SECOND HEART SOUND Dr SHAJUDEEN K DM Cardiology


























- Slides: 90
SECOND HEART SOUND Dr SHAJUDEEN. K DM Cardiology Resident Calicut Medical college

History • “S 2 is the key to auscultation” : Aubrey Leathem • Respiratory variation first described by Potain (1866) • Term “Hangout interval” coined by shaver

Genesis of S 2 • During systole blood flow from LV to Aorta & RV to PA. Once pressure in the great vessels becomes more than corresponding ventricle and hang out interval is over, blood flow reverses , this retrograde flow is stopped suddenly by semilunar valves when the elastic limits of the tensed leaflets are met during closure of valves
• This causes vibrations in the cardiohemic system. High frequency generated from this vibration is the Second heart sound.

Timing Of S 2

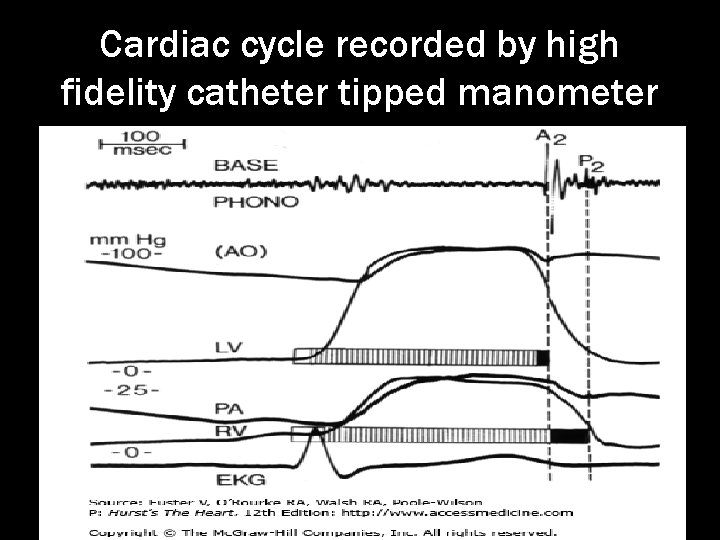
Hang out interval • It is the time interval from the crossover of the pressure between RV and PA or LV and Aorta during the ejection phase of systole to the actual closure of the Pulmonary or Aortic valve respectively.
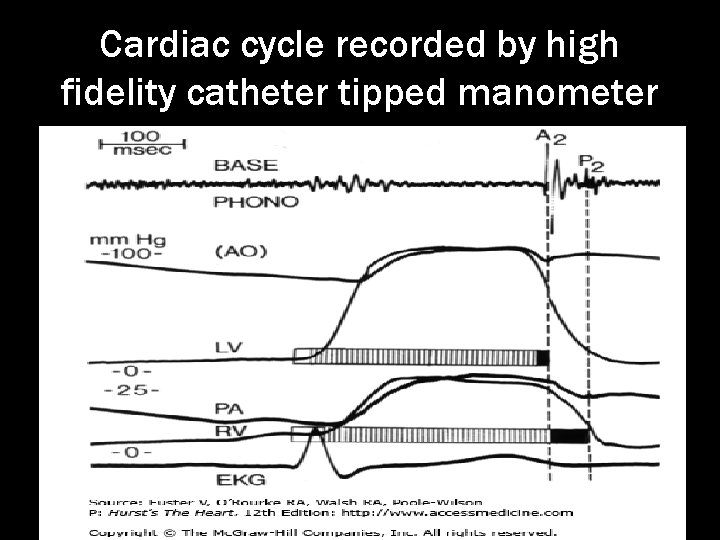
Cardiac cycle recorded by high fidelity catheter tipped manometer

Normal values of Hangout intervals • Pulmonary circulation: 43 -86 msec • Systemic circulation : < 15 msec • ie Pulmonary hangout interval >Systemic
Factors influencing the duration of Hangout interval • Pressure in the arteries • Vascular resistance • Compliance of Vessels
• Aorta is a higher pressure and less compliant vessel so hangout interval of aortic is less than the pulmonary side • Pulmonary circulation is Low pressure , low resistance, high capacitance circulation. So hang out interval more
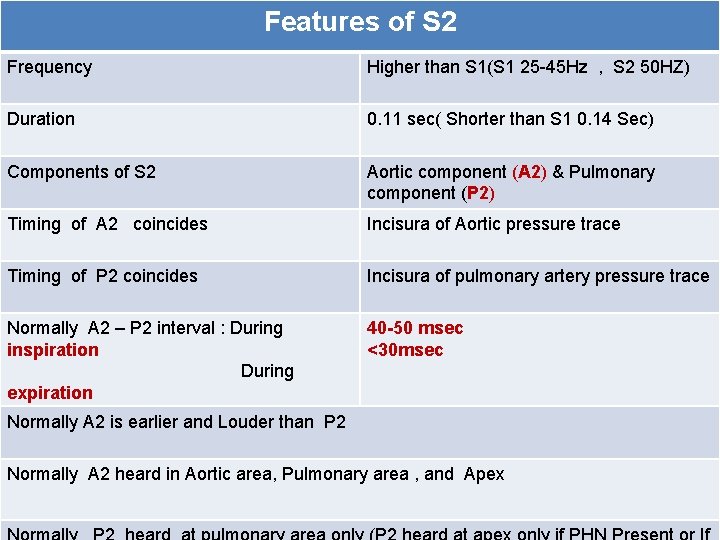
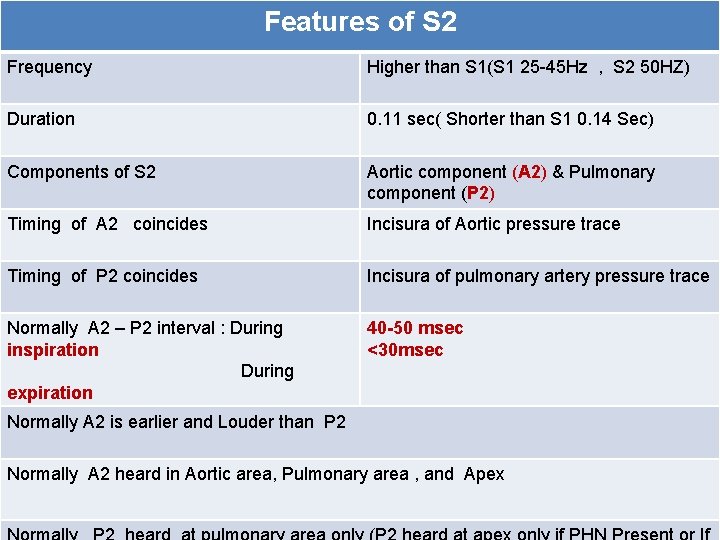
Features of S 2 Frequency Higher than S 1(S 1 25 -45 Hz , S 2 50 HZ) Duration 0. 11 sec( Shorter than S 1 0. 14 Sec) Components of S 2 Aortic component (A 2) & Pulmonary component (P 2) Timing of A 2 coincides Incisura of Aortic pressure trace Timing of P 2 coincides Incisura of pulmonary artery pressure trace Normally A 2 – P 2 interval : During inspiration During expiration 40 -50 msec <30 msec Normally A 2 is earlier and Louder than P 2 Normally A 2 heard in Aortic area, Pulmonary area , and Apex
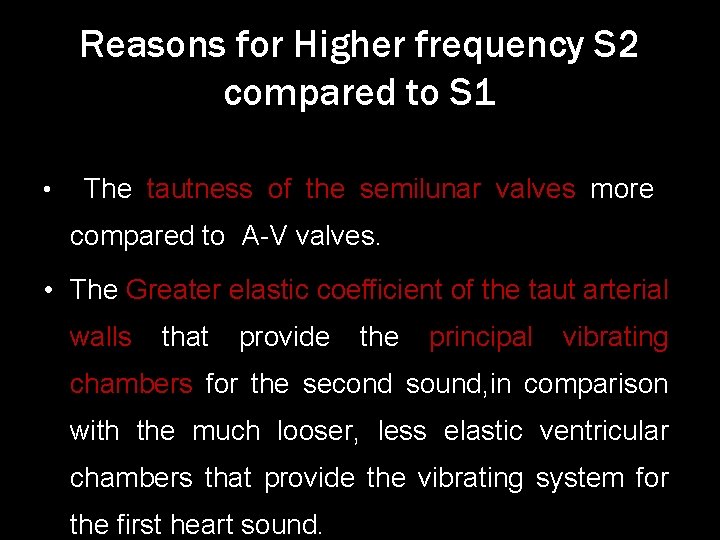
Reasons for Higher frequency S 2 compared to S 1 • The tautness of the semilunar valves more compared to A-V valves. • The Greater elastic coefficient of the taut arterial walls that provide the principal vibrating chambers for the second sound, in comparison with the much looser, less elastic ventricular chambers that provide the vibrating system for the first heart sound.
Why S 2 duration shorter than S 1? • Normally duration of S 1 is 0. 14 second and S 2 is 0. 11 second. • The reason is that, semilunar valves are more taut than the A-V valves, so they vibrate for a shorter time than do the A-V valves.
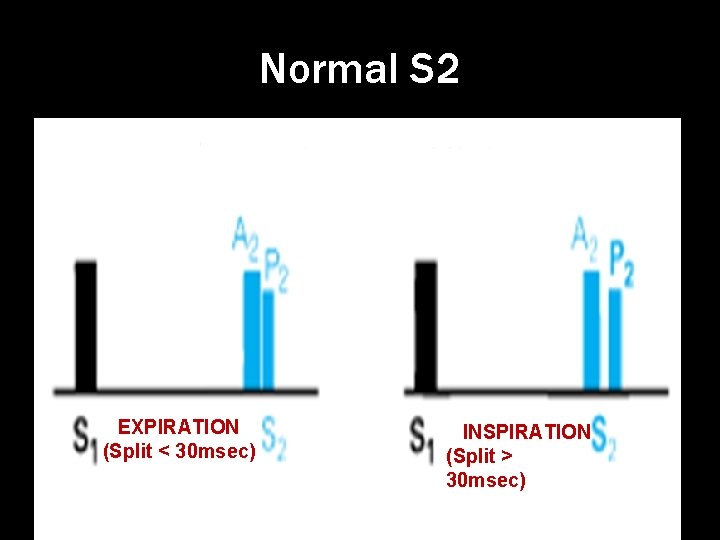
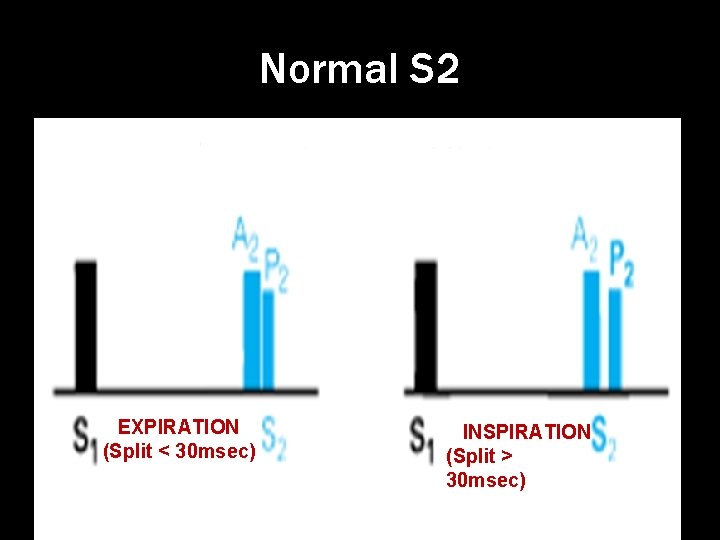
Normal S 2 EXPIRATION (Split < 30 msec) INSPIRATION (Split > 30 msec)
Why P 2 Delayed? • RV systolic ejection last longer than LV ejection even though RV and LV Mechanical systole has same duration • This occurs due to prolonged hangout interval of pulmonary circulation.

Why A 2 is earlier and louder than P 2 • Due to High Diastolic pressure gradient acoss the aortic valve • When compared to pulmonary circulation, LV ejection time is small as aortic hangout interval is less
Clinical Examination Of s 2 • At 2 nd to 3 rd Left ICS preferably with Diaphram of the stethescope. • Spliting best apreciated at second Left intercostal space.
Clinical examination of S 2 Two important Points to observe while examining for S 2 are. • Splitting of S 2 • Intensity of each component of S 2
Splitting Of S 2

Normal Splitting of S 2 EXPIRATION (Split < 30 msec) INSPIRATION (Split > 30 msec)
Normal splitting of S 2 Normal A 2 P 2 interval During expiration : < 30 msec During inspiration : 40 -50 ms Splitting occurs because of delayed P 2 (73%) and early A 2 (27%).
Factors affecting normal splitting of S 2 • Age : As age increases split duration decreases. Sing S 2 during both phases of respiration is a norm finding in subjects with age >40 yrs • Depth of respiration • Position of body : In recumbent position prominent splitting in both phases of respiration is a normal finding

Mechanism of increased split in inspiration
Recent views regarding inspiratory widening of split • Complex interplay of dynamic changes in pulmonary vascular impedence and changes in pulmonary and systemic venous return. Net effect is prolonged RV ejection and a concomittent decrease in LV ejection causing widening of split in inspiration.

Inspiration causes more negative intrathoracic pressure 1) Increased venous return 2) Increase capacitance of the pulmonary vessels Pulmonary hang out interval increases & RV ejection time increases Decreased pulmonary venous flow to the left atrium. So LV ejection time decreases so A 2 occurs early So A 2 P 2 interval > 30 msec
Abnormal Splitting Of S 2
• Abnormal splitting can be either absent/inaudible split (single S 2) or presence of audible expiratory splitting both in supine and upright position
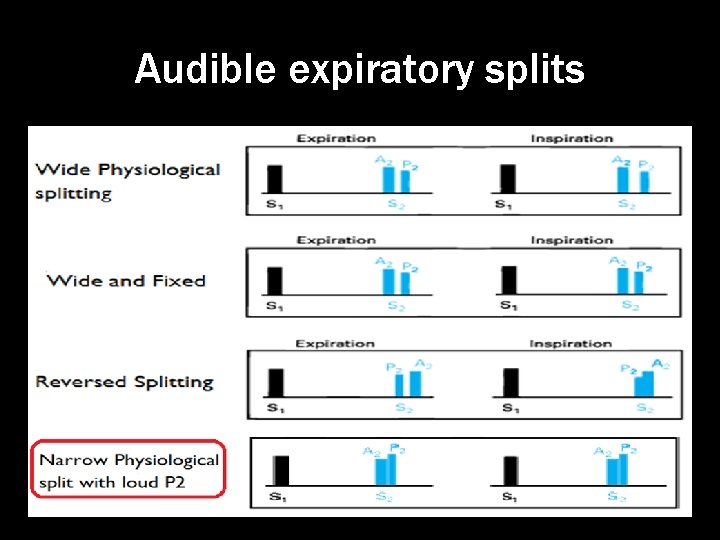
Abnormal Splitting of S 2 includes • Persistent physiological split • Wide fixed split of S 2 Expiratory split interval> 30 msec • Reverse split of S 2 • Narrow Physiological split with Loud P 2 • No Split : ie Single S 2
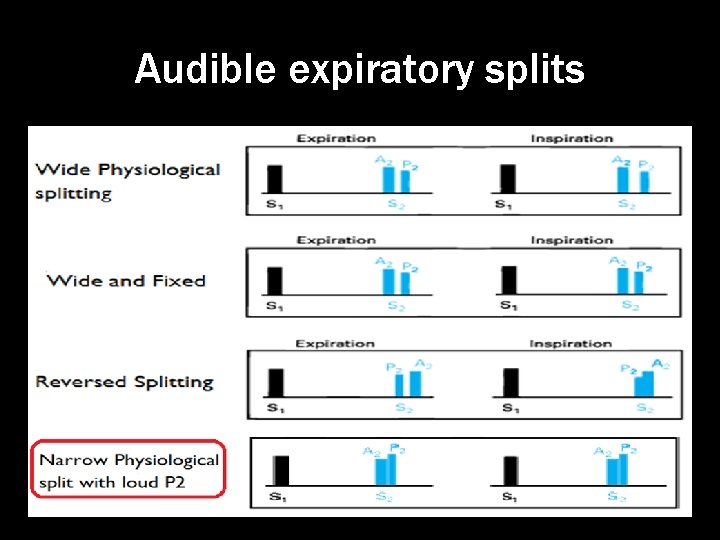
Audible expiratory splits
Wide Persistent physiological split
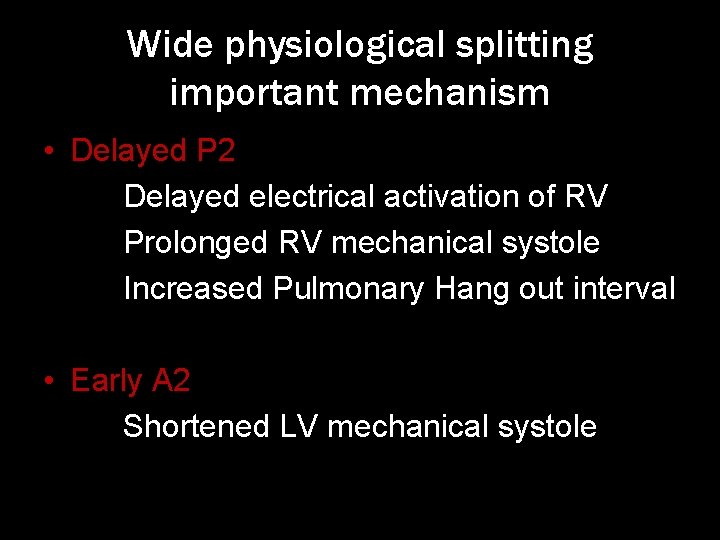
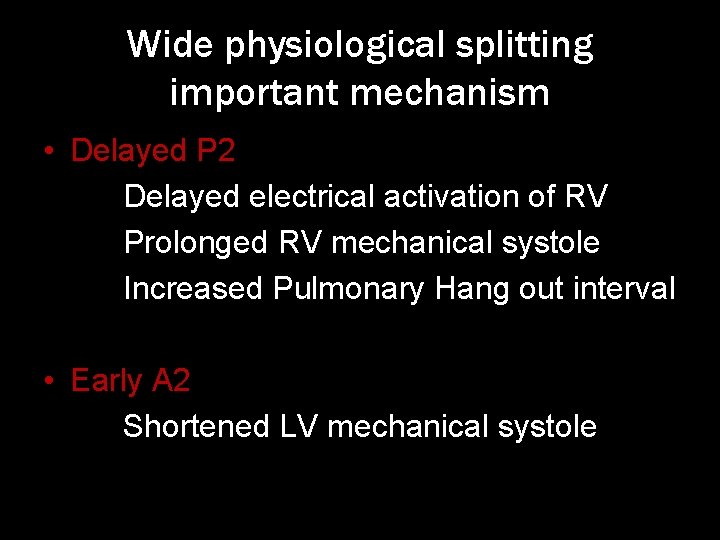
Wide physiological splitting important mechanism • Delayed P 2 Delayed electrical activation of RV Prolonged RV mechanical systole Increased Pulmonary Hang out interval • Early A 2 Shortened LV mechanical systole
Delayed electrical activation of RV • Complete RBBB • LV ectopic beat • LV pacing
Prolonged RV mechanical systole • Moderate to severe PS with intact IVS • Right heart failure • Acute Massive pulmonary embolism • Anomalous venous connection to RA
Increased Hangout interval • Mild Pulmonary stenosis • Idiopathic dilatation of pulmonary artery • Normo tensive ASD • Unexplained audible expiratory splitting in normal subjects
Shortened LV mechanical systole • Severe Mitral Regurgitation • Moderate to Large VSD

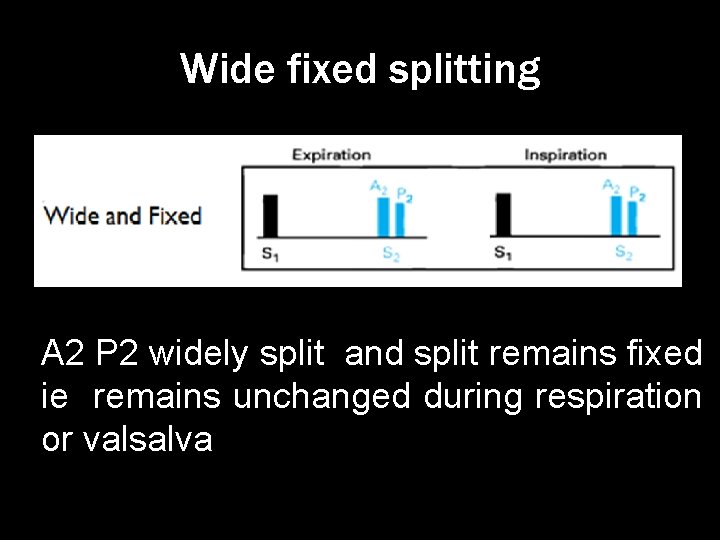
Wide fixed splitting
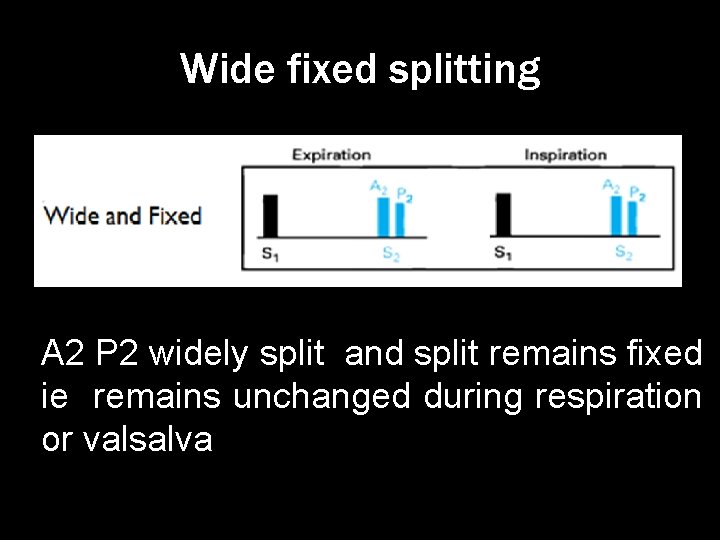
Wide fixed splitting A 2 P 2 widely split and split remains fixed ie remains unchanged during respiration or valsalva
• Wide : Due to delay in P 2 because of increased pulmonary vascular capacitance prolonging the hangout increased RV ejection time interval and
• Fixed : As little or no change in RV filling and stroke volume during inspiration. so little or no inspiratory delay occurs to P 2

Causes of wide fixed split • Moderate to Large Ostium Secundum ASD • Severe right heart failure

Reverse or paradoxical splitting of S 2
Reverse or paradoxical splitting • S 2 Split>30 msec during expiration with reversal of sequence ie P 2 -A 2 • Presence of reverse splitting always indicate significant underlying Heart disease • Almost all cases of reversed split are due to dalayed A 2
Types of Reversed split • Type 1 or classic : Only this type is audible clinically • Type 2 Detected Phonographically • Type 3
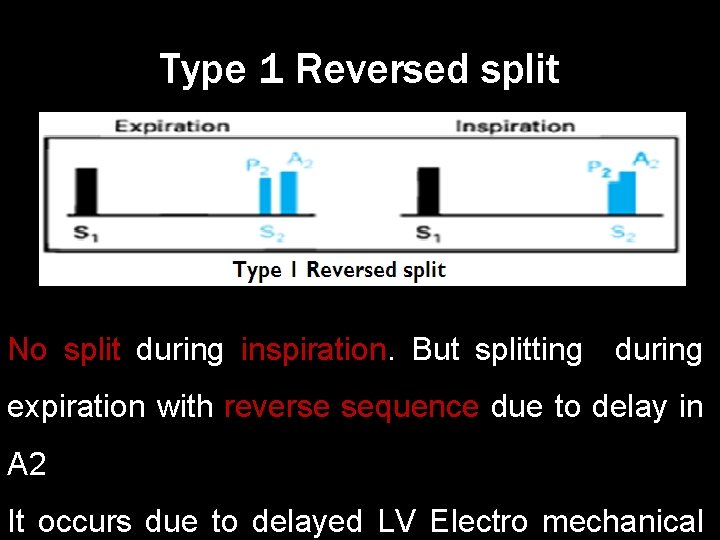
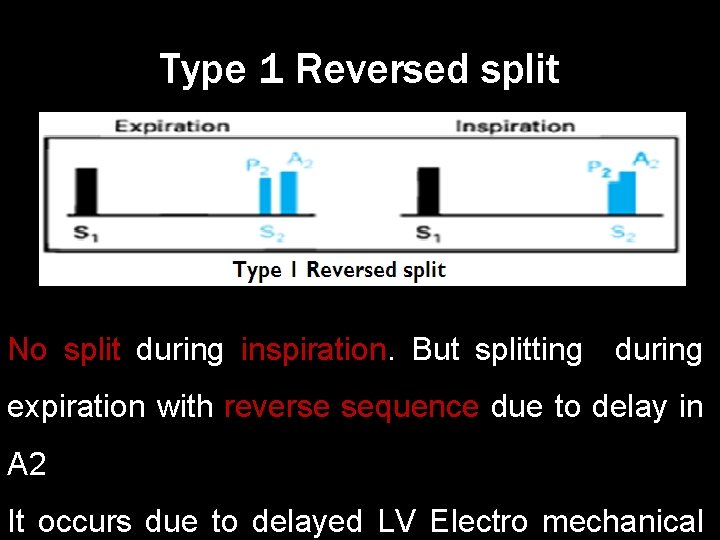
Type 1 Reversed split No split during inspiration. But splitting during expiration with reverse sequence due to delay in A 2 It occurs due to delayed LV Electro mechanical
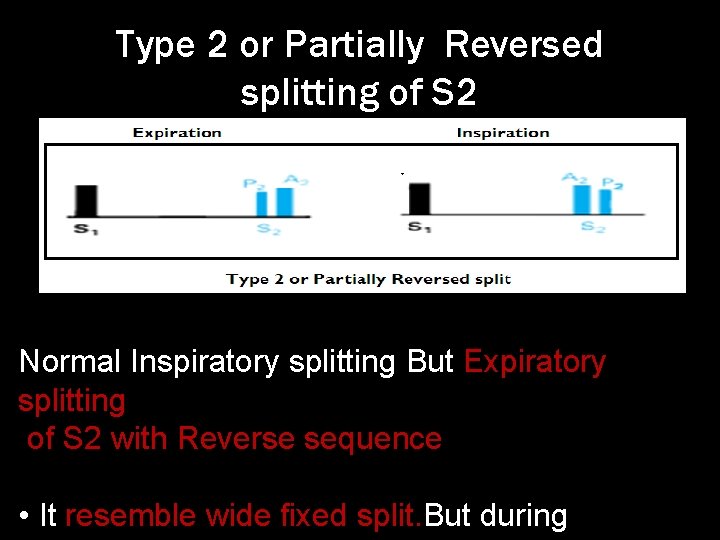
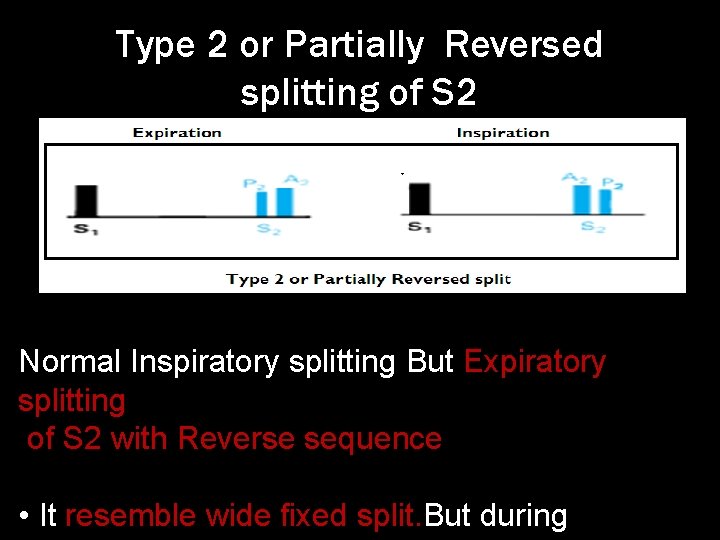
Type 2 or Partially Reversed splitting of S 2 Normal Inspiratory splitting But Expiratory splitting of S 2 with Reverse sequence • It resemble wide fixed split. But during
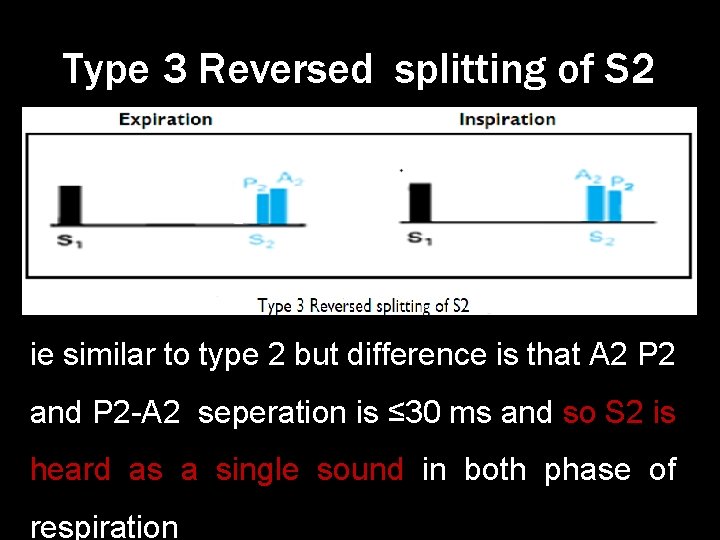
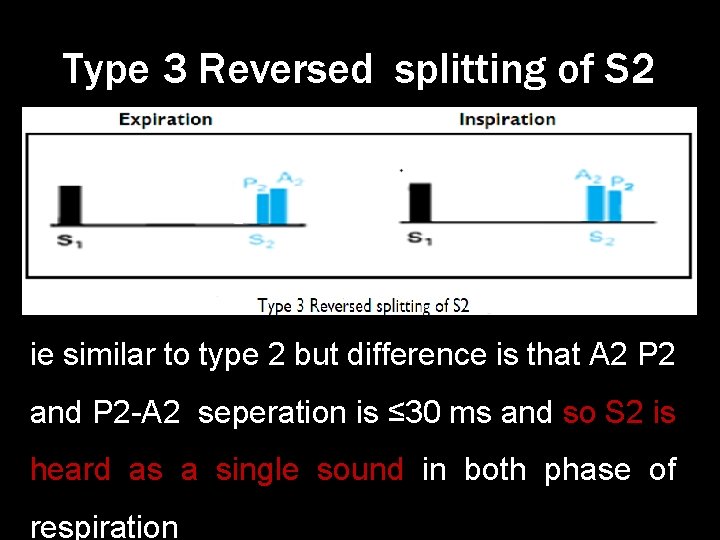
Type 3 Reversed splitting of S 2 ie similar to type 2 but difference is that A 2 P 2 and P 2 -A 2 seperation is ≤ 30 ms and so S 2 is heard as a single sound in both phase of respiration

Clinical recognition of Reversed split of S 2 • Trace the two components of S 2 to the apex. If the second component of S 2 is tracable up to apex , reverse split present. • (normally only first component of S 2(ie A 2) is tracable up to apex, And second component is heard only at pulonary area. In reverse split A 2 is the second component. )

Clinical recognition of Reversed split of S 2 • Valsalva testing Normally S 2 becomes Reversed split S 2 becomes Strain phase Split narrows widens Release phase widens Splitt narrows
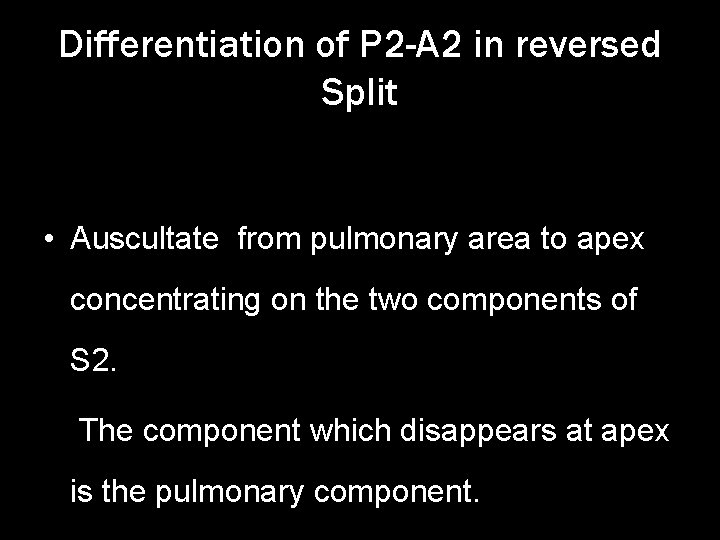
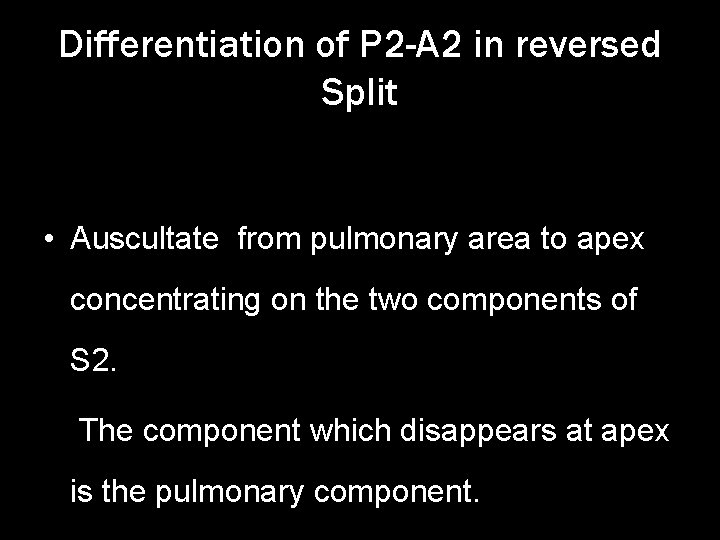
Differentiation of P 2 -A 2 in reversed Split • Auscultate from pulmonary area to apex concentrating on the two components of S 2. The component which disappears at apex is the pulmonary component.
Causes of Reversed spliting • Due to Delayed A 2 Early P 2
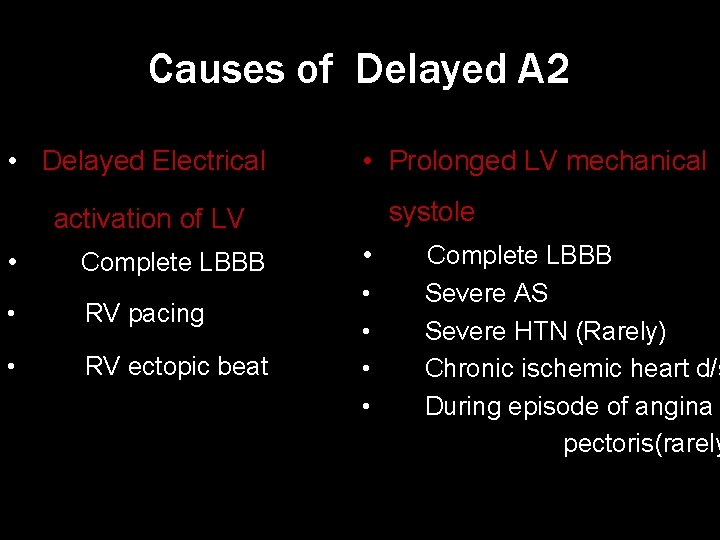
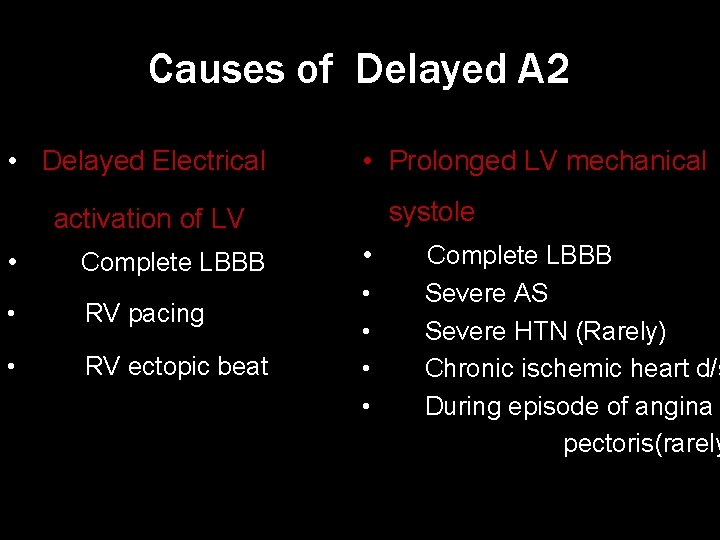
Causes of Delayed A 2 • Delayed Electrical • Prolonged LV mechanical systole activation of LV • Complete LBBB • RV pacing • RV ectopic beat • • • Complete LBBB Severe AS Severe HTN (Rarely) Chronic ischemic heart d/s During episode of angina pectoris(rarely
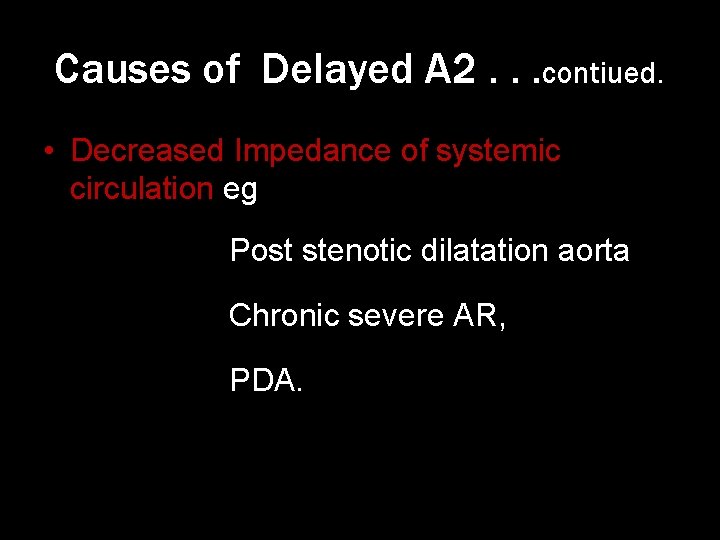
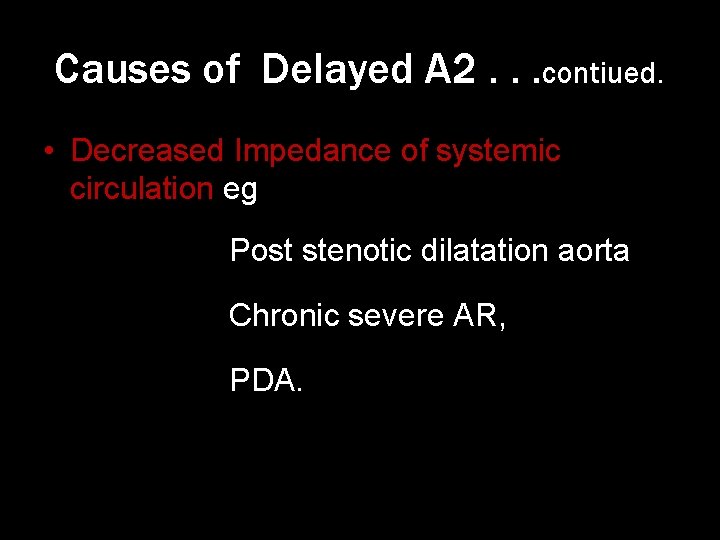
Causes of Delayed A 2. . . contiued. • Decreased Impedance of systemic circulation eg Post stenotic dilatation aorta Chronic severe AR, PDA.
Early P 2 Due to Type B WPW Syndrome
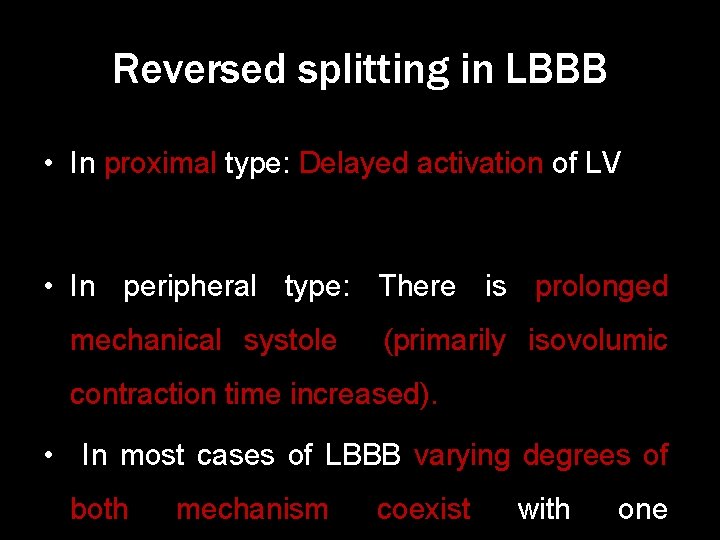
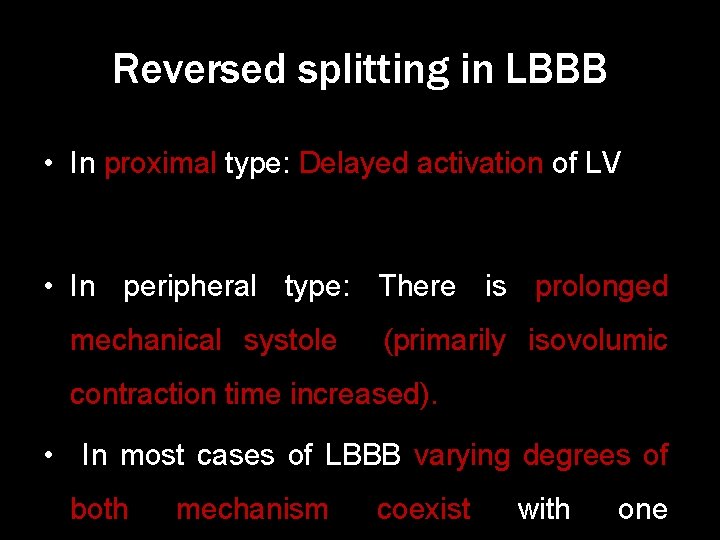
Reversed splitting in LBBB • In proximal type: Delayed activation of LV • In peripheral type: There is prolonged mechanical systole (primarily isovolumic contraction time increased). • In most cases of LBBB varying degrees of both mechanism coexist with one
Reversed split in angina pectoris • It occurs rarely • Proposed mechanisms are 1) Prolonged isovolumetric contraction time of ischemic LV 2) Systemic hypertension prolonging LVETime

Reverse splitting in HTN • In HTN Loud A 2 with normal split is the common finding • Reverse split occurs rarely especially in acute hypertension. Due to increased LV ejection & isovolumetric contraction time

Single S 2
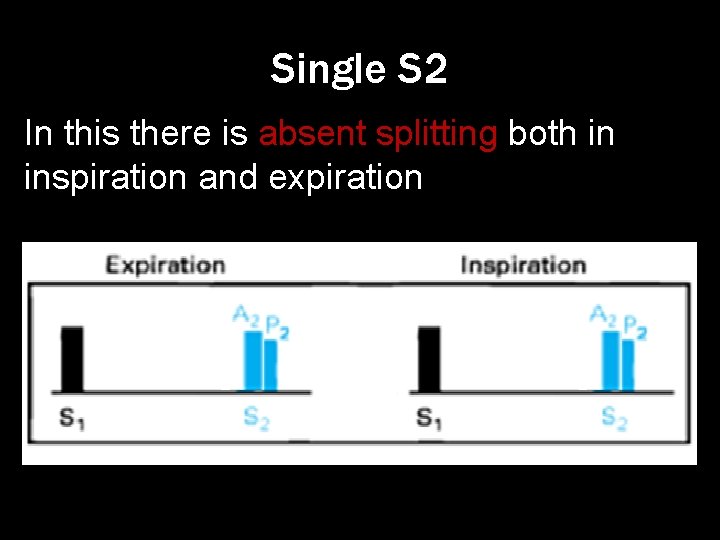
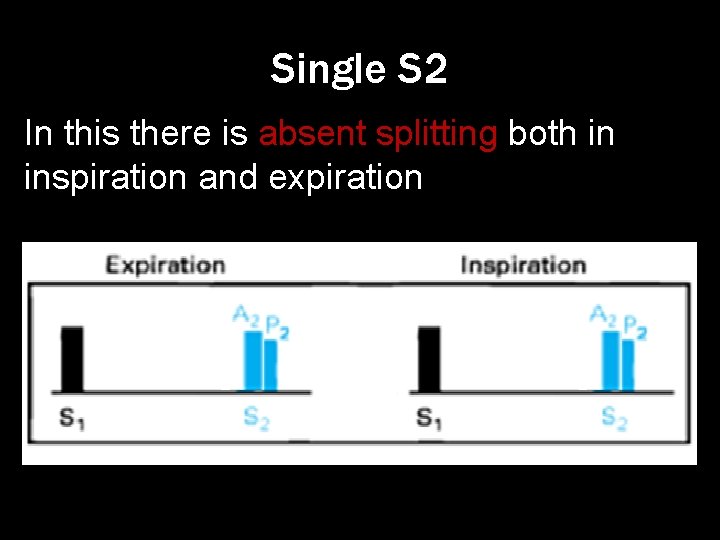
Single S 2 In this there is absent splitting both in inspiration and expiration
Single S 2: Mechanism • If only one semilunar valve present: eg: Aortic or Pulmonary atresia, Persistent truncus arteriosis • When P 2 inaudible: TGA, TOF, Severe PS, PA • When Delayed A 2 coincides with P 2: Sever AS
• When early P 2 coincides with A 2 : Severe PHTN, VSD+PHTN • Any condition producing Paradoxical split with A 2 P 2 interval ≤ 30 msec • A 2 sound drowned by murmur of AS/MR/VSD
INTENSITY OF S 2(A 2 P 2)
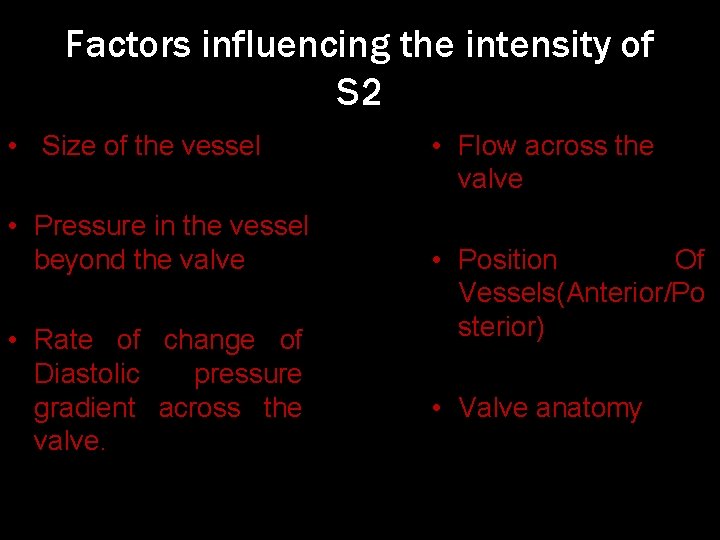
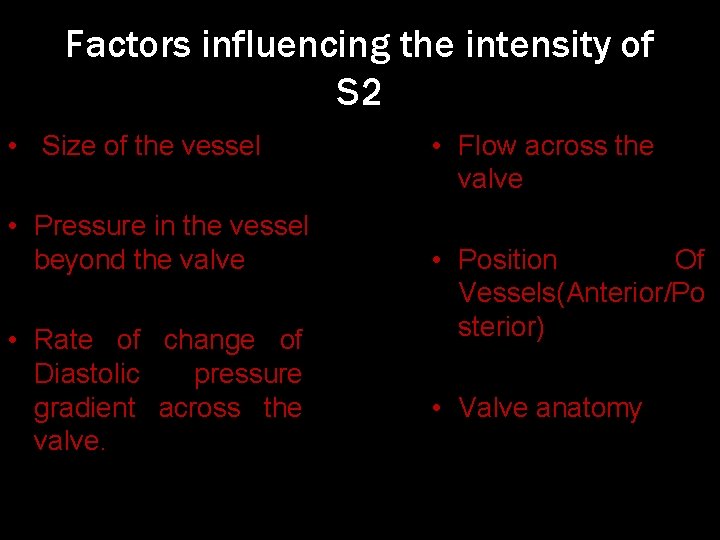
Factors influencing the intensity of S 2 • Size of the vessel • Pressure in the vessel beyond the valve • Rate of change of Diastolic pressure gradient across the valve. • Flow across the valve • Position Of Vessels(Anterior/Po sterior) • Valve anatomy

S 2 intensity relation to the rate of change of the diastolic pressure gradient that develops across the valves It is the driving forces accelerating the blood mass retrograde into the base of the great vessels. This pressure gradient is the result of the level of diastolic pressure in the great vessel and the rate of pressure decline in the ventricle. ,
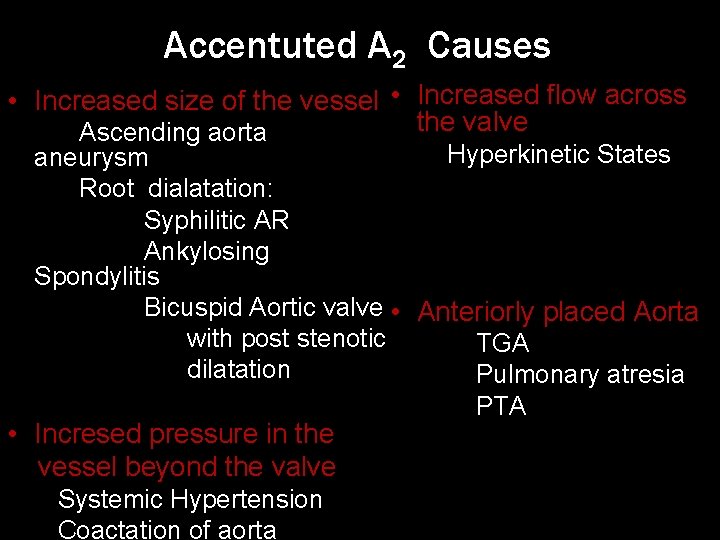
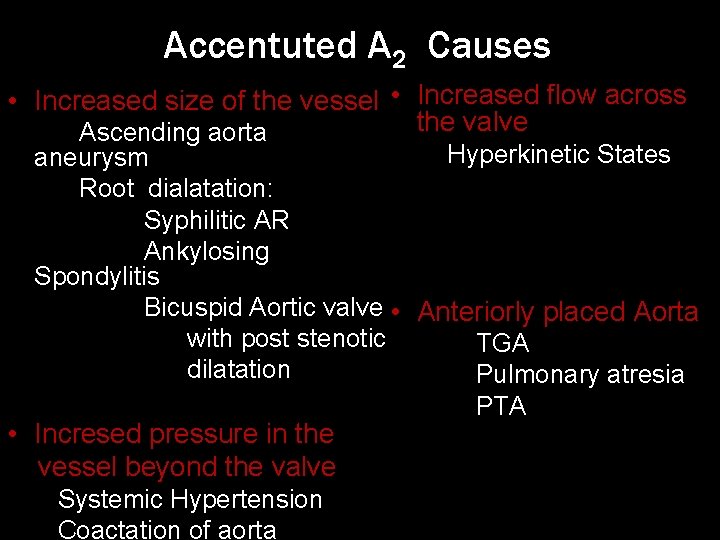
Accentuted A 2 Causes • Increased size of the vessel • Increased flow across the valve Ascending aorta Hyperkinetic States aneurysm Root dialatation: Syphilitic AR Ankylosing Spondylitis Bicuspid Aortic valve • Anteriorly placed Aorta with post stenotic TGA dilatation Pulmonary atresia PTA • Incresed pressure in the vessel beyond the valve Systemic Hypertension Coactation of aorta
Diminished A 2 • Occurs due to distortion of aortic leaflet eg Aortic sclerosis, Calcific AS, Valvular AR Aortic atresia(HLHS).

Loud P 2 • Increased size of the • Increased flow across vessel: the valve Idiopathic dilatation Hyperkinetic States of pulmonary artery, ASD • Distance From the site of origin of sound to the chest wall: • Incresed pressure in the vessel beyond the Thin Chest wall valve: Straight Back PHTN syndrome
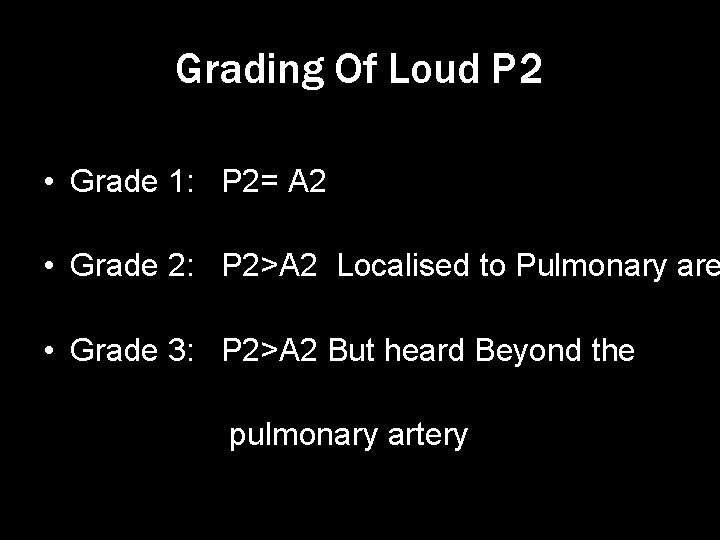
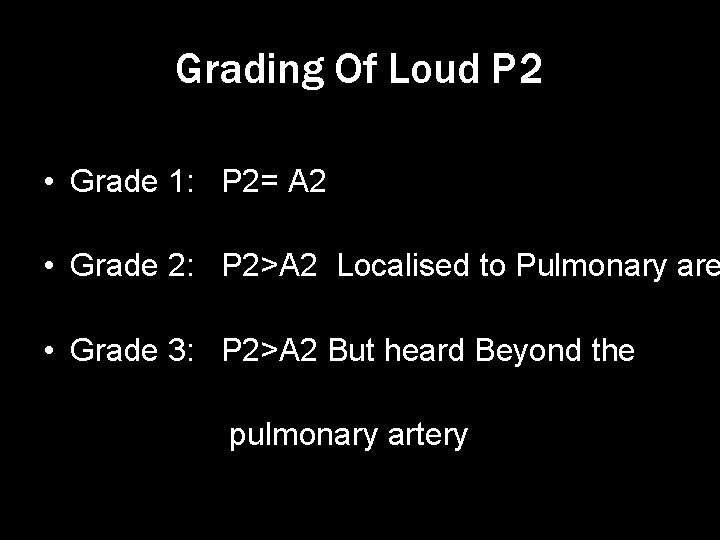
Grading Of Loud P 2 • Grade 1: P 2= A 2 • Grade 2: P 2>A 2 Localised to Pulmonary are • Grade 3: P 2>A 2 But heard Beyond the pulmonary artery

Relation Between P 2 intensity and Pulmonary pressure Pulmonary Systolic pressure Mean pulmonary pressure Grade 1 Mild PHTN 30 -49 mm of Hg 21 -34 mm of Hg Grade 2 Moderate PHTN 50 -75 mm of Hg 35 -50 mm of Hg Grade 3 Severe PHTN > 50 mm of Hg > 75 mm of Hg
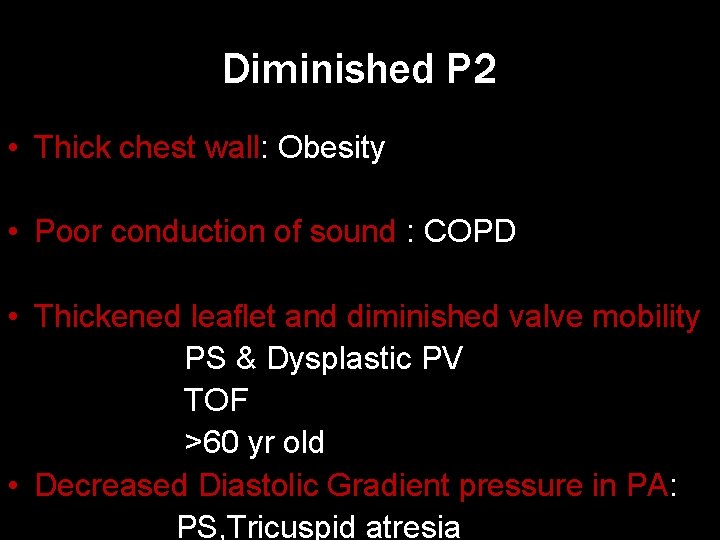
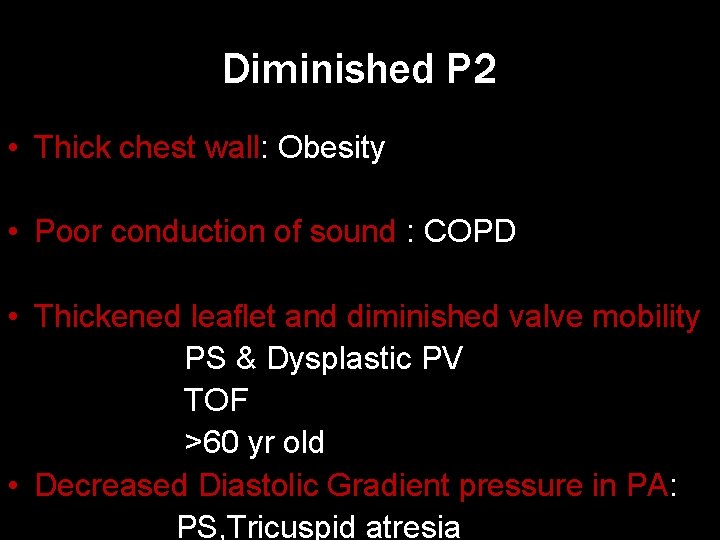
Diminished P 2 • Thick chest wall: Obesity • Poor conduction of sound : COPD • Thickened leaflet and diminished valve mobility PS & Dysplastic PV TOF >60 yr old • Decreased Diastolic Gradient pressure in PA: PS, Tricuspid atresia

S 2 in different cardiac conditions
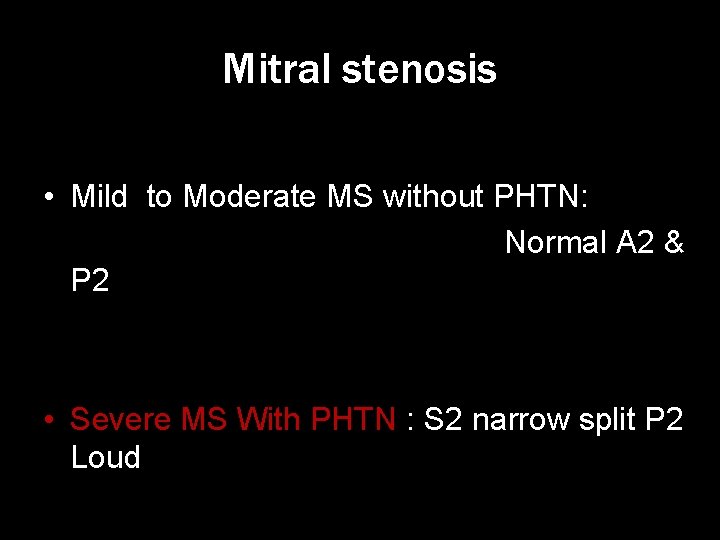
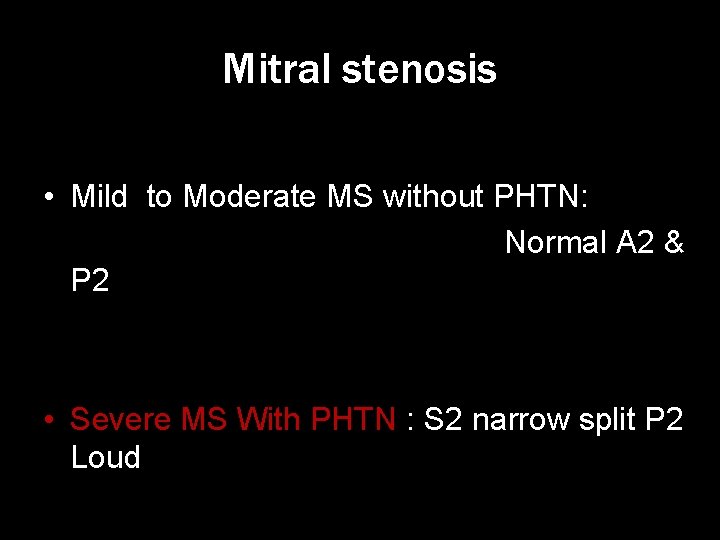
Mitral stenosis • Mild to Moderate MS without PHTN: Normal A 2 & P 2 • Severe MS With PHTN : S 2 narrow split P 2 Loud
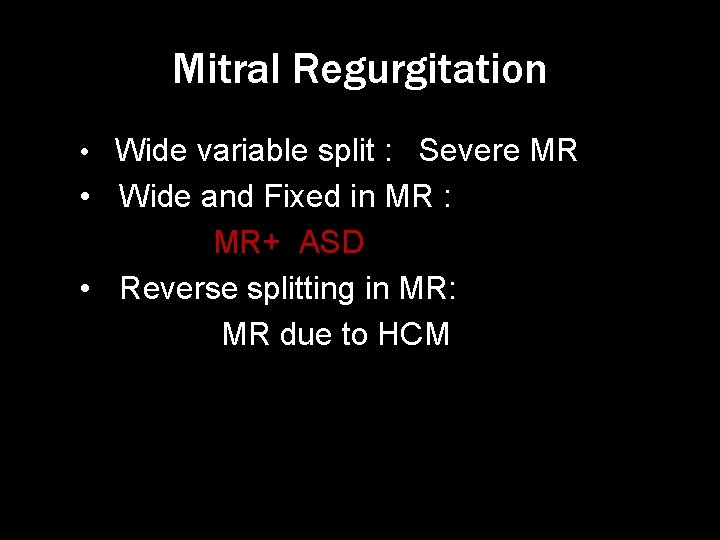
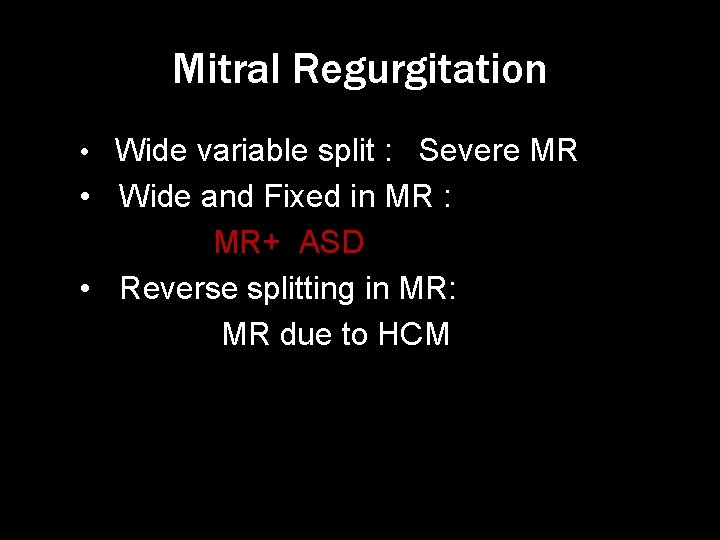
Mitral Regurgitation • Wide variable split : Severe MR • Wide and Fixed in MR : MR+ ASD • Reverse splitting in MR: MR due to HCM
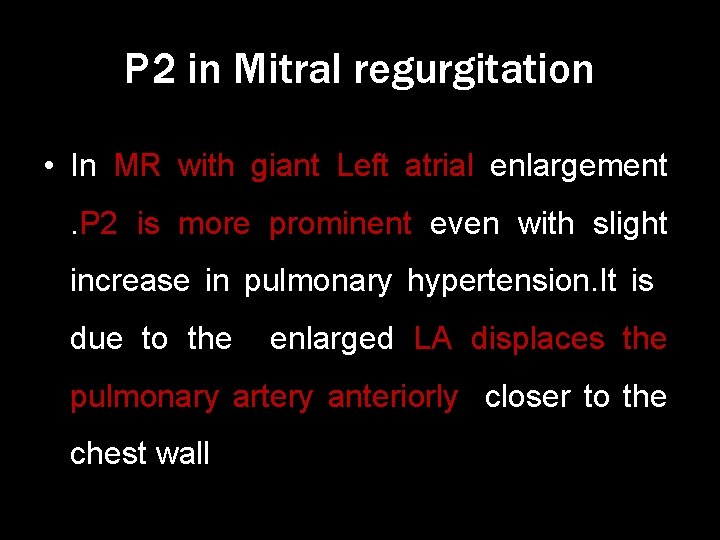
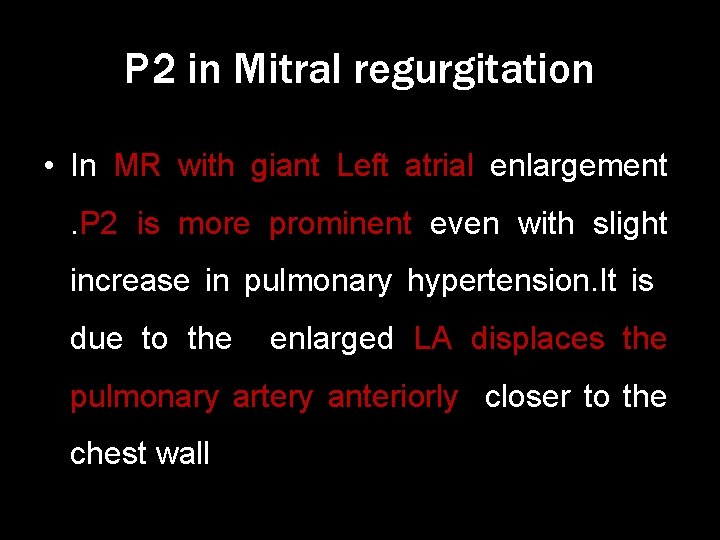
P 2 in Mitral regurgitation • In MR with giant Left atrial enlargement. P 2 is more prominent even with slight increase in pulmonary hypertension. It is due to the enlarged LA displaces the pulmonary artery anteriorly closer to the chest wall

Aortic stenosis • Reverse split : Due to Delayed A 2 in Severe AS • Single S 2 : If A 2 is Absent/soft or A 2 drowned in the murmur
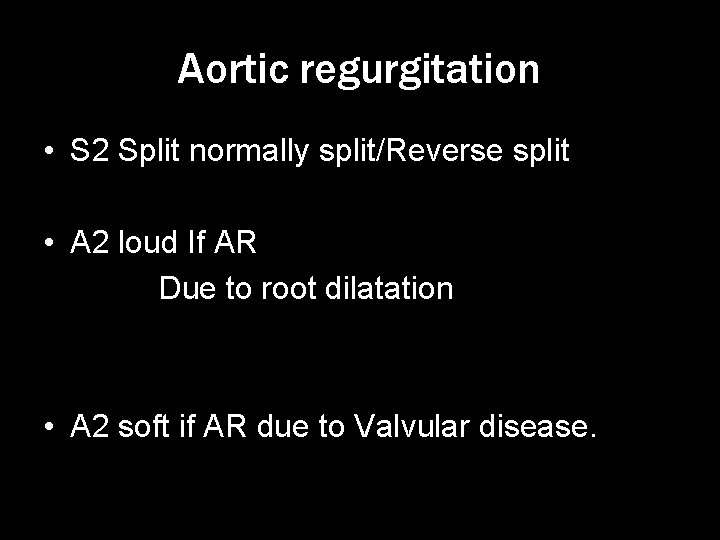
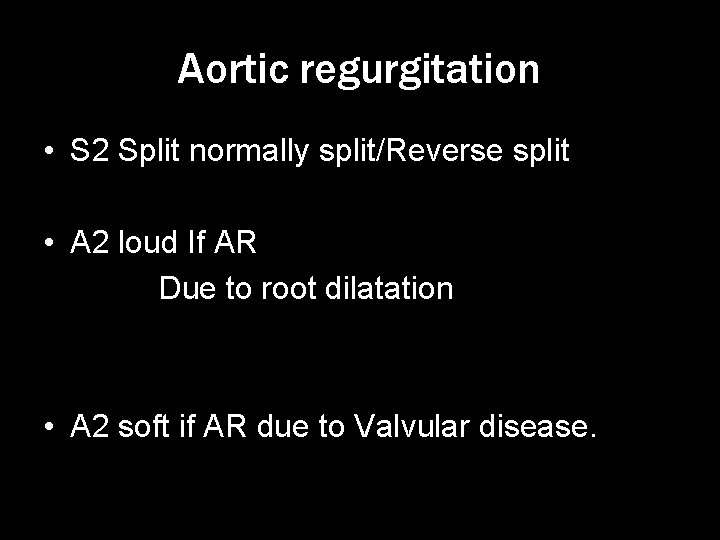
Aortic regurgitation • S 2 Split normally split/Reverse split • A 2 loud If AR Due to root dilatation • A 2 soft if AR due to Valvular disease.
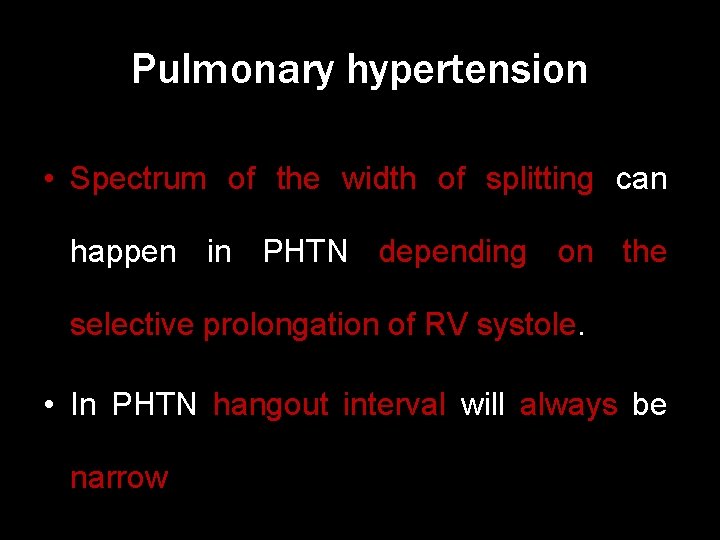
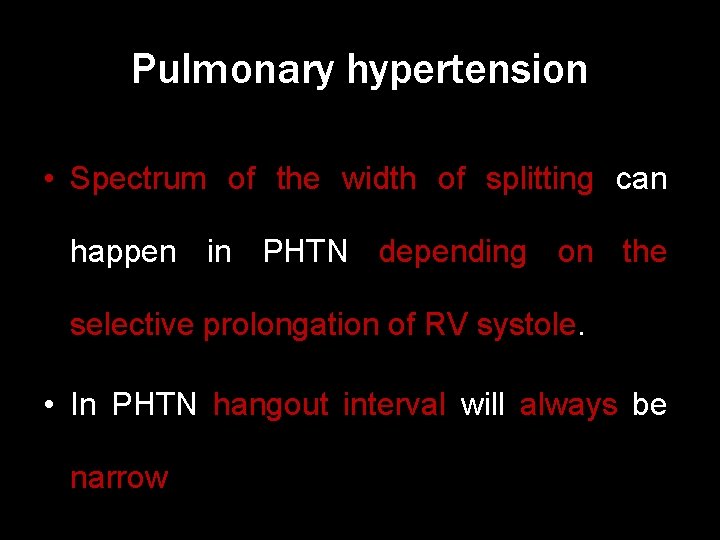
Pulmonary hypertension • Spectrum of the width of splitting can happen in PHTN depending on the selective prolongation of RV systole. • In PHTN hangout interval will always be narrow
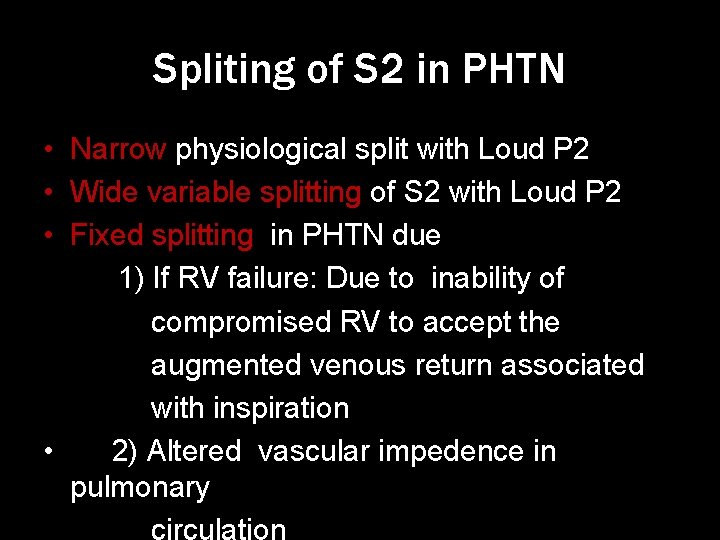
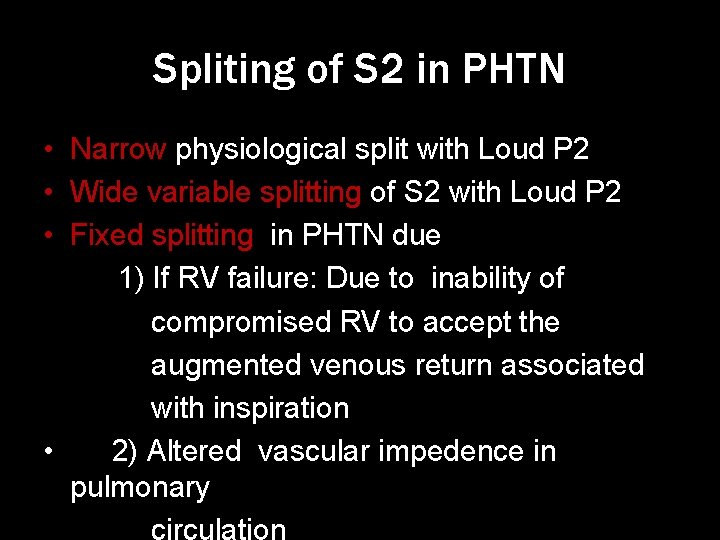
Spliting of S 2 in PHTN • Narrow physiological split with Loud P 2 • Wide variable splitting of S 2 with Loud P 2 • Fixed splitting in PHTN due 1) If RV failure: Due to inability of compromised RV to accept the augmented venous return associated with inspiration • 2) Altered vascular impedence in pulmonary
S 2 in CONGENITAL HEART DISEASE
ASD • Wide fixed split with loud p 2 in absence of PHTN is the hallmark of ASD P 2 Loud because Dilated P 2 is close to the chest wall.

Fixed split in ASD Mechanism: • Fixed : Inspiratory augmentation of systemic venous return produces less Left to Right shunt and it causes delayed A 2. And expiratory decrease in systemic venous return causes increased Left to right shunt producing early A 2.

VSD • Small VSD : normal Normal S 2 split with intensity P 2 • Moderate VSD: Normal split with moderate accentuation of P 2 • Large VSD : Wide variable Split with Loud P 2 • VSD with PS physiology : Single Loud S 2

PDA • Small PDA : Normal S 2 split and normal intensity P 2 but S 2 masked by continous murmur • Large PDA: Normal S 2 split with accentuated P 2. Occationally paradoxical splitting can be seen.
Pulmonary stenosis • Mild PS: Normal S 2 Split with decreased intensity P 2 • Moderate – Severe PS: Wide Variable Split With Diminished P 2 • Severe PS : P 2 absent • Dysplastic pulmonary valve : P 2 can be normal or inaudible depending severity of stenosis

BISCUSPID AORTIC VALVE • In the absence of significant AS or AR S 2 normally split with accentuated A 2 • If significant AS: S 2 Reversed split
COA • Normally splitting S 2 with accentuated A 2 due to hypertension • sometimes reverse split can also happen
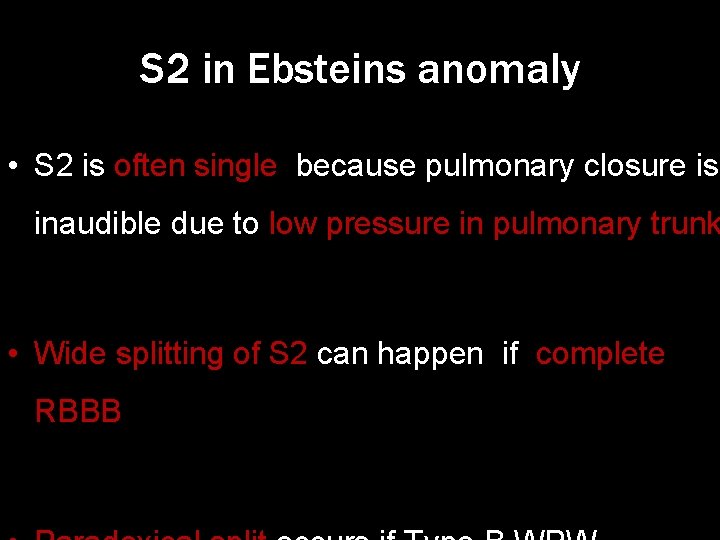
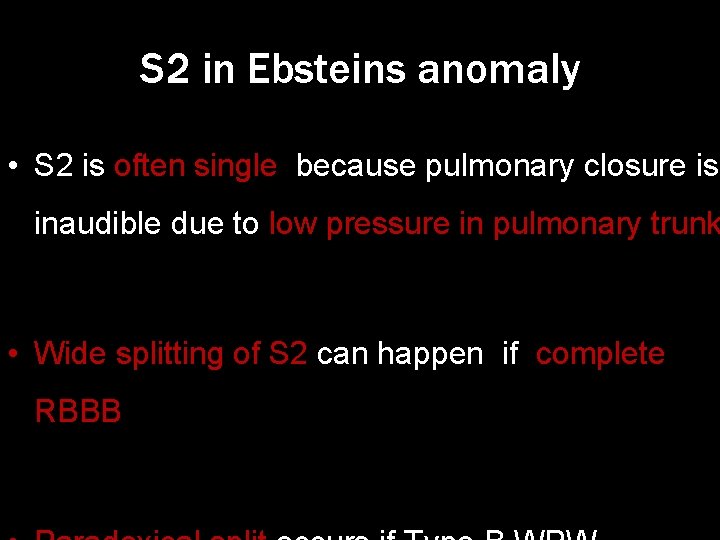
S 2 in Ebsteins anomaly • S 2 is often single because pulmonary closure is inaudible due to low pressure in pulmonary trunk • Wide splitting of S 2 can happen if complete RBBB

S 2 in Anomalous pulmonary venous connection • If Associated ASD : Wide fixed split • If Atrial septum intact: S 2 normal split with normal respiratory variation
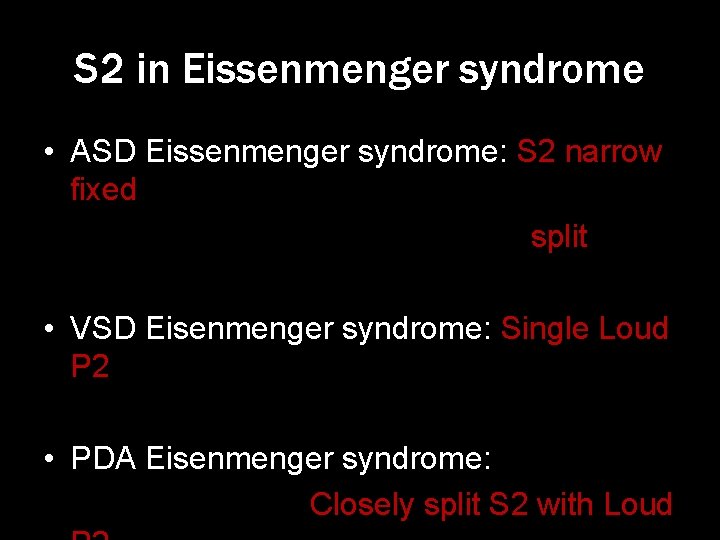
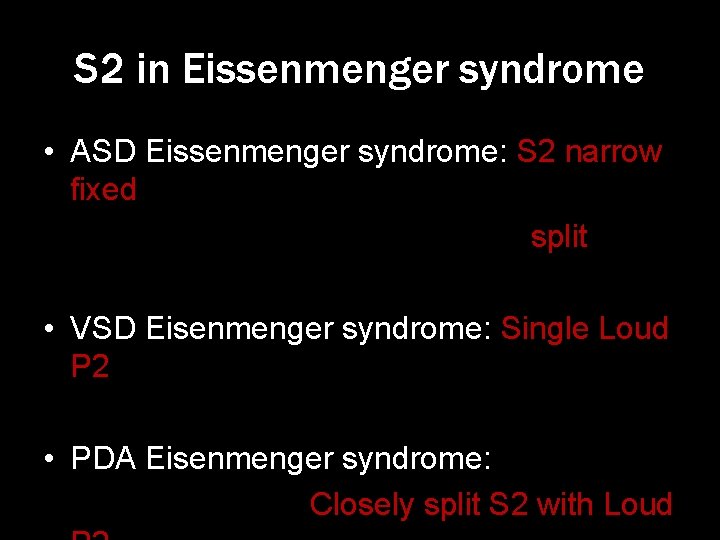
S 2 in Eissenmenger syndrome • ASD Eissenmenger syndrome: S 2 narrow fixed split • VSD Eisenmenger syndrome: Single Loud P 2 • PDA Eisenmenger syndrome: Closely split S 2 with Loud
THANK U
 Splitting of heart sounds
Splitting of heart sounds Accp cardiology prn
Accp cardiology prn Muse cardiology
Muse cardiology Westcliffe cardiology shipley
Westcliffe cardiology shipley Enloe cardiology
Enloe cardiology Acc sports cardiology
Acc sports cardiology Elias hanna cardiology
Elias hanna cardiology Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Justin davies cardiology
Justin davies cardiology Service line strategy
Service line strategy Craig ainsworth cardiology
Craig ainsworth cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Accp cardiology prn journal club
Accp cardiology prn journal club Structured reporting cardiology
Structured reporting cardiology Dr nick gall cardiologist
Dr nick gall cardiologist Hall-garcia cardiology associates
Hall-garcia cardiology associates 27 miles per gallon into kilometers per liter
27 miles per gallon into kilometers per liter “a sound mind is in a sound body”
“a sound mind is in a sound body” The higher the amplitude, the _______the sound.
The higher the amplitude, the _______the sound. Second heart assist
Second heart assist Second degree heart block
Second degree heart block Second heart of the body
Second heart of the body Premonitiry
Premonitiry Machinary murmur
Machinary murmur Pansystolic murmur causes
Pansystolic murmur causes Grading of murmurs
Grading of murmurs Heard
Heard 5 heart sound locations
5 heart sound locations 5 cardiac landmarks
5 cardiac landmarks S3gallop
S3gallop Heart dullness
Heart dullness Sheep heart labeled
Sheep heart labeled Heart 2 heart
Heart 2 heart Stratum germinativum
Stratum germinativum Ffa creed pictogram
Ffa creed pictogram Accounting principles second canadian edition
Accounting principles second canadian edition When the pellet fired into the spiral tube
When the pellet fired into the spiral tube One subject of felipe alfaus second novel grammar
One subject of felipe alfaus second novel grammar Second language acquisition questions
Second language acquisition questions First order change examples
First order change examples Biology second semester final exam answers
Biology second semester final exam answers Every second matters
Every second matters Creed fccla
Creed fccla Newtons second kaw
Newtons second kaw Tor: the second-generation onion router
Tor: the second-generation onion router Psycholinguistic approach to second language acquisition
Psycholinguistic approach to second language acquisition Second major in data analytics
Second major in data analytics Organigramme second empire
Organigramme second empire Second fundamental theorem of calculus
Second fundamental theorem of calculus Second level analysis
Second level analysis What is french classical menu
What is french classical menu Second chances lumi
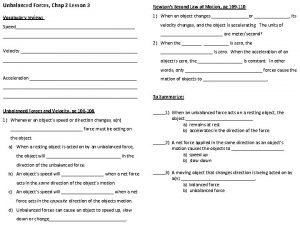
Second chances lumi Chapter 2 lesson 3 newton's second law
Chapter 2 lesson 3 newton's second law Basic components of computer
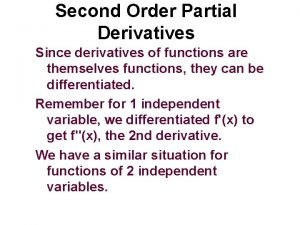
Basic components of computer Second partials test
Second partials test Newton's second law comic strip
Newton's second law comic strip Second order band pass filter transfer function
Second order band pass filter transfer function False start 10 second runoff
False start 10 second runoff Second life
Second life The second rome
The second rome Second grade homework
Second grade homework The second moroccan crisis (1911)
The second moroccan crisis (1911) Second order process
Second order process Fick's second law of diffusion
Fick's second law of diffusion Second law of thermodynamics
Second law of thermodynamics Who are second hand smokers
Who are second hand smokers Newtons second law in soccer
Newtons second law in soccer Money laundering stacking
Money laundering stacking Second coming
Second coming Mike rutherford 30 second feedback
Mike rutherford 30 second feedback This is the longest epic of the world
This is the longest epic of the world Second generation of romantic poets
Second generation of romantic poets Waddell triad second impact
Waddell triad second impact Second moment
Second moment Authors purpose second grade
Authors purpose second grade Map rizal's second sojourn
Map rizal's second sojourn Yugoslav war casualties
Yugoslav war casualties Newtons first lw
Newtons first lw Second wave of colonialism
Second wave of colonialism The first cartoons
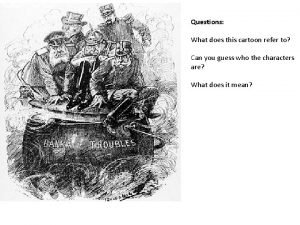
The first cartoons Pendulum second order differential equation
Pendulum second order differential equation Chapter 3 geometry test
Chapter 3 geometry test Blast off second ignition
Blast off second ignition Double marginalization
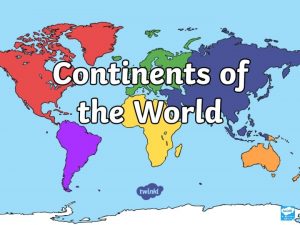
Double marginalization Fourth biggest continent
Fourth biggest continent Second order partial derivatives examples
Second order partial derivatives examples Third person narrative
Third person narrative Third generation computer images
Third generation computer images Entropy change formula
Entropy change formula Transient response specifications of second order system
Transient response specifications of second order system Second world war
Second world war