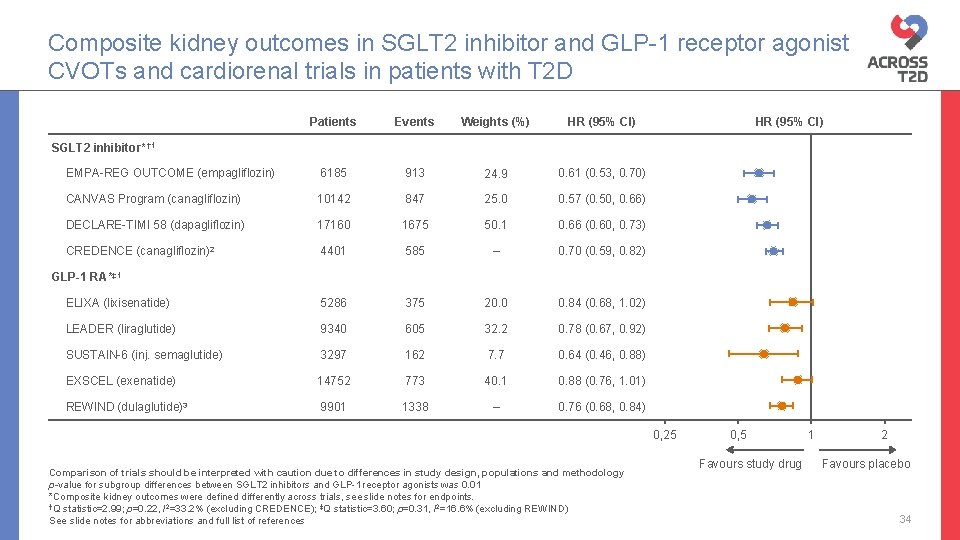
Composite kidney outcomes in SGLT 2 inhibitor and GLP-1 receptor agonist CVOTs and cardiorenal trials in patients with T 2 D Patients Events Weights (%) HR (95% CI) EMPA-REG OUTCOME (empagliflozin) 6185 913 24. 9 0. 61 (0. 53, 0. 70) CANVAS Program (canagliflozin) 10142 847 25. 0 0. 57 (0. 50, 0. 66) DECLARE-TIMI 58 (dapagliflozin) 17160 1675 50. 1 0. 66 (0. 60, 0. 73) CREDENCE (canagliflozin)2 4401 585 – 0. 70 (0. 59, 0. 82) ELIXA (lixisenatide) 5286 375 20. 0 0. 84 (0. 68, 1. 02) LEADER (liraglutide) 9340 605 32. 2 0. 78 (0. 67, 0. 92) SUSTAIN-6 (inj. semaglutide) 3297 162 7. 7 0. 64 (0. 46, 0. 88) EXSCEL (exenatide) 14752 773 40. 1 0. 88 (0. 76, 1. 01) REWIND (dulaglutide)3 9901 1338 – 0. 76 (0. 68, 0. 84) HR (95% CI) SGLT 2 inhibitor* † 1 GLP-1 RA*‡ 1 0, 25 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology p-value for subgroup differences between SGLT 2 inhibitors and GLP-1 receptor agonists was 0. 01 *Composite kidney outcomes were defined differently across trials, see slide notes for endpoints. †Q statistic=2. 99; p=0. 22, I 2=33. 2% (excluding CREDENCE); ‡Q statistic=3. 60; p=0. 31, I 2=16. 6% (excluding REWIND) See slide notes for abbreviations and full list of references 0, 5 Favours study drug 1 2 Favours placebo 34
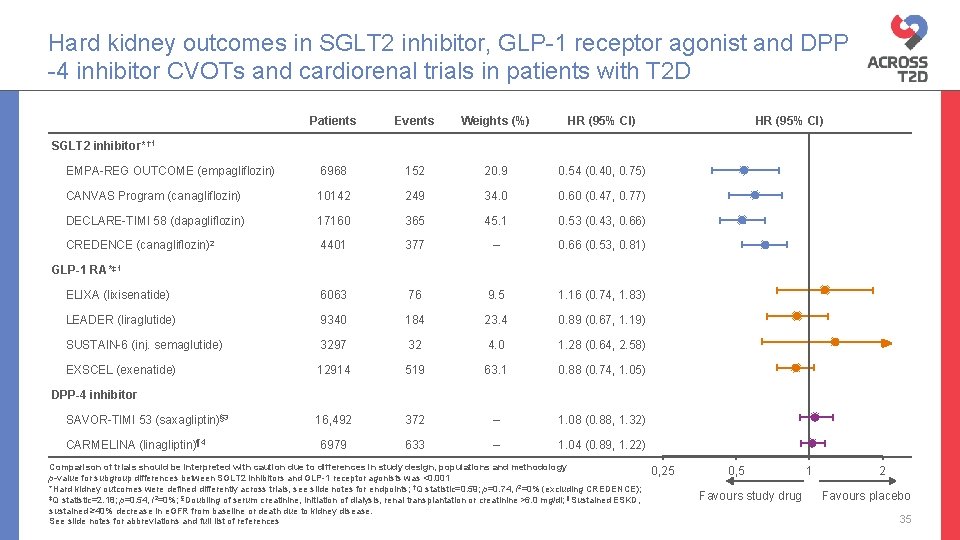
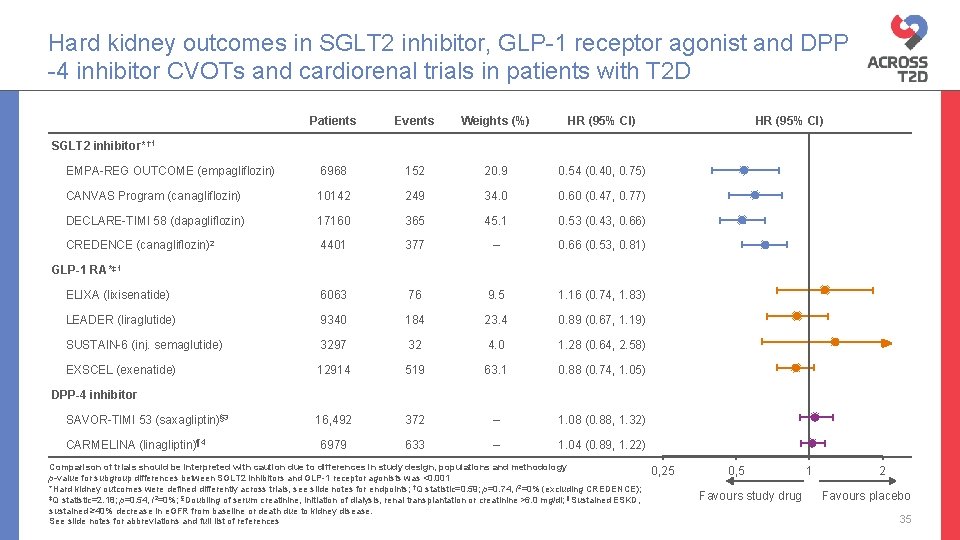
Hard kidney outcomes in SGLT 2 inhibitor, GLP-1 receptor agonist and DPP -4 inhibitor CVOTs and cardiorenal trials in patients with T 2 D Patients Events Weights (%) HR (95% CI) EMPA-REG OUTCOME (empagliflozin) 6968 152 20. 9 0. 54 (0. 40, 0. 75) CANVAS Program (canagliflozin) 10142 249 34. 0 0. 60 (0. 47, 0. 77) DECLARE-TIMI 58 (dapagliflozin) 17160 365 45. 1 0. 53 (0. 43, 0. 66) CREDENCE (canagliflozin)2 4401 377 – 0. 66 (0. 53, 0. 81) ELIXA (lixisenatide) 6063 76 9. 5 1. 16 (0. 74, 1. 83) LEADER (liraglutide) 9340 184 23. 4 0. 89 (0. 67, 1. 19) SUSTAIN-6 (inj. semaglutide) 3297 32 4. 0 1. 28 (0. 64, 2. 58) EXSCEL (exenatide) 12914 519 63. 1 0. 88 (0. 74, 1. 05) 16, 492 372 – 1. 08 (0. 88, 1. 32) 6979 633 – 1. 04 (0. 89, 1. 22) HR (95% CI) SGLT 2 inhibitor* † 1 GLP-1 RA*‡ 1 DPP-4 inhibitor SAVOR-TIMI 53 (saxagliptin)§ 3 CARMELINA (linagliptin)¶ 4 Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology p-value for subgroup differences between SGLT 2 inhibitors and GLP-1 receptor agonists was <0. 001 *Hard kidney outcomes were defined differently across trials, see slide notes for endpoints; †Q statistic=0. 59; p=0. 74, I 2=0% (excluding CREDENCE); ‡Q statistic=2. 18; p=0. 54, I 2=0%; §Doubling of serum creatinine, initiation of dialysis, renal transplantation or creatinine >6. 0 mg/dl; ¶Sustained ESKD, sustained ≥ 40% decrease in e. GFR from baseline or death due to kidney disease. See slide notes for abbreviations and full list of references 0, 25 0, 5 Favours study drug 1 2 Favours placebo 35
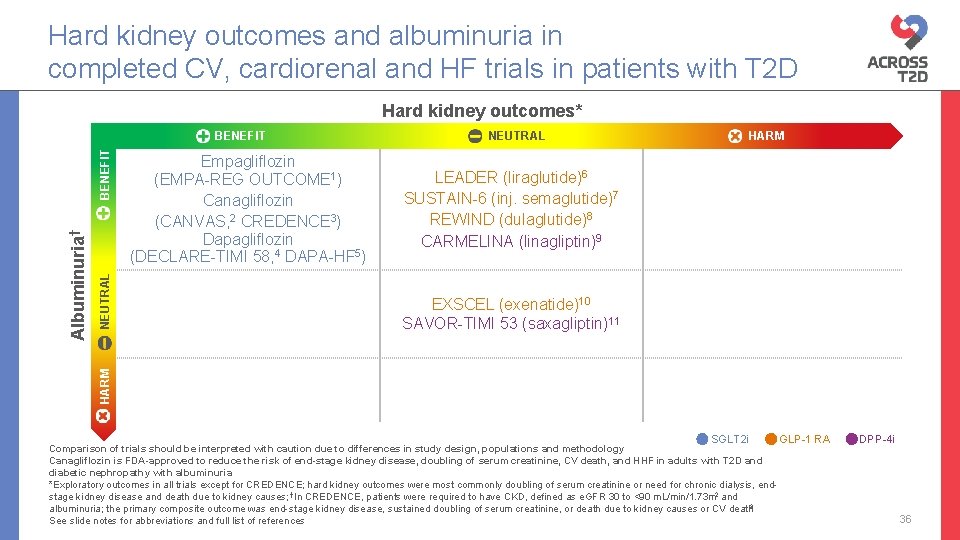
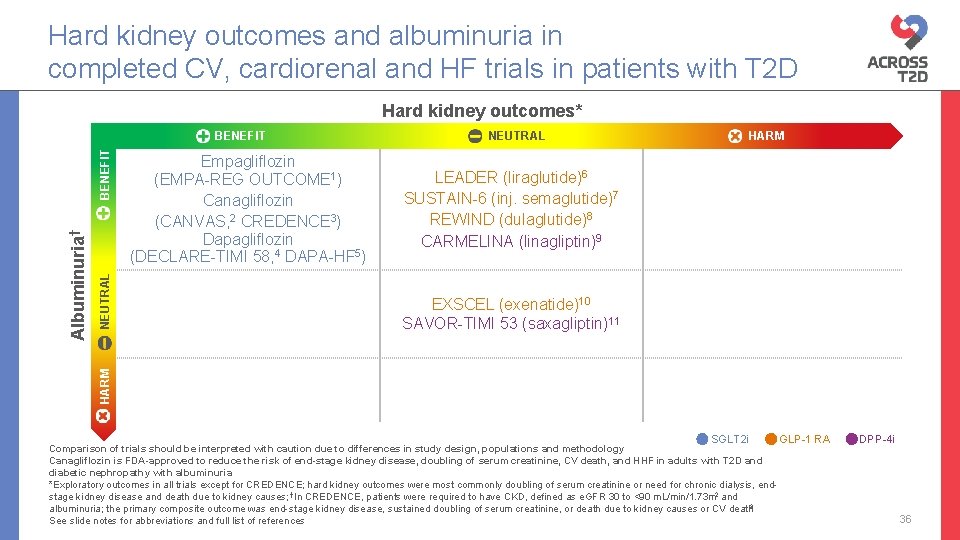
Hard kidney outcomes and albuminuria in completed CV, cardiorenal and HF trials in patients with T 2 D Hard kidney outcomes* NEUTRAL Empagliflozin (EMPA-REG OUTCOME 1) Canagliflozin (CANVAS, 2 CREDENCE 3) Dapagliflozin (DECLARE-TIMI 58, 4 DAPA-HF 5) NEUTRAL HARM LEADER (liraglutide)6 SUSTAIN-6 (inj. semaglutide)7 REWIND (dulaglutide)8 CARMELINA (linagliptin)9 EXSCEL (exenatide)10 SAVOR-TIMI 53 (saxagliptin)11 HARM Albuminuria† BENEFIT SGLT 2 i Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology Canagliflozin is FDA-approved to reduce the risk of end-stage kidney disease, doubling of serum creatinine, CV death, and HHF in adults with T 2 D and diabetic nephropathy with albuminuria *Exploratory outcomes in all trials except for CREDENCE; hard kidney outcomes were most commonly doubling of serum creatinine or need for chronic dialysis, endstage kidney disease and death due to kidney causes; †In CREDENCE, patients were required to have CKD, defined as e. GFR 30 to <90 m. L/min/1. 73 m 2 and albuminuria; the primary composite outcome was end-stage kidney disease, sustained doubling of serum creatinine, or death due to kidney causes or CV death 3 See slide notes for abbreviations and full list of references GLP-1 RA DPP-4 i 36
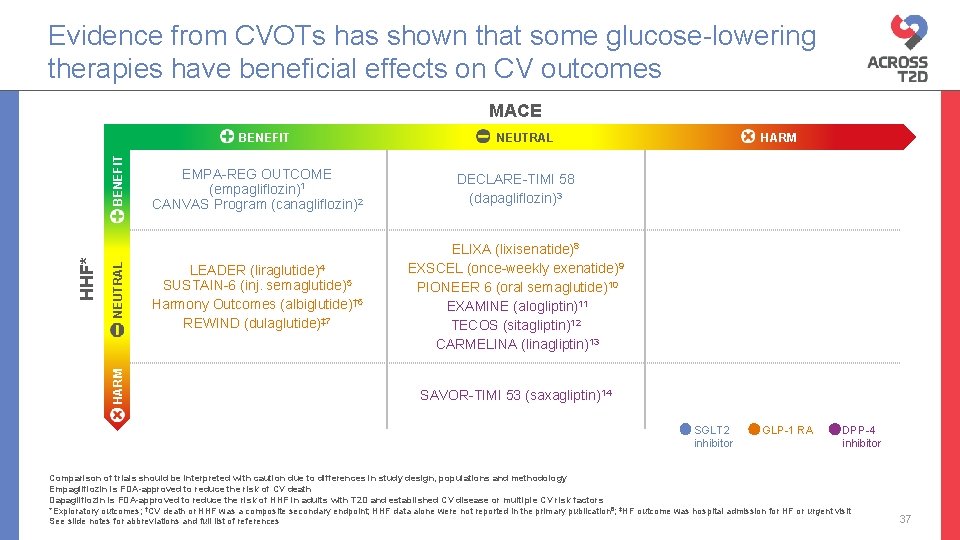
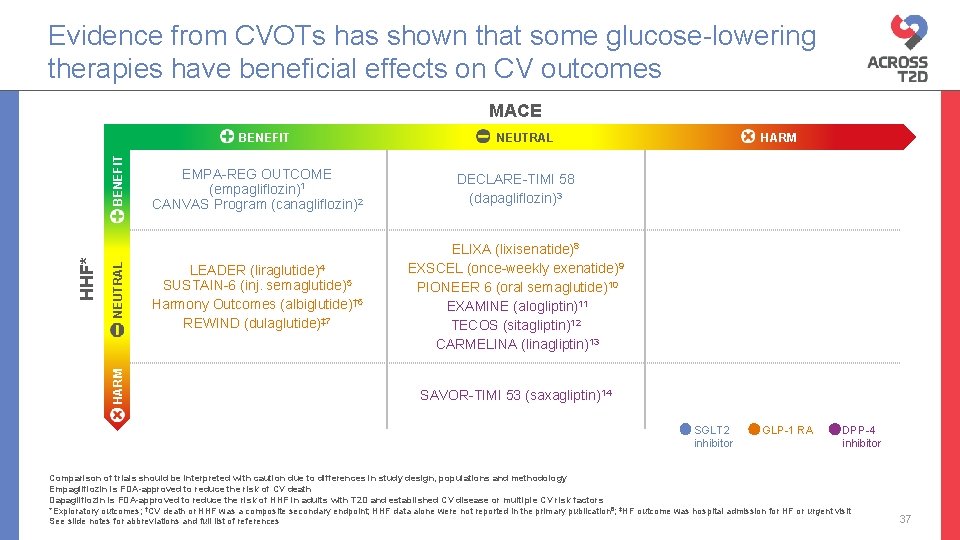
Evidence from CVOTs has shown that some glucose-lowering therapies have beneficial effects on CV outcomes MACE NEUTRAL HARM HHF* BENEFIT NEUTRAL EMPA-REG OUTCOME (empagliflozin)1 CANVAS Program (canagliflozin)2 DECLARE-TIMI 58 (dapagliflozin)3 LEADER (liraglutide)4 SUSTAIN-6 (inj. semaglutide)5 Harmony Outcomes (albiglutide)† 6 REWIND (dulaglutide)‡ 7 ELIXA (lixisenatide)8 EXSCEL (once-weekly exenatide)9 PIONEER 6 (oral semaglutide)10 EXAMINE (alogliptin)11 TECOS (sitagliptin)12 CARMELINA (linagliptin)13 HARM SAVOR-TIMI 53 (saxagliptin)14 SGLT 2 inhibitor GLP-1 RA DPP-4 inhibitor Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology Empagliflozin is FDA-approved to reduce the risk of CV death Dapagliflozin is FDA-approved to reduce the risk of HHF in adults with T 2 D and established CV disease or multiple CV risk factors *Exploratory outcomes; †CV death or HHF was a composite secondary endpoint; HHF data alone were not reported in the primary publication 6; ‡HF outcome was hospital admission for HF or urgent visit See slide notes for abbreviations and full list of references 37
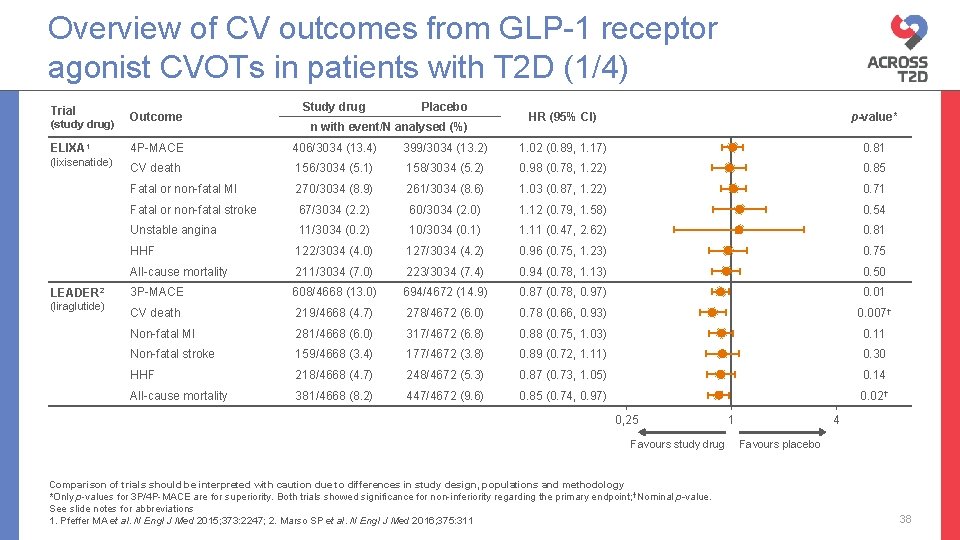
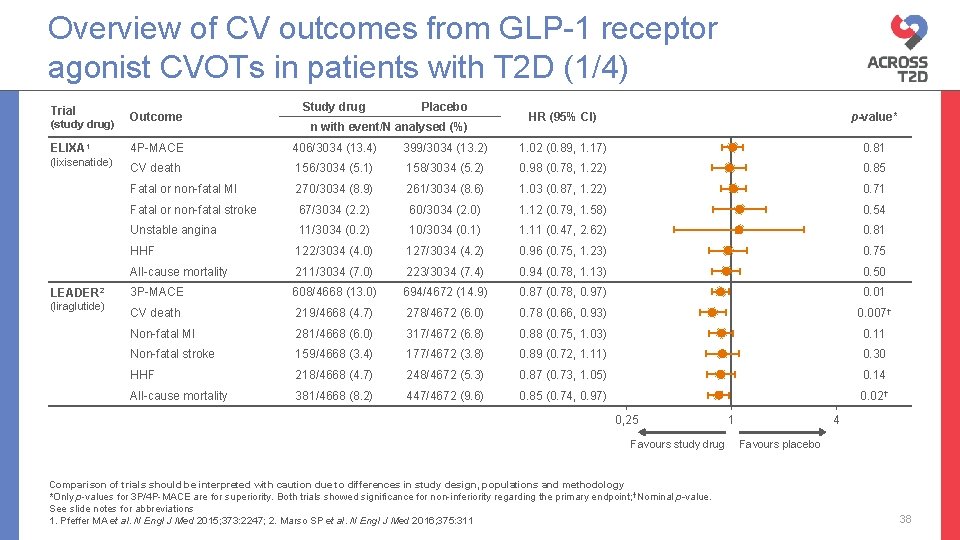
Overview of CV outcomes from GLP-1 receptor agonist CVOTs in patients with T 2 D (1/4) Trial (study drug) ELIXA 1 (lixisenatide) LEADER 2 (liraglutide) Outcome Study drug Placebo n with event/N analysed (%) HR (95% CI) p-value* 4 P-MACE 406/3034 (13. 4) 399/3034 (13. 2) 1. 02 (0. 89, 1. 17) 0. 81 CV death 156/3034 (5. 1) 158/3034 (5. 2) 0. 98 (0. 78, 1. 22) 0. 85 Fatal or non-fatal MI 270/3034 (8. 9) 261/3034 (8. 6) 1. 03 (0. 87, 1. 22) 0. 71 Fatal or non-fatal stroke 67/3034 (2. 2) 60/3034 (2. 0) 1. 12 (0. 79, 1. 58) 0. 54 Unstable angina 11/3034 (0. 2) 10/3034 (0. 1) 1. 11 (0. 47, 2. 62) 0. 81 HHF 122/3034 (4. 0) 127/3034 (4. 2) 0. 96 (0. 75, 1. 23) 0. 75 All-cause mortality 211/3034 (7. 0) 223/3034 (7. 4) 0. 94 (0. 78, 1. 13) 0. 50 3 P-MACE 608/4668 (13. 0) 694/4672 (14. 9) 0. 87 (0. 78, 0. 97) 0. 01 CV death 219/4668 (4. 7) 278/4672 (6. 0) 0. 78 (0. 66, 0. 93) 0. 007† Non-fatal MI 281/4668 (6. 0) 317/4672 (6. 8) 0. 88 (0. 75, 1. 03) 0. 11 Non-fatal stroke 159/4668 (3. 4) 177/4672 (3. 8) 0. 89 (0. 72, 1. 11) 0. 30 HHF 218/4668 (4. 7) 248/4672 (5. 3) 0. 87 (0. 73, 1. 05) 0. 14 All-cause mortality 381/4668 (8. 2) 447/4672 (9. 6) 0. 85 (0. 74, 0. 97) 0. 02† 0, 25 Favours study drug Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Only p-values for 3 P/4 P-MACE are for superiority. Both trials showed significance for non-inferiority regarding the primary endpoint; †Nominal p-value. See slide notes for abbreviations 1. Pfeffer MA et al. N Engl J Med 2015; 373: 2247; 2. Marso SP et al. N Engl J Med 2016; 375: 311 1 4 Favours placebo 38
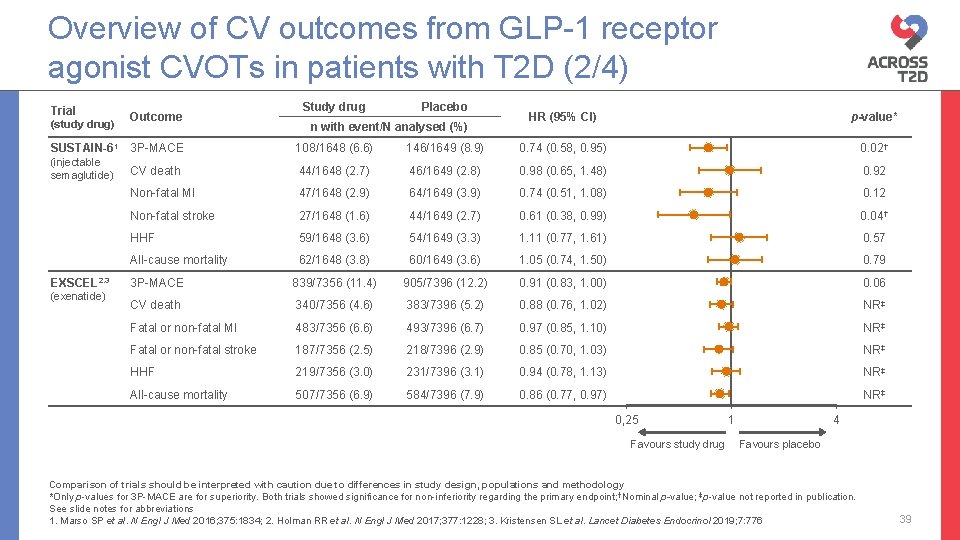
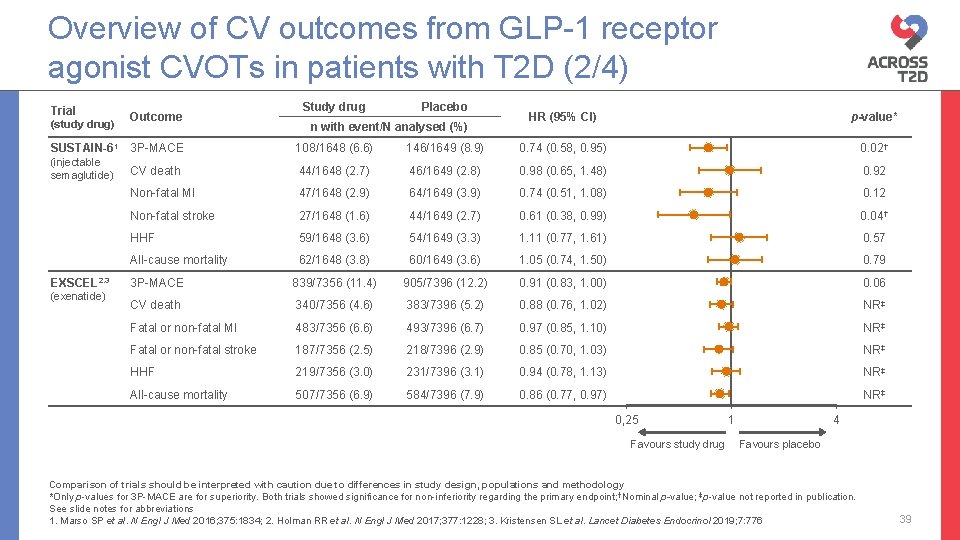
Overview of CV outcomes from GLP-1 receptor agonist CVOTs in patients with T 2 D (2/4) Trial (study drug) Outcome SUSTAIN-61 3 P-MACE (injectable semaglutide) EXSCEL 2, 3 (exenatide) Study drug Placebo n with event/N analysed (%) HR (95% CI) p-value* 108/1648 (6. 6) 146/1649 (8. 9) 0. 74 (0. 58, 0. 95) 0. 02† CV death 44/1648 (2. 7) 46/1649 (2. 8) 0. 98 (0. 65, 1. 48) 0. 92 Non-fatal MI 47/1648 (2. 9) 64/1649 (3. 9) 0. 74 (0. 51, 1. 08) 0. 12 Non-fatal stroke 27/1648 (1. 6) 44/1649 (2. 7) 0. 61 (0. 38, 0. 99) 0. 04† HHF 59/1648 (3. 6) 54/1649 (3. 3) 1. 11 (0. 77, 1. 61) 0. 57 All-cause mortality 62/1648 (3. 8) 60/1649 (3. 6) 1. 05 (0. 74, 1. 50) 0. 79 3 P-MACE 839/7356 (11. 4) 905/7396 (12. 2) 0. 91 (0. 83, 1. 00) 0. 06 CV death 340/7356 (4. 6) 383/7396 (5. 2) 0. 88 (0. 76, 1. 02) NR‡ Fatal or non-fatal MI 483/7356 (6. 6) 493/7396 (6. 7) 0. 97 (0. 85, 1. 10) NR‡ Fatal or non-fatal stroke 187/7356 (2. 5) 218/7396 (2. 9) 0. 85 (0. 70, 1. 03) NR‡ HHF 219/7356 (3. 0) 231/7396 (3. 1) 0. 94 (0. 78, 1. 13) NR‡ All-cause mortality 507/7356 (6. 9) 584/7396 (7. 9) 0. 86 (0. 77, 0. 97) NR‡ 0, 25 Favours study drug 1 4 Favours placebo Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Only p-values for 3 P-MACE are for superiority. Both trials showed significance for non-inferiority regarding the primary endpoint; †Nominal p-value; ‡p-value not reported in publication. See slide notes for abbreviations 1. Marso SP et al. N Engl J Med 2016; 375: 1834; 2. Holman RR et al. N Engl J Med 2017; 377: 1228; 3. Kristensen SL et al. Lancet Diabetes Endocrinol 2019; 7: 776 39
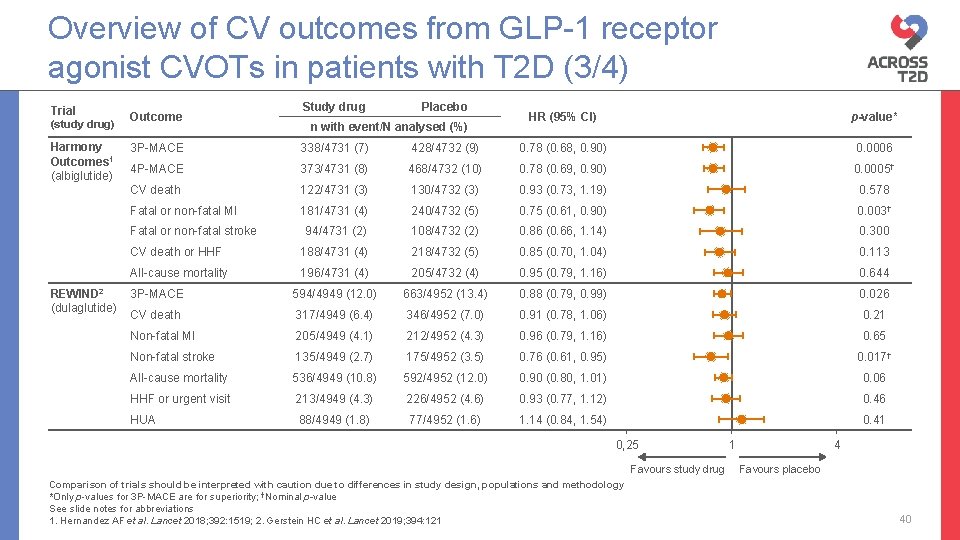
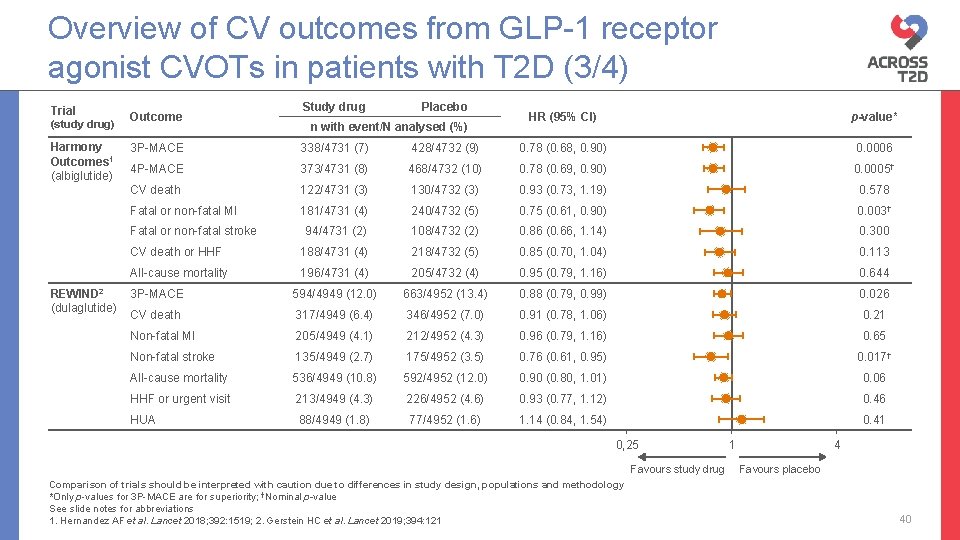
Overview of CV outcomes from GLP-1 receptor agonist CVOTs in patients with T 2 D (3/4) Trial (study drug) Harmony Outcomes 1 (albiglutide) Outcome Placebo n with event/N analysed (%) HR (95% CI) p-value* 3 P-MACE 338/4731 (7) 428/4732 (9) 0. 78 (0. 68, 0. 90) 0. 0006 4 P-MACE 373/4731 (8) 468/4732 (10) 0. 78 (0. 69, 0. 90) 0. 0005† CV death 122/4731 (3) 130/4732 (3) 0. 93 (0. 73, 1. 19) 0. 578 Fatal or non-fatal MI 181/4731 (4) 240/4732 (5) 0. 75 (0. 61, 0. 90) 0. 003† 94/4731 (2) 108/4732 (2) 0. 86 (0. 66, 1. 14) 0. 300 CV death or HHF 188/4731 (4) 218/4732 (5) 0. 85 (0. 70, 1. 04) 0. 113 All-cause mortality 196/4731 (4) 205/4732 (4) 0. 95 (0. 79, 1. 16) 0. 644 3 P-MACE 594/4949 (12. 0) 663/4952 (13. 4) 0. 88 (0. 79, 0. 99) 0. 026 CV death 317/4949 (6. 4) 346/4952 (7. 0) 0. 91 (0. 78, 1. 06) 0. 21 Non-fatal MI 205/4949 (4. 1) 212/4952 (4. 3) 0. 96 (0. 79, 1. 16) 0. 65 Non-fatal stroke 135/4949 (2. 7) 175/4952 (3. 5) 0. 76 (0. 61, 0. 95) 0. 017† All-cause mortality 536/4949 (10. 8) 592/4952 (12. 0) 0. 90 (0. 80, 1. 01) 0. 06 HHF or urgent visit 213/4949 (4. 3) 226/4952 (4. 6) 0. 93 (0. 77, 1. 12) 0. 46 HUA 88/4949 (1. 8) 77/4952 (1. 6) 1. 14 (0. 84, 1. 54) 0. 41 Fatal or non-fatal stroke REWIND 2 (dulaglutide) Study drug 0, 25 Favours study drug Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *Only p-values for 3 P-MACE are for superiority; †Nominal p-value See slide notes for abbreviations 1. Hernandez AF et al. Lancet 2018; 392: 1519; 2. Gerstein HC et al. Lancet 2019; 394: 121 1 4 Favours placebo 40
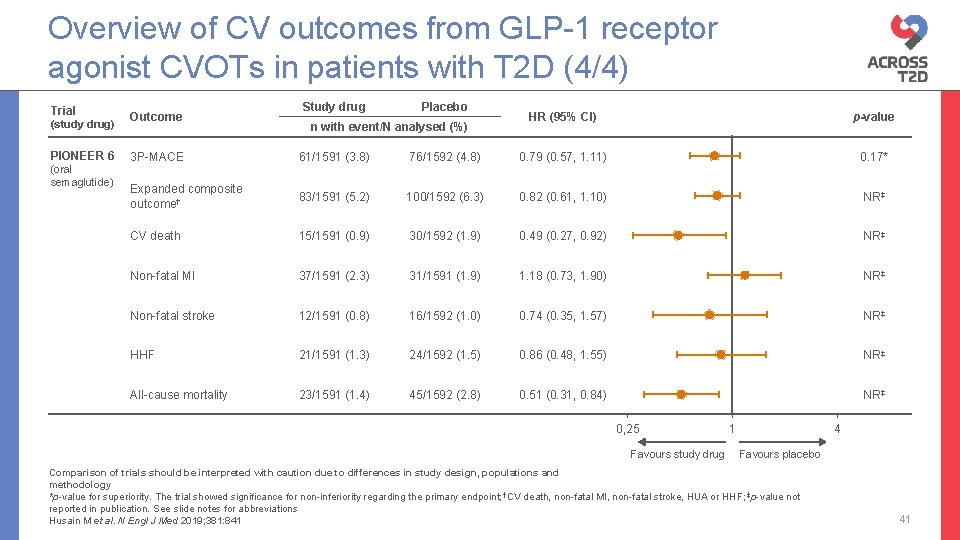
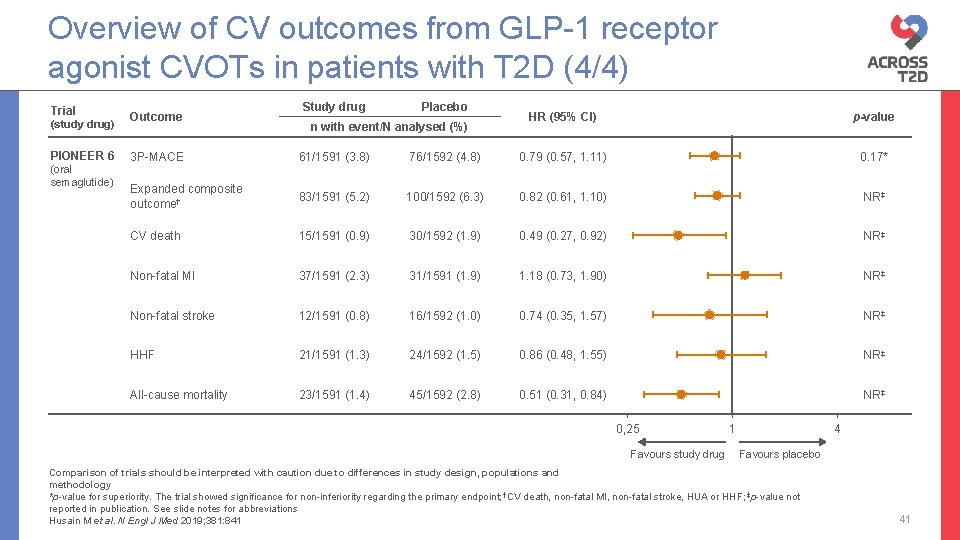
Overview of CV outcomes from GLP-1 receptor agonist CVOTs in patients with T 2 D (4/4) Trial (study drug) PIONEER 6 (oral semaglutide) Outcome Study drug Placebo n with event/N analysed (%) HR (95% CI) p-value 3 P-MACE 61/1591 (3. 8) 76/1592 (4. 8) 0. 79 (0. 57, 1. 11) 0. 17* Expanded composite outcome† 83/1591 (5. 2) 100/1592 (6. 3) 0. 82 (0. 61, 1. 10) NR‡ CV death 15/1591 (0. 9) 30/1592 (1. 9) 0. 49 (0. 27, 0. 92) NR‡ Non-fatal MI 37/1591 (2. 3) 31/1591 (1. 9) 1. 18 (0. 73, 1. 90) NR‡ Non-fatal stroke 12/1591 (0. 8) 16/1592 (1. 0) 0. 74 (0. 35, 1. 57) NR‡ HHF 21/1591 (1. 3) 24/1592 (1. 5) 0. 86 (0. 48, 1. 55) NR‡ All-cause mortality 23/1591 (1. 4) 45/1592 (2. 8) 0. 51 (0. 31, 0. 84) NR‡ 0, 25 Favours study drug 1 4 Favours placebo Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology *p-value for superiority. The trial showed significance for non-inferiority regarding the primary endpoint; †CV death, non-fatal MI, non-fatal stroke, HUA or HHF; ‡p-value not reported in publication. See slide notes for abbreviations Husain M et al. N Engl J Med 2019; 381: 841 41
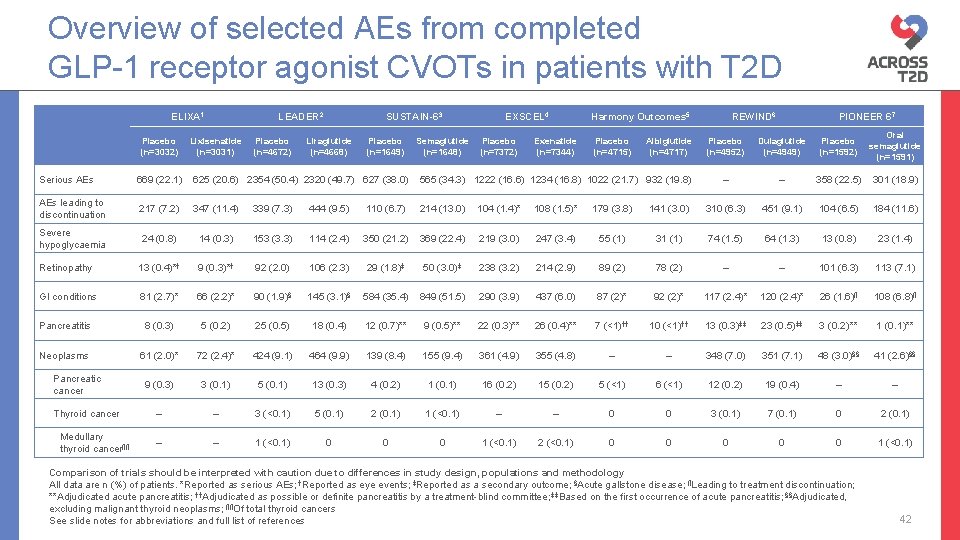
Overview of selected AEs from completed GLP-1 receptor agonist CVOTs in patients with T 2 D ELIXA 1 Placebo (n=3032) LEADER 2 Lixisenatide (n=3031) Placebo (n=4672) SUSTAIN-63 Liraglutide (n=4668) Placebo (n=1649) Semaglutide (n=1648) EXSCEL 4 Placebo (n=7372) Harmony Outcomes 5 Exenatide (n=7344) Placebo (n=4715) Albiglutide (n=4717) REWIND 6 PIONEER 67 Placebo (n=4952) Dulaglutide (n=4949) Placebo (n=1592) Oral semaglutide (n=1591) – – 358 (22. 5) 301 (18. 9) Serious AEs 669 (22. 1) 625 (20. 6) 2354 (50. 4) 2320 (49. 7) 627 (38. 0) 565 (34. 3) 1222 (16. 6) 1234 (16. 8) 1022 (21. 7) 932 (19. 8) AEs leading to discontinuation 217 (7. 2) 347 (11. 4) 339 (7. 3) 444 (9. 5) 110 (6. 7) 214 (13. 0) 104 (1. 4)* 108 (1. 5)* 179 (3. 8) 141 (3. 0) 310 (6. 3) 451 (9. 1) 104 (6. 5) 184 (11. 6) Severe hypoglycaemia 24 (0. 8) 14 (0. 3) 153 (3. 3) 114 (2. 4) 350 (21. 2) 369 (22. 4) 219 (3. 0) 247 (3. 4) 55 (1) 31 (1) 74 (1. 5) 64 (1. 3) 13 (0. 8) 23 (1. 4) Retinopathy 13 (0. 4)*† 9 (0. 3)*† 92 (2. 0) 106 (2. 3) 29 (1. 8)‡ 50 (3. 0)‡ 238 (3. 2) 214 (2. 9) 89 (2) 78 (2) – – 101 (6. 3) 113 (7. 1) GI conditions 81 (2. 7)* 66 (2. 2)* 90 (1. 9)§ 145 (3. 1)§ 584 (35. 4) 849 (51. 5) 290 (3. 9) 437 (6. 0) 87 (2)* 92 (2)* 117 (2. 4)* 120 (2. 4)* 26 (1. 6)¶ 108 (6. 8)¶ Pancreatitis 8 (0. 3) 5 (0. 2) 25 (0. 5) 18 (0. 4) 12 (0. 7)** 9 (0. 5)** 22 (0. 3)** 26 (0. 4)** 7 (<1)†† 10 (<1)†† 13 (0. 3)‡‡ 23 (0. 5)‡‡ 3 (0. 2)** 1 (0. 1)** Neoplasms 61 (2. 0)* 72 (2. 4)* 424 (9. 1) 464 (9. 9) 139 (8. 4) 155 (9. 4) 361 (4. 9) 355 (4. 8) – – 348 (7. 0) 351 (7. 1) 48 (3. 0)§§ 41 (2. 6)§§ 9 (0. 3) 3 (0. 1) 5 (0. 1) 13 (0. 3) 4 (0. 2) 1 (0. 1) 16 (0. 2) 15 (0. 2) 5 (<1) 6 (<1) 12 (0. 2) 19 (0. 4) – – 3 (<0. 1) 5 (0. 1) 2 (0. 1) 1 (<0. 1) – – 0 0 3 (0. 1) 7 (0. 1) 0 2 (0. 1) – – 1 (<0. 1) 0 0 0 1 (<0. 1) 2 (<0. 1) 0 0 0 1 (<0. 1) Pancreatic cancer Thyroid cancer Medullary thyroid cancer¶¶ Comparison of trials should be interpreted with caution due to differences in study design, populations and methodology All data are n (%) of patients. *Reported as serious AEs; †Reported as eye events; ‡Reported as a secondary outcome; §Acute gallstone disease; ¶Leading to treatment discontinuation; **Adjudicated acute pancreatitis; ††Adjudicated as possible or definite pancreatitis by a treatment-blind committee; ‡‡Based on the first occurrence of acute pancreatitis; §§Adjudicated, excluding malignant thyroid neoplasms; ¶¶Of total thyroid cancers See slide notes for abbreviations and full list of references 42
 Dpp4 vs glp1
Dpp4 vs glp1 Cl channel
Cl channel Indirect acting cholinergic drugs
Indirect acting cholinergic drugs Direct-acting cholinergic drugs
Direct-acting cholinergic drugs Witch
Witch Ndsu corn variety trials
Ndsu corn variety trials Dhl atyrau
Dhl atyrau Drug development timeline
Drug development timeline York trials unit
York trials unit Japanese bridging studies
Japanese bridging studies Nida clinical trial network
Nida clinical trial network Ccea
Ccea Clinical trials.gov login
Clinical trials.gov login How is the crucible unlike the salem witch trials?
How is the crucible unlike the salem witch trials? Hercules wife
Hercules wife Hawk irb
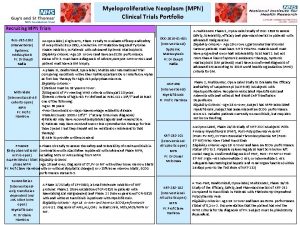
Hawk irb Mpn clinical trials
Mpn clinical trials Role of statistician in clinical trials
Role of statistician in clinical trials Repeated bernoulli trials
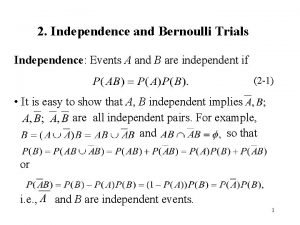
Repeated bernoulli trials Ohsu clinical trials office
Ohsu clinical trials office Clinical hysteria salem witch trials
Clinical hysteria salem witch trials What caused the salem witch trial hysteria of 1692 dbq
What caused the salem witch trial hysteria of 1692 dbq Clinical trials quality by design
Clinical trials quality by design Andrew nunn
Andrew nunn Malta football trials
Malta football trials Do these situations involve bernoulli trials
Do these situations involve bernoulli trials Strom thurmond apush
Strom thurmond apush Salem witch trials rebecca nurse
Salem witch trials rebecca nurse Future search trials
Future search trials Clinical trials
Clinical trials The six trials of jesus
The six trials of jesus Salem witch trials discovery education
Salem witch trials discovery education Pediatric trials network
Pediatric trials network Poe trials
Poe trials Design and analysis of cross-over trials
Design and analysis of cross-over trials Salem witch trials facts
Salem witch trials facts Many kids called unfit for adult trials
Many kids called unfit for adult trials Clinical trials
Clinical trials Site initiation visit powerpoint presentation
Site initiation visit powerpoint presentation Korean bridging phase 1 trials
Korean bridging phase 1 trials Iwr clinical research
Iwr clinical research Professor claire harrison
Professor claire harrison Clinicaltrials gov api
Clinicaltrials gov api