2019 Priority Setting and Resource Allocations Norfolk TGA

- Slides: 37
2019 Priority Setting and Resource Allocations
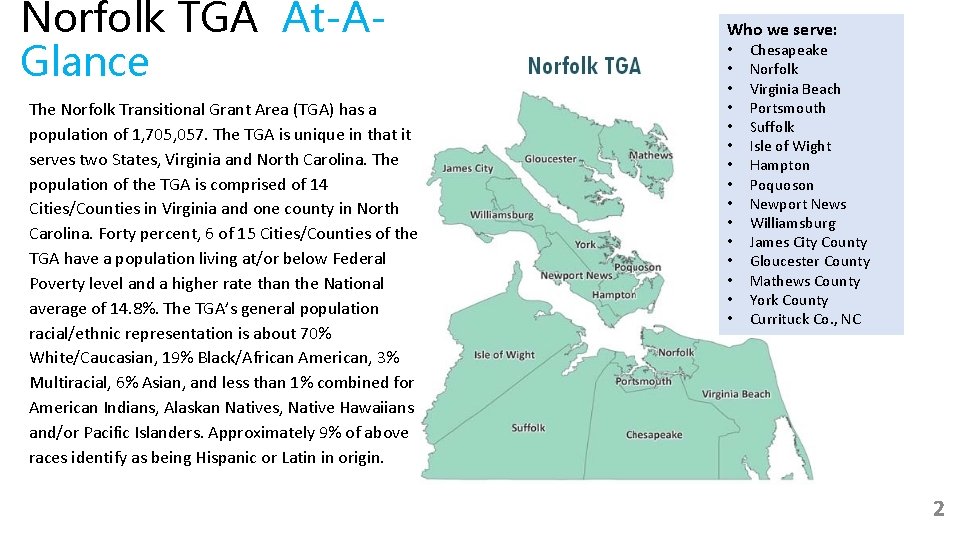
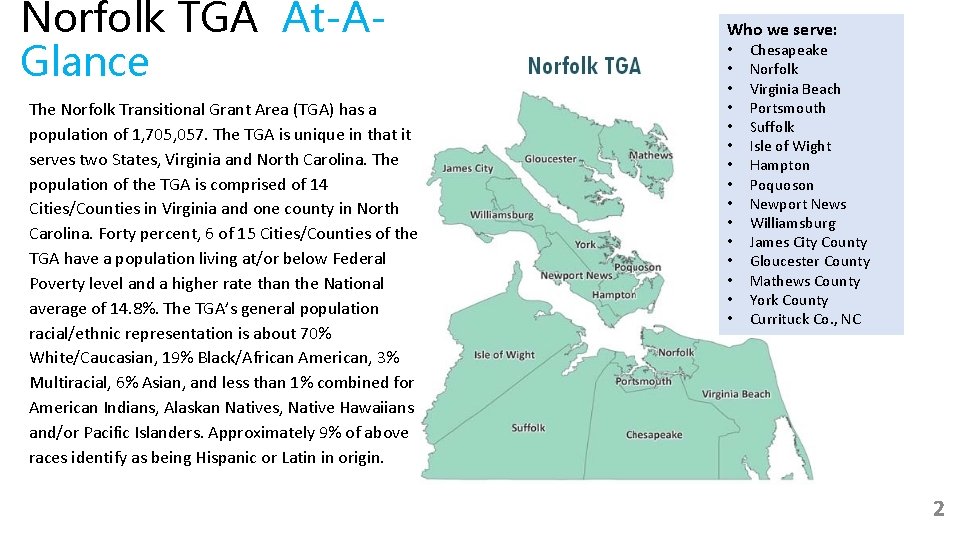
Norfolk TGA At-AGlance The Norfolk Transitional Grant Area (TGA) has a population of 1, 705, 057. The TGA is unique in that it serves two States, Virginia and North Carolina. The population of the TGA is comprised of 14 Cities/Counties in Virginia and one county in North Carolina. Forty percent, 6 of 15 Cities/Counties of the TGA have a population living at/or below Federal Poverty level and a higher rate than the National average of 14. 8%. The TGA’s general population racial/ethnic representation is about 70% White/Caucasian, 19% Black/African American, 3% Multiracial, 6% Asian, and less than 1% combined for American Indians, Alaskan Natives, Native Hawaiians and/or Pacific Islanders. Approximately 9% of above races identify as being Hispanic or Latin in origin. Who we serve: • • • • Chesapeake Norfolk Virginia Beach Portsmouth Suffolk Isle of Wight Hampton Poquoson Newport News Williamsburg James City County Gloucester County Mathews County York County Currituck Co. , NC 2
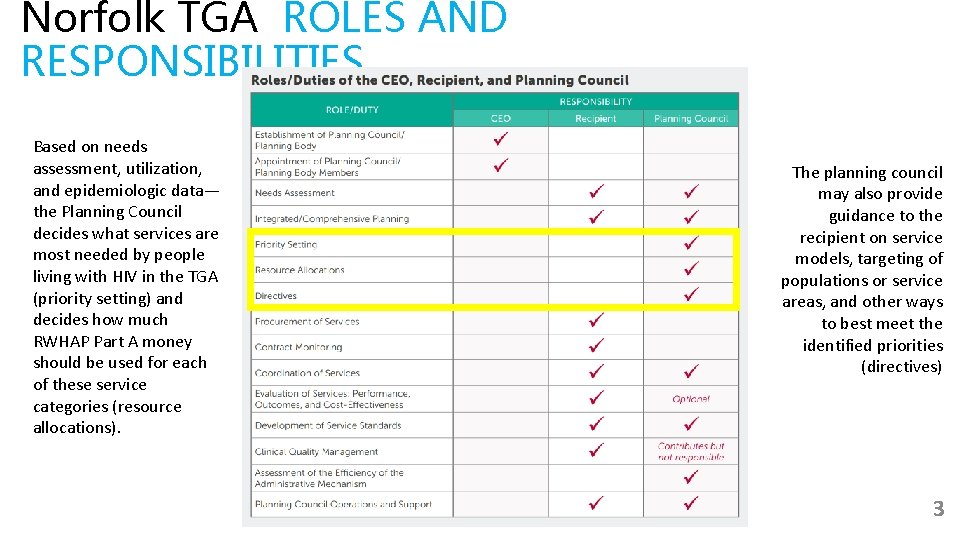
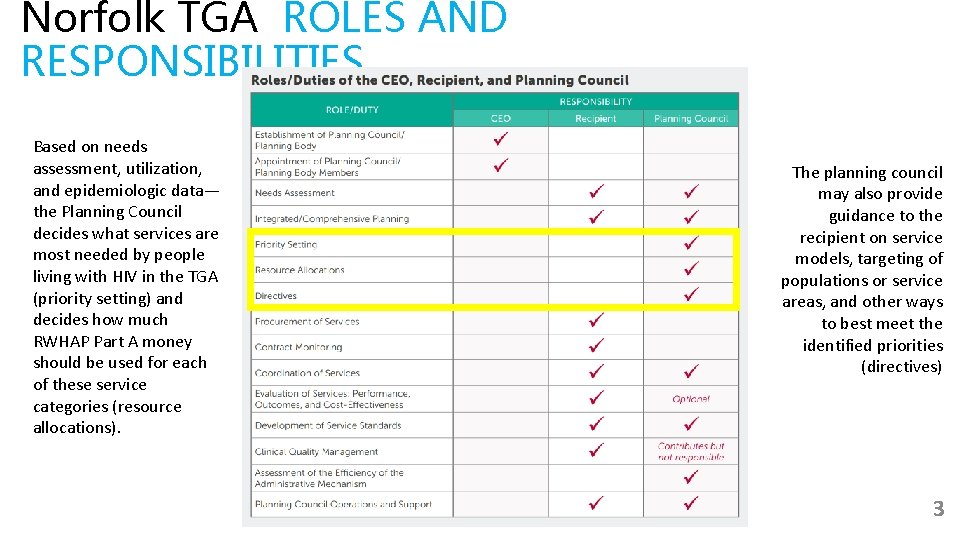
Norfolk TGA ROLES AND RESPONSIBILITIES Based on needs assessment, utilization, and epidemiologic data— the Planning Council decides what services are most needed by people living with HIV in the TGA (priority setting) and decides how much RWHAP Part A money should be used for each of these service categories (resource allocations). The planning council may also provide guidance to the recipient on service models, targeting of populations or service areas, and other ways to best meet the identified priorities (directives) 3
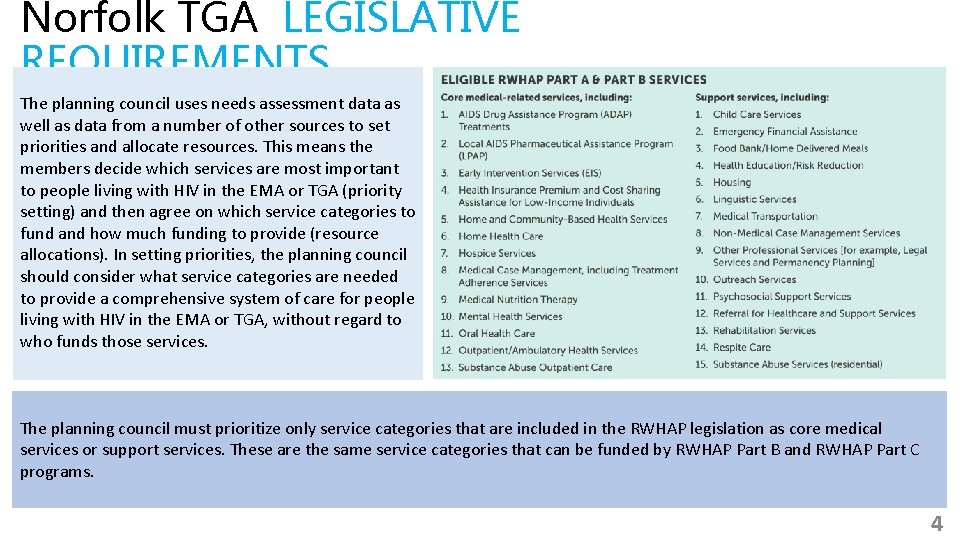
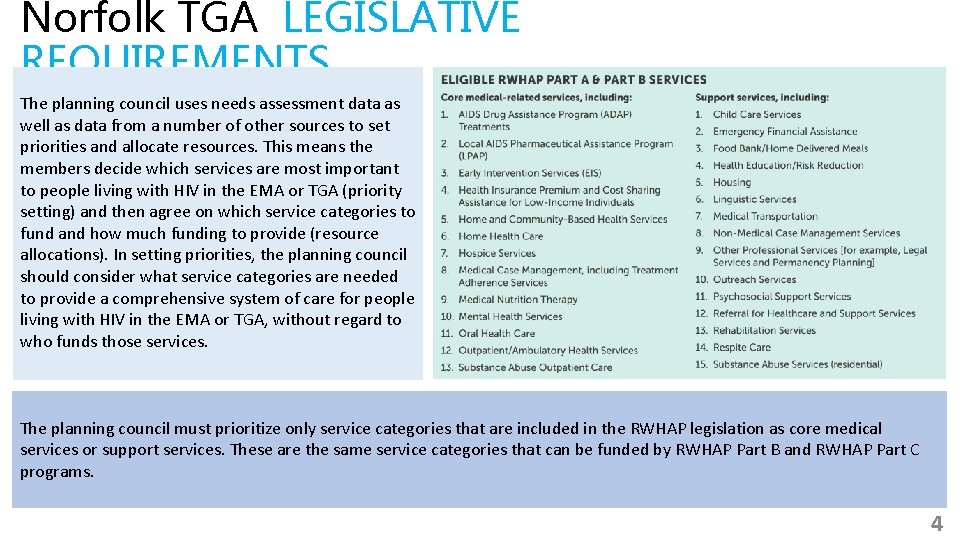
Norfolk TGA LEGISLATIVE REQUIREMENTS The planning council uses needs assessment data as well as data from a number of other sources to set priorities and allocate resources. This means the members decide which services are most important to people living with HIV in the EMA or TGA (priority setting) and then agree on which service categories to fund and how much funding to provide (resource allocations). In setting priorities, the planning council should consider what service categories are needed to provide a comprehensive system of care for people living with HIV in the EMA or TGA, without regard to who funds those services. The planning council must prioritize only service categories that are included in the RWHAP legislation as core medical services or support services. These are the same service categories that can be funded by RWHAP Part B and RWHAP Part C programs. 4
Norfolk TGA LEGISLATIVE REQUIREMENTS 75% Core 25% SUPP ORT After it sets priorities, the planning council must allocate resources, which means it decides how much RWHAP Part A funding will be used for each of these service priorities. For example, the planning council decides how much funding should go for outpatient/ ambulatory health services, mental health services, etc. In allocating resources, planning councils need to focus on the legislative requirement that at least 75 percent of funds must go to cover medical services and not more than 25 percent to support services, unless the EMA or TGA has obtained a waiver of this requirement. Support services must contribute to positive medical outcomes for clients. Typically, the planning council makes resource allocations using three scenarios that assume unchanged, increased, and decreased funding in the coming program year. The planning council makes decisions about priorities and resource allocations based on many factors, including: • Needs assessment findings; • Information about the most successful and economical ways of providing services; • Actual service cost and utilization data (provided by the recipient); • Priorities of people living with HIV who will use services ; • Use of RWHAP Part A funds to work well with other services like HIV prevention and substance abuse treatment services, and within the changing healthcare landscape; and • The amount of funds provided by other sources like Medicaid, Medicare, state and local government, and private funders— since RWHAP is the “payor of last resort” and should not pay for services that can be provided with other funding. 5
Norfolk TGA Notice of funding opportunity Funding Opportunity Number: HRSA-19 -033 Funding Opportunity Type(s): Competing Continuation Catalog of Federal Domestic Assistance (CFDA) Number: 93. 914 Application Due Date: September 21, 2018 B. Planning Responsibilities Section 2602(b)(4)(C) of the PHS Act requires PC/PBs to determine the priority for RWHAP allowable services and service allocations of RWHAP Part A funds every year. To fulfill this responsibility, EMA/TGA PC/PBs set service priorities and allocate RWHAP Part A funds based on the size, demographics, and needs of people living with or affected by HIV, with particular focus on individuals who know their HIV status but are not in care. The RWHAP Part A PC/PBs also are responsible for evaluating the efficiency of the recipient in distributing funds to service providers. PC/PBs analyze information to develop an in-depth understanding of the current HIV epidemic and its impact on the service area. PC/PBs review needs assessment data, HIV epidemiologic data, and co-occurring conditions data. The review includes service utilization data related to complexity of providing care, including service availability and unit cost per service, as well as service needs of emerging populations. The purpose of these data reviews is to guide decisions about HIV-related services and resources in the EMA/TGA. Furthermore, planning and implementation of the RWHAP Part A is driven by overall comprehensive planning and the recently developed Integrated HIV Prevention and Care Plan, including the Statewide Coordinated Statement of Need, CY 2017 - 2021 as a roadmap for relevant goals, objectives, and strategies for delivering RWHAP Part A services along the HIV continuum of care 6
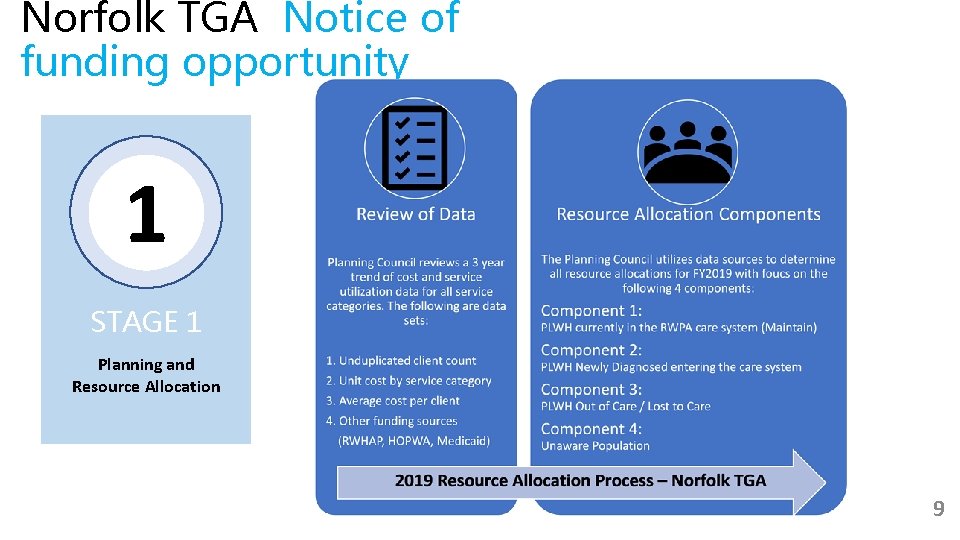
Norfolk TGA Notice of funding opportunity 1 STAGE 1 Planning and Resource Allocation The purpose of this section is to document the existence of a functioning planning process in the EMA/TGA that is consistent with RWHAP and HRSA program requirements. Such a planning process is imperative for effective local and state decision making to develop systems of prevention and care that are responsive to the needs of persons at risk for HIV infection and PLWH. Both HRSA and CDC support activities that facilitate collaboration and/or develop a joint planning body to address prevention and care. Community engagement is an essential component for planning comprehensive, effective HIV prevention and care programs in the United States. The composition of the PC/PB must reflect the demographics of the HIV epidemic in the EMA/TGA and be representative of various required categories of membership as cited in Sec. 2602(b)(1)-(2) of the PHS Act. PC/PB members must be trained regarding their legislatively mandated responsibilities and other competencies necessary for full participation in collaborative decision-making. PC/PBs are encouraged to educate members about service issues related to the prevention of domestic and sexual violence, opioid and other drug use, and trauma informed care as part of their ongoing training. PC/PBs should also consider recruiting members who are knowledgeable about these issues. 7
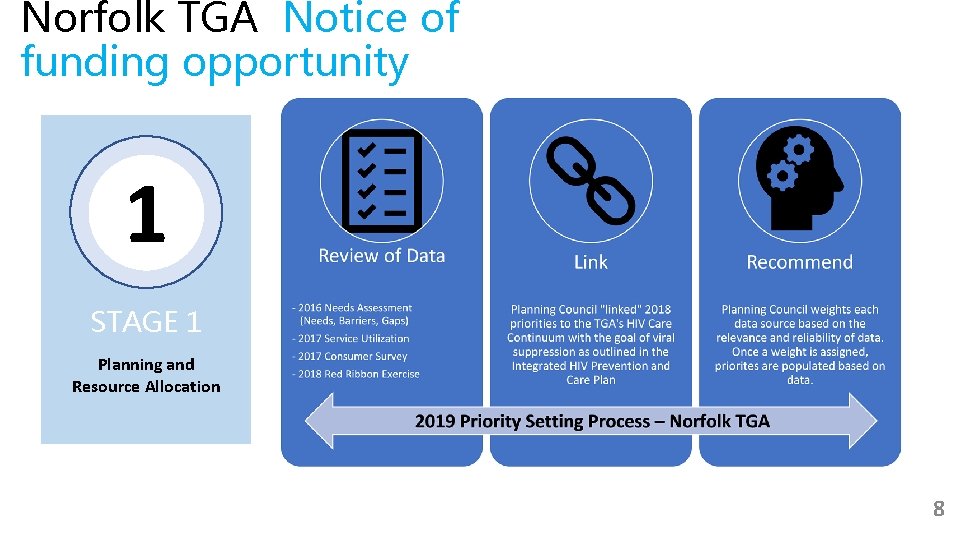
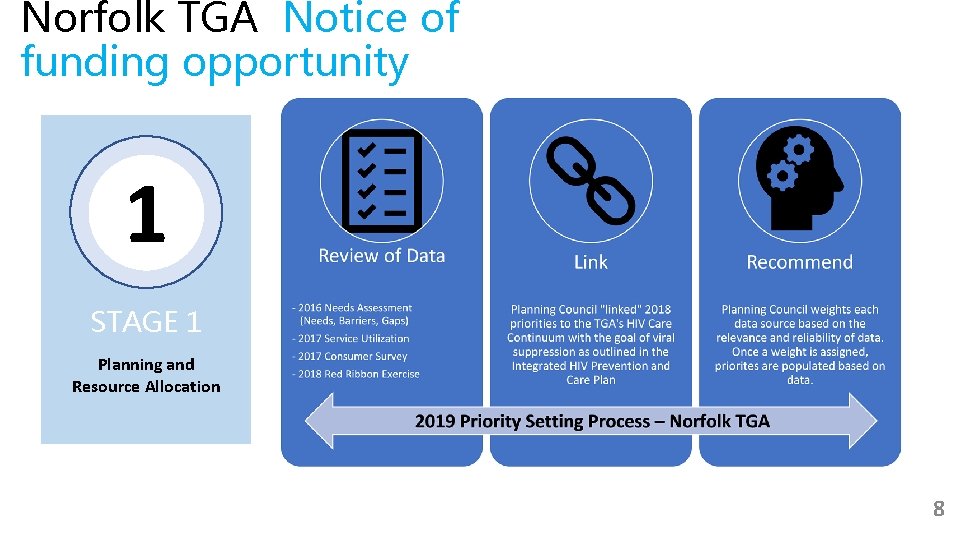
Norfolk TGA Notice of funding opportunity 1 STAGE 1 Planning and Resource Allocation 8
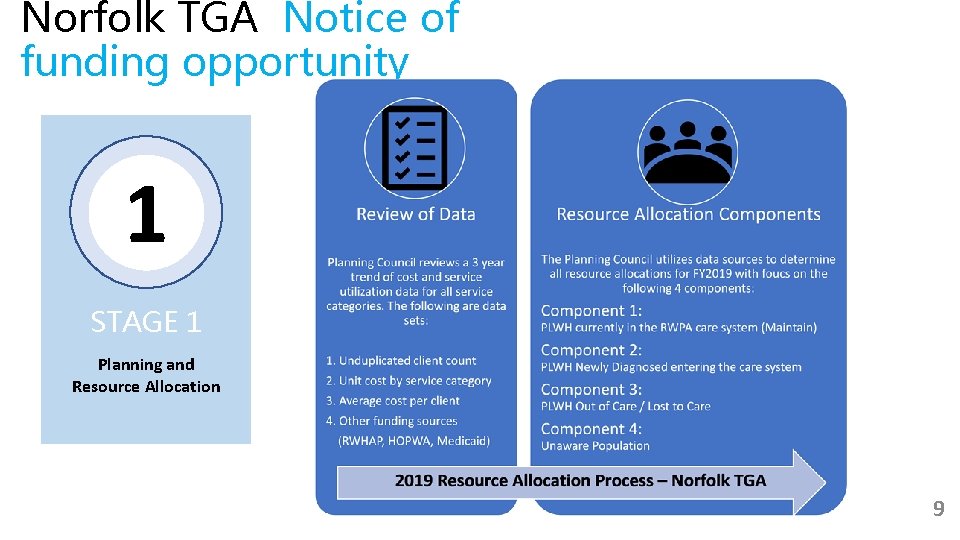
Norfolk TGA Notice of funding opportunity 1 STAGE 1 Planning and Resource Allocation 9
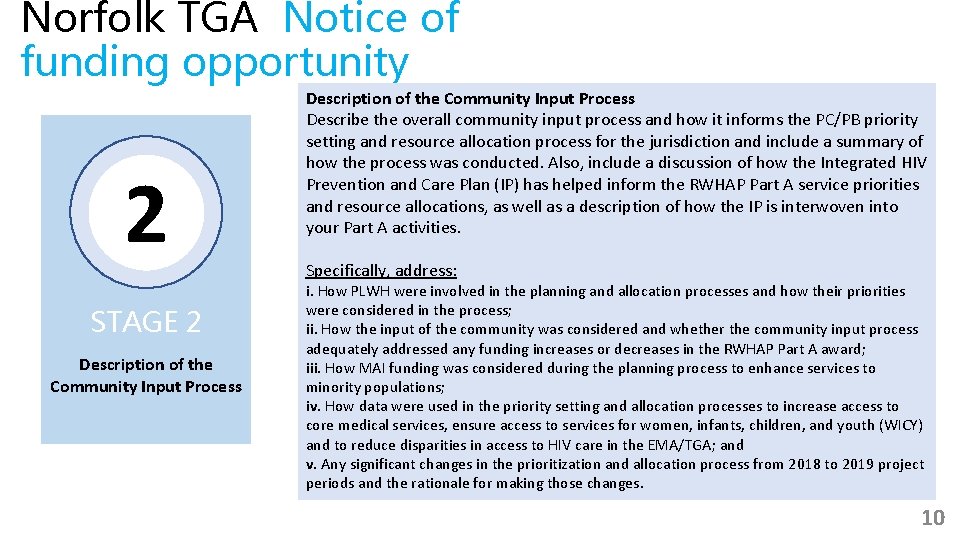
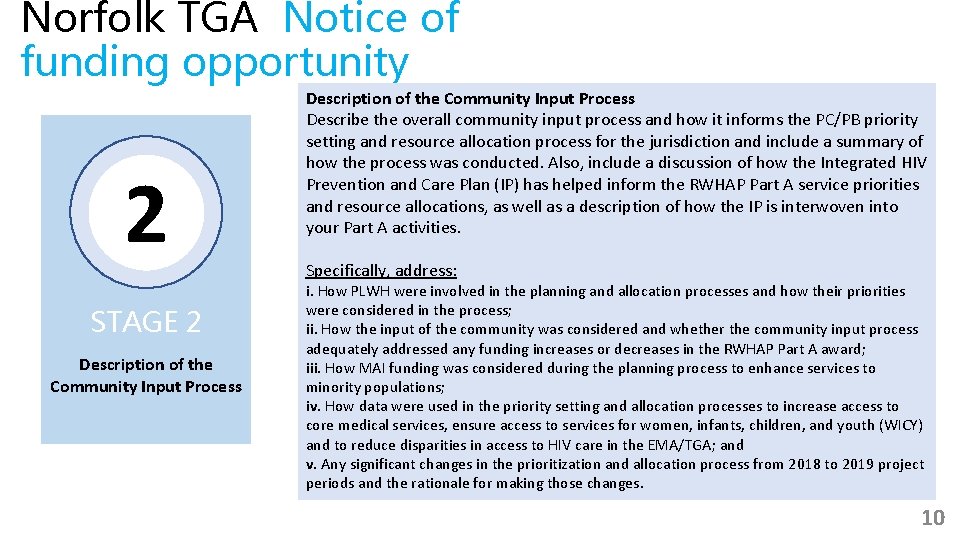
Norfolk TGA Notice of funding opportunity 2 STAGE 2 Description of the Community Input Process Describe the overall community input process and how it informs the PC/PB priority setting and resource allocation process for the jurisdiction and include a summary of how the process was conducted. Also, include a discussion of how the Integrated HIV Prevention and Care Plan (IP) has helped inform the RWHAP Part A service priorities and resource allocations, as well as a description of how the IP is interwoven into your Part A activities. Specifically, address: i. How PLWH were involved in the planning and allocation processes and how their priorities were considered in the process; ii. How the input of the community was considered and whether the community input process adequately addressed any funding increases or decreases in the RWHAP Part A award; iii. How MAI funding was considered during the planning process to enhance services to minority populations; iv. How data were used in the priority setting and allocation processes to increase access to core medical services, ensure access to services for women, infants, children, and youth (WICY) and to reduce disparities in access to HIV care in the EMA/TGA; and v. Any significant changes in the prioritization and allocation process from 2018 to 2019 project periods and the rationale for making those changes. 10
Norfolk TGA Notice of funding opportunity 2 STAGE 2 Description of the Community Input Process 11

REVIEW OF DATA
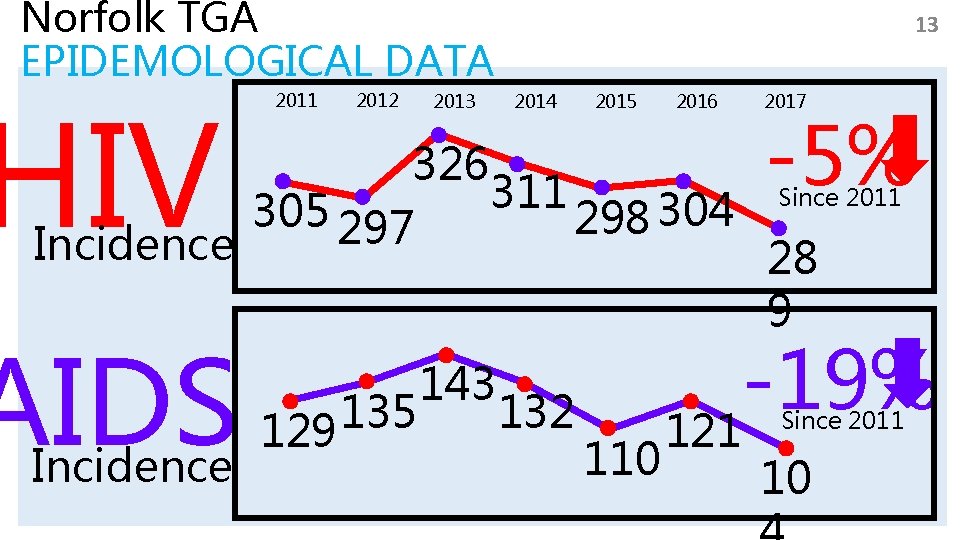
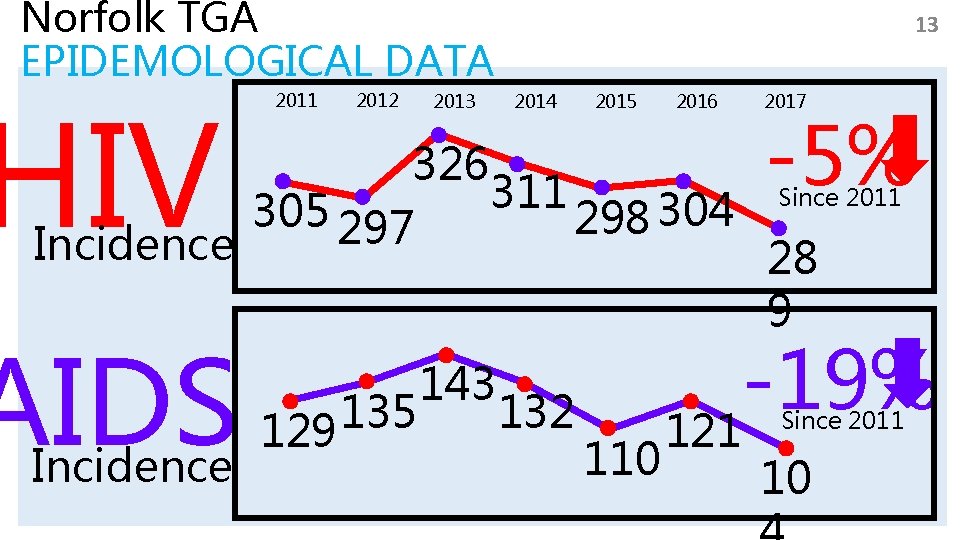
Norfolk TGA EPIDEMOLOGICAL DATA HIV 2011 2012 2013 13 2014 2015 2016 2017 -5% 326 Since 2011 305 297 298 304 Incidence 28 9 AIDS Incidence 135 129 143 132 110 -19% 121 Since 2011 10
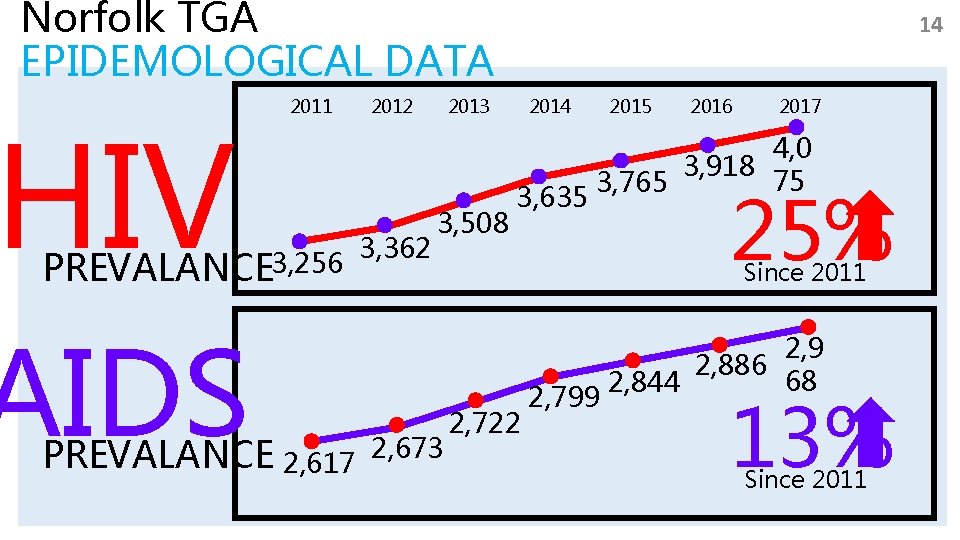
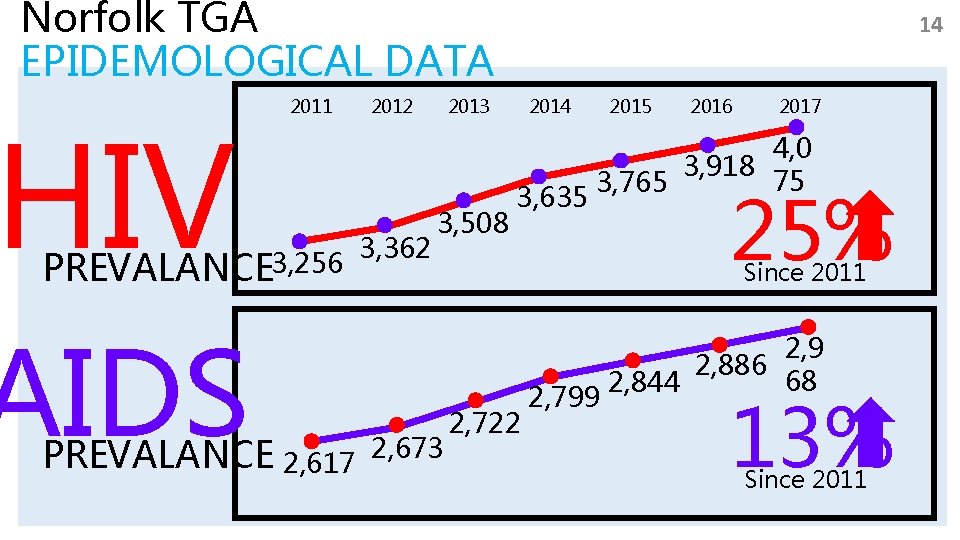
Norfolk TGA EPIDEMOLOGICAL DATA HIV 2011 PREVALANCE 3, 256 AIDS PREVALANCE 2, 617 2012 3, 362 14 2013 3, 508 2, 673 2015 2014 3, 635 2016 2017 4, 0 3, 918 75 3, 765 25% Since 2011 2, 722 2, 799 2, 886 68 2, 844 13% Since 2011
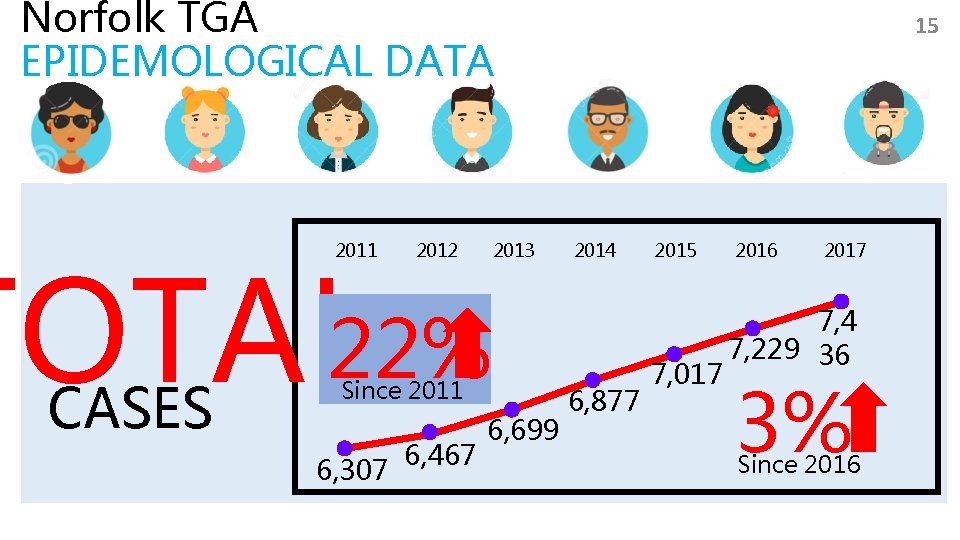
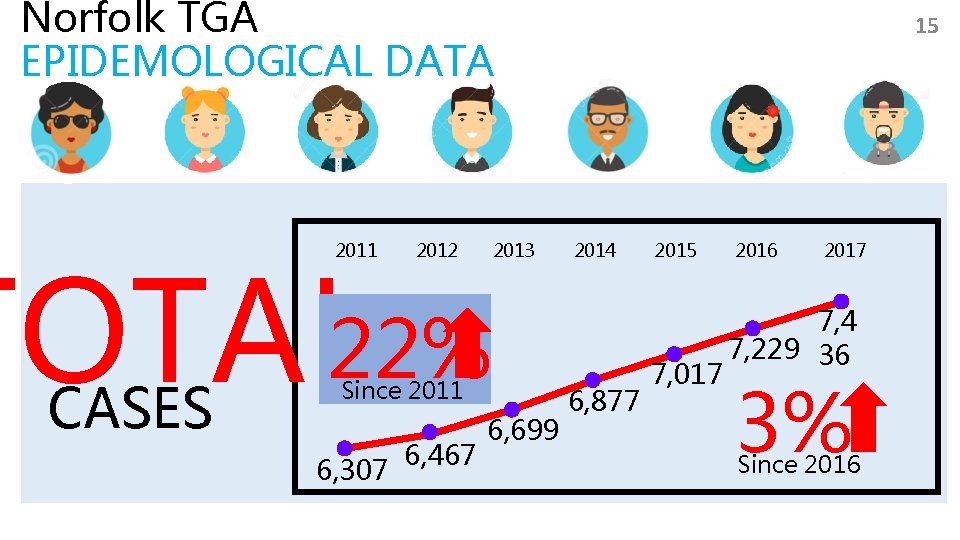
Norfolk TGA EPIDEMOLOGICAL DATA TOTAL 22% 2011 CASES 2012 2013 Since 2011 6, 307 6, 467 6, 699 15 2014 6, 877 2015 7, 017 2016 2017 7, 4 7, 229 36 3% Since 2016
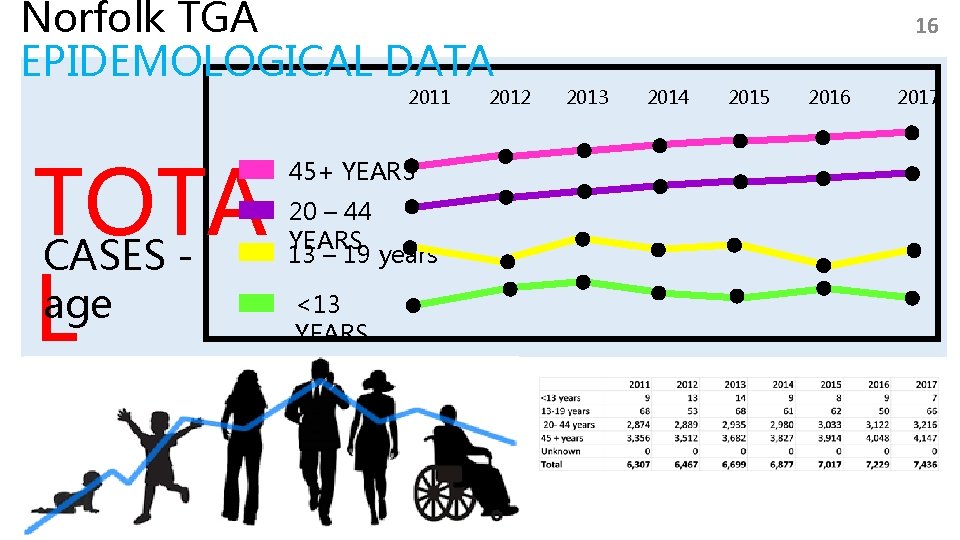
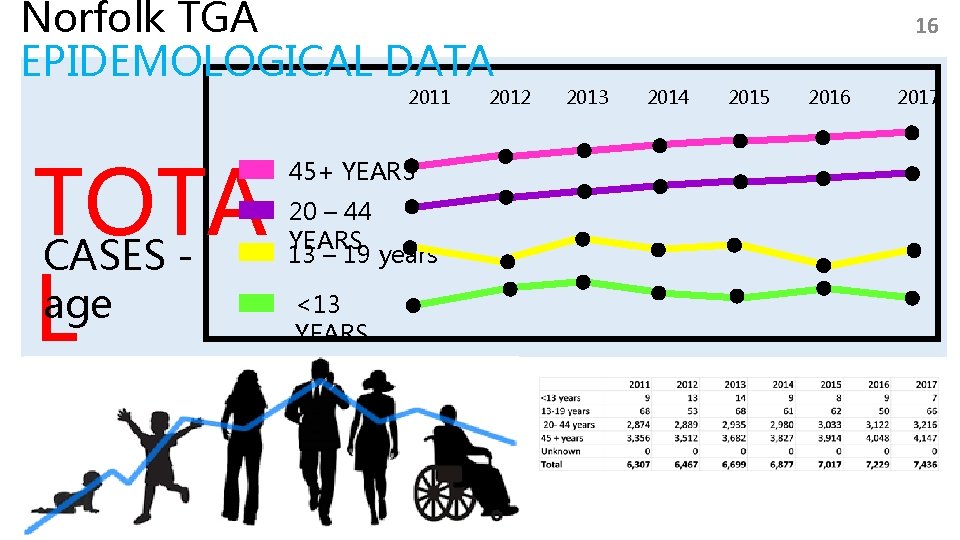
Norfolk TGA EPIDEMOLOGICAL DATA 2011 TOTA CASES age L 45+ YEARS 20 – 44 YEARS 13 – 19 years <13 YEARS 2012 16 2013 2014 2015 2016 2017
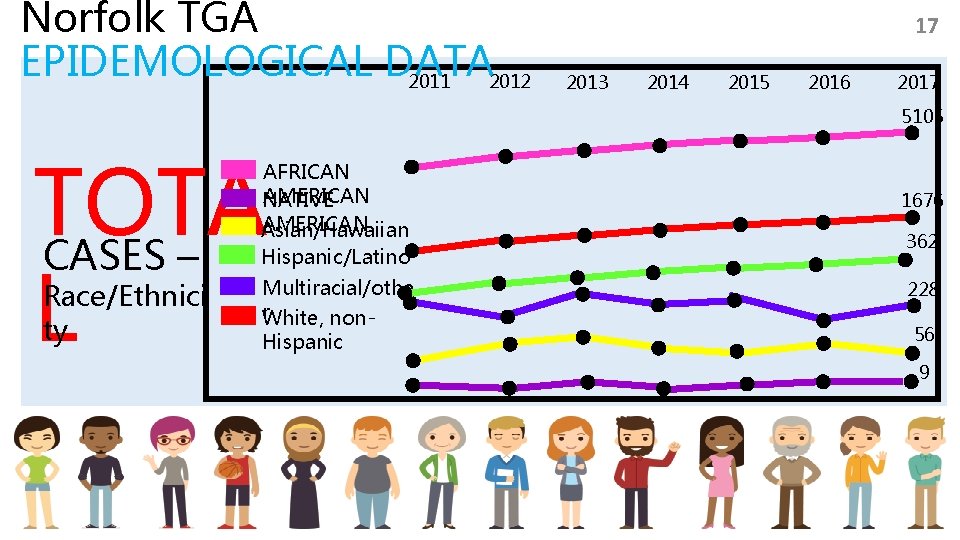
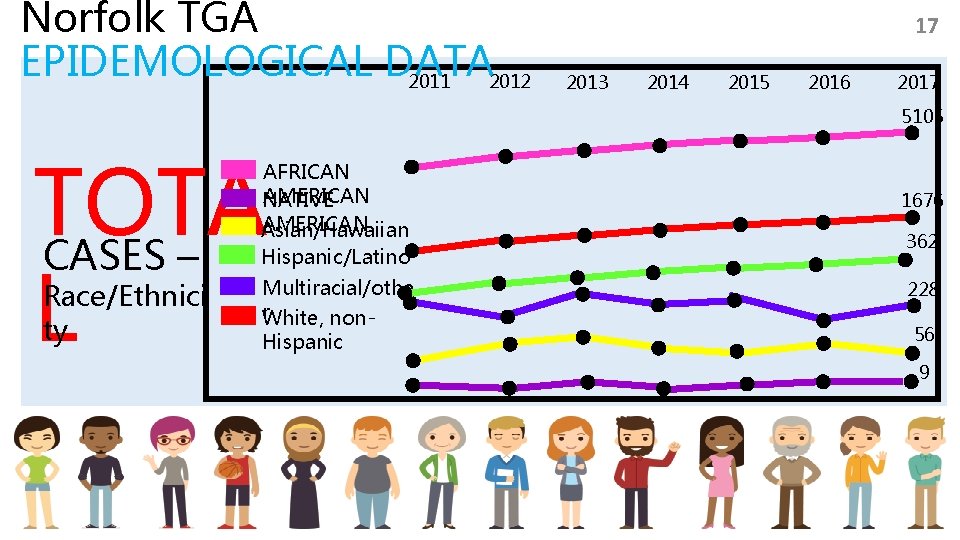
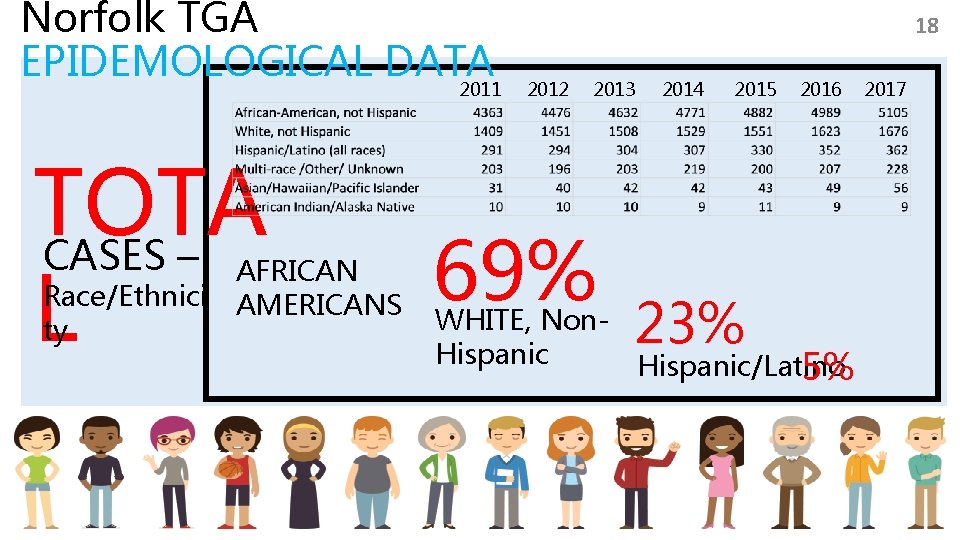
Norfolk TGA EPIDEMOLOGICAL DATA 2011 2012 17 2013 2014 2015 2016 2017 5105 TOTA CASES – L AFRICAN AMERICAN NATIVE AMERICAN Asian/Hawaiian Hispanic/Latino Race/Ethnici ty Multiracial/othe r. White, non. Hispanic 1676 362 228 56 9
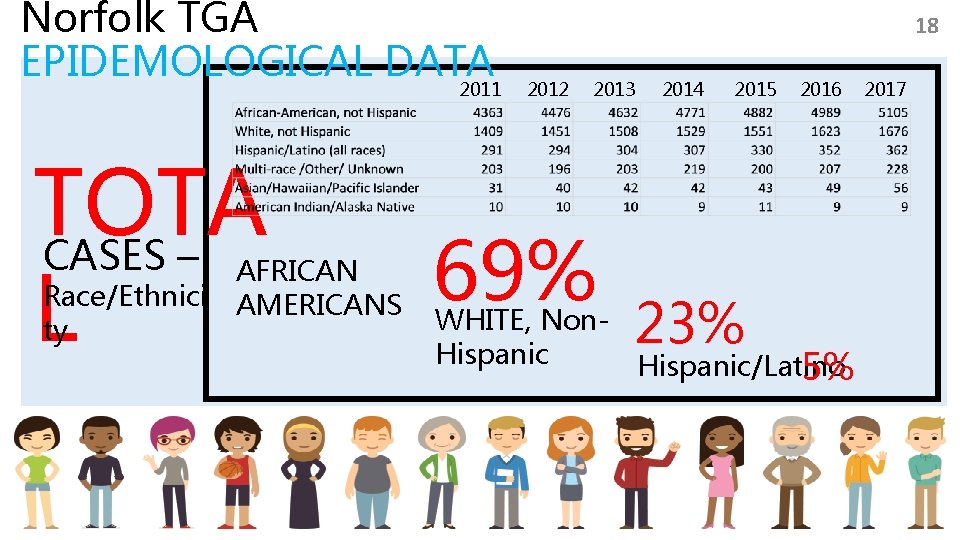
Norfolk TGA EPIDEMOLOGICAL DATA 2011 TOTA CASES – L Race/Ethnici ty AFRICAN AMERICANS 18 2012 2013 69% 2014 2015 23% 2016 WHITE, Non. Hispanic/Latino 5% 2017
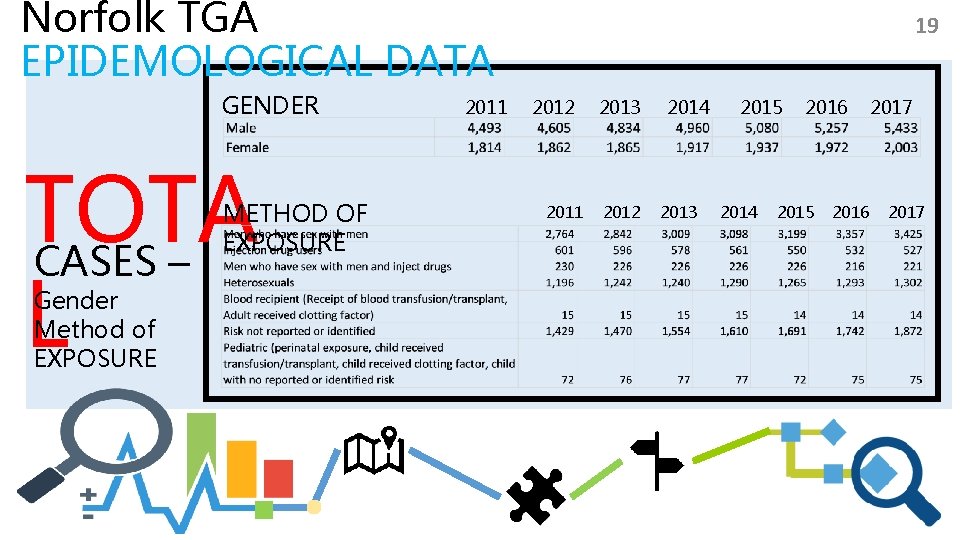
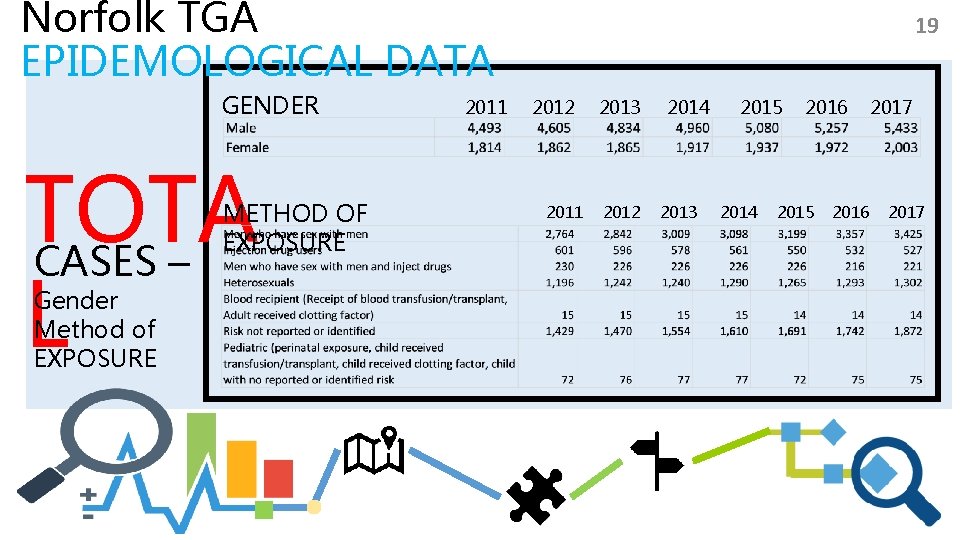
Norfolk TGA EPIDEMOLOGICAL DATA GENDER TOTA CASES – L METHOD OF EXPOSURE Gender Method of EXPOSURE 2011 19 2012 2011 2013 2012 2014 2013 2015 2014 2016 2015 2016 2017
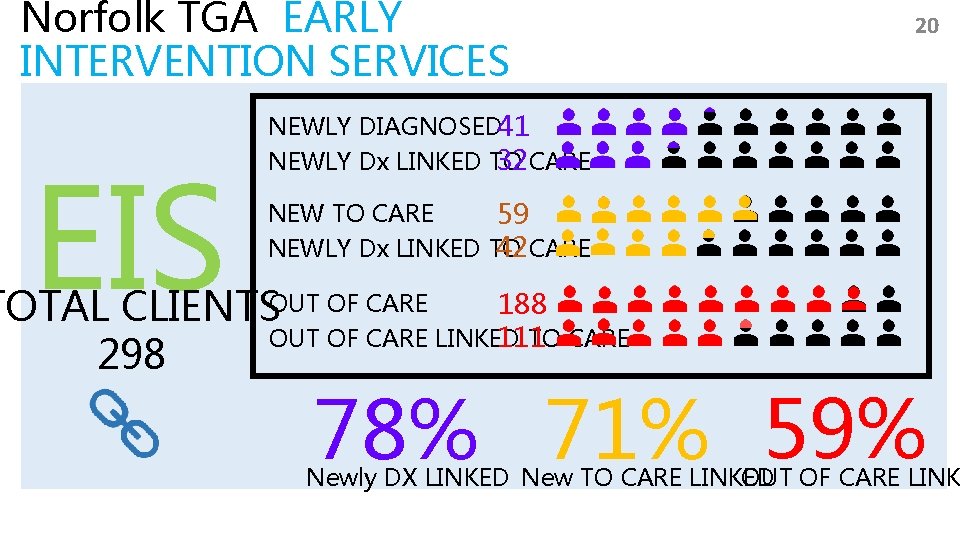
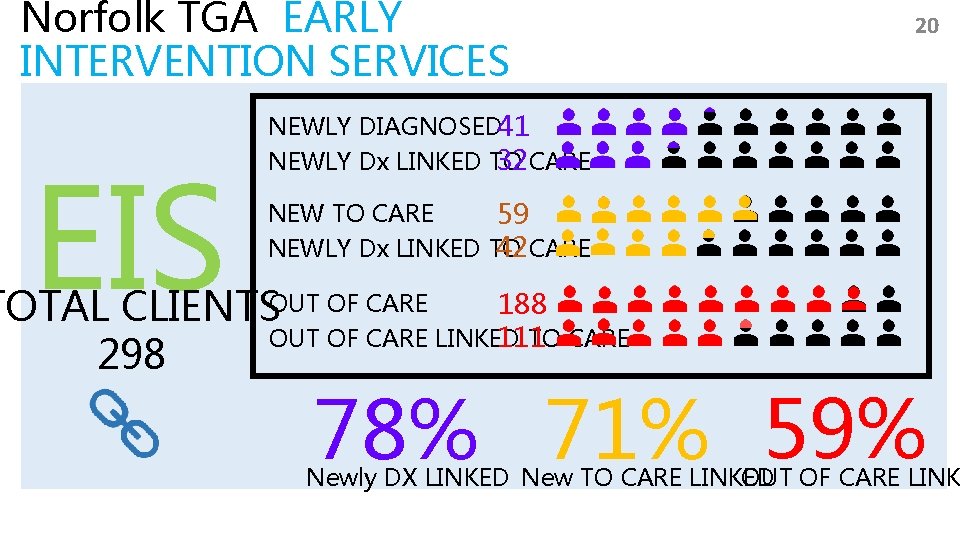
Norfolk TGA EARLY INTERVENTION SERVICES EIS 20 NEWLY DIAGNOSED 41 NEWLY Dx LINKED TO 32 CARE NEW TO CARE 59 NEWLY Dx LINKED TO 42 CARE 188 TOTAL CLIENTSOUT OF CARE LINKED TO CARE 111 298 78% 71% 59% OUT OF CARE LINK Newly DX LINKED New TO CARE LINKED
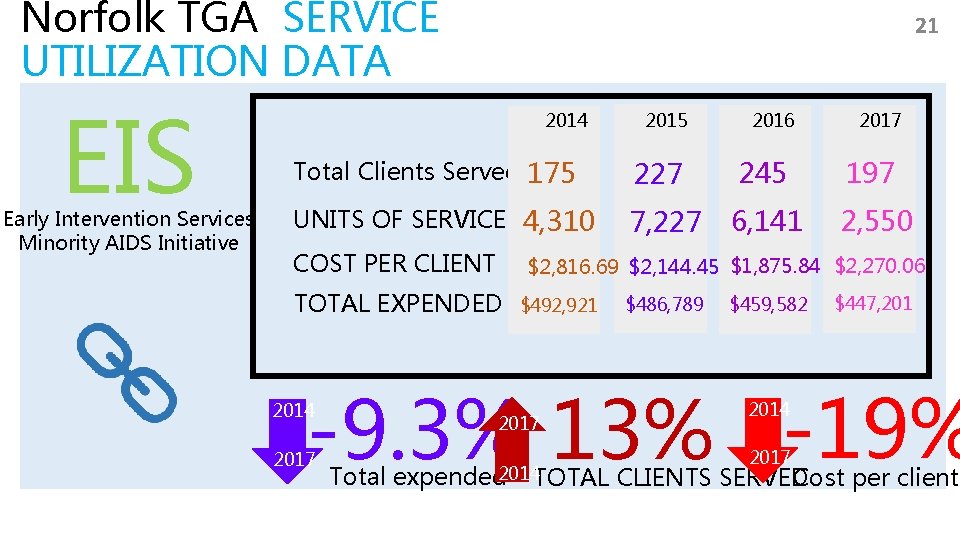
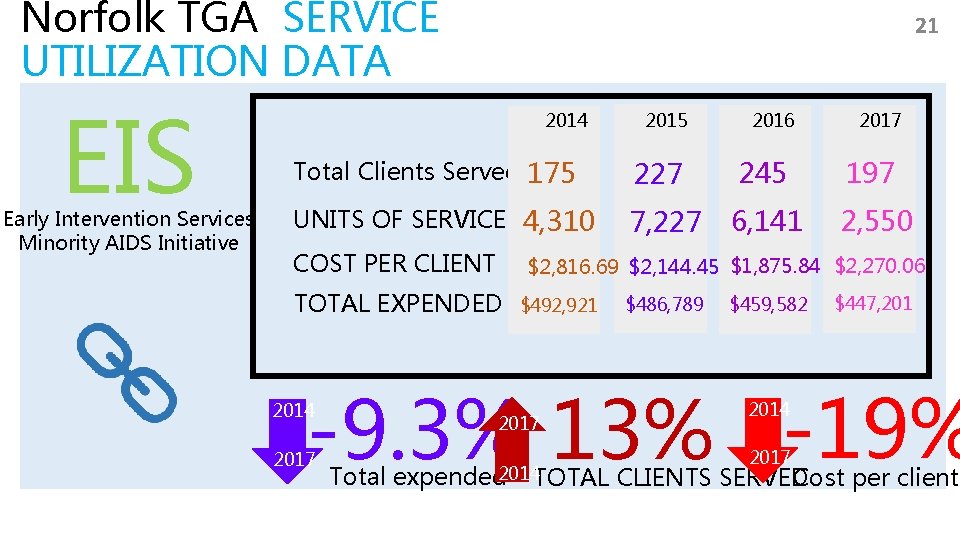
Norfolk TGA SERVICE UTILIZATION DATA EIS Early Intervention Services Minority AIDS Initiative 21 2014 2015 2016 2017 Total Clients Served 175 227 245 197 UNITS OF SERVICE 4, 310 7, 227 6, 141 2, 550 COST PER CLIENT $2, 816. 69 $2, 144. 45 $1, 875. 84 $2, 270. 06 TOTAL EXPENDED $492, 921 $486, 789 $459, 582 $447, 201 -9. 3% 13% -19% 2014 2017 Total expended 2014 TOTAL 2014 2017 Cost per client CLIENTS SERVED
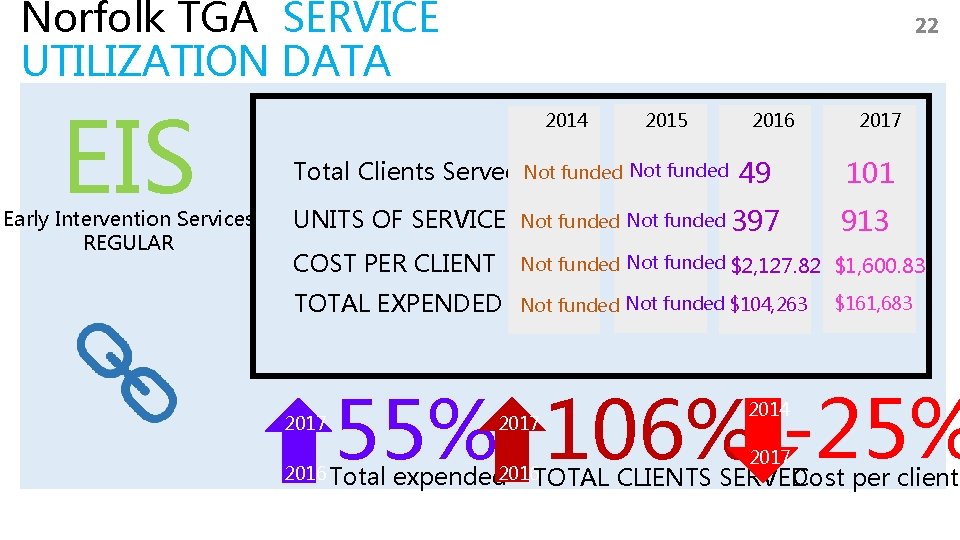
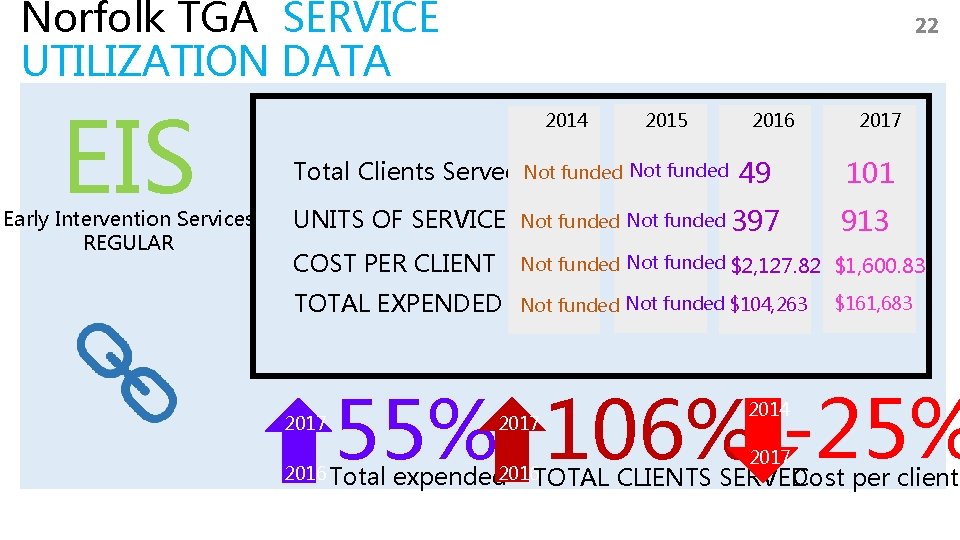
Norfolk TGA SERVICE UTILIZATION DATA EIS Early Intervention Services REGULAR 22 2014 2015 2016 Total Clients Served Not funded 49 2017 101 UNITS OF SERVICE Not funded 397 COST PER CLIENT Not funded $2, 127. 82 $1, 600. 83 TOTAL EXPENDED Not funded $104, 263 2017 913 $161, 683 55% 106% -25% 2016 Total 2017 expended 2016 TOTAL 2014 2017 Cost per client CLIENTS SERVED
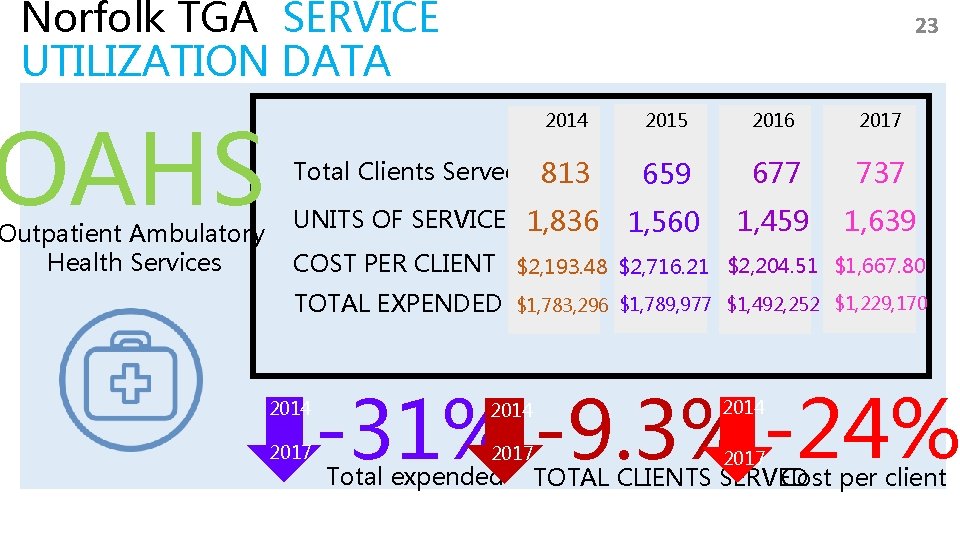
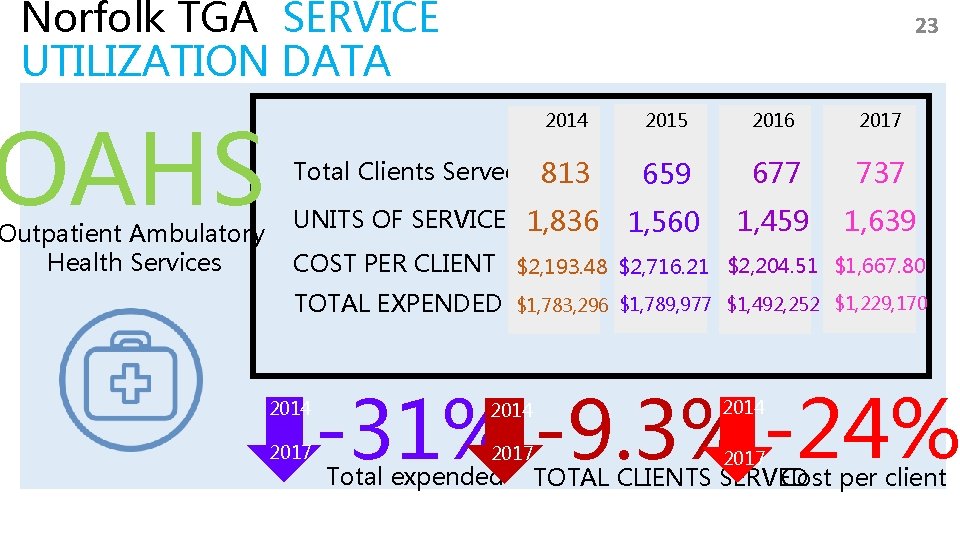
Norfolk TGA SERVICE UTILIZATION DATA OAHS Outpatient Ambulatory Health Services 23 2014 2015 2016 2017 Total Clients Served 813 659 677 737 UNITS OF SERVICE 1, 836 1, 560 1, 459 1, 639 COST PER CLIENT $2, 193. 48 $2, 716. 21 $2, 204. 51 $1, 667. 80 TOTAL EXPENDED 2014 2017 $1, 783, 296 $1, 789, 977 $1, 492, 252 $1, 229, 170 -31% -9. 3% -24% 2014 2017 Total expended Cost per client TOTAL CLIENTS SERVED
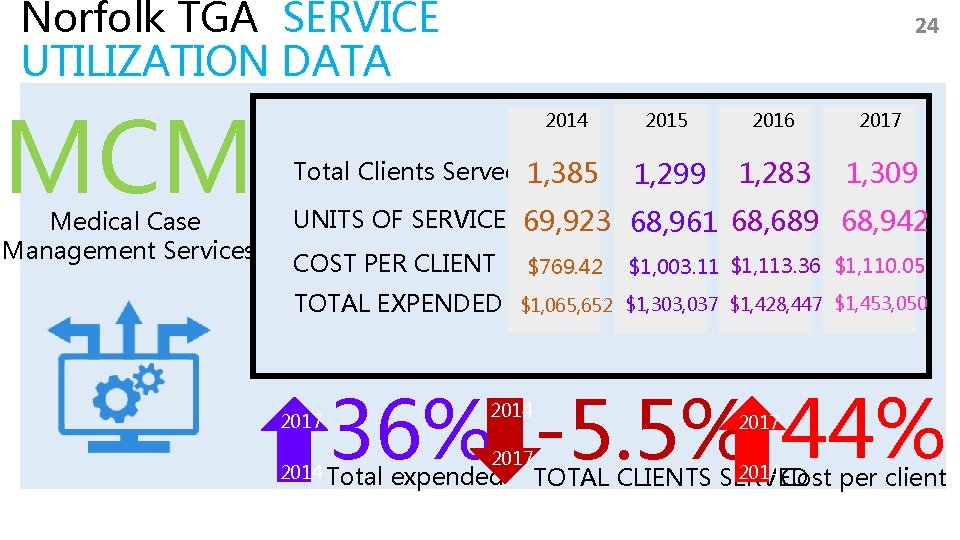
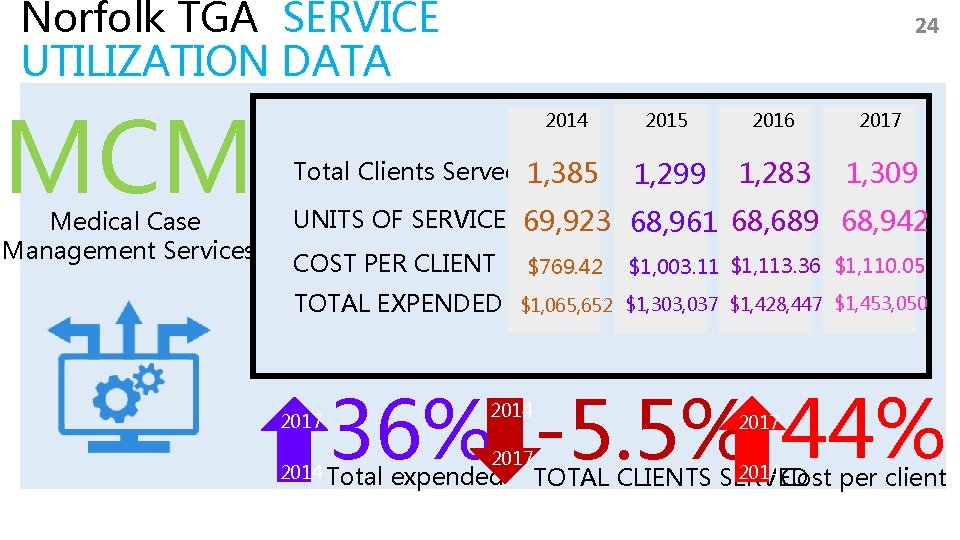
Norfolk TGA SERVICE UTILIZATION DATA MCM Medical Case Management Services 24 2014 Total Clients Served 1, 385 2016 2017 1, 299 1, 283 1, 309 UNITS OF SERVICE 69, 923 68, 961 68, 689 68, 942 COST PER CLIENT TOTAL EXPENDED 2017 $769. 42 $1, 003. 11 $1, 113. 36 $1, 110. 05 $1, 065, 652 $1, 303, 037 $1, 428, 447 $1, 453, 050 36% -5. 5% 44% 2014 Total 2014 2017 expended 2017 2014 Cost per client TOTAL CLIENTS SERVED
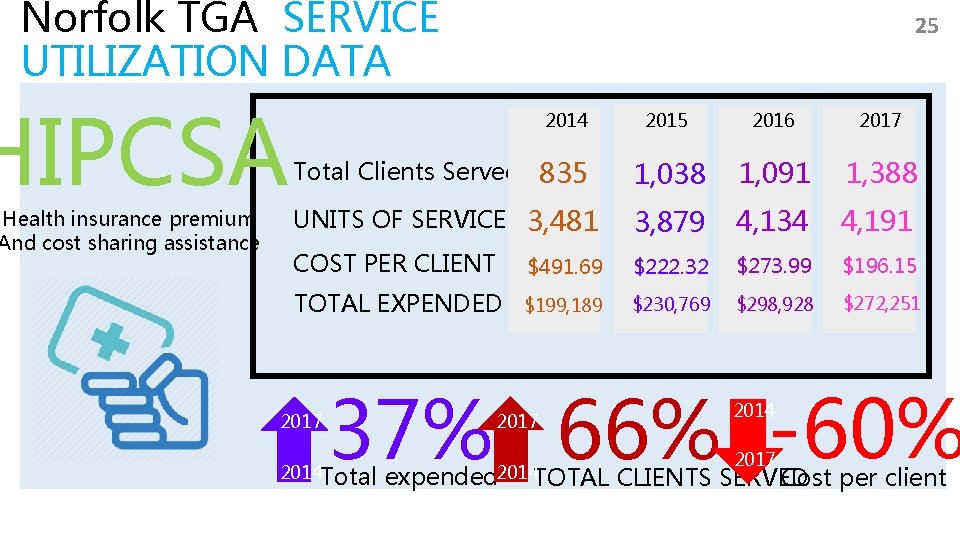
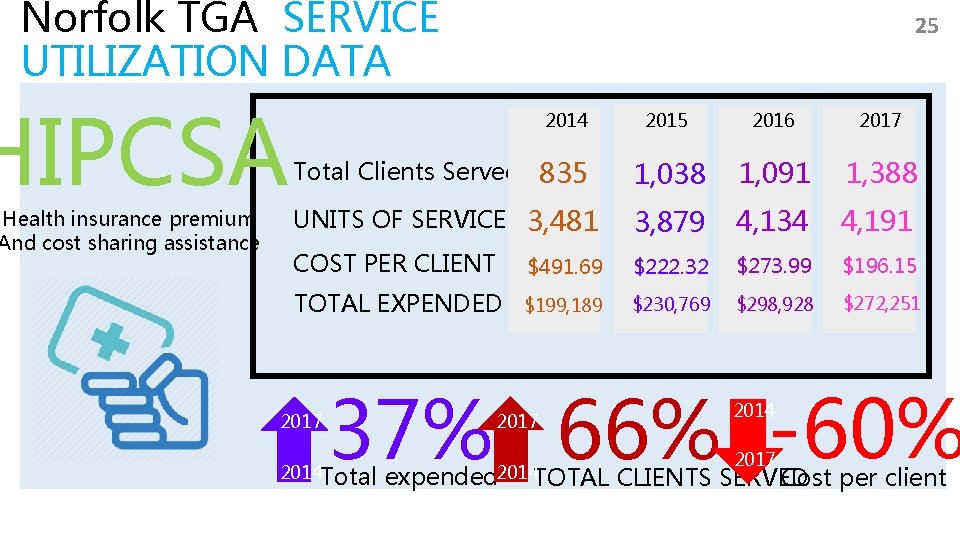
Norfolk TGA SERVICE UTILIZATION DATA HIPCSA Health insurance premium And cost sharing assistance 25 2014 2015 2016 2017 Total Clients Served 835 1, 038 1, 091 1, 388 UNITS OF SERVICE 3, 481 3, 879 4, 134 4, 191 COST PER CLIENT $491. 69 $222. 32 $273. 99 $196. 15 TOTAL EXPENDED $199, 189 $230, 769 $298, 928 $272, 251 2017 37% 66% -60% 2014 Total 2017 expended 2014 TOTAL 2014 2017 Cost per client CLIENTS SERVED
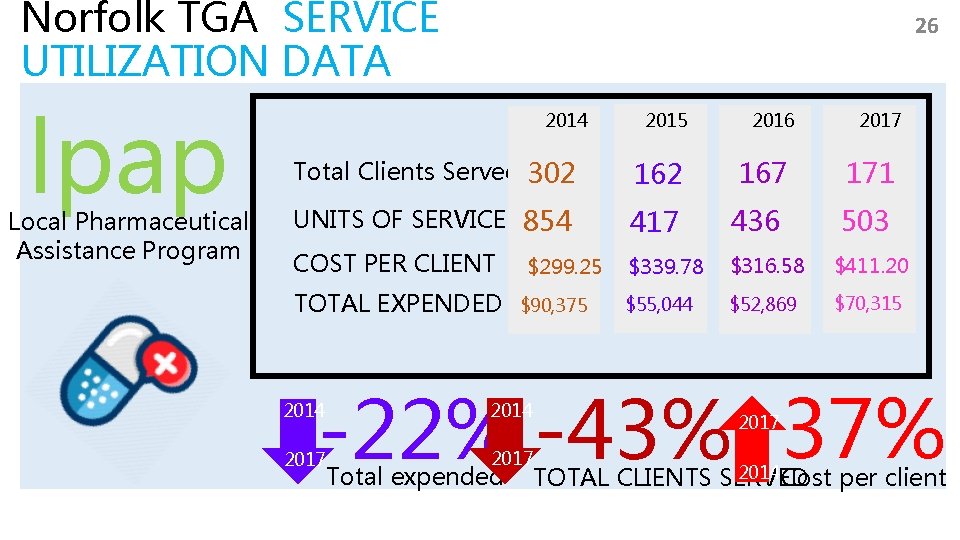
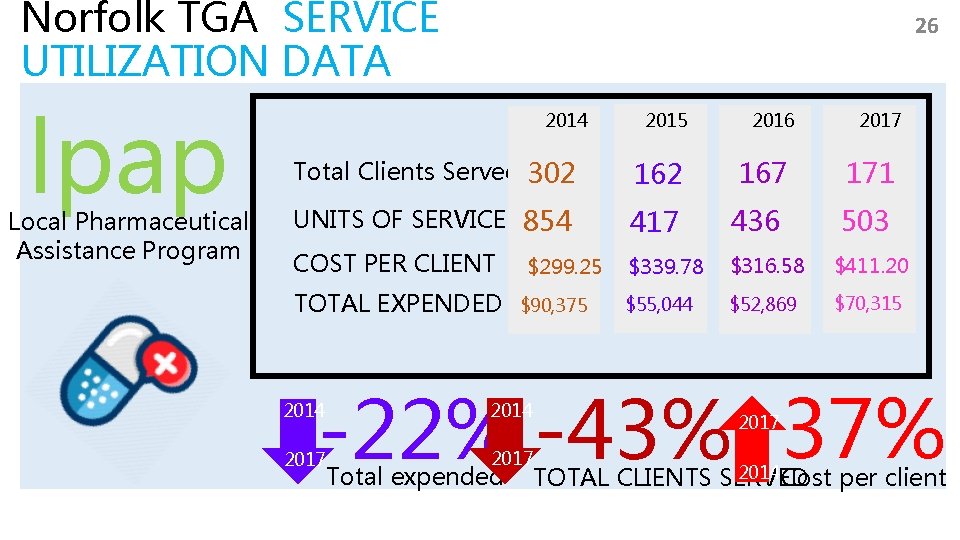
Norfolk TGA SERVICE UTILIZATION DATA lpap Local Pharmaceutical Assistance Program 26 2014 2015 2016 2017 Total Clients Served 302 167 171 UNITS OF SERVICE 854 417 436 503 COST PER CLIENT $339. 78 $316. 58 $411. 20 $55, 044 $52, 869 $70, 315 TOTAL EXPENDED $299. 25 $90, 375 -22% -43% 37% 2014 2017 Total expended 2017 2014 Cost per client TOTAL CLIENTS SERVED
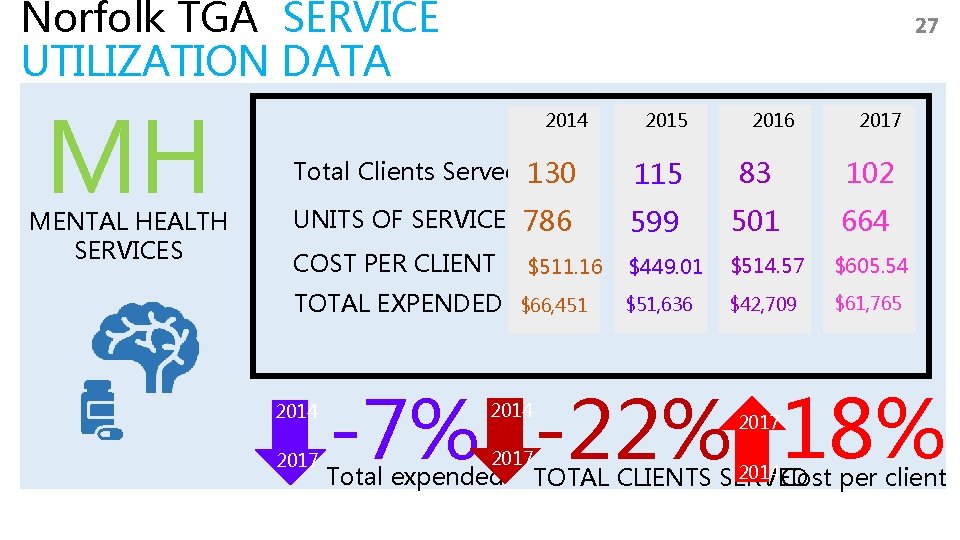
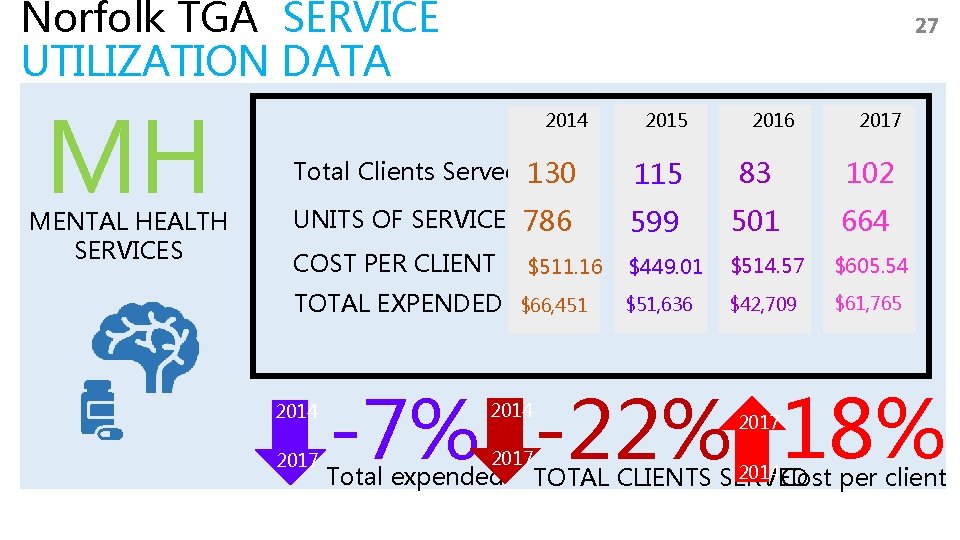
Norfolk TGA SERVICE UTILIZATION DATA MH MENTAL HEALTH SERVICES 27 2014 2015 2016 2017 Total Clients Served 130 115 83 102 UNITS OF SERVICE 786 599 501 664 COST PER CLIENT $449. 01 $514. 57 $605. 54 $51, 636 $42, 709 $61, 765 TOTAL EXPENDED 2014 2017 $511. 16 $66, 451 -7% -22% 18% 2014 2017 Total expended 2017 2014 Cost per client TOTAL CLIENTS SERVED
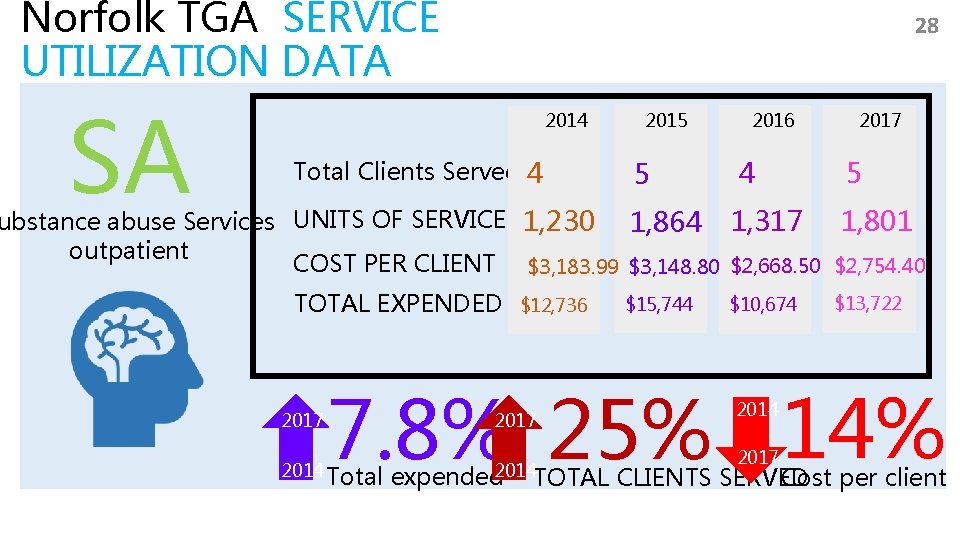
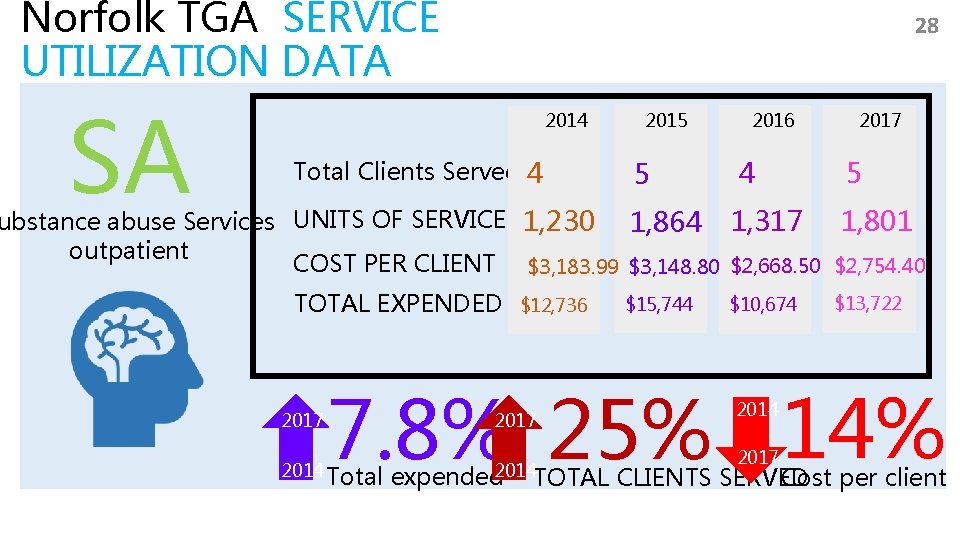
Norfolk TGA SERVICE UTILIZATION DATA SA 28 2014 Total Clients Served 4 2015 5 2016 4 2017 5 ubstance abuse Services UNITS OF SERVICE 1, 230 1, 864 1, 317 1, 801 outpatient COST PER CLIENT $3, 183. 99 $3, 148. 80 $2, 668. 50 $2, 754. 40 TOTAL EXPENDED 2017 $12, 736 $15, 744 $10, 674 $13, 722 7. 8% 25% 14% 2014 Total 2017 expended 2014 TOTAL 2014 2017 Cost per client CLIENTS SERVED
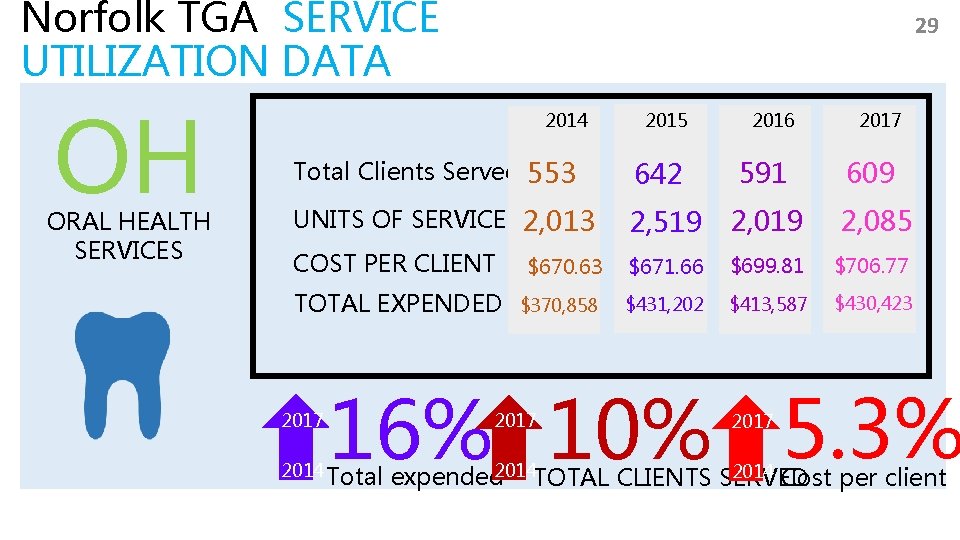
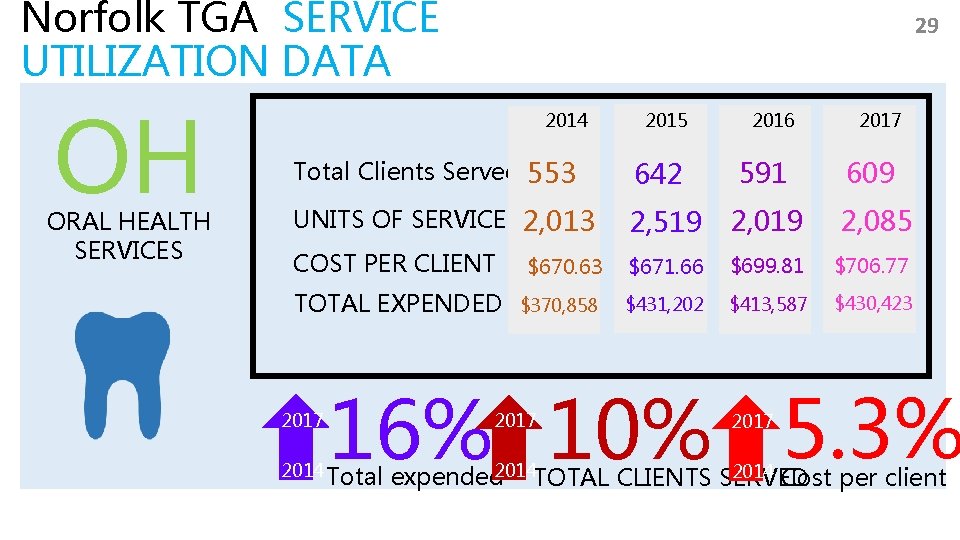
Norfolk TGA SERVICE UTILIZATION DATA OH ORAL HEALTH SERVICES 29 2014 2015 2016 2017 Total Clients Served 553 642 591 609 UNITS OF SERVICE 2, 013 2, 519 2, 085 COST PER CLIENT $670. 63 $671. 66 $699. 81 $706. 77 $370, 858 $431, 202 $413, 587 $430, 423 TOTAL EXPENDED 2017 16% 10% 5. 3% 2014 Total 2017 2014 Cost per client expended 2014 TOTAL CLIENTS SERVED
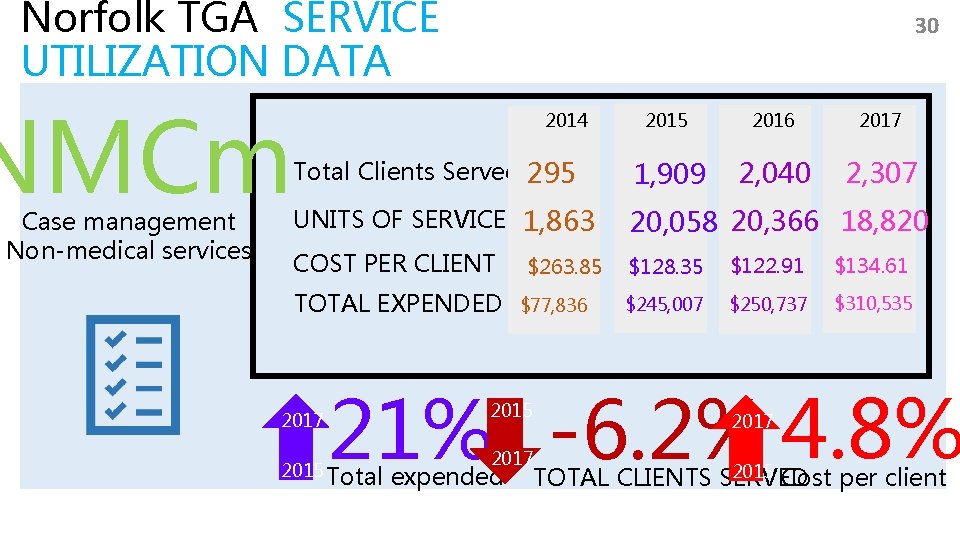
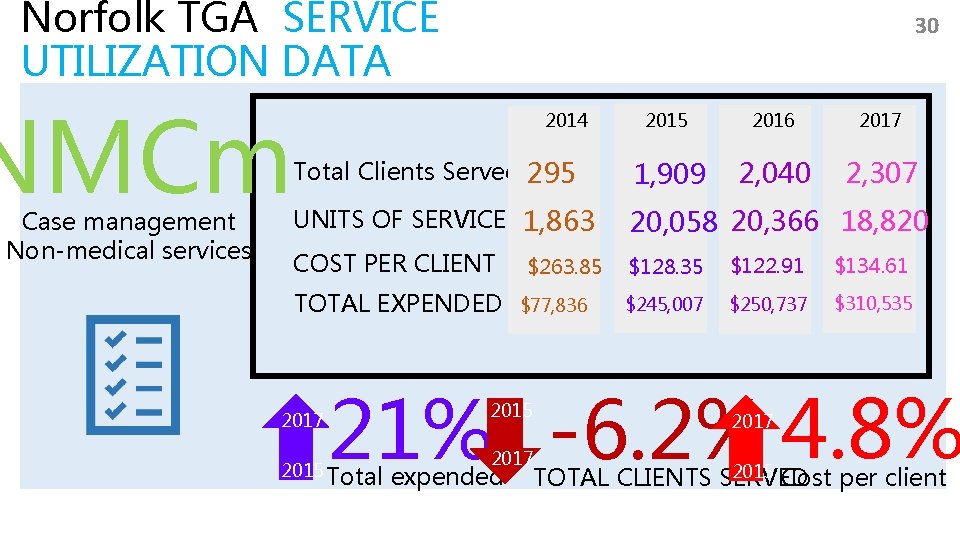
Norfolk TGA SERVICE UTILIZATION DATA NMCm Case management Non-medical services 30 2014 2015 2016 2017 Total Clients Served 295 1, 909 2, 040 2, 307 UNITS OF SERVICE 1, 863 20, 058 20, 366 18, 820 COST PER CLIENT $128. 35 $122. 91 $134. 61 $245, 007 $250, 737 $310, 535 TOTAL EXPENDED 2017 $263. 85 $77, 836 21% -6. 2% 4. 8% 2015 Total 2015 2017 expended 2017 2015 Cost per client TOTAL CLIENTS SERVED
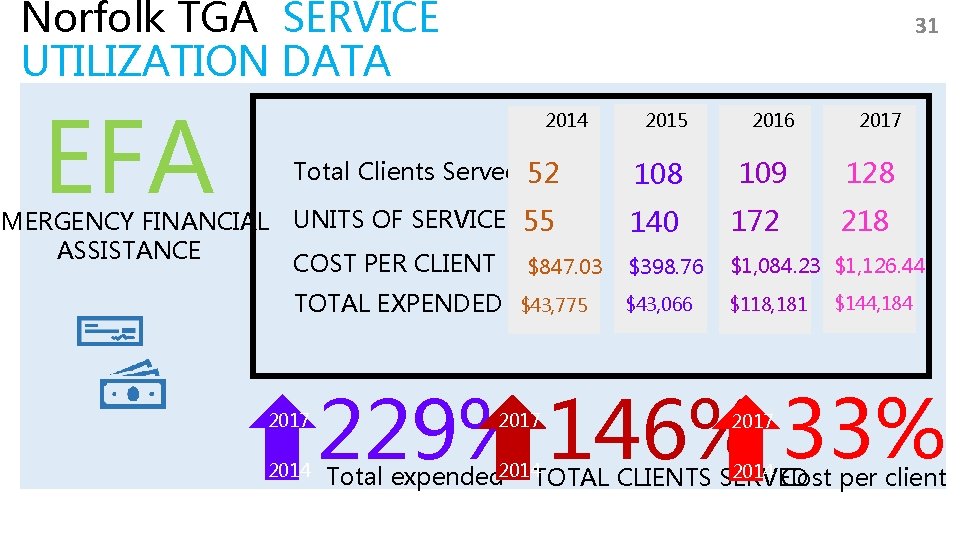
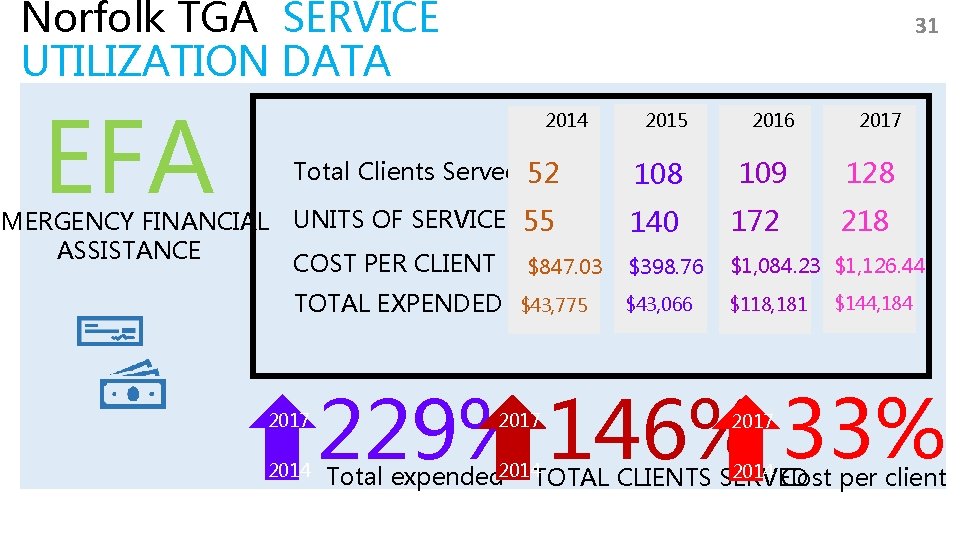
Norfolk TGA SERVICE UTILIZATION DATA EFA 31 2014 Total Clients Served 52 EMERGENCY FINANCIAL UNITS OF SERVICE 55 ASSISTANCE COST PER CLIENT $847. 03 TOTAL EXPENDED 2017 2014 $43, 775 2016 2017 108 109 128 140 172 218 $398. 76 $1, 084. 23 $1, 126. 44 $43, 066 $118, 181 $144, 184 229% 146% 33% 2017 2014 Cost per client Total expended 2014 TOTAL CLIENTS SERVED
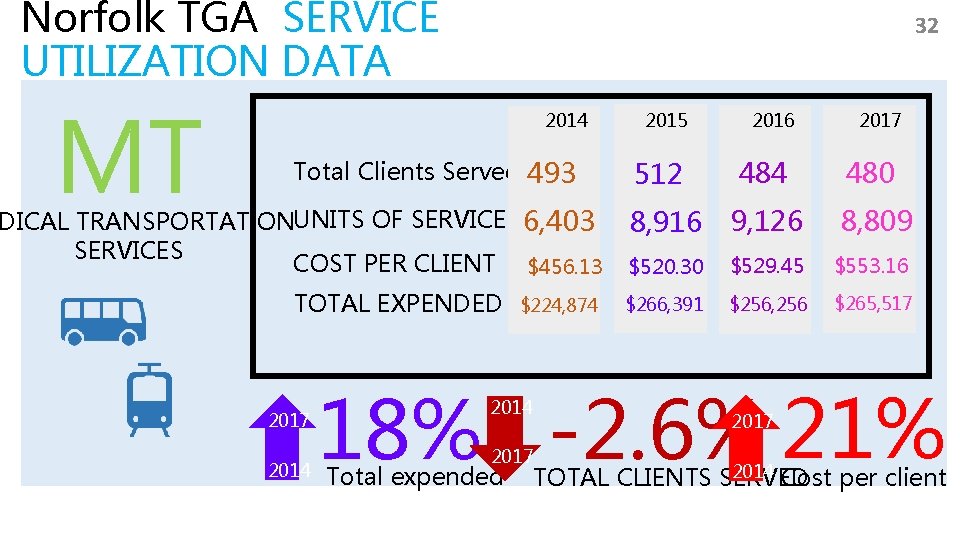
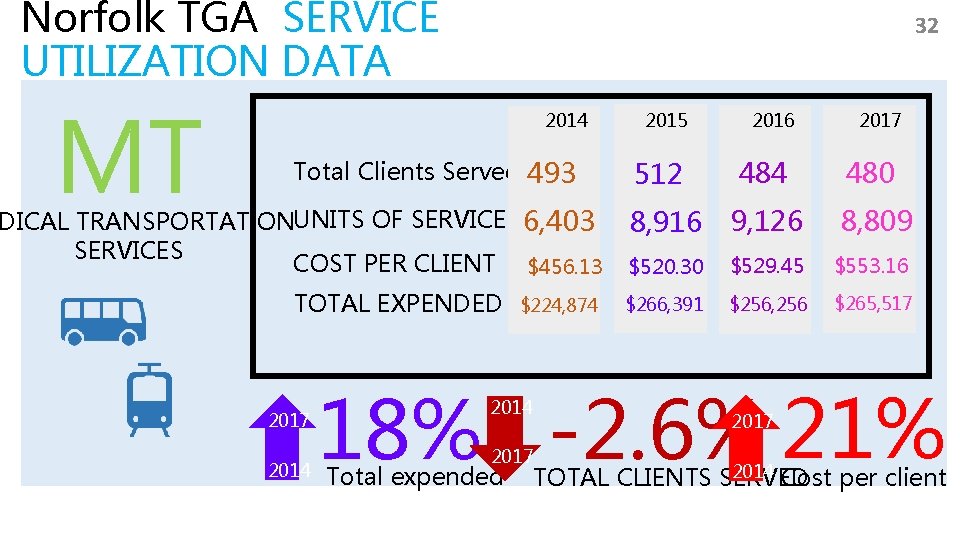
Norfolk TGA SERVICE UTILIZATION DATA MT 32 2014 Total Clients Served 493 DICAL TRANSPORTATIONUNITS OF SERVICE 6, 403 SERVICES COST PER CLIENT $456. 13 TOTAL EXPENDED 2017 2014 $224, 874 2015 2016 2017 512 484 480 8, 916 9, 126 8, 809 $520. 30 $529. 45 $553. 16 $266, 391 $256, 256 $265, 517 18% -2. 6% 21% 2014 2017 Total expended 2017 2014 Cost per client TOTAL CLIENTS SERVED
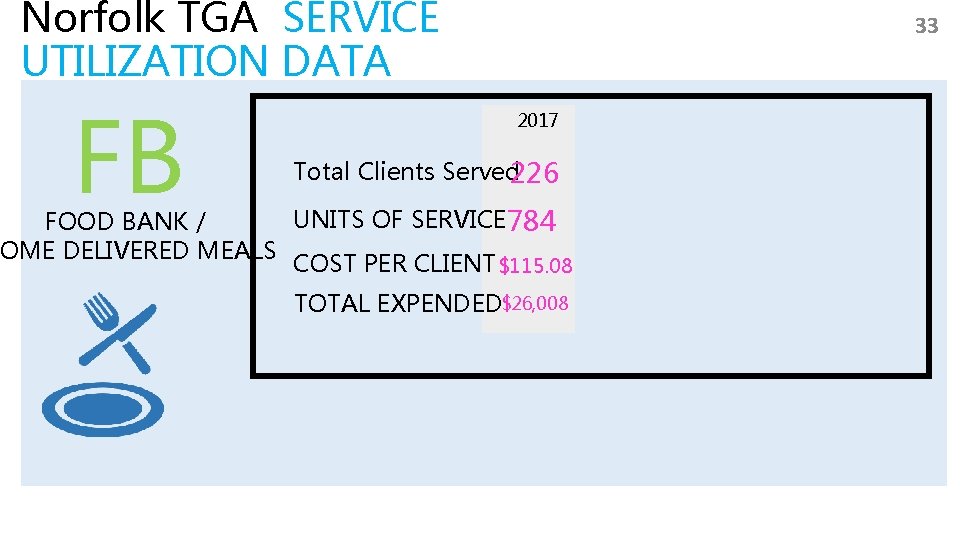
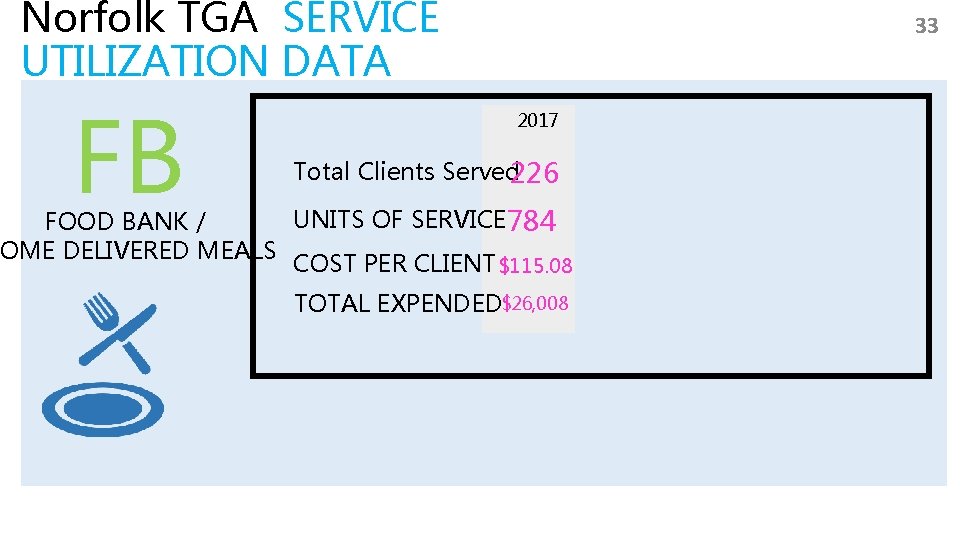
Norfolk TGA SERVICE UTILIZATION DATA FB 33 2017 Total Clients Served 226 UNITS OF SERVICE 784 FOOD BANK / OME DELIVERED MEALS COST PER CLIENT $115. 08 TOTAL EXPENDED$26, 008
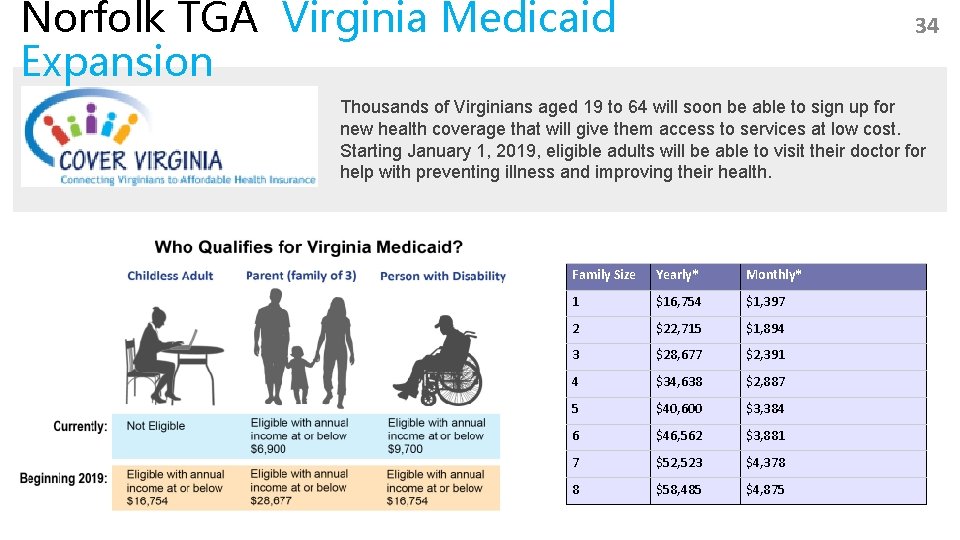
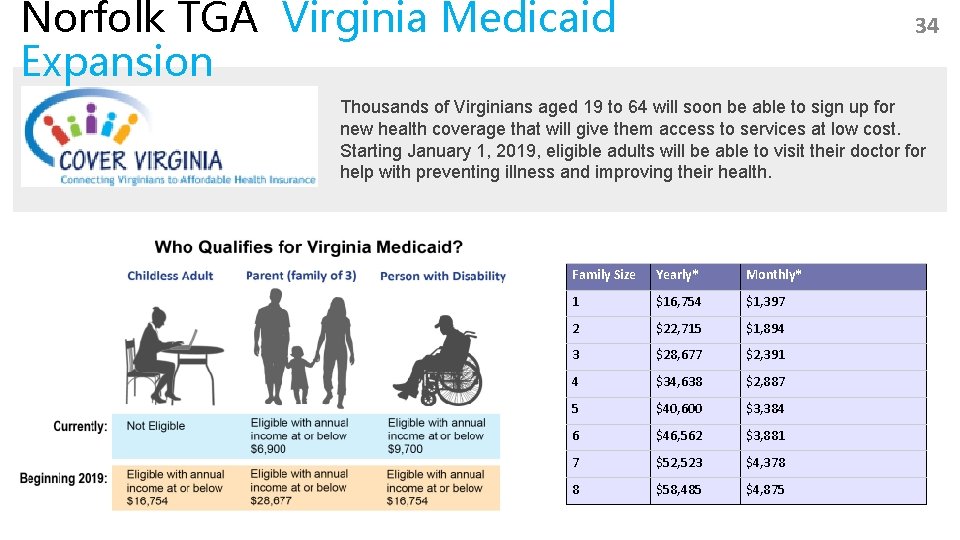
Norfolk TGA Virginia Medicaid Expansion 34 Thousands of Virginians aged 19 to 64 will soon be able to sign up for new health coverage that will give them access to services at low cost. Starting January 1, 2019, eligible adults will be able to visit their doctor for help with preventing illness and improving their health. Family Size Yearly* Monthly* 1 $16, 754 $1, 397 2 $22, 715 $1, 894 3 $28, 677 $2, 391 4 $34, 638 $2, 887 5 $40, 600 $3, 384 6 $46, 562 $3, 881 7 $52, 523 $4, 378 8 $58, 485 $4, 875
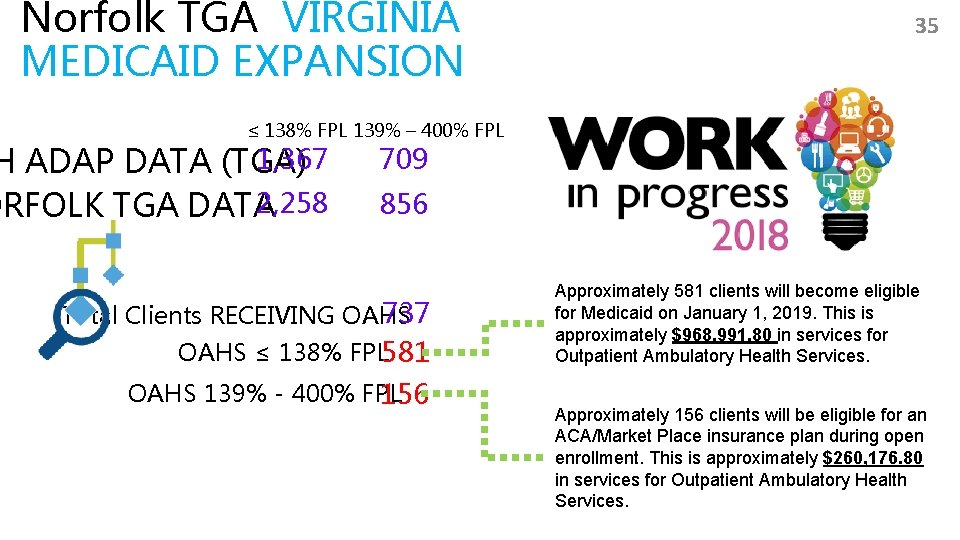
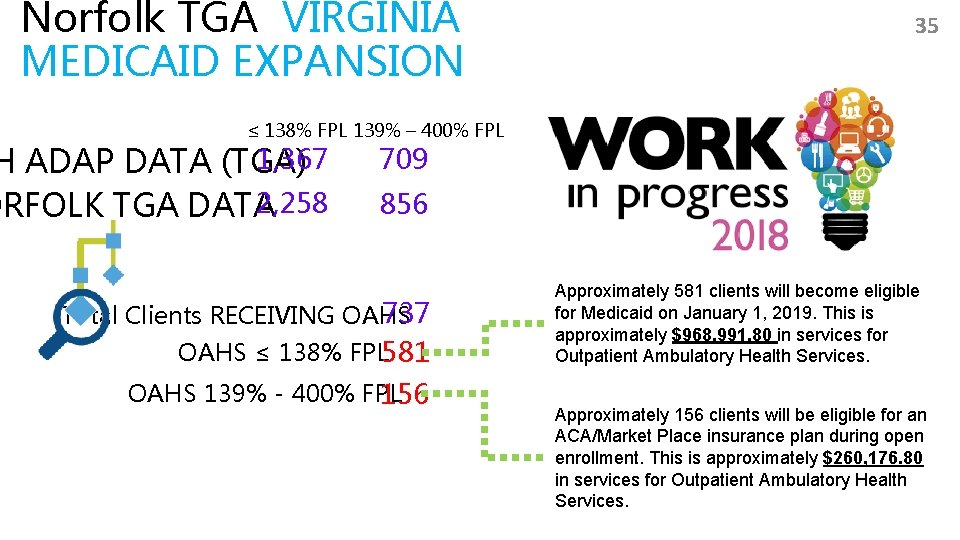
Norfolk TGA VIRGINIA MEDICAID EXPANSION 35 ≤ 138% FPL 139% – 400% FPL 1, 367 H ADAP DATA (TGA) 2, 258 ORFOLK TGA DATA 709 856 737 Total Clients RECEIVING OAHS ≤ 138% FPL 581 OAHS 139% - 400% FPL 156 Approximately 581 clients will become eligible for Medicaid on January 1, 2019. This is approximately $968, 991. 80 in services for Outpatient Ambulatory Health Services. Approximately 156 clients will be eligible for an ACA/Market Place insurance plan during open enrollment. This is approximately $260, 176. 80 in services for Outpatient Ambulatory Health Services.
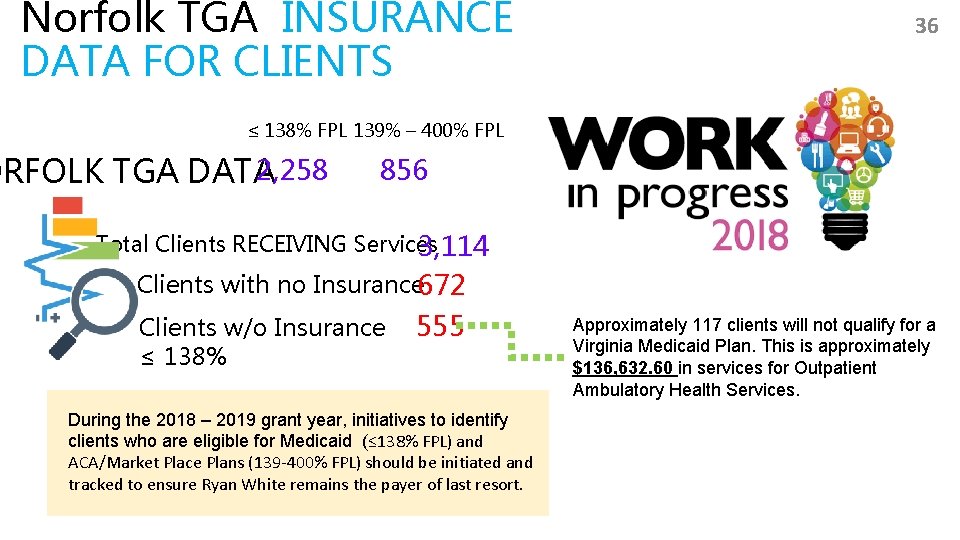
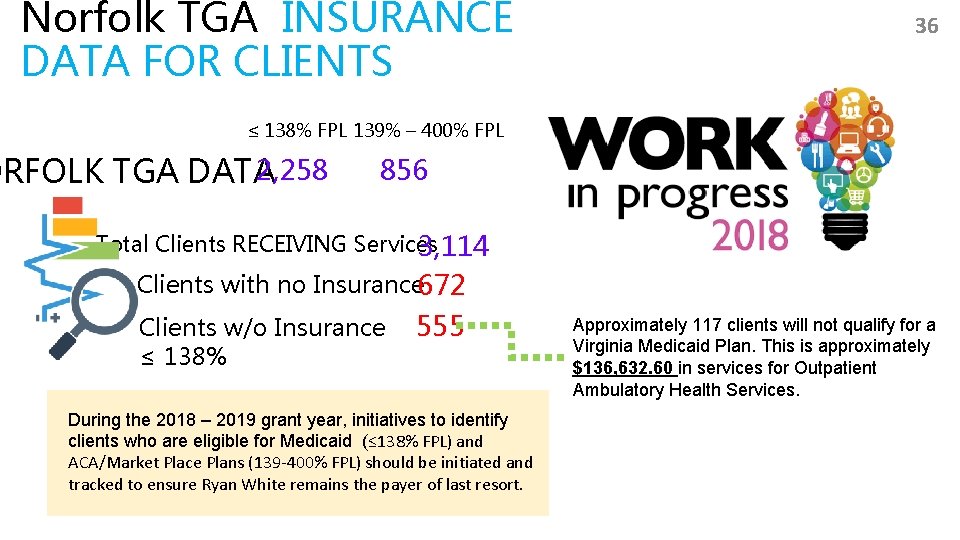
Norfolk TGA INSURANCE DATA FOR CLIENTS 36 ≤ 138% FPL 139% – 400% FPL 2, 258 ORFOLK TGA DATA 856 Total Clients RECEIVING Services 3, 114 Clients with no Insurance 672 Clients w/o Insurance ≤ 138% 555 During the 2018 – 2019 grant year, initiatives to identify clients who are eligible for Medicaid (≤ 138% FPL) and ACA/Market Place Plans (139 -400% FPL) should be initiated and tracked to ensure Ryan White remains the payer of last resort. Approximately 117 clients will not qualify for a Virginia Medicaid Plan. This is approximately $136, 632. 60 in services for Outpatient Ambulatory Health Services.
37 QUESTI ONS?