12 Lead ECGs Ischemia Injury Infarction Terry White
- Slides: 59
12 Lead ECGs: Ischemia, Injury & Infarction Terry White, RN, EMT-P
Ischemia, Injury & Infarction H Definitions H Injury/Infarct Recognition H Localization & Evolution H Reciprocal Changes H The High Acuity Patient
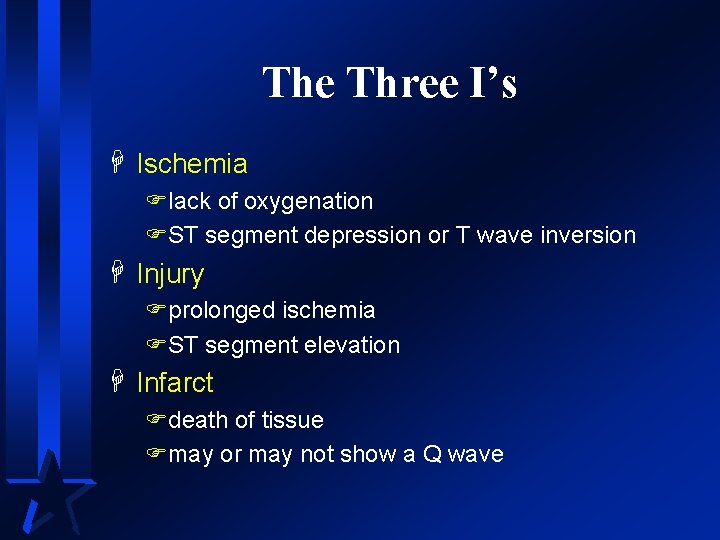
The Three I’s H Ischemia Flack of oxygenation FST segment depression or T wave inversion H Injury Fprolonged ischemia FST segment elevation H Infarct Fdeath of tissue Fmay or may not show a Q wave
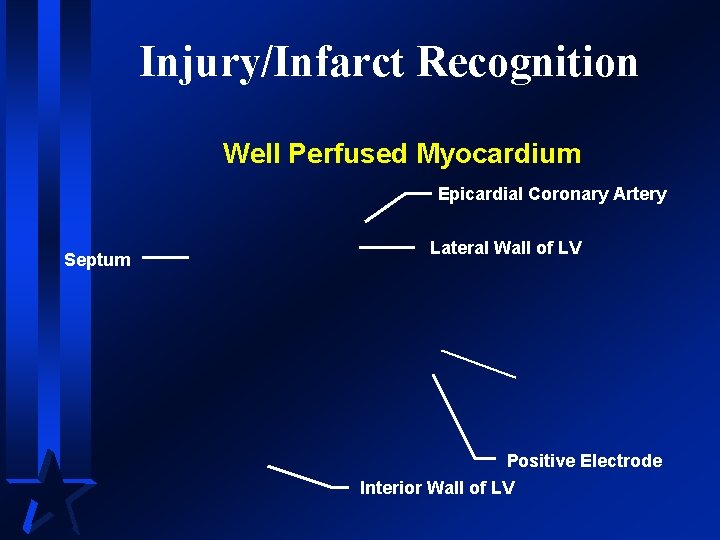
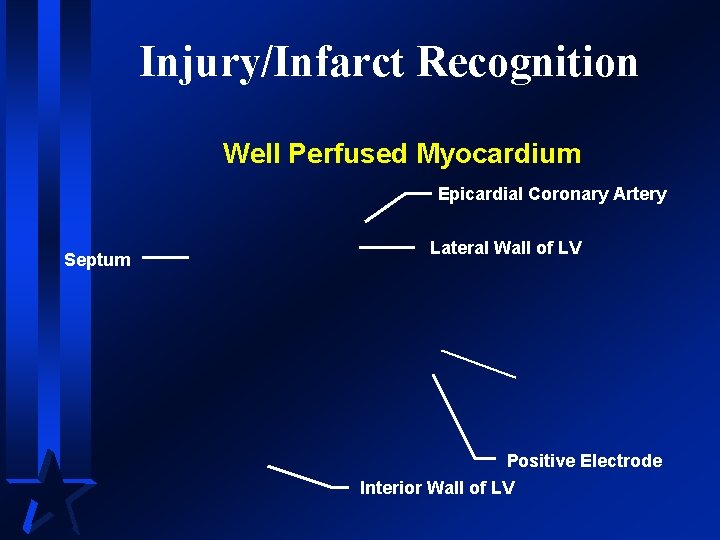
Injury/Infarct Recognition Well Perfused Myocardium Epicardial Coronary Artery Septum Lateral Wall of LV Positive Electrode Interior Wall of LV
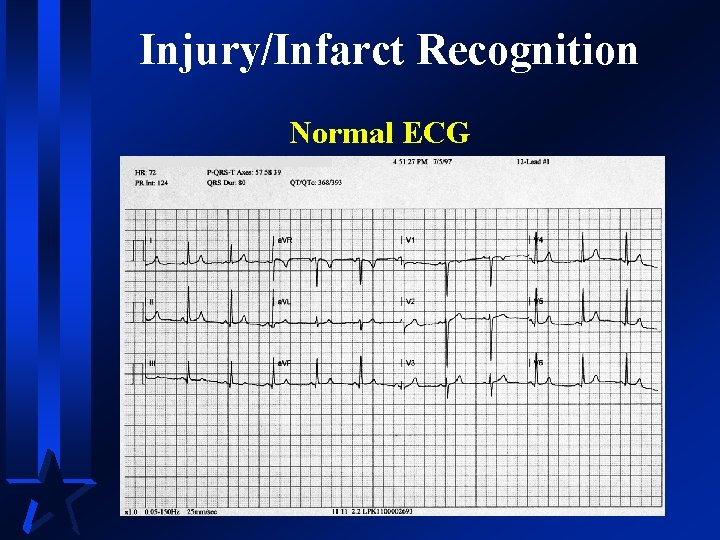
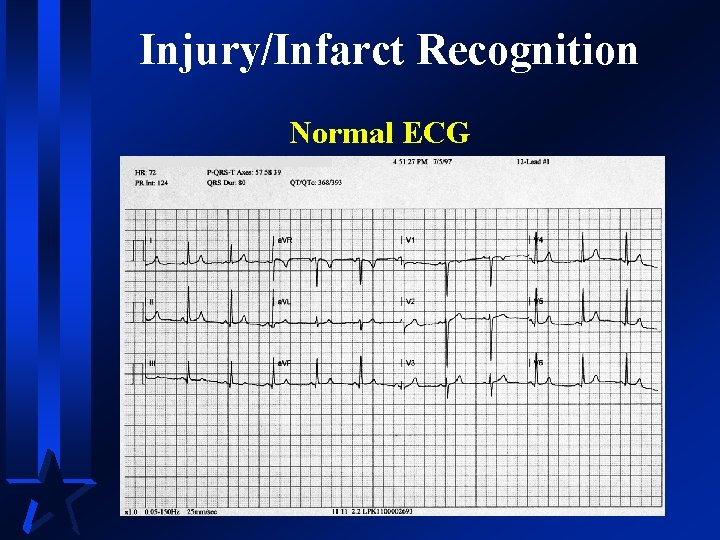
Injury/Infarct Recognition Normal ECG
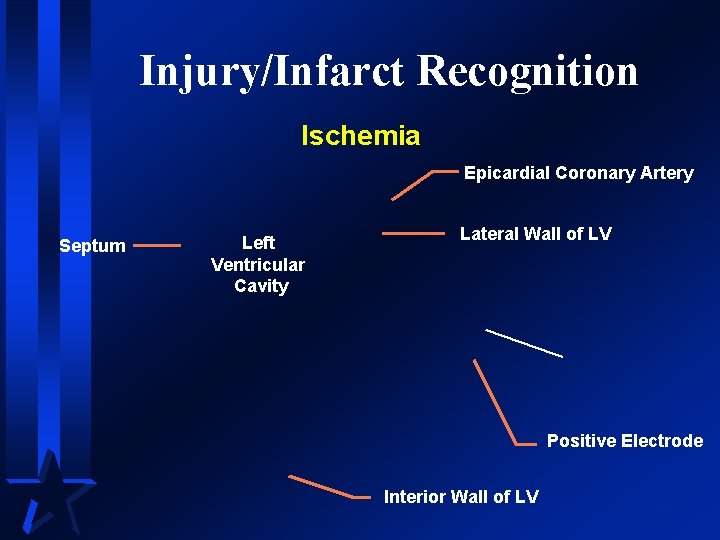
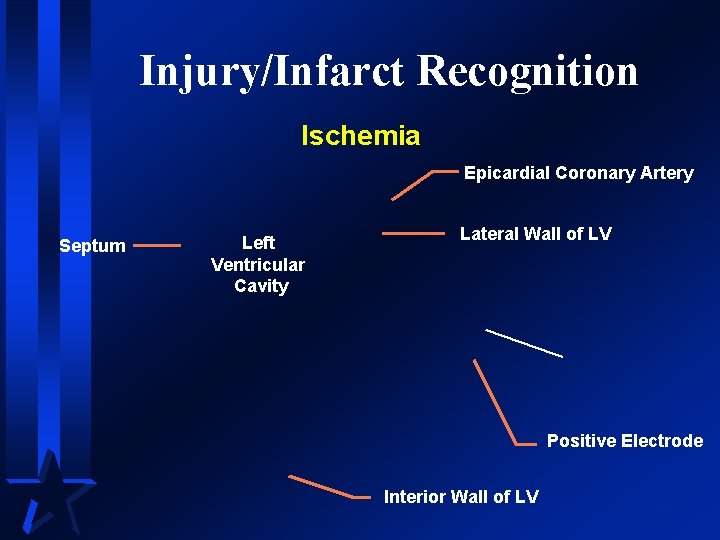
Injury/Infarct Recognition Ischemia Epicardial Coronary Artery Septum Left Ventricular Cavity Lateral Wall of LV Positive Electrode Interior Wall of LV
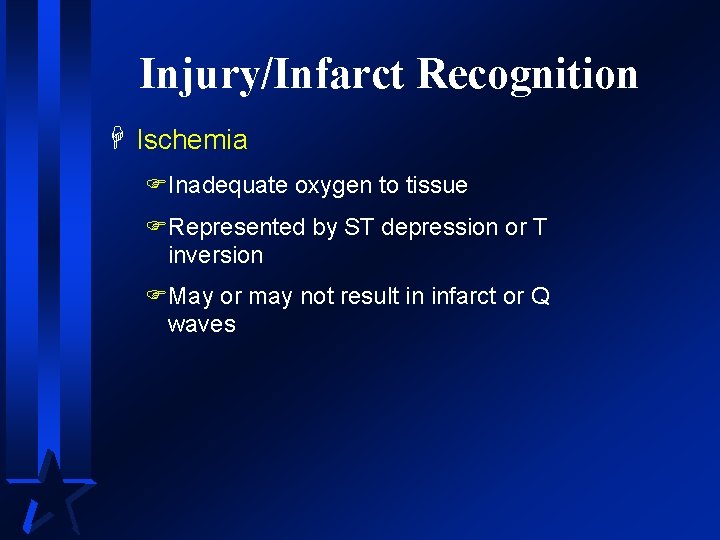
Injury/Infarct Recognition H Ischemia FInadequate oxygen to tissue FRepresented by ST depression or T inversion FMay or may not result in infarct or Q waves
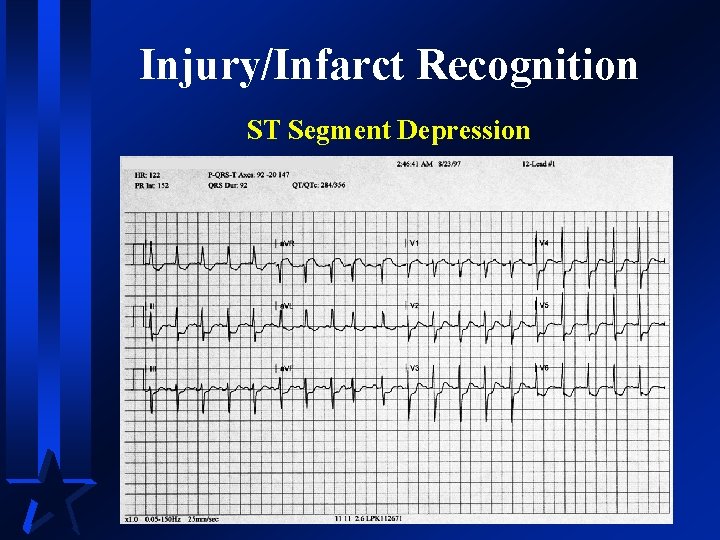
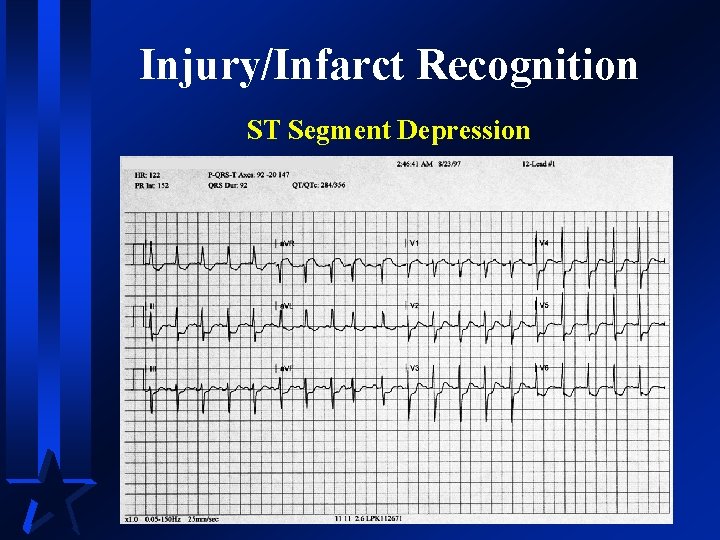
Injury/Infarct Recognition ST Segment Depression
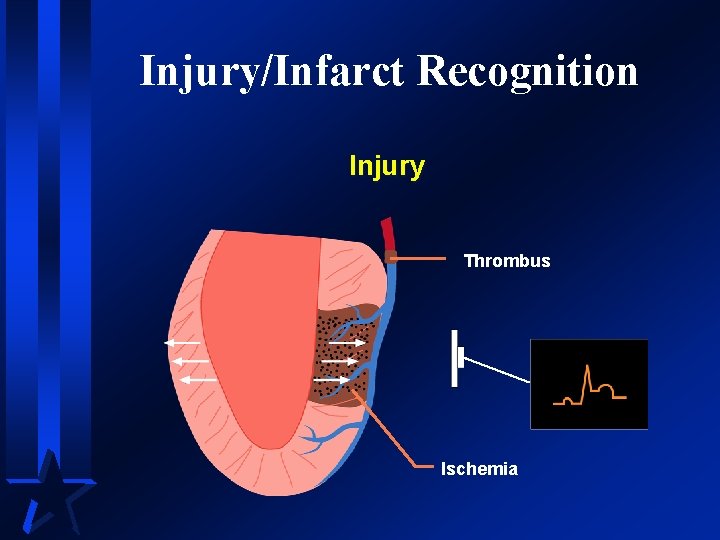
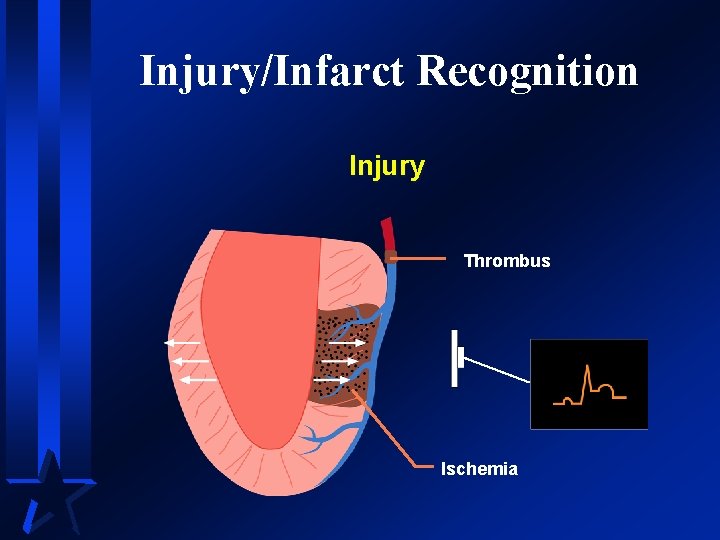
Injury/Infarct Recognition Injury Thrombus Ischemia
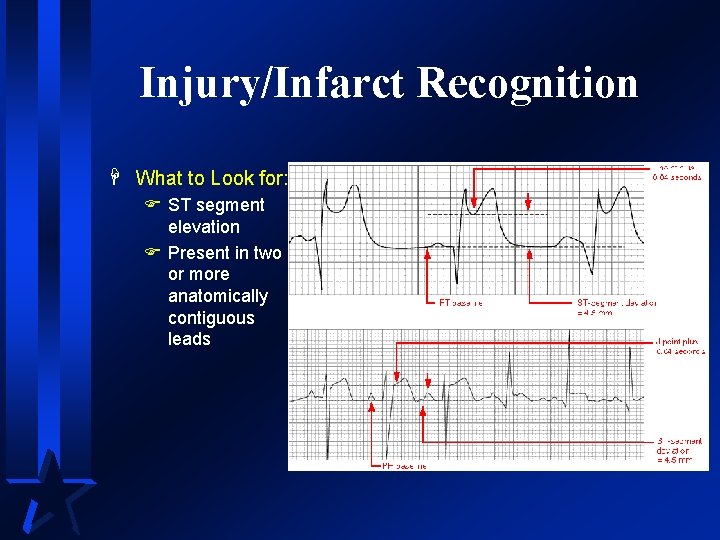
Injury/Infarct Recognition H Injury FProlonged ischemia FRepresented by ST elevation W referred to as an “injury pattern” FUsually results in infarct W may or may not develop Q wave
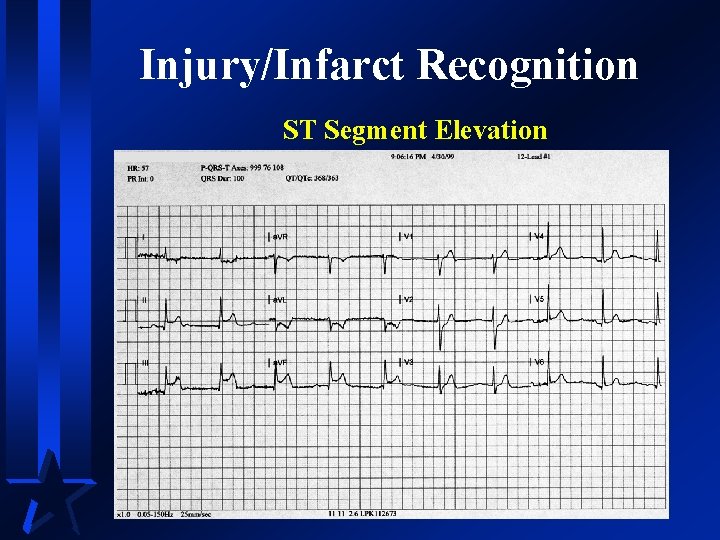
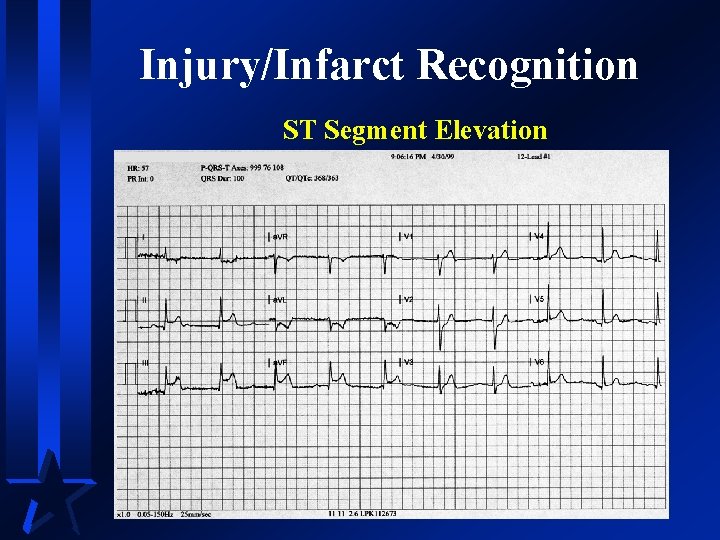
Injury/Infarct Recognition ST Segment Elevation
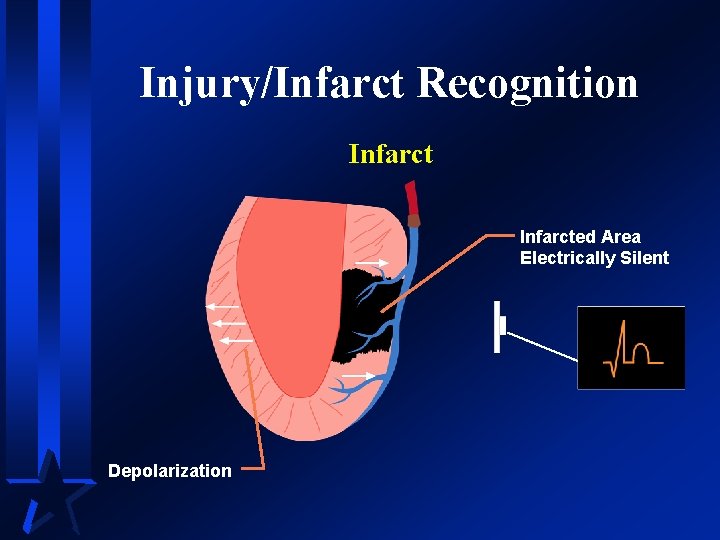
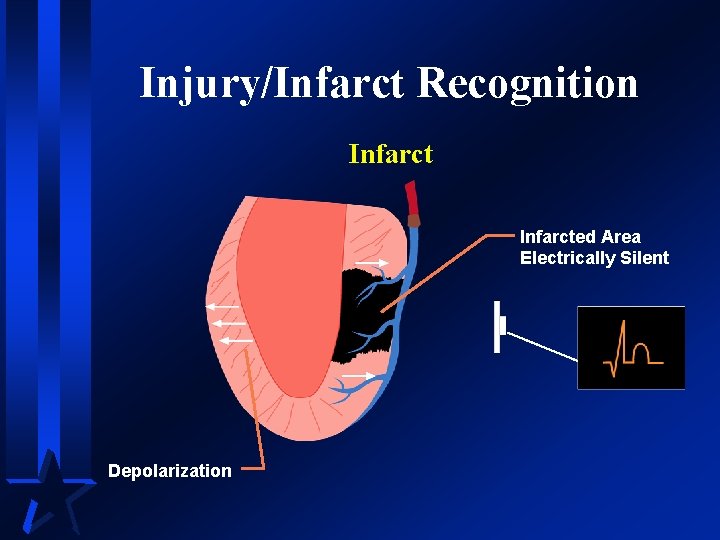
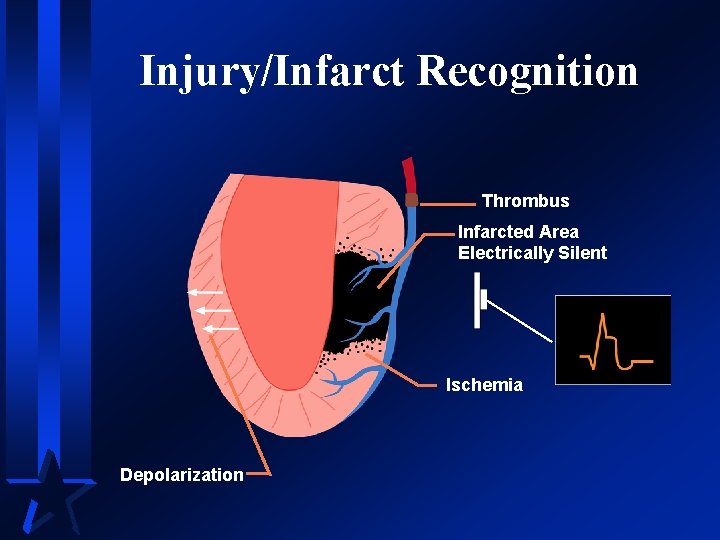
Injury/Infarct Recognition Infarcted Area Electrically Silent Depolarization
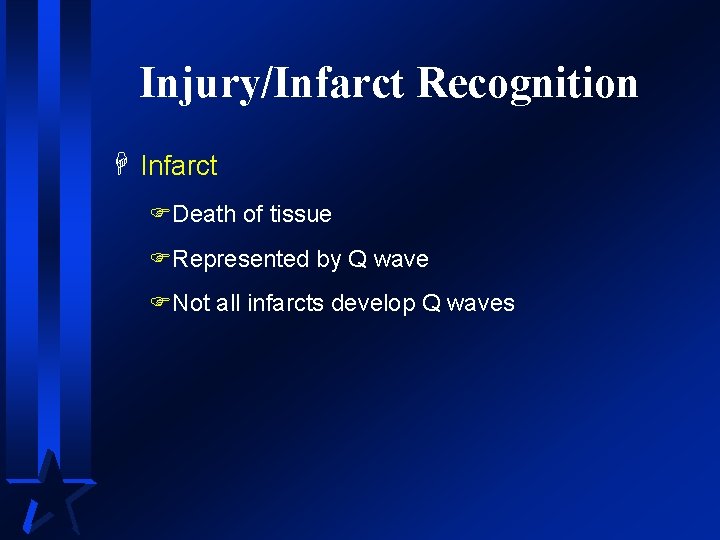
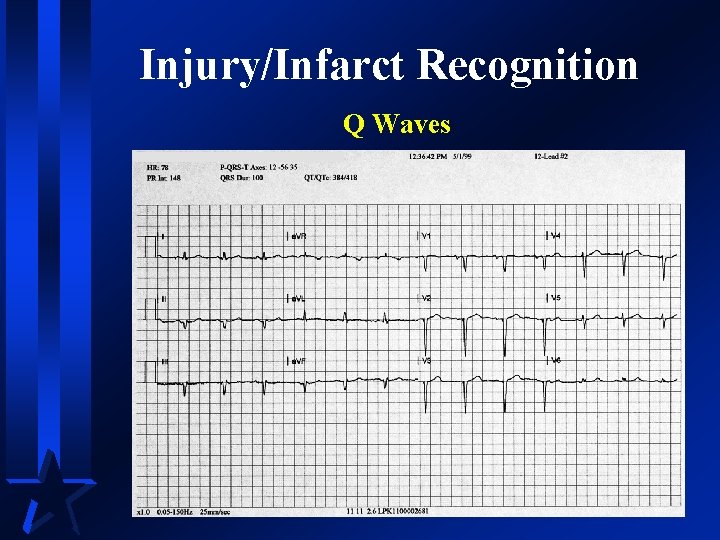
Injury/Infarct Recognition H Infarct FDeath of tissue FRepresented by Q wave FNot all infarcts develop Q waves
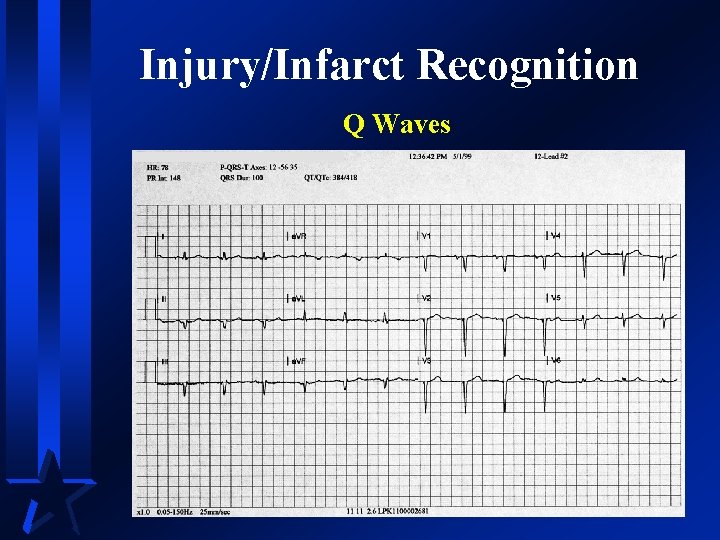
Injury/Infarct Recognition Q Waves
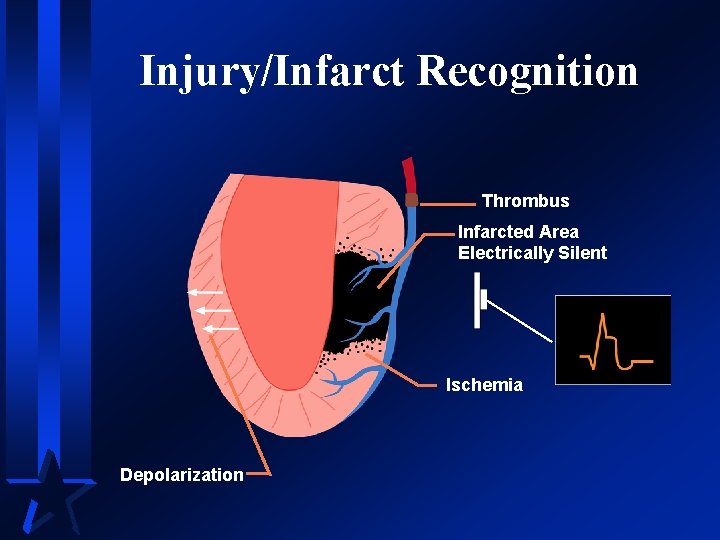
Injury/Infarct Recognition Thrombus Infarcted Area Electrically Silent Ischemia Depolarization
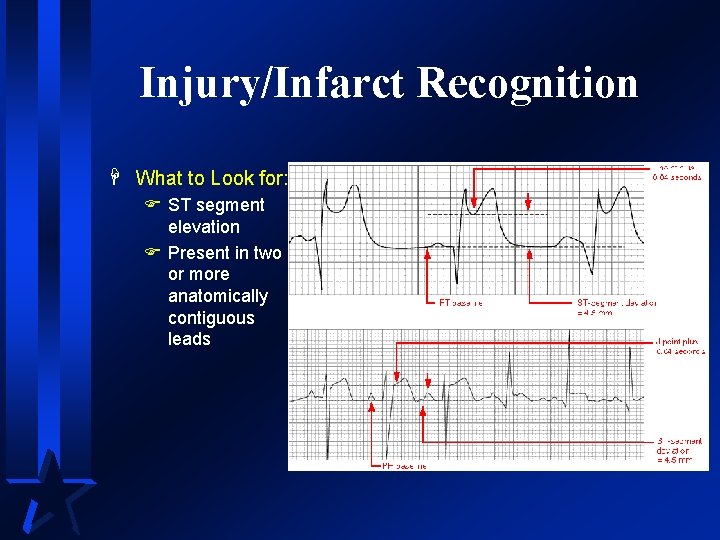
Injury/Infarct Recognition H What to Look for: F ST segment elevation F Present in two or more anatomically contiguous leads
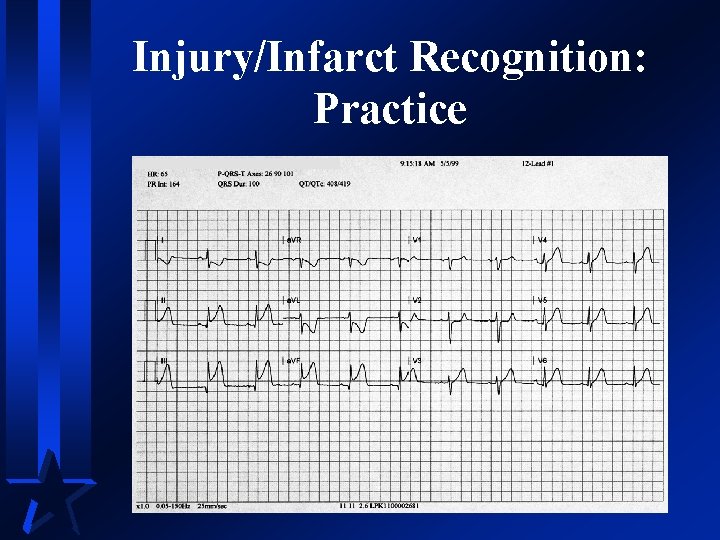
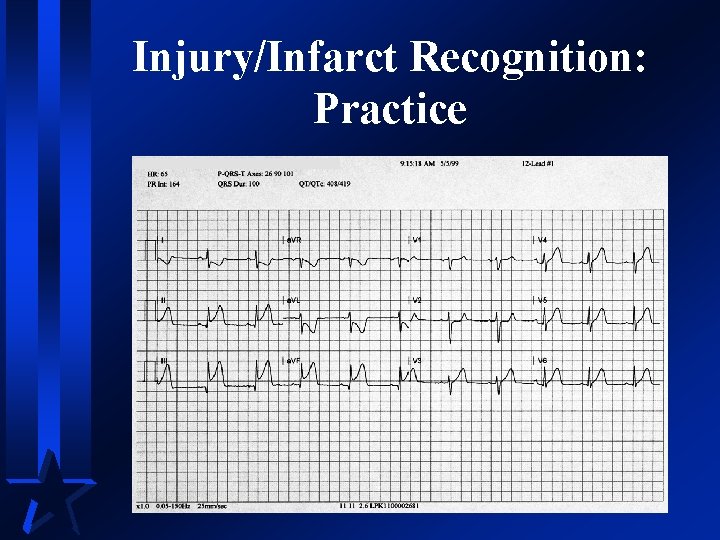
Injury/Infarct Recognition: Practice
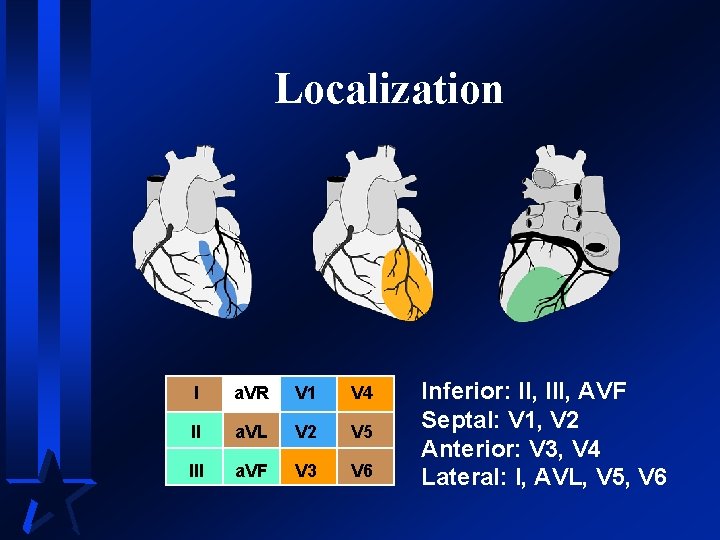
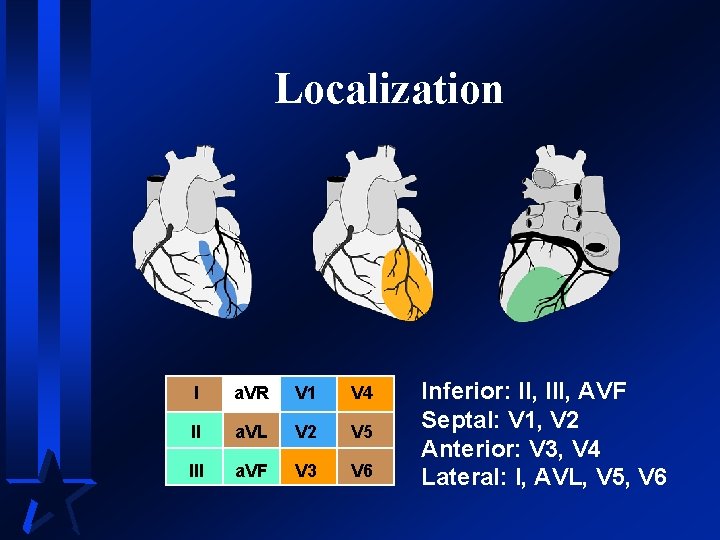
Localization I a. VR V 1 V 4 II a. VL V 2 V 5 III a. VF V 3 V 6 Inferior: II, III, AVF Septal: V 1, V 2 Anterior: V 3, V 4 Lateral: I, AVL, V 5, V 6
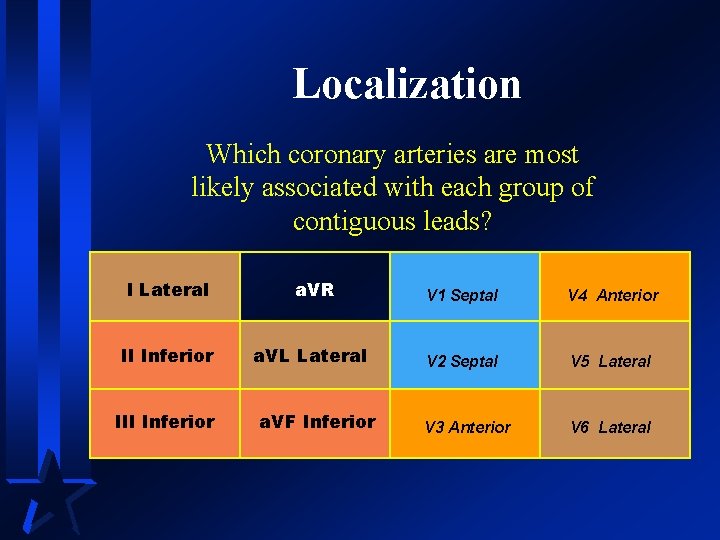
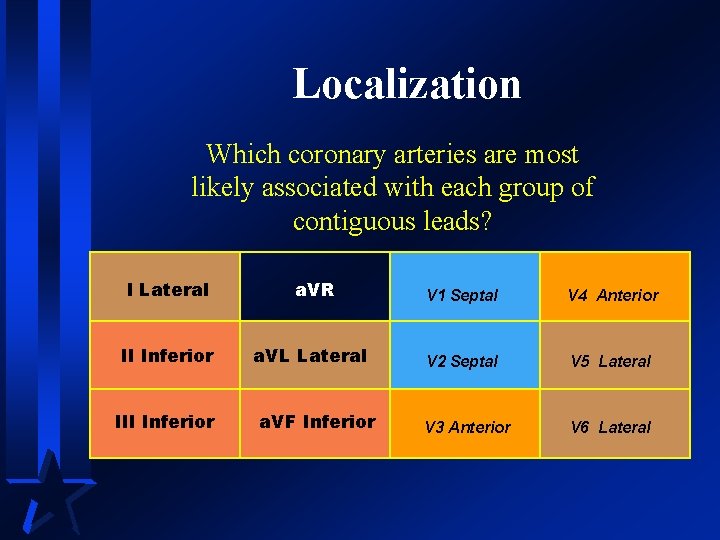
Localization Which coronary arteries are most likely associated with each group of contiguous leads? I Lateral a. VR II Inferior a. VL Lateral III Inferior a. VF Inferior V 1 Septal V 4 Anterior V 2 Septal V 5 Lateral V 3 Anterior V 6 Lateral
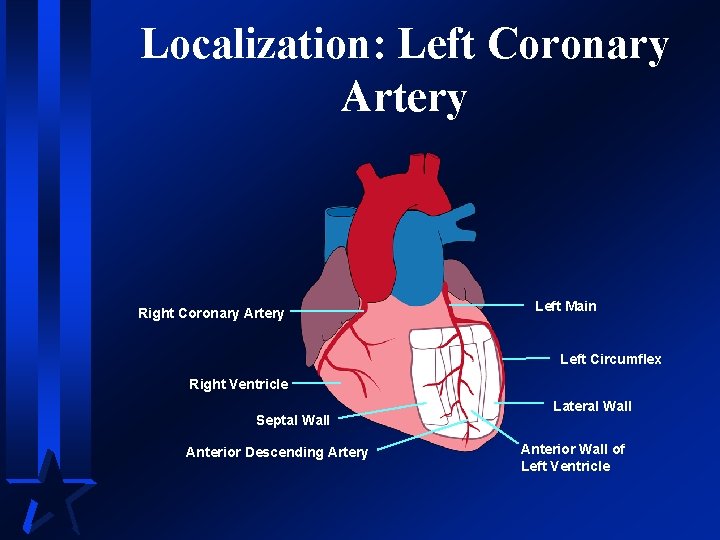
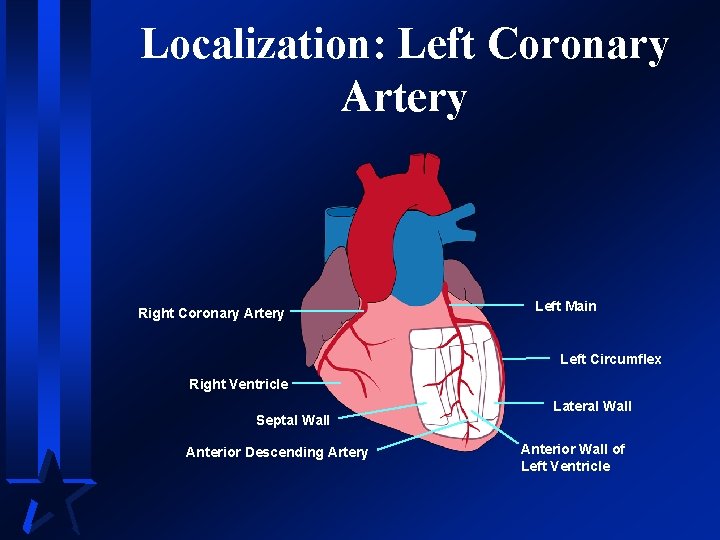
Localization: Left Coronary Artery Right Coronary Artery Left Main Left Circumflex Right Ventricle Septal Wall Anterior Descending Artery Lateral Wall Anterior Wall of Left Ventricle
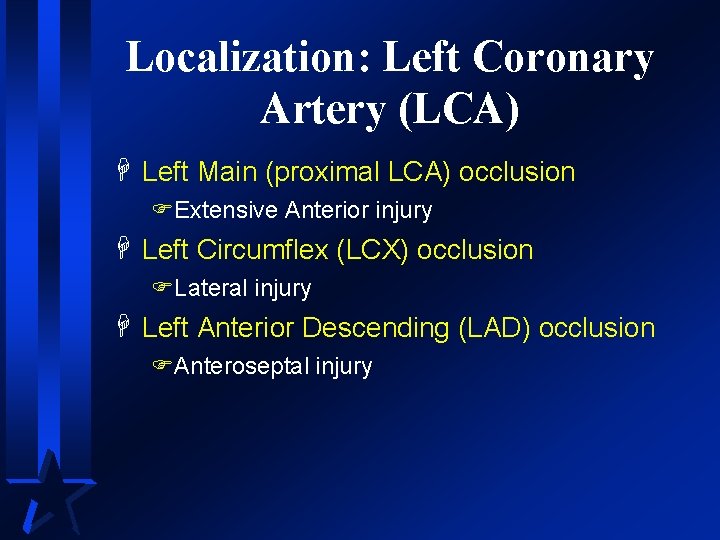
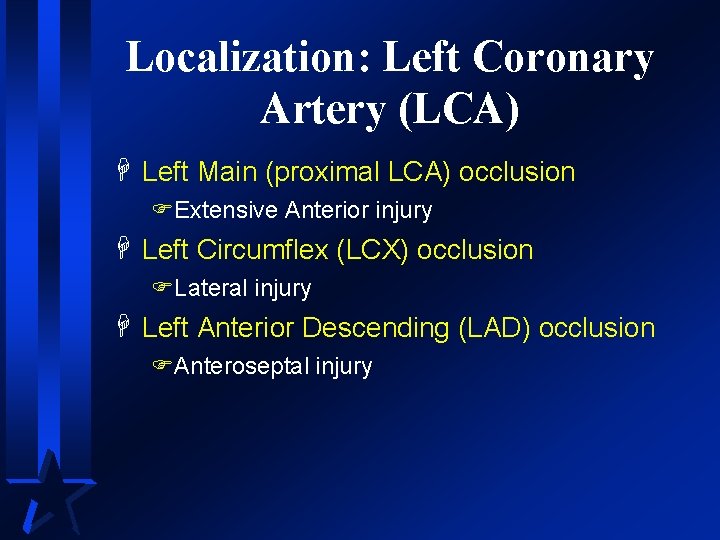
Localization: Left Coronary Artery (LCA) H Left Main (proximal LCA) occlusion FExtensive Anterior injury H Left Circumflex (LCX) occlusion FLateral injury H Left Anterior Descending (LAD) occlusion FAnteroseptal injury
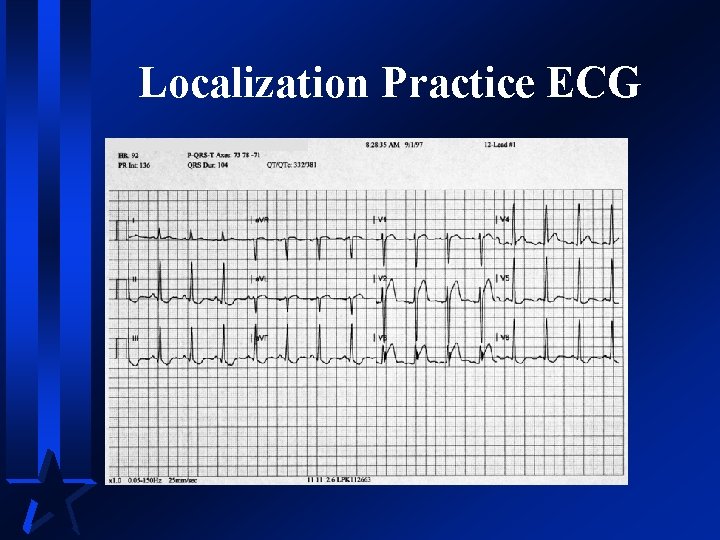
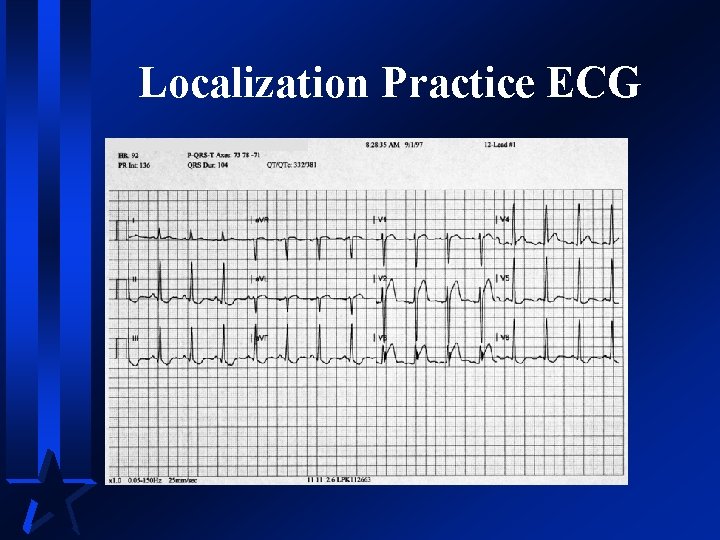
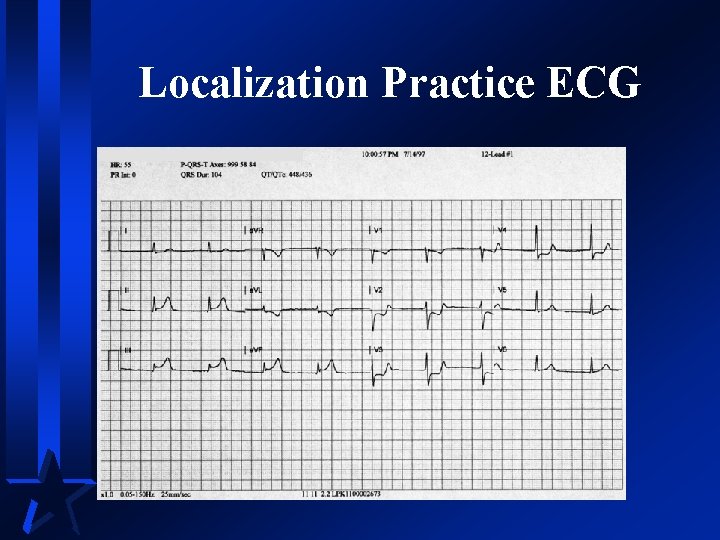
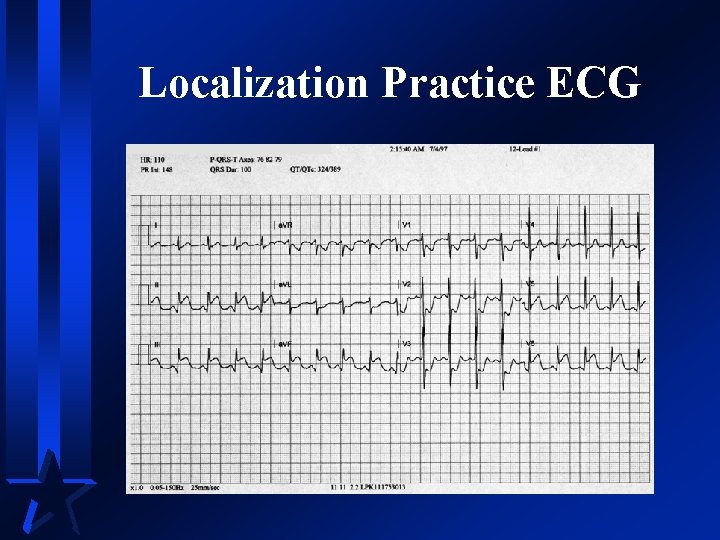
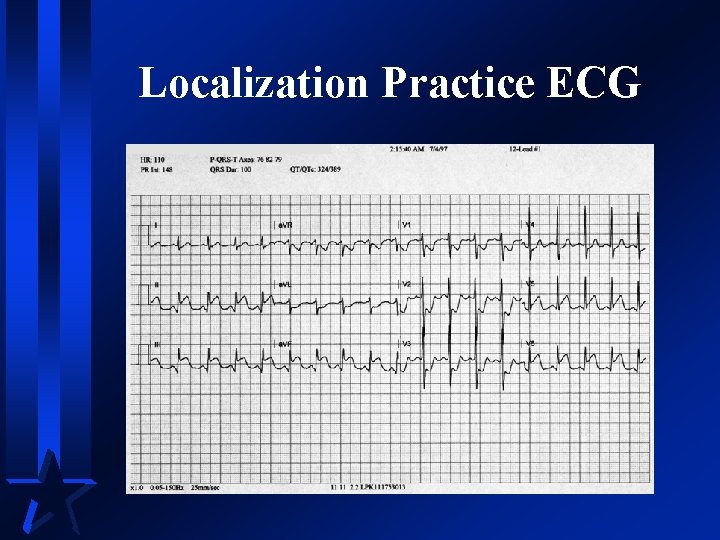
Localization Practice ECG
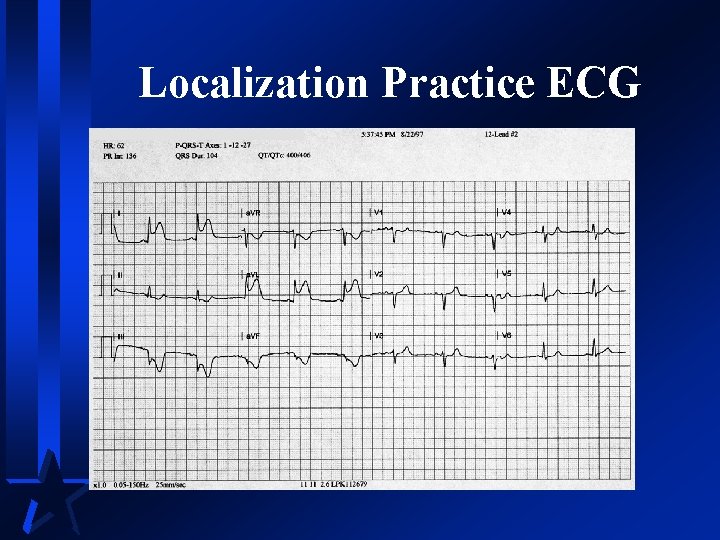
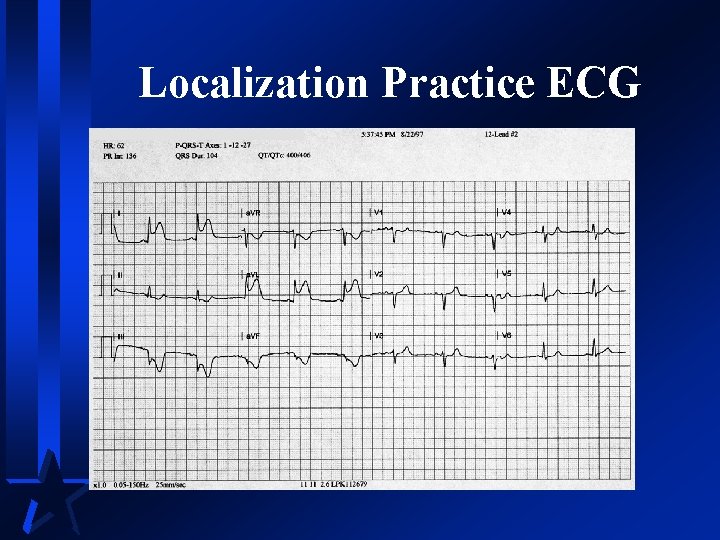
Localization Practice ECG
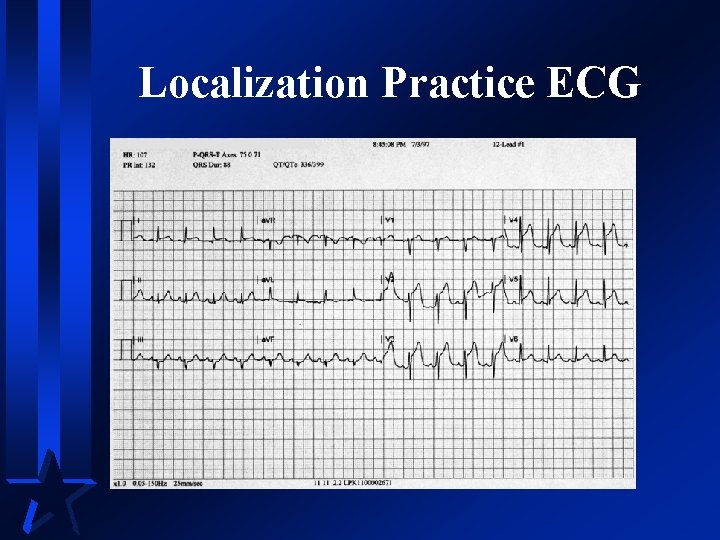
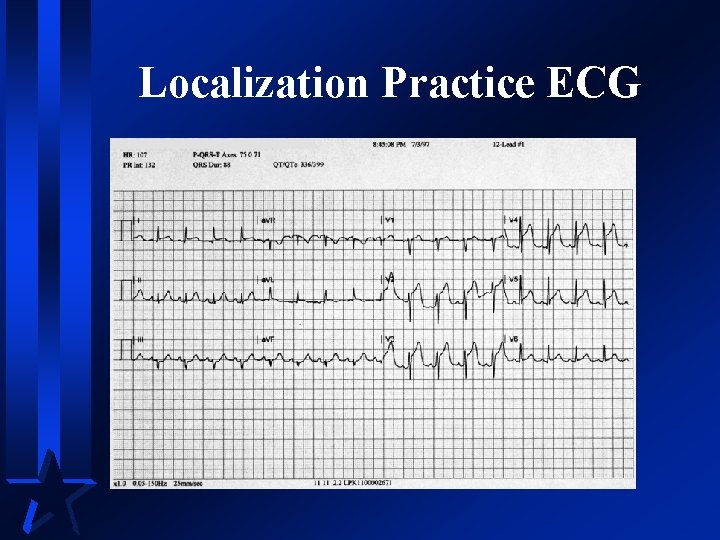
Localization Practice ECG
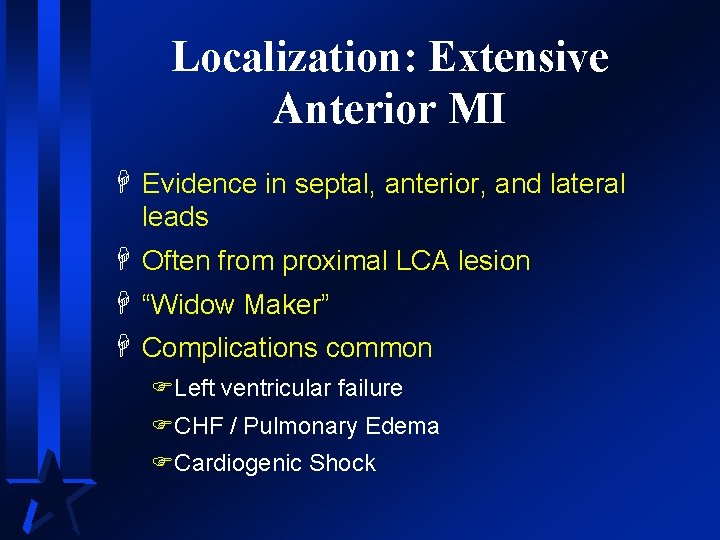
Localization: Extensive Anterior MI H Evidence in septal, anterior, and lateral leads H Often from proximal LCA lesion H “Widow Maker” H Complications common FLeft ventricular failure FCHF / Pulmonary Edema FCardiogenic Shock
Localization: Definitive Therapy for Extensive AWMI H Normal blood pressure FThrombolysis may be indicated H Signs of shock FPTCA FCABG
Localization: LCA Occlusions H Other considerations FBundle branches supplied by LCA FSerious infranodal heart block may occur
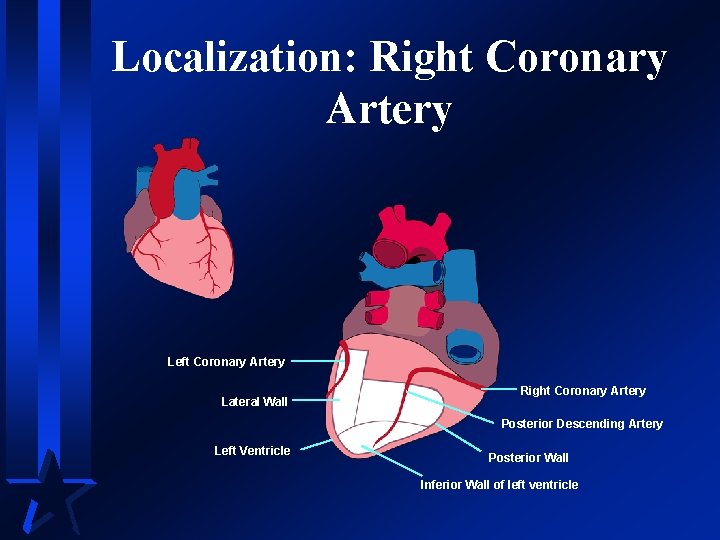
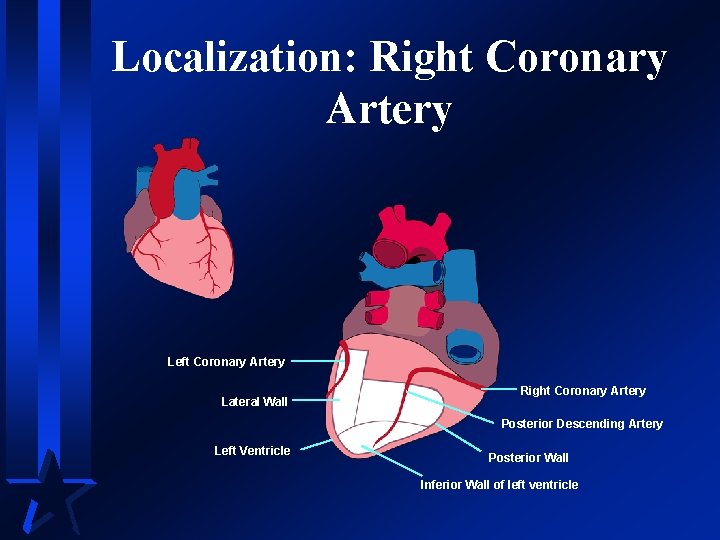
Localization: Right Coronary Artery Left Coronary Artery Lateral Wall Right Coronary Artery Posterior Descending Artery Left Ventricle Posterior Wall Inferior Wall of left ventricle
Localization: Right Coronary Artery (RCA) H Proximal RCA occlusion FRight Ventricle injured FPosterior wall of left ventricle injured FInferior wall of left ventricle injured H Posterior descending artery (PDA) occlusion FInferior wall of right ventricle injured
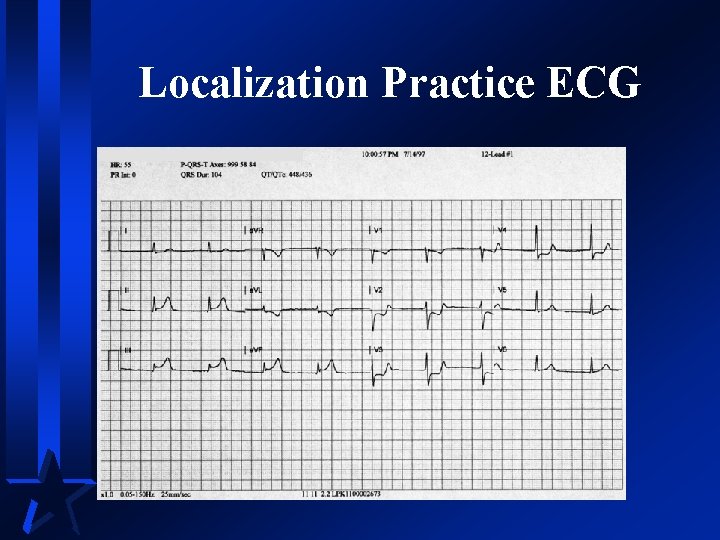
Localization Practice ECG
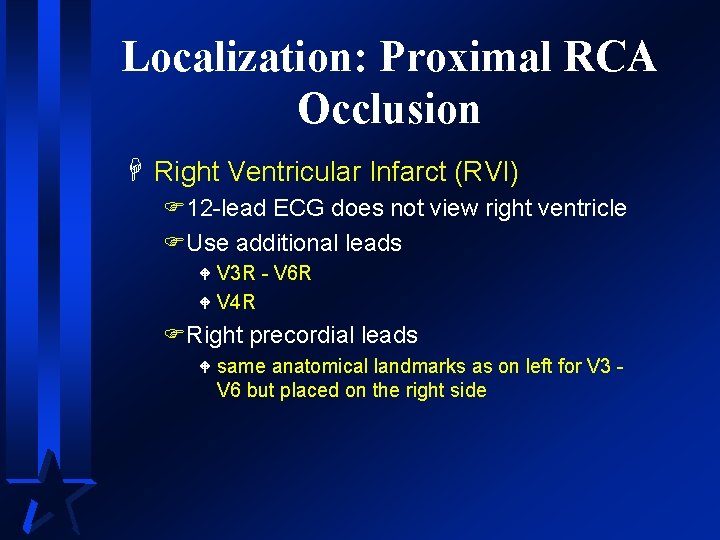
Localization: Proximal RCA Occlusion H Right Ventricular Infarct (RVI) F 12 -lead ECG does not view right ventricle FUse additional leads V 3 R - V 6 R W V 4 R W FRight precordial leads W same anatomical landmarks as on left for V 3 V 6 but placed on the right side
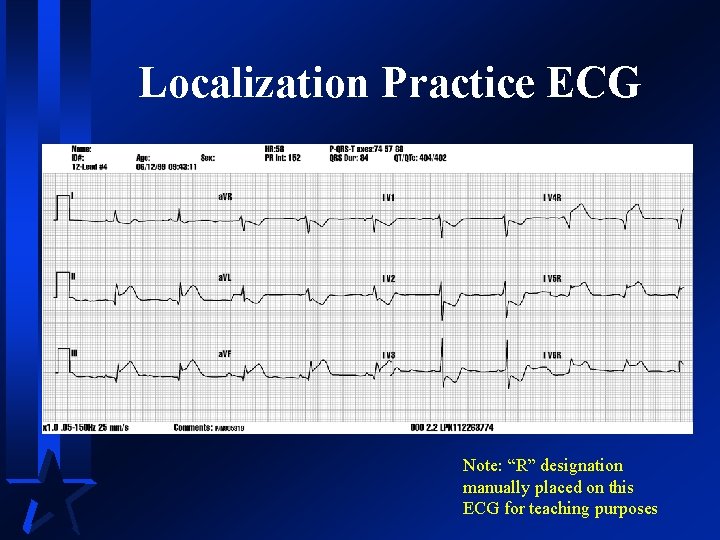
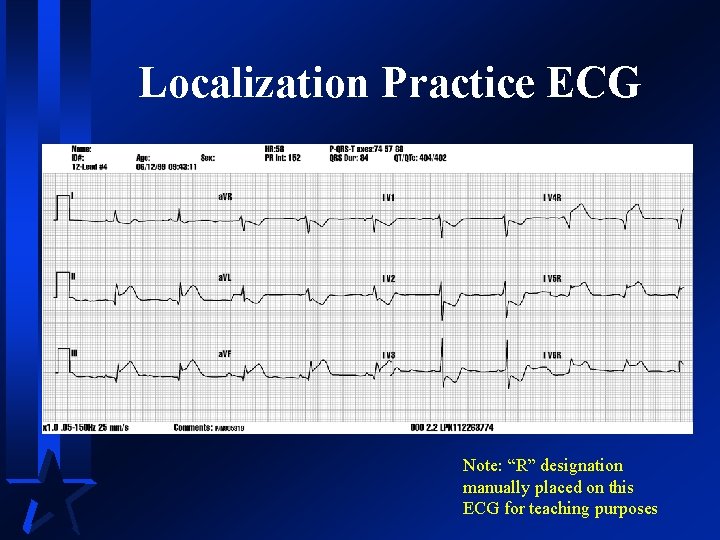
Localization Practice ECG Note: “R” designation manually placed on this ECG for teaching purposes
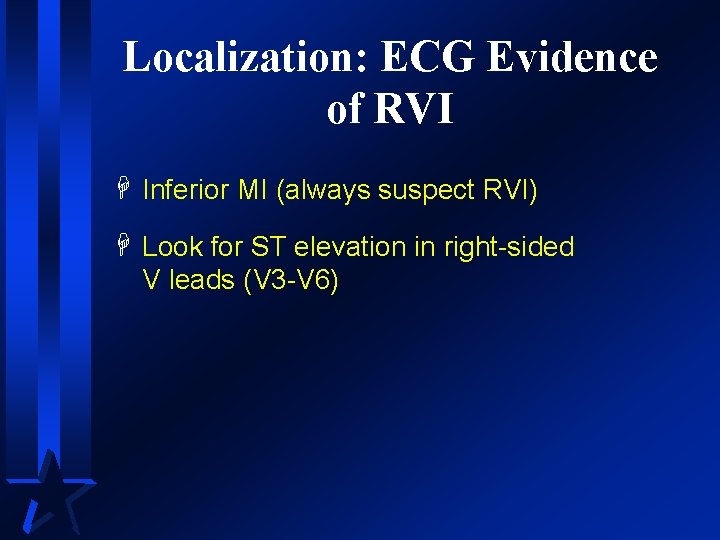
Localization: ECG Evidence of RVI H Inferior MI (always suspect RVI) H Look for ST elevation in right-sided V leads (V 3 -V 6)
Localization: Physical Evidence of RVI H Dyspnea with clear lungs H Jugular vein distension H Hypotension FRelative or absolute
Localization: Treatment for RVI H Use caution with vasodilators FSmall incremental doses of MS FNTG by drip H Treat hypotension with fluid FOne to two liters may be required FLarge bore IV lines
Localization: Posterior Wall MI (PWMI) H Usually extension of an inferior or lateral MI FPosterior wall receives blood from RCA & LCA H Common with proximal RCA occlusions H Occurs with LCX occlusions H Identified by reciprocal changes in V 1 -V 4 FMay also use Posterior leads to identify W V 7: posterior axillary line level with V 6 W V 8: mid-scapular line level with V 6 W V 9: left para-vertebral level with V 6
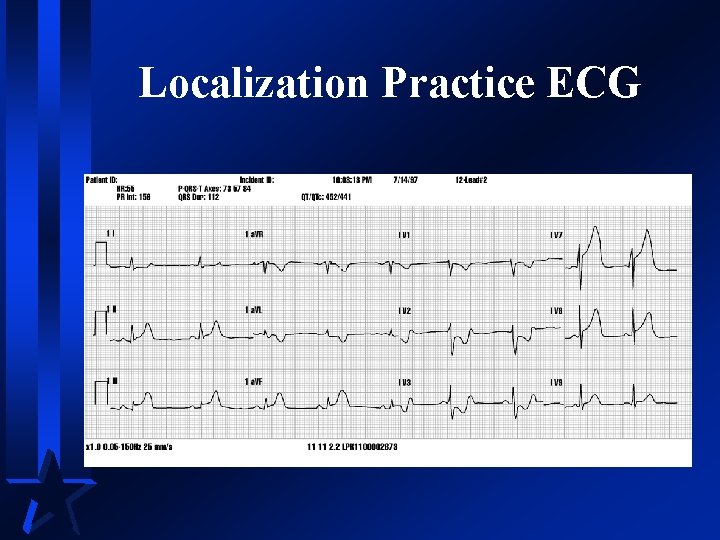
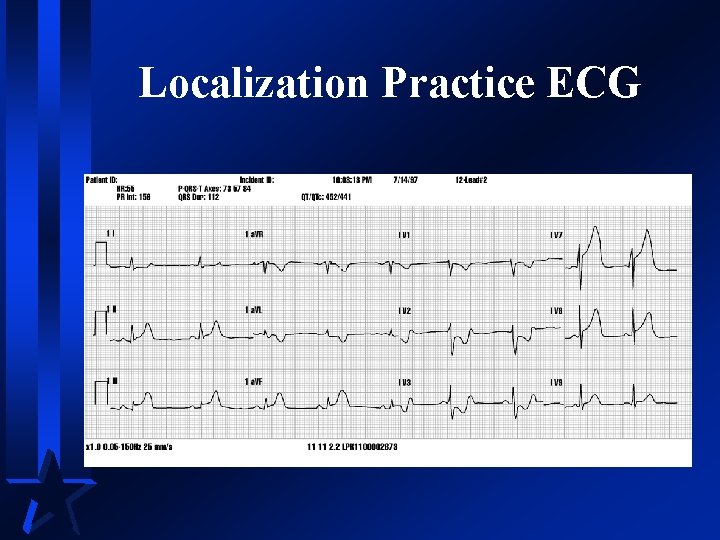
Localization Practice ECG
Localization: Left Coronary Dominance H Approximately 10% of population FLCX connects to posterior descending artery and dominates inferior wall perfusion H In these cases when LCX is occluded, lateral and inferior walls infarct FInferolateral MI
Localization Practice ECG
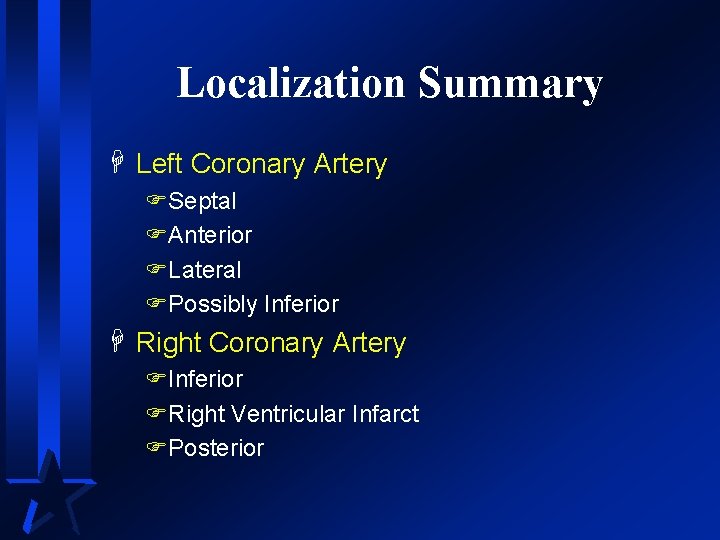
Localization Summary H Left Coronary Artery FSeptal FAnterior FLateral FPossibly Inferior H Right Coronary Artery FInferior FRight Ventricular Infarct FPosterior
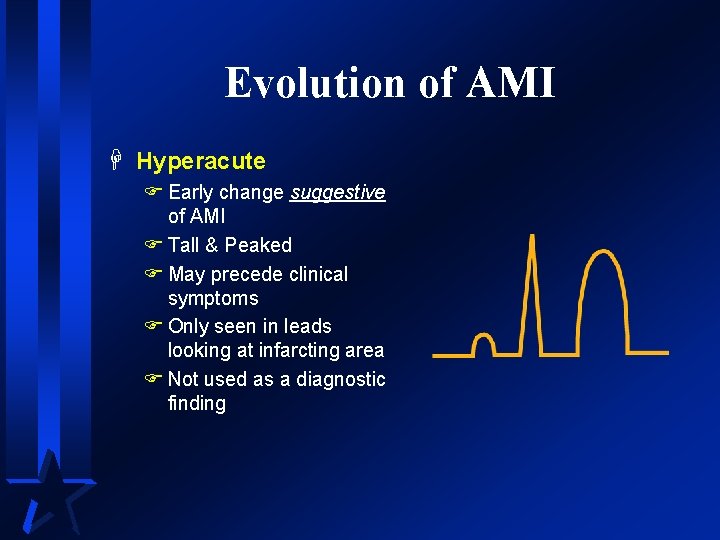
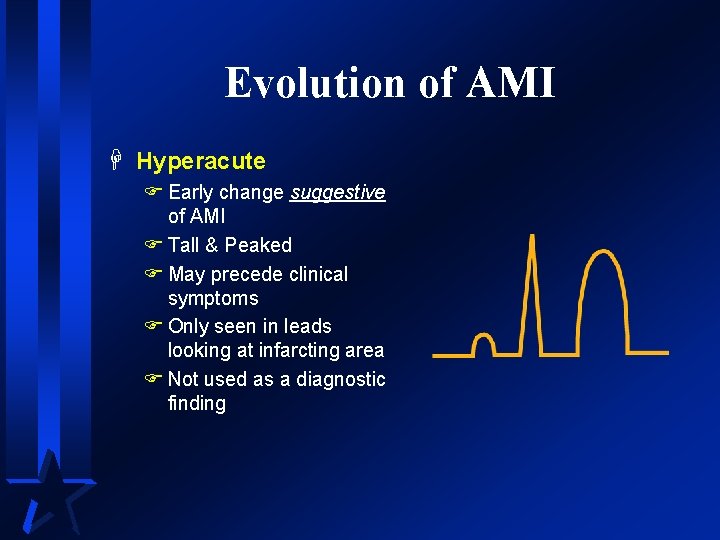
Evolution of AMI H Hyperacute F Early change suggestive of AMI F Tall & Peaked F May precede clinical symptoms F Only seen in leads looking at infarcting area F Not used as a diagnostic finding
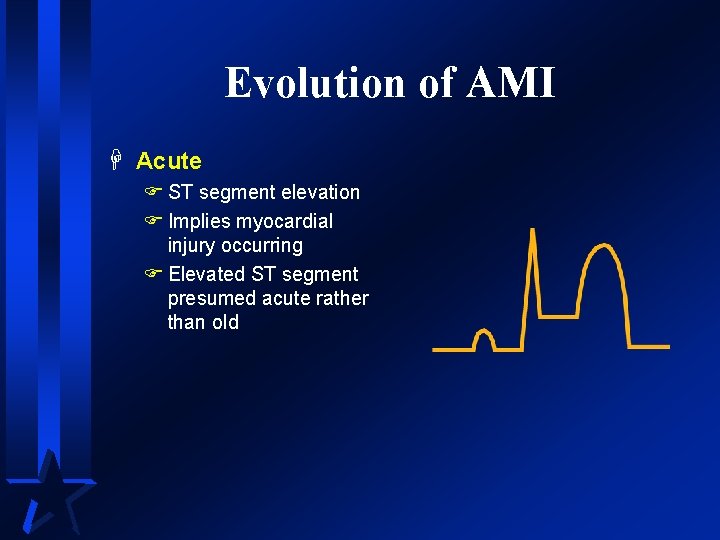
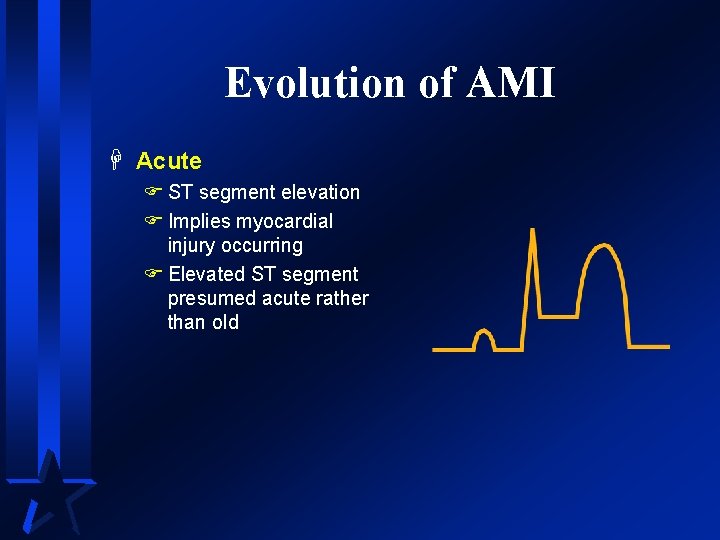
Evolution of AMI H Acute F ST segment elevation F Implies myocardial injury occurring F Elevated ST segment presumed acute rather than old
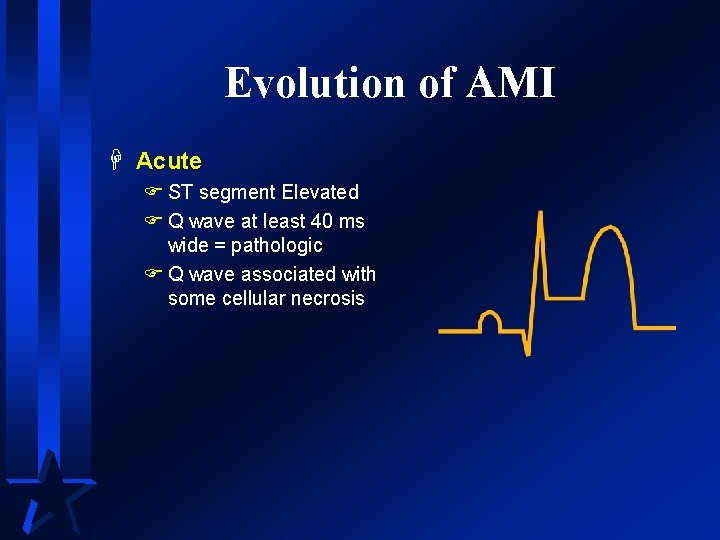
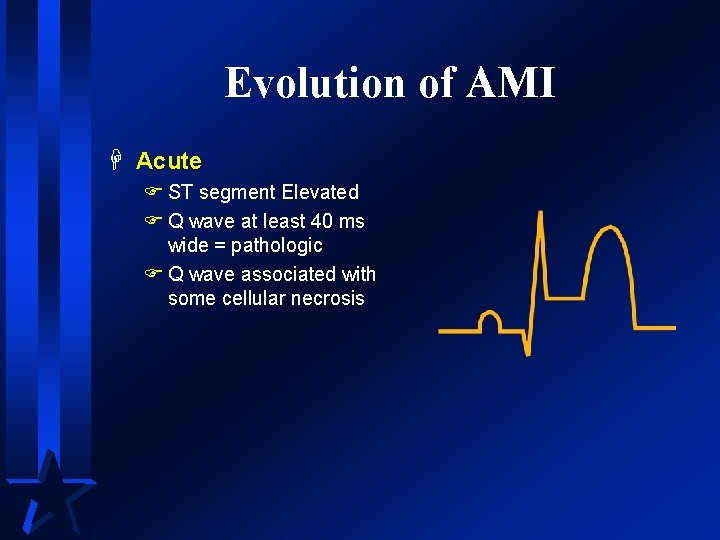
Evolution of AMI H Acute F ST segment Elevated F Q wave at least 40 ms wide = pathologic F Q wave associated with some cellular necrosis
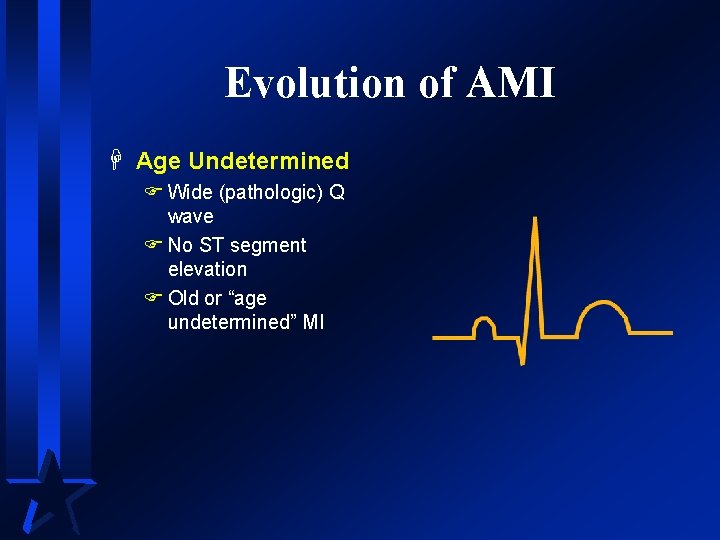
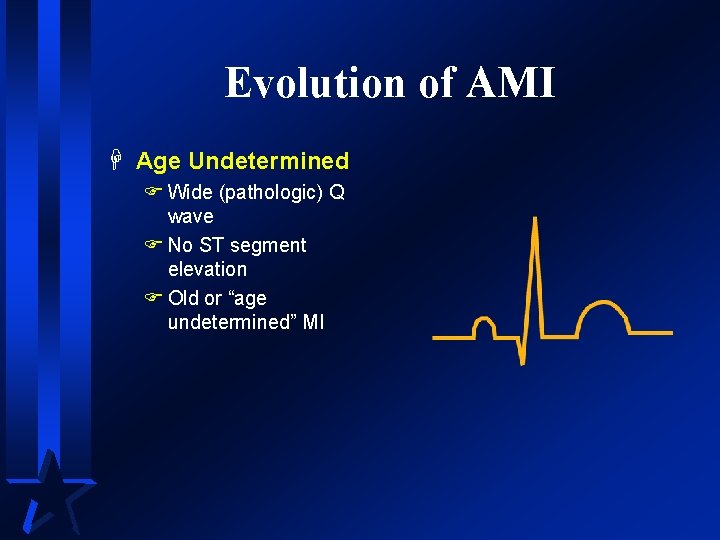
Evolution of AMI H Age Undetermined F Wide (pathologic) Q wave F No ST segment elevation F Old or “age undetermined” MI
AMI Recognition A normal 12 -lead ECG DOES NOT mean the patient is not having acute ischemia, injury or infarction!!!
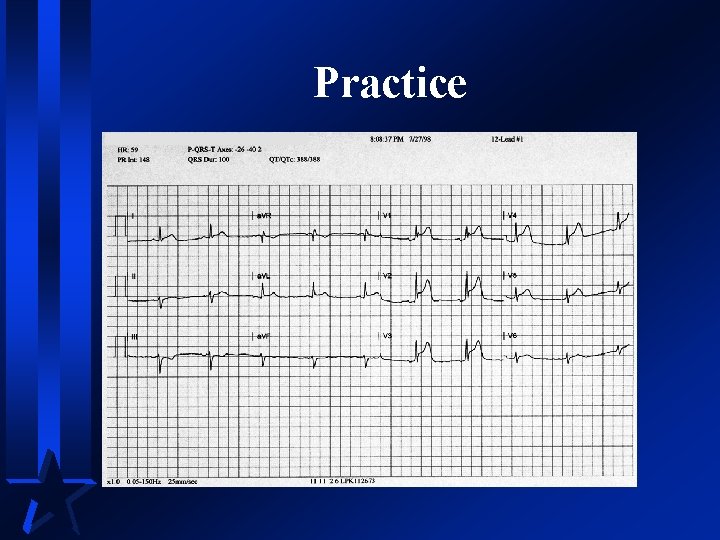
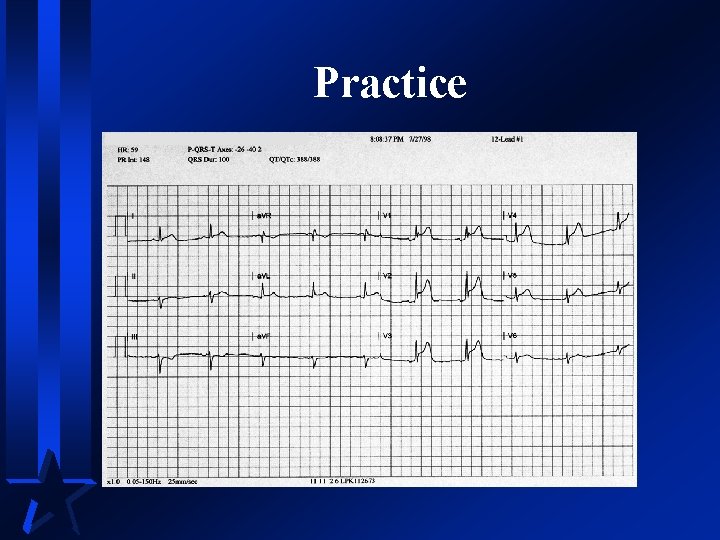
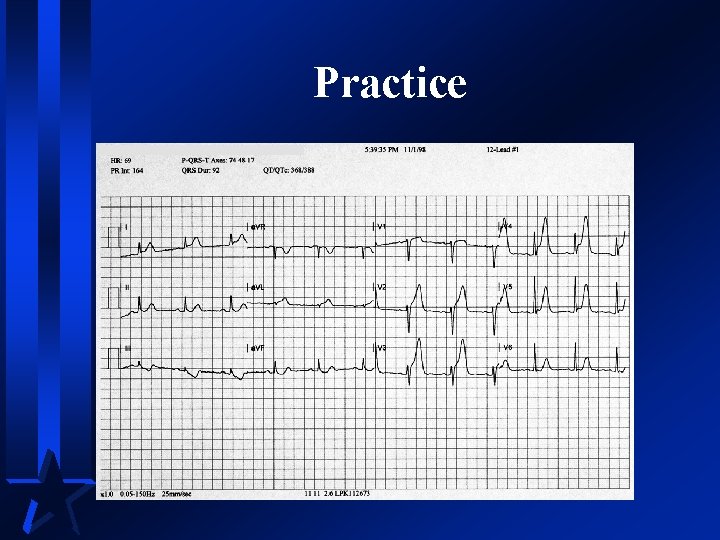
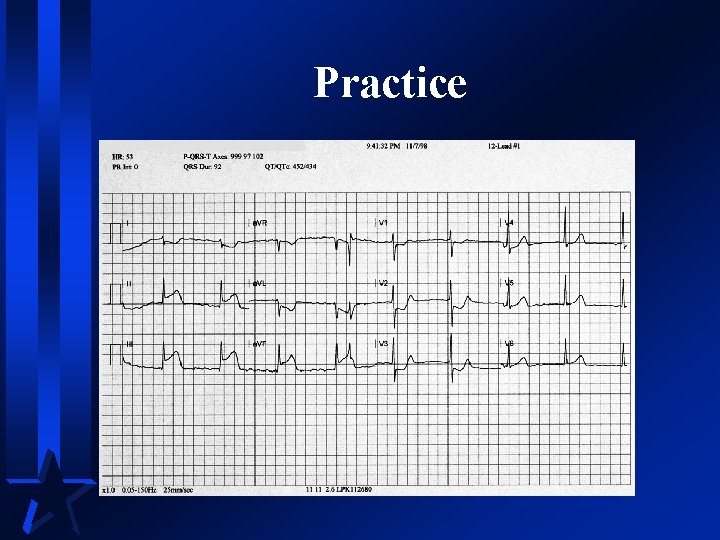
Practice
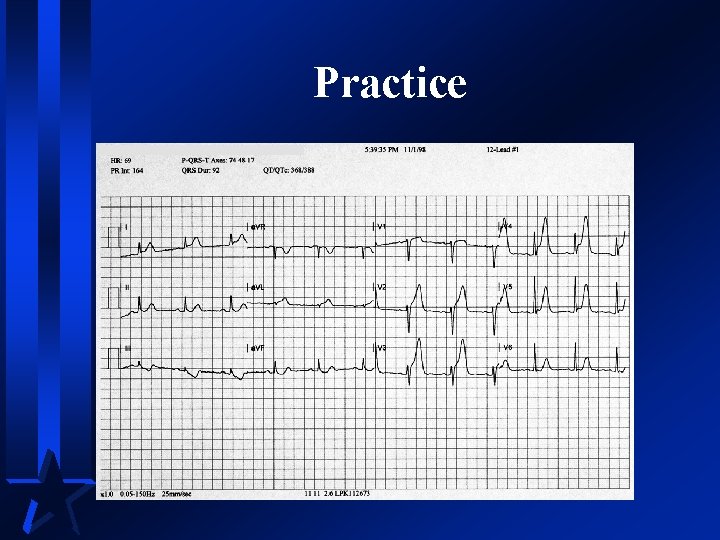
Practice
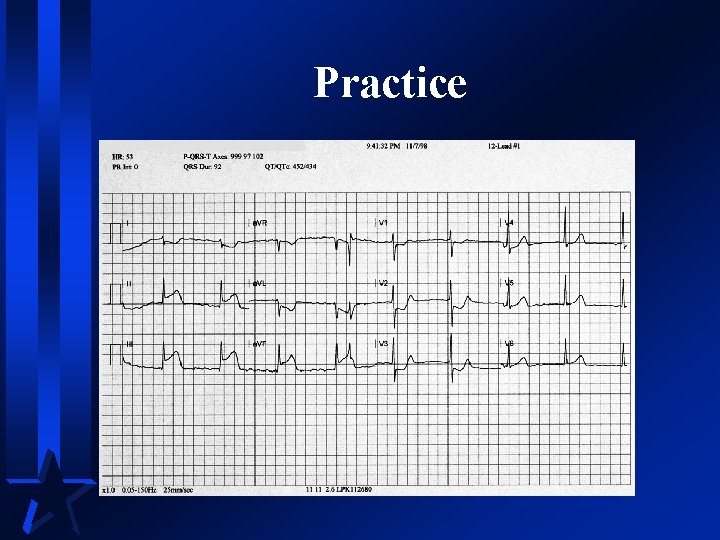
Practice
Reciprocal Changes
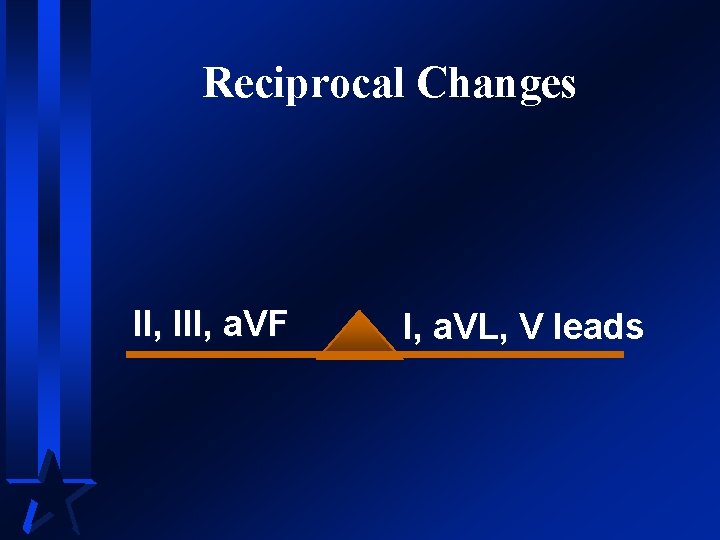
Reciprocal Changes II, III, a. VF I, a. VL, V leads
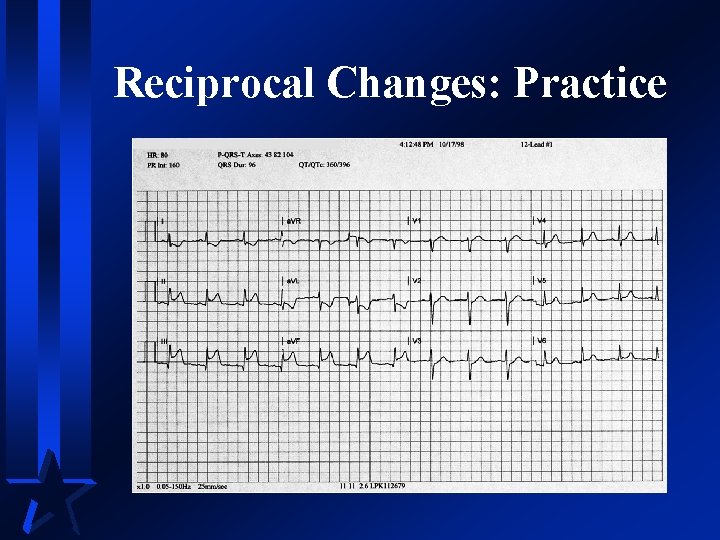
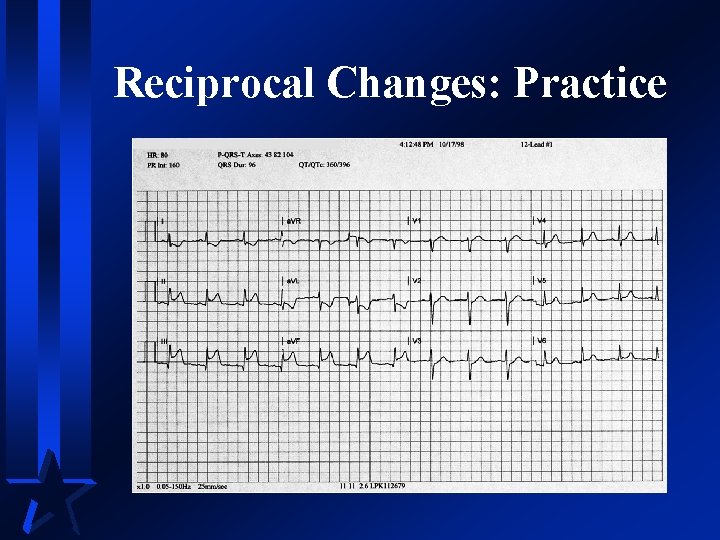
Reciprocal Changes: Practice
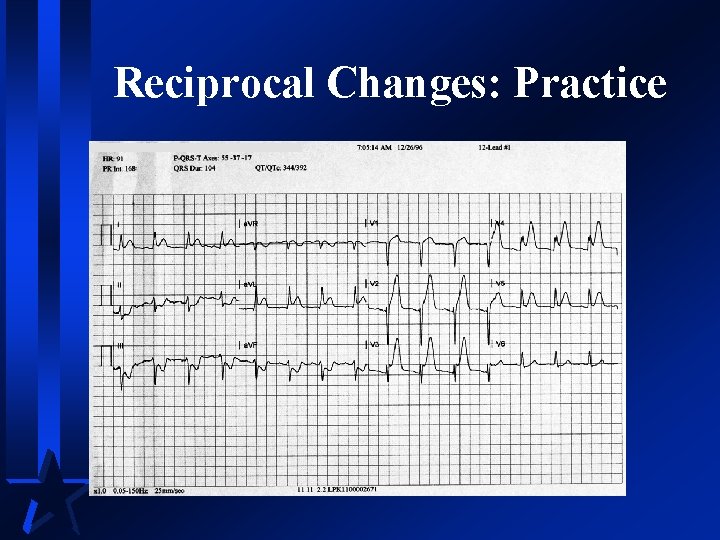
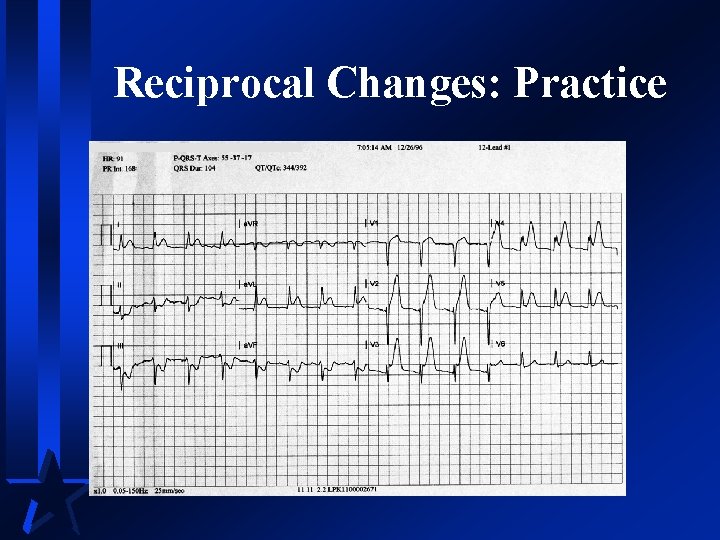
Reciprocal Changes: Practice
AMI Recognition H Reciprocal changes FNot necessary to presume infarction FStrong confirming evidence when present FNot all AMIs result in reciprocal changes
Summary H ST segment elevation is presumptive evidence for AMI H Other conditions may also cause ST elevation FKnown as Imposters
Practice Case 1 H 48 year old male F Dull central CP 2/10, began at rest H Pale and wet H Overweight, smoker H Vital signs: RR 18, P 80, BP 180/110, Sa 02 94% on room air
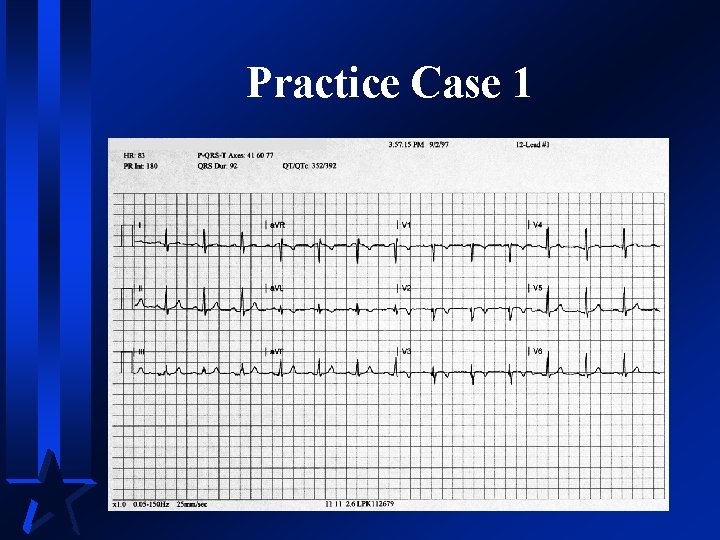
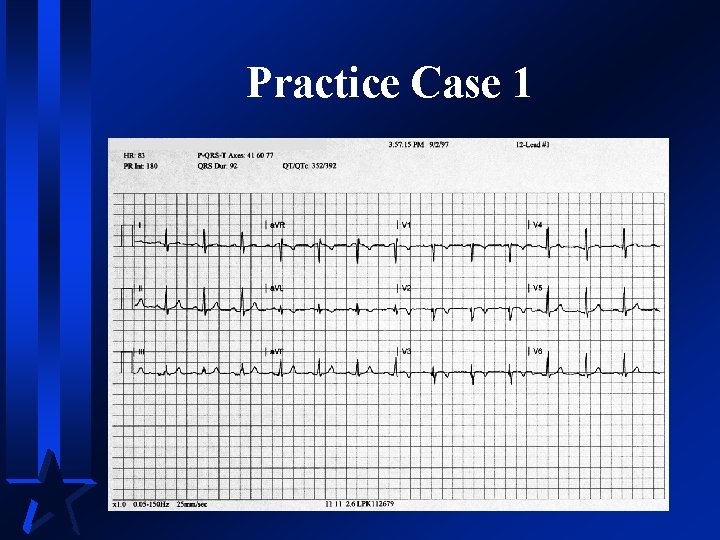
Practice Case 1
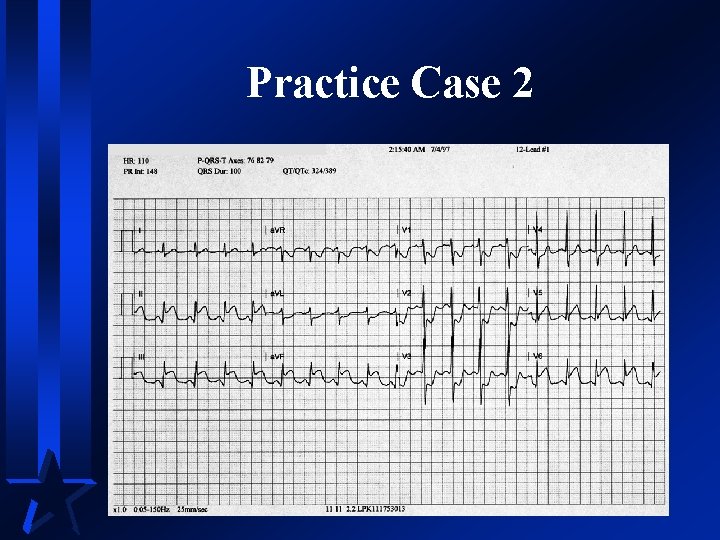
Practice Case 2 H 68 year old female F Sudden onset of anxiety and restlessness, F States she “can’t catch her breath” F Denies chest pain or other discomfort H History of IDDM and hypertension H RR 22, P 110, BP 190/90, Sa 02 88% on NC at 4 lpm
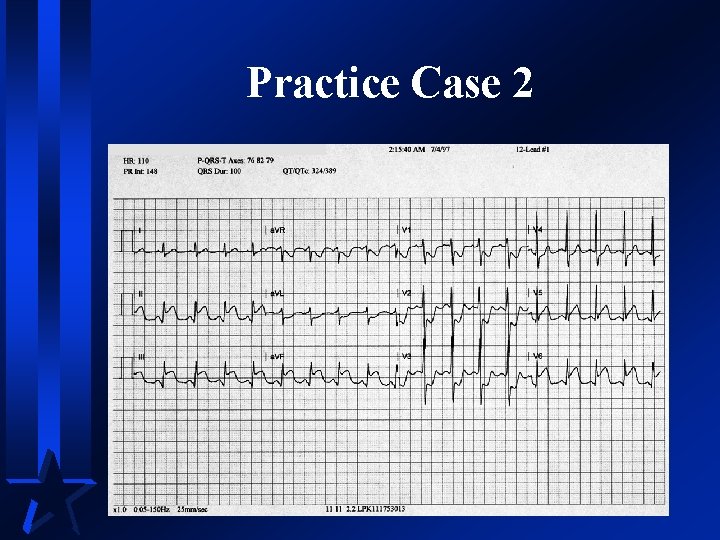
Practice Case 2
Practice Case Summary H Must take into Account FStory FRisk factors FECG FTreatment
 Ecgs
Ecgs Intentional injury examples
Intentional injury examples Normal pr interval
Normal pr interval Myocardial ischemia meaning
Myocardial ischemia meaning Q wave
Q wave Ischemia acuta degli arti
Ischemia acuta degli arti Ischemia-guided strategy
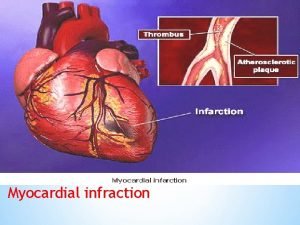
Ischemia-guided strategy Myocardial injury
Myocardial injury Pancreas wiki
Pancreas wiki Cerebral infarction
Cerebral infarction Acute pericarditis
Acute pericarditis Idioventricular rhythm ecg
Idioventricular rhythm ecg Pico question myocardial infarction
Pico question myocardial infarction Stemi location chart
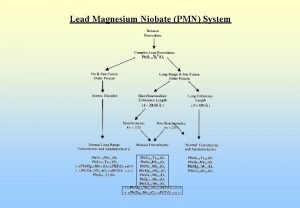
Stemi location chart Lead magnesium niobate/lead titanate
Lead magnesium niobate/lead titanate Biography of ellen g white
Biography of ellen g white Nonsense poem
Nonsense poem Teori pengambilan keputusan menurut george r terry
Teori pengambilan keputusan menurut george r terry Terry goh
Terry goh Bryan connell
Bryan connell Nttml -10v3
Nttml -10v3 Duke pre med
Duke pre med Terry geo doc download
Terry geo doc download Terry howerton
Terry howerton Trust fund terry instagram
Trust fund terry instagram Dr terry weaver
Dr terry weaver Kolokvijum na engleskom
Kolokvijum na engleskom Pbr membership
Pbr membership La direccion como proceso administrativo
La direccion como proceso administrativo Terry mc kirchy
Terry mc kirchy Terry richardson abuse
Terry richardson abuse Dr. terry wong
Dr. terry wong Tipe perencanaan asas asas manajemen
Tipe perencanaan asas asas manajemen Terry fox paragraph
Terry fox paragraph Terry cross cultural competence
Terry cross cultural competence Terry vs ohio
Terry vs ohio Terry tadlock
Terry tadlock Terry mc kirchy
Terry mc kirchy Terry laster
Terry laster Vance jennings
Vance jennings Terry holliday
Terry holliday Terry landscaping & lawn care
Terry landscaping & lawn care Terry moritz
Terry moritz Terry treasure stagg
Terry treasure stagg Christopher terry iml
Christopher terry iml Terry krupa
Terry krupa Terry betts
Terry betts Harriet josephine terry
Harriet josephine terry Arthur terry school death
Arthur terry school death Terrynazon
Terrynazon Terry roe
Terry roe Terry gage
Terry gage Terry sams
Terry sams Sleeping beauty retold by brent lansing genre
Sleeping beauty retold by brent lansing genre Terry jeffers
Terry jeffers Terry has a number cube that is numbered from 1 to 6
Terry has a number cube that is numbered from 1 to 6 Terry biddington
Terry biddington Shanna terry
Shanna terry Robotc code examples
Robotc code examples Terry goh
Terry goh