Neonatal resuscitation Mr Matthews Apgar Score The Apgar
- Slides: 16
Neonatal resuscitation Mr Matthews
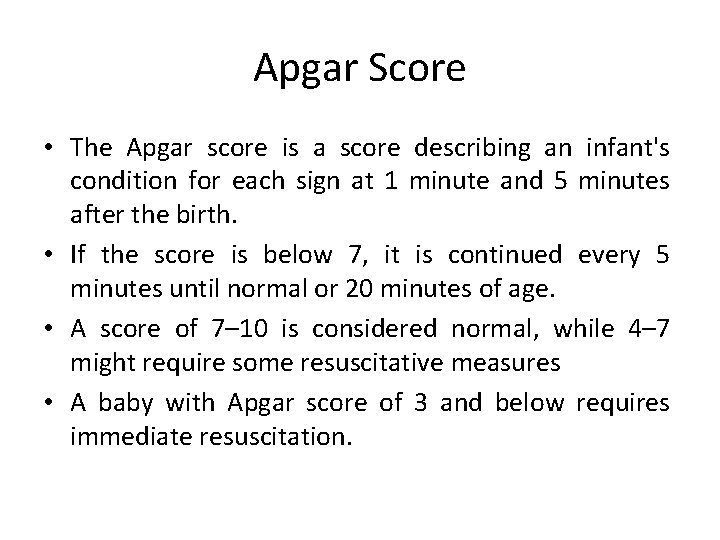
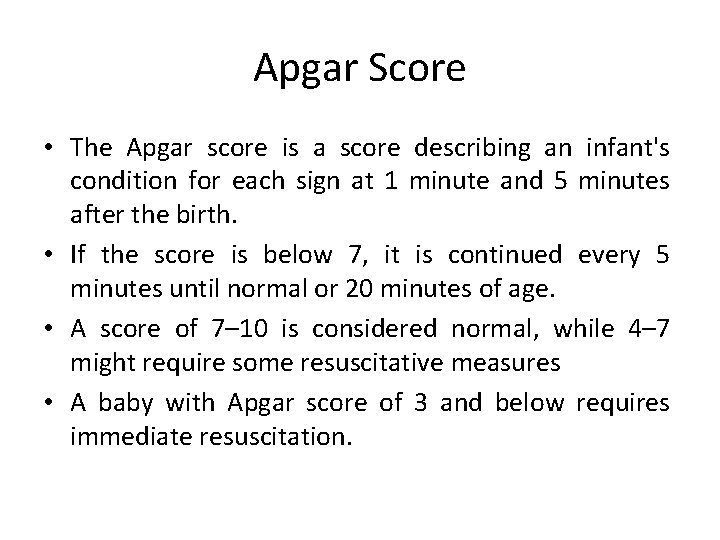
Apgar Score • The Apgar score is a score describing an infant's condition for each sign at 1 minute and 5 minutes after the birth. • If the score is below 7, it is continued every 5 minutes until normal or 20 minutes of age. • A score of 7– 10 is considered normal, while 4– 7 might require some resuscitative measures • A baby with Apgar score of 3 and below requires immediate resuscitation.
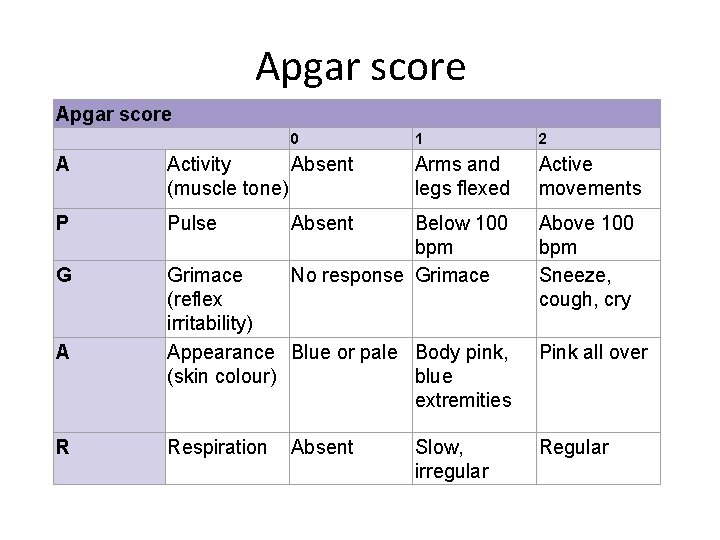
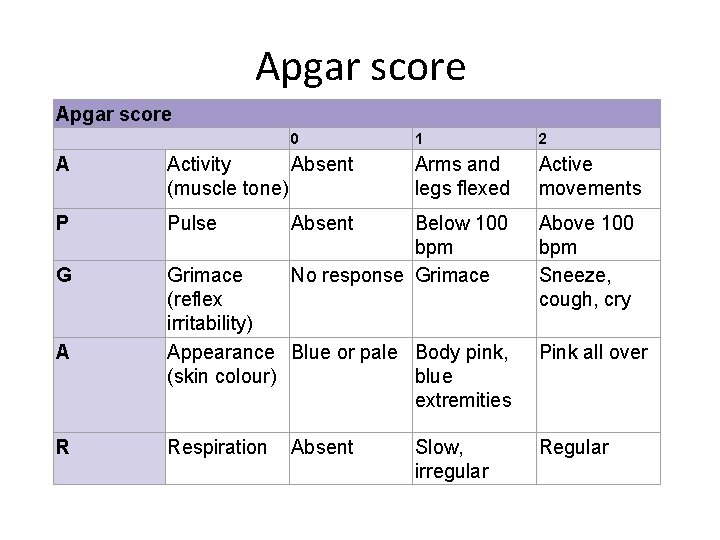
Apgar score 0 1 2 Arms and legs flexed Active movements A Activity Absent (muscle tone) P Pulse G Grimace (reflex irritability) Appearance Blue or pale Body pink, (skin colour) blue extremities A R Respiration Absent Below 100 bpm No response Grimace Absent Slow, irregular Above 100 bpm Sneeze, cough, cry Pink all over Regular
WHICH BABIES REQUIRE RESUSCITATION? q Most Newly Born Babies Are Vigorous q. Only Approximately 10% Newborns Require Some Assistance q. Only 1% Need Major Resuscitative Measures, e. g. Intubation, Chest Compressions, And/Or Medications, To Survive
• Can you describe an Apgar score in preterm infants? • Is the Apgar score a good indicator of long-term neurological outcome?
NEWBORN RESUSCITATION v THE CLINICAL SEQUENCES? v HOW TO BE READY & CARRY OUT RESUSCITATION?
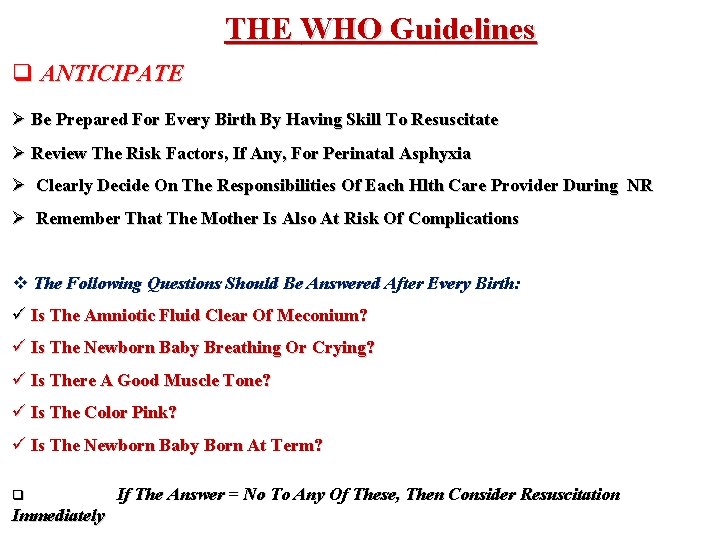
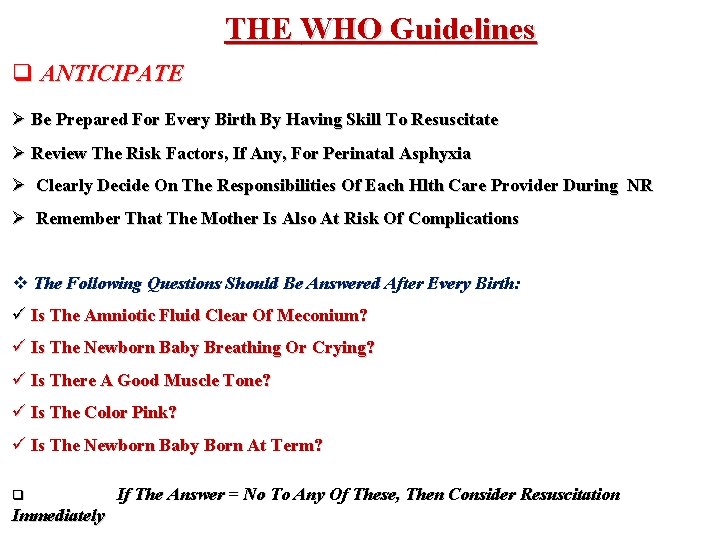
THE WHO Guidelines q ANTICIPATE Ø Be Prepared For Every Birth By Having Skill To Resuscitate Ø Review The Risk Factors, If Any, For Perinatal Asphyxia Ø Clearly Decide On The Responsibilities Of Each Hlth Care Provider During NR Ø Remember That The Mother Is Also At Risk Of Complications v The Following Questions Should Be Answered After Every Birth: ü Is The Amniotic Fluid Clear Of Meconium? ü Is The Newborn Baby Breathing Or Crying? ü Is There A Good Muscle Tone? ü Is The Color Pink? ü Is The Newborn Baby Born At Term? q Immediately If The Answer = No To Any Of These, Then Consider Resuscitation
PREPARATION FOR RESUSCITATION: PERSONNEL AND EQUIPMENT FACTS Ø Every Delivery To Be Attended By At Least 1 Person Whose Only Responsibility Is The Baby & Who Is Capable Of Initiating Resuscitation Ø Either That Person Or Someone Else Who Is Immediately Available Should Have Skills Required To Perform A Complete Resuscitation Ø When Resuscitation Is Anticipated, Additional Personnel Should Be Present In The DR Before The Delivery Occurs ü Prepare Necessary Equipment ü Turn On Radiant Warmer ü Check Resuscitation Equipment
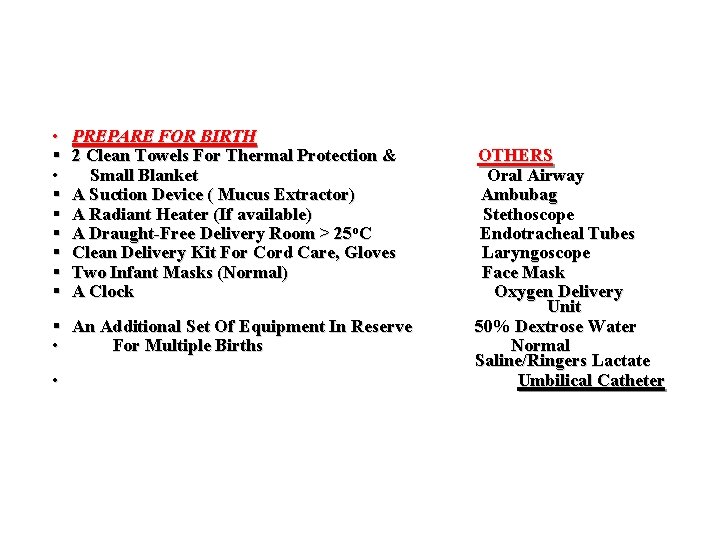
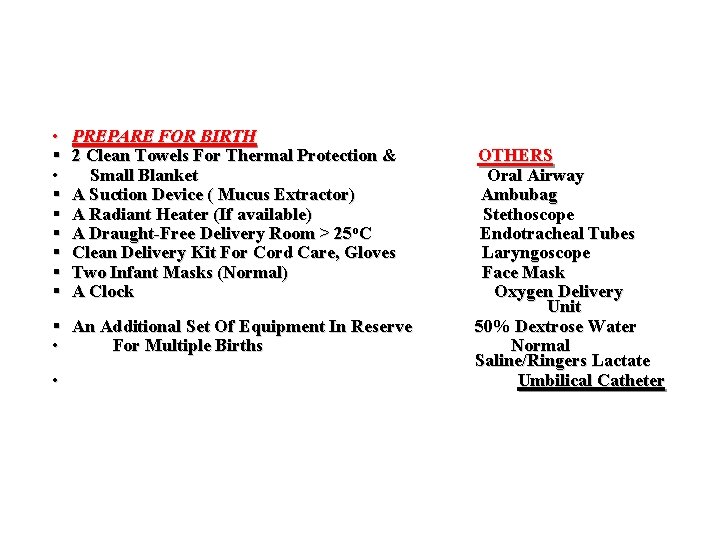
• § § § § PREPARE FOR BIRTH 2 Clean Towels For Thermal Protection & Small Blanket A Suction Device ( Mucus Extractor) A Radiant Heater (If available) A Draught-Free Delivery Room > 25 o. C Clean Delivery Kit For Cord Care, Gloves Two Infant Masks (Normal) A Clock § An Additional Set Of Equipment In Reserve • For Multiple Births • OTHERS Oral Airway Ambubag Stethoscope Endotracheal Tubes Laryngoscope Face Mask Oxygen Delivery Unit 50% Dextrose Water Normal Saline/Ringers Lactate Umbilical Catheter
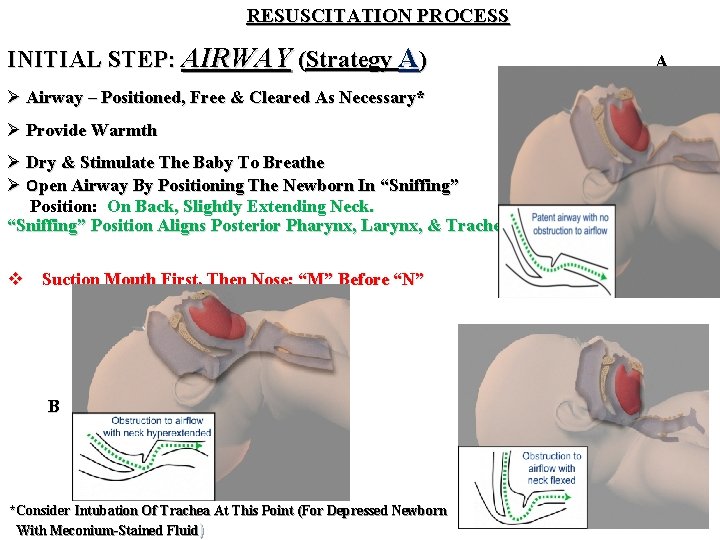
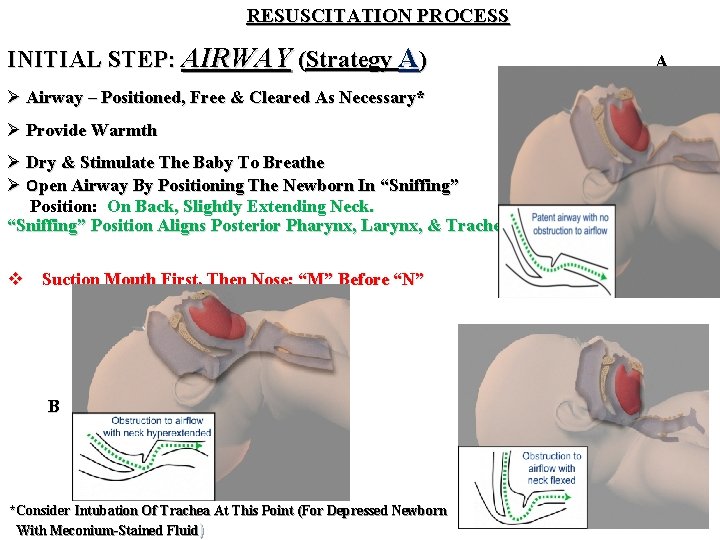
RESUSCITATION PROCESS INITIAL STEP: AIRWAY (Strategy A) A Ø Airway – Positioned, Free & Cleared As Necessary* Ø Provide Warmth Ø Dry & Stimulate The Baby To Breathe Ø Open Airway By Positioning The Newborn In “Sniffing” Position: On Back, Slightly Extending Neck. “Sniffing” Position Aligns Posterior Pharynx, Larynx, & Trachea v Suction Mouth First, Then Nose; “M” Before “N” B B *Consider Intubation Of Trachea At This Point (For Depressed Newborn With Meconium-Stained Fluid) C
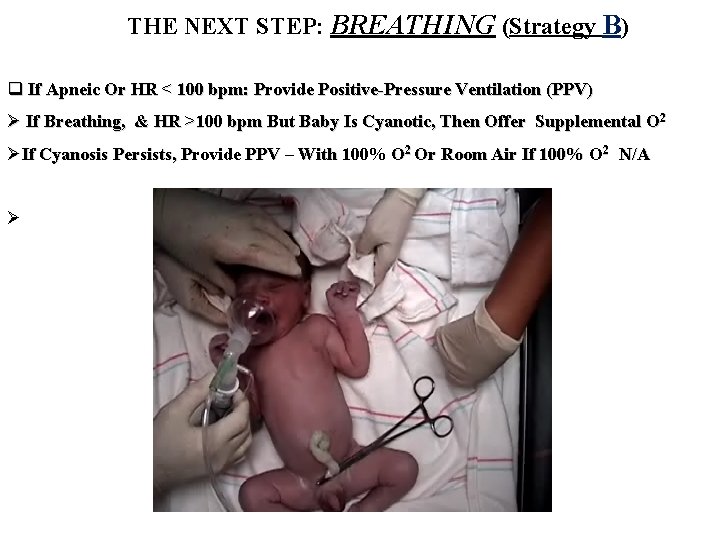
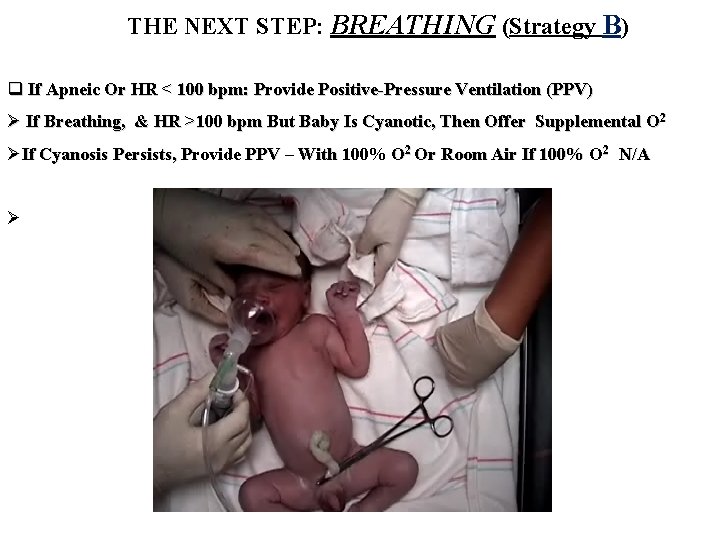
THE NEXT STEP: BREATHING (Strategy B) q If Apneic Or HR < 100 bpm: Provide Positive-Pressure Ventilation (PPV) Ø If Breathing, & HR >100 bpm But Baby Is Cyanotic, Then Offer Supplemental O 2 ØIf Cyanosis Persists, Provide PPV – With 100% O 2 Or Room Air If 100% O 2 N/A Ø
NEXT STEP: CIRCULATION/CARDIAC (Strategy C) q If HR<60 bpm Despite Adequate Ventilation For 30 Seconds: ü Provide Chest Compressions As You Continue Assisted Ventilation ü Then Evaluate Again; If HR Still <60 bpm, Then Start Strategy D
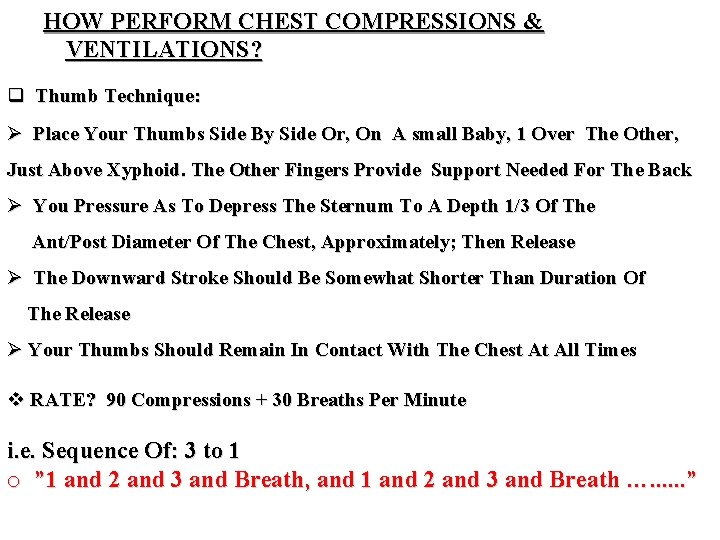
HOW PERFORM CHEST COMPRESSIONS & VENTILATIONS? q Thumb Technique: Ø Place Your Thumbs Side By Side Or, On A small Baby, 1 Over The Other, Just Above Xyphoid. The Other Fingers Provide Support Needed For The Back Ø You Pressure As To Depress The Sternum To A Depth 1/3 Of The Ant/Post Diameter Of The Chest, Approximately; Then Release Ø The Downward Stroke Should Be Somewhat Shorter Than Duration Of The Release Ø Your Thumbs Should Remain In Contact With The Chest At All Times v RATE? 90 Compressions + 30 Breaths Per Minute i. e. Sequence Of: 3 to 1 o ” 1 and 2 and 3 and Breath, and 1 and 2 and 3 and Breath …. . . ”
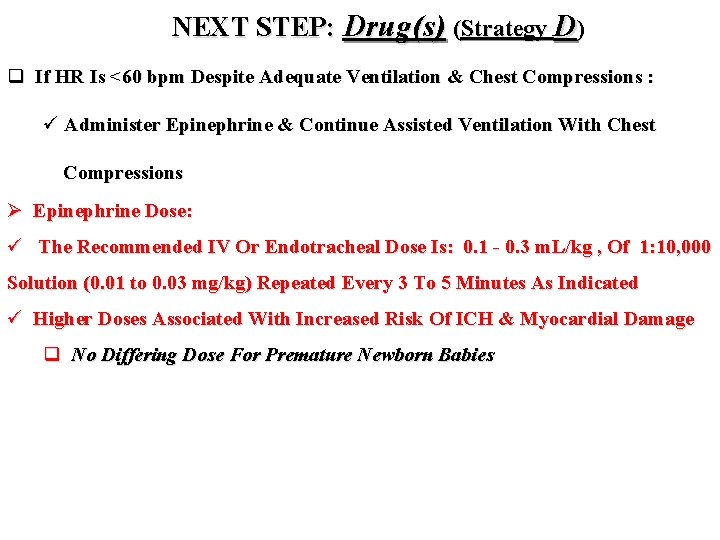
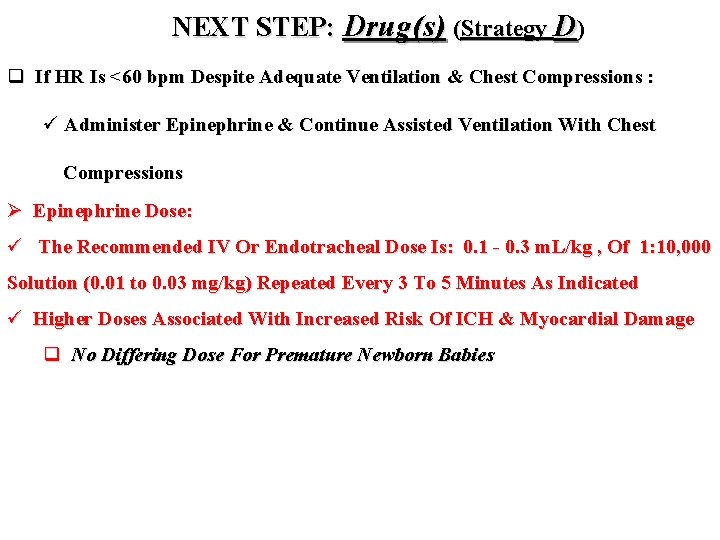
NEXT STEP: Drug(s) (Strategy D) q If HR Is <60 bpm Despite Adequate Ventilation & Chest Compressions : ü Administer Epinephrine & Continue Assisted Ventilation With Chest Compressions Ø Epinephrine Dose: ü The Recommended IV Or Endotracheal Dose Is: 0. 1 - 0. 3 m. L/kg , Of 1: 10, 000 Solution (0. 01 to 0. 03 mg/kg) Repeated Every 3 To 5 Minutes As Indicated ü Higher Doses Associated With Increased Risk Of ICH & Myocardial Damage q No Differing Dose For Premature Newborn Babies
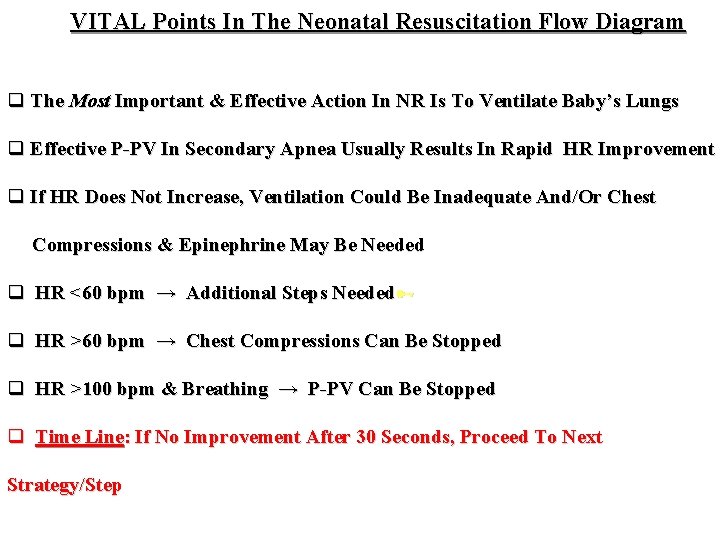
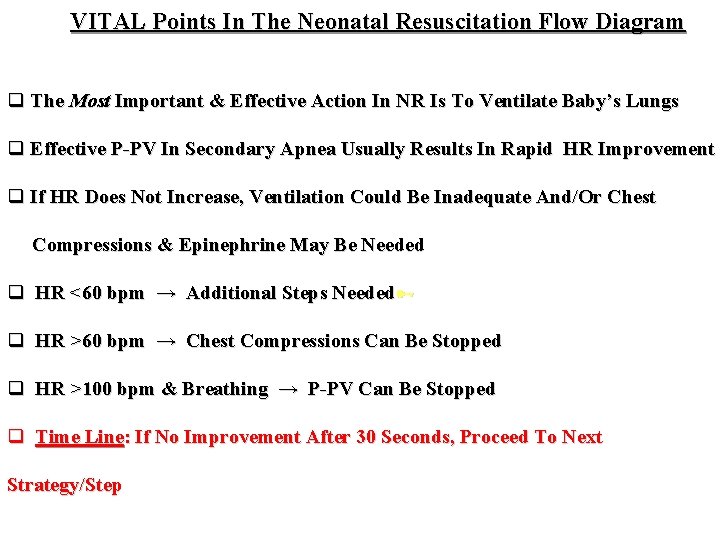
VITAL Points In The Neonatal Resuscitation Flow Diagram q The Most Important & Effective Action In NR Is To Ventilate Baby’s Lungs q Effective P-PV In Secondary Apnea Usually Results In Rapid HR Improvement q If HR Does Not Increase, Ventilation Could Be Inadequate And/Or Chest Compressions & Epinephrine May Be Needed q HR <60 bpm → Additional Steps Needed q HR >60 bpm → Chest Compressions Can Be Stopped q HR >100 bpm & Breathing → P-PV Can Be Stopped q Time Line: If No Improvement After 30 Seconds, Proceed To Next Strategy/Step
Potentially Hazardous Forms Of Stimulation q Slapping Back Or Buttocks q Squeezing Rib Cage q Forcing Thighs Onto Abdomen q Dilating Anal Sphincter q Hot Or Cold Compresses Or Baths q Shaking q DRUGS, e. g. Hydrocortisone, Na. HCO 3 - Especially With Apnea
 Normal apgar score
Normal apgar score Dope neonatal resuscitation
Dope neonatal resuscitation Dr sneha sood
Dr sneha sood Preterm classification
Preterm classification Gcs scale
Gcs scale Score d'apgar
Score d'apgar Apgar score
Apgar score Inopinable
Inopinable C5oh name
C5oh name Apgar 1 minute score
Apgar 1 minute score Apgar score chart
Apgar score chart Apgar score meaning
Apgar score meaning Grimace apgar
Grimace apgar Mount vernon formula
Mount vernon formula Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Principles of resuscitation
Principles of resuscitation Bls
Bls