Virus Description Genus Papovaviridae Morphology Naked icosahedral 55




- Slides: 61
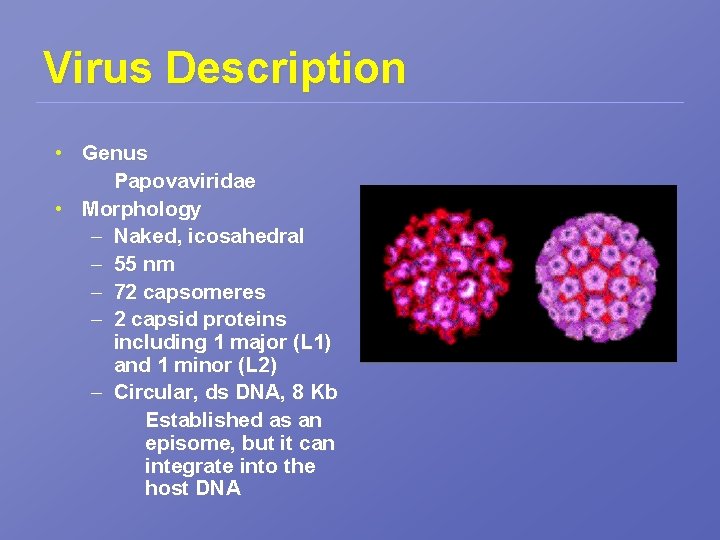
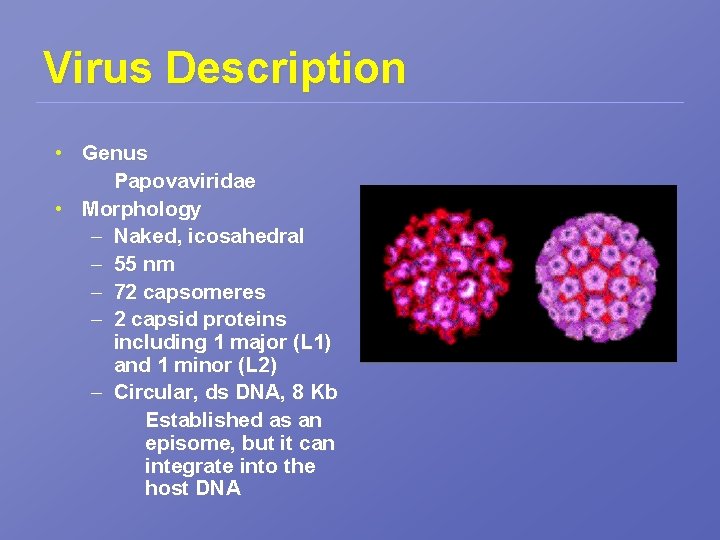
Virus Description • Genus Papovaviridae • Morphology – Naked, icosahedral – 55 nm – 72 capsomeres – 2 capsid proteins including 1 major (L 1) and 1 minor (L 2) – Circular, ds DNA, 8 Kb Established as an episome, but it can integrate into the host DNA
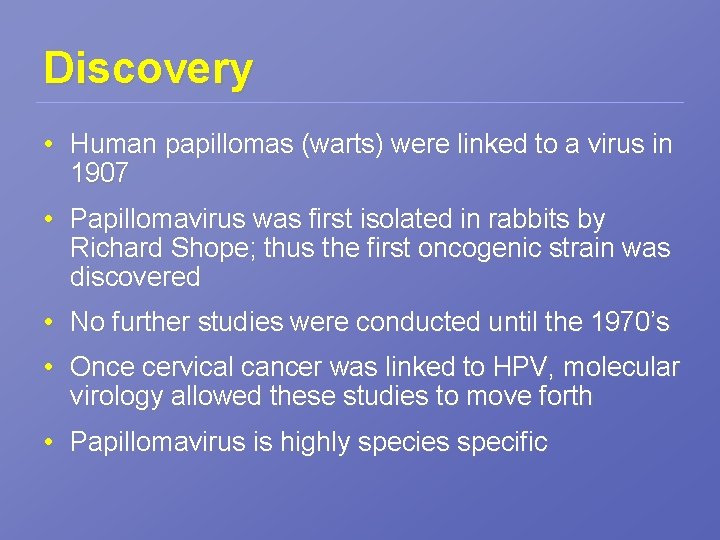
Discovery • Human papillomas (warts) were linked to a virus in 1907 • Papillomavirus was first isolated in rabbits by Richard Shope; thus the first oncogenic strain was discovered • No further studies were conducted until the 1970’s • Once cervical cancer was linked to HPV, molecular virology allowed these studies to move forth • Papillomavirus is highly species specific
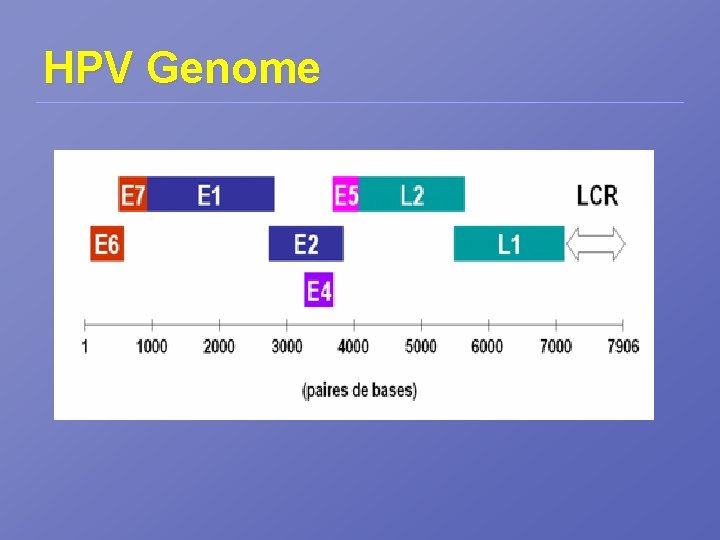
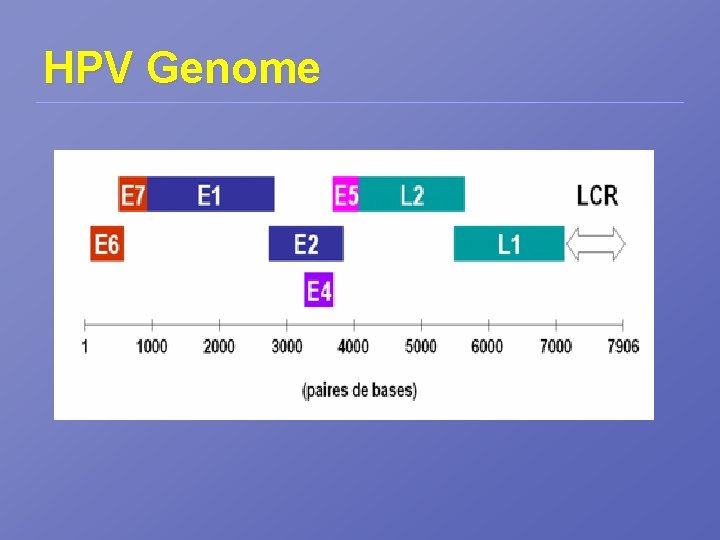
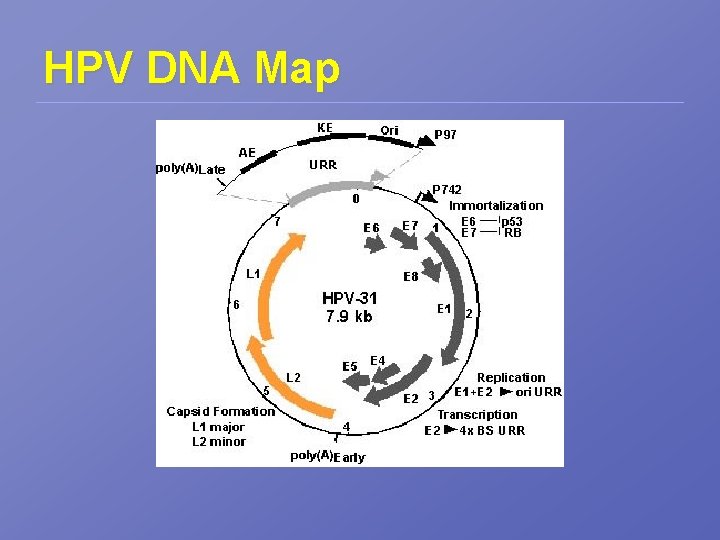
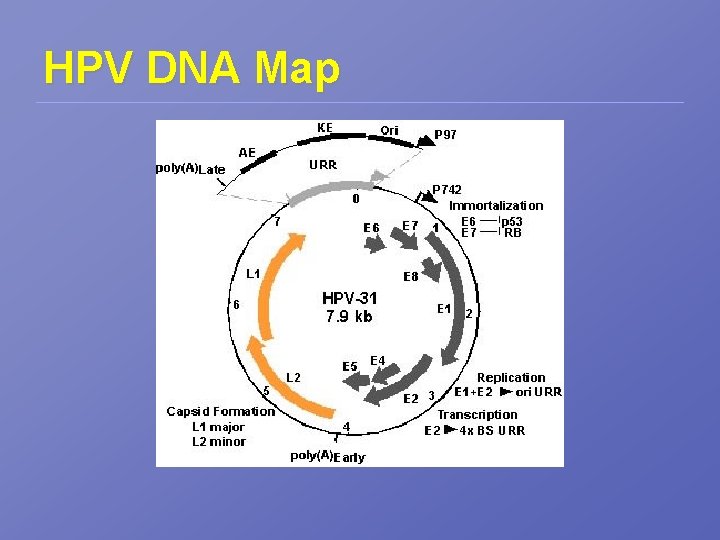
HPV Genome
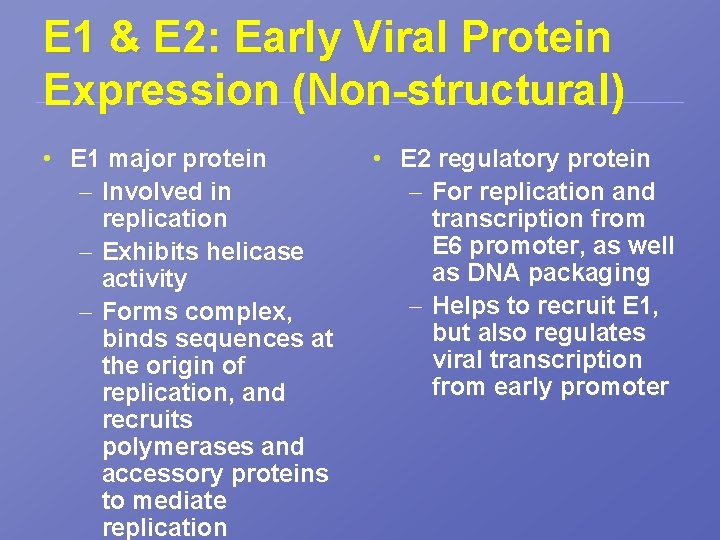
E 1 & E 2: Early Viral Protein Expression (Non-structural) • E 1 major protein – Involved in replication – Exhibits helicase activity – Forms complex, binds sequences at the origin of replication, and recruits polymerases and accessory proteins to mediate replication • E 2 regulatory protein – For replication and transcription from E 6 promoter, as well as DNA packaging – Helps to recruit E 1, but also regulates viral transcription from early promoter
E 4 & E 5 • The functions of E 4 & E 5 are not fully understood; however, they may be involved in late viral functions
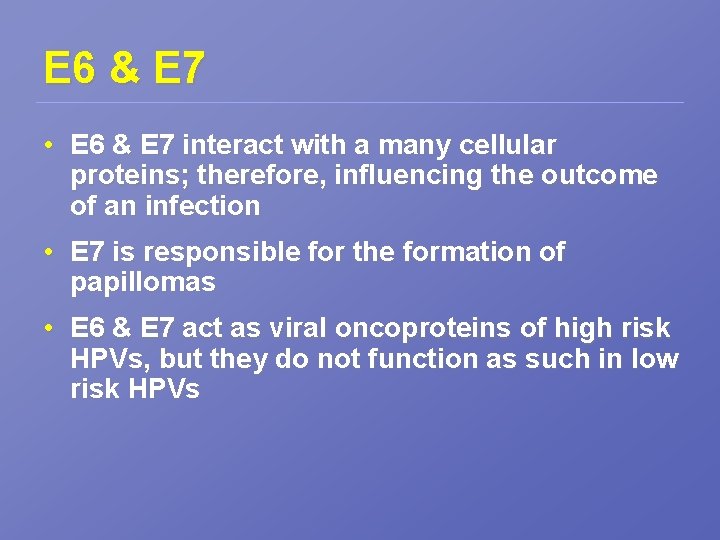
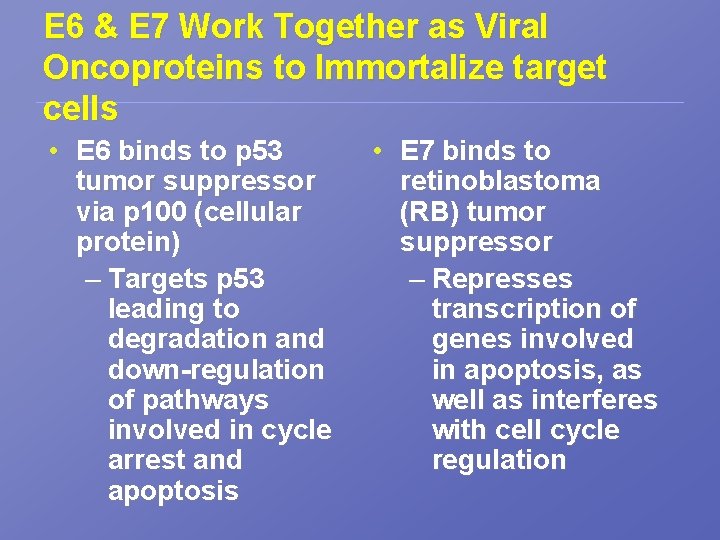
E 6 & E 7 • E 6 & E 7 interact with a many cellular proteins; therefore, influencing the outcome of an infection • E 7 is responsible for the formation of papillomas • E 6 & E 7 act as viral oncoproteins of high risk HPVs, but they do not function as such in low risk HPVs

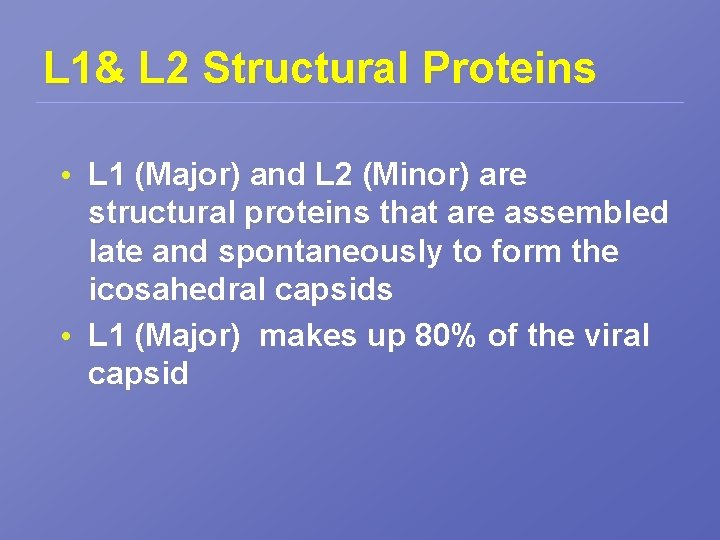
L 1& L 2 Structural Proteins • L 1 (Major) and L 2 (Minor) are structural proteins that are assembled late and spontaneously to form the icosahedral capsids • L 1 (Major) makes up 80% of the viral capsid
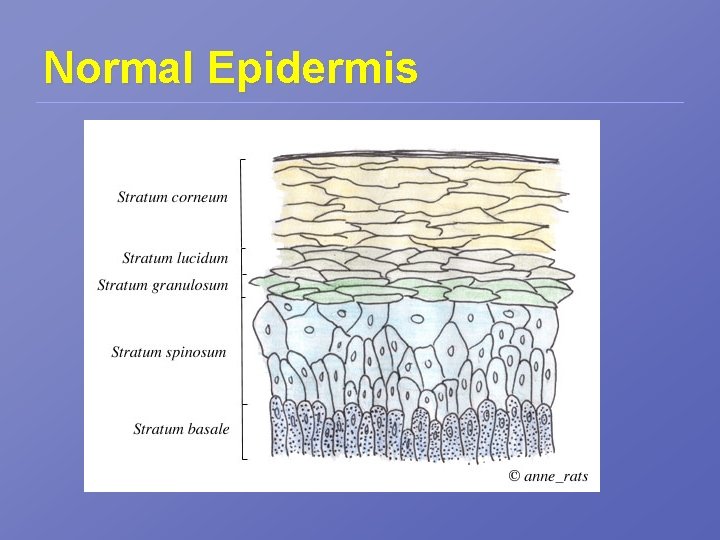
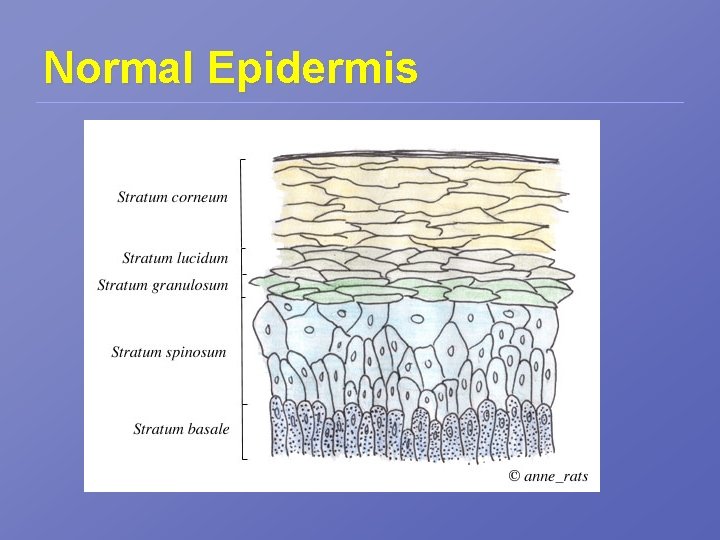
Normal Epidermis
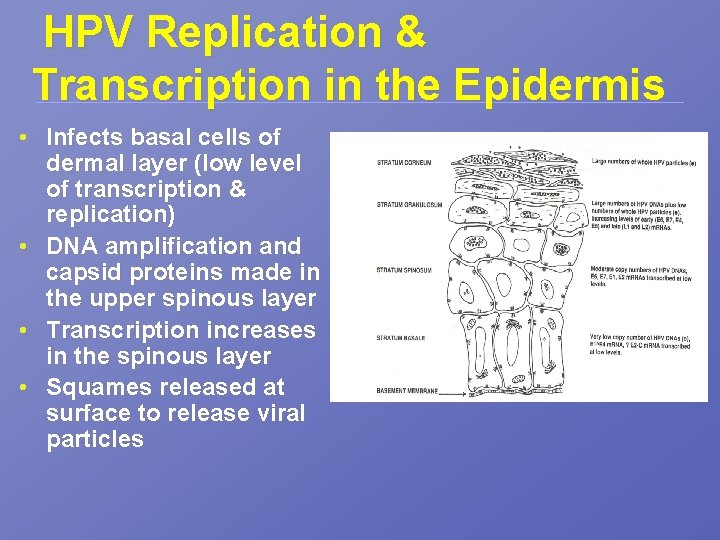
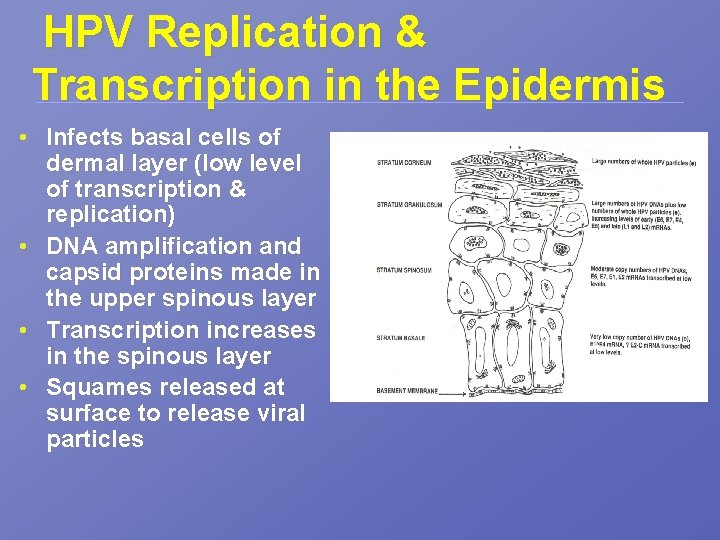
HPV Replication & Transcription in the Epidermis • Infects basal cells of dermal layer (low level of transcription & replication) • DNA amplification and capsid proteins made in the upper spinous layer • Transcription increases in the spinous layer • Squames released at surface to release viral particles
E 6 & E 7 Work Together as Viral Oncoproteins to Immortalize target cells • E 6 binds to p 53 tumor suppressor via p 100 (cellular protein) – Targets p 53 leading to degradation and down-regulation of pathways involved in cycle arrest and apoptosis • E 7 binds to retinoblastoma (RB) tumor suppressor – Represses transcription of genes involved in apoptosis, as well as interferes with cell cycle regulation
HPV DNA Map
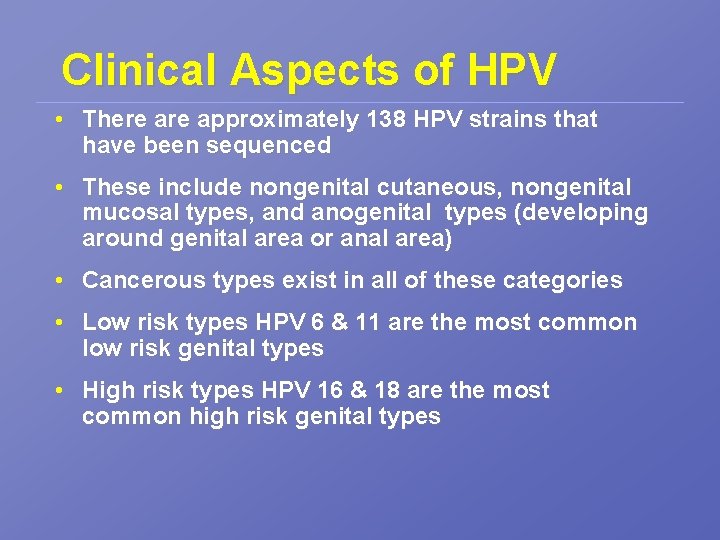
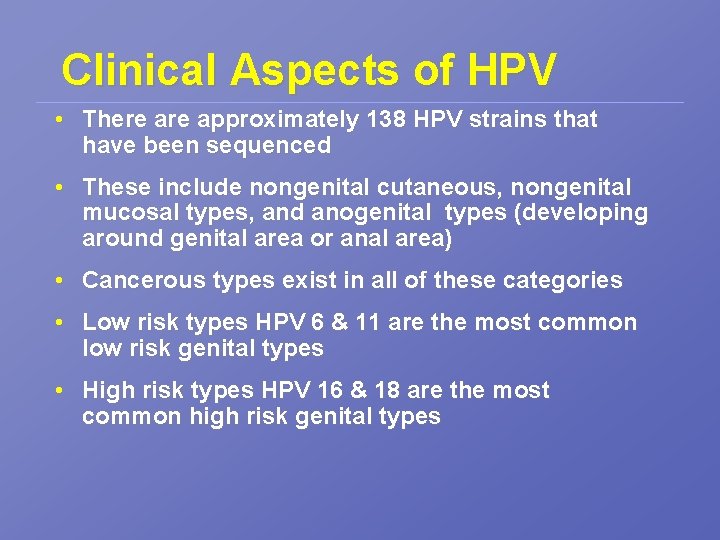
Clinical Aspects of HPV • There approximately 138 HPV strains that have been sequenced • These include nongenital cutaneous, nongenital mucosal types, and anogenital types (developing around genital area or anal area) • Cancerous types exist in all of these categories • Low risk types HPV 6 & 11 are the most common low risk genital types • High risk types HPV 16 & 18 are the most common high risk genital types
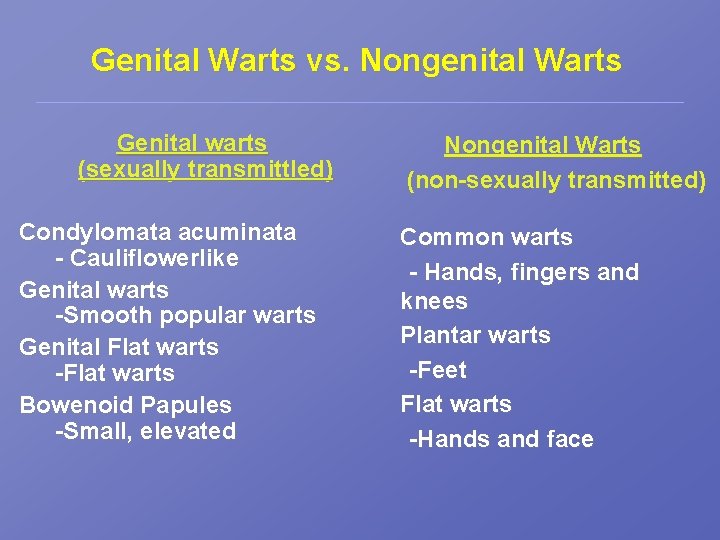
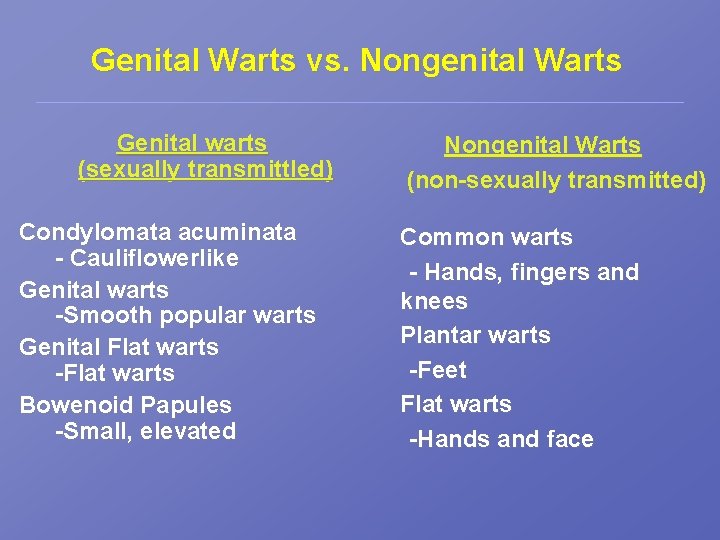
Genital Warts vs. Nongenital Warts Genital warts (sexually transmittled) Condylomata acuminata - Cauliflowerlike Genital warts -Smooth popular warts Genital Flat warts -Flat warts Bowenoid Papules -Small, elevated Nongenital Warts (non-sexually transmitted) Common warts - Hands, fingers and knees Plantar warts -Feet Flat warts -Hands and face
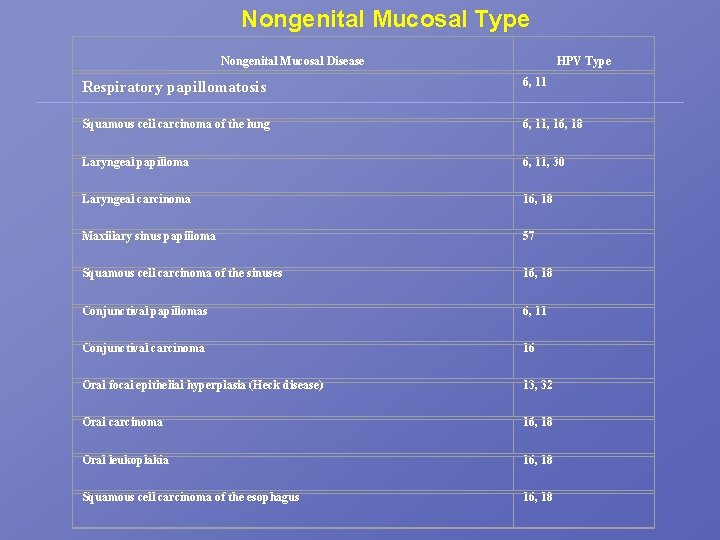
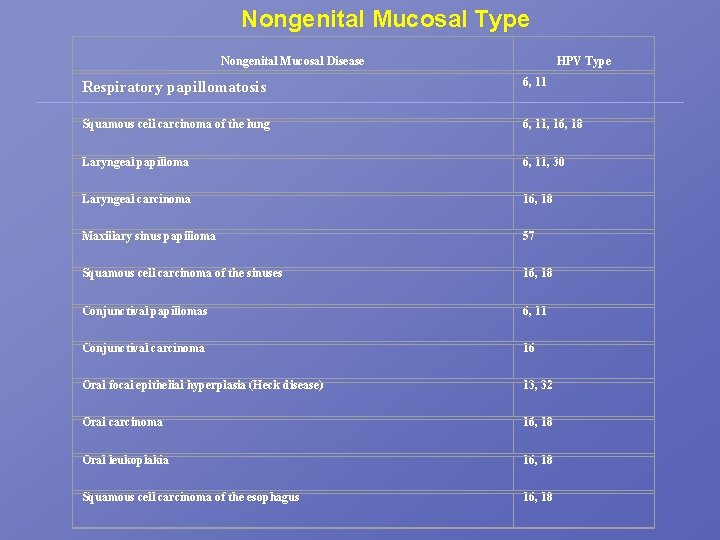
Nongenital Mucosal Type Nongenital Mucosal Disease HPV Type Respiratory papillomatosis 6, 11 Squamous cell carcinoma of the lung 6, 11, 16, 18 Laryngeal papilloma 6, 11, 30 Laryngeal carcinoma 16, 18 Maxillary sinus papilloma 57 Squamous cell carcinoma of the sinuses 16, 18 Conjunctival papillomas 6, 11 Conjunctival carcinoma 16 Oral focal epithelial hyperplasia (Heck disease) 13, 32 Oral carcinoma 16, 18 Oral leukoplakia 16, 18 Squamous cell carcinoma of the esophagus 16, 18
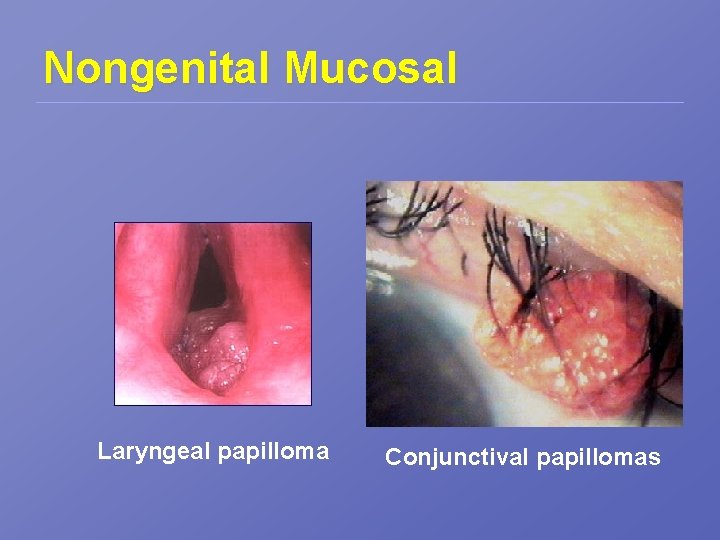
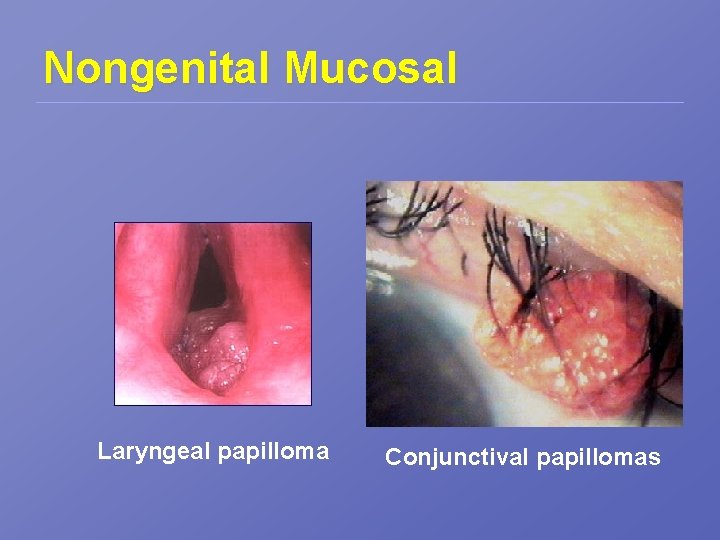
Nongenital Mucosal Laryngeal papilloma Conjunctival papillomas
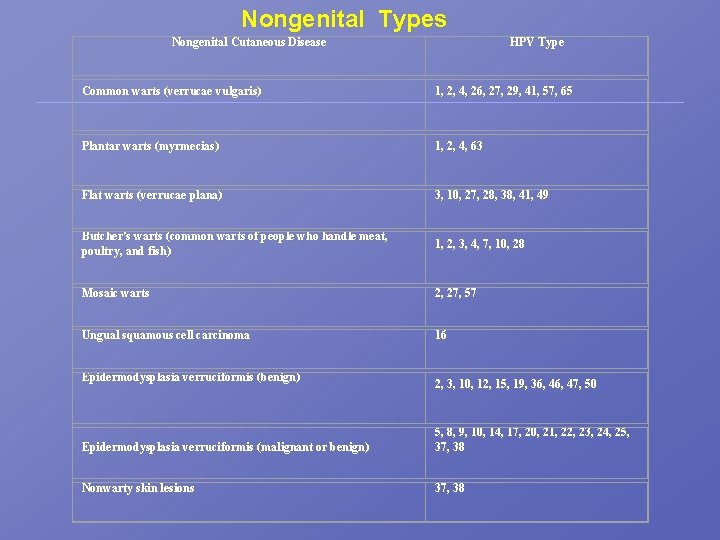
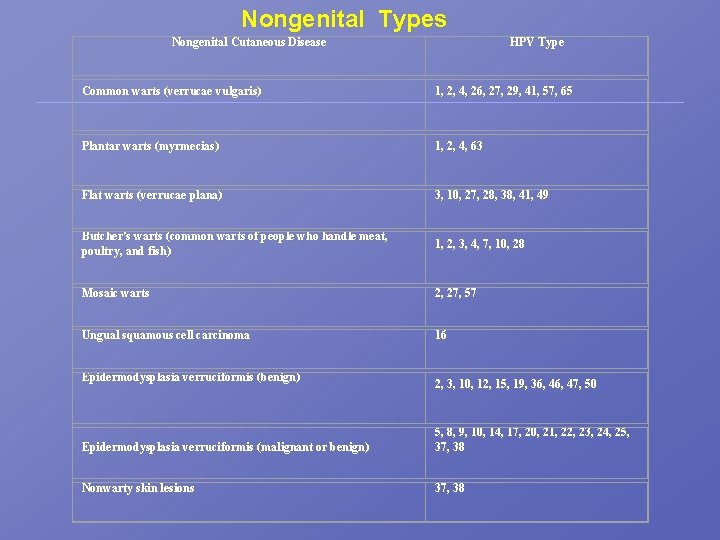
Nongenital Types Nongenital Cutaneous Disease HPV Type Common warts (verrucae vulgaris) 1, 2, 4, 26, 27, 29, 41, 57, 65 Plantar warts (myrmecias)) 1, 2, 4, 63 Flat warts (verrucae plana) 3, 10, 27, 28, 38, 41, 49 Butcher's warts (common warts of people who handle meat, poultry, and fish) 1, 2, 3, 4, 7, 10, 28 Mosaic warts 2, 27, 57 Ungual squamous cell carcinoma 16 Epidermodysplasia verruciformis (benign) 2, 3, 10, 12, 15, 19, 36, 47, 50 Epidermodysplasia verruciformis (malignant or benign) 5, 8, 9, 10, 14, 17, 20, 21, 22, 23, 24, 25, 37, 38 Nonwarty skin lesions 37, 38

Common & Plantar Warts
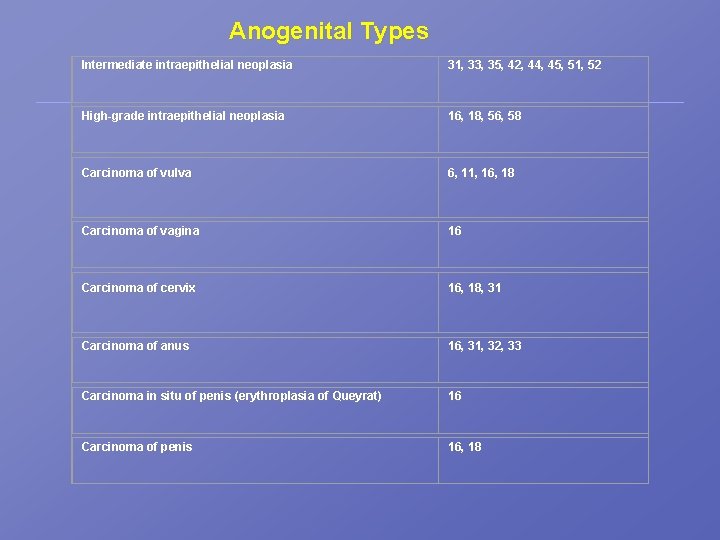
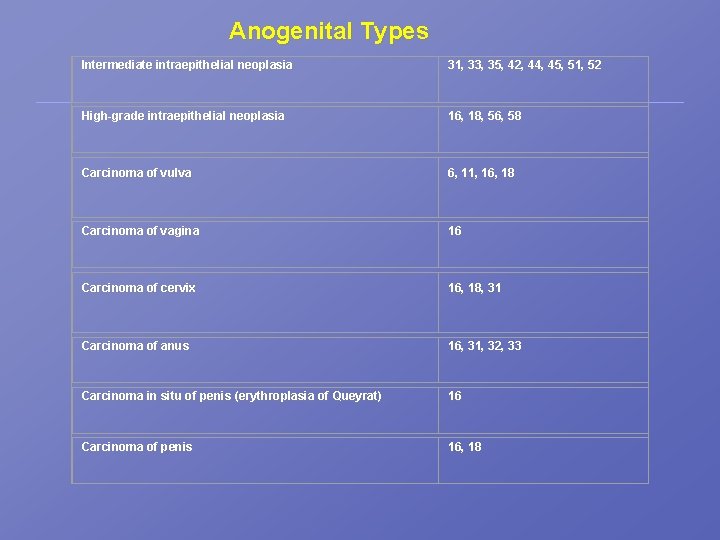
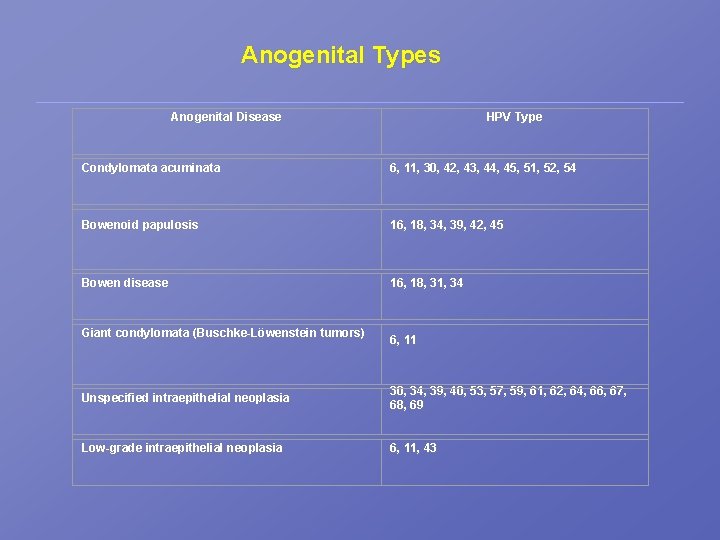
Anogenital Types Intermediate intraepithelial neoplasia 31, 33, 35, 42, 44, 45, 51, 52 High-grade intraepithelial neoplasia 16, 18, 56, 58 Carcinoma of vulva 6, 11, 16, 18 Carcinoma of vagina 16 Carcinoma of cervix 16, 18, 31 Carcinoma of anus 16, 31, 32, 33 Carcinoma in situ of penis (erythroplasia of Queyrat) 16 Carcinoma of penis 16, 18
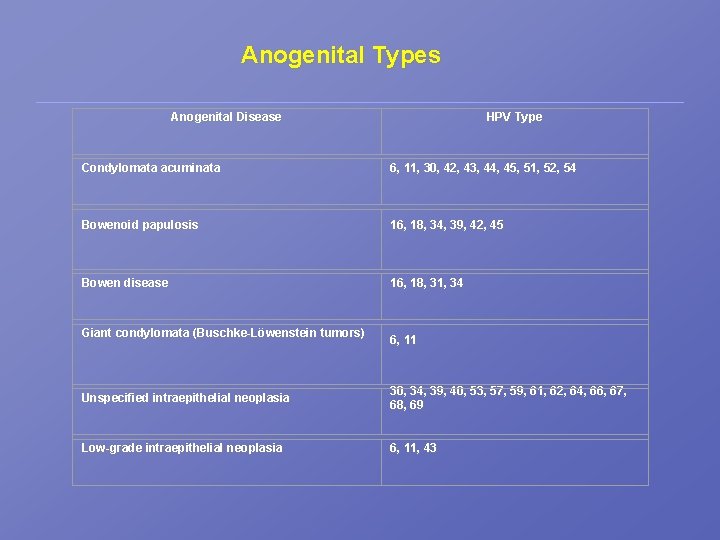
Anogenital Types Anogenital Disease HPV Type Condylomata acuminata 6, 11, 30, 42, 43, 44, 45, 51, 52, 54 Bowenoid papulosis 16, 18, 34, 39, 42, 45 Bowen disease 16, 18, 31, 34 Giant condylomata (Buschke-Löwenstein tumors) 6, 11 Unspecified intraepithelial neoplasia 30, 34, 39, 40, 53, 57, 59, 61, 62, 64, 66, 67, 68, 69 Low-grade intraepithelial neoplasia 6, 11, 43

Genital Warts
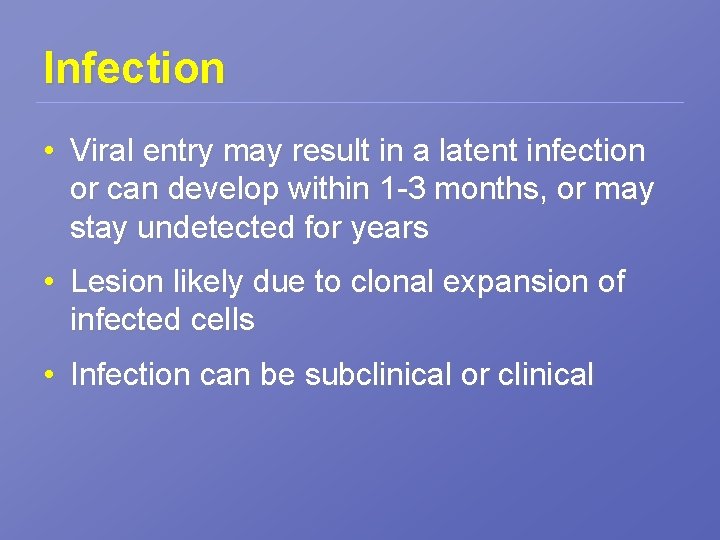
Infection • Viral entry may result in a latent infection or can develop within 1 -3 months, or may stay undetected for years • Lesion likely due to clonal expansion of infected cells • Infection can be subclinical or clinical
Transmission • HPV is released from the desquamating superficial keratinocytes of the infected stratified epithelia • Transmission of cutaneous HPVs occurs through direct contact with infected tissue or through indirect contact with contaminated objects and surfaces such as poolsides • Transmission of genital HPV typically occurs through sexual contact
HPV & Cervical Disease • 99. 7 % of cervical cancers are a result of HPV-16 & HPV-18 • HPV infection of the cervix corresponds to low-grade CIN (Cervical intraepithelial Neoplasia) – mostly flat aceto-whitening areas including flat condyloma
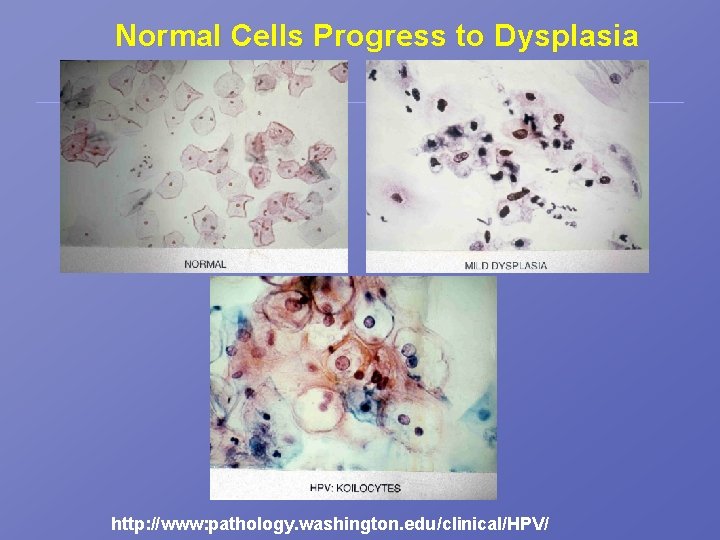
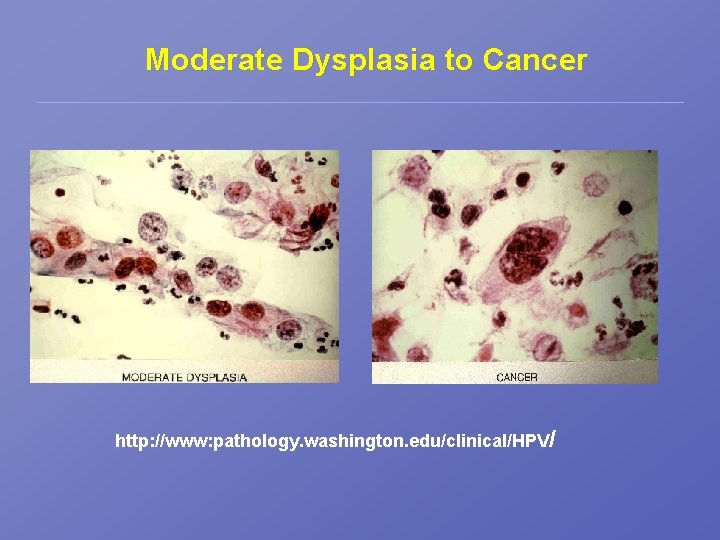
Progressive Cervical Disease • Starts as a benign noninvasive or squamous intraepithelial lesion (SIL) or CIN • Most low-grade intraepithelial lesions regress; however, some remain unchanged • 10 -15% progress to moderate or severe dysplasia; carcinoma in situ • High grade CIN may develop into invasive cancer after years or decades – HPV 16, 18, and 45 are the most prevalent detected
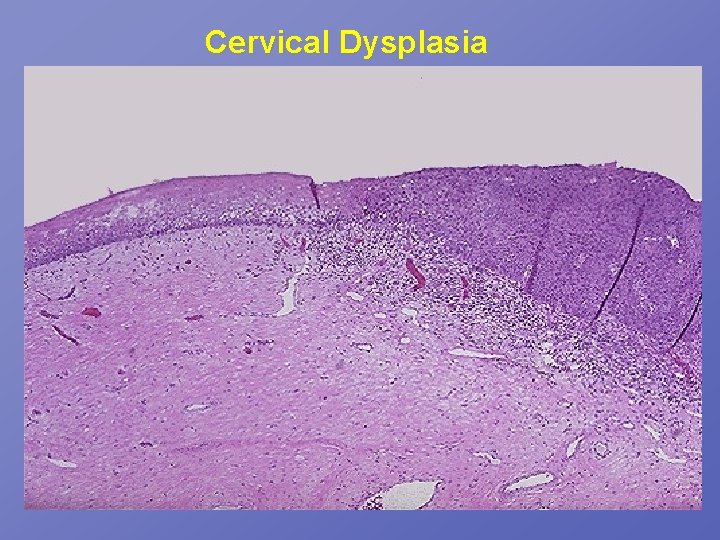
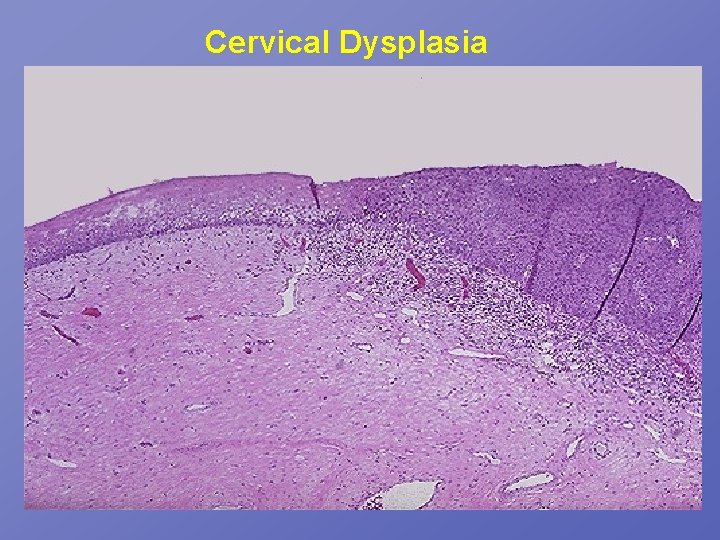
Cervical Dysplasia
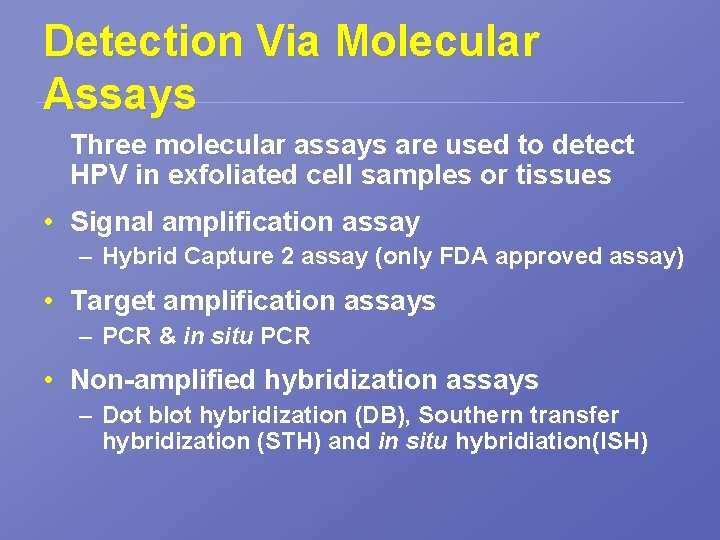
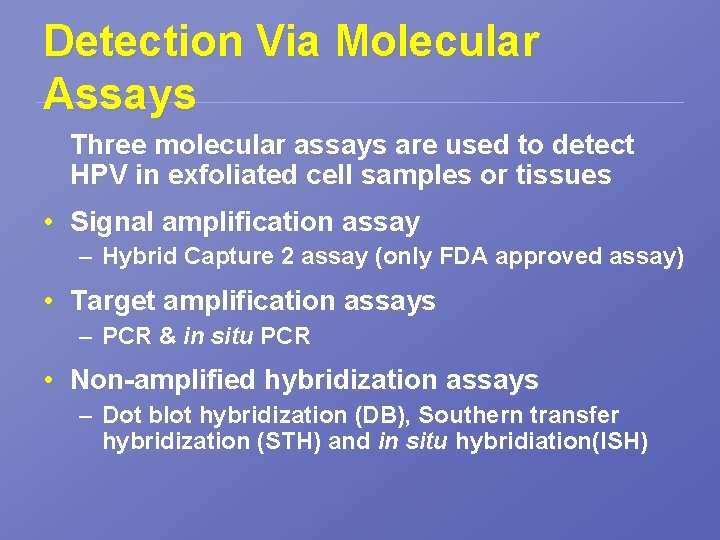
Detection Via Molecular Assays Three molecular assays are used to detect HPV in exfoliated cell samples or tissues • Signal amplification assay – Hybrid Capture 2 assay (only FDA approved assay) • Target amplification assays – PCR & in situ PCR • Non-amplified hybridization assays – Dot blot hybridization (DB), Southern transfer hybridization (STH) and in situ hybridiation(ISH)
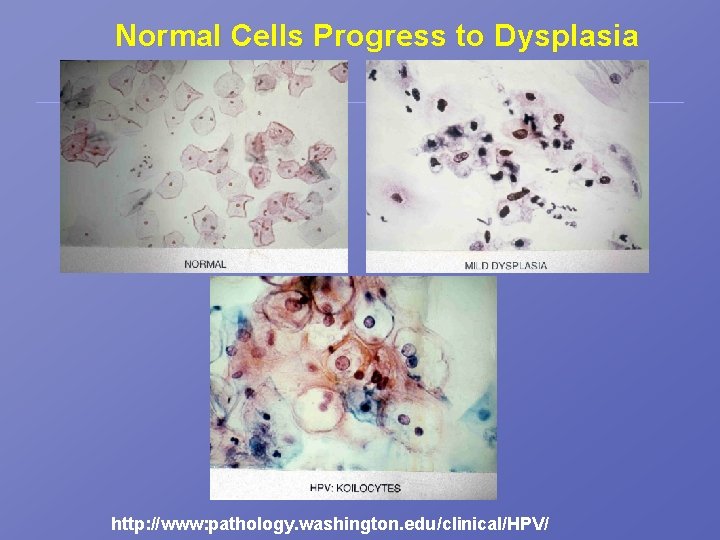
Normal Cells Progress to Dysplasia http: //www: pathology. washington. edu/clinical/HPV/
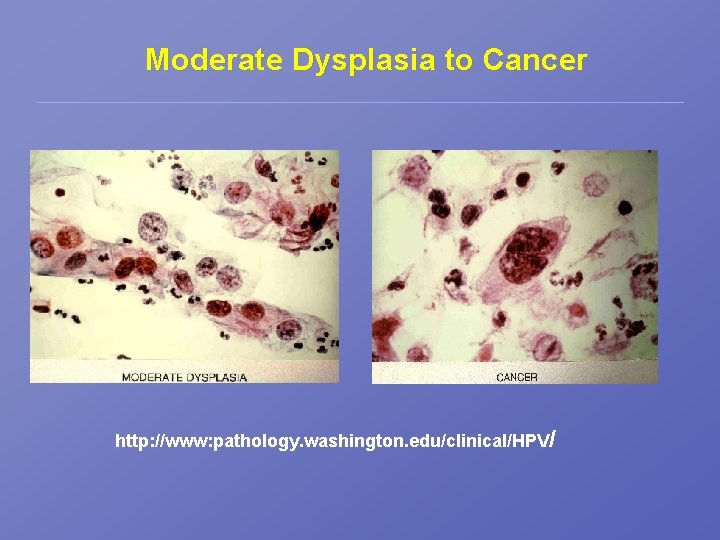
Moderate Dysplasia to Cancer http: //www: pathology. washington. edu/clinical/HPV/
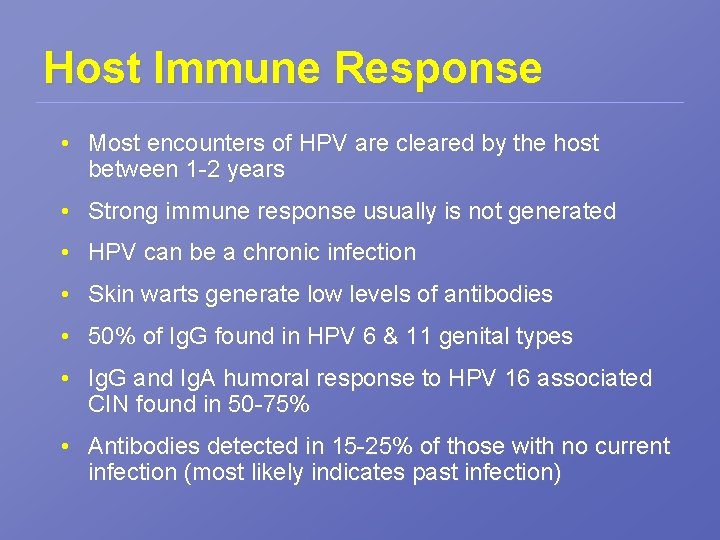
Host Immune Response • Most encounters of HPV are cleared by the host between 1 -2 years • Strong immune response usually is not generated • HPV can be a chronic infection • Skin warts generate low levels of antibodies • 50% of Ig. G found in HPV 6 & 11 genital types • Ig. G and Ig. A humoral response to HPV 16 associated CIN found in 50 -75% • Antibodies detected in 15 -25% of those with no current infection (most likely indicates past infection)
Host Immune Response • Antibodies are rarely detected in patients with premalignant cervical lesions • Antibodies detected in 50% of women with latestage invasive HPV-16 associated with cervical carcinoma • Cell mediated immunity (CMI) is probably extensively involved in control of the infection – High incidence of cutaneous and anogenital HPV associated disease is observed among patients with genetic or aquired CMI deficiencies
Host Immune Response • Immunological and genetic aspects likely to attribute to persistence and progression of CIN – Higher frequency found in HIV infected women • Functional alterations of LCs have been shown to correspond with initiation and progression of HPV related cervical disease
History of HPV Detection • 1927 Georges Papanicalaou did research on diagnostic cytology of the cervix • 1940 s His research was published. First Paps were in Korea • 1950 s Paps began being used widely • 1975 Harold zur Hausen linked HPV with cervical cancer • 1980 s His team isolated several genotypes linked to cervical cancer and genital warts • 1999 PCR assay found HPV DNA in 99. 7% of cervical cancers studied
Genital HPV Types • Only 40 types of HPV infect the genital tract • Only these types can lead cause carcinoma: – Types 16, 31, 33, 35, 52, 58 – Types 18, 39, 45, 70 (flat – in cervix, create tumors) • Infections with certain “high-risk” HPV types can progress to dysphasias or cancer of the cervix, penis, anus, vagina and tonsils.
Prevalence of HPV • HPV can show up in women on the cervix and the vulva, inside the surrounding areas of the vagina, and anus. • It is common for HPV to exhibit no symptoms • HPV can be acquired and cleared without the person ever knowing that they were infected • HPV is commonly passed unintentionally by people who have no symptoms • This is one reason why HPV is so common.
Most Women will be Infected • HPV infection is estimated to involve 80% of the sexually active population. • As sexually active people you will probably contract HPV at some point in your life. • 3 of 4 Americans between the ages of 15 and 50 have been infected with HPV at some point. • Your immune system will most likely clear it. • HPV represents the most common sexually transmitted viruses.
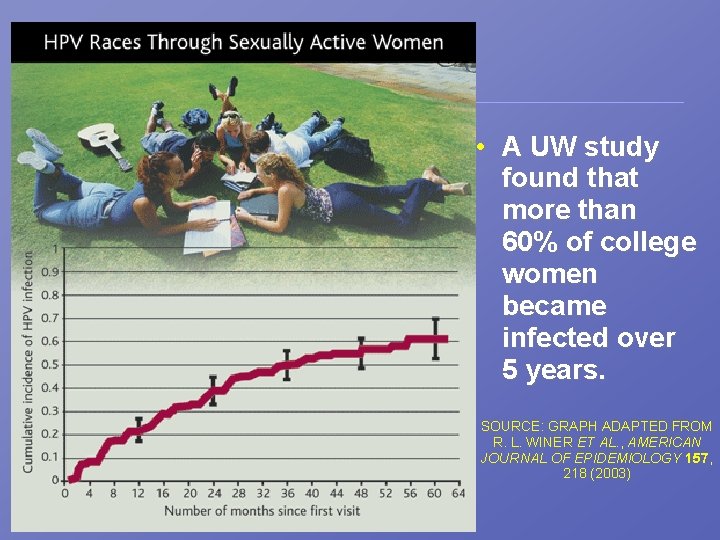
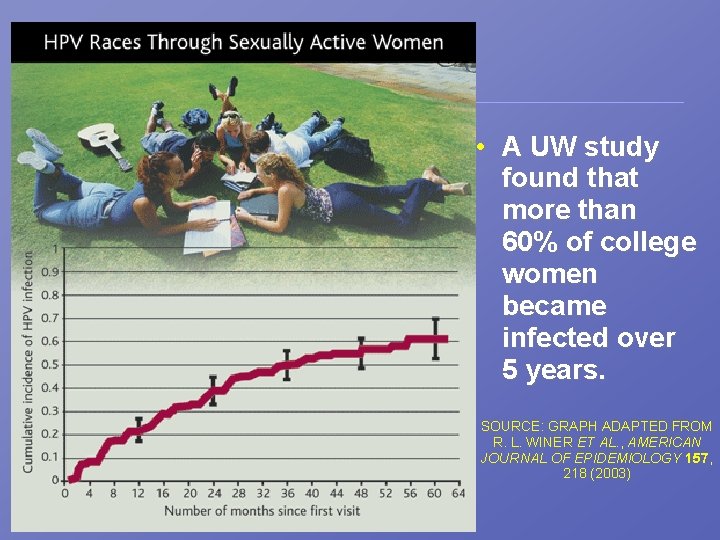
UW Students • A UW study found that more than 60% of college women became infected over 5 years. SOURCE: GRAPH ADAPTED FROM R. L. WINER ET AL. , AMERICAN JOURNAL OF EPIDEMIOLOGY 157, 218 (2003)
HPV Persistence • Most young women clear the virus, but it is unknown how many completely clear it. • Some HPV may go into remission after an active period of months or years, but they are not usually fully eliminated. – “Active viral infections typically re-emerge from latency during transient or permanent immunodeficiency associated with sunburn, pregnancy, physical and emotional stress, HIV infection and cancer chemotherapy. ” (WSDOH) • There is no way to tell how long you have been infected or when HPV will express.
Men and HPV • Men also harbour and express HPV in the form of penile, perennial and urethral papillomas. • Men are much more likely to be carriers and not develop cancer. • A urethral swab for males to collect exfoliated cells for Pap analysis exists but rarely practiced. • There is not a FDA approved test for men. • Clinically it is hard to get men in to get tested.
HPV Infection in the US • An estimated 5. 5 million people become infected with various types of HPV each year in the U. S. • An estimated 20 million people are currently infected with at least one HPV type in the U. S. • The “high risk” HPV associated cancers can take years to develop, upwards of 10 to 20 years. • Cervical cancer affects younger women more frequently than most other types of cancer.
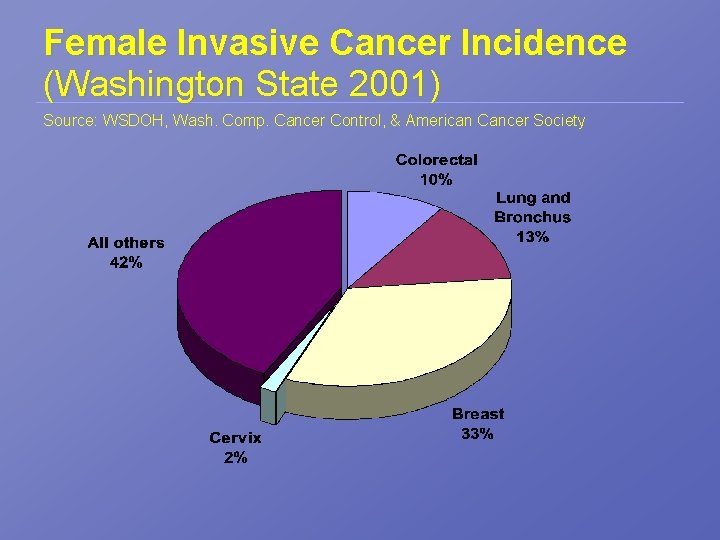
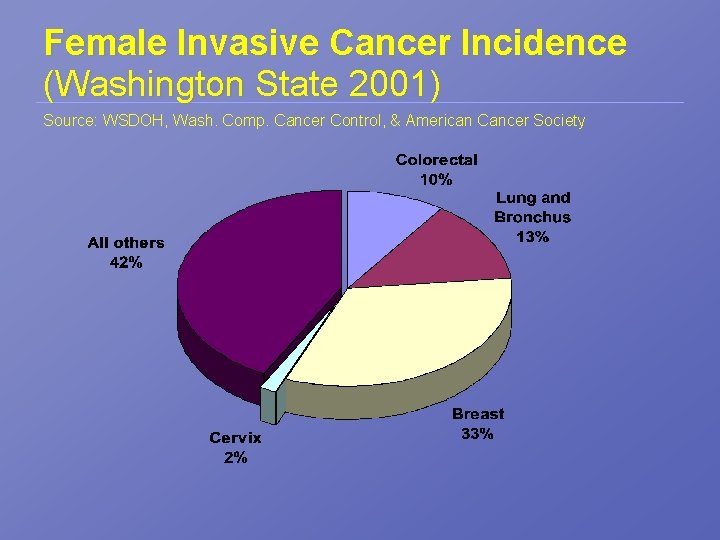
Female Invasive Cancer Incidence (Washington State 2001) Source: WSDOH, Wash. Comp. Cancer Control, & American Cancer Society
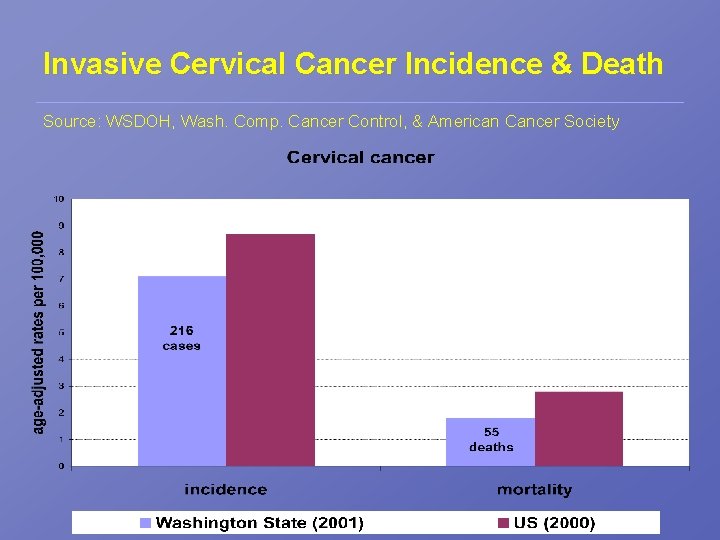
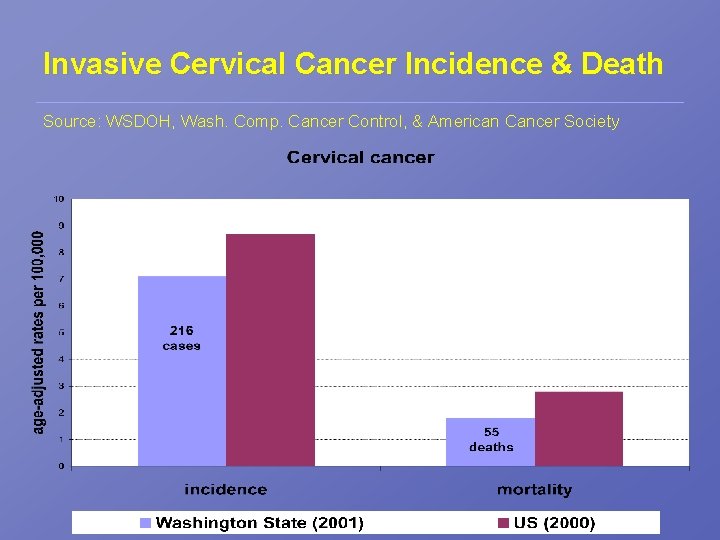
Invasive Cervical Cancer Incidence & Death Source: WSDOH, Wash. Comp. Cancer Control, & American Cancer Society
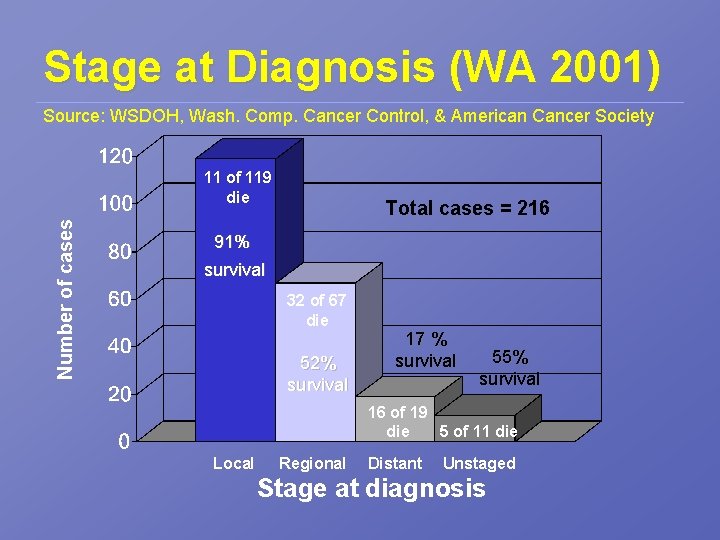
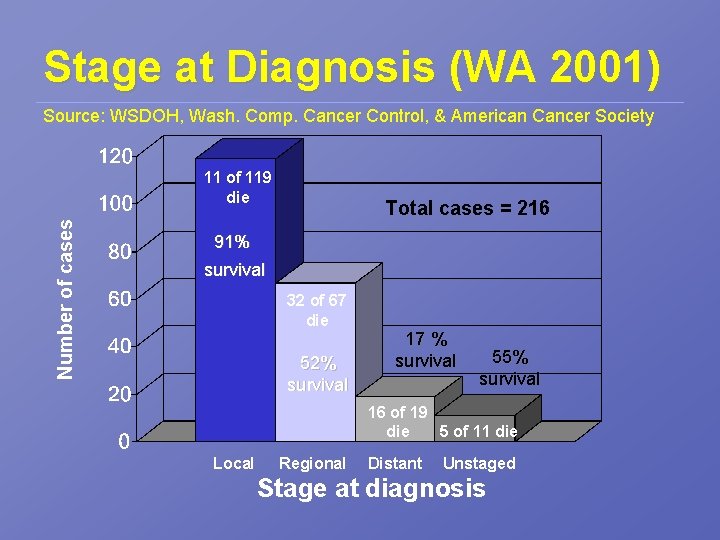
Stage at Diagnosis (WA 2001) Source: WSDOH, Wash. Comp. Cancer Control, & American Cancer Society Number of cases 11 of 119 die Total cases = 216 91% survival 32 of 67 die 52% survival 17 % survival 55% survival 16 of 19 die 5 of 11 die Local Regional Distant Unstaged Stage at diagnosis
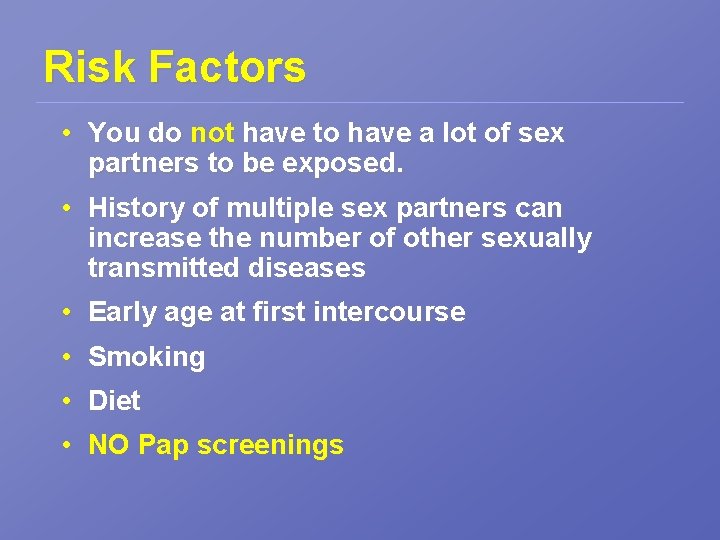
Risk Factors • You do not have to have a lot of sex partners to be exposed. • History of multiple sex partners can increase the number of other sexually transmitted diseases • Early age at first intercourse • Smoking • Diet • NO Pap screenings
Pap Smears • Invasive cervical cancer is one of the most preventable types of cancer due to the effectiveness of the Pap test. • Half of the women who develop cervical cancer have not had regular Pap tests.
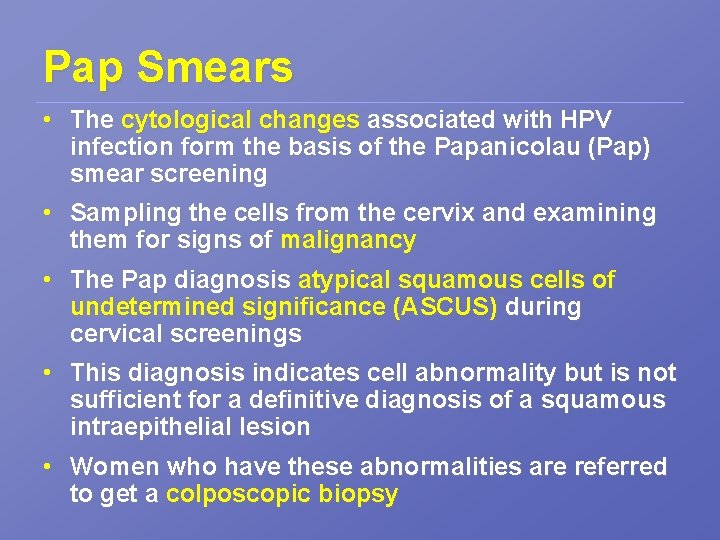
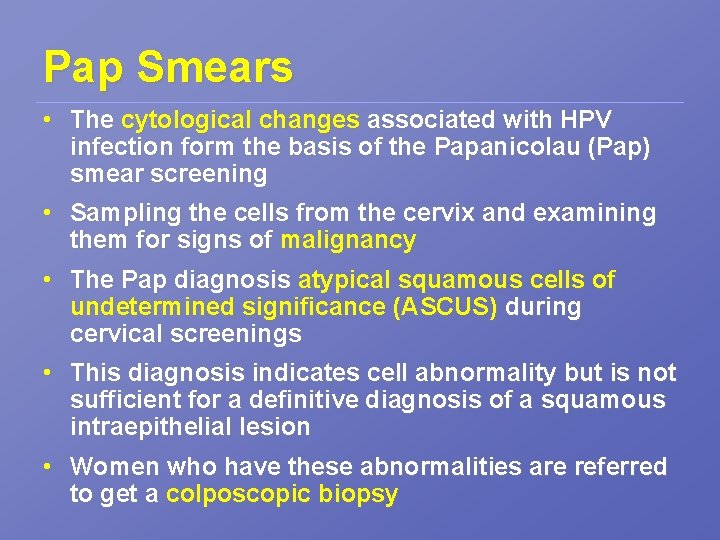
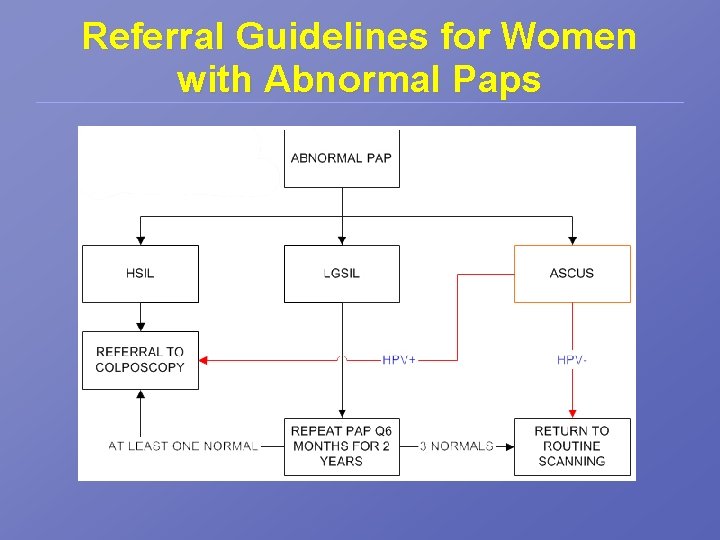
Pap Smears • The cytological changes associated with HPV infection form the basis of the Papanicolau (Pap) smear screening • Sampling the cells from the cervix and examining them for signs of malignancy • The Pap diagnosis atypical squamous cells of undetermined significance (ASCUS) during cervical screenings • This diagnosis indicates cell abnormality but is not sufficient for a definitive diagnosis of a squamous intraepithelial lesion • Women who have these abnormalities are referred to get a colposcopic biopsy
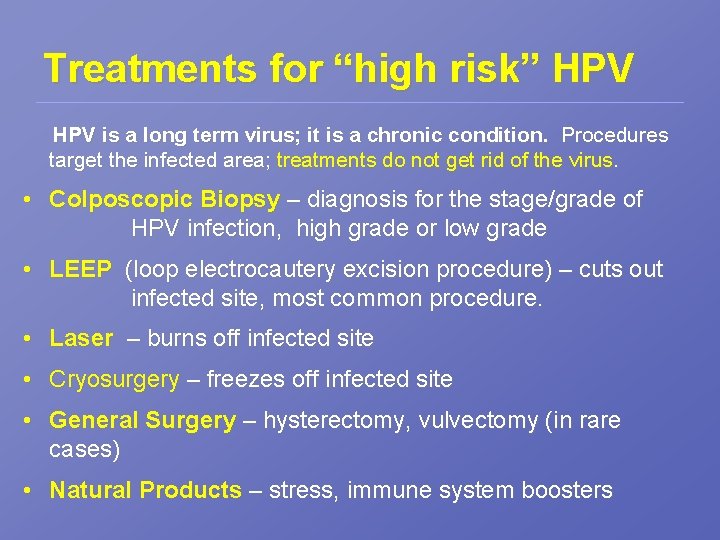
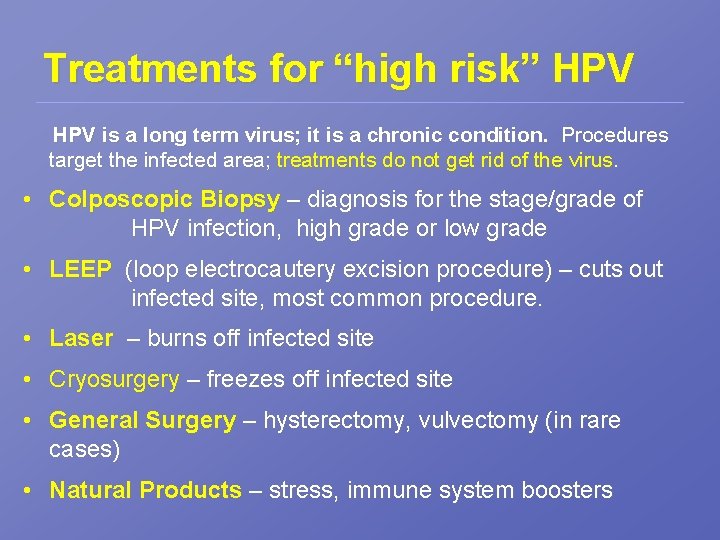
Treatments for “high risk” HPV is a long term virus; it is a chronic condition. Procedures target the infected area; treatments do not get rid of the virus. • Colposcopic Biopsy – diagnosis for the stage/grade of HPV infection, high grade or low grade • LEEP (loop electrocautery excision procedure) – cuts out infected site, most common procedure. • Laser – burns off infected site • Cryosurgery – freezes off infected site • General Surgery – hysterectomy, vulvectomy (in rare cases) • Natural Products – stress, immune system boosters
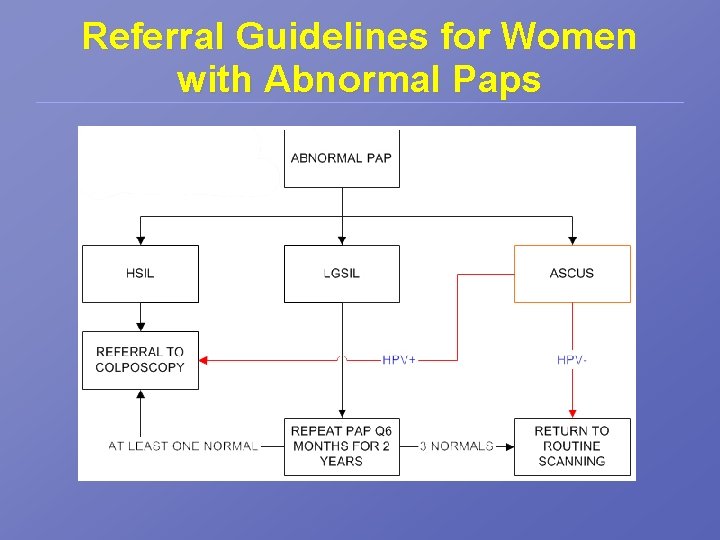
Referral Guidelines for Women with Abnormal Paps
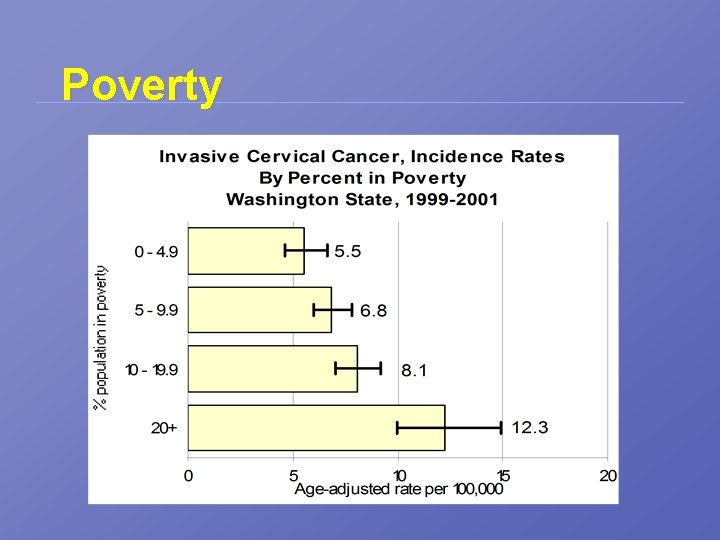
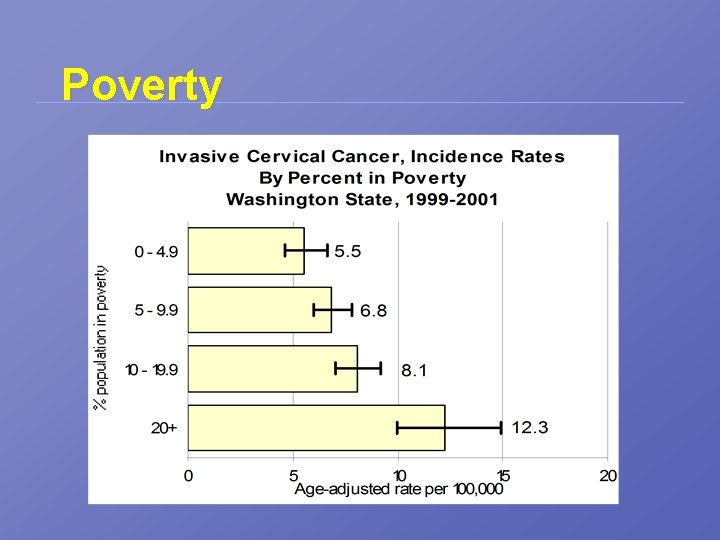
% population in poverty Poverty
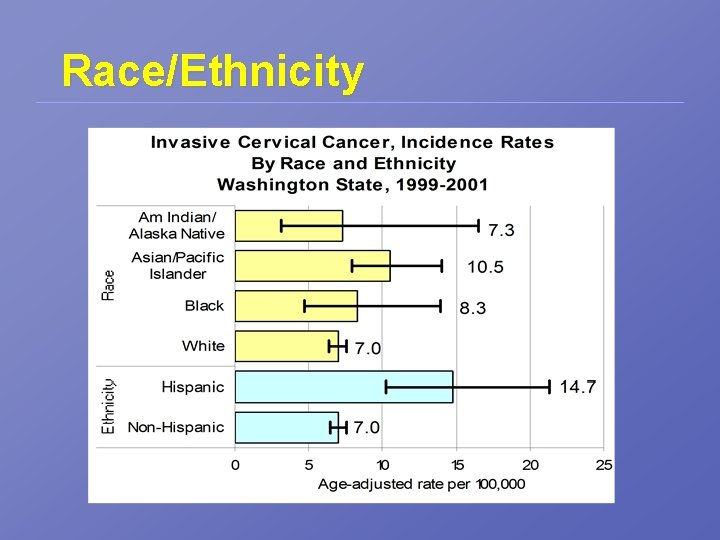
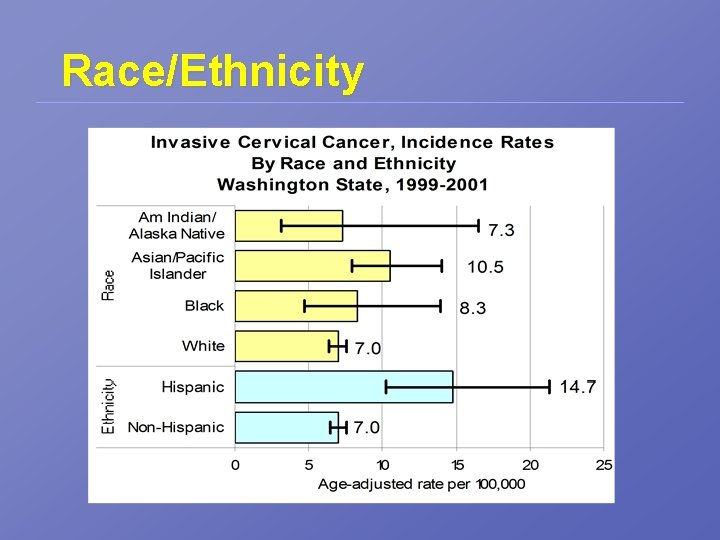
Race/Ethnicity
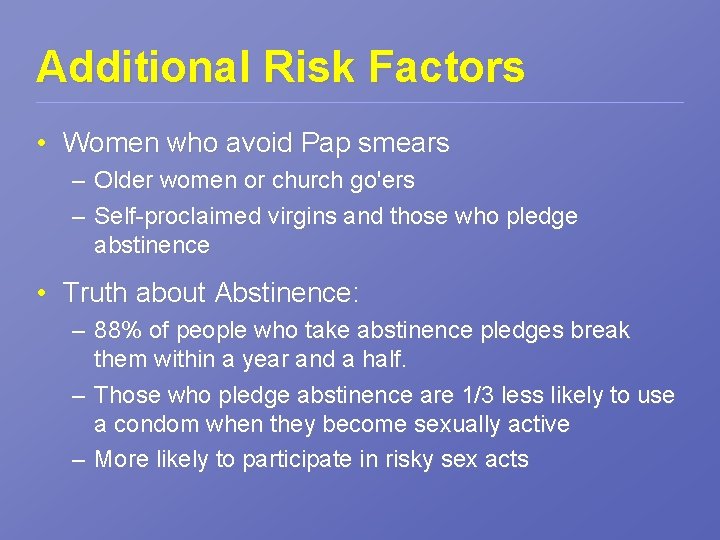
Additional Risk Factors • Women who avoid Pap smears – Older women or church go'ers – Self-proclaimed virgins and those who pledge abstinence • Truth about Abstinence: – 88% of people who take abstinence pledges break them within a year and a half. – Those who pledge abstinence are 1/3 less likely to use a condom when they become sexually active – More likely to participate in risky sex acts
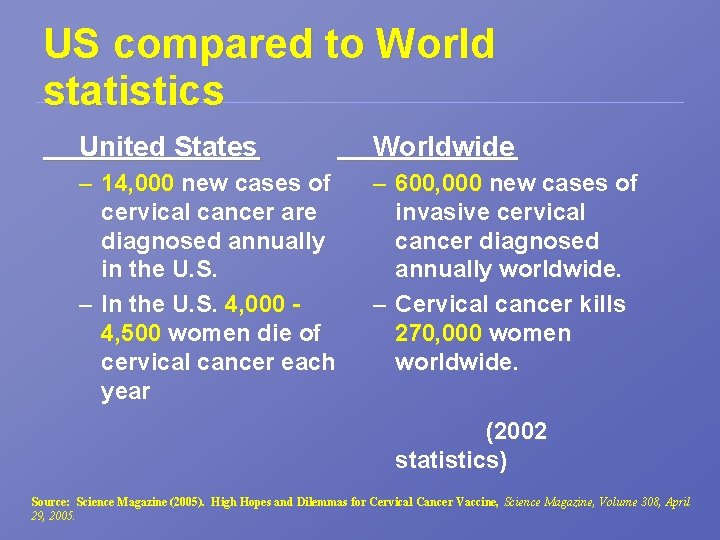
US compared to World statistics United States Worldwide – 14, 000 new cases of cervical cancer are diagnosed annually in the U. S. – In the U. S. 4, 000 4, 500 women die of cervical cancer each year – 600, 000 new cases of invasive cervical cancer diagnosed annually worldwide. – Cervical cancer kills 270, 000 women worldwide. (2002 statistics) Source: Science Magazine (2005). High Hopes and Dilemmas for Cervical Cancer Vaccine, Science Magazine, Volume 308, April 29, 2005.
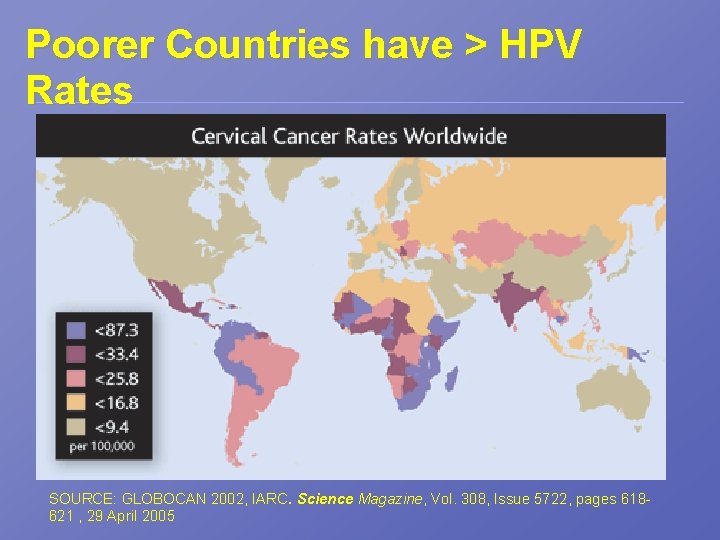
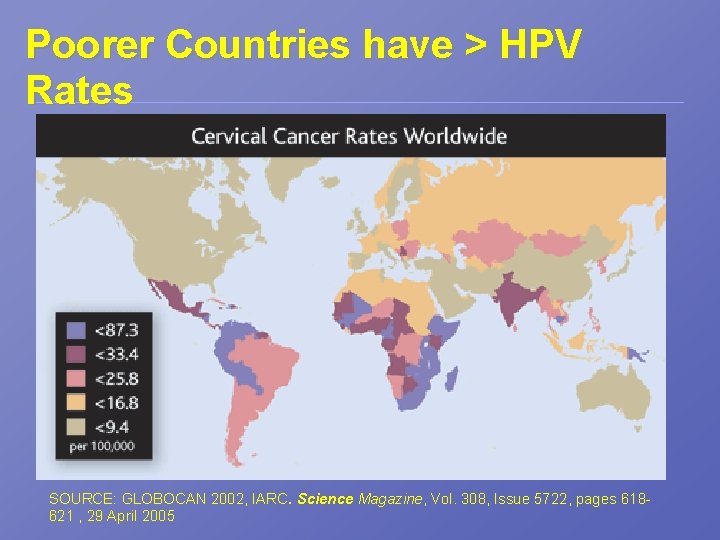
Poorer Countries have > HPV Rates SOURCE: GLOBOCAN 2002, IARC. Science Magazine, Vol. 308, Issue 5722, pages 618621 , 29 April 2005
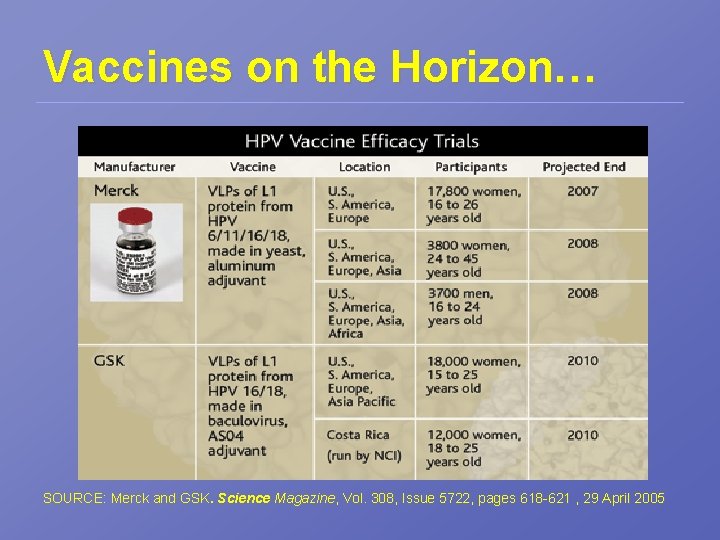
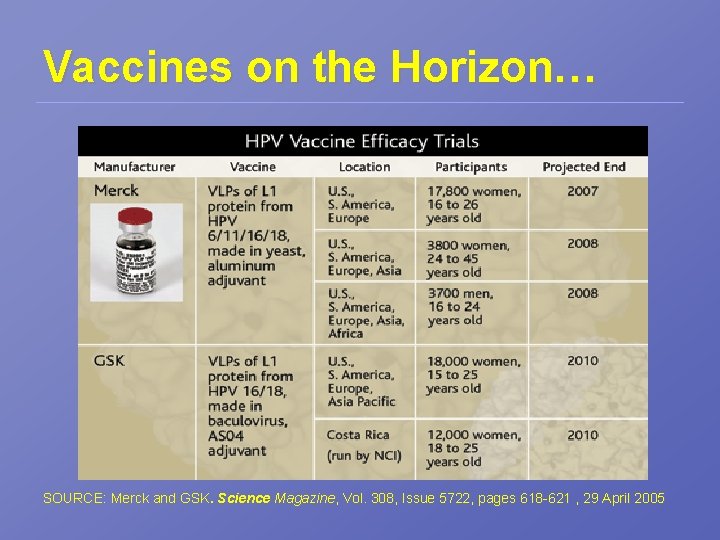
Vaccines on the Horizon… SOURCE: Merck and GSK. Science Magazine, Vol. 308, Issue 5722, pages 618 -621 , 29 April 2005
Challenges with the Vaccine • Vaccine may have little impact on the cases of cervical cancer • Access to a provider and preventive screenings/vaccines will still be an issue • Poorer countries have a higher need for the vaccine, but wealthier countries will get it 1 st
Prevention • Get regular Pap smears ! • Don’t smoke • Avoid exposure to HPV – use a condom • Advocate for greater access to preventive screenings for all populations • Live Healthy and Eat Healthy

Nutritional Support for HPV • The following are suggested for protection, as well as support for those who are infected – Vitamin C – Vitamin A & beta-carotene – Folic acid – Pyridoxine (B 6) – Selenium – Zinc Correlation has been found between Copper: Zinc ratio (higher copper and lower zinc) in CIN and cancer patients
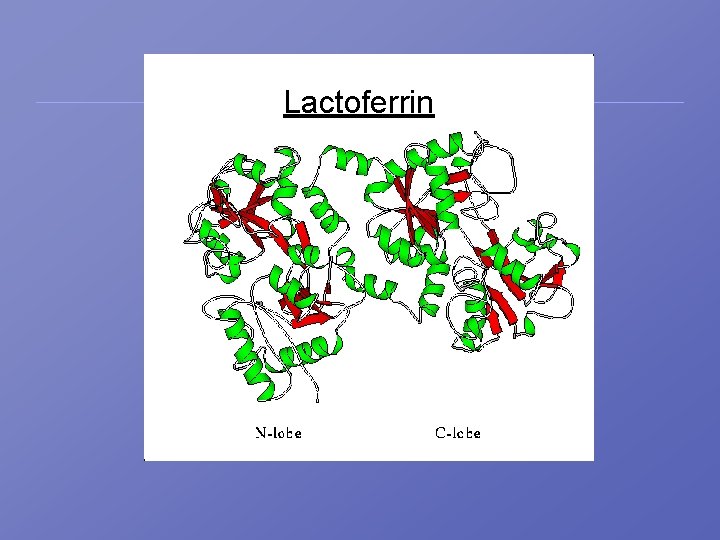
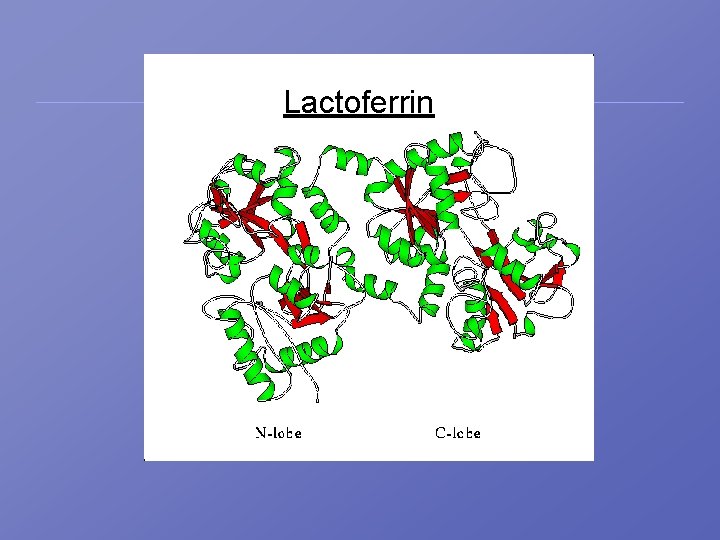
Lactoferrin
Therapeutic Use of Lactoferrin • Lactoferrin (LF) – Iron binding glycoprotein is present in many mucosal secretions including saliva, tears, as well as vaginal and seminal fluids – Found in Human breast milk (HLF) as well as bovine milk (BLF) – Lf exhibits bacterialcidal and fungicidal activity(particularly Candida species) by depriving bacteria and fungus from iron
Therapeutic Use of Lactoferrin • Lf also exhibits anti-viral activity by inhibiting viral binding to glycosamines such as heparin sulphite; it is hypothesized that heparin sulphite mediates the binding of HPV to the host cell • Studies have shown that BLF is a better inhibitor than LF and it effectively inhibits HPV 16
 Familia papovaviridae
Familia papovaviridae Papoviridae
Papoviridae Familia papovaviridae
Familia papovaviridae Icosahedral adalah
Icosahedral adalah 2 fold symmetry
2 fold symmetry Brome mosaic virus
Brome mosaic virus What is inflectional and derivational morphology
What is inflectional and derivational morphology Plastic bag american beauty quote
Plastic bag american beauty quote Patricia jordan naked
Patricia jordan naked Importance of gymnosperms
Importance of gymnosperms Becca bowen naked
Becca bowen naked Pico naked
Pico naked Naked egg drop
Naked egg drop Numberblocks 3000
Numberblocks 3000 Naked short seller
Naked short seller Helmer aslaksen
Helmer aslaksen Alex clarke naked
Alex clarke naked Dr brenda shen
Dr brenda shen Lara lewington naked
Lara lewington naked Mundo naked
Mundo naked Indian people called gymnastics as naked art.
Indian people called gymnastics as naked art. Barbara gail montero
Barbara gail montero Partes del cuerpo humano
Partes del cuerpo humano Naked
Naked Benefits supervisor sleeping naked man with rat
Benefits supervisor sleeping naked man with rat Motives concealer
Motives concealer They were both naked
They were both naked Francesco ruggiero naked
Francesco ruggiero naked Naked filipino
Naked filipino Kelly elkins naked
Kelly elkins naked Naked boy
Naked boy Ascomycota kingdom
Ascomycota kingdom Presentation nude
Presentation nude Appreciate naked
Appreciate naked Naked naber
Naked naber Naked seeds
Naked seeds Banana genus
Banana genus Maestra giulia verbi
Maestra giulia verbi Genus defination
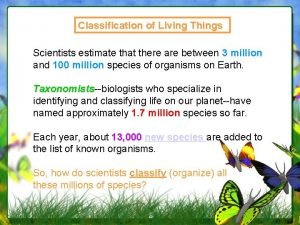
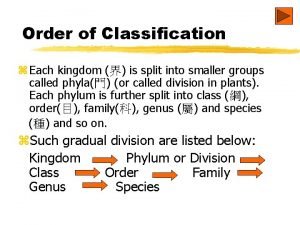
Genus defination Kingdom family genus species
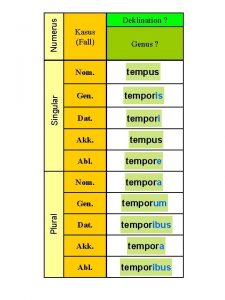
Kingdom family genus species Numerus genus
Numerus genus Is scientific name italicized
Is scientific name italicized The organism quercus phellos is a member of the genus
The organism quercus phellos is a member of the genus Plant classification order
Plant classification order Genus
Genus Genus of tea
Genus of tea Ovary squid
Ovary squid Genus species format
Genus species format Maggots mc
Maggots mc Biology
Biology Streptococcus genus
Streptococcus genus Balantidium coli genus
Balantidium coli genus Genus proximum differentia specifica
Genus proximum differentia specifica Domain kingdom phylum
Domain kingdom phylum Genus of sweet potato
Genus of sweet potato Igitur iis genus aetas eloquentia
Igitur iis genus aetas eloquentia Lateris dextri
Lateris dextri Finding order in diversity
Finding order in diversity What is the genus name of canis familiaris
What is the genus name of canis familiaris Genus and species examples
Genus and species examples Genus
Genus Genus tool
Genus tool