Raigmore Critical Care Guidelines Paediatric Asthma Guidelines Aim
- Slides: 2
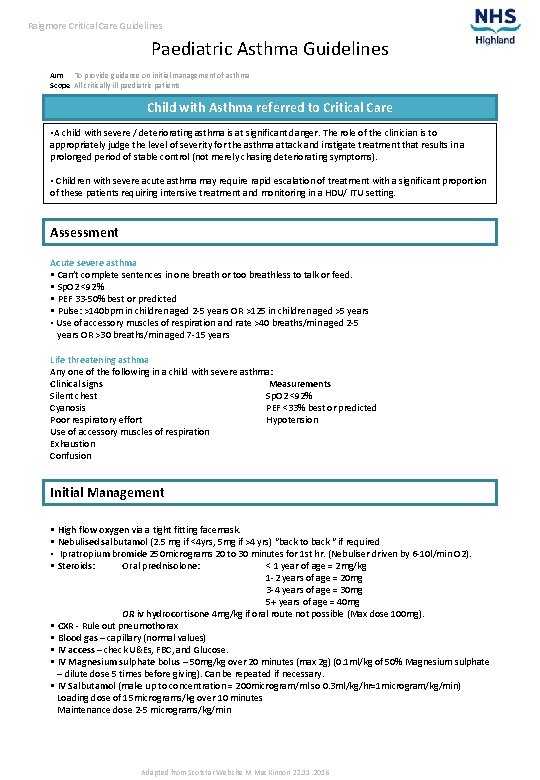
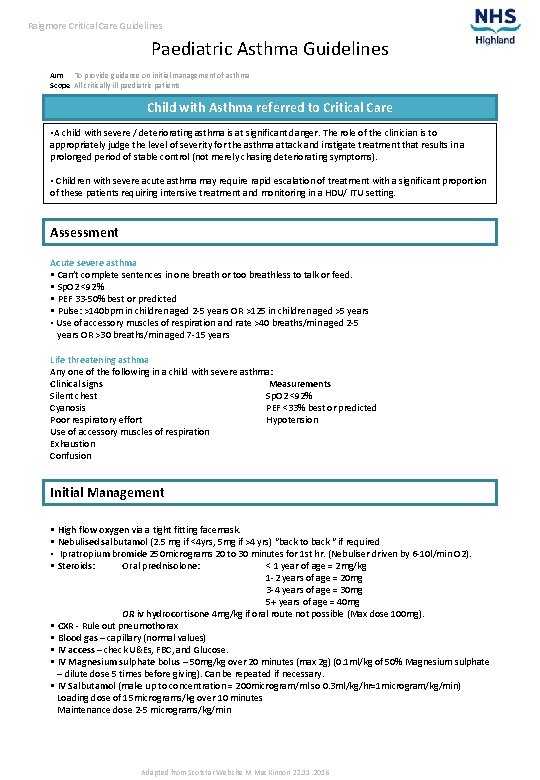
Raigmore Critical Care Guidelines Paediatric Asthma Guidelines Aim To provide guidance on initial management of asthma Scope All critically ill paediatric patients Child with Asthma referred to Critical Care • A child with severe / deteriorating asthma is at significant danger. The role of the clinician is to appropriately judge the level of severity for the asthma attack and instigate treatment that results in a prolonged period of stable control (not merely chasing deteriorating symptoms). • Children with severe acute asthma may require rapid escalation of treatment with a significant proportion of these patients requiring intensive treatment and monitoring in a HDU/ ITU setting. Assessment Acute severe asthma • Can’t complete sentences in one breath or too breathless to talk or feed. • Sp. O 2 <92% • PEF 33 -50% best or predicted • Pulse: >140 bpm in children aged 2 -5 years OR >125 in children aged >5 years • Use of accessory muscles of respiration and rate >40 breaths/min aged 2 -5 years OR >30 breaths/min aged 7 -15 years Life threatening asthma Any one of the following in a child with severe asthma: Clinical signs Measurements Silent chest Sp. O 2 <92% Cyanosis PEF <33% best or predicted Poor respiratory effort Hypotension Use of accessory muscles of respiration Exhaustion Confusion Initial Management • High flow oxygen via a tight fitting facemask. • Nebulised salbutamol (2. 5 mg if <4 yrs, 5 mg if >4 yrs) “back to back “ if required • Ipratropium bromide 250 micrograms 20 to 30 minutes for 1 st hr. (Nebuliser driven by 6 -10 l/min O 2). • Steroids: Oral prednisolone: < 1 year of age = 2 mg/kg 1 -2 years of age = 20 mg 3 -4 years of age = 30 mg 5+ years of age = 40 mg OR iv hydrocortisone 4 mg/kg if oral route not possible (Max dose 100 mg). • CXR - Rule out pneumothorax • Blood gas – capillary (normal values) • IV access – check U&Es, FBC, and Glucose. • IV Magnesium sulphate bolus – 50 mg/kg over 20 minutes (max 2 g) (0. 1 ml/kg of 50% Magnesium sulphate – dilute dose 5 times before giving). Can be repeated if necessary. • IV Salbutamol (make up to concentration = 200 microgram/ml so 0. 3 ml/kg/hr=1 microgram/kg/min) Loading dose of 15 micrograms/kg over 10 minutes Maintenance dose 2 -5 micrograms/kg/min Adapted from Scotstar Website M Mac. Kinnon 22. 11. 2016
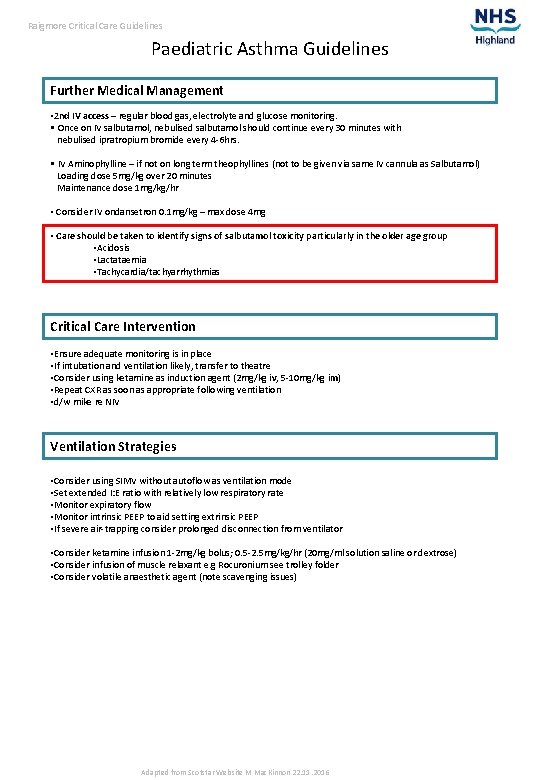
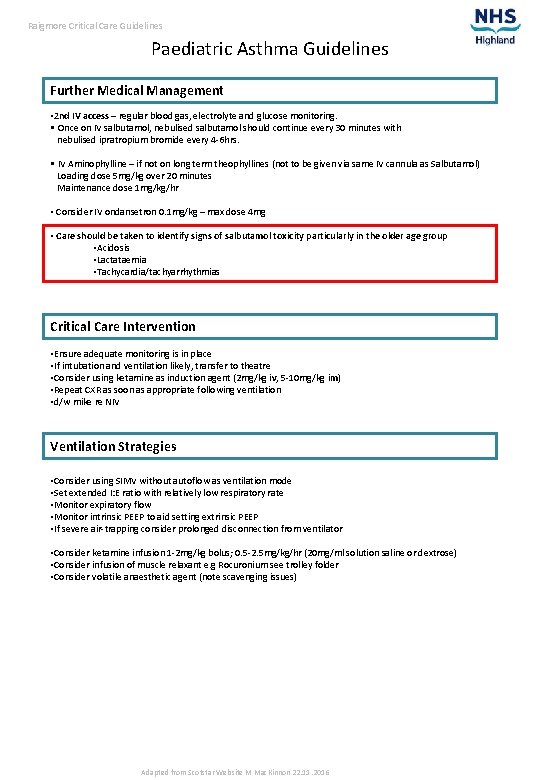
Raigmore Critical Care Guidelines Paediatric Asthma Guidelines Further Medical Management • 2 nd IV access – regular blood gas, electrolyte and glucose monitoring. • Once on IV salbutamol, nebulised salbutamol should continue every 30 minutes with nebulised ipratropium bromide every 4 -6 hrs. • IV Aminophylline – if not on long term theophyllines (not to be given via same IV cannula as Salbutamol) Loading dose 5 mg/kg over 20 minutes Maintenance dose 1 mg/kg/hr • Consider IV ondansetron 0. 1 mg/kg – max dose 4 mg • Care should be taken to identify signs of salbutamol toxicity particularly in the older age group • Acidosis • Lactataemia • Tachycardia/tachyarrhythmias Critical Care Intervention • Ensure adequate monitoring is in place • If intubation and ventilation likely, transfer to theatre • Consider using ketamine as induction agent (2 mg/kg iv, 5 -10 mg/kg im) • Repeat CXR as soon as appropriate following ventilation • d/w mike re NIV Ventilation Strategies • Consider using SIMV without autoflow as ventilation mode • Set extended I: E ratio with relatively low respiratory rate • Monitor expiratory flow • Monitor intrinsic PEEP to aid setting extrinsic PEEP • If severe air-trapping consider prolonged disconnection from ventilator • Consider ketamine infusion 1 -2 mg/kg bolus; 0. 5 -2. 5 mg/kg/hr (20 mg/ml solution saline or dextrose) • Consider infusion of muscle relaxant e. g Rocuronium see trolley folder • Consider volatile anaesthetic agent (note scavenging issues) Adapted from Scotstar Website M Mac. Kinnon 22. 11. 2016