Clinical pharmacology of antiseizure drugs Domina Petric MD








- Slides: 45

Clinical pharmacology of antiseizure drugs Domina Petric, MD
Partial seizures I.
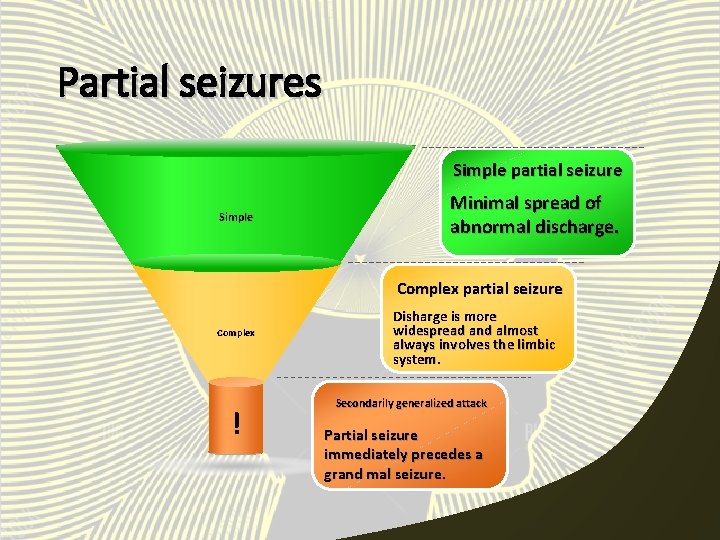
Partial seizures • The attack begins in a specific locus in the brain. Types of partial seizures: • simple partial seizure • complex partial seizure • secondarily generalized attack

Simple partial seizure • It is characterized by minimal spread of the abnormal discharge such that normal consciousness and awareness are preserved. • The patient may have a sudden onset of clonic jerking of an extremity lasting 60 -90 seconds. • Residual weakness may last for 15 -30 minutes after the attack.
Simple partial seizure The patient is completely aware of the attack and can describe it in detail. The EEG (electroencephalogram) may show an abnormal discharge highly localized to the involved portion of the brain.
Complex partial seizure • It has also a localized onset. • The discharge becomes more widespread (usually bilateral) and almost always involves the limbic system. • Most complex partial seizures arise from one of the temporal lobes. • Temporal lobes are susceptible to insults such as hypoxia or infection.
Complex partial seizure • The patient may have a brief warning followed by an alteration of consciousness during which some patients stare and other stagger or even fall. • Most attacks demonstrate fragments of integrated motor behavior: automatisms. • Patient has no memory for automatisms.
Complex partial seizure • Typical automatisms are lip smacking, swallowing, fumbling, scratching and even walking about. • After 30 -120 seconds, the patient makes a gradual recovery to normal consciousness, but may feel tired or ill for several hours after the attack.
Secondarily generalized attack Partial seizure immediately precedes a generalized tonic-clonic (grand mal) seizure.
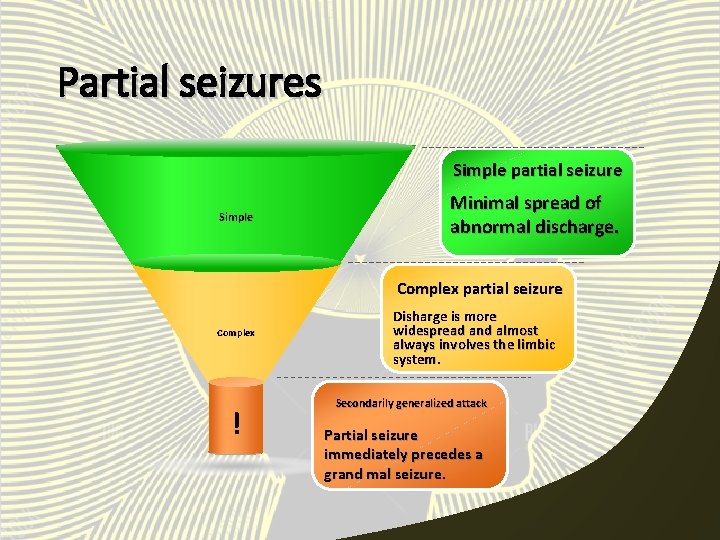
Partial seizures Simple partial seizure Simple Minimal spread of abnormal discharge. Complex partial seizure Complex ! Disharge is more widespread and almost always involves the limbic system. Secondarily generalized attack Partial seizure immediately precedes a grand mal seizure.
Generalized seizures II.
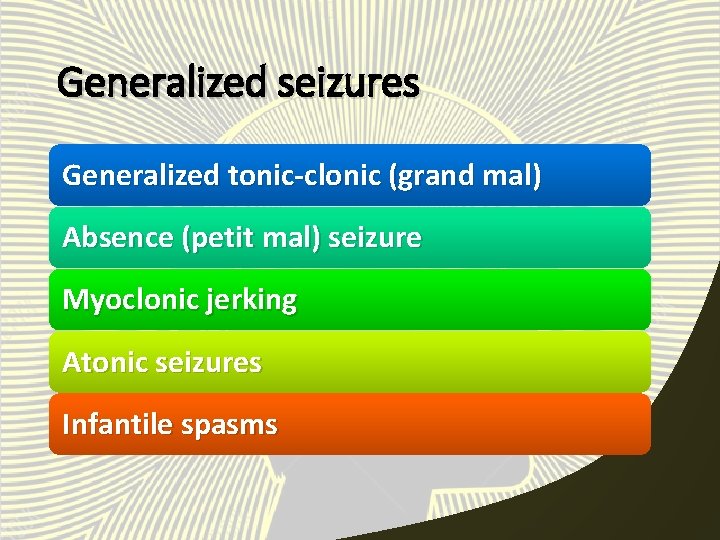
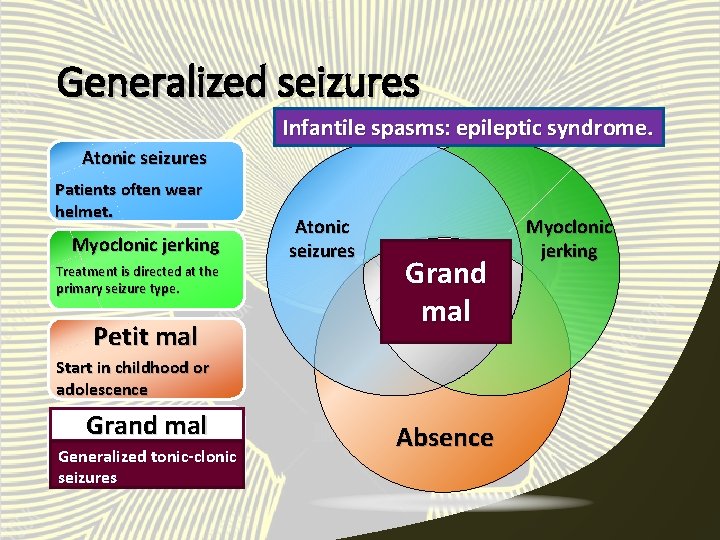
Generalized seizures Generalized tonic-clonic (grand mal) Absence (petit mal) seizure Myoclonic jerking Atonic seizures Infantile spasms
Generalized tonic-clonic • Grand mal seizures are the most dramatic of all epileptic seizures. • These seizures are characterized by tonic rigidity of all extremities, followed in 1530 seconds by a tremor. • Tremor is actually an interruption of the tonus by relaxation.
Generalized tonic-clonic • As the relaxation phase becomes longer, the attack enters the clonic phase, with massive jerking of the body. • The clonic jerking slows over 60 -120 seconds. • The patient is usually left in a stuporous state. • The tongue or cheek may be bitten. • Urinary incontinence is common.
Generalized tonic-clonic Primary generalized tonic-clonic seizures begin without evidence of localized onset. Secondarily generalized seizures are preceded by another seizure type, usually a partial seizure.

Absence seizure • Petit mal seizure is characterized by both sudden onset and abrupt cessation. • Its duration is usually less than 10 seconds and rarely more than 45 seconds. • Consciousness is altered. • The attack may also be associated with mild clonic jerking of the eyelids or extremities, with postural tone changes, autonomic phenomena and automatisms.
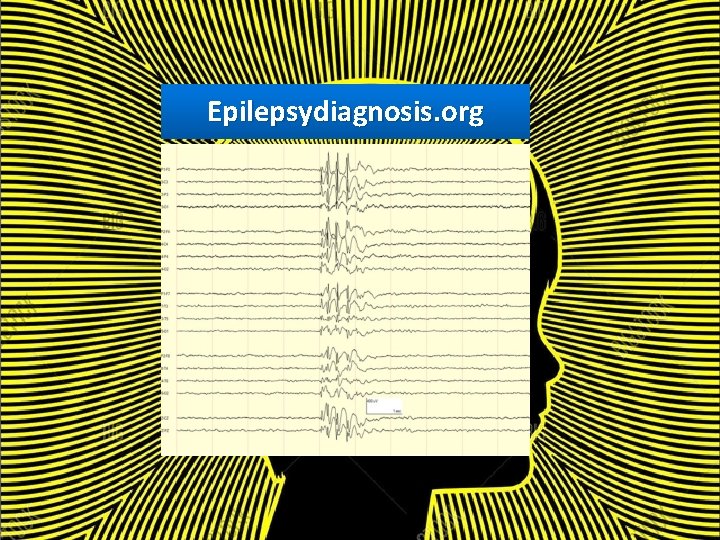
Absence seizure • Absence attacks begin in childhood or adolescence and may occur up to hundreds of times a day. • EEG: 2, 5 -3, 5 Hz spike-and-wave pattern.
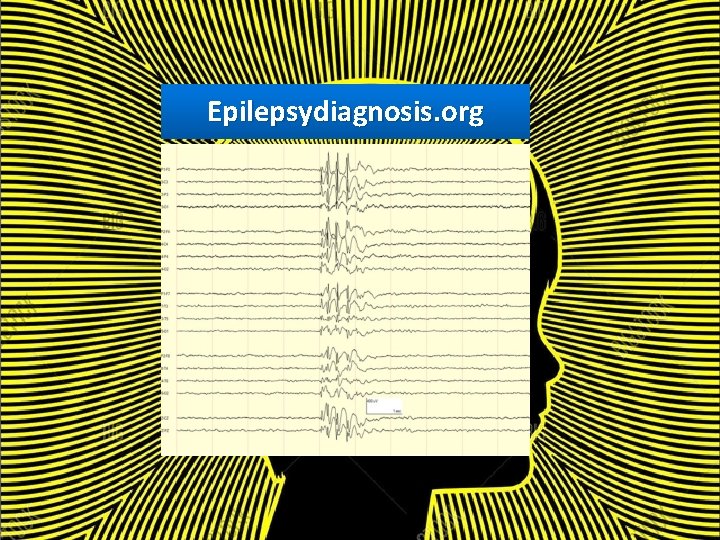
Epilepsydiagnosis. org
Atypical absence Seizures with more abrupt postural changes. Such patients are often mentally retarded. EEG: slower spike-and-wave discharge. Seizures may be more refractory to therapy.
Myoclonic jerking • It is seen in generalized tonic-clonic, partial and absence seizures, and infantile spasms. • Treatment should be directed at the primary seizure type. • Some patients have myoclonic jerking and occasional generalized tonic-clonic seizures without overt signs of neurologic deficit.

Atonic seizures • The patient has sudden loss of postural tone. • If standing, the patient falls suddenly to the floor and may be injured. • If seated, the head and torso may suddenly drop forward. • Most often in children, but not unusual in adults. • Many patients wear helmet.
Atonic seizures Momentary increased tone may be observed in some patients: tonicatonic seizure.


Infantile spasms Epileptic syndrome. The attack is most often bilateral. Infantile spasms are most often characterized clinically by brief, recurrent myoclonic jerks of the body with sudden flexion or extension of the body and limbs. • 90% of affected patients have their first attack before the age of 1 year. • Most patients are intellectually delayed. • • •
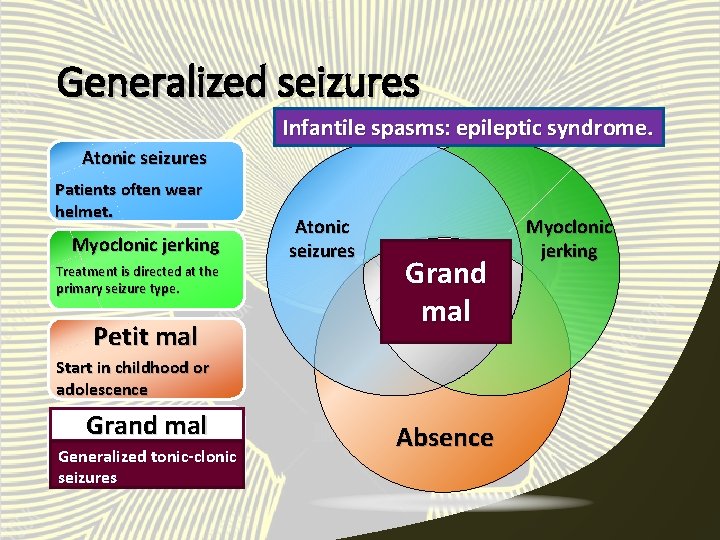
Generalized seizures Infantile spasms: epileptic syndrome. Atonic seizures Patients often wear helmet. Myoclonic jerking Treatment is directed at the primary seizure type. Petit mal Atonic seizures Grand mal Start in childhood or adolescence Grand mal Generalized tonic-clonic seizures Absence Myoclonic jerking

Therapeutic strategy III.
Therapeutic strategy • The use of a single drug is preferred, especially in patients who are not severely affected and who can benefit from the advantage of fewer adverse effects. • For patients with hard-to-control seizures, multiple drugs are usually utilized simultaneously.
Therapeutic strategy • The therapeutic index for most antiseizure drugs is low. • Toxicity is not uncommon. • Effective treatment of seizures often requires an awareness of therapeutic levels and pharmacokinetic properties as well as the characteristic toxicities of each agent.
Therapeutic strategy Measurements of antiseizure drug plasma levels can be very useful when combined with clinical observations and pharmacokinetic data.
Management of epilepsy IV.
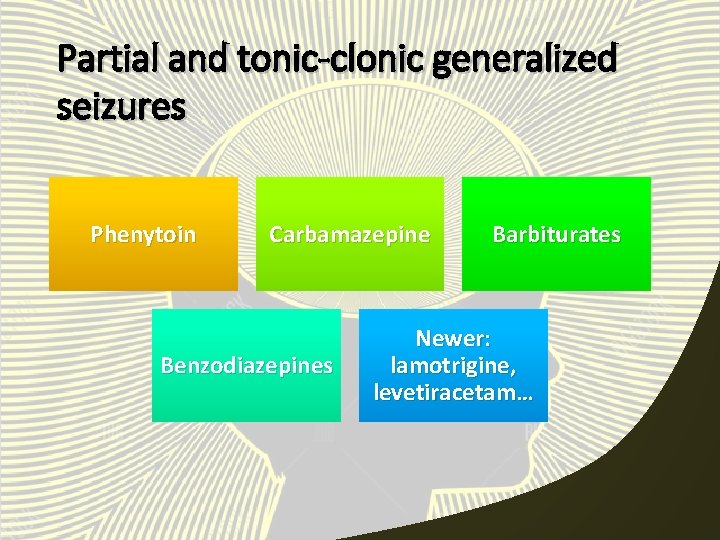
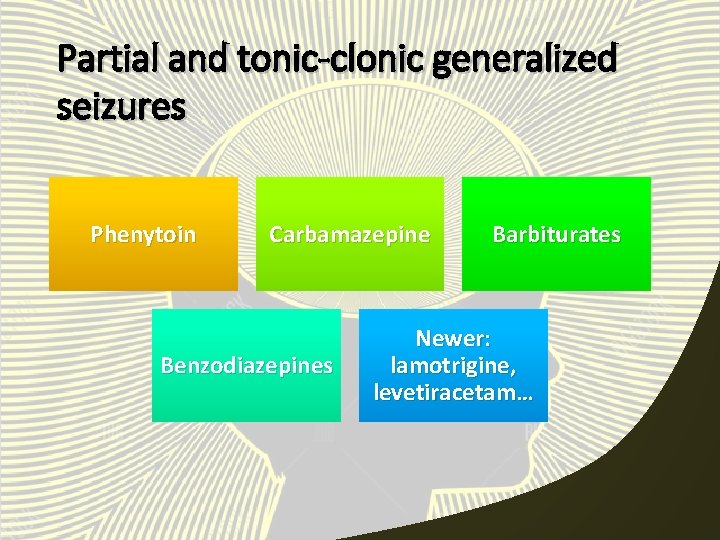
Partial and tonic-clonic generalized seizures Phenytoin Carbamazepine Benzodiazepines Barbiturates Newer: lamotrigine, levetiracetam…
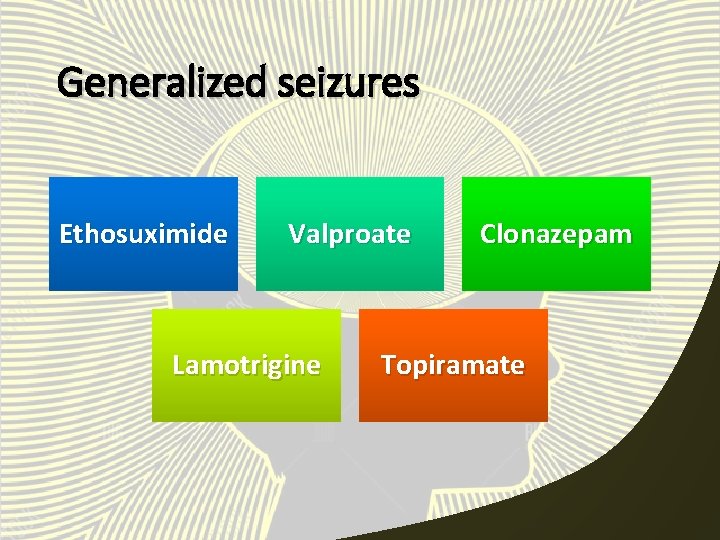
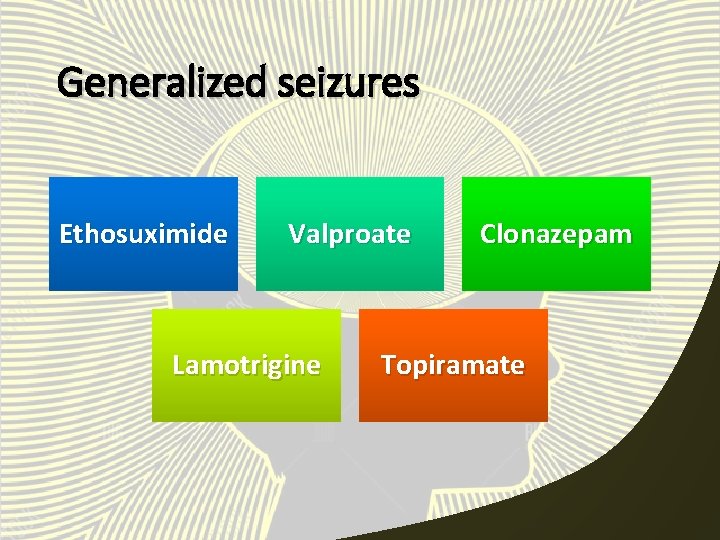
Generalized seizures Ethosuximide Valproate Lamotrigine Clonazepam Topiramate
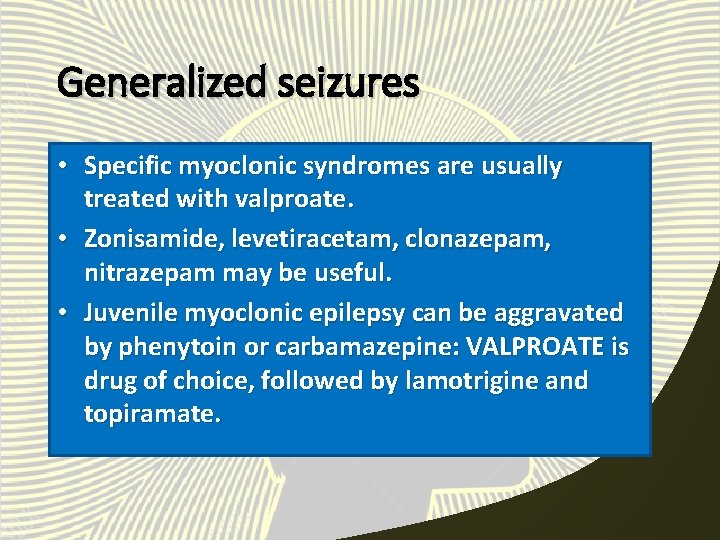
Generalized seizures • Specific myoclonic syndromes are usually treated with valproate. • Zonisamide, levetiracetam, clonazepam, nitrazepam may be useful. • Juvenile myoclonic epilepsy can be aggravated by phenytoin or carbamazepine: VALPROATE is drug of choice, followed by lamotrigine and topiramate.
Generalized seizures Atonic seizures are often refractory to all available medications. Valproate, lamotrigine, benzodiazepines and felbamate may be helpful is some patients. The ketogenic diet may also be useful.

Infantile spasms • The treatment is limited to improvement of control of the seizures. • Most patients receive a course of im. corticotropin. • Prednisone may be equally effective and can be given orally. • Other drugs: clonazepam, nitrazepam, vigabatrin.
Status epilepticus • Diazepam is the most effective drug in most patients. • It is given iv. 10 mg bolus up to 20 -30 mg in adults. • It may depress respiration and, less frequently, cardiovascular function. • Lorazepam has longer duration of action.
Generalized seizures • Fosphenytoin iv. • Phenobarbital 100 -200 mg iv. to a total of 400 -800 mg. • Lidocaine iv. • Benzodiazepines or iv. valproate for absence status.
Toxicology of antiseizure drugs V.
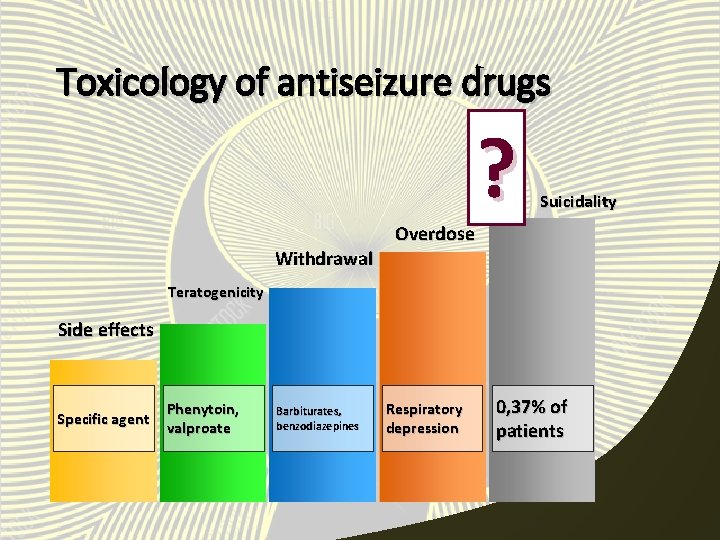
Teratogenicity • Children born to mothers taking antiseizure drugs have an increased risk of congenital malformations. • Phenytoin cause fetal hydantoin syndrome. • Pregnant woman taking valproic acid or sodium valproate has a 1 -2% risk of having a child with spina bifida.
Withdrawal • Withdrawal of antiseizure drugs can cause increased seizure frequency and severity. • Withdrawal of anti-absence drugs is easier than withdrawal of drugs needed for partial or generalized tonic-clonic seizures. • Barbiturates and benzodiazepines are the most difficult to discontinue.
Overdose • The most dangerous effect of antiseizure drugs after large overdoses is respiratory depression, which may be potentiated by other agents (for example, alcohol). • Treatment is supportive.
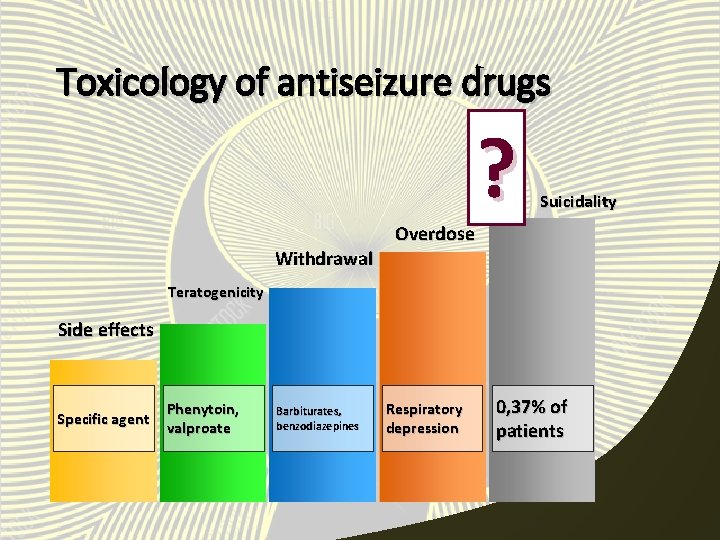
Toxicology of antiseizure drugs Withdrawal Overdose ? Suicidality Teratogenicity Side effects Specific agent Phenytoin, valproate Barbiturates, benzodiazepines Respiratory depression 0, 37% of patients
Literature • Katzung, Masters, Trevor. Basic and clinical pharmacology. • A. D. A. M. pictures • Epilepsydiagnosis. org
 Domina petric
Domina petric Pseudomonopolar
Pseudomonopolar Inr check
Inr check Domina tasks
Domina tasks Domina petric
Domina petric Quasi vitamin b
Quasi vitamin b Domina petric
Domina petric Adrenal drugs pharmacology
Adrenal drugs pharmacology Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Basic & clinical pharmacology
Basic & clinical pharmacology Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Analglesia
Analglesia Clinical pharmacology
Clinical pharmacology Clinical pharmacology seminar
Clinical pharmacology seminar Clinical pharmacology residency
Clinical pharmacology residency Basic & clinical pharmacology
Basic & clinical pharmacology Clinical pharmacology seminar
Clinical pharmacology seminar Jure petric
Jure petric Lucija petric
Lucija petric Quimestres
Quimestres Casi indiretti
Casi indiretti Cada miembro domina una parcela determinada del proyecto
Cada miembro domina una parcela determinada del proyecto Carbonic anhydrase use
Carbonic anhydrase use 8 atitudes vencedoras
8 atitudes vencedoras Türkische domina
Türkische domina Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Hepatic extraction ratio
Hepatic extraction ratio Basic principles of pharmacology
Basic principles of pharmacology Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology Define pharmacology
Define pharmacology Ion trapping definition
Ion trapping definition Glomerular filtration
Glomerular filtration Define pharmacology
Define pharmacology Rationale meaning in pharmacology
Rationale meaning in pharmacology What is ion trapping in pharmacology
What is ion trapping in pharmacology Pharmacology newcastle
Pharmacology newcastle First pass effect
First pass effect Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals Potency vs efficacy
Potency vs efficacy Fundamentals of pharmacology for veterinary technicians
Fundamentals of pharmacology for veterinary technicians Pharmacology pay
Pharmacology pay What is pharmacology
What is pharmacology Ion trapping
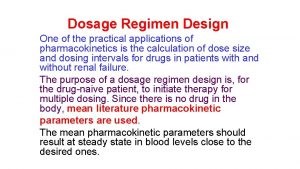
Ion trapping Loading dose
Loading dose What is ion trapping in pharmacology
What is ion trapping in pharmacology Concept of essential drugs
Concept of essential drugs