Antiseizure drugs and agents used in neurodegenerative diseases























- Slides: 47
Antiseizure drugs and agents used in neurodegenerative diseases School of Medicine Split Department of Pharmacology
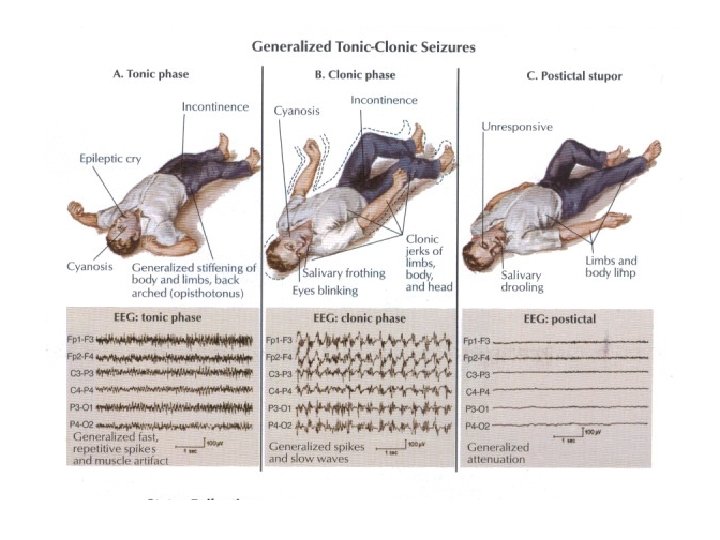
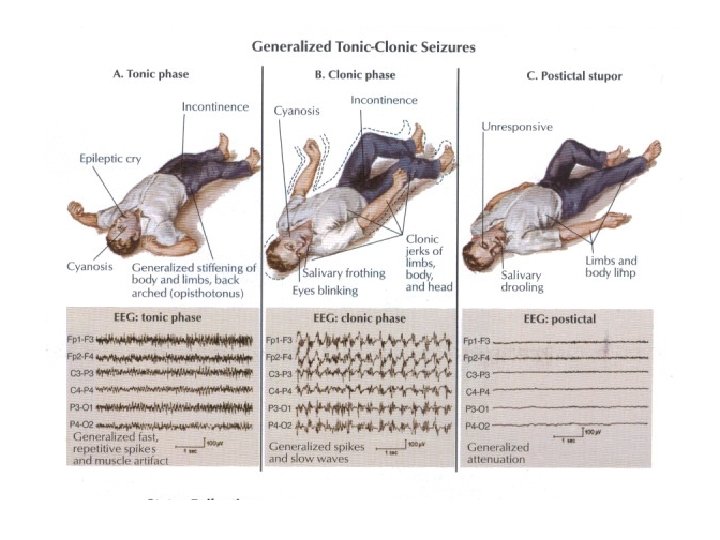
Antiseizure drugs Epilepsy = a chronic disorder characterized by reccurent seizures Seizure = finate episode of brain dysfunction resulting from abnormal discharge of cerebral neurons
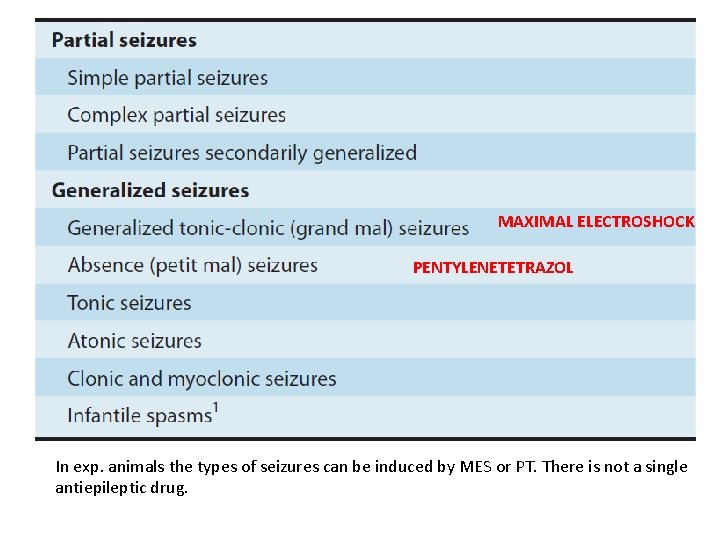
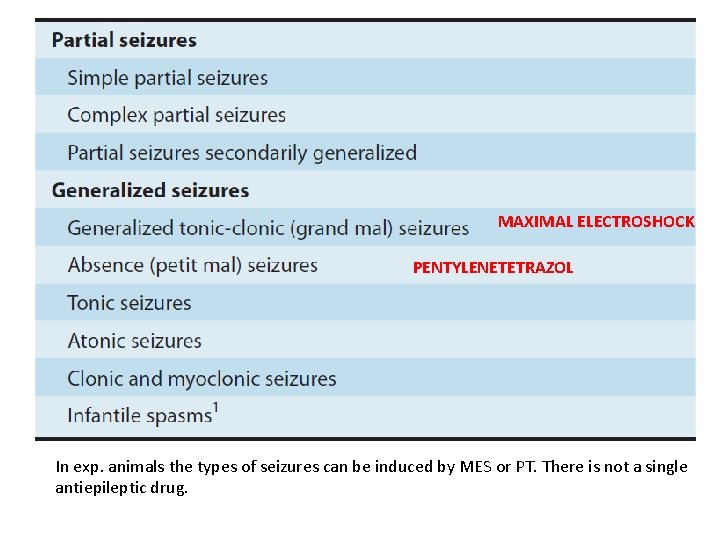
MAXIMAL ELECTROSHOCK PENTYLENETETRAZOL In exp. animals the types of seizures can be induced by MES or PT. There is not a single antiepileptic drug.

http: //www. youtube. com/watch? v=r. TWGEf. Hr WNE http: //www. youtube. com/watch? v=N 20 bxt. C 0 RAo




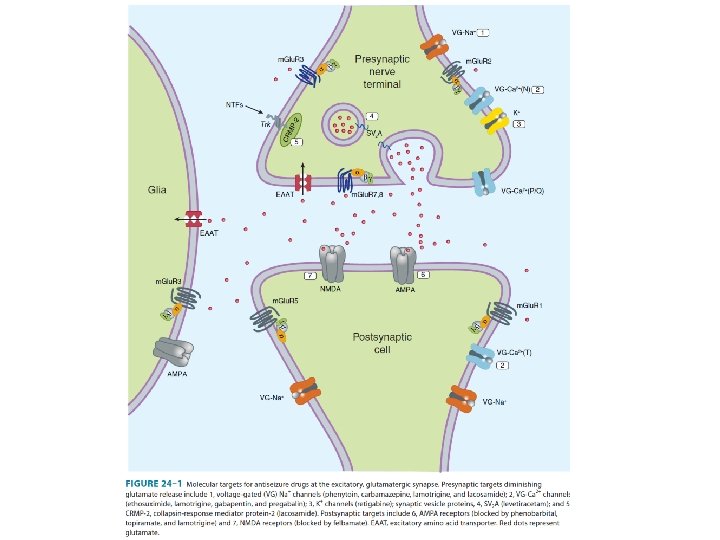
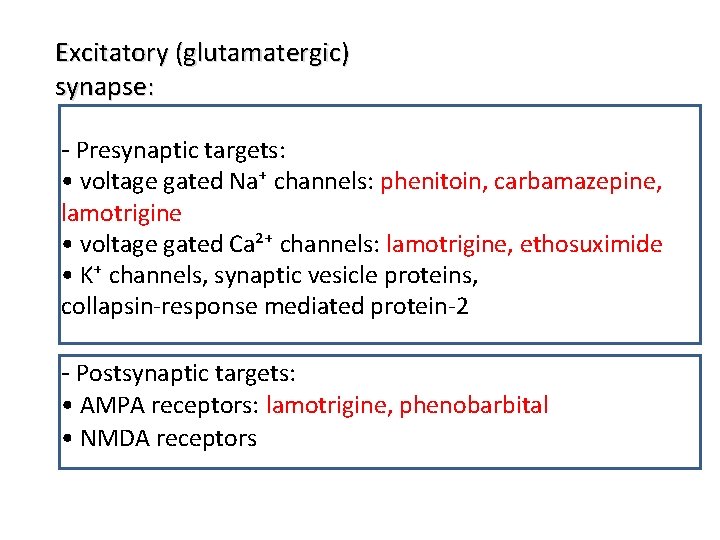
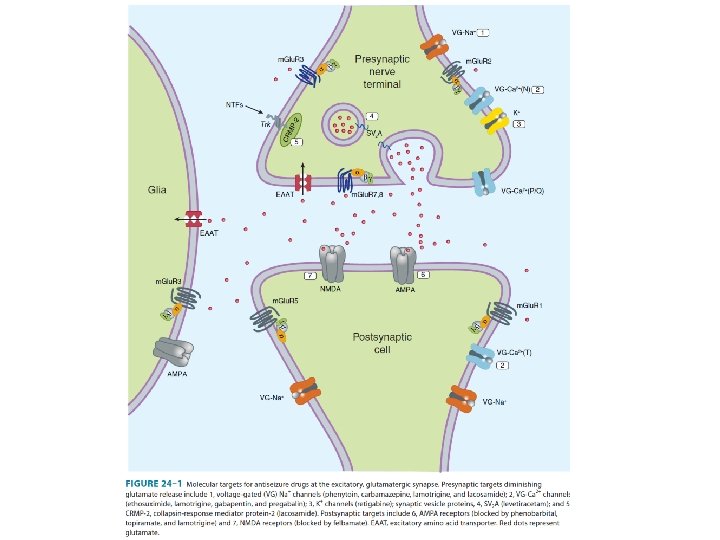
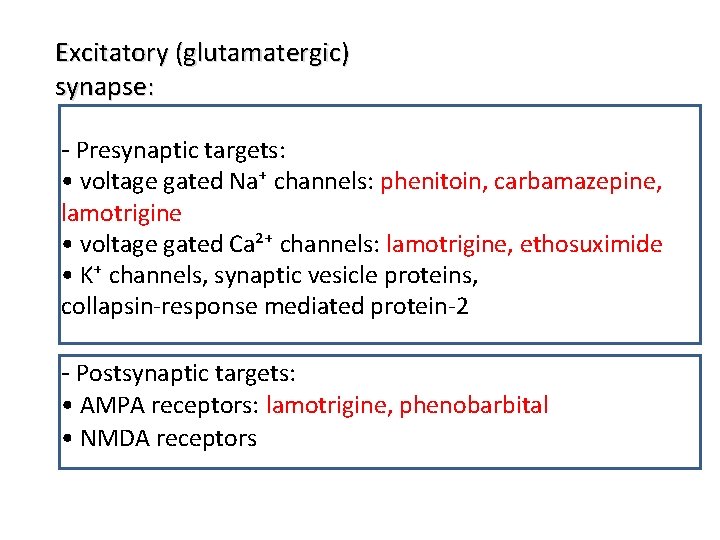
Excitatory (glutamatergic) synapse: - Presynaptic targets: • voltage gated Na⁺ channels: phenitoin, carbamazepine, lamotrigine • voltage gated Ca²⁺ channels: lamotrigine, ethosuximide • K⁺ channels, synaptic vesicle proteins, collapsin-response mediated protein-2 - Postsynaptic targets: • AMPA receptors: lamotrigine, phenobarbital • NMDA receptors

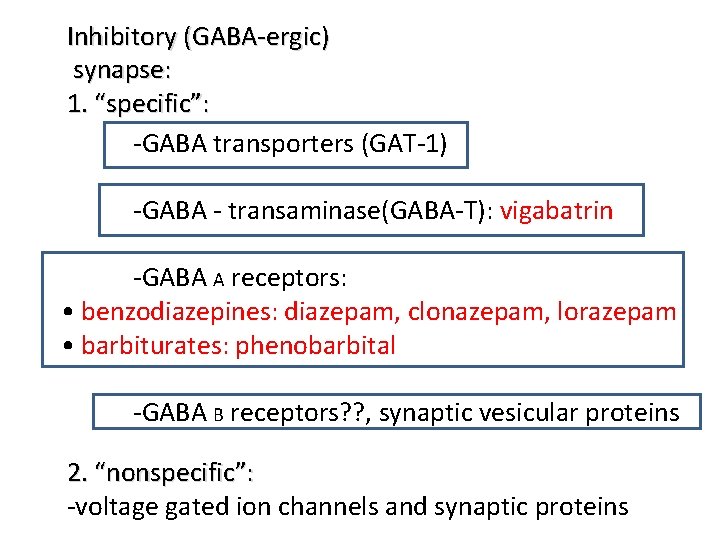
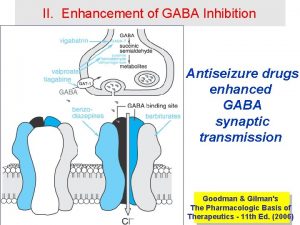
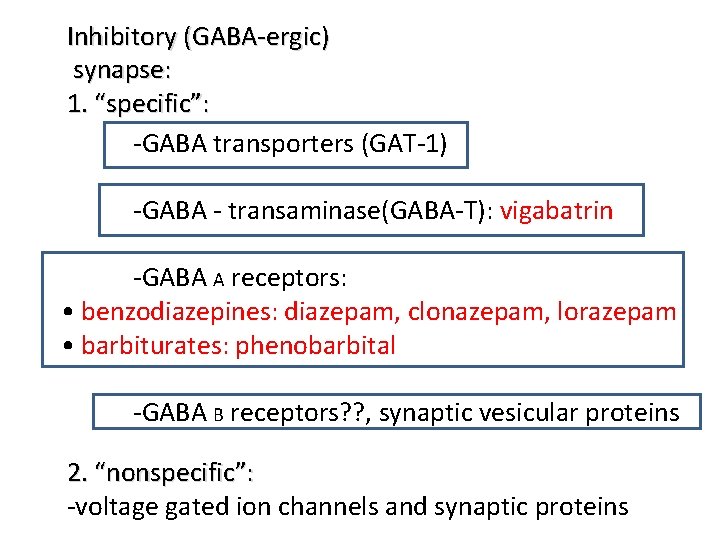
Inhibitory (GABA-ergic) synapse: 1. “specific”: -GABA transporters (GAT-1) -GABA - transaminase(GABA-T): vigabatrin -GABA A receptors: • benzodiazepines: diazepam, clonazepam, lorazepam • barbiturates: phenobarbital -GABA B receptors? ? , synaptic vesicular proteins 2. “nonspecific”: -voltage gated ion channels and synaptic proteins

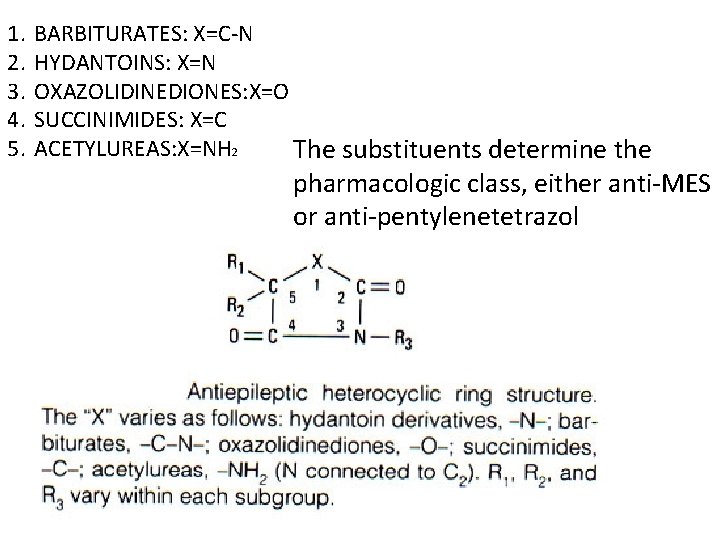
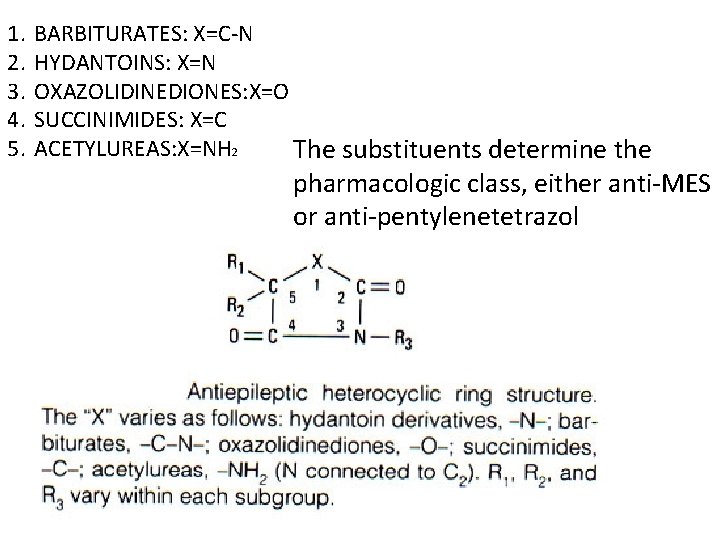
1. 2. 3. 4. 5. BARBITURATES: X=C-N HYDANTOINS: X=N OXAZOLIDINEDIONES: X=O SUCCINIMIDES: X=C ACETYLUREAS: X=NH 2 The substituents determine the pharmacologic class, either anti-MES or anti-pentylenetetrazol
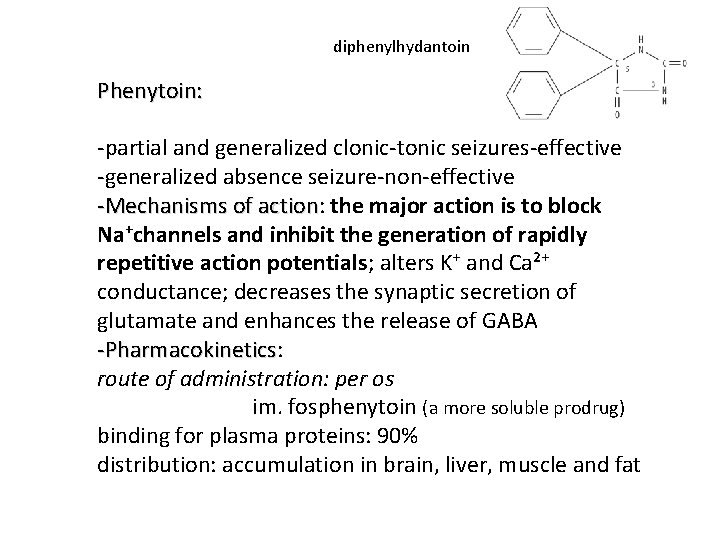
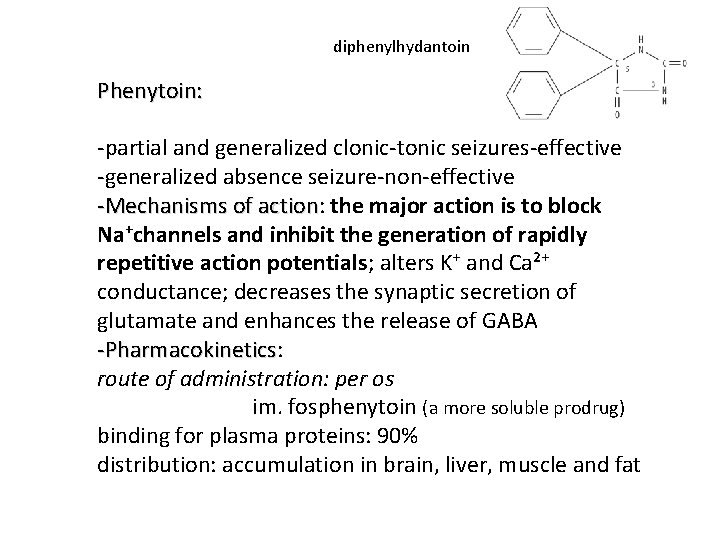
diphenylhydantoin Phenytoin: -partial and generalized clonic-tonic seizures-effective -generalized absence seizure-non-effective -Mechanisms of action: action the major action is to block Na⁺channels and inhibit the generation of rapidly repetitive action potentials; alters K⁺ and Ca²⁺ conductance; decreases the synaptic secretion of glutamate and enhances the release of GABA -Pharmacokinetics: -Pharmacokinetics route of administration: per os im. fosphenytoin (a more soluble prodrug) binding for plasma proteins: 90% distribution: accumulation in brain, liver, muscle and fat
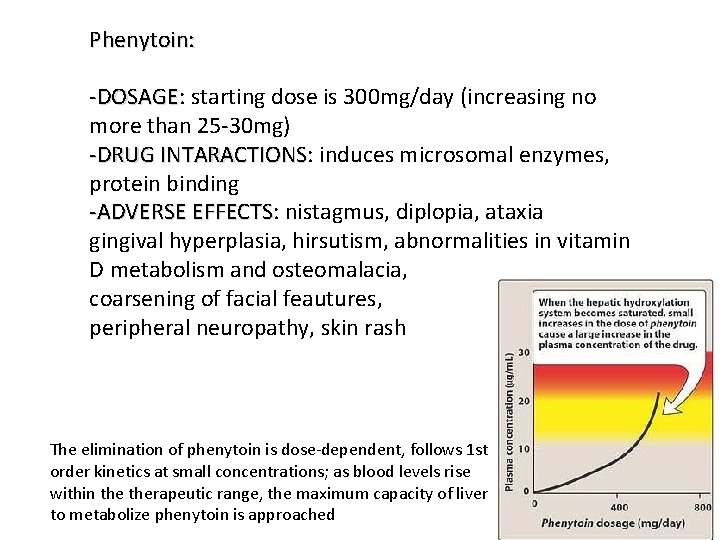
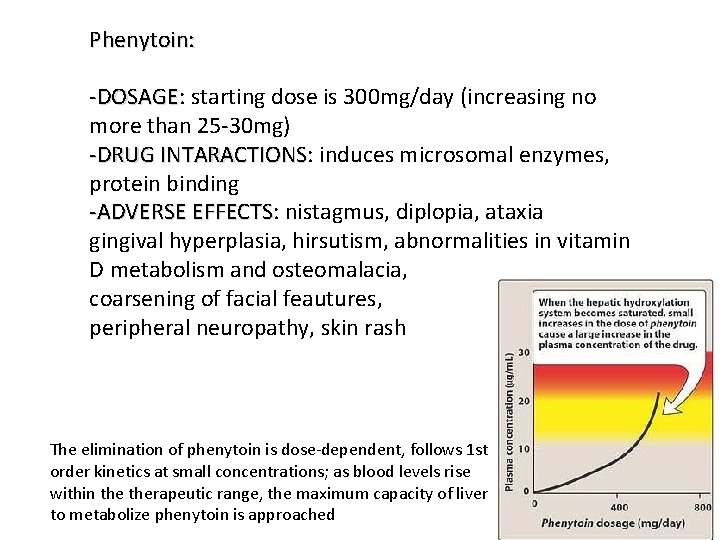
Phenytoin: -DOSAGE: DOSAGE starting dose is 300 mg/day (increasing no more than 25 -30 mg) -DRUG INTARACTIONS: INTARACTIONS induces microsomal enzymes, protein binding -ADVERSE EFFECTS: EFFECTS nistagmus, diplopia, ataxia gingival hyperplasia, hirsutism, abnormalities in vitamin D metabolism and osteomalacia, coarsening of facial feautures, peripheral neuropathy, skin rash The elimination of phenytoin is dose-dependent, follows 1 st order kinetics at small concentrations; as blood levels rise within therapeutic range, the maximum capacity of liver to metabolize phenytoin is approached
ureide moiety Carbamazepine: -partial and generalized clonic-tonic seizures-effective -generalized absence seizure-non-effective -trigeminal neuralgia; (mania in) bipolar depressioneffective -Mechanism of action: action the major action is to block Na⁺channels and inhibit the generation of rapidly repetitive action potentials, descreases synaptic transmission, potentiate volatage-gated K⁺ current
-DOSAGE: DOSAGE several times a day 1 -2 g - DRUG INTARACTIONS : induction of hepatic microsomal enzymes!!!! (CYP 3 -A 4) - ADVERSE EFFECTS diplopia and ataxia, gastrointestinal upsets, hyponatriemia with water intoxication, leukopenia, erythematous skin rash (idiosincratic)
VIGABATRIN: -complex partial seizures, infantile spasmseffective -MECHANISMS OF ACTION: ACTION irreversible inhibition of GABA-aminotransferase -per os -DOSAGE: DOSAGE several times a day 2 -3 g -INTERACTIONS: -INTERACTIONS relative contraidication is psychosis -ADVERSE EFFECTS: EFFECTS drawsiness, dizziness, weight gain, agitation, confusion, psychosis, peripheral visual field defects

LAMOTRIGINE: -monotherapy for partial seizures; absence, myoclonic seizures, Lennox-Gastaut syndrome-effective -MECHANISMS OF ACTION: ACTION the major action is to block Na⁺channels and inhibit the generation of rapidly repetitive action potentials; Ca²⁺ conductance; decreases the synaptic secretion of glutamate -DOSAGE: DOSAGE 200 -300 mg/day -INTERACTIONS: -INTERACTIONS valproate couses a two-fold increase in the half-life of lamotrigine -ADVERSE EFFECTS: EFFECTS dizziness, headache, diplopia, somnolence, nausea and skin rush,

VALPROIC ACID AND SODIUM VALPROATE: • CHEMISTRY: CHEMISTRY monocarbocylic acid (8 C atoms) • Clinical uses: absence and clonic-tonic seizures • Mechanisms of actions: Na⁺ and Ca ²⁺- channels inhibition and decreased GABA degradation • Adverse effects: - hair loss, anorexia, nausea, vomiting - hepatotoxicity (children) - teratogenicity Inhibition of drugs that are metabolized by CYP 2 C 9 (phenitoin, phenobarbital)!



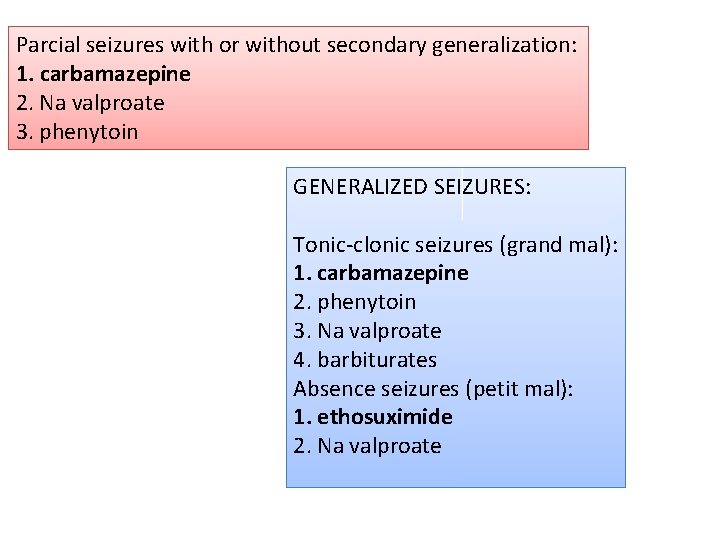
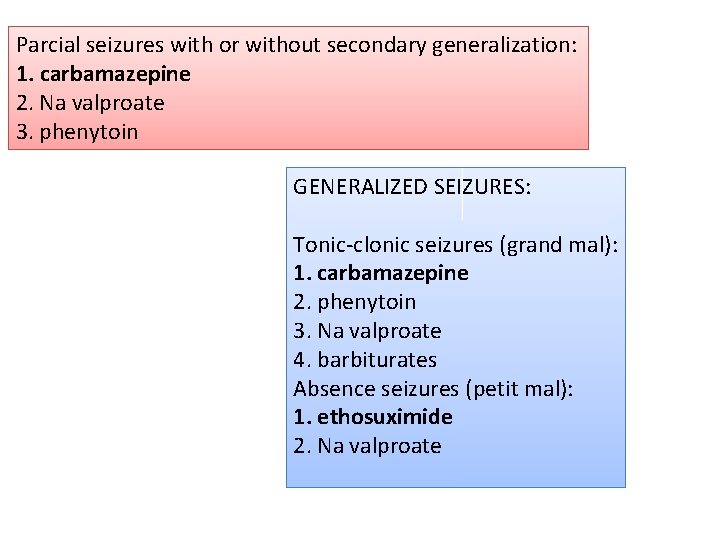
Parcial seizures with or without secondary generalization: 1. carbamazepine 2. Na valproate 3. phenytoin GENERALIZED SEIZURES: Tonic-clonic seizures (grand mal): 1. carbamazepine 2. phenytoin 3. Na valproate 4. barbiturates Absence seizures (petit mal): 1. ethosuximide 2. Na valproate

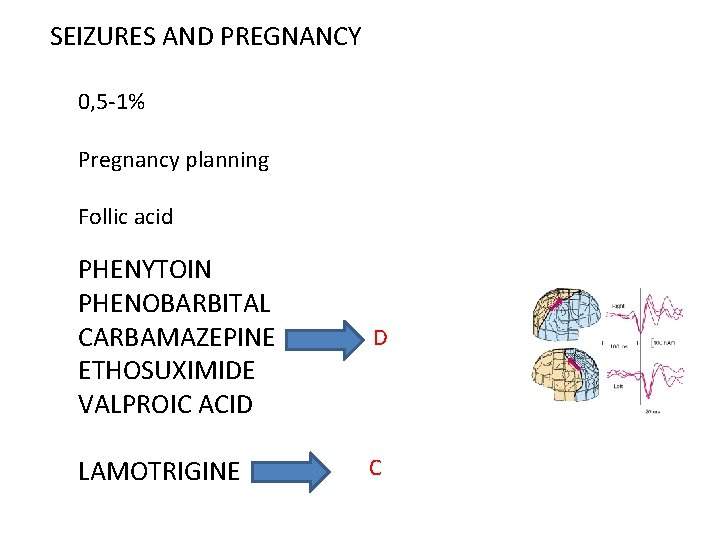
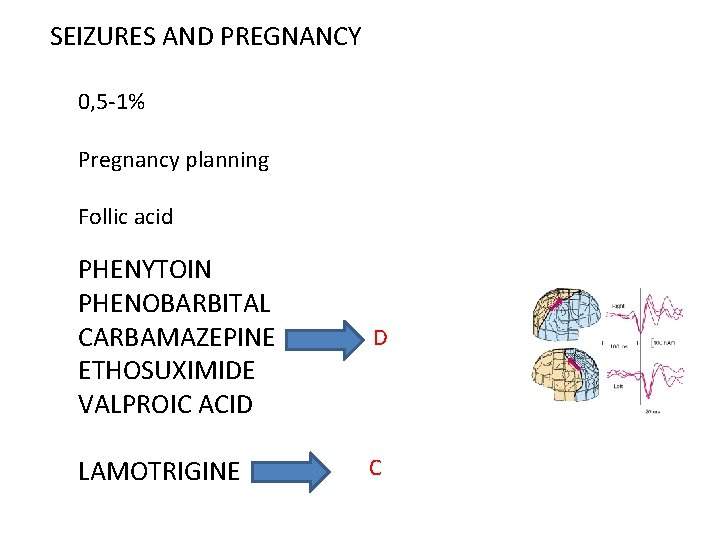
SEIZURES AND PREGNANCY 0, 5 -1% Pregnancy planning Follic acid PHENYTOIN PHENOBARBITAL CARBAMAZEPINE ETHOSUXIMIDE VALPROIC ACID D LAMOTRIGINE C
AGENTS USED IN NEURODEGENERATIVE DISEASES 1. Drugs used in Parkinson’s disease 2. Drugs used in Alzheimer’s disease (Rivastigmine)
Parkinson’s disease • Definition: - Progressive neurodegenerative diseaseof the basal ganglia causing: - tremor at rest - hipokinesia - muscle rigidity -often with dementia and autonomic dysfunction





NEUROCHEMICAL CHANGES: • Low level of dopamine • Other monoamines (noradrenaline and serotonine) are much less affected • Gradual loss of dopamnine occurs over several years with symtoms of PD appearing only when the striatal dopamine content has fallen to 20 -40 % of normal • The symtom most clearly related to dopamine defficiency is hypokinesiawhich occurs immediately • Hyperreactivity of cholinergic neurons contributes significantly to the symtoms of PD


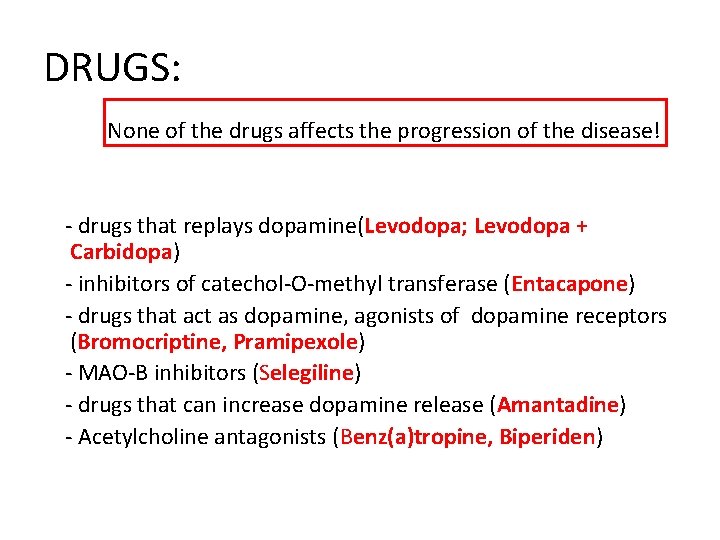
DRUGS: None of the drugs affects the progression of the disease! - drugs that replays dopamine(Levodopa; Levodopa + Carbidopa) - inhibitors of catechol-O-methyl transferase (Entacapone) - drugs that act as dopamine, agonists of dopamine receptors (Bromocriptine, Pramipexole) - MAO-B inhibitors (Selegiline) - drugs that can increase dopamine release (Amantadine) - Acetylcholine antagonists (Benz(a)tropine, Biperiden)
LEVODOPA • Dopamin does not penetrate the blood-braine barrier. The immediate precursor of dopamine LEVODOPA enters the brain where it is decarbocylated to dopamine • Only about 1 -3 % of administered levodopa actually enters the brain unaltered; the reminder is metabilized extracerebrally into dopamine • It is given in combination with a peripheral dopa decarboxilase inhibitor (carbidopa); peripheral metabolism is reduced, plasma levels are higher and half-life is longer

Therapeutic efficacy • Particulary effective in …. relieving bradykinesia Adverse effects • After 3 or 4 years of • Dyskinesias (choreoathetosis of treatment the benefits the face and distal extremities. begin to diminish • Fluctuation in clinical response: 1. wearing-off or and-of–doseakinesia 2. unrelated to the timing of dose, on-off phenomenon (off - periods of marked akinesia alternate over the course of few hours with on – peiods with improved mobility but marked dyskinesias


 Leavening agents in quick breads
Leavening agents in quick breads Examples of pour batter
Examples of pour batter Leavening agents used in quick breads
Leavening agents used in quick breads Syrup dosage form
Syrup dosage form Diagnostic agents are the compounds used to
Diagnostic agents are the compounds used to Hydroalcoholic solution are syrups
Hydroalcoholic solution are syrups Eva tray in labour room
Eva tray in labour room Fetal hydantoin syndrome
Fetal hydantoin syndrome Modern lifestyle and hypokinetic diseases
Modern lifestyle and hypokinetic diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Section 19-3 diseases caused by bacteria and viruses
Section 19-3 diseases caused by bacteria and viruses Chapter 8 skin disorders and diseases
Chapter 8 skin disorders and diseases Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Nail diseases and disorders milady
Nail diseases and disorders milady Seborrheic keratoses
Seborrheic keratoses Describe how to conduct nail and skin analysis
Describe how to conduct nail and skin analysis Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Cardiovascular system diseases and disorders chapter 8
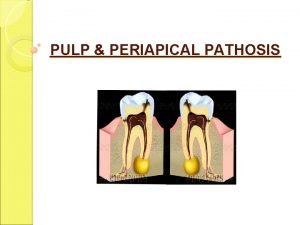
Cardiovascular system diseases and disorders chapter 8 Periapical granuloma vs abscess
Periapical granuloma vs abscess Milady chapter 8 skin disorders and diseases
Milady chapter 8 skin disorders and diseases Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Purulent diseases of lungs and pleura
Purulent diseases of lungs and pleura Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Albugo eye
Albugo eye Venn diagram of communicable and non-communicable diseases
Venn diagram of communicable and non-communicable diseases Macronutrients elements
Macronutrients elements Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Different types of diseases
Different types of diseases Gurus of tqm
Gurus of tqm Protein deficiency diseases
Protein deficiency diseases Natural history of disease
Natural history of disease Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Inflammation of maxillofacial area
Inflammation of maxillofacial area Prescriptive screening vs prospective
Prescriptive screening vs prospective Human diseases a systemic approach
Human diseases a systemic approach Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Periradicular tissues
Periradicular tissues Chapter 32 childhood communicable diseases bioterrorism
Chapter 32 childhood communicable diseases bioterrorism Sarophytes
Sarophytes X linked diseases
X linked diseases Whats a sex linked trait
Whats a sex linked trait