Approaches to Measuring Population Health Ian Mc Dowell













- Slides: 55

Approaches to Measuring Population Health Ian Mc. Dowell March, 2010 1. Mortality-based summary measures 2. Combined disability & mortality methods 3. Conceptual rationale for summary measures 4. Environmental indicators 5. Global indicators EPI 5343
1. Why do we need measures of population health? Governments wish to monitor health of citizens – – – – To set priorities for health services & policies To evaluate social and health policies To compare health of different regions To identify pressing health needs To draw attention to inequalities in health Highlight balance between length and quality of life Numerical index desirable: a “GNP of Health”
Classifying Population Health Measures by their Purpose 1. Measures that describe current state: i. Health or disability status (e. g. , surveys) ii. Evaluative measures (e. g. , to assess outcomes of health policies) 2. Analytic measures include an implicit time dimension: iii. Predictive methods look forwards (risk assessment; projections of disease burden) iv. Explanatory measures (income inequality or social cohesion) look backwards.
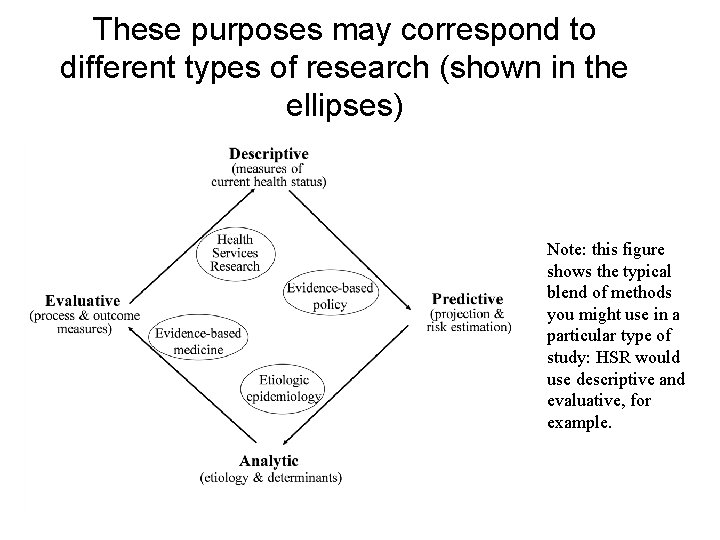
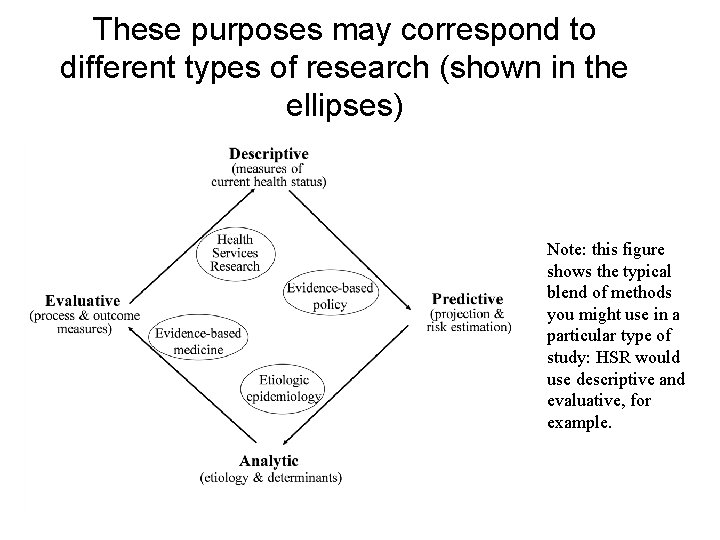
These purposes may correspond to different types of research (shown in the ellipses) Note: this figure shows the typical blend of methods you might use in a particular type of study: HSR would use descriptive and evaluative, for example.
Classifying population health measures by their focus 1. Aggregate measures combine data from individual people, summarized at regional or national levels. E. g. , rates of smoking or lung cancer. 2. Environmental health indicators record physical or social characteristics of the place in which people live and cover factors external to the individual, such as air or water quality, or the number of community associations that exist in a neighborhood. These can have analogues at the individual level. 3. Global health indicators have no obvious individual analogue. Examples include contextual indicators such as the existence of healthy public policy; laws restricting smoking in public places, or social equity in access to care; social cohesion, etc. Morgenstern H. Ecologic studies in epidemiology: concepts, principles, and methods. Annual Reviews of Public Health 1995; 16: 61 -81.
Linking the focus of a measure to its application • Aggregate measures are typically used in descriptive studies; they focus on the individuals within the population, i. e. idiographic. They measure health in the population • Environmental measures can be used in descriptive, analytic or explanatory studies • Global measures mainly used in analytic studies; focus on generating theory (nomothetic studies). They could measure health of the population
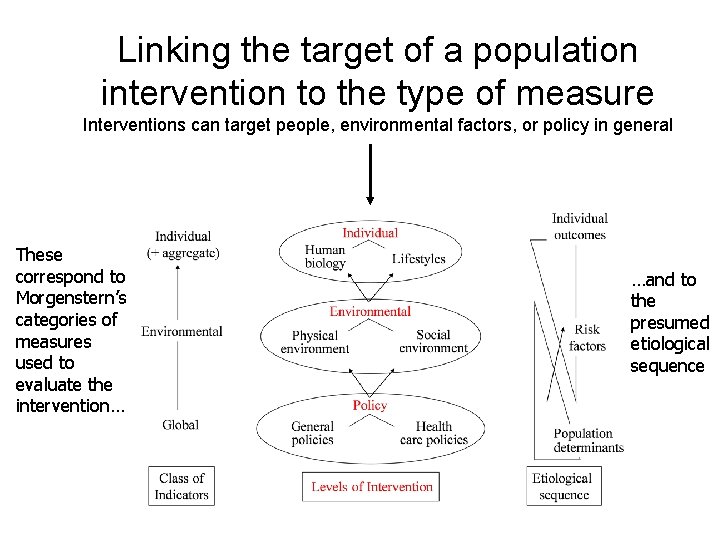
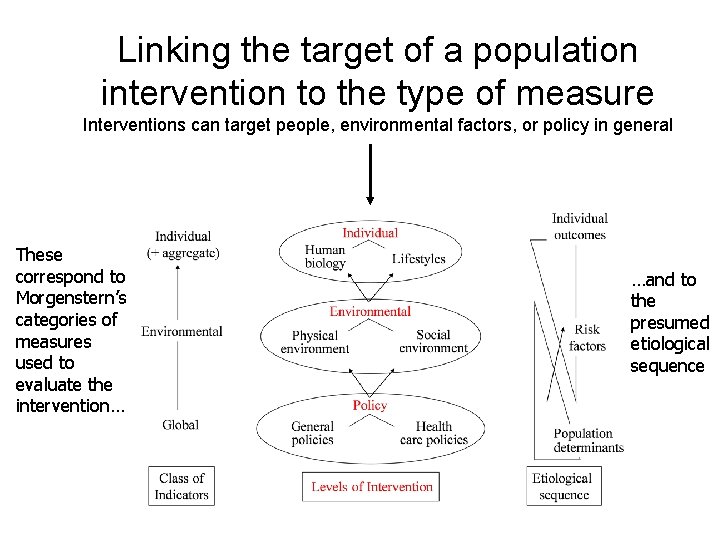
Linking the target of a population intervention to the type of measure Interventions can target people, environmental factors, or policy in general These correspond to Morgenstern’s categories of measures used to evaluate the intervention… …and to the presumed etiological sequence
History of changing approaches to measuring population health • Originally based on mortality rates. IMR is often used to describe level of development of a country • With declining mortality, people with chronic disease survive; morbidity & disability gain importance • Concern with quality of life, not mere survival • To compare populations at different stages of economic development, it may be desirable to combine mortality and morbidity in a single, composite index
Two rival conceptions of “population health” 1. Population health = sum total of individual health. • Idiographic: focus is on individual • No attention to dynamics, complexity, etc. • Factors “outside the skin” seen as determinants, not aspects of population health. • Responsibility for health lies principally with individuals, so a survey of population health need only consider final outcomes. 2. Emergent model. • Here “population” implies more then individuals within it: community health. • Ability of the society / community / population to respond to challenges is central to defining its health. • Externalities that influence individual health seen as aspects of population health: social capital, the existence of health protection legislation, acceptance of “the greater good, ” etc. • Summary measures record outcomes of this process, but the core population health dynamics actually lie upstream. Indicators of population health need to be broader than just measures of individuals in the population.
2. Aggregate Measures: Mortality-Based Indicators Life expectancy Expected years of life lost Potential years of life lost

Life Expectancy • Summary of all age-specific mortality rates • Estimates hypothetical length of life of a cohort born in a particular year – This assumes that current mortality rates will continue
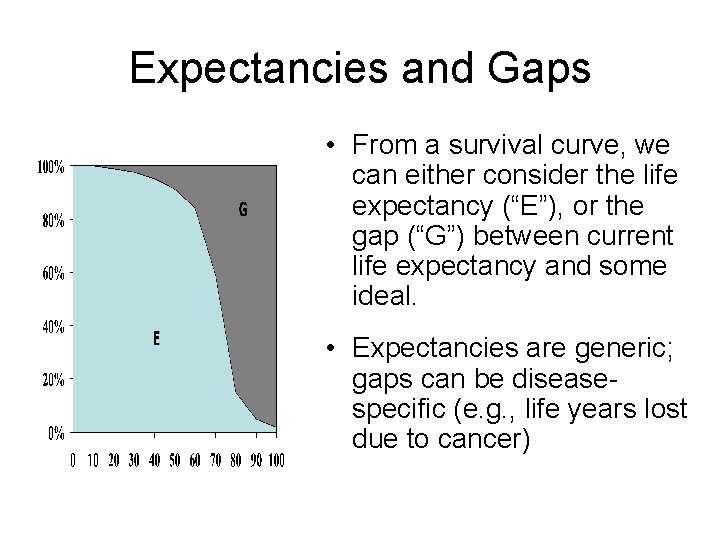
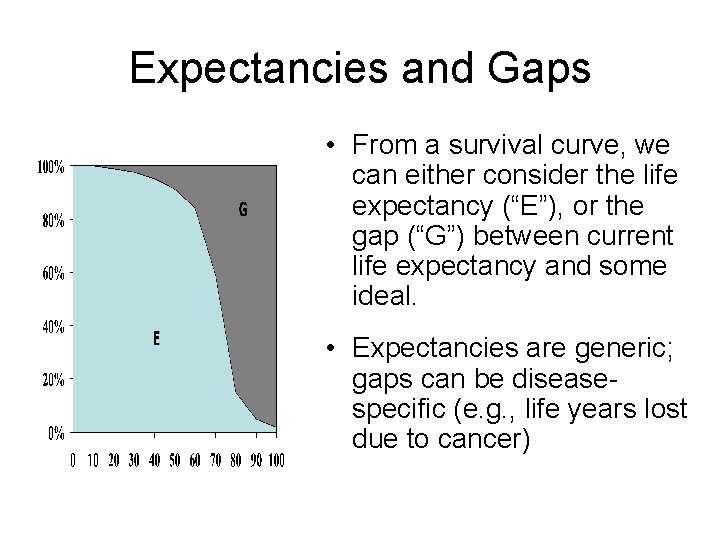
Expectancies and Gaps • From a survival curve, we can either consider the life expectancy (“E”), or the gap (“G”) between current life expectancy and some ideal. • Expectancies are generic; gaps can be diseasespecific (e. g. , life years lost due to cancer)
Classifying Health Gaps • Gap compare population health to some target: Difference between time lived in health states less than ideal health and the target ideal • The implied norm or target can be arbitrary, but must be explicit and the same for all populations being compared. The precise value does not matter
Gap measures: Expected Years of Life Lost • Compares individuals’ age of death to population life expectancy – Problems: different countries may have different life expectancies – It’s overall mortality, so cannot identify impact of a particular disease. • Standard Expected Years of Life Lost – Reference is to an “ideal” life expectancy • E. g. , Japan (82 years for women) • Area between survivorship curve and the chosen norm
Potential Years of Life Lost (PYLL) • PYLL = ( “normal age at death” – actual age at death). Doesn’t much matter what age is chosen as reference; typically 75 • Attempts to represent impact of a disease on the population: death at a young age is a greater loss than death of an elderly person • Focuses attention on conditions that kill younger people (accidents; cancers) • All-cause or cause-specific
3. Aggregate Measures that Combine Mortality & Morbidity Health expectancies Health gaps
Composite Measures • Broader representation of health of a population • Composite measures combine morbidity and mortality into a health index. (An index is a numerical summary of several indicators of health) • Mortality data typically derived from life tables; morbidity indicators from health surveys, e. g. • Self-rated health • Disability or activity limitations • A generic health index
Point to Ponder… What types of individual measure can be meaningfully aggregated? Can you make an index out of – Fingerprint patterns – Personality – Eye colour – Loneliness?
Sidebar: Different Types of Morbidity Scales for Use in Composite Measures • Generic instruments cover a wide range of health topics, e. g. reflecting the WHO definition. These can be health profiles (e. g. , Sickness Impact Profile, SF-36) or “health indexes” (e. g. , Health Utilities Index, Euro. Qol) • Specific instruments – Disease-specific (e. g. , Arthritis Impact Measurement Scale) – Age-specific (e. g. , Child Behavior Checklist) – Gender-specific (e. g. , Women’s Health Questionnaire)
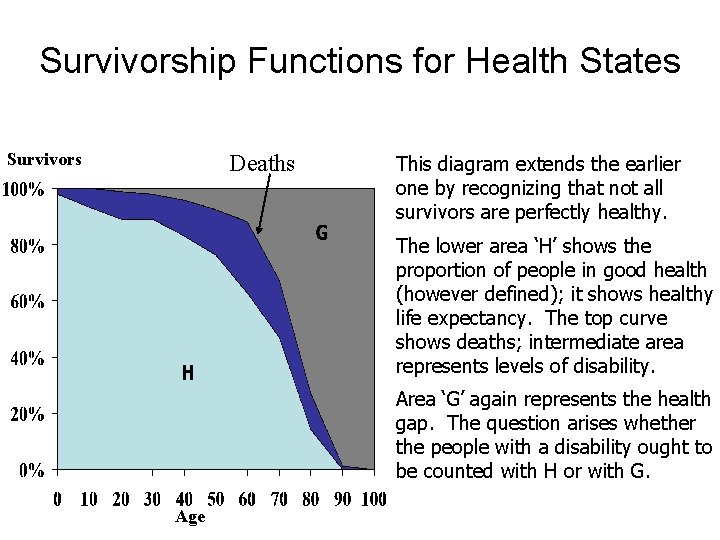
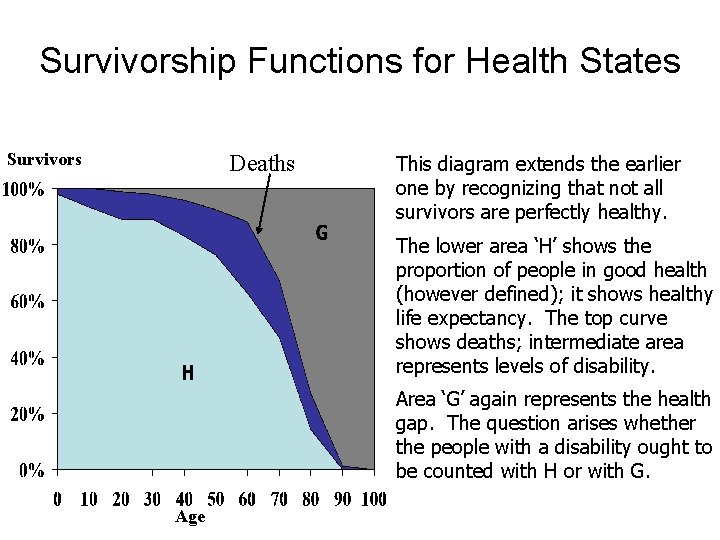
Survivorship Functions for Health States Survivors Deaths This diagram extends the earlier one by recognizing that not all survivors are perfectly healthy. The lower area ‘H’ shows the proportion of people in good health (however defined); it shows healthy life expectancy. The top curve shows deaths; intermediate area represents levels of disability. Area ‘G’ again represents the health gap. The question arises whether the people with a disability ought to be counted with H or with G. Age

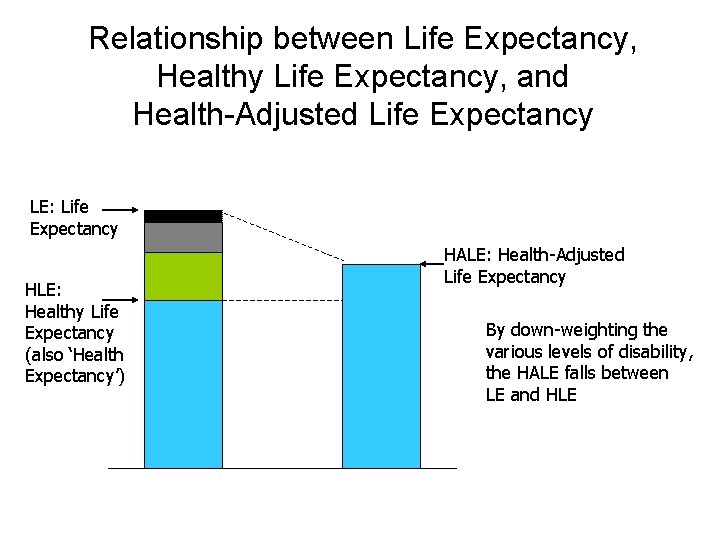
More details on the combined indicators • From the previous chart: – We can still read from the bottom, and talk of “health expectancies, ” or from the top, and create gap indexes: years of life lost, etc. – The value of a life lived in less than perfect health is less than a healthy life-year. This leads to “health-adjusted life expectancy” – The indicators will fall in a descending sequence: overall life expectancy, then health-adjusted life expectancy, then healthy life expectancy.

A Simple Presentation: Life Expectancy and Disability-Free Life Expectancy, Canada, 1986 -1991 Years Life Expectancy from birth Disability-Free Life Expectancy (‘DFLE’) M F 1986 M 1991 F
Health expectancy measures • Generic term: expected duration of life in various states of health. • Includes more specific terms such as Disability-Free Life Expectancy (DFLE) • Two main classes: 1. Dichotomous rating: healthy vs. unhealthy 2. Health state valuations for a range of levels
I. Dichotomous expectancies • Full health is rated 1; any state of poor health (mild, moderate, severe disability) is rated 0. • Average across a population. • This leads to Disability-free life expectancy (DFLE): weight of 1 for “no disability” and 0 for all other states. • = Expectation of life with no disability, or “Healthy Life Expectancy (HLE)”. • Very sensitive to threshold chosen for defining ‘disability’.

II. Polytomous states and valuations • These incorporate many levels of disability into life expectancy estimates, counting time spent in each level of disability. • Weights assigned to each disability level; generally 0 to 1. 0. These are multiplied by average time in each level and summed over different diseases. • = “Health-adjusted life expectancy (HALE)” • Recent work uses utility weights, e. g. from Health Utilities Index, Quality of Well-Being Scale, EUROQo. L, etc.
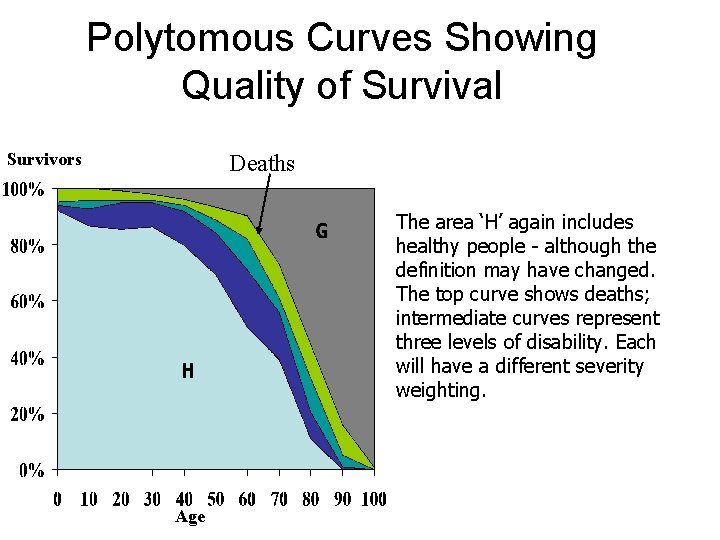
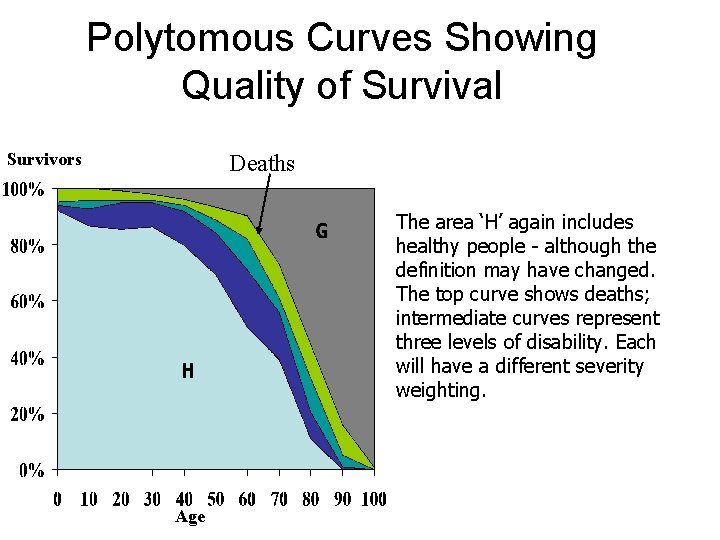
Polytomous Curves Showing Quality of Survival Survivors Deaths The area ‘H’ again includes healthy people - although the definition may have changed. The top curve shows deaths; intermediate curves represent three levels of disability. Each will have a different severity weighting. Age
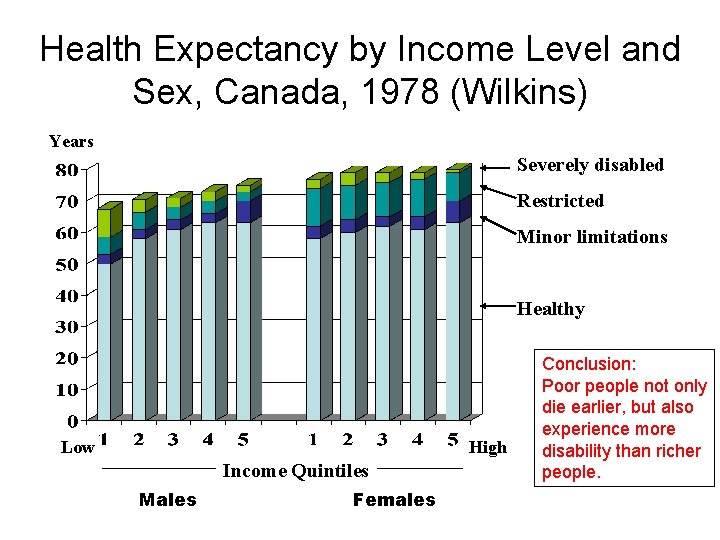
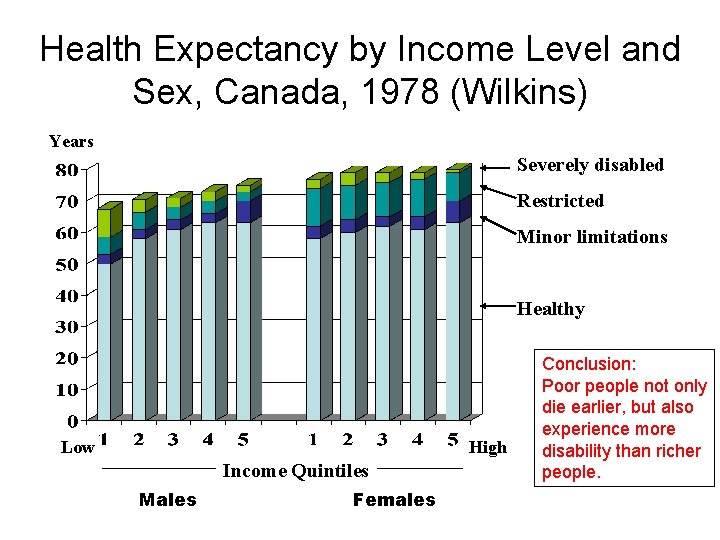
Health Expectancy by Income Level and Sex, Canada, 1978 (Wilkins) Years Severely disabled Restricted Minor limitations Healthy Low High Income Quintiles Males Females Conclusion: Poor people not only die earlier, but also experience more disability than richer people.
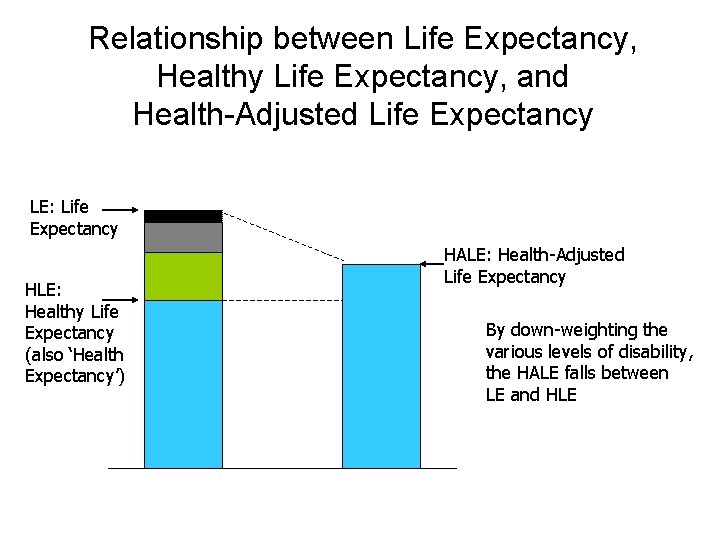
Relationship between Life Expectancy, Healthy Life Expectancy, and Health-Adjusted Life Expectancy LE: Life Expectancy HLE: Healthy Life Expectancy (also ‘Health Expectancy’) HALE: Health-Adjusted Life Expectancy By down-weighting the various levels of disability, the HALE falls between LE and HLE
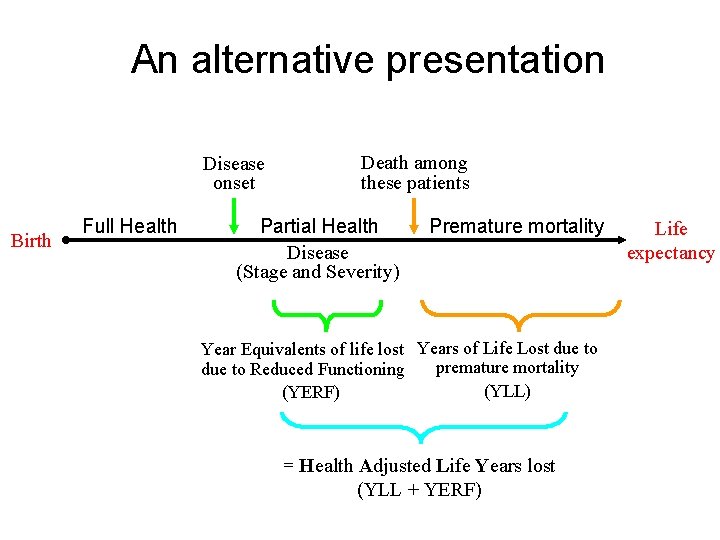
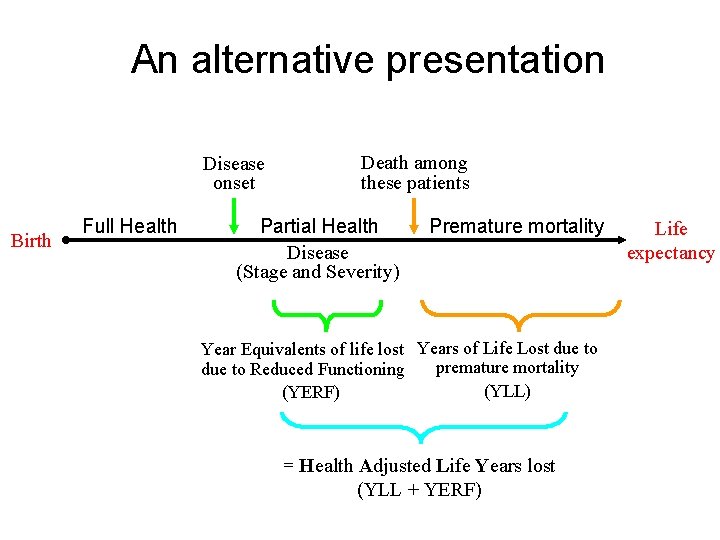
An alternative presentation Disease onset Birth Full Health Death among these patients Partial Health Premature mortality Disease (Stage and Severity) Year Equivalents of life lost Years of Life Lost due to premature mortality due to Reduced Functioning (YLL) (YERF) = Health Adjusted Life Years lost (YLL + YERF) Life expectancy
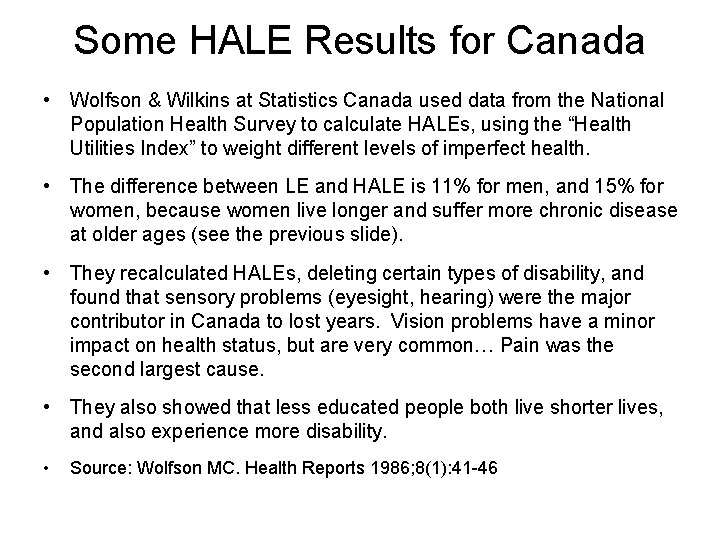
Some HALE Results for Canada • Wolfson & Wilkins at Statistics Canada used data from the National Population Health Survey to calculate HALEs, using the “Health Utilities Index” to weight different levels of imperfect health. • The difference between LE and HALE is 11% for men, and 15% for women, because women live longer and suffer more chronic disease at older ages (see the previous slide). • They recalculated HALEs, deleting certain types of disability, and found that sensory problems (eyesight, hearing) were the major contributor in Canada to lost years. Vision problems have a minor impact on health status, but are very common… Pain was the second largest cause. • They also showed that less educated people both live shorter lives, and also experience more disability. • Source: Wolfson MC. Health Reports 1986; 8(1): 41 -46
Gap Measures: QALYs & DALYs • Gap measures can also use a weighting for intermediate health states. This is necessary to combine time lost due to ill health with time lost due to premature mortality • Quality Adjusted Life Years (QALYs) – Can be expressed as lost (to disease) or gained (through an intervention) – Common outcome measurement in clinical trials, program evaluation, recording extra years of life provided by therapy + the quality of that life – Typically use utility scale running from 0 to 1 • DALYS (disability-adjusted life years) lost = basically the same idea.

Standard Life Expectancy (SLE) Health expectancy measures Health-Adjusted or Disability-Adjusted Life Years lost (HALYs or DALYs) Age Mean Life Expectancy (LE) Years Lived with Disability (YLD) Health-Adjusted, or Disability-Adjusted Life Expectancy (HALE or DALE) Healthy Life Expectancy (HLE), or Disability-Free Life Expectancy (DFLE) Health gap measures Standard Expected Years of Life Lost (SEYLL)

4. When do we Use Each Type of Measure? Towards a Functional Classification
Recall our Classification of Measures: 1. Descriptive measures: i. To record current health status; ii. To evaluate change in health status 2. Analytic measures: iii. Predictive methods that look forward; iv. Explanatory measures that look backwards.
Characteristics of Descriptive Measures • • • Intuitively simple – cover themes of interest to people in general (“quality of life”, etc) Reflect values; possible political influence Time frame = present Emphasis on modifiable themes Goal = to make broad classifications
Characteristics of Evaluative Measures • • • Fine-grained: select indicators that sample densely from relevant level of severity Need to be sensitive to change produced by particular intervention Content tailored to intervention; usually not comprehensive Common emphasis on summary score But should also cover potential side-effects

Match the Instrument to the Application Population Monitoring Outcomes Research Patient Management 4 3 2 1 Source: John Ware, October 2000

Characteristics of Predictive Measures • • Content can be selective rather than comprehensive Items not necessarily modifiable, or even very important If derived from discriminant analysis, likely to be parsimonious Focus on algorithmic scoring and interpretation (e. g. , either x or y, plus z in the absence of w)
Characteristics of Explanatory Measures • • Can combine various types of measures & classifications, ranging from distal to proximal Based on a conceptual model, rather than empirically based There can therefore be rival explanatory approaches Content not necessarily modifiable factors, but these would be desirable
5. Environmental Measures Compositional vs. Contextual Measures
Compositional • Demographics; age, ethnic composition, lone parents, dependency ratios, etc • Population resources: wealth, educational levels, etc • Community: social cohesion, watch programs, participation (voting, donations, etc)

Contextual • Neighbourhood type, quality; amenities, transportation • Employment opportunities • Access to care • Environmental quality: pollution levels: air, water, noise • Climate • Equity

Assymetries Some aggregated measures do not have Some environmental variables have no a meaningful individual counterpart: – – Population density Income inequality % unemployed GNP – – Air quality (SO 2) Road traffic density Ambient temperature Land use
6. Global Measures Income inequalities, Health inequalities.
Some examples of global measures • Social solidarity; sense of identity; artistic output; public interest in health issues, etc. • Indicators of societal support: the “safety net” • Quality of social institutions for health (health protection laws, etc. ) • Social cohesion, neighbourhood quality, social capital
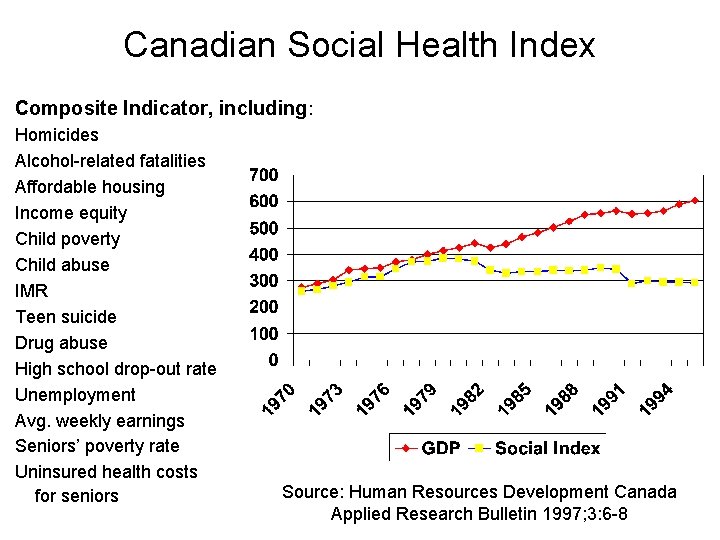
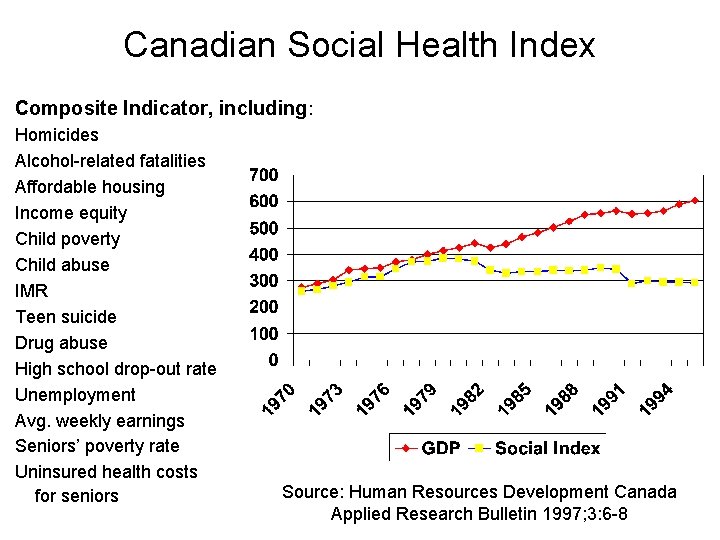
Canadian Social Health Index Composite Indicator, including: Homicides Alcohol-related fatalities Affordable housing Income equity Child poverty Child abuse IMR Teen suicide Drug abuse High school drop-out rate Unemployment Avg. weekly earnings Seniors’ poverty rate Uninsured health costs for seniors Source: Human Resources Development Canada Applied Research Bulletin 1997; 3: 6 -8

Measures of health distribution: Health Inequalities • Several possible indicators; • Can be relative or absolute; • They may choose different reference points and vary in whether they weight scores by population size. • The choice of summary measure of disparity affects the interpretation of changes in health disparities.
Indicators of Relative Disparities (1) • Rate Ratio (RR) - the ratio of the health status of the least healthy group to that of the most healthy. Value = 1 if no disparity. • Index of Disparity (IDisp) - average difference between rates of disease in several groups and a reference rate, expressed as the proportion of the reference rate (i. e. a ratio). Commonly the best group rate is used as the reference since it represents the rate that all groups might aspire to. If no disparity, the index = 0. • Relative Index of Inequality (RII): Ratio of morbidity or mortality rates between those at bottom of SES range to those at top. This is estimated using regression and corrects for other factors. •

Relative Disparities (2) • Relative Concentration Index (RCI) - how much health or illness is concentrated among ranked social groups (e. g. educational levels, or wealth). Index weighted according to relative size of the groups. It takes on positive or negative values, showing direction of the relationship. Score = 0 when no disparity. • Theil Index (TI) and Mean Log Deviation (MLD) - these summarize disproportionality between shares of health and shares of population, expressed as a ratio on a log scale, compared to overall rate in the population and weighted by group sizes. Log scale makes this index more sensitive to health differences further from the average than other measures. • [Note that using weighting as in RCI or Theil counts all individuals equally, while unweighted indices count all groups
Absolute Indicators of Disparities • Rate difference (RD) - simple arithmetic difference, typically between the lowest & highest disease rates. Also known as the Slope Index of Inequality • Between-group variance (BGV) – sum of squared deviations from a population average, weighted by group sizes. • Absolute Concentration Index (ACI) - measures the extent to which health or illness is concentrated among particular social groups on the absolute scale, used with ordinally ranked social groups. Calculated as RCI x mean of the health variable. If no disparity, ACI = 0. • Index of Dissimilarity: Absolute number or percentage of all cases that must be redistributed to obtain the same mortality rate for all SES groups.
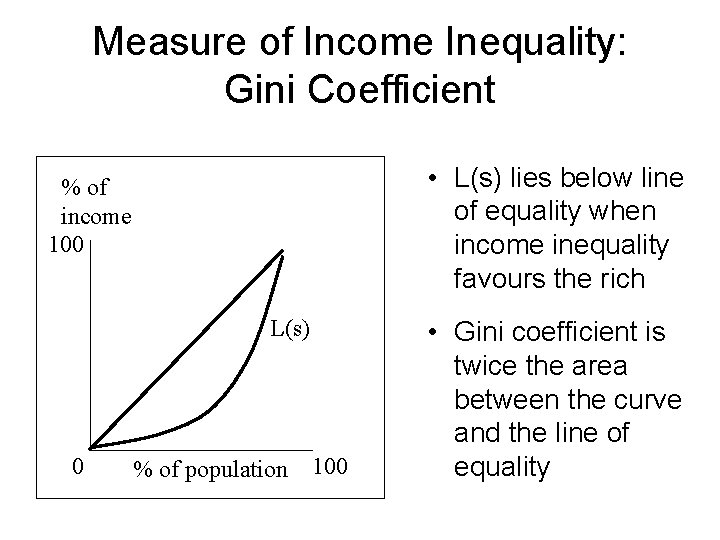
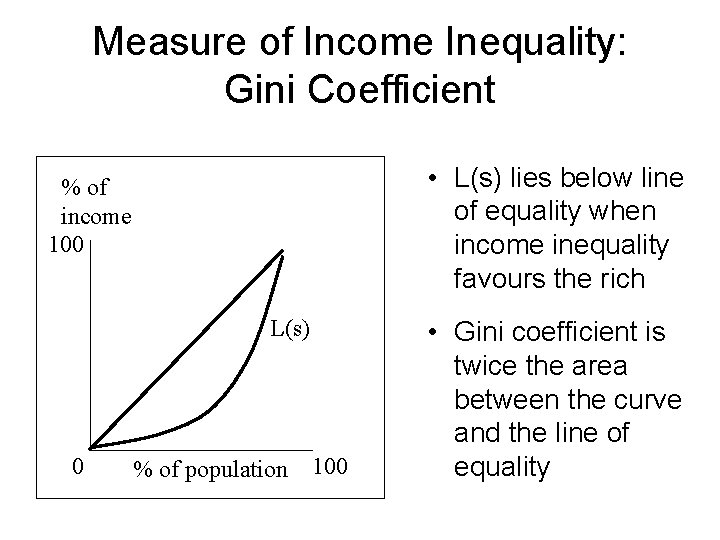
Measure of Income Inequality: Gini Coefficient • L(s) lies below line of equality when income inequality favours the rich % of income 100 L(s) 0 % of population 100 • Gini coefficient is twice the area between the curve and the line of equality
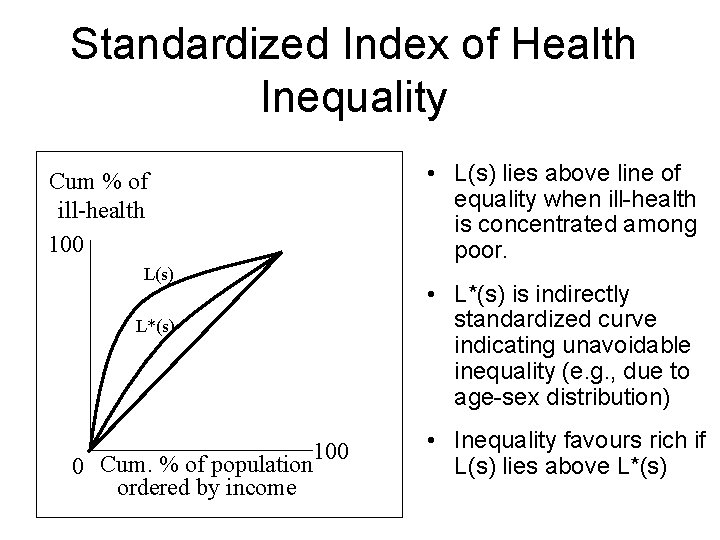
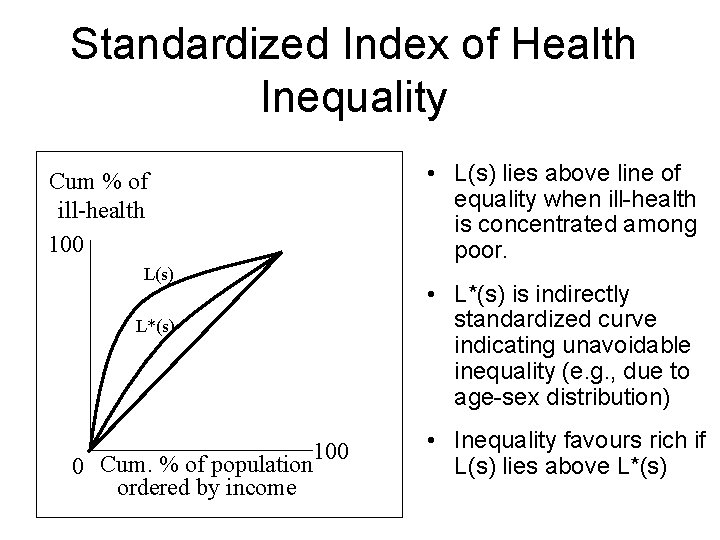
Standardized Index of Health Inequality Cum % of ill-health 100 L(s) L*(s) 100 0 Cum. % of population ordered by income • L(s) lies above line of equality when ill-health is concentrated among poor. • L*(s) is indirectly standardized curve indicating unavoidable inequality (e. g. , due to age-sex distribution) • Inequality favours rich if L(s) lies above L*(s)
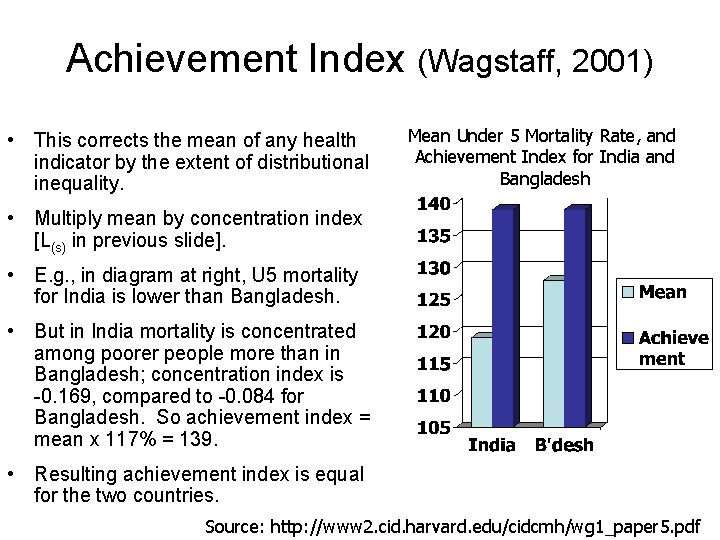
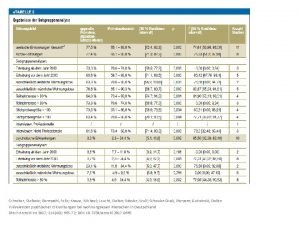
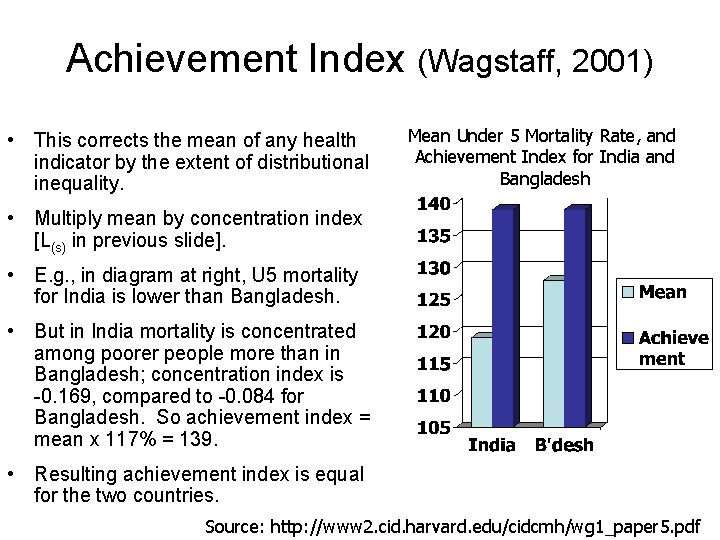
Achievement Index (Wagstaff, 2001) • This corrects the mean of any health indicator by the extent of distributional inequality. Mean Under 5 Mortality Rate, and Achievement Index for India and Bangladesh • Multiply mean by concentration index [L(s) in previous slide]. • E. g. , in diagram at right, U 5 mortality for India is lower than Bangladesh. • But in India mortality is concentrated among poorer people more than in Bangladesh; concentration index is -0. 169, compared to -0. 084 for Bangladesh. So achievement index = mean x 117% = 139. • Resulting achievement index is equal for the two countries. Source: http: //www 2. cid. harvard. edu/cidcmh/wg 1_paper 5. pdf
Acute Multidimensional Poverty: An Index for Developing Countries • Sabina Alkire, Oxford Poverty & Human Development Initiative. • Multidimensional Poverty Index (MPI) for 104 developing countries. It assesses the nature and intensity of poverty at the individual level in education, health outcomes, and standard of living. • The MPI captures direct failures in functionings that Amartya Sen argues should form the focus for describing poverty. It is used to target the poorest, track the Millennium Development Goals, and design policies that address the interlocking deprivations poor people experience. • 1, 700 million people in the world live in acute poverty, a figure that is between the $1. 25/day and $2/day poverty rates • MPI available at: http: //www. ophi. org. uk/policy/multidimensionalpoverty-index/ • Report available online PDF [133 p. ] at: http: //bit. ly/9 Ds 9 wt
Measures of Impact of Interventions to Reduce Inequalities • Population attributable risk: The reduction in health gap that would occur if everyone experienced the rates in the highest socioeconomic group • Population attributable life lost index: The absolute or proportional increase in life expectancy if everyone experienced the life expectancy of the highest SES group
 Factors of 2
Factors of 2 Mc dowell
Mc dowell Leone lattes biography
Leone lattes biography Dowell
Dowell Dowell curves
Dowell curves What are the approaches to measuring performance
What are the approaches to measuring performance Defining performance and choosing a measurement approach
Defining performance and choosing a measurement approach Section 1 population dynamics answer key
Section 1 population dynamics answer key Population ecology section 1 population dynamics answer key
Population ecology section 1 population dynamics answer key Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Population ecology section 1 population dynamics
Population ecology section 1 population dynamics Health promotion approaches
Health promotion approaches Public health approaches
Public health approaches Electromagnetic waves vocabulary
Electromagnetic waves vocabulary Population health risk assessment and management
Population health risk assessment and management Key issue 3 why do some places face health challenges
Key issue 3 why do some places face health challenges 99243 cpt code
99243 cpt code Population health 101
Population health 101 Population health program manager
Population health program manager Ian milborrow pwc
Ian milborrow pwc Ian juliano
Ian juliano Cloud ral
Cloud ral Dr ian arnott
Dr ian arnott Ian scott international
Ian scott international Ian lipio
Ian lipio Ian coddington
Ian coddington Ian j goodfellow
Ian j goodfellow Ian crotty
Ian crotty Ian slater dwf
Ian slater dwf Ian lindsley
Ian lindsley Ian proulx
Ian proulx Ian rice md
Ian rice md A mcpherson pro reunion
A mcpherson pro reunion Ian thurgood
Ian thurgood Ian jarman
Ian jarman Ian mundy
Ian mundy Thinking history ian dawson
Thinking history ian dawson Ian gordon lawyer
Ian gordon lawyer Overfitting
Overfitting Gans
Gans Ian tibbetts
Ian tibbetts Ian white ucl
Ian white ucl Cmu proxy
Cmu proxy Ian hembry
Ian hembry Dr ian sando
Dr ian sando Ian watt the rise of the novel summary
Ian watt the rise of the novel summary Michael leucht
Michael leucht Ian tharp
Ian tharp Oak tree care services
Oak tree care services Mungol
Mungol Dr ian gallimore
Dr ian gallimore Mr lawson ict
Mr lawson ict Ian walker economics
Ian walker economics Professor ian wilcox
Professor ian wilcox Ian viney
Ian viney Ian buck nvidia
Ian buck nvidia