ASD Dr H Sadeghian 1 ASD ostium secondum
- Slides: 52
ASD Dr. H. Sadeghian
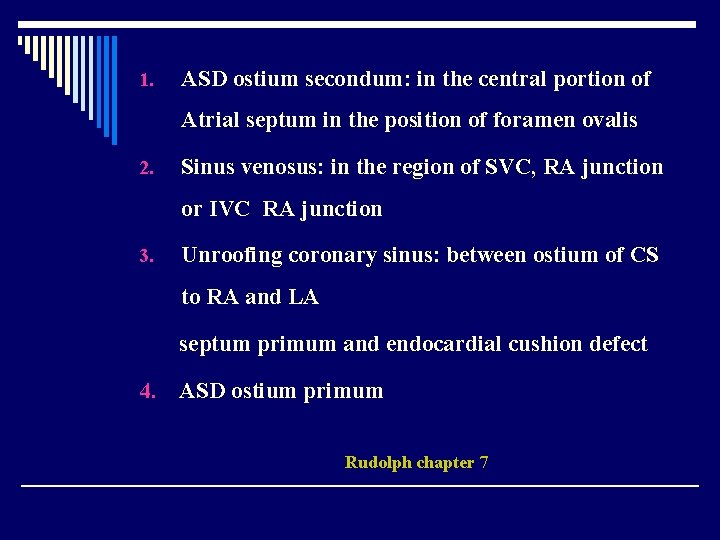
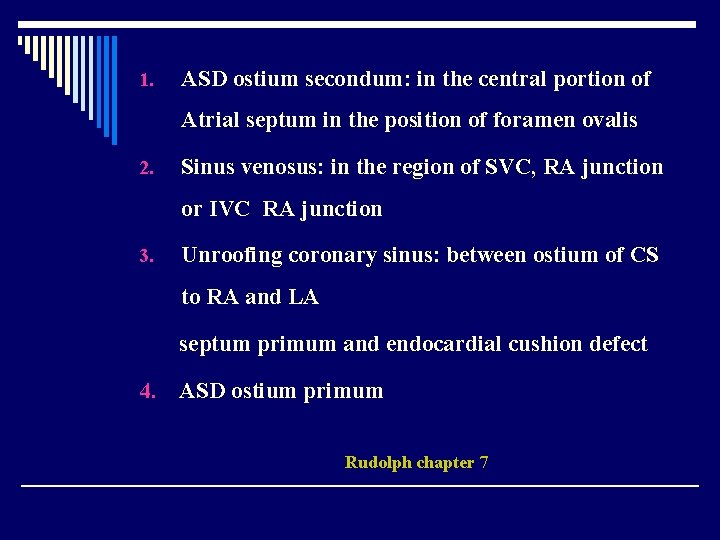
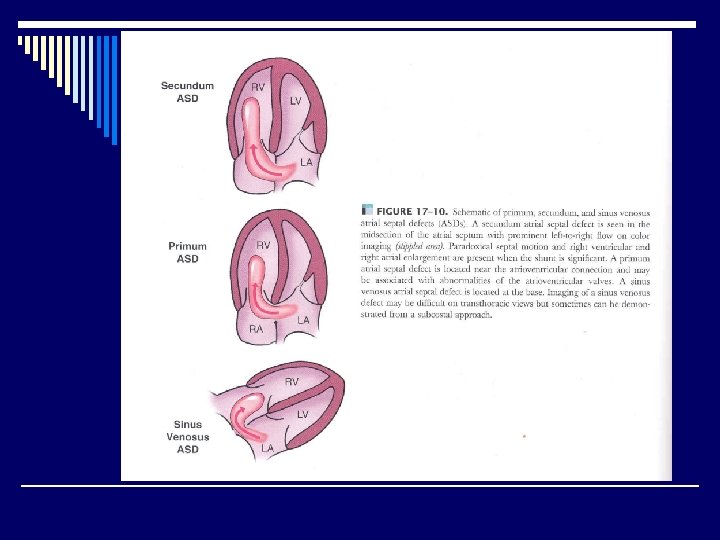
1. ASD ostium secondum: in the central portion of Atrial septum in the position of foramen ovalis 2. Sinus venosus: in the region of SVC, RA junction or IVC RA junction 3. Unroofing coronary sinus: between ostium of CS to RA and LA septum primum and endocardial cushion defect 4. ASD ostium primum Rudolph chapter 7
Sinus venosus : 3 – 10% ASD ostiom serondun: more common F / M = 2/1 5% ASD + PS (valvuler) Muller, chapter 22
PVR abn < 10% As. D ostium secondum almost always ASD SV Associates PVRAb Braunwald
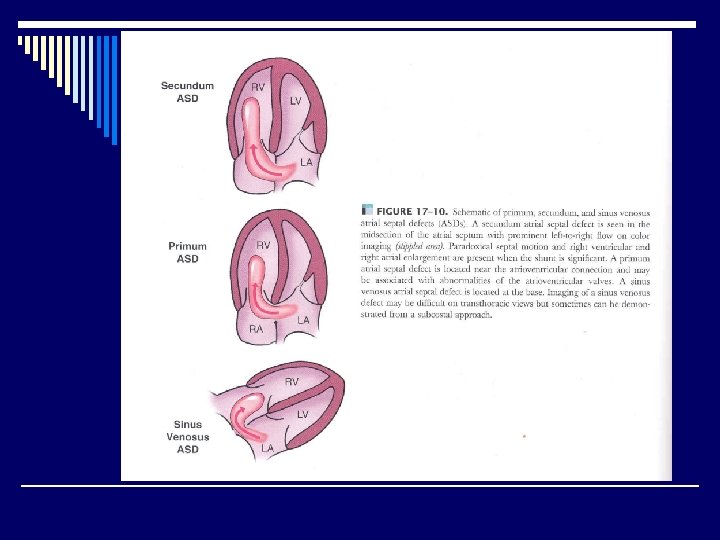
Morphologic and Embriologic considerations Septum primum grows from posterosuperior side (SVC side) toward A-V junction where endocardial cushion separotes Atria from ventricles. The lower part of the septum primum is completed by fusion with endocardial cushion tissue. Rudolph chapter 7
Some fenestrations develop in midportion of septum primum. Septum secrodum just grows in the posterosuperior portion of IAS (near SVC) but right to the septum primum. It grows toward the AV junction and it partly covers the central hole of septum prinum. It has a semilunar edge which is concave toward TV. Rudolph chapter 7
Ostium secondum defects 1. Large hole in septum primum or 2. Inadequite development of septum secondum Rudolph chapter 7
1. Sinus venosus defects: septum primum or secondum 2. Unroofing CS: the well between CS and LA, may involved a portion of septum or whole septum and are frequently associated with LPSVC Rudolph chapter 7
LAP 1 -2 mm. Hg >RAP two ventricles fill with one pressure so RV will be distended. Rudolph chapter 7
The degree of left to right Shout depends on the 1 - The size of the defect 2 - Filling pressure of ventricles Braunwald
Infants Large defects: QP/Qs > 2. 5 : 1 Produce symptoms Medium size defects: do not cause symptoms during infancy and early childhood Rudolph chapter 7
ASD beyond infancy The majority of children even those with large defeats do not experience symptoms. Unlike VSD most of them tend to be smaller with growing, ASD usually grows in proportion to heart size and there is evidence suggesting that some defects may become larger as age increase. Rudolph chapter 7
40% ASDs in infants will close spontonously ASD < 3 mm in first 3 months always close ASD > 8 mm is unlikely to close Muller, chapter 22
Spontanous closure of ASD may occur within the 1 year of life. < 7 mm in neonatal period may reduce in size and require no intervention Braunwald
Natural history of growth of ASD ostiun secondum and implication Heart 2002, 87, 256 -9
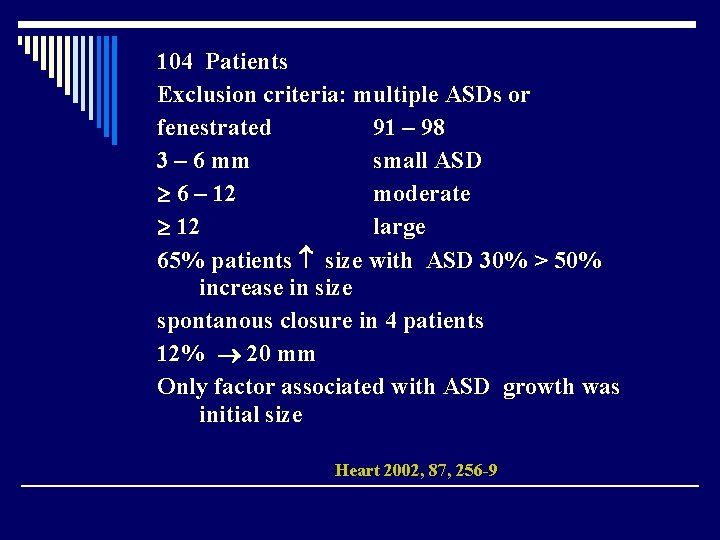
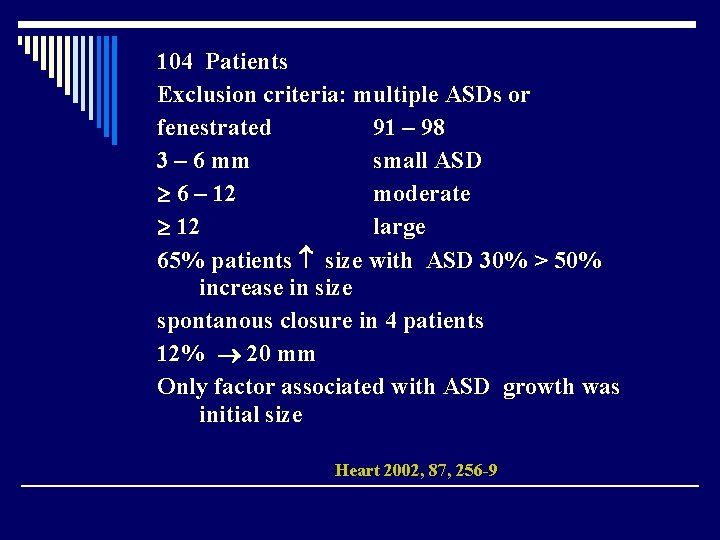
104 Patients Exclusion criteria: multiple ASDs or fenestrated 91 – 98 3 – 6 mm small ASD 6 – 12 moderate 12 large 65% patients size with ASD 30% > 50% increase in size spontanous closure in 4 patients 12% 20 mm Only factor associated with ASD growth was initial size Heart 2002, 87, 256 -9
ASD growth was independent of age of patients Conclusion: 2/3 of ASDs growth with time Heart 2002, 87, 256 -9
Defects < 6 mm 66% spontanous closure Mean age of diagnosis: 4. 5 years F / M / 2. 2/1 Heart 2002, 87, 256 -9
Small ASD group 33% had small defects(34 P) FO 3 p closed spontounsly 26% (27 p) ASD 1 small mod 3 small large 1. 6 mm/y size Mean FO : 3. 2 y Heart 2002, 87, 256 -9
Mod ASD group 40 p (38%) FO 31% mod 3 small 8 large 1. 6 mm/y mean FO: 3. 3 y Heart 2002, 87, 256 -9
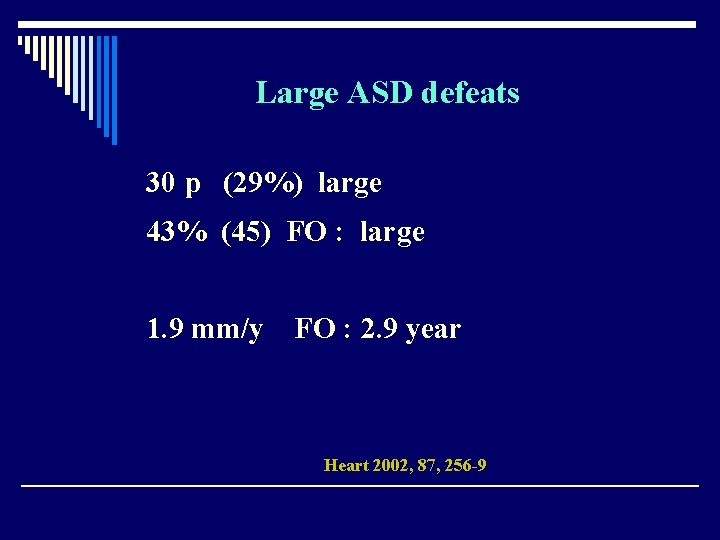
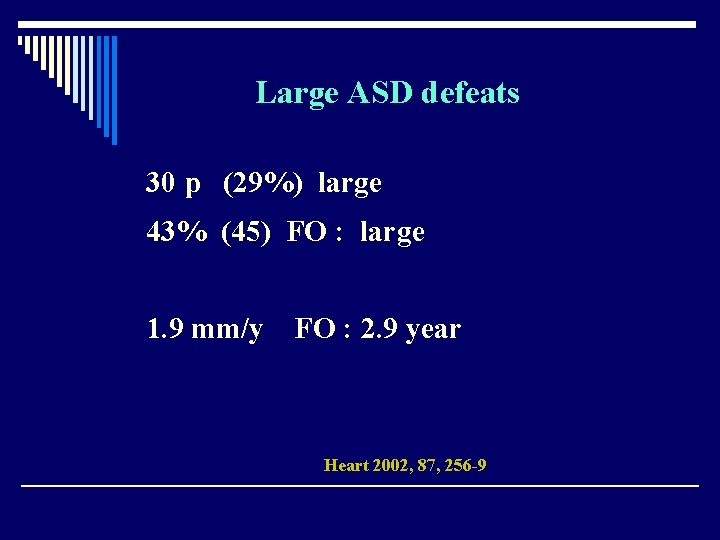
Large ASD defeats 30 p (29%) large 43% (45) FO : large 1. 9 mm/y FO : 2. 9 year Heart 2002, 87, 256 -9
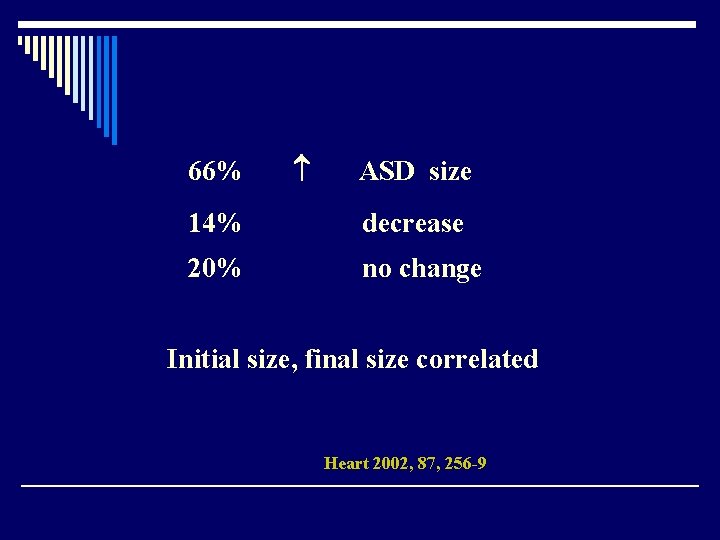
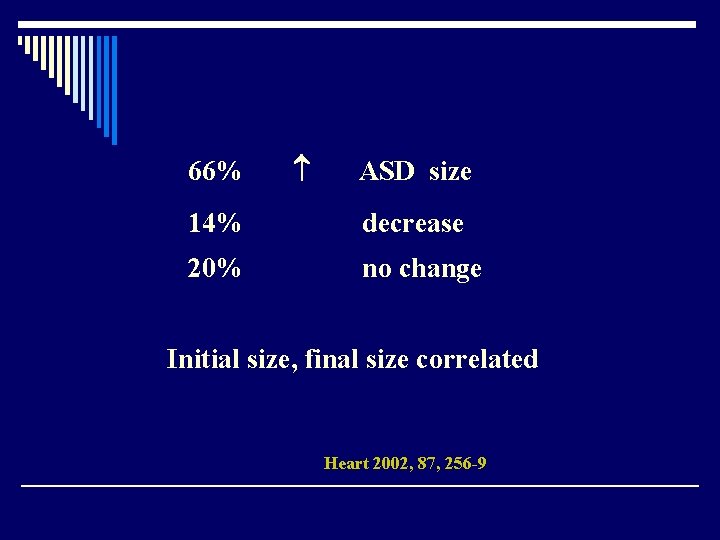
66% ASD size 14% decrease 20% no change Initial size, final size correlated Heart 2002, 87, 256 -9
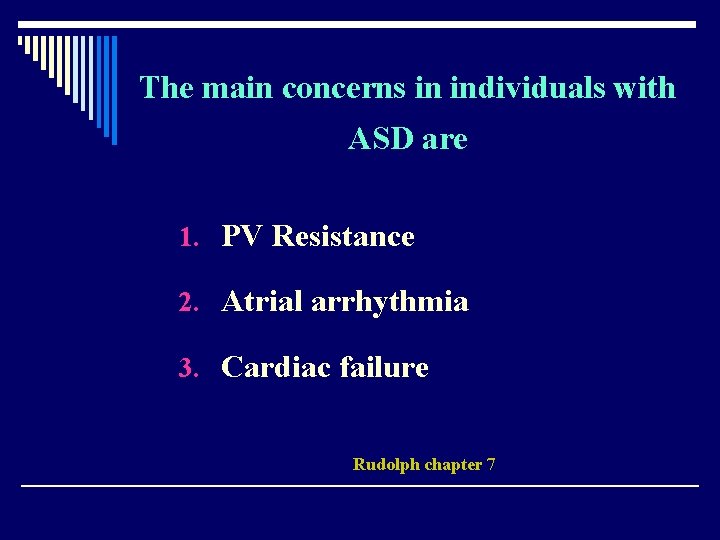
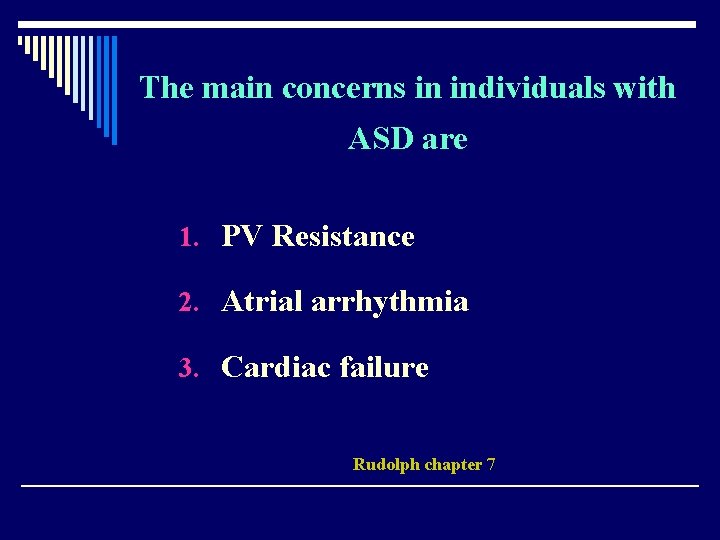
The main concerns in individuals with ASD are 1. PV Resistance 2. Atrial arrhythmia 3. Cardiac failure Rudolph chapter 7
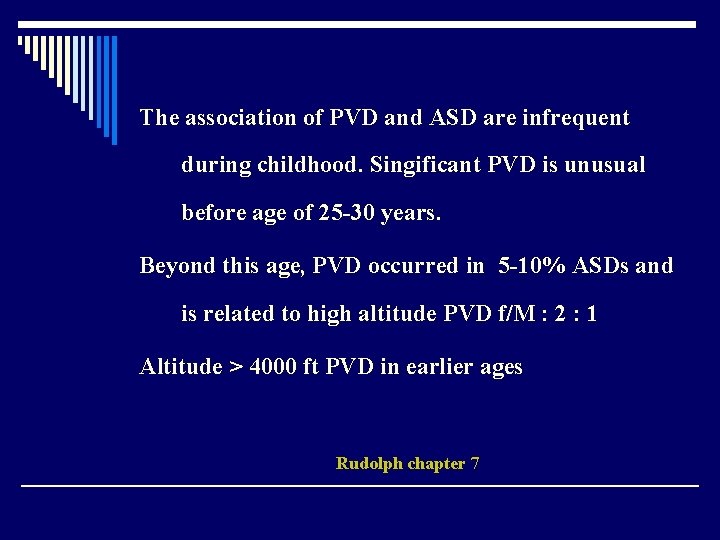
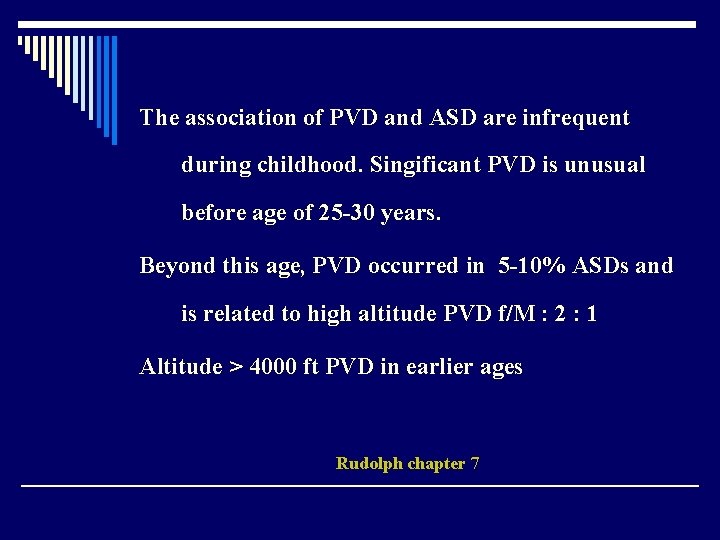
The association of PVD and ASD are infrequent during childhood. Singificant PVD is unusual before age of 25 -30 years. Beyond this age, PVD occurred in 5 -10% ASDs and is related to high altitude PVD f/M : 2 : 1 Altitude > 4000 ft PVD in earlier ages Rudolph chapter 7
PVR in ASD usually is normal , 1 unit / m 2 3 considerable Rudolph chapter 7
Atrial arrhythmia Af , Flutter , PAT occurs commonly in older patients. They are probably related to large shunts. < 20 y 1 - 2% > 20 y 15 - 50% Rudolph chapter 7
Cardiac failure >20 y , Right sided Failure Rudolph chapter 7
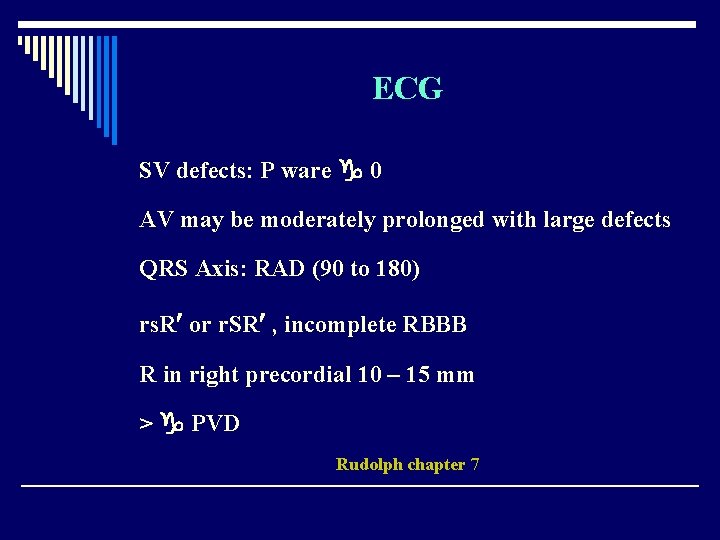
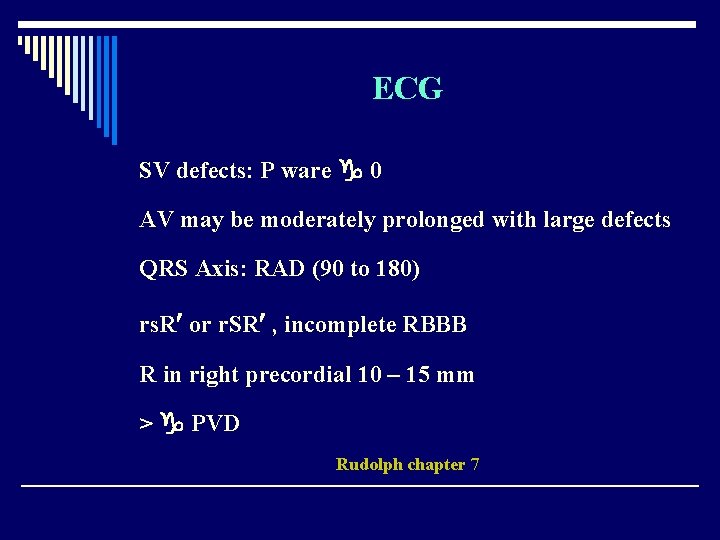
ECG SV defects: P ware 0 AV may be moderately prolonged with large defects QRS Axis: RAD (90 to 180) rs. R or r. SR , incomplete RBBB R in right precordial 10 – 15 mm > PVD Rudolph chapter 7
Negative P in Inferior leads ASD SV below SVC Braunwald
Echo 1. RV Enlargement 2. QP/QS 3. PVR , SVR 4. PAP , TR , PAPm , d 5. RV function Rudolph chapter 7
Subcostal : bicaval
Pressures 15 – 30 mm. Hg Pressure RV-PA 10 – 15 mm. Hg MPA , branches Rudolph chapter 7
30% of the patients have effort dyspnea in third decade and more than 73% by fifth decade Braunwald
SV arrhythmia and RSF 10%> 40 y Paradoxical embolic may occur Braunwald
Cyanosis 1 - Isenmenger 2 - Prominent eustachien valve which leads IVC flow to ASD 3 - ASD SV below IVC Braunwald
Management Large ASD QP/Qs < 2 : 1 QP/QS < 1. 5 : 1 Follow up Rudolph chapter 7
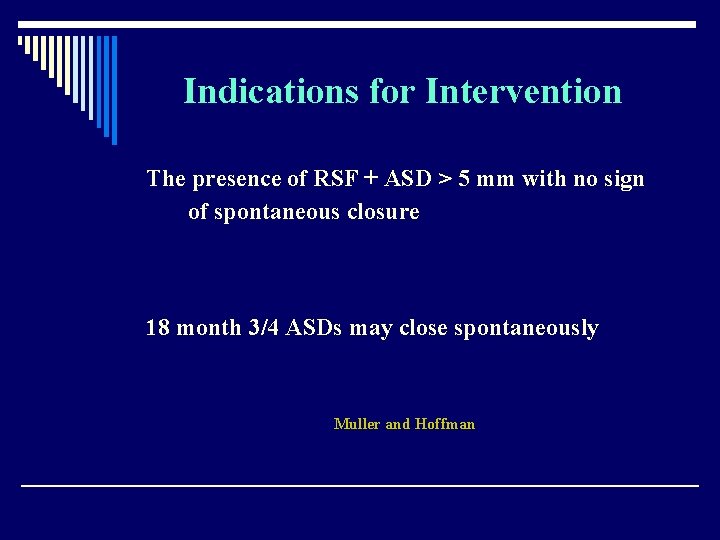
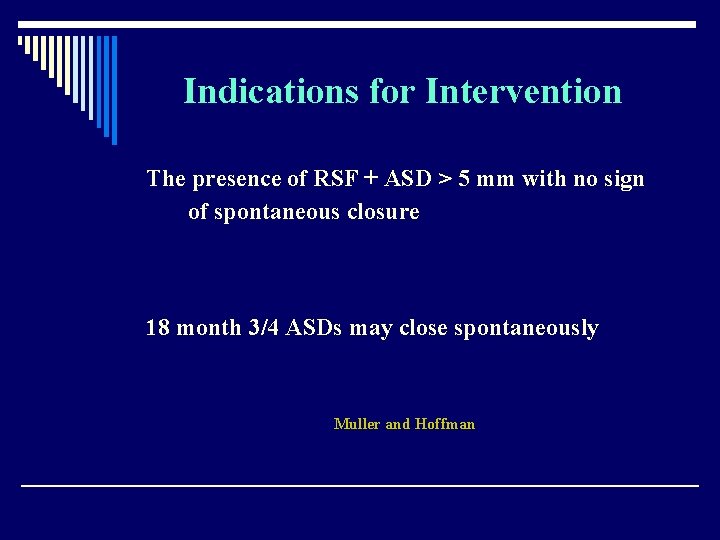
Indications for Intervention The presence of RSF + ASD > 5 mm with no sign of spontaneous closure 18 month 3/4 ASDs may close spontaneously Muller and Hoffman
QP QS < 1. 5 : don’t want Closure except for paradoxical emboli Braunwald
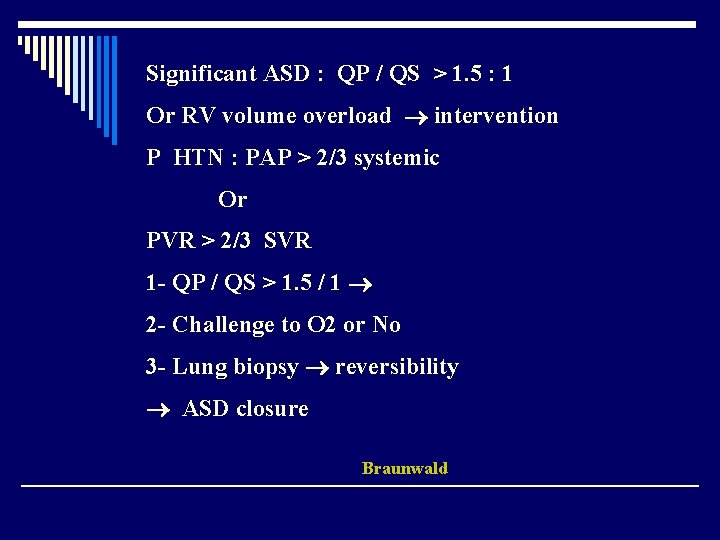
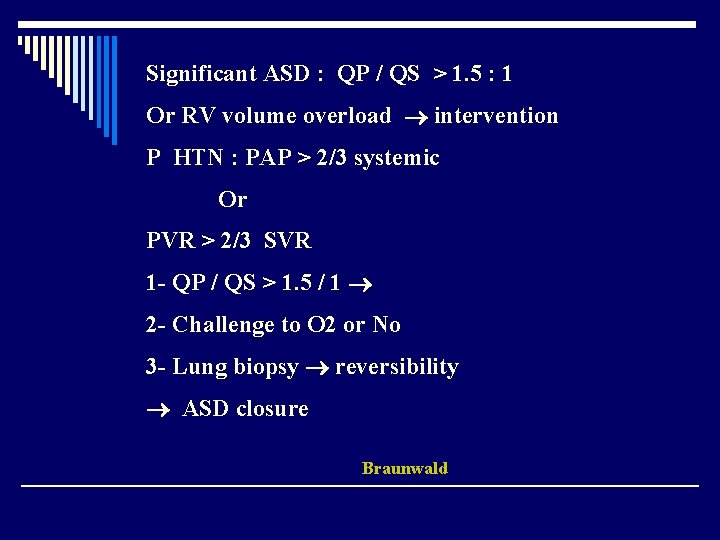
Significant ASD : QP / QS > 1. 5 : 1 Or RV volume overload intervention P HTN : PAP > 2/3 systemic Or PVR > 2/3 SVR 1 - QP / QS > 1. 5 / 1 2 - Challenge to O 2 or No 3 - Lung biopsy reversibility ASD closure Braunwald
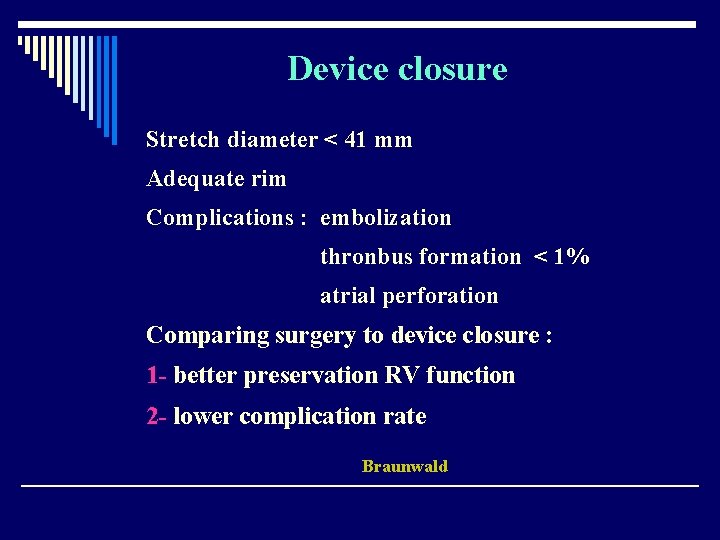
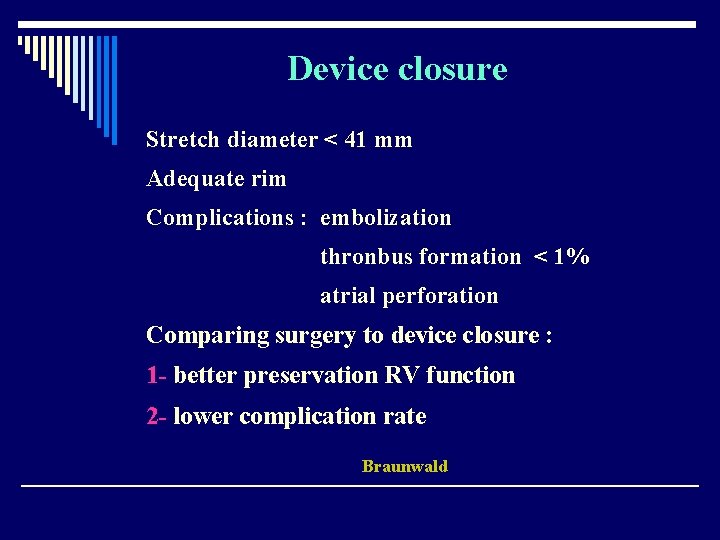
Device closure Stretch diameter < 41 mm Adequate rim Complications : embolization thronbus formation < 1% atrial perforation Comparing surgery to device closure : 1 - better preservation RV function 2 - lower complication rate Braunwald
Surgery - Sinus venosus - Ostium primum - Ostium serondum not suitable for device closure Mortality < 1% Braunwald
ASD with P HTN PVR > 8 – 12 unit / m 2 : high mortality PVR > 12 unit / m 2 FO PVR 4 – 8 unit / m 2 mortality 10% Rudolph chapter 7
After device closure - Aspirin 6 mouths - Prophylaxis of IE 6 mouths Braunwald
Long surveillance 1 - ASD SV : Caval or PV stenosis 2 - RV Failure 3 - Atrial arrhythmia Braunwald
< 10% ASD PHTN PPHTN in association with ASD > 50% patients > 45 y AF Muller, chapter 22
Post op Atrial arrhythmia Soon after surgery to later years 30 – 50% incidence PAT , AF and flutter but brady-tachy arrhythmia pace Transcatheter closure incidence arrhythmia? Rudolph chapter 7
AF 25% patients > 20 y 5% patients < 20 y Late post operative arrhythmia : 2 - 9 % children 2 - 33% adults Early after repair : 14% Atrial arrhthmia espicially in SV defects Muller
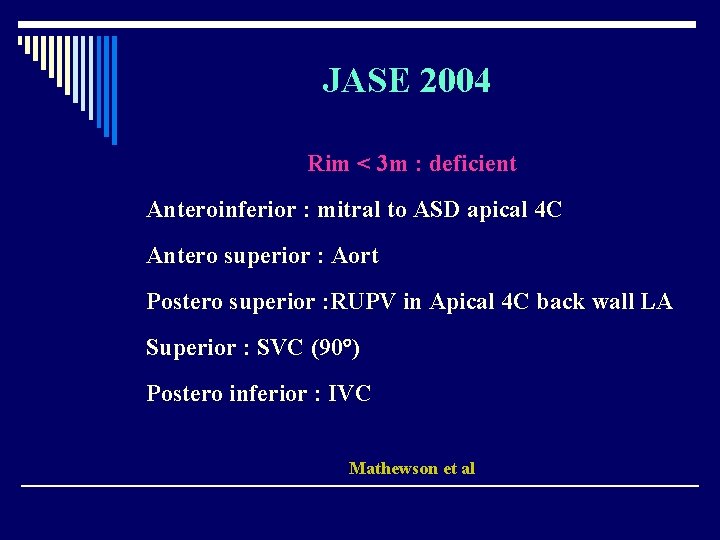
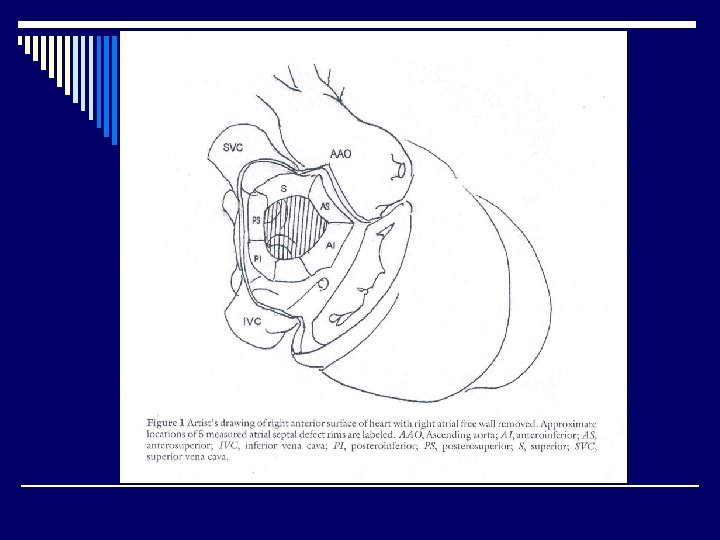
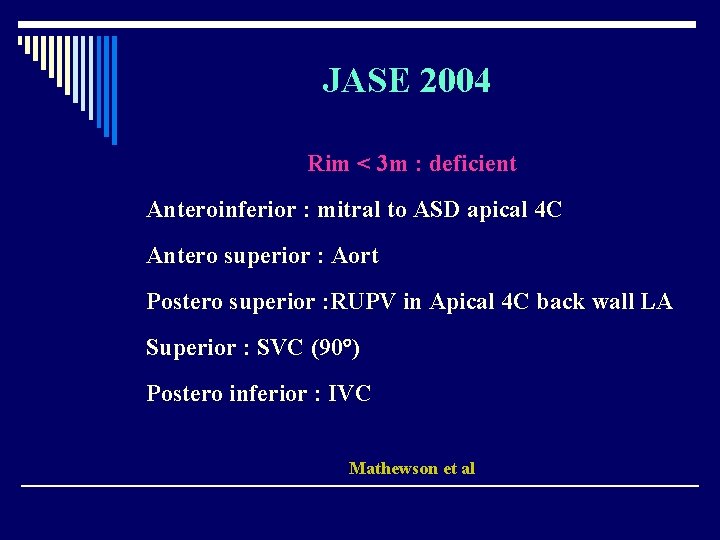
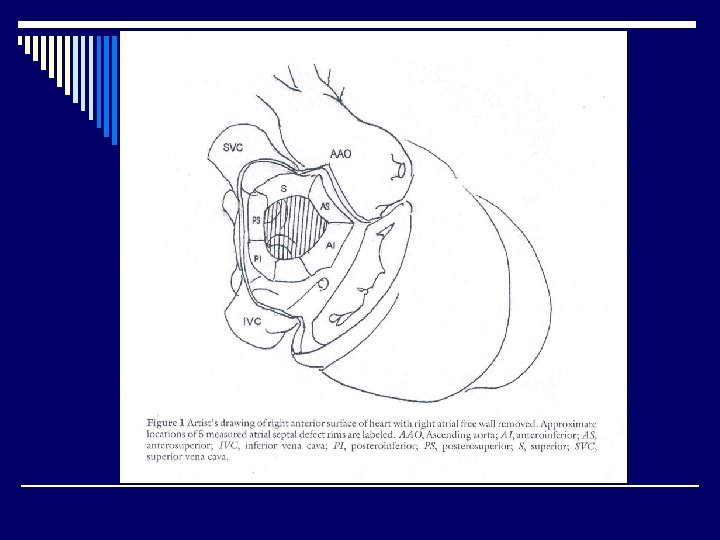
JASE 2004 Rim < 3 m : deficient Anteroinferior : mitral to ASD apical 4 C Antero superior : Aort Postero superior : RUPV in Apical 4 C back wall LA Superior : SVC (90 ) Postero inferior : IVC Mathewson et al