Applying the 2007 asthma guidelines the Asthma APGAR

- Slides: 64
Applying the 2007 asthma guidelines: the Asthma APGAR Barbara P. Yawn, MD MSc FAAFP Member EPR-3 panel Director of Research Olmsted Medical Center Rochester, MN Adjunct Professor, Family and Community Health University of Minnesota byawn@olmmed. org
Objectives: Use cases as examples Apply the guidelines Discuss areas of judgment and evidence Highlight use of severity and control Highlight hierarchy of pharmacotherapy Highlight importance of non-pharma-cotherapy
Care should focus on: Outcomes that matter to patients Outcomes that matter to families Outcomes that matter to clinicians Outcomes that matter to quality monitors In that order
Work Absenteeism Presenteeism Promotion
Play Focus on Fun Person centered Not disease centered
Sleep Enough Not interrupted
$, $, $ Not consumed by asthma
Outcomes that matter to families

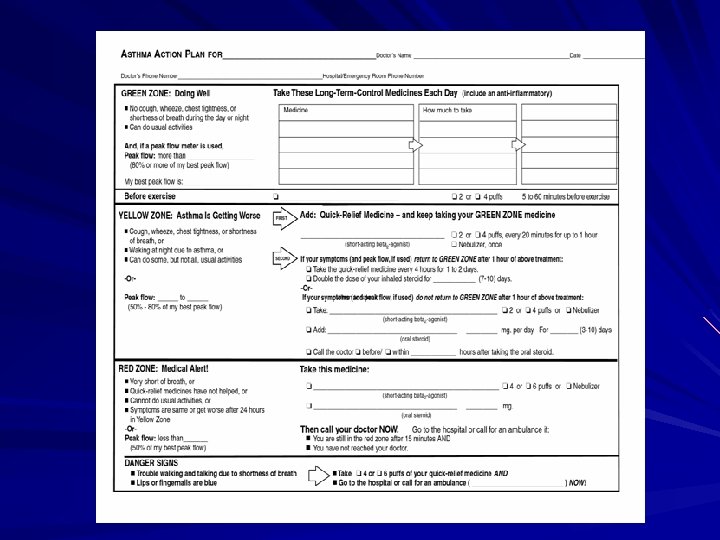
More normal lifestyle Simple treatment plans – ? ? Long acting medications – Lowest amount of therapy—step down Fewer urgent visits – Schedule regular visits – Know what to do during those visits Have a plan for regular visits
More “normal” lifestyle (con’t) No hospitalizations – Prevention – Chronic care attitude Less stress and less obsession with asthma – Knowing what to do to help – Knowing how to assess level of control Education, tools for self assessment
Practice outcomes Fewer unscheduled visits Fewer phone calls Shorter phone calls Better self management Written plans or any plans
Meeting Quotas or Outcomes That Matter to Administrators Correct drug ratios “Appropriate” use of medications Fewer ED and urgent care visits Fewer hospitalizations HEDIS Pay for performance Others? ?
First priority is to meet patient and family needs Understand disease from their perspective Affirm their concerns Negotiate a common ground and goals Provide environment for communication and education Control symptoms Patient Centered Focus
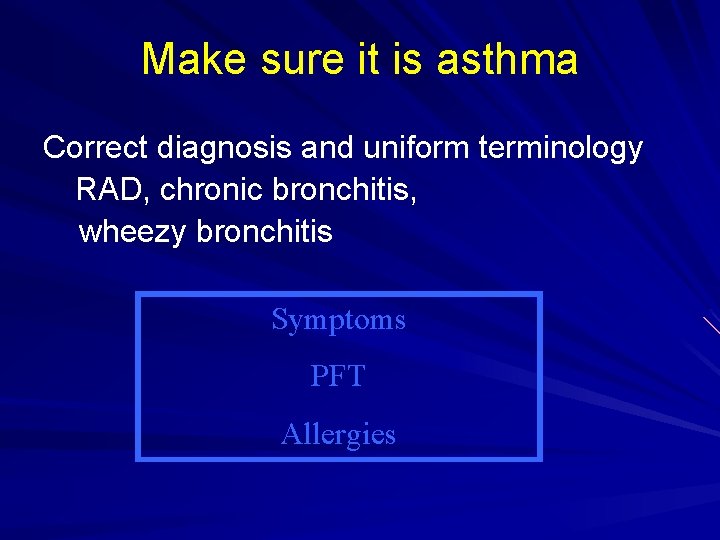
Make sure it is asthma Correct diagnosis and uniform terminology RAD, chronic bronchitis, wheezy bronchitis Symptoms PFT Allergies
Your diagnosis? Danny comes for catch up immunizations 2 months ago hospitalized for RSV—negative RSV Coughing and wheezing responded to beta agonists and inhaled steroids given by nebulizer. Discharged on ICS and SABA by inhaler and mask. Medications continued for about 6 weeks and DC’d. Danny’s mother asks about the ‘reactive airway disease’ she overheard the hospital nurses report as Danny’s diagnosis.
Danny’s respiratory history Recurrent bouts of airflow limitations Atopy by history Family history of asthma Improved with beta agonists Stayed better with steroids
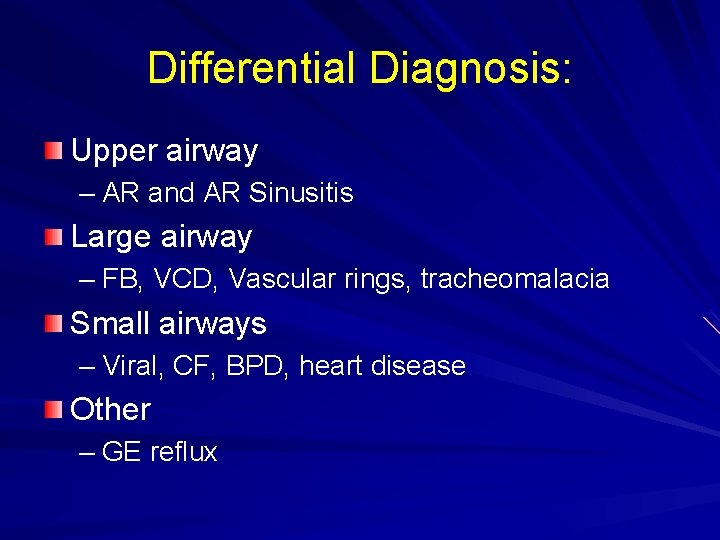
Differential Diagnosis: Upper airway – AR and AR Sinusitis Large airway – FB, VCD, Vascular rings, tracheomalacia Small airways – Viral, CF, BPD, heart disease Other – GE reflux
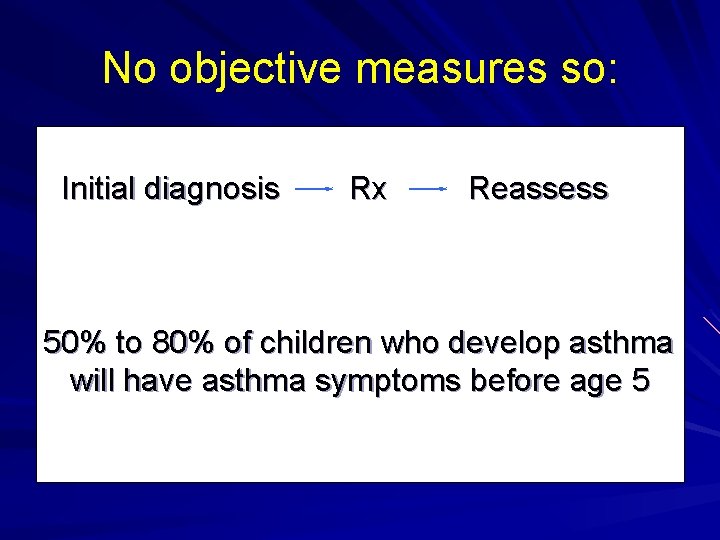
No objective measures so: Initial diagnosis Rx Reassess 50% to 80% of children who develop asthma will have asthma symptoms before age 5
Danny is not a candidate for spirometry testing Diagnosis based on pattern of symptoms, risk factors and response to therapy. He has had 2 hospitalizations for “pneumonia” Two negative chest x-rays Therefore, cardio-vascular disease, and foreign body aspirations are unlikely. Of differential diagnoses, asthma is most likely.
Danny Recurrent episodes respond to bronchodilators Has not yet been tired on inhaled ICS therapy. Called “reactive airway disease”(RAD) It may be used temporarily Using the diagnosis of RAD does not reassure patients nor improve a child’s care. In fact it may confuse and anger patients. [21]) We are ready to talk to Danny’s parents about asthma and to begin asthma therapy.
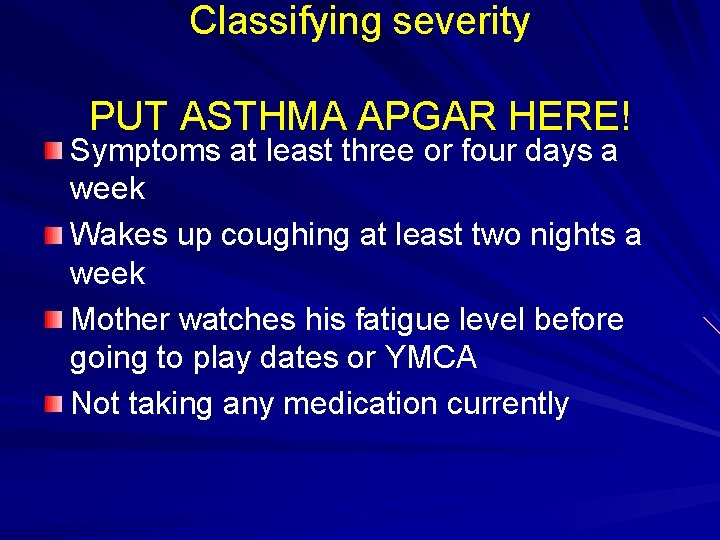
Classifying severity PUT ASTHMA APGAR HERE! Symptoms at least three or four days a week Wakes up coughing at least two nights a week Mother watches his fatigue level before going to play dates or YMCA Not taking any medication currently
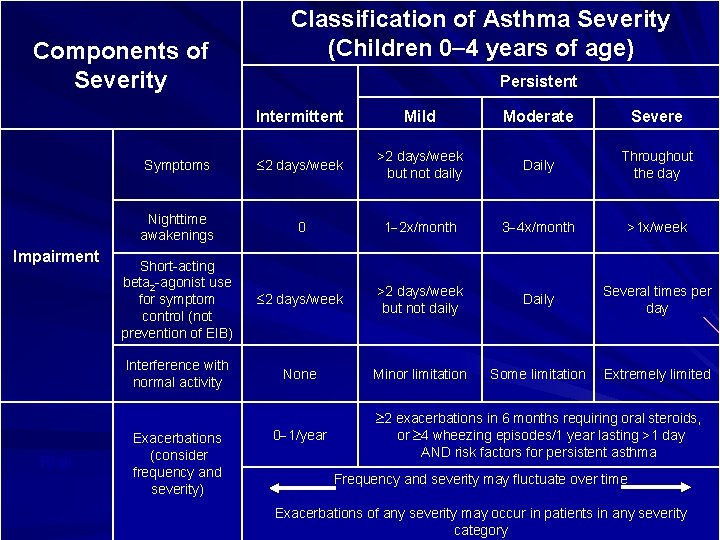
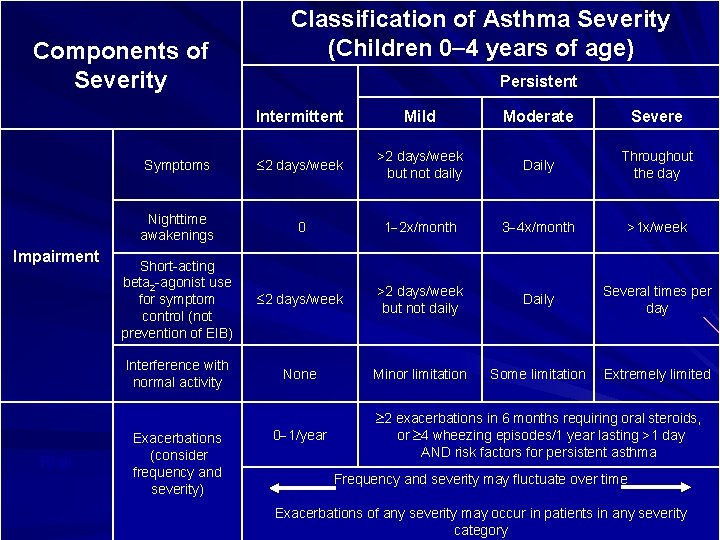
Components of Severity Impairment Risk Classification of Asthma Severity (Children 0 4 years of age) Persistent Intermittent Mild Moderate Severe Symptoms 2 days/week >2 days/week but not daily Daily Throughout the day Nighttime awakenings 0 1 2 x/month 3 4 x/month >1 x/week Short-acting beta 2 -agonist use for symptom control (not prevention of EIB) 2 days/week >2 days/week but not daily Daily Several times per day Interference with normal activity None Minor limitation Some limitation Extremely limited Exacerbations (consider frequency and severity) 0 1/year 2 exacerbations in 6 months requiring oral steroids, or 4 wheezing episodes/1 year lasting >1 day AND risk factors for persistent asthma Frequency and severity may fluctuate over time Exacerbations of any severity may occur in patients in any severity category
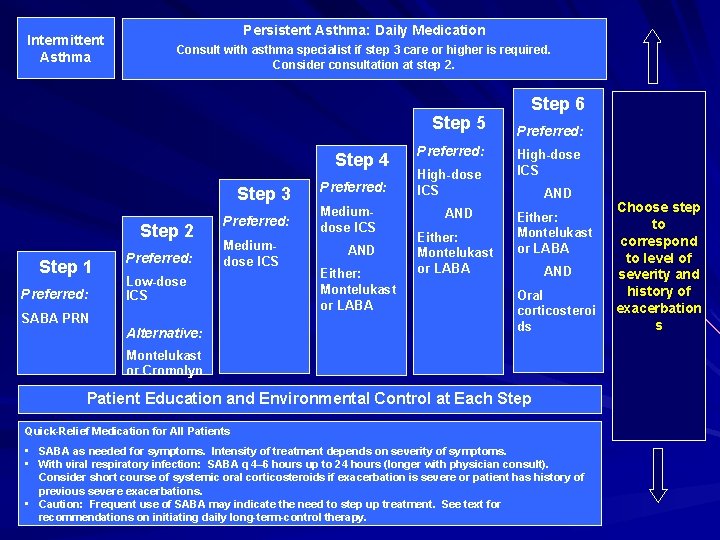
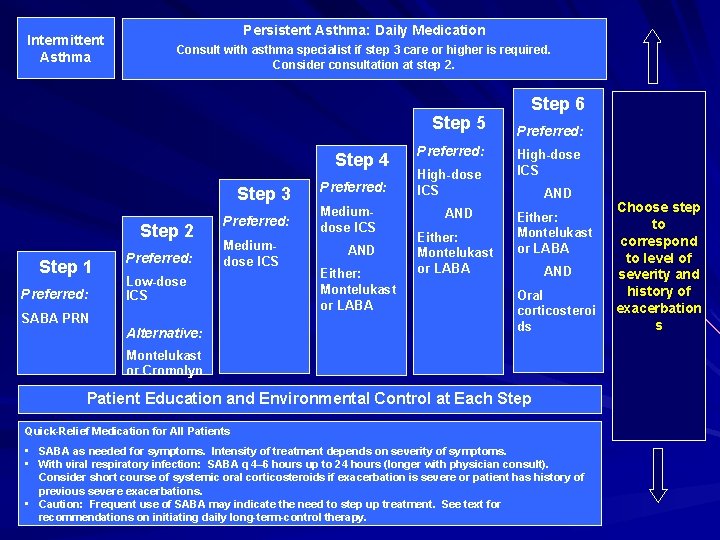
Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 3 care or higher is required. Consider consultation at step 2. Step 5 Step 4 Step 3 Step 2 Step 1 Preferred: Mediumdose ICS Low-dose ICS SABA PRN Alternative: Preferred: Mediumdose ICS AND Either: Montelukast or LABA Preferred: High-dose ICS AND Either: Montelukast or LABA Step 6 Preferred: High-dose ICS AND Either: Montelukast or LABA AND Oral corticosteroi ds Montelukast or Cromolyn Patient Education and Environmental Control at Each Step Quick-Relief Medication for All Patients • SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms. • With viral respiratory infection: SABA q 4– 6 hours up to 24 hours (longer with physician consult). Consider short course of systemic oral corticosteroids if exacerbation is severe or patient has history of previous severe exacerbations. • Caution: Frequent use of SABA may indicate the need to step up treatment. See text for recommendations on initiating daily long-term-control therapy. Choose step to correspond to level of severity and history of exacerbation s
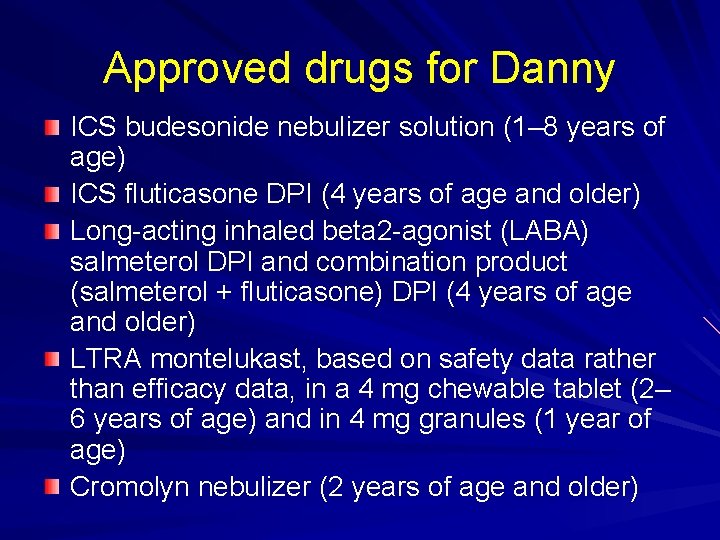
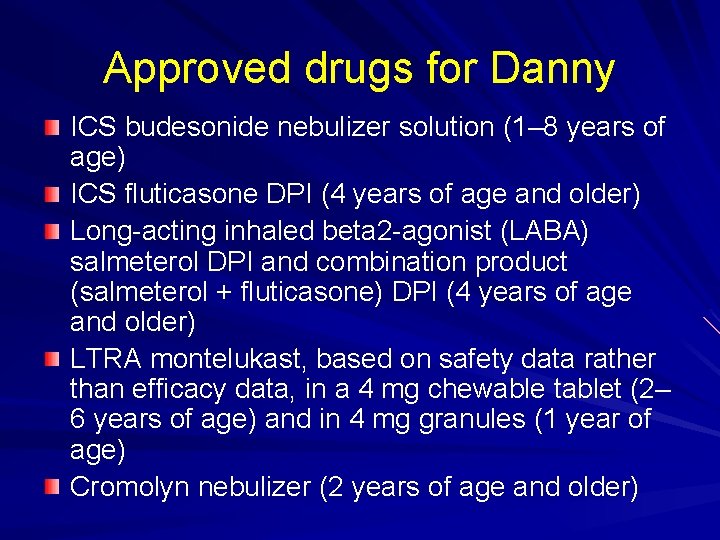
Approved drugs for Danny ICS budesonide nebulizer solution (1– 8 years of age) ICS fluticasone DPI (4 years of age and older) Long-acting inhaled beta 2 -agonist (LABA) salmeterol DPI and combination product (salmeterol + fluticasone) DPI (4 years of age and older) LTRA montelukast, based on safety data rather than efficacy data, in a 4 mg chewable tablet (2– 6 years of age) and in 4 mg granules (1 year of age) Cromolyn nebulizer (2 years of age and older)
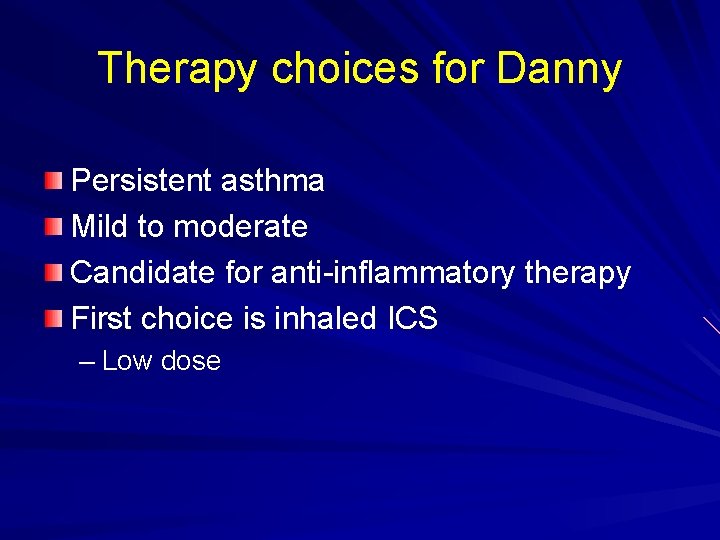
Therapy choices for Danny Persistent asthma Mild to moderate Candidate for anti-inflammatory therapy First choice is inhaled ICS – Low dose
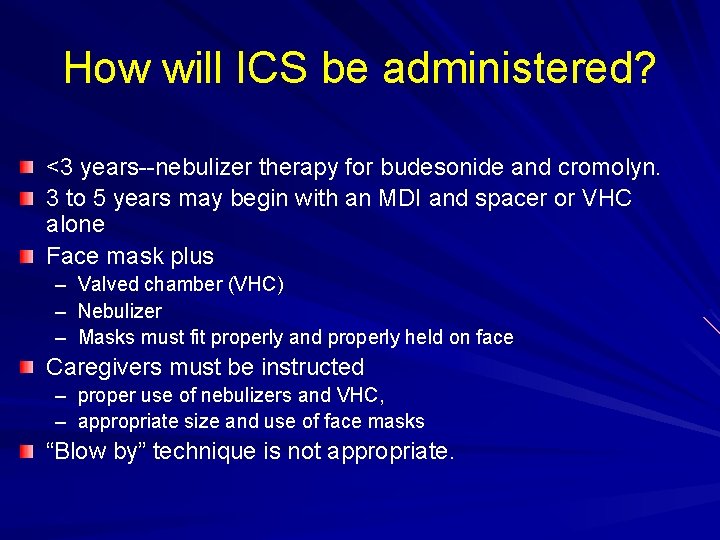
How will ICS be administered? <3 years--nebulizer therapy for budesonide and cromolyn. 3 to 5 years may begin with an MDI and spacer or VHC alone Face mask plus – – – Valved chamber (VHC) Nebulizer Masks must fit properly and properly held on face Caregivers must be instructed – proper use of nebulizers and VHC, – appropriate size and use of face masks “Blow by” technique is not appropriate.
Planned care Begin Danny on ICS low dose Nebulizer and face mask See back in two weeks, reassess APGAR Begin education about asthma related to mother’s desire for “what information first”
Now Mary using control status Mary is 10, comes for recheck Asthma diagnosed 2 yrs ago. Recorded as mild persistent asthma Prescribed daily low dose ICS 3 refills over past 6 months Increasing problems with wheezing during school Been to school health aid almost daily for 3 weeks.
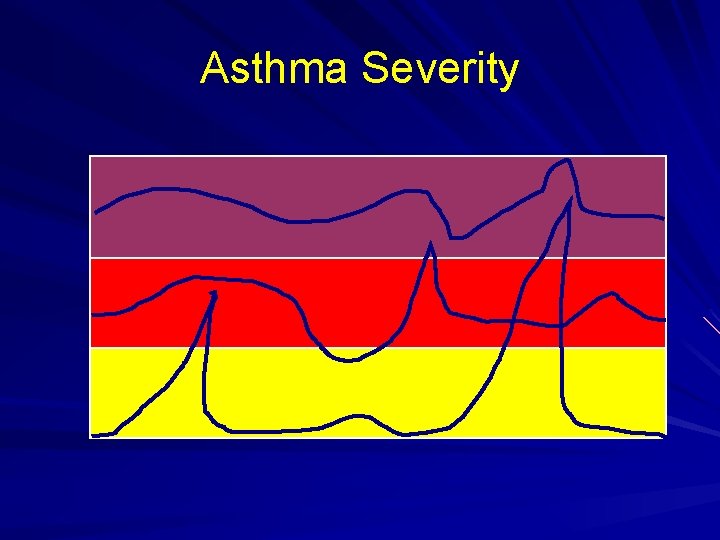
Asthma Severity
Mary continued: Gets a dose of her “rescue” medication, improves rapidly and back to class in about 30 min. No action plan. Seems to always happen in math class. Mary says she is using daily ICS in the late afternoon, her mother agrees and both say her open mouth inhaler technique is good. No problems on weekends or after school.
Assessing symptoms: Don’t ask --- Don’t tell --- Don’t Document Has never worked for anything!!!!!
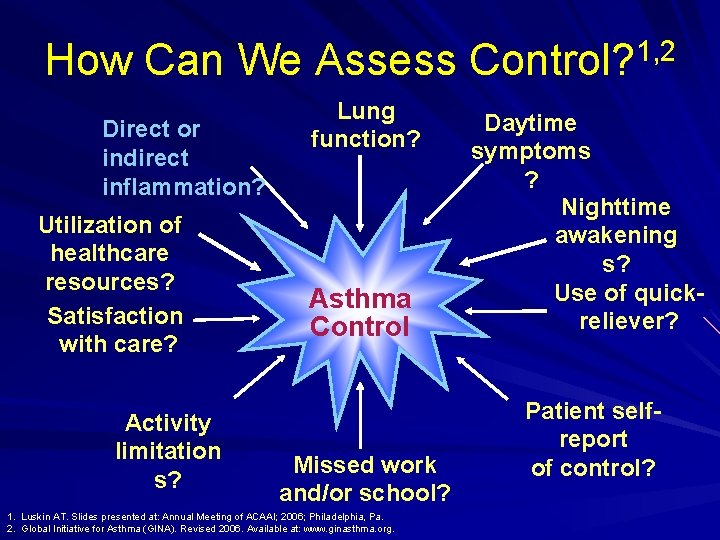
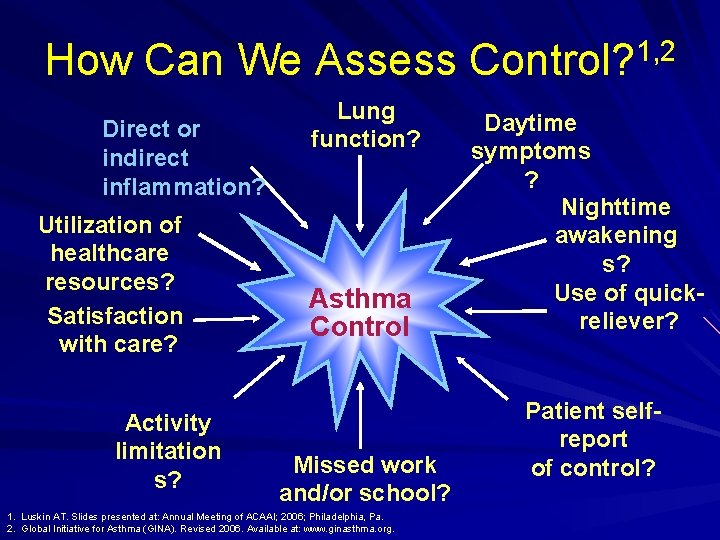
How Can We Assess Control? 1, 2 Direct or indirect inflammation? Utilization of healthcare resources? Satisfaction with care? Activity limitation s? Lung function? Asthma Control Missed work and/or school? 1. Luskin AT. Slides presented at: Annual Meeting of ACAAI; 2006; Philadelphia, Pa. 2. Global Initiative for Asthma (GINA). Revised 2006. Available at: www. ginasthma. org. Daytime symptoms ? Nighttime awakening s? Use of quickreliever? Patient selfreport of control?
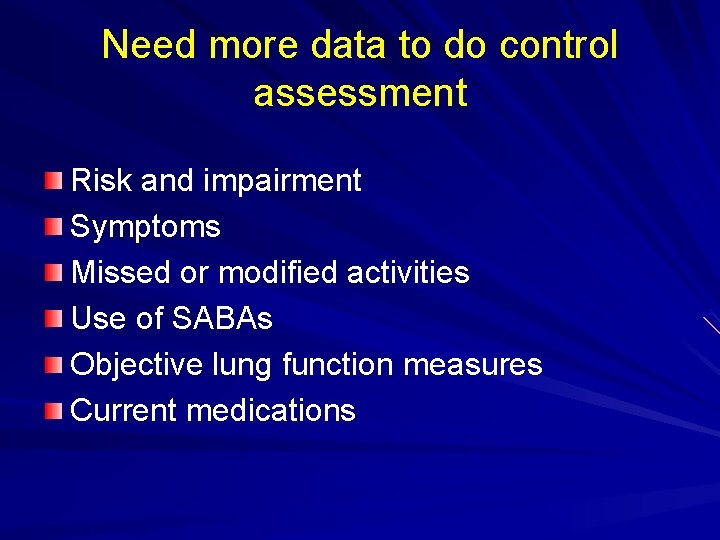
Need more data to do control assessment Risk and impairment Symptoms Missed or modified activities Use of SABAs Objective lung function measures Current medications
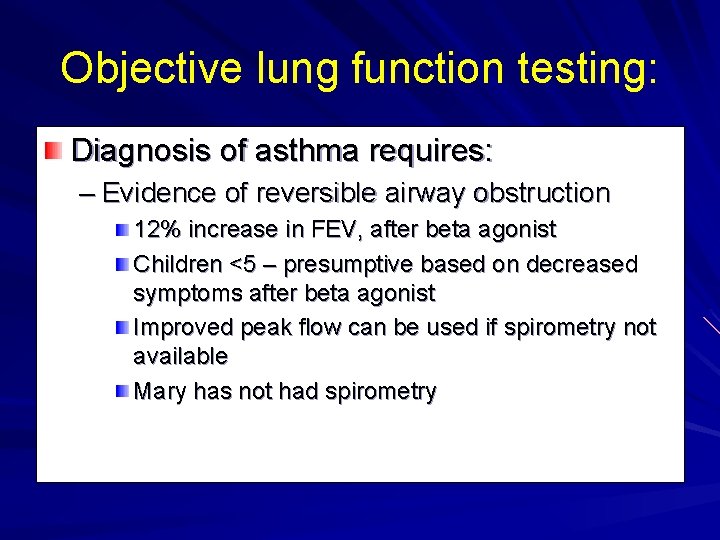
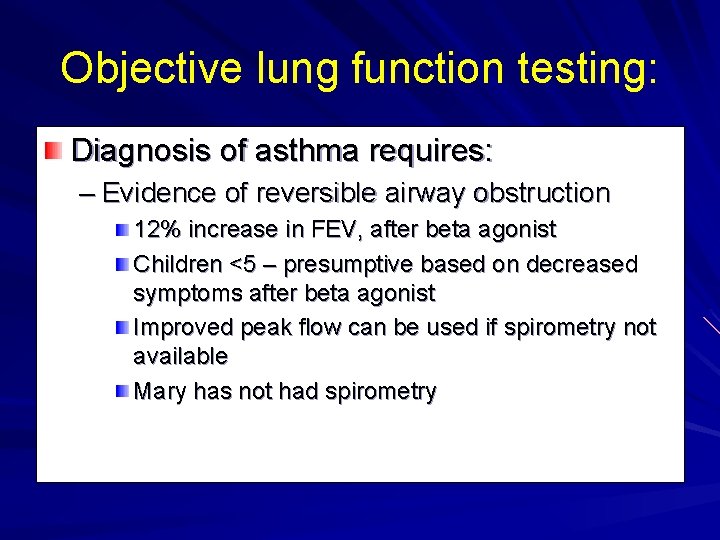
Objective lung function testing: Diagnosis of asthma requires: – Evidence of reversible airway obstruction 12% increase in FEV, after beta agonist Children <5 – presumptive based on decreased symptoms after beta agonist Improved peak flow can be used if spirometry not available Mary has not had spirometry
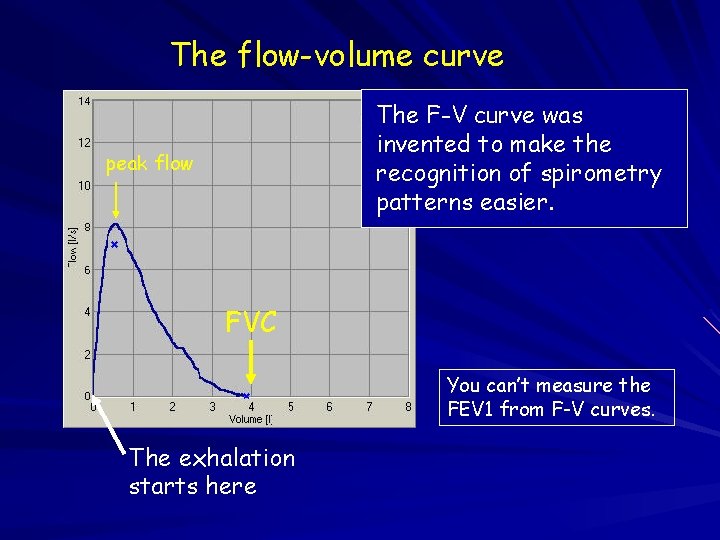
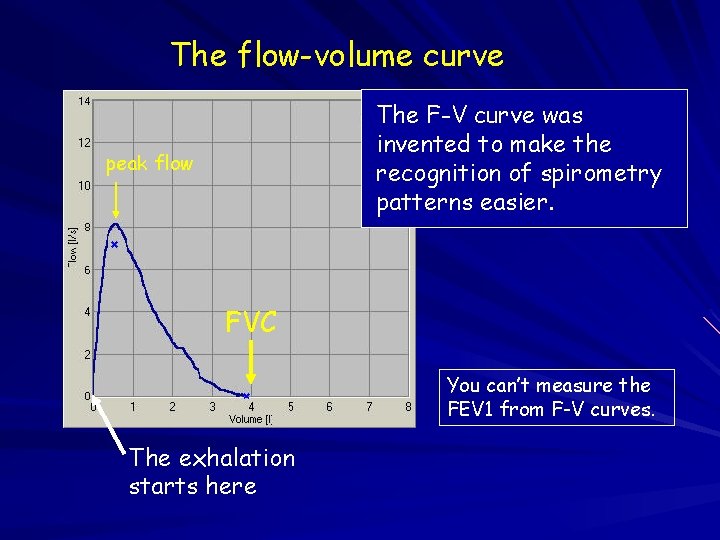
The flow-volume curve The F-V curve was invented to make the recognition of spirometry patterns easier. peak flow FVC You can’t measure the FEV 1 from F-V curves. The exhalation starts here
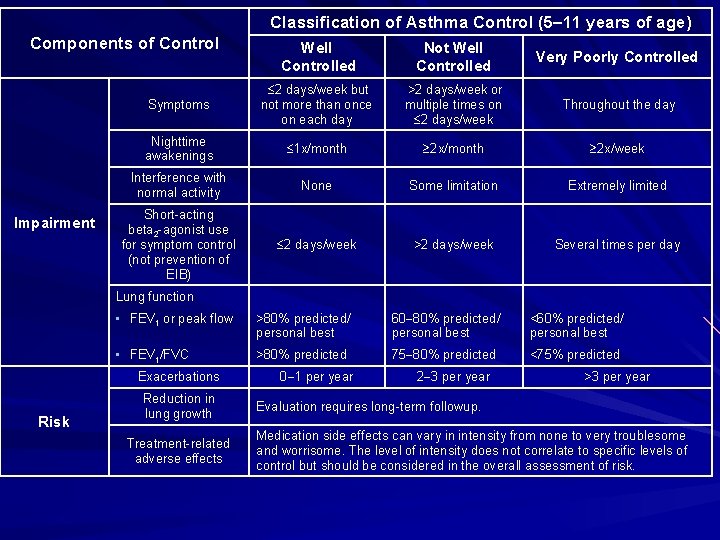
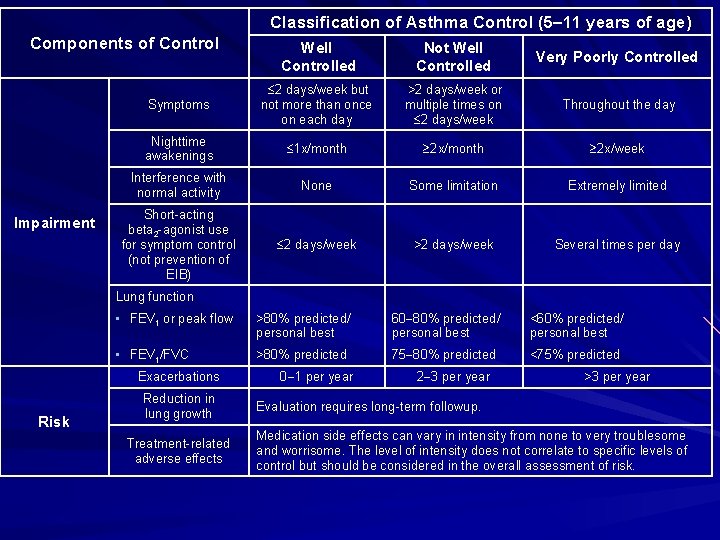
Classification of Asthma Control (5 11 years of age) Components of Control Impairment Well Controlled Not Well Controlled Very Poorly Controlled Symptoms 2 days/week but not more than once on each day >2 days/week or multiple times on 2 days/week Throughout the day Nighttime awakenings 1 x/month 2 x/week Interference with normal activity None Some limitation Extremely limited Short-acting beta 2 -agonist use for symptom control (not prevention of EIB) 2 days/week >2 days/week Several times per day Lung function • FEV 1 or peak flow >80% predicted/ personal best 60 80% predicted/ personal best <60% predicted/ personal best • FEV 1/FVC >80% predicted 75 80% predicted <75% predicted Exacerbations Risk Reduction in lung growth Treatment-related adverse effects 0 1 per year 2 3 per year >3 per year Evaluation requires long-term followup. Medication side effects can vary in intensity from none to very troublesome and worrisome. The level of intensity does not correlate to specific levels of control but should be considered in the overall assessment of risk.
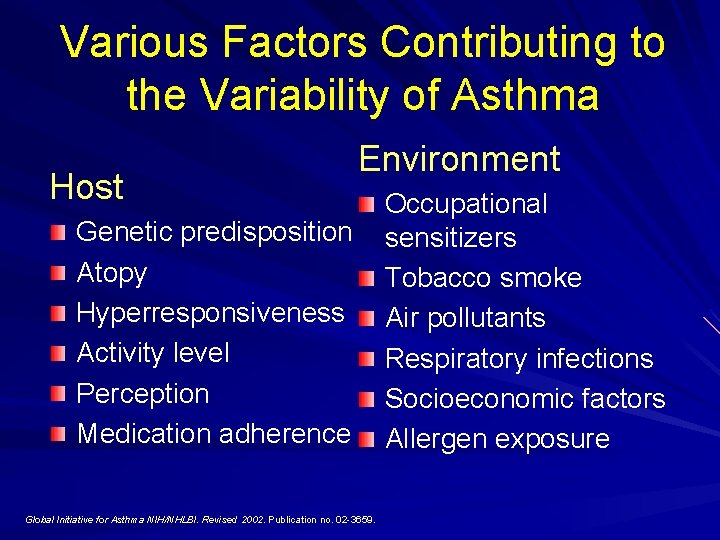
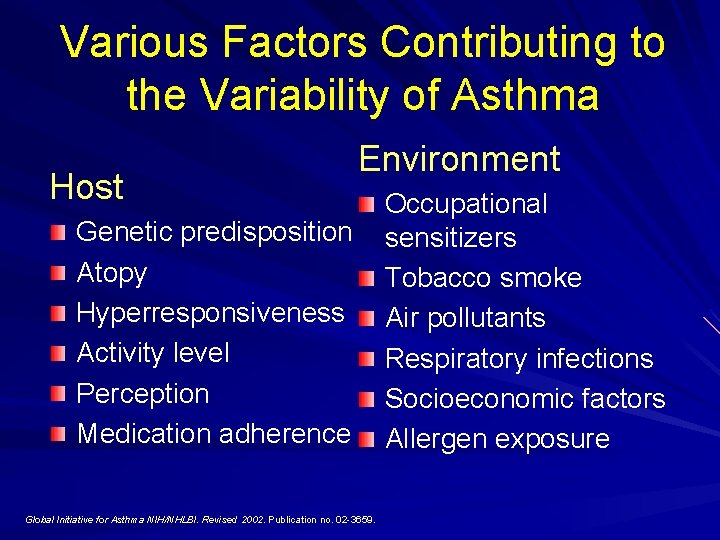
Various Factors Contributing to the Variability of Asthma Host Environment Genetic predisposition Atopy Hyperresponsiveness Activity level Perception Medication adherence Global Initiative for Asthma NIH/NHLBI. Revised 2002. Publication no. 02 -3659. Occupational sensitizers Tobacco smoke Air pollutants Respiratory infections Socioeconomic factors Allergen exposure
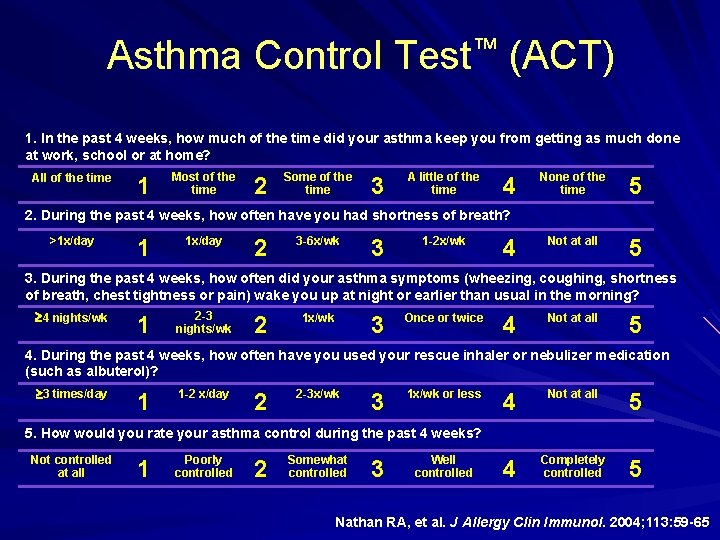
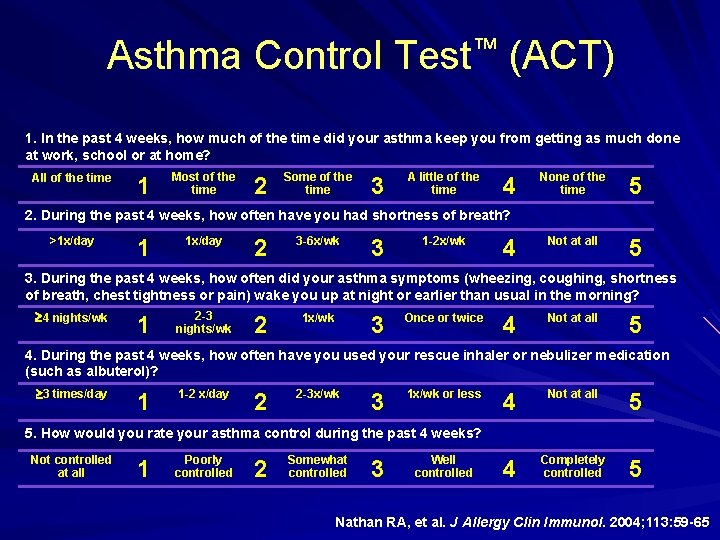
Asthma Control Test™ (ACT) 1. In the past 4 weeks, how much of the time did your asthma keep you from getting as much done at work, school or at home? All of the time 1 Most of the time 2 Some of the time 3 A little of the time 4 None of the time 5 Not at all 5 2. During the past 4 weeks, how often have you had shortness of breath? >1 x/day 1 1 x/day 2 3 -6 x/wk 3 1 -2 x/wk 4 3. During the past 4 weeks, how often did your asthma symptoms (wheezing, coughing, shortness of breath, chest tightness or pain) wake you up at night or earlier than usual in the morning? 4 nights/wk 1 2 -3 nights/wk 2 1 x/wk 3 Once or twice 4 Not at all 5 4. During the past 4 weeks, how often have you used your rescue inhaler or nebulizer medication (such as albuterol)? 3 times/day 1 1 -2 x/day 2 2 -3 x/wk 3 1 x/wk or less 4 Not at all 5 4 Completely controlled 5 5. How would you rate your asthma control during the past 4 weeks? Not controlled at all 1 Poorly controlled 2 Somewhat controlled 3 Well controlled Nathan RA, et al. J Allergy Clin Immunol. 2004; 113: 59 -65
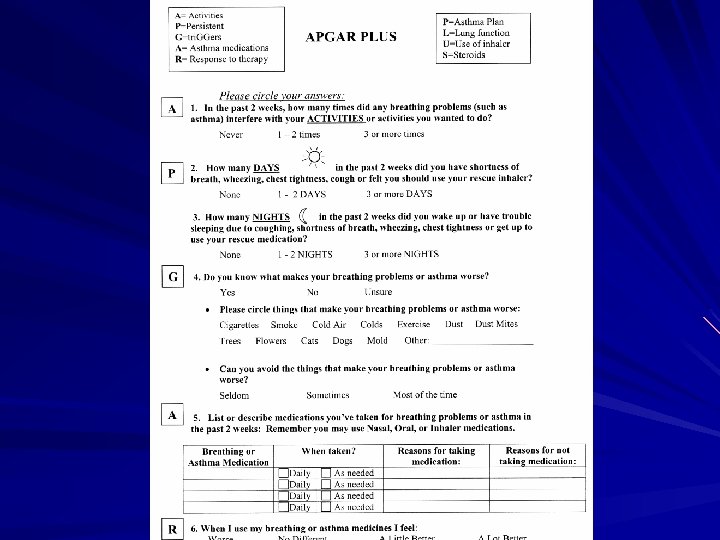
Asthma APGAR
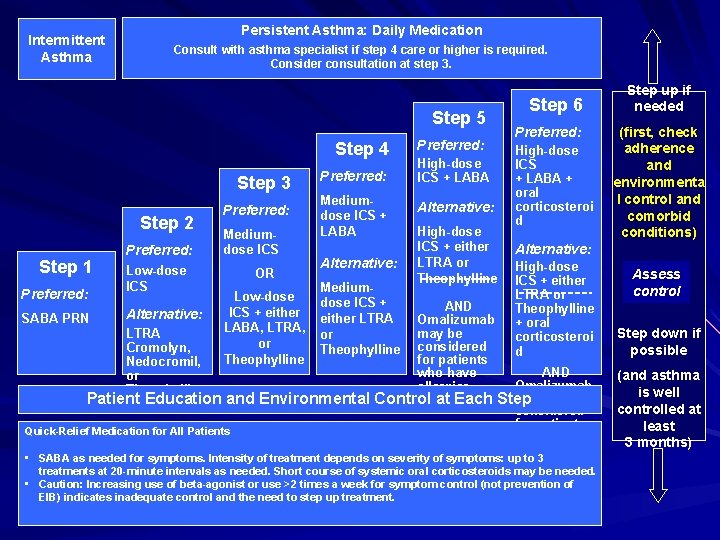
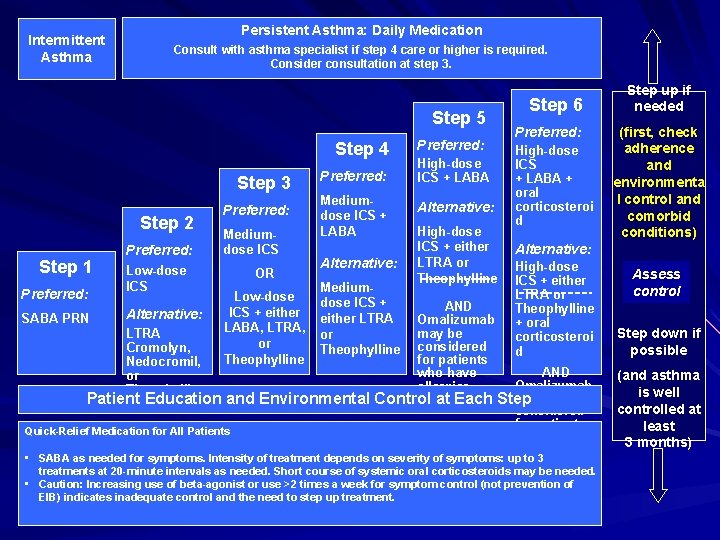
Intermittent Asthma Persistent Asthma: Daily Medication Consult with asthma specialist if step 4 care or higher is required. Consider consultation at step 3. Step 6 Step 5 Step 4 Step 3 Step 2 Step 1 Preferred: SABA PRN Preferred: Low-dose ICS Alternative: LTRA Cromolyn, Nedocromil, or Theophylline Preferred: Mediumdose ICS OR Low-dose ICS + either LABA, LTRA, or Theophylline Preferred: Mediumdose ICS + LABA Alternative: Mediumdose ICS + either LTRA or Theophylline High-dose ICS + LABA Alternative: High-dose ICS + either LTRA or Theophylline AND Omalizumab may be considered for patients who have allergies Patient Education and Environmental Control at Each Quick-Relief Medication for All Patients Preferred: High-dose ICS + LABA + oral corticosteroi d Step up if needed (first, check adherence and environmenta l control and comorbid conditions) Alternative: High-dose ICS + either LTRA or Theophylline + oral corticosteroi d Step down if possible AND Omalizumab may be Step considered for patients who have allergies (and asthma is well controlled at least 3 months) • SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20 -minute intervals as needed. Short course of systemic oral corticosteroids may be needed. • Caution: Increasing use of beta-agonist or use >2 times a week for symptom control (not prevention of EIB) indicates inadequate control and the need to step up treatment. Assess control
APGAR Algorithm
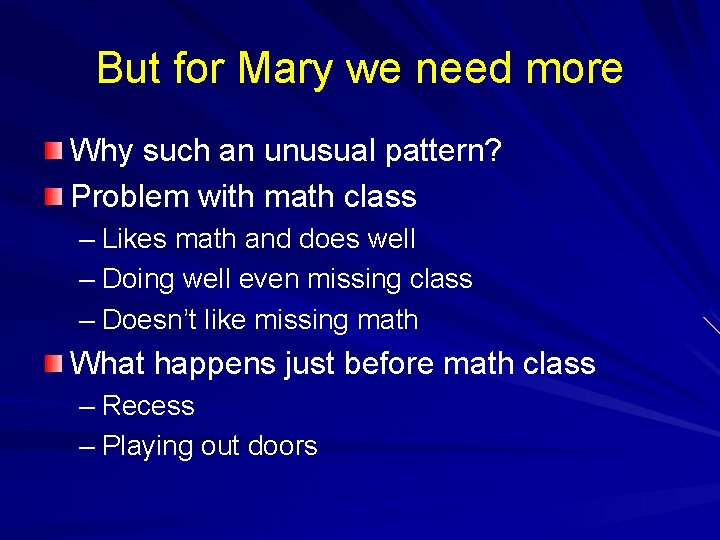
But for Mary we need more Why such an unusual pattern? Problem with math class – Likes math and does well – Doing well even missing class – Doesn’t like missing math What happens just before math class – Recess – Playing out doors
Triggers and Allergens Exercise? Pollens? Other envirnomental things?
Where to look for help Websites for current outdoor allergen levels include: http: //www. usatoday. com/life/health/allergies/seas onal. htm http: //www. weather. com/activities/health/pollen/. Allergic rhinitis common Allergic rhinitis symptoms can be very helpful in determining the presence of seasonal versus persistent exposure to allergens of consequence
Mary Consider increasing therapy for pollen season Consider using pre-med before recess Consider keeping Mary in from recess Must reassess after first freeze
KISS IT Choose the essential elements Focus on a few Let them ask for more Translate to the basic tasks of any clinical visit Make it flexible Use their data
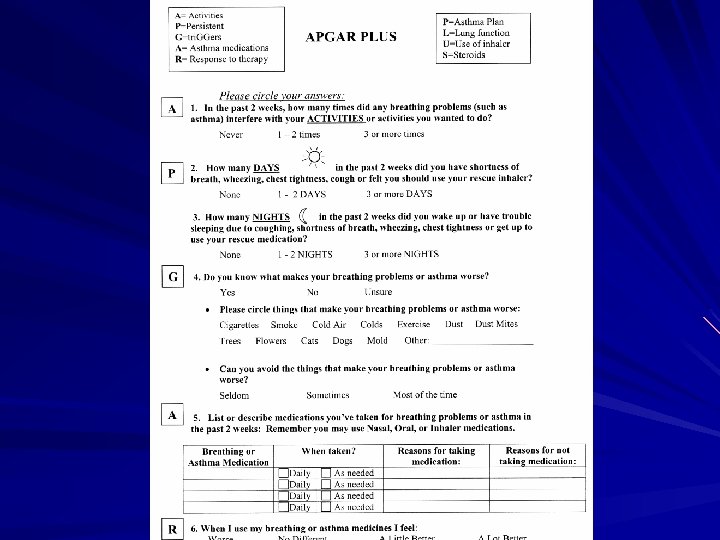
ASTHMA APGAR A=Activities P=Persistence G=tri. GGers A=Asthma Medications R=Response to Therapy
Phase 1 Apgar 4 Sites: Rural Family Practice 1 st Meeting: Asthma CME & Apgar – MD & RN abstract 10 -20 charts 2 nd Meeting: Review Data – Gaps Identified by Staff – Ideas for Practice Change Utilize Apgar in practice 3 months Review Additional 10 charts
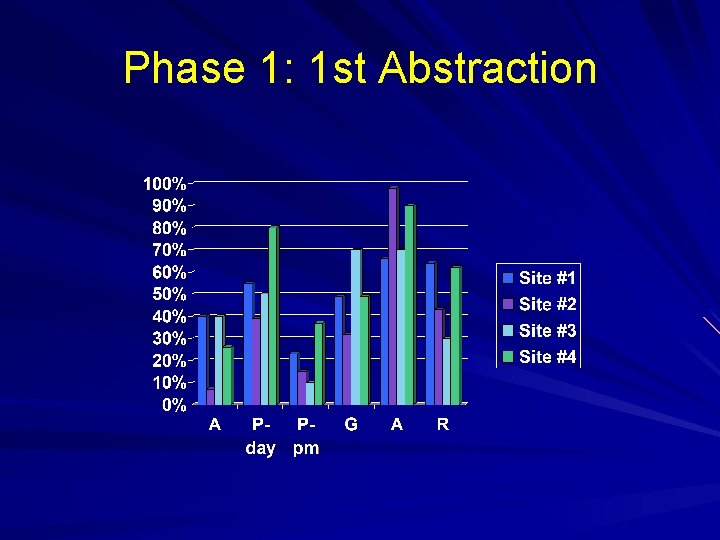
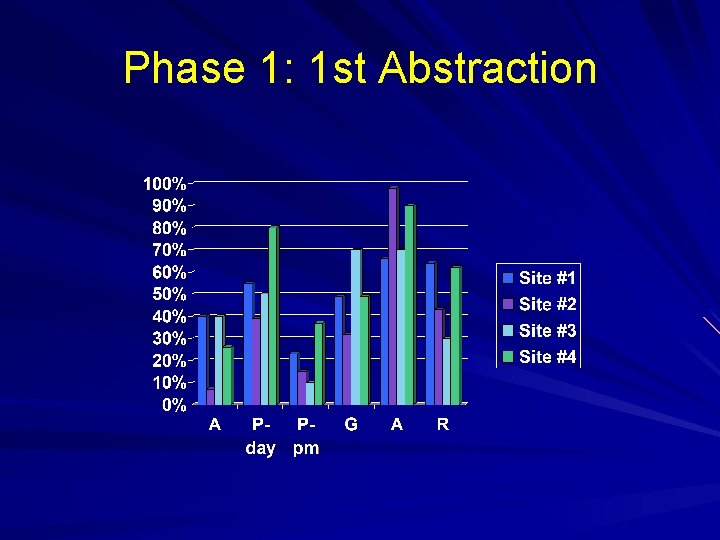
Phase 1: 1 st Abstraction
Gaps Identified Knowing what to ask in asthma evaluation. Know how to do asthma evaluation and record it. Don’t know what medications patient really taking. Inhalers not identified by patients as medication Staff and patients need review of inhaler technique Do not know asthma symptom frequency and activity limitations based on documentation. Patient history not clear to physicians. Difficult to follow progression of care. Do not know when asthma patient is being seen in clinic for other reasons.
Practice Changes Breathing evaluation for patients Memory aids for staff Pink Lung Apgar Wallet sized Apgar Red stamp on visit sheet identifies those with asthma/smokers Electronic template Inhaler technique information sheets Language change when asking patients to bring in medications Staff review inhaler technique once/yr Have patients demonstrate inhaler technique
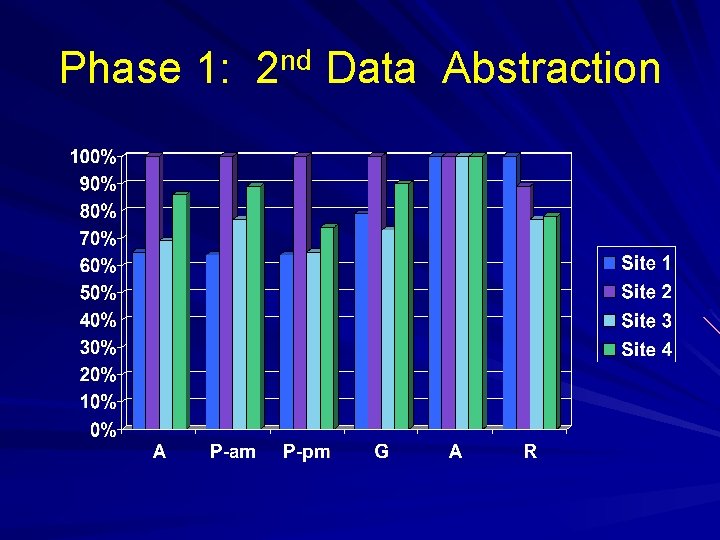
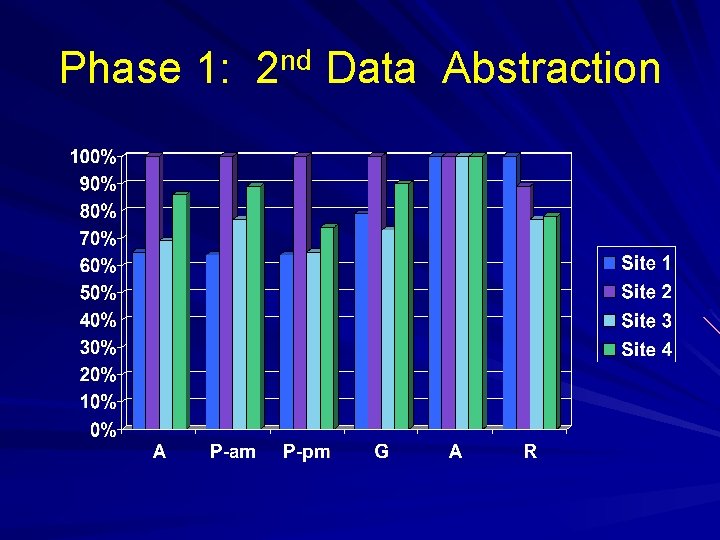
Phase 1: 2 nd Data Abstraction
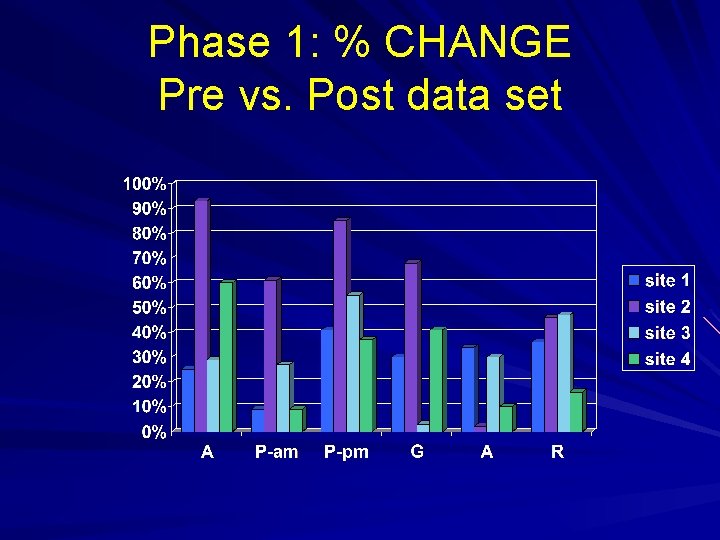
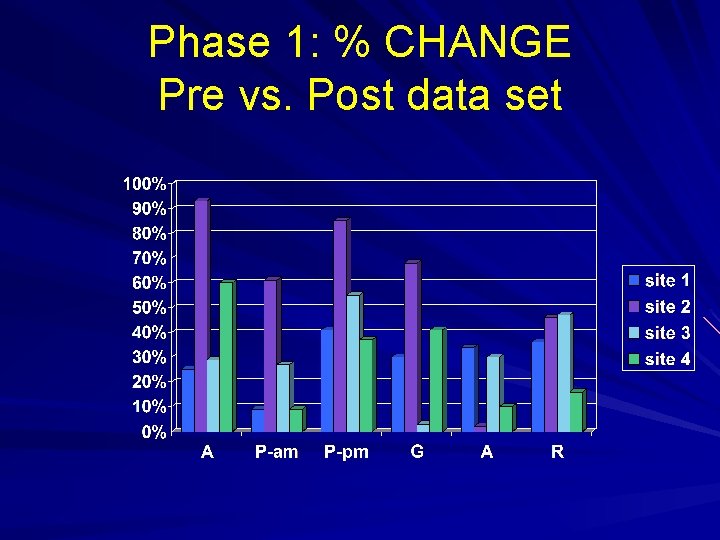
Phase 1: % CHANGE Pre vs. Post data set
ISSUES Documentation Patients minimize their disease. Asthma not viewed as chronic illness. Activities Triggers Medications Allergy testing. Response to Therapy Nurses/Asthma educators Patient should be the one to determine how he/she is doing. Time is an issue Streamline
Phase 2 asthma Apgar 10 Minnesota FP Sites agree to participate Contact only by phone – Teach abstract process using Apgar Reviewed 20 charts Telephone Conference to review data – Identify Gaps in care – Identify Practice Changes – Implement practice changes x 3 months n Review additional 20 charts
Phase 2 Comments “I’m sure we’re doing OK, but you can’t prove it by reading the note (in the chart). ” “We ask more than we chart. ” “We’re making a lot of work for each other due to a lack of charting. ” “This (Apgar) was a cognitive leap; it’s not something I think about. I need to add it to my assessment with adults. ” Data represents increase in practitioners’ time if charting is not done adequately. Inadequate charting is represented by other diseases as well, i. e. diabetes, heart disease.
Moving to Patient Apgar Participatory research Start with previous work Conceptualize the tool Plan implementation strategies Develop outcome measures Develop methods to collect outcome measures
General principle #1 The physician’s and nurses’ question determine the tone and specificity of the visit. How is your asthma doing? I would like to know about how asthma is affecting you. – APGAR questions
General principle #2 What we ask is what the patients will perceive we think is important They will begin to notice what we ask them to evaluate
General principle #3 APGAR concept work for all chronic diseases – How does disease impact your activities? – How often are you having symptoms? Day Night – What makes it better and worse – How are you actually able to take medications – Do the medications make it better or worse
One plan for most conditions Asthma Apgar as a template Processes that can be translated Practice friendly processes Patient friendly processes
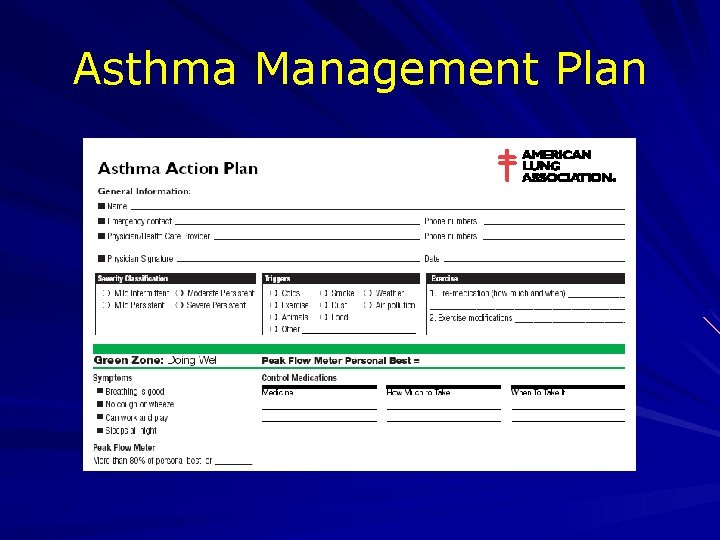
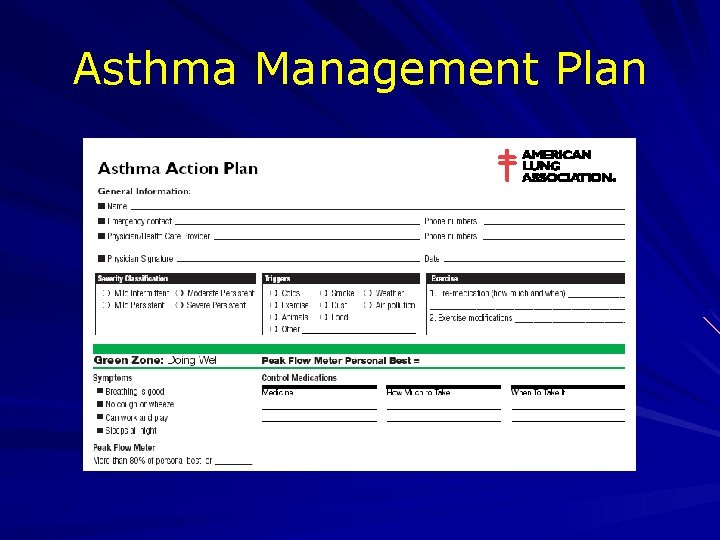
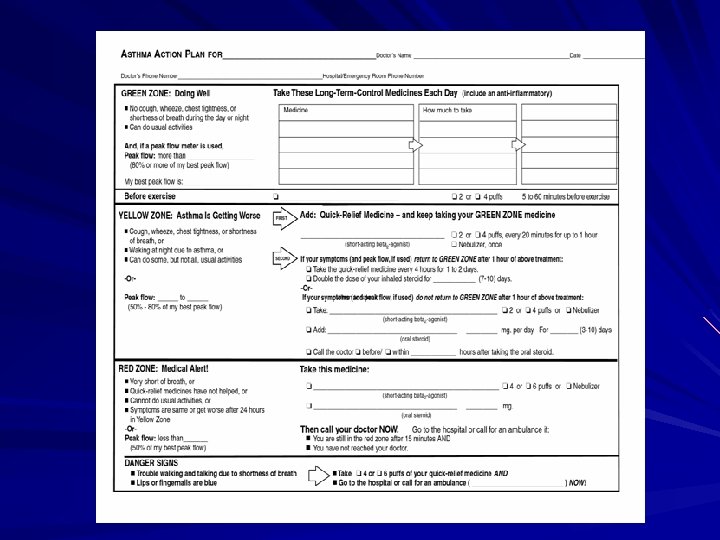
Asthma Management Plan
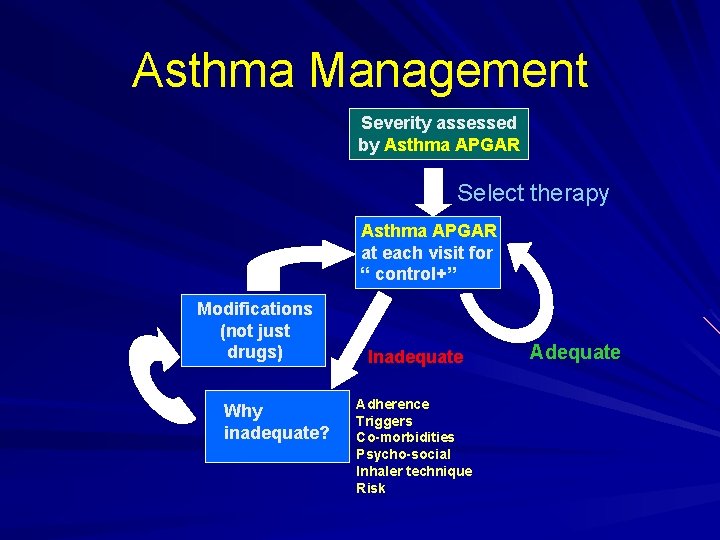
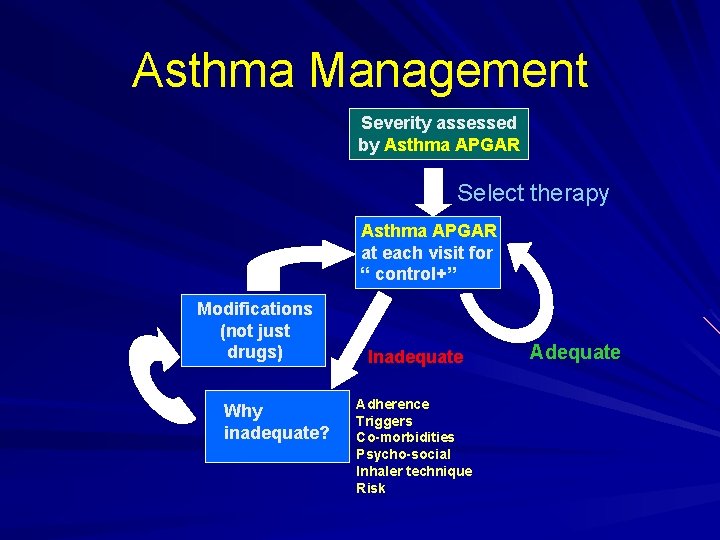
Asthma Management Severity assessed by Asthma APGAR Select therapy Asthma APGAR at each visit for “ control+” Modifications (not just drugs) Why inadequate? Inadequate Adherence Triggers Co-morbidities Psycho-social Inhaler technique Risk Adequate