Approach to patients with Dyspnea Dr Hadil Al
















- Slides: 42
Approach to patients with Dyspnea Dr. Hadil Al Otair MRCP, FCCP
Dyspnea • Definition: An unpleasant or uncomfortable awareness of breathing.
• Outline: - Control of breathing - Causes of acute dyspnea & their clinical features - Causes of chronic dyspnea - Investigations for chronic dyspnea
Dyspnoea An unpleasant or uncomfortable awareness of breathing Ability to breathing ↑Demand
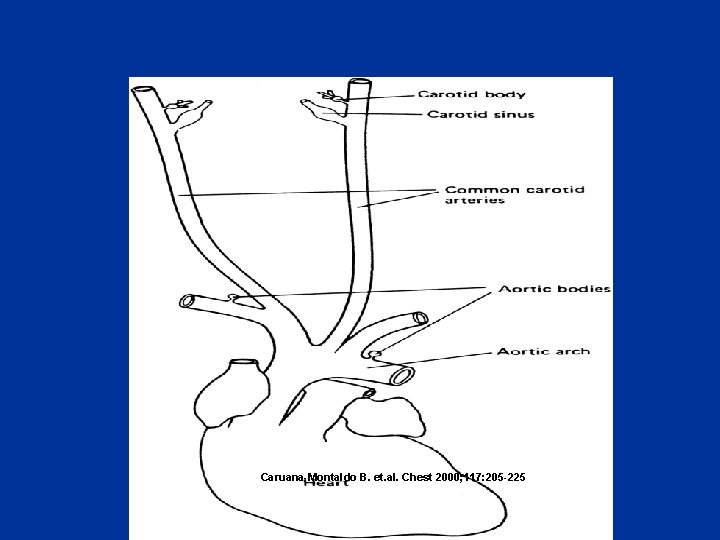
Control of breathing • Afferent (sensory ) information Chemoreceptors: Central (medulla) Peripheral (Carotid &Aortic bodies) Mechanoreceptors (Airways , lungs, chest wall) • Respiratory control system • Efferent respiratory discharges to ventilatory muscles

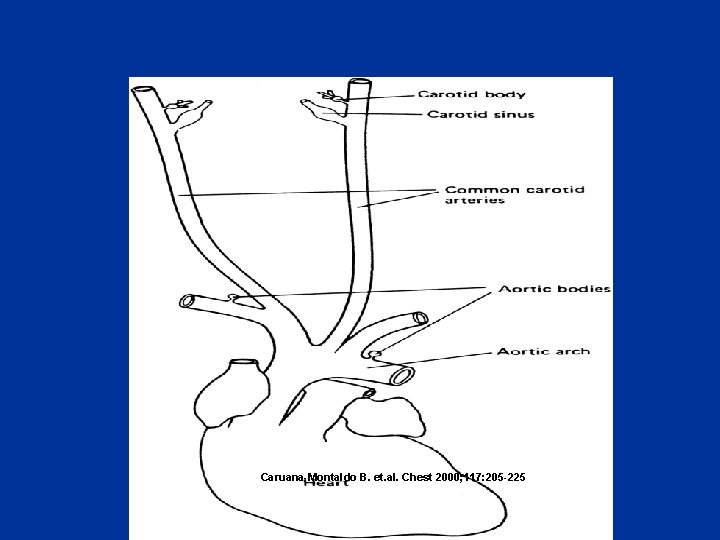
Caruana-Montaldo B. et. al. Chest 2000; 117: 205 -225



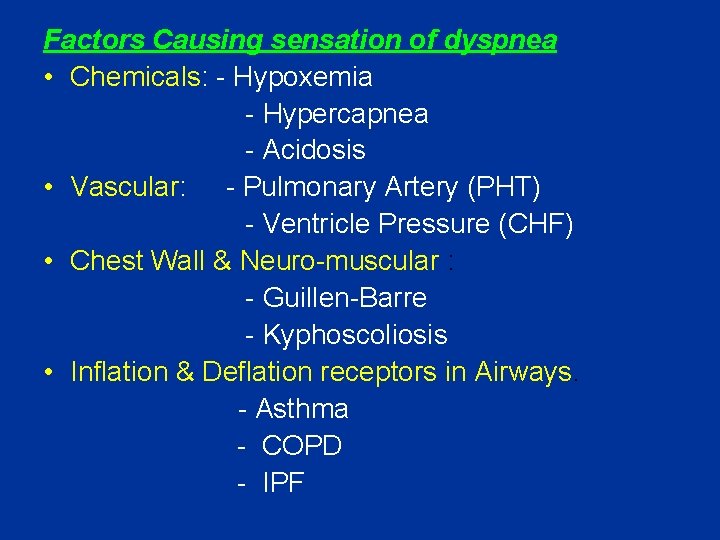
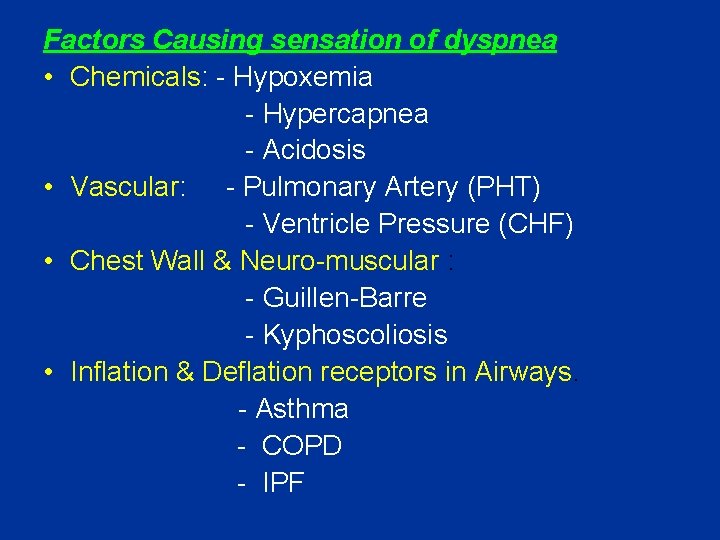
Factors Causing sensation of dyspnea • Chemicals: - Hypoxemia - Hypercapnea - Acidosis • Vascular: - Pulmonary Artery (PHT) - Ventricle Pressure (CHF) • Chest Wall & Neuro-muscular : - Guillen-Barre - Kyphoscoliosis • Inflation & Deflation receptors in Airways. - Asthma - COPD - IPF
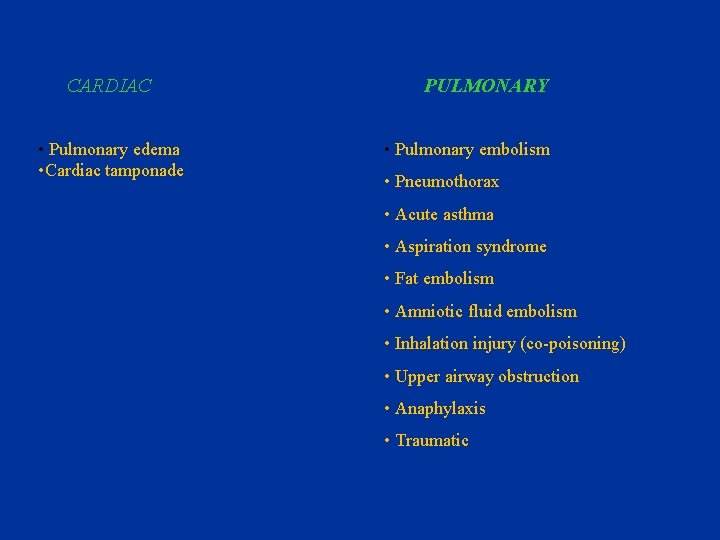
CARDIAC • Pulmonary edema • Cardiac tamponade PULMONARY • Pulmonary embolism • Pneumothorax • Acute asthma • Aspiration syndrome • Fat embolism • Amniotic fluid embolism • Inhalation injury (co-poisoning) • Upper airway obstruction • Anaphylaxis • Traumatic

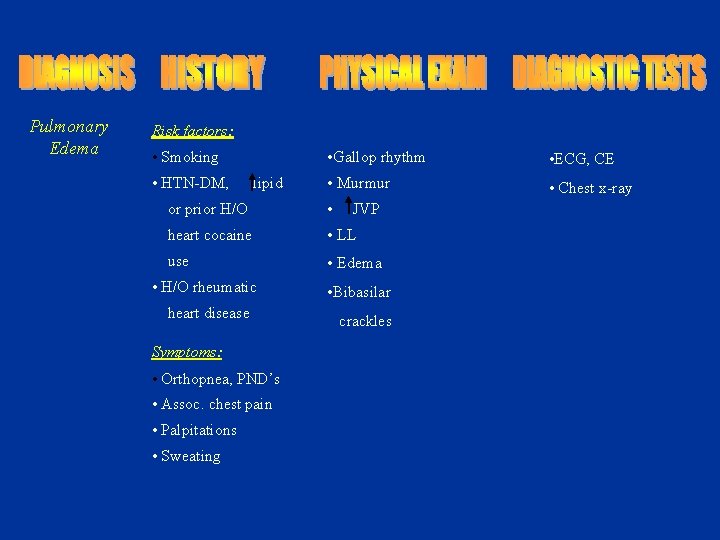
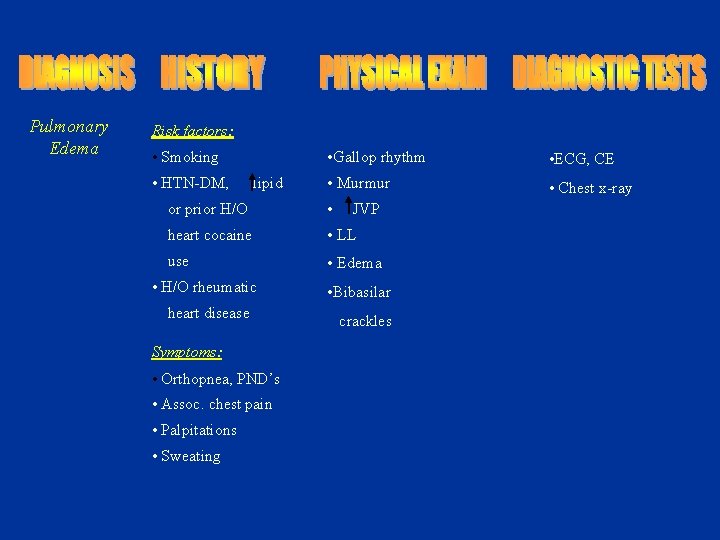
Pulmonary Edema Risk factors: • Smoking • HTN-DM, lipid • Gallop rhythm • ECG, CE • Murmur • Chest x-ray or prior H/O • heart cocaine • LL use • Edema • H/O rheumatic heart disease Symptoms: • Orthopnea, PND’s • Assoc. chest pain • Palpitations • Sweating JVP • Bibasilar crackles
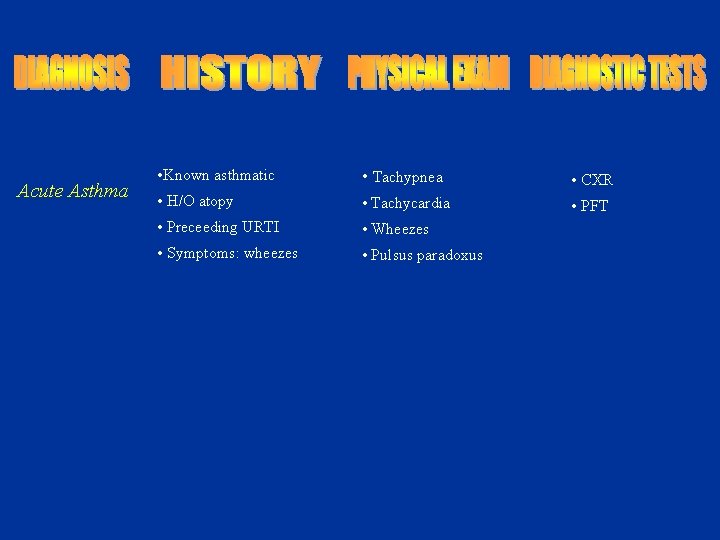
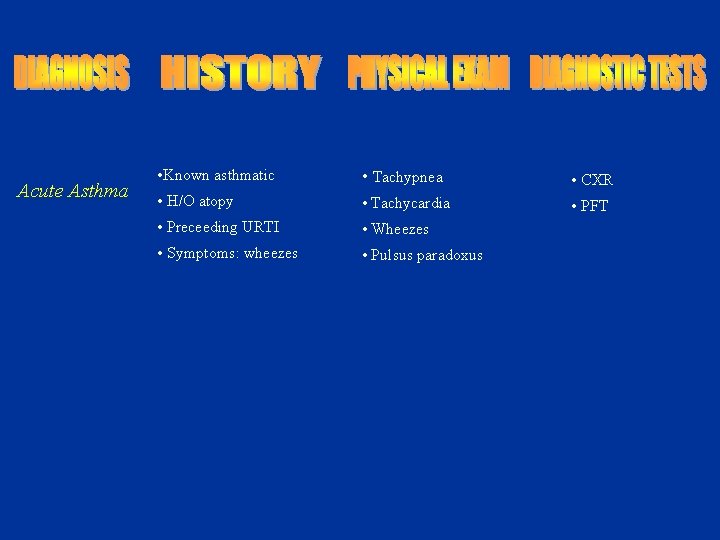
Acute Asthma • Known asthmatic • Tachypnea • CXR • H/O atopy • Tachycardia • PFT • Preceeding URTI • Wheezes • Symptoms: wheezes • Pulsus paradoxus
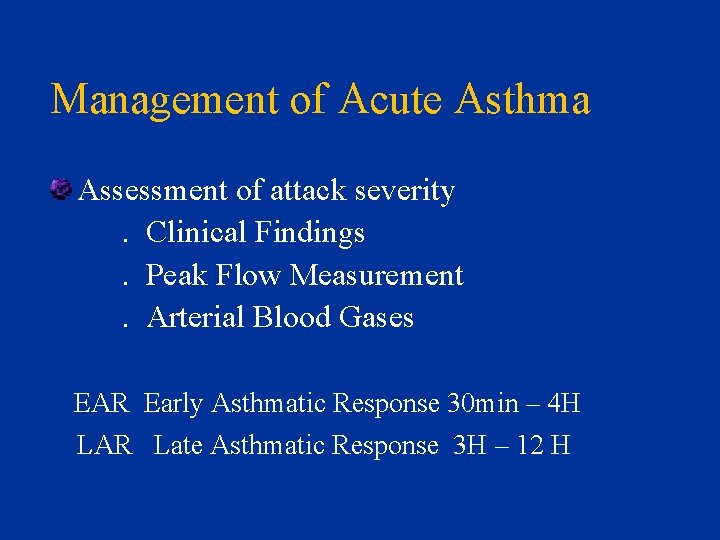
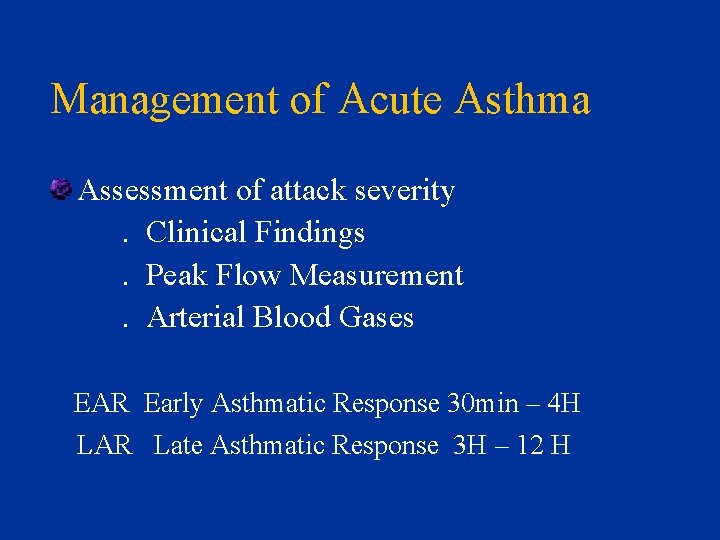
Management of Acute Asthma Assessment of attack severity. Clinical Findings. Peak Flow Measurement. Arterial Blood Gases EAR Early Asthmatic Response 30 min – 4 H LAR Late Asthmatic Response 3 H – 12 H



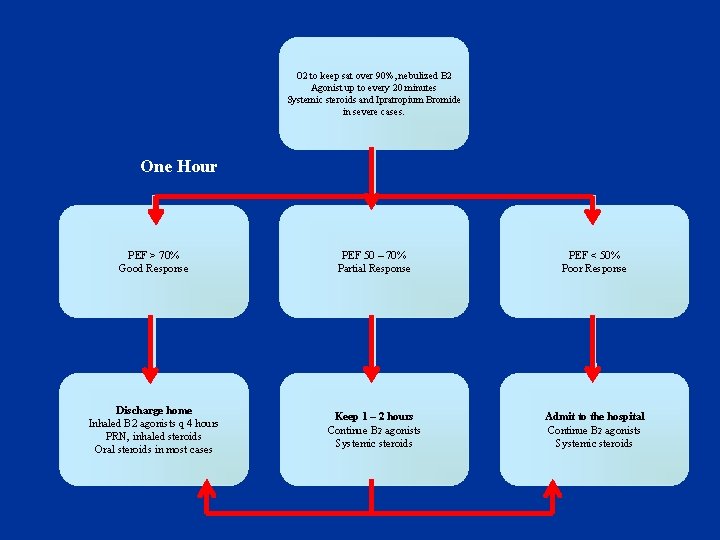
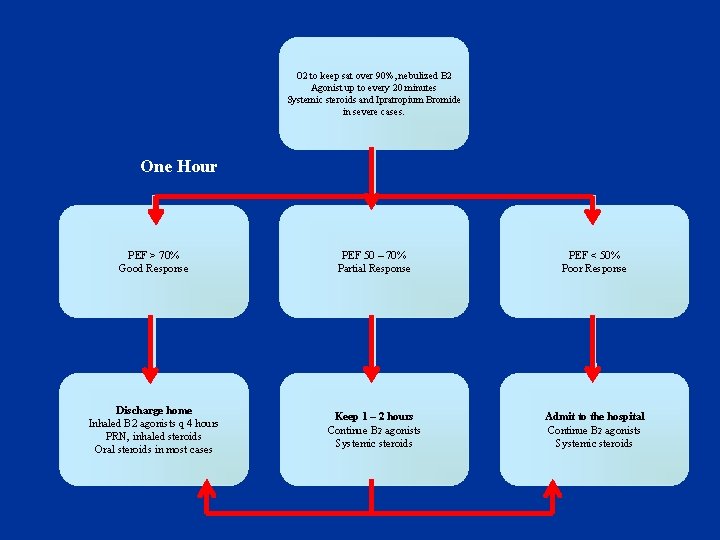
O 2 to keep sat over 90%, nebulized B 2 Agonist up to every 20 minutes Systemic steroids and Ipratropium Bromide in severe cases. One Hour PEF > 70% Good Response PEF 50 – 70% Partial Response PEF < 50% Poor Response Discharge home Inhaled B 2 agonists q 4 hours PRN, inhaled steroids Oral steroids in most cases Keep 1 – 2 hours Continue B 2 agonists Systemic steroids Admit to the hospital Continue B 2 agonists Systemic steroids
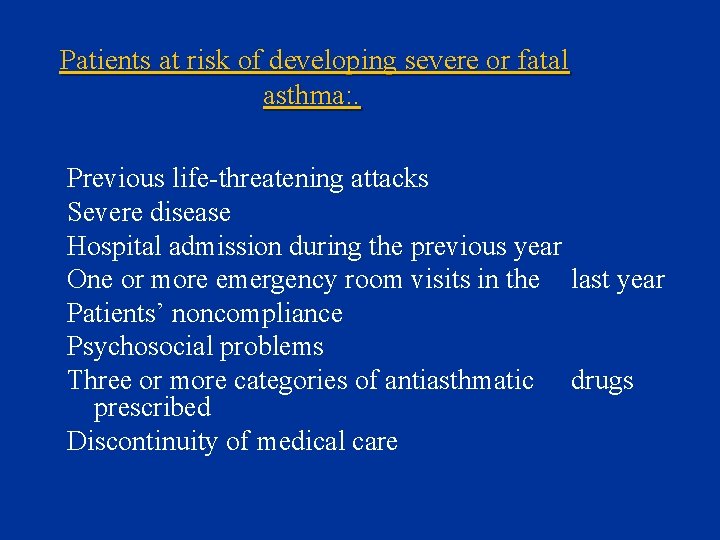
Patients at risk of developing severe or fatal asthma: . Previous life-threatening attacks Severe disease Hospital admission during the previous year One or more emergency room visits in the last year Patients’ noncompliance Psychosocial problems Three or more categories of antiasthmatic drugs prescribed Discontinuity of medical care
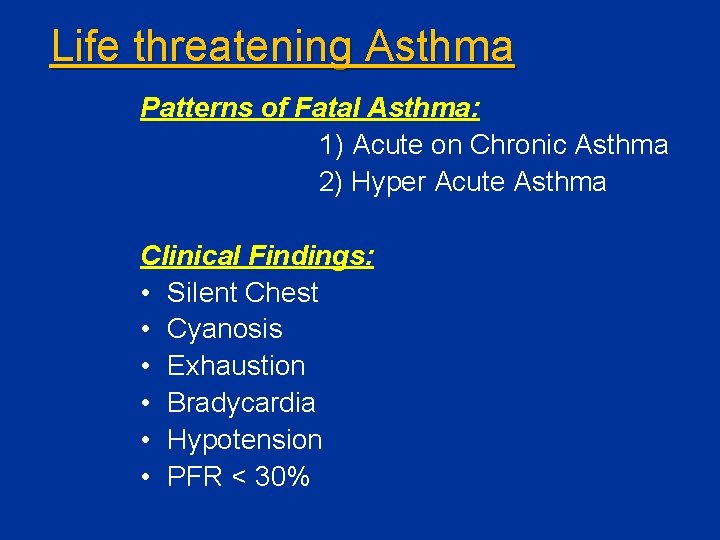
Life threatening Asthma Patterns of Fatal Asthma: 1) Acute on Chronic Asthma 2) Hyper Acute Asthma Clinical Findings: • Silent Chest • Cyanosis • Exhaustion • Bradycardia • Hypotension • PFR < 30%
PULMONARY EMBOLISM • • • Risk factors Presenting Symptoms Physical Findings Investigations Therapy
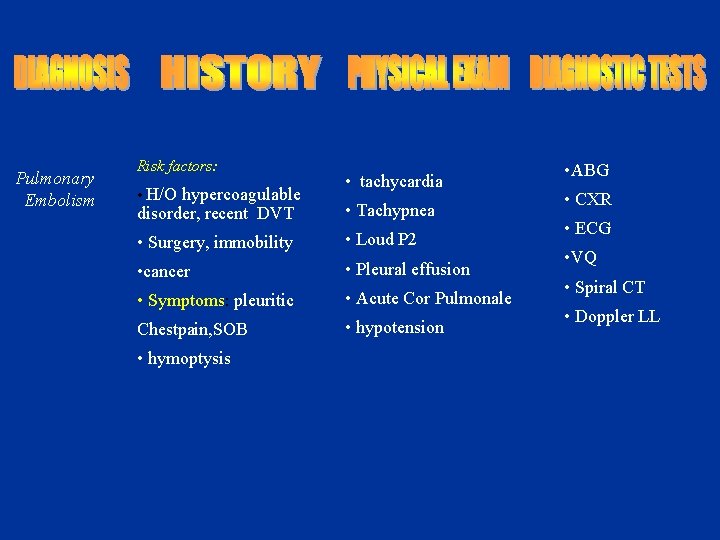
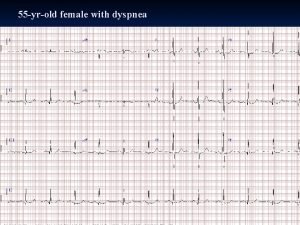
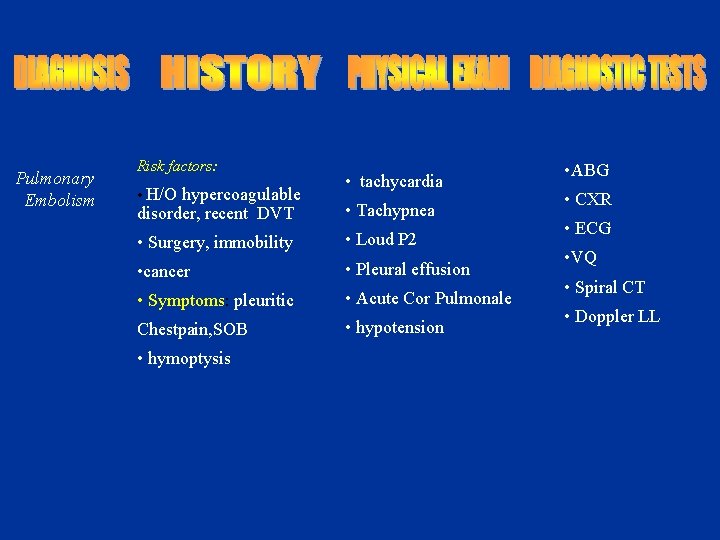
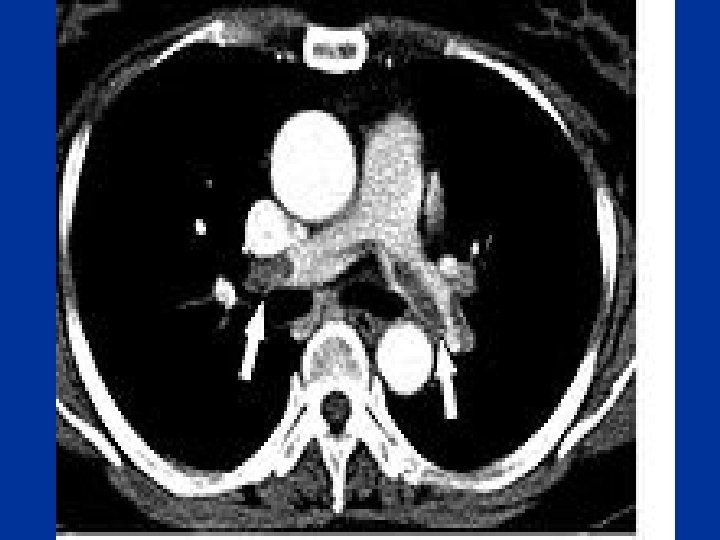
Pulmonary Embolism Risk factors: • H/O hypercoagulable • tachycardia disorder, recent DVT • Tachypnea • Surgery, immobility • Loud P 2 • cancer • Pleural effusion • Symptoms: pleuritic • Acute Cor Pulmonale Chestpain, SOB • hypotension • hymoptysis • ABG • CXR • ECG • VQ • Spiral CT • Doppler LL


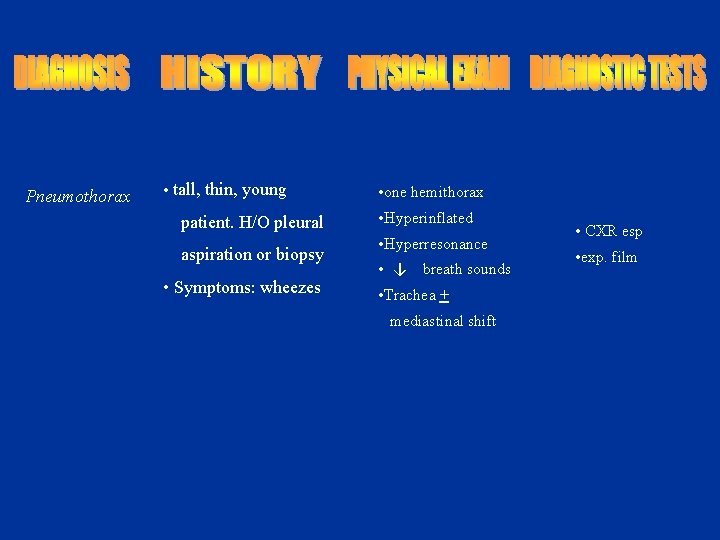
Pneumothorax • tall, thin, young patient. H/O pleural aspiration or biopsy • Symptoms: wheezes • one hemithorax • Hyperinflated • Hyperresonance • ↓ breath sounds • Trachea + mediastinal shift • CXR esp • exp. film

Pneumothorax • Major Types: • Spontaneous: Primary peak 20 -30 yrs, 4: 1 male : female • Tall thin , cigarette smokers, positive family history Secondary: Parenchymal lung disease e. g sarcoidosis, IPF, Emphysema, Necrotising pneumonia incl. Tb, PCP, • Iatrogenic: Pleural tap, transbronchial lung biopsy, positive pressure ventilation. • Traumatic: Rib fracture, bronchial rupture, esophageal rupture
Pneumothorax Mechanism • rupture of subpleural bleb or parenchymal process eroding visceral pleura this may also cause partial bronchial obstruction(check -valve mechanism) & hyperinflation
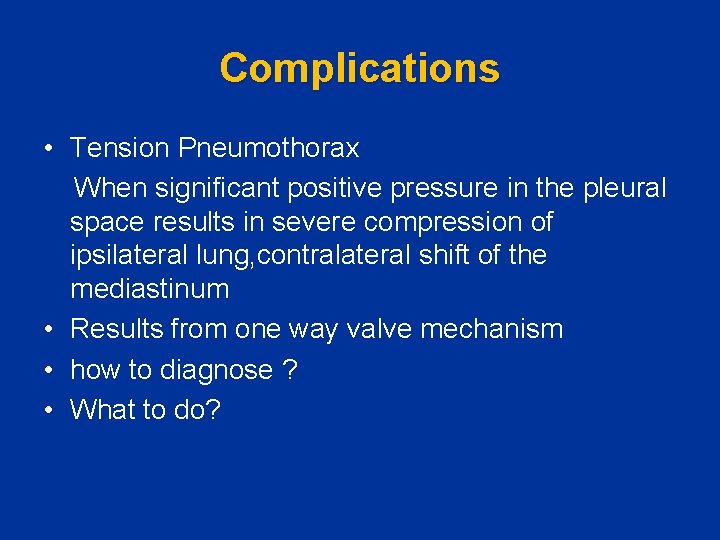
Complications • Tension Pneumothorax When significant positive pressure in the pleural space results in severe compression of ipsilateral lung, contralateral shift of the mediastinum • Results from one way valve mechanism • how to diagnose ? • What to do?
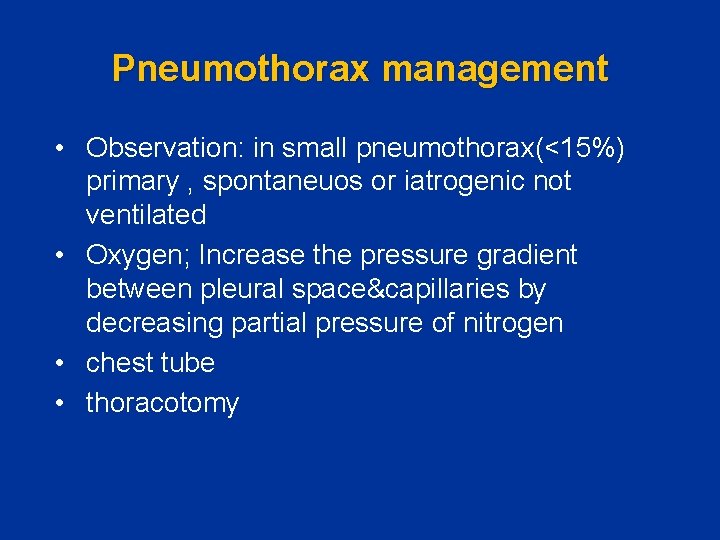
Pneumothorax management • Observation: in small pneumothorax(<15%) primary , spontaneuos or iatrogenic not ventilated • Oxygen; Increase the pressure gradient between pleural space&capillaries by decreasing partial pressure of nitrogen • chest tube • thoracotomy
• Recurrence: 10 -50% • 60% after the second recurrence • Sclerotherapy, Thoracotomy
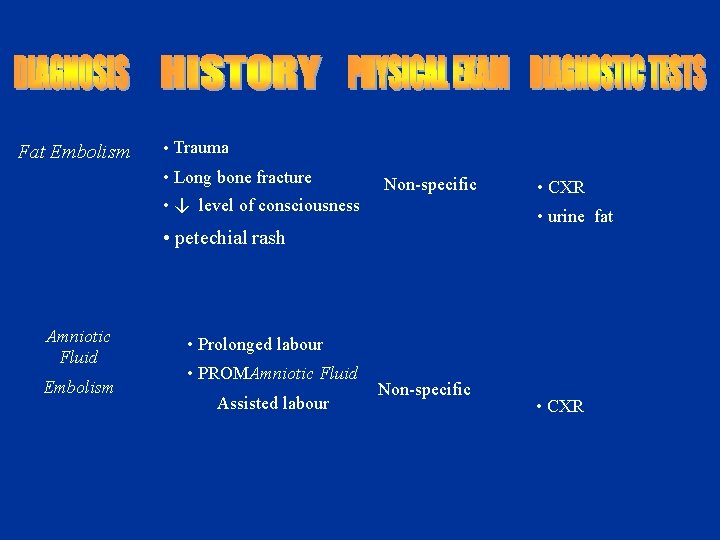
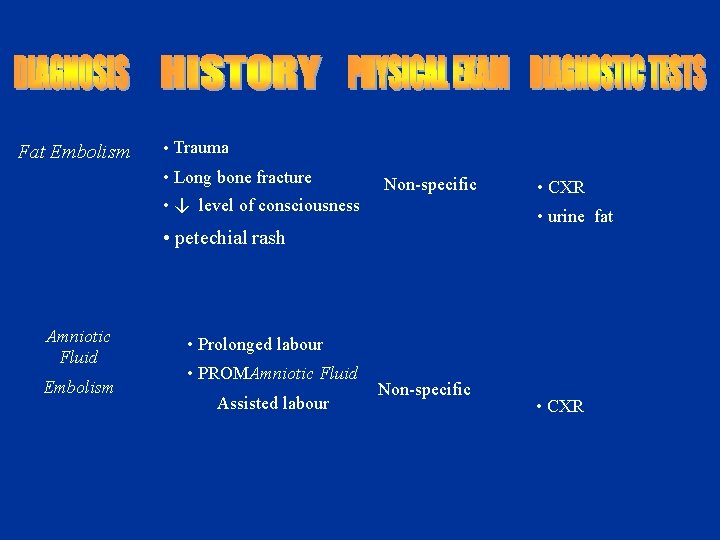
Fat Embolism • Trauma • Long bone fracture Non-specific • ↓ level of consciousness • urine fat • petechial rash Amniotic Fluid Embolism • CXR • Prolonged labour • PROMAmniotic Fluid Assisted labour Non-specific • CXR
Chronic dyspnea • Major causes: Asthma COPD Bronchiectasis Interstitial lung disease Heart failure or cardiomyopathy
Evaluation • • • History& physical exam CXR PFTS Oximetry Echocardiogram CT-lungs - I. L. D _ Bronchiectasis - Occult emphysema - Chronic thromboembolic dis. • Cardiopulmonary exercise





THANK YOU
 Hadil el jamal
Hadil el jamal Dyspnea approach
Dyspnea approach Grades of dyspnea nyha
Grades of dyspnea nyha Define dyspnea
Define dyspnea Josuel ora
Josuel ora Occupational asthma
Occupational asthma Nyha classification
Nyha classification 5 cardinal signs
5 cardinal signs Paroxysmal nocturnal dyspnea pathophysiology
Paroxysmal nocturnal dyspnea pathophysiology Dr marwa a. ahmed
Dr marwa a. ahmed Grades of dyspnea
Grades of dyspnea Dyspnea grading nyha
Dyspnea grading nyha Dyspnea exertion scale
Dyspnea exertion scale Borg dyspnea scale
Borg dyspnea scale Dyspnea index formula
Dyspnea index formula Avoidance
Avoidance Tony wagner's seven survival skills
Tony wagner's seven survival skills A switch in a datagram network uses
A switch in a datagram network uses Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Approach research meaning
Approach research meaning Waterfall vs shower approach
Waterfall vs shower approach Traditional approach to system development
Traditional approach to system development Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Periodontal therapy in female patients
Periodontal therapy in female patients Nursing care plan for breast cancer ppt
Nursing care plan for breast cancer ppt Pico question
Pico question Cva
Cva Nursing management of patient with cataract
Nursing management of patient with cataract Dr carlson advises his depressed patients
Dr carlson advises his depressed patients Medicare improvements for patients and providers act
Medicare improvements for patients and providers act 10 patient rights
10 patient rights Diagnosis and treatment planning in complete denture
Diagnosis and treatment planning in complete denture Dealing with challenging patients
Dealing with challenging patients Patients with special challenges
Patients with special challenges Wheeled ambulance stretcher
Wheeled ambulance stretcher Factors of care patients can expect
Factors of care patients can expect Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. Safe staffing ratios: benefiting nurses and patients
Safe staffing ratios: benefiting nurses and patients Safe patient handling algorithms
Safe patient handling algorithms Wendylett sheets 1 carer
Wendylett sheets 1 carer Lifting and transporting patients introduction
Lifting and transporting patients introduction Life expectancy of sickle cell patients
Life expectancy of sickle cell patients