Dyspnea Psychological Impact on Patients Families Health Care


- Slides: 14

Dyspnea: Psychological Impact on Patients & Families & Health Care Providers Larry Librach MD, CCFP, FCFP Professor, Dept. of Family & Community Medicine Sun Life Financial Chair in Bioethics & Director Joint Centre for Bioethics, University of Toronto QI Lead , Temmy Latner Centre for Palliative Care

Importance • Perception of dyspnea is considered analogous to the perception of pain & consists of sensory (intensity) & affective (unpleasantness) dimensions • Similar cortical processes appear to underlie experience of dyspnea & pain Temmy Latner Centre 2
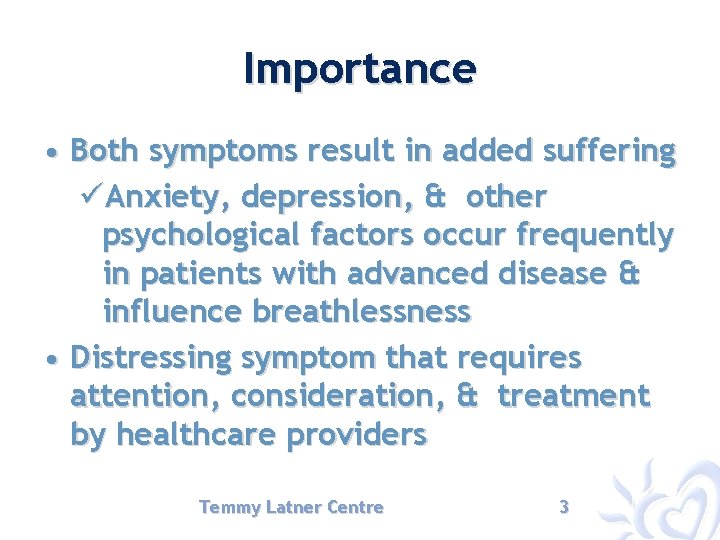
Importance • Both symptoms result in added suffering üAnxiety, depression, & other psychological factors occur frequently in patients with advanced disease & influence breathlessness • Distressing symptom that requires attention, consideration, & treatment by healthcare providers Temmy Latner Centre 3
Importance • HCPs are ethically obligated to treat dyspnea, & patients & their families should be reassured that they will be provided the means to effectively treat this symptom • Approach to care should be reflected in goals of care & care plan that involves a holistic approach Temmy Latner Centre 4
Goals of Care for Dyspnea • Because patients do not experience dyspnea in isolation but rather in conjunction with other symptoms, concomitant stressors, & spiritual or existential distress üDyspnea cannot be fully addressed unless these physical & nonphysical factors are understood. Temmy Latner Centre 5
Psychological Impact Temmy Latner Centre 6
Psychological Impact-Patient FEAR ! üOf suffocation üAdded suffering üAdded burden for family üNeed for hastened death Temmy Latner Centre 7
Neurophysiology • Anterior cingulate gyrus on cortex is area of brain that is responsible for emotional impact of physical symptoms like pain & dyspnea üLinked to thalamus by opioid sensitive pathway Temmy Latner Centre 8
Psychological Impact-Patient • Manifestations include: üAnxiety üPanic üPoor sleep üDepression Temmy Latner Centre 9
Psychological Impact-Patient • Opioids appropriate • Approach requires more than medication • Oxygen is not a panacea and may actually increase anxiety • Counselling important üReassuring conversations & education üOutline expectations üDiscuss continuing evaluation Temmy Latner Centre 10
Psychological Impact-Family • Again fear of suffocation & witnessing an agonizing death • Sense of helplessness • Anxiety about the very end of life & whether hospital the best place Temmy Latner Centre 11
Psychological Impact-Family • Approach requires regular visits, reassurance re: accessibility • Also reassurance re: role of oxygen as it is not a panacea Temmy Latner Centre 12
Psychological Impact Health Care Providers • Sense of “need to do something” • Anxiety around need for oxygen • Foreboding about suffocation • Anxiety around when to institute sedation Temmy Latner Centre 13
Summary • Dyspnea is a common symptom in palliative care üInduces great fear • Success is most likely when as many as possible of the patient’s individual dyspnea stressors & concomitant symptoms (i. e. , anxiety, depression, panic attacks) are identified & addressed Temmy Latner Centre 14
 Little families
Little families Approach to dyspnea
Approach to dyspnea Borg breathlessness scale
Borg breathlessness scale Borg dyspnea scale
Borg dyspnea scale Paroxysmal nocturnal dyspnea pathophysiology
Paroxysmal nocturnal dyspnea pathophysiology Dyspnea grading nyha
Dyspnea grading nyha Chuck kitchen
Chuck kitchen Nyha classification
Nyha classification Jihan nezir
Jihan nezir Dyspnea exertion scale
Dyspnea exertion scale Define dyspnea
Define dyspnea Nursing management of dyspnea ppt
Nursing management of dyspnea ppt Dyspnea grading
Dyspnea grading Dyspneic index formula
Dyspneic index formula Occupational asthma
Occupational asthma