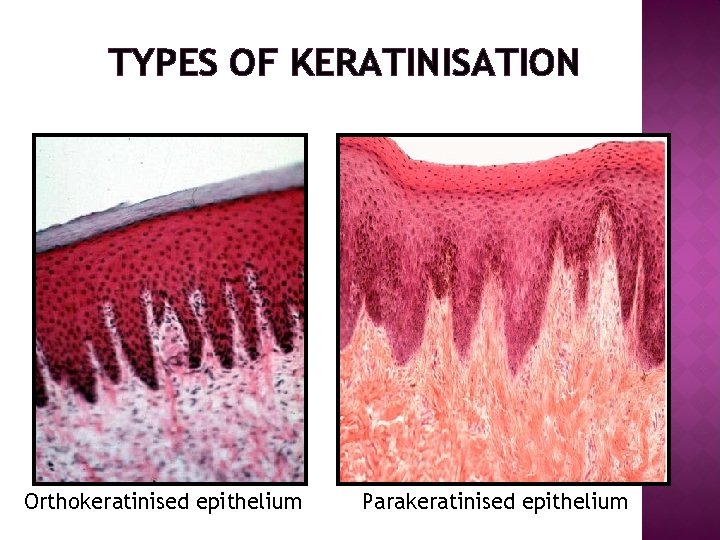
TYPES OF KERATINISATION Orthokeratinised epithelium Parakeratinised epithelium NON


- Slides: 39

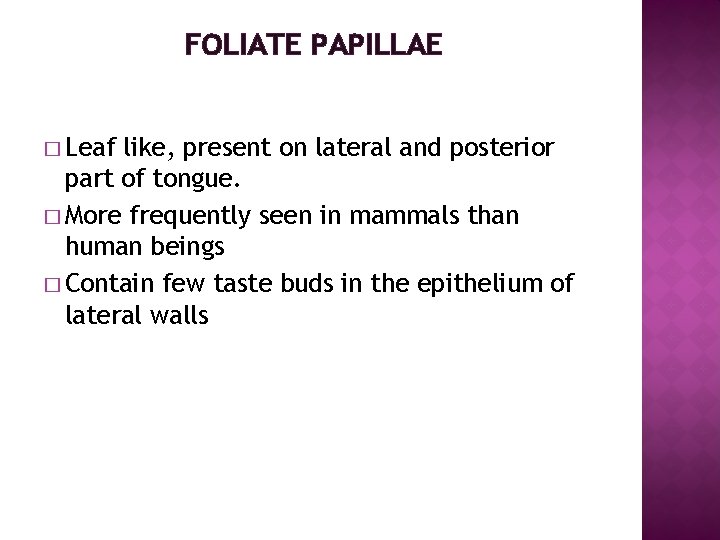
TYPES OF KERATINISATION Orthokeratinised epithelium Parakeratinised epithelium
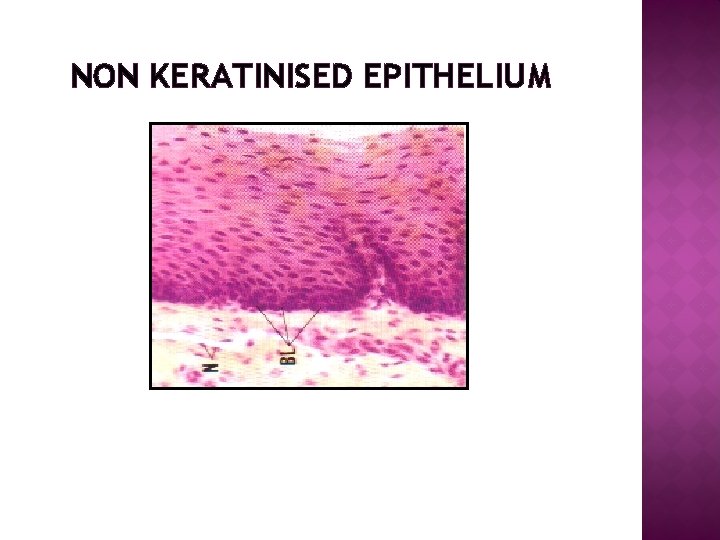
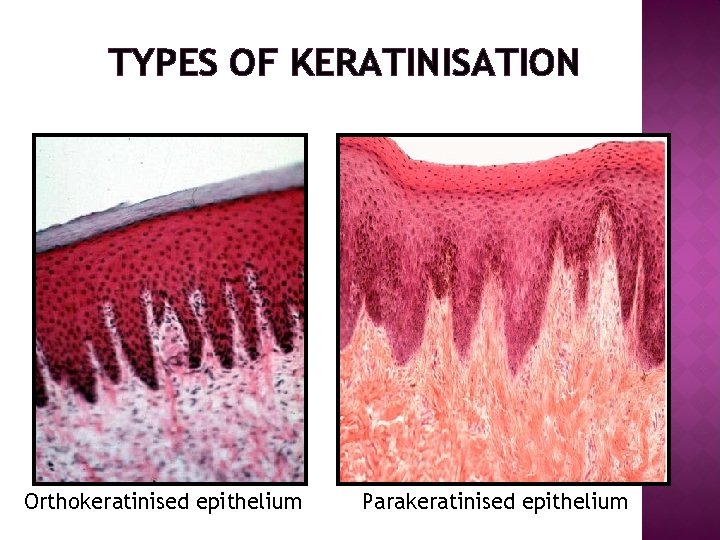
NON KERATINISED EPITHELIUM
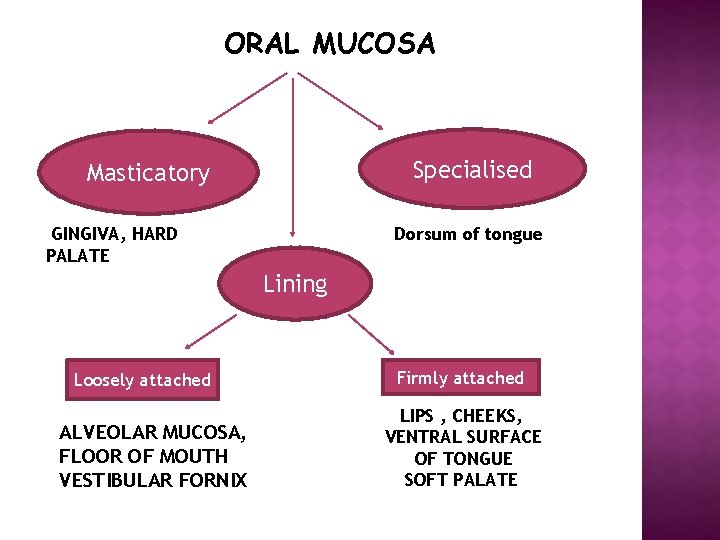
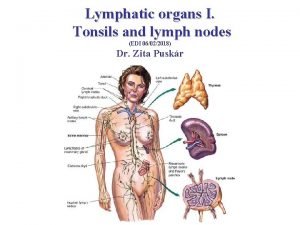
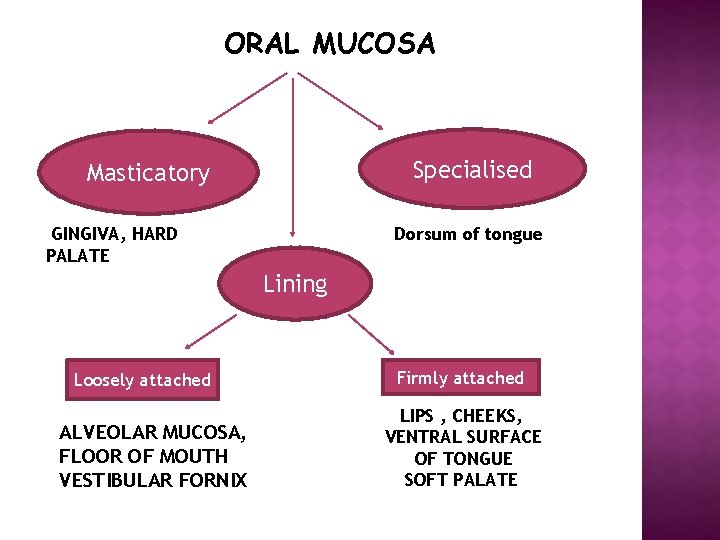
ORAL MUCOSA Specialised Masticatory GINGIVA, HARD PALATE Dorsum of tongue Lining Loosely attached ALVEOLAR MUCOSA, FLOOR OF MOUTH VESTIBULAR FORNIX Firmly attached LIPS , CHEEKS, VENTRAL SURFACE OF TONGUE SOFT PALATE
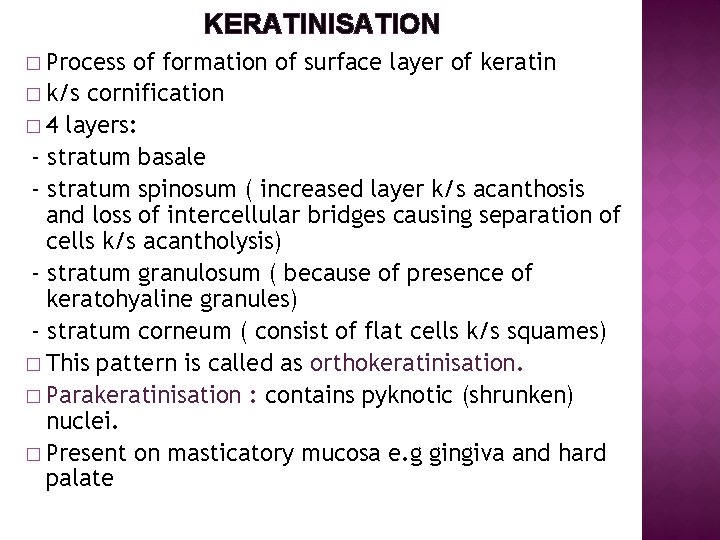
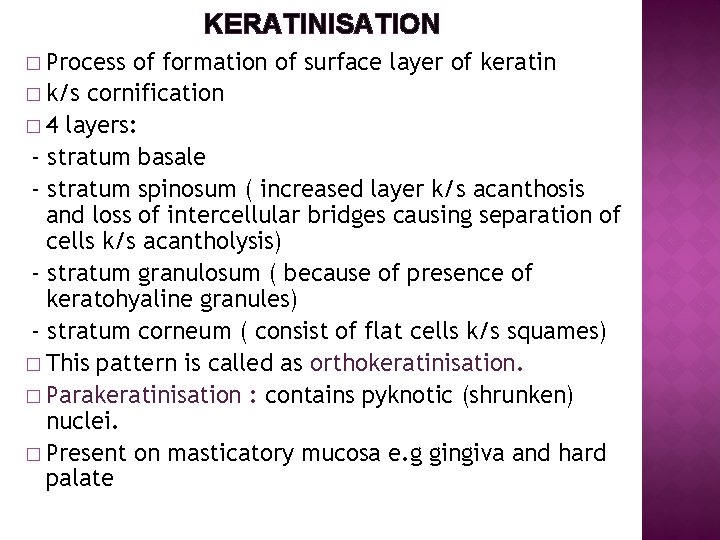
KERATINISATION � Process of formation of surface layer of keratin � k/s cornification � 4 layers: - stratum basale - stratum spinosum ( increased layer k/s acanthosis and loss of intercellular bridges causing separation of cells k/s acantholysis) - stratum granulosum ( because of presence of keratohyaline granules) - stratum corneum ( consist of flat cells k/s squames) � This pattern is called as orthokeratinisation. � Parakeratinisation : contains pyknotic (shrunken) nuclei. � Present on masticatory mucosa e. g gingiva and hard palate
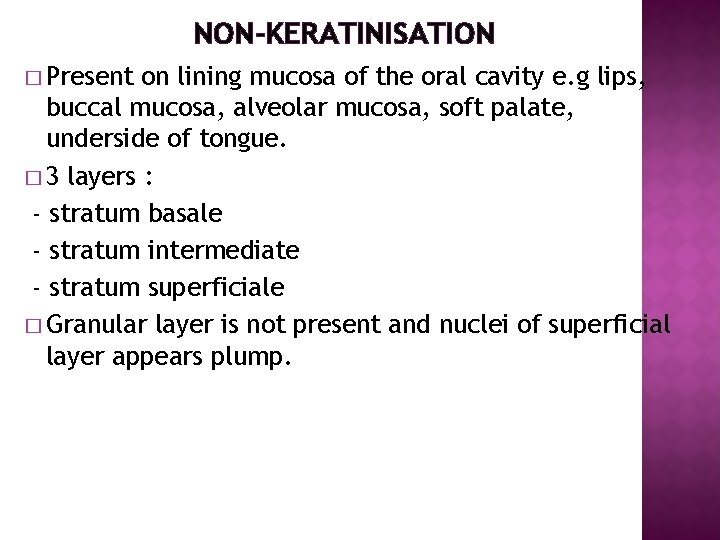
NON-KERATINISATION � Present on lining mucosa of the oral cavity e. g lips, buccal mucosa, alveolar mucosa, soft palate, underside of tongue. � 3 layers : - stratum basale - stratum intermediate - stratum superficiale � Granular layer is not present and nuclei of superficial layer appears plump.
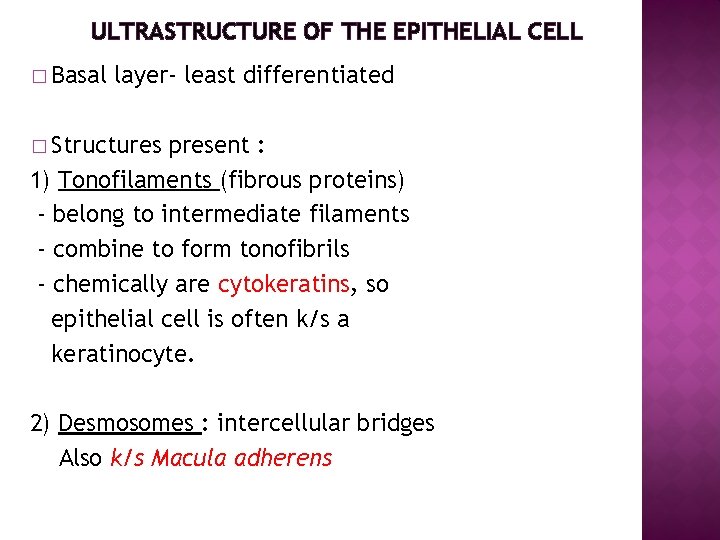
ULTRASTRUCTURE OF THE EPITHELIAL CELL � Basal layer- least differentiated � Structures present : 1) Tonofilaments (fibrous proteins) - belong to intermediate filaments - combine to form tonofibrils - chemically are cytokeratins, so epithelial cell is often k/s a keratinocyte. 2) Desmosomes : intercellular bridges Also k/s Macula adherens
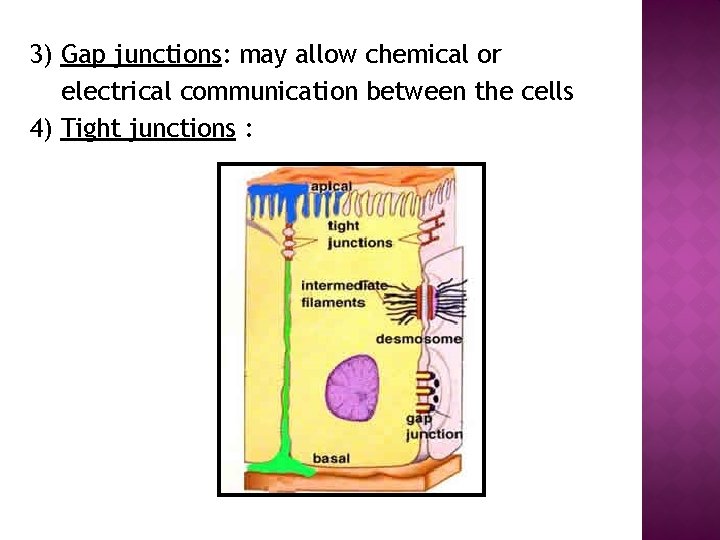
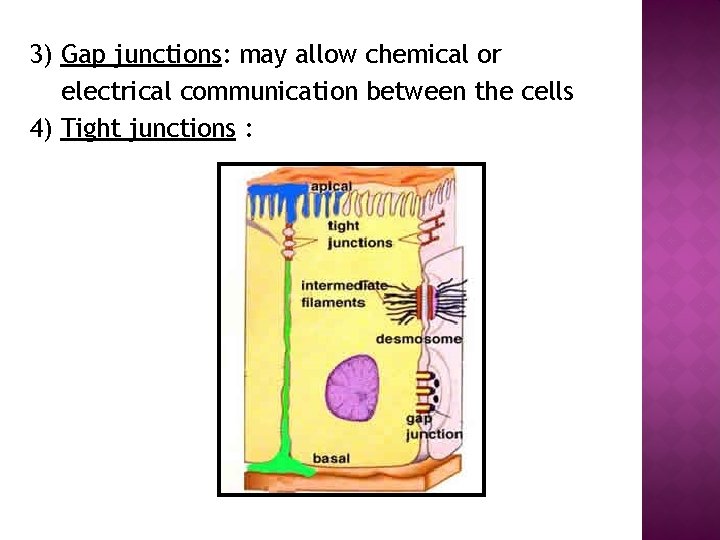
3) Gap junctions: may allow chemical or electrical communication between the cells 4) Tight junctions :
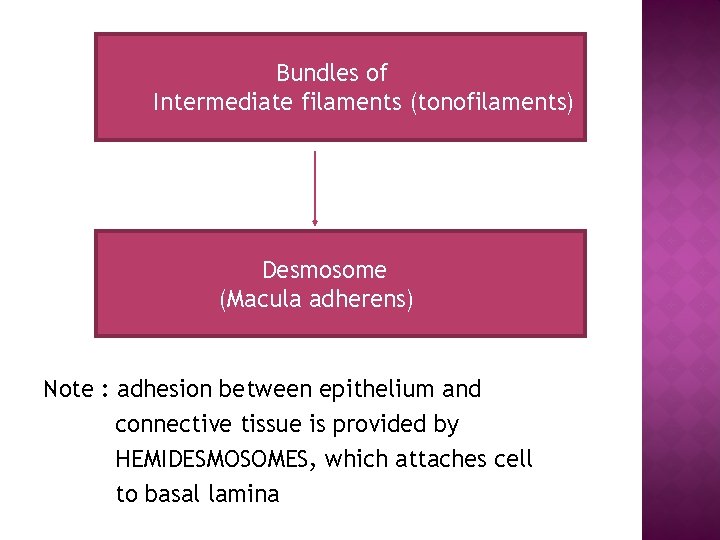
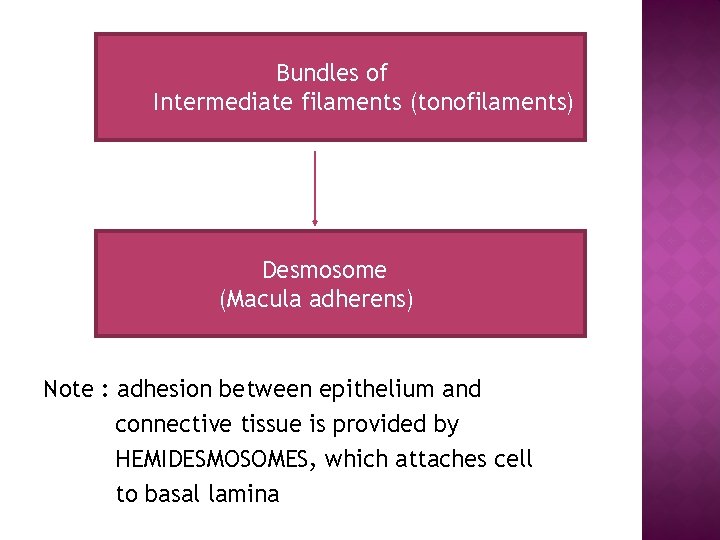
Bundles of Intermediate filaments (tonofilaments) Desmosome (Macula adherens) Note : adhesion between epithelium and connective tissue is provided by HEMIDESMOSOMES, which attaches cell to basal lamina
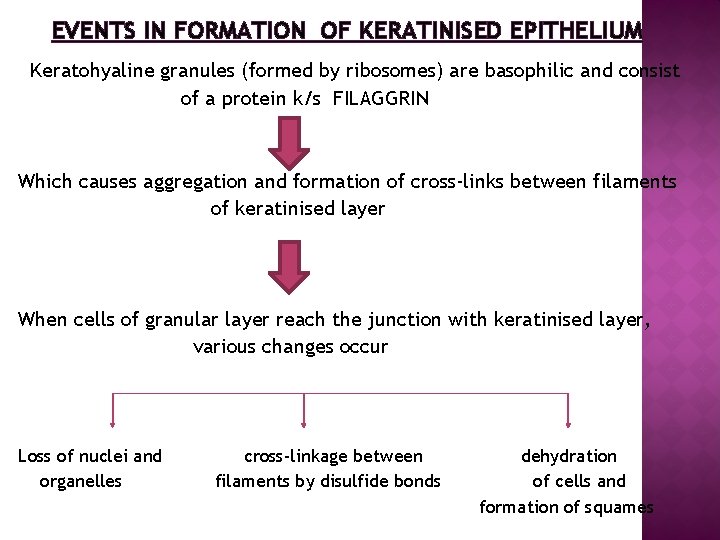
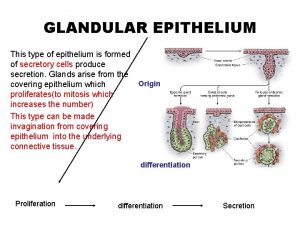
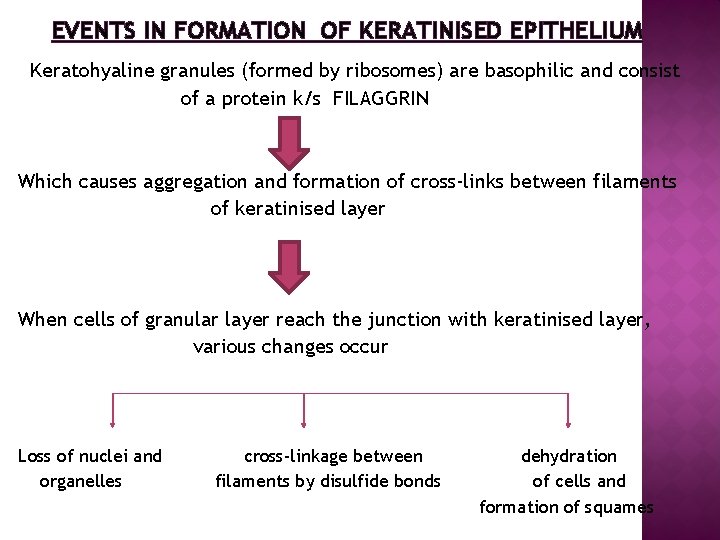
EVENTS IN FORMATION OF KERATINISED EPITHELIUM Keratohyaline granules (formed by ribosomes) are basophilic and consist of a protein k/s FILAGGRIN Which causes aggregation and formation of cross-links between filaments of keratinised layer When cells of granular layer reach the junction with keratinised layer, various changes occur Loss of nuclei and organelles cross-linkage between filaments by disulfide bonds dehydration of cells and formation of squames
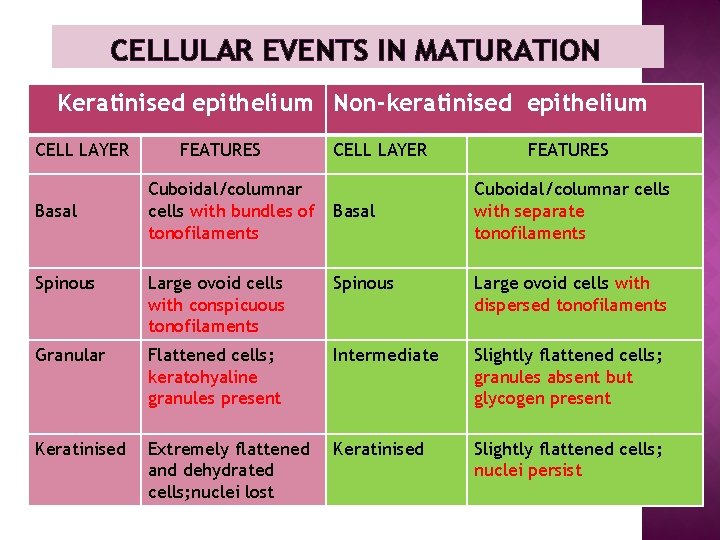
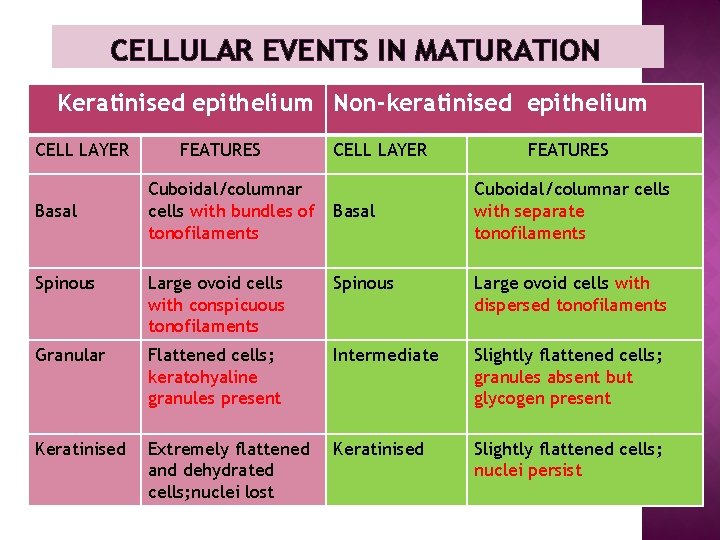
CELLULAR EVENTS IN MATURATION Keratinised epithelium Non-keratinised epithelium CELL LAYER Basal FEATURES Cuboidal/columnar cells with bundles of tonofilaments CELL LAYER Basal FEATURES Cuboidal/columnar cells with separate tonofilaments Spinous Large ovoid cells with conspicuous tonofilaments Spinous Large ovoid cells with dispersed tonofilaments Granular Flattened cells; keratohyaline granules present Intermediate Slightly flattened cells; granules absent but glycogen present Keratinised Extremely flattened and dehydrated cells; nuclei lost Keratinised Slightly flattened cells; nuclei persist
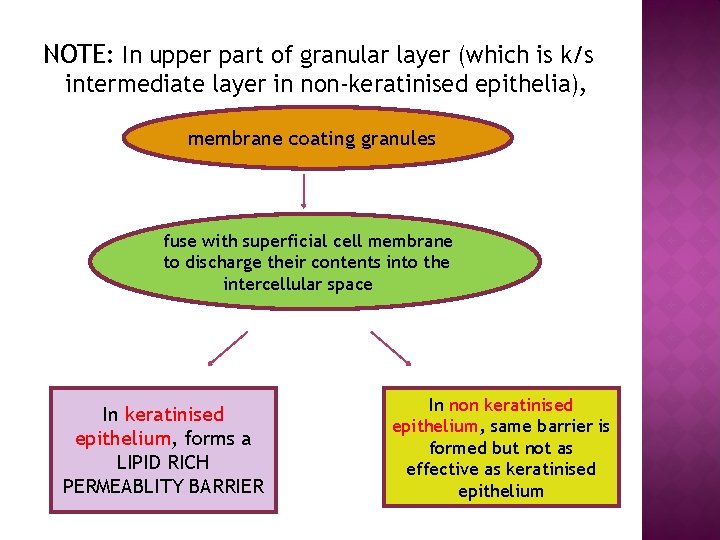
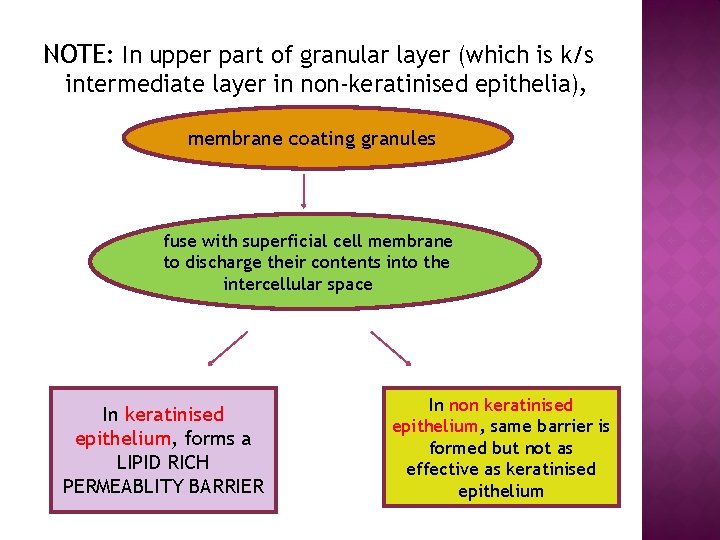
NOTE: In upper part of granular layer (which is k/s intermediate layer in non-keratinised epithelia), membrane coating granules fuse with superficial cell membrane to discharge their contents into the intercellular space In keratinised epithelium, forms a LIPID RICH PERMEABLITY BARRIER In non keratinised epithelium, same barrier is formed but not as effective as keratinised epithelium
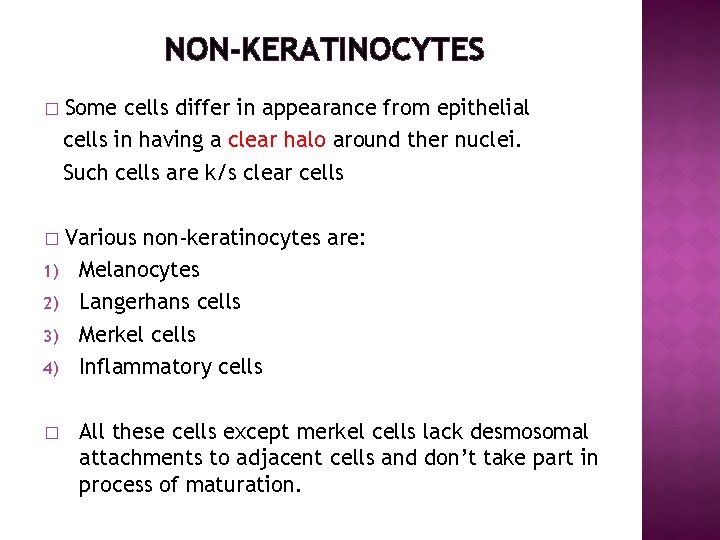
NON-KERATINOCYTES � Some cells differ in appearance from epithelial cells in having a clear halo around ther nuclei. Such cells are k/s clear cells � Various non-keratinocytes are: Melanocytes Langerhans cells Merkel cells Inflammatory cells 1) 2) 3) 4) � All these cells except merkel cells lack desmosomal attachments to adjacent cells and don’t take part in process of maturation.
1) MELANOCYTES Specialised pigment cells situated in basal layer. � originate embryologically from neural crest ectoderm and enter epithelium at 11 weeks of gestation. � Lack desmosomes and tonofilaments but possess long dendritic processes that extend between keratinocytes. � Have specialised structures called as melanosomes within them which produce melanin. Melanin is responsible for color and pigmentation of oral mucosa. � Melanophages are macrophages that have taken up melanosomes produced by melanocytes. � Applied aspect: melanocytes can cause development of several lesions in oral mucosa �
� - Applied aspect: melanocytes can cause development of several lesions in oral mucosa like Oral melanotic macule Nevus (mole) Melanoma (malignant tumor)
2) LANGERHANS CELLS � Another dendritic cell seen above the basal layer. � SOURCE : Bone marrow � Lacks desmosomal attachments to the surrounding cells, so appear as clear cells. � Characterised ultrastructurally by a small rod or flask shaped granule k/s BIRBECK’S GRANULES. � Unlike melanocytes, they move in and out of the epithelium.
3) MERKEL CELLS � Situated in the basal layer of oral epithelium. � Non-dendritic � ORIGIN: may arise from division of an epithelial cell � Possess keratin tonofilaments and occasionally desmosomes. � Characteristic feature : possess small membranebound vesicles in the cytoplasm, sometimes adjacent to a nerve fiber associated with the cell. These granules may liberate a neurotransmitter like substance across the synapses like junction between the merkel cell and nerve fiber, thus triggering an impulse.
4) INFLAMMATORY CELLS Often can be seen in nucleated cell layers. � Transient cells, not reproduce themselves as other non-keratinocytes. � e. g lymphocytes, PMNLs and mast cells. � Lymphocytes are associated with langerhans cells and are capable of activating T-lymphocytes. �
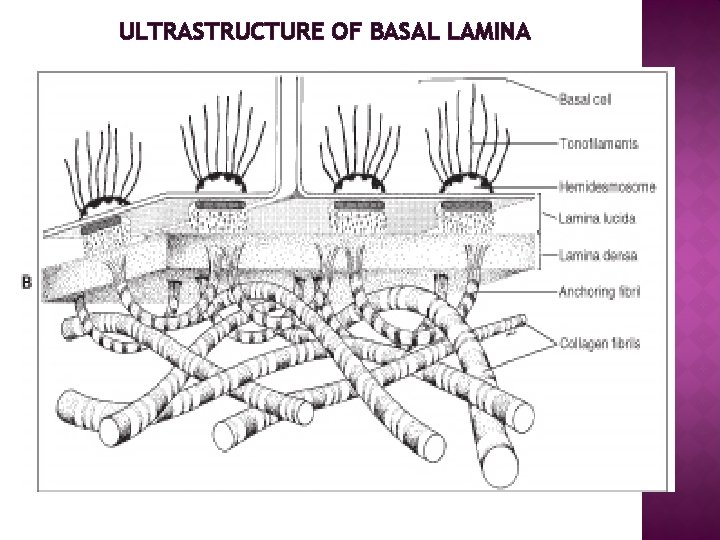
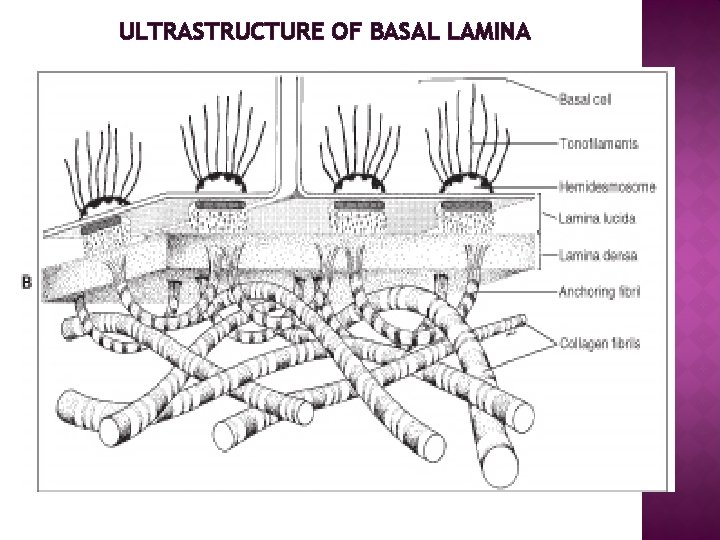
ULTRASTRUCTURE OF BASAL LAMINA
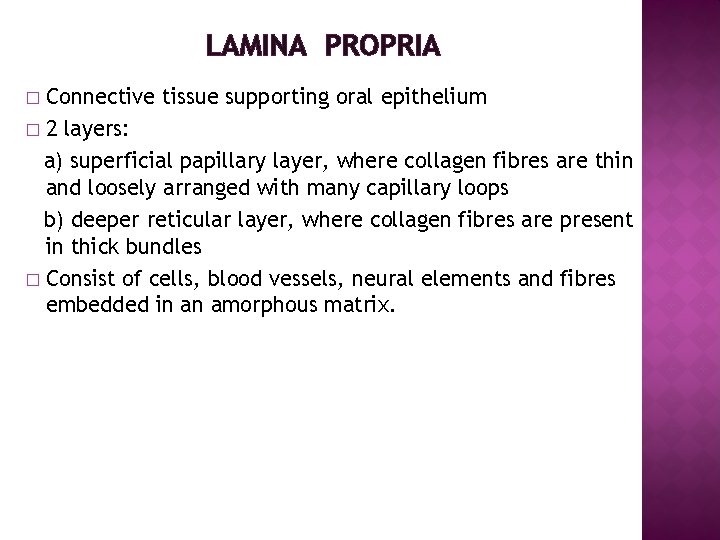
LAMINA PROPRIA Connective tissue supporting oral epithelium � 2 layers: a) superficial papillary layer, where collagen fibres are thin and loosely arranged with many capillary loops b) deeper reticular layer, where collagen fibres are present in thick bundles � Consist of cells, blood vessels, neural elements and fibres embedded in an amorphous matrix. �
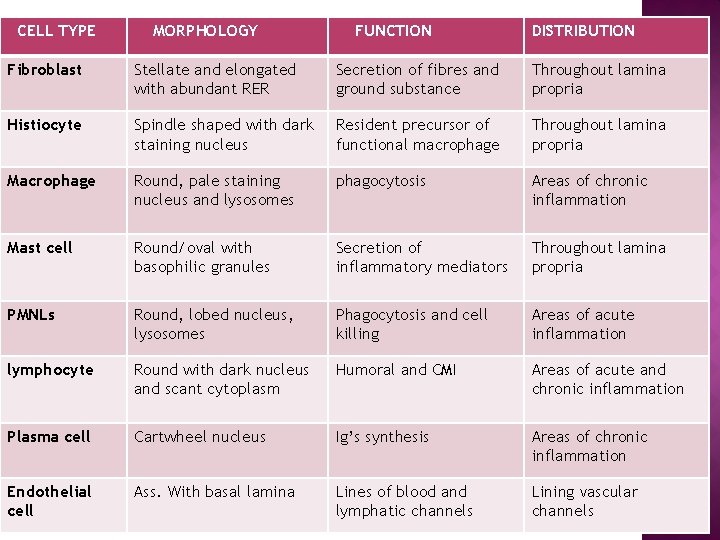
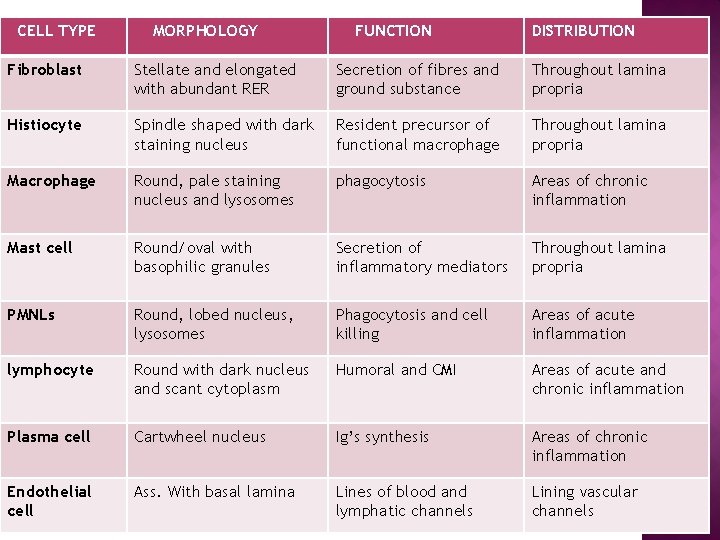
CELL TYPE MORPHOLOGY FUNCTION DISTRIBUTION Fibroblast Stellate and elongated with abundant RER Secretion of fibres and ground substance Throughout lamina propria Histiocyte Spindle shaped with dark staining nucleus Resident precursor of functional macrophage Throughout lamina propria Macrophage Round, pale staining nucleus and lysosomes phagocytosis Areas of chronic inflammation Mast cell Round/oval with basophilic granules Secretion of inflammatory mediators Throughout lamina propria PMNLs Round, lobed nucleus, lysosomes Phagocytosis and cell killing Areas of acute inflammation lymphocyte Round with dark nucleus and scant cytoplasm Humoral and CMI Areas of acute and chronic inflammation Plasma cell Cartwheel nucleus Ig’s synthesis Areas of chronic inflammation Endothelial cell Ass. With basal lamina Lines of blood and lymphatic channels Lining vascular channels
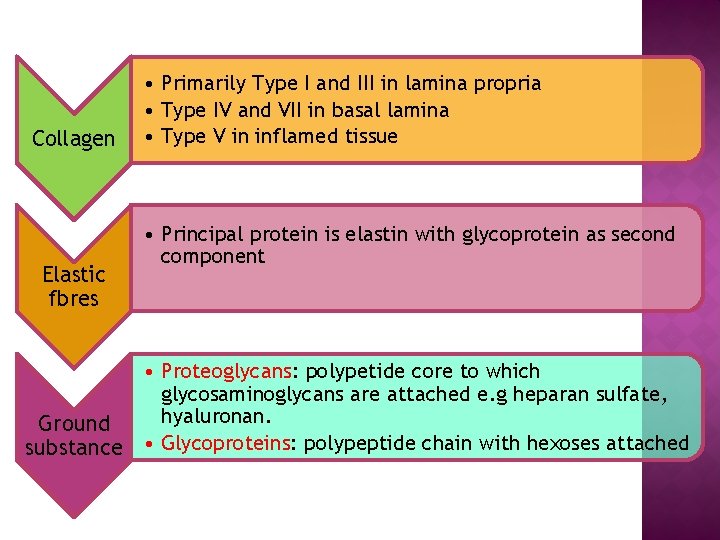
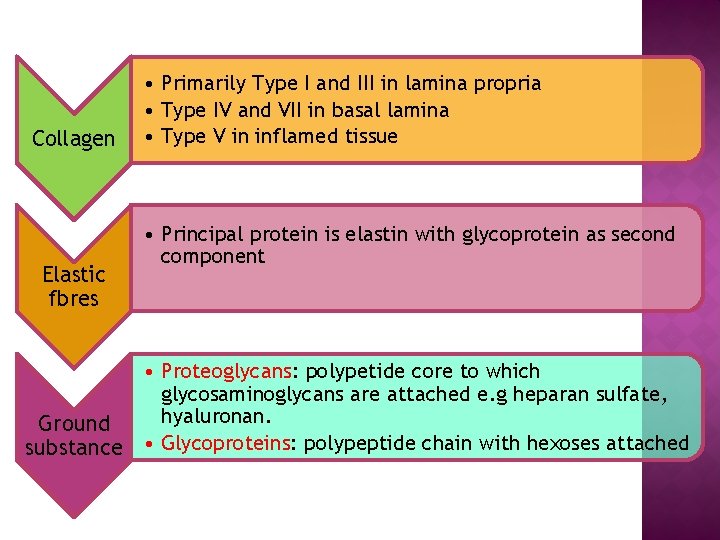
Collagen Elastic fbres • Primarily Type I and III in lamina propria • Type IV and VII in basal lamina • Type V in inflamed tissue • Principal protein is elastin with glycoprotein as second component • Proteoglycans: polypetide core to which glycosaminoglycans are attached e. g heparan sulfate, hyaluronan. Ground substance • Glycoproteins: polypeptide chain with hexoses attached
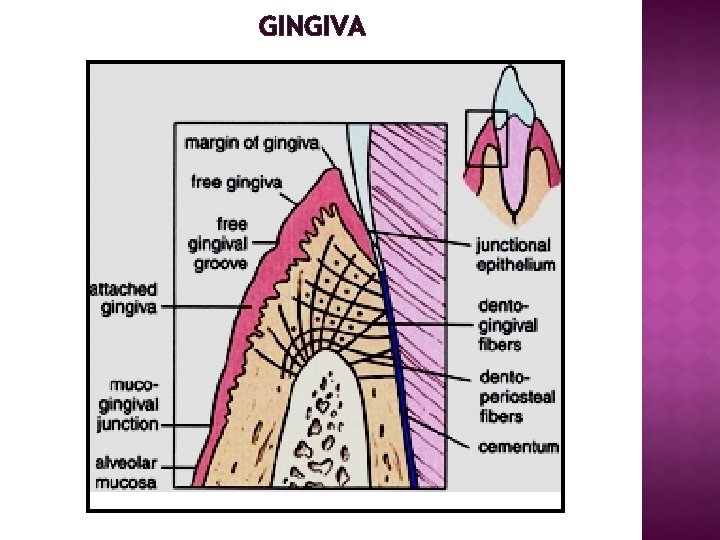
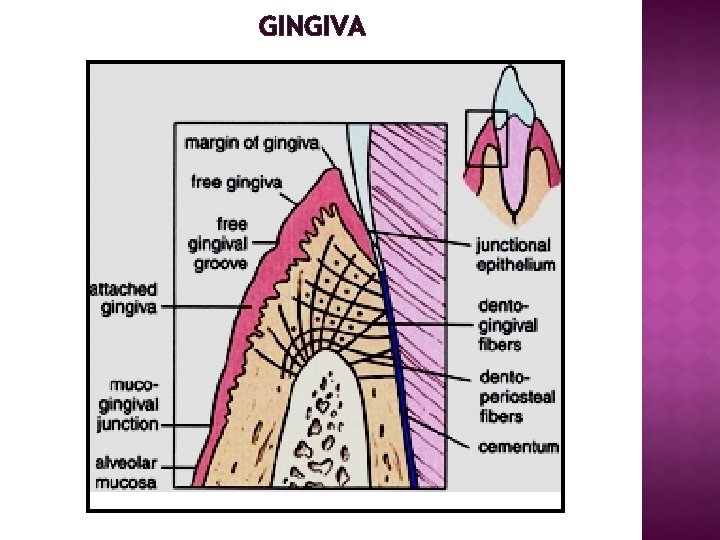
GINGIVA

HISTOLOGY OF GINGIVA NO SUBMUCOSA Keratinised epithelium Epithelial ridges Connective tissue papilla Lamina propria
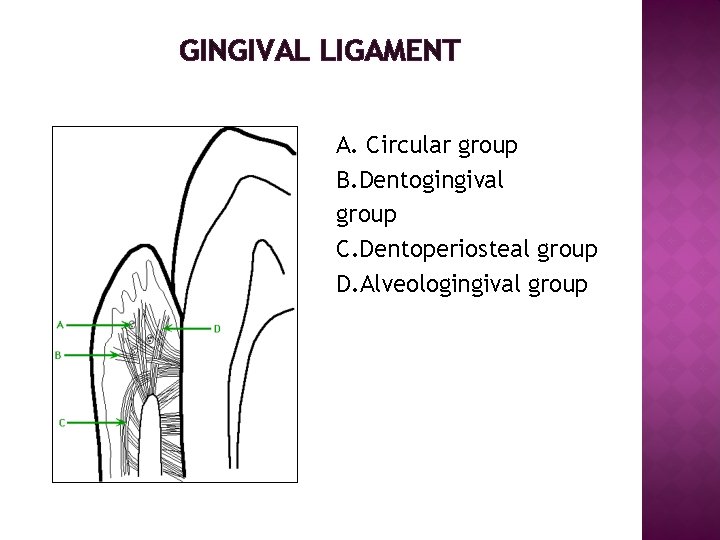
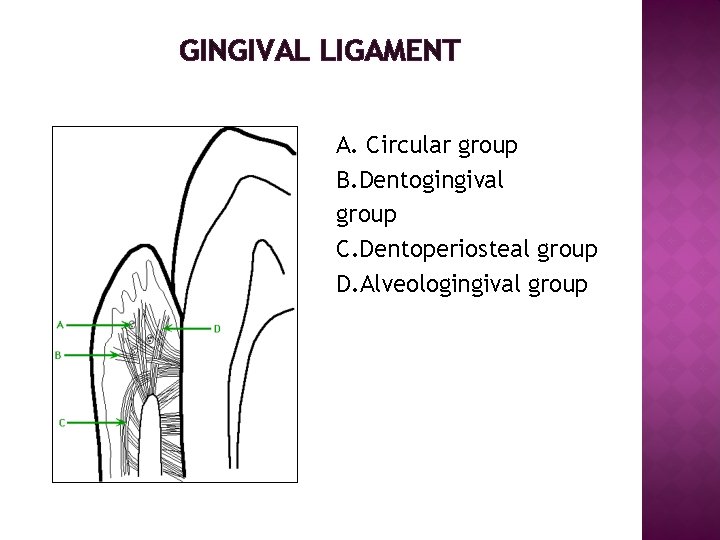
GINGIVAL LIGAMENT A. Circular group B. Dentogingival group C. Dentoperiosteal group D. Alveologingival group
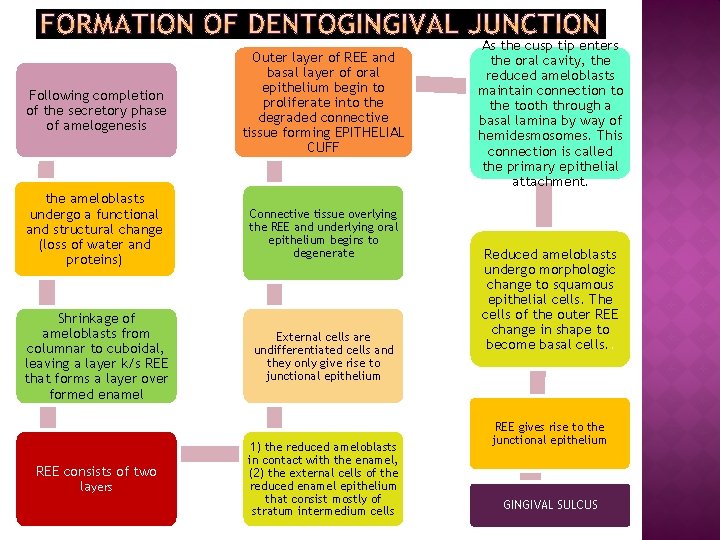
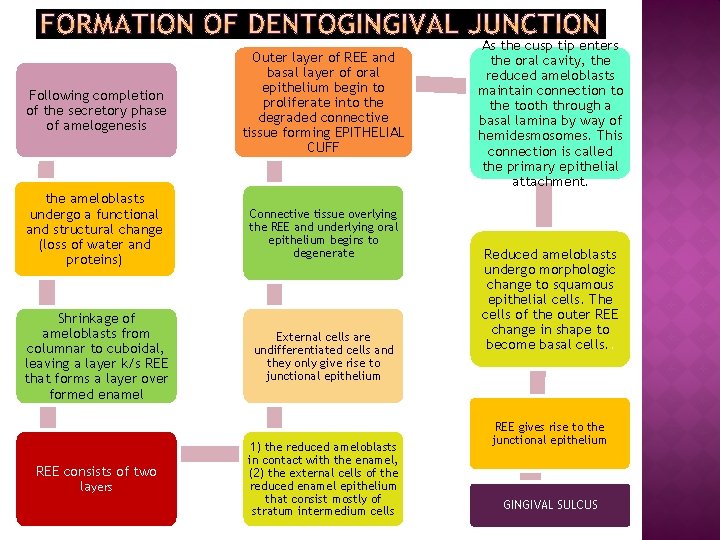
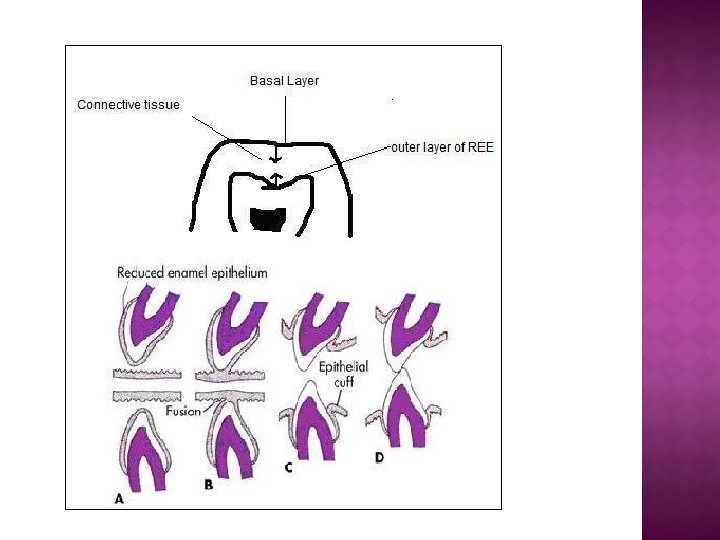
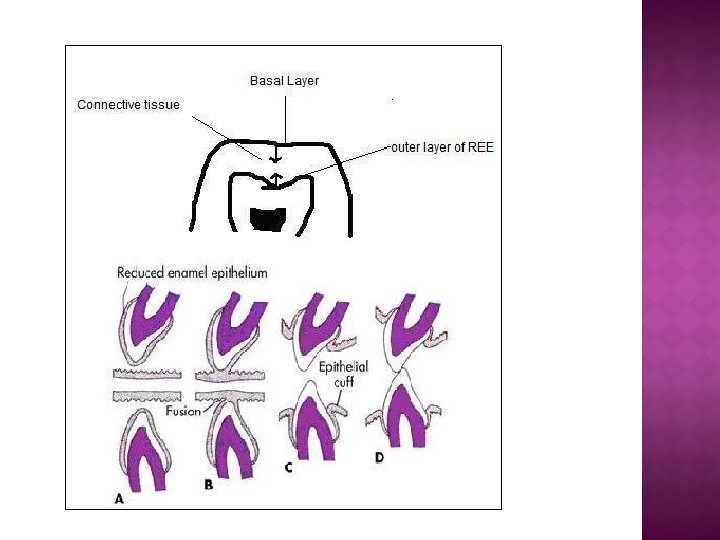
Following completion of the secretory phase of amelogenesis Outer layer of REE and basal layer of oral epithelium begin to proliferate into the degraded connective tissue forming EPITHELIAL CUFF the ameloblasts undergo a functional and structural change (loss of water and proteins) Connective tissue overlying the REE and underlying oral epithelium begins to degenerate Shrinkage of ameloblasts from columnar to cuboidal, leaving a layer k/s REE that forms a layer over formed enamel External cells are undifferentiated cells and they only give rise to junctional epithelium REE consists of two layers 1) the reduced ameloblasts in contact with the enamel, (2) the external cells of the reduced enamel epithelium that consist mostly of stratum intermedium cells As the cusp tip enters the oral cavity, the reduced ameloblasts maintain connection to the tooth through a basal lamina by way of hemidesmosomes. This connection is called the primary epithelial attachment. Reduced ameloblasts undergo morphologic change to squamous epithelial cells. The cells of the outer REE change in shape to become basal cells. . REE gives rise to the junctional epithelium GINGIVAL SULCUS
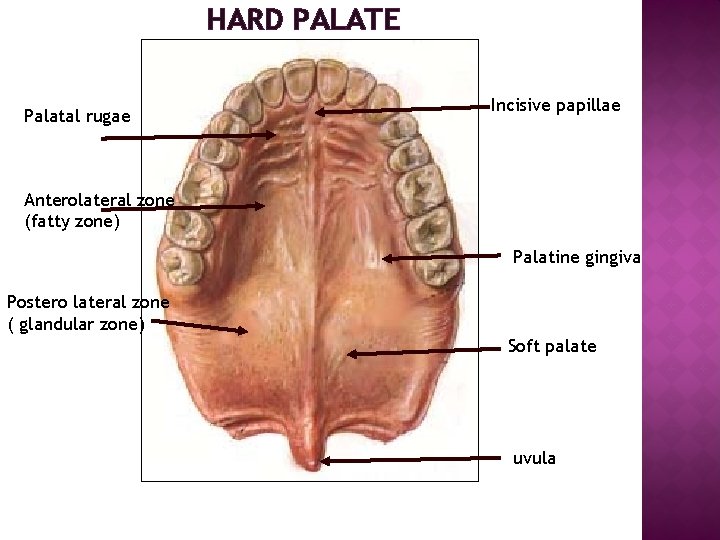
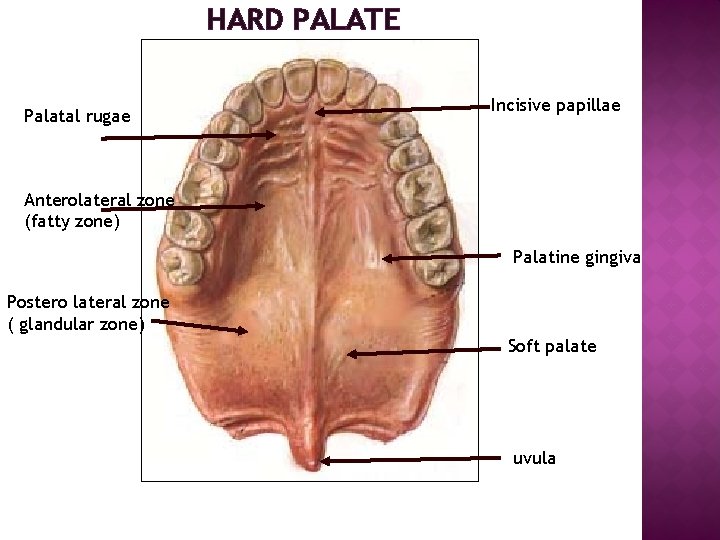
HARD PALATE Palatal rugae Incisive papillae Anterolateral zone (fatty zone) Palatine gingiva Postero lateral zone ( glandular zone) Soft palate uvula
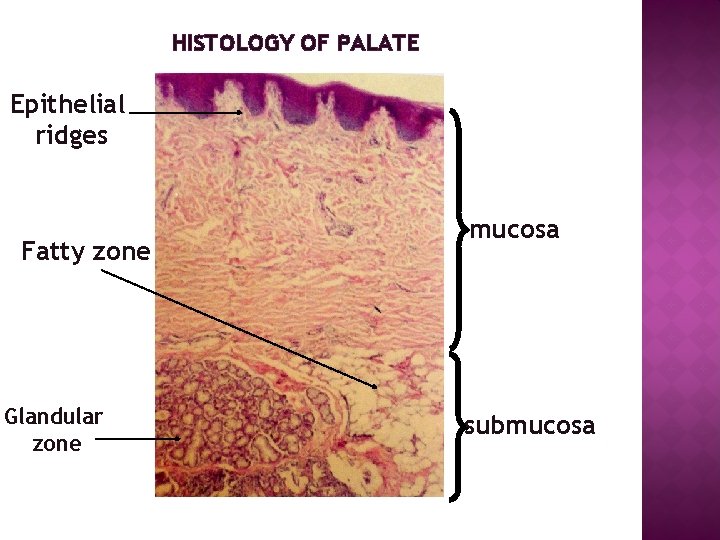
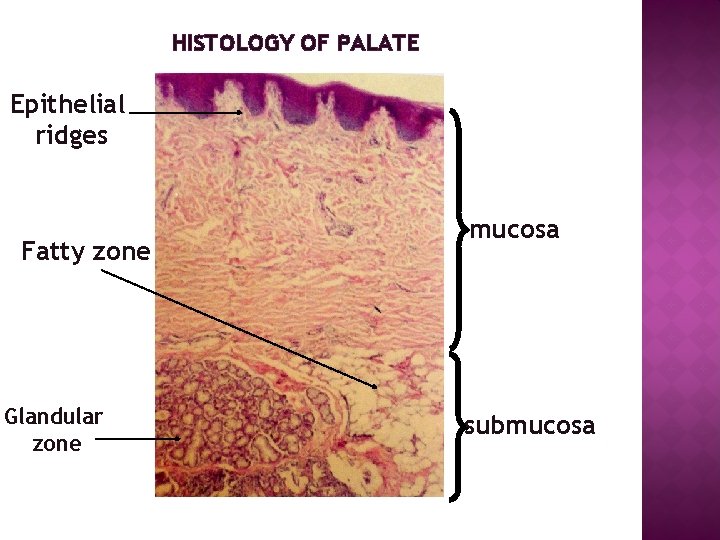
HISTOLOGY OF PALATE Epithelial ridges Fatty zone Glandular zone mucosa submucosa
II) LINING MUCOSA � Loosely attached – e. g alveolar mucosa, floor of mouth, vestibular fornix � Firmly attached – e. g lips , cheeks, ventral surface, tongue, soft palate
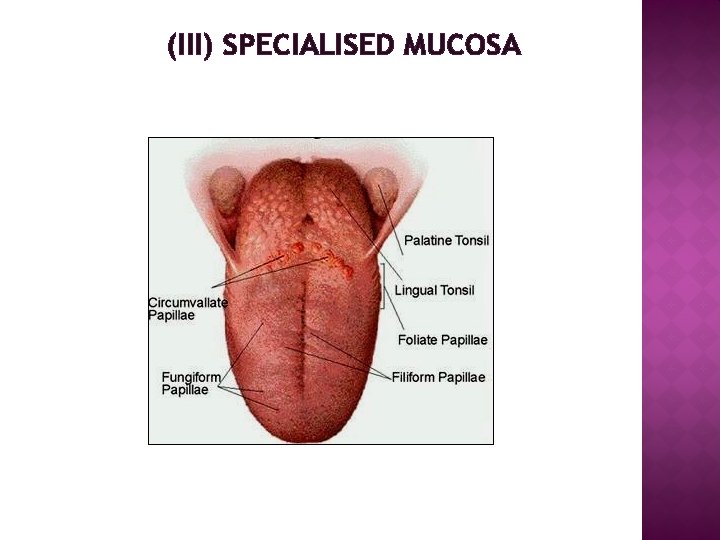
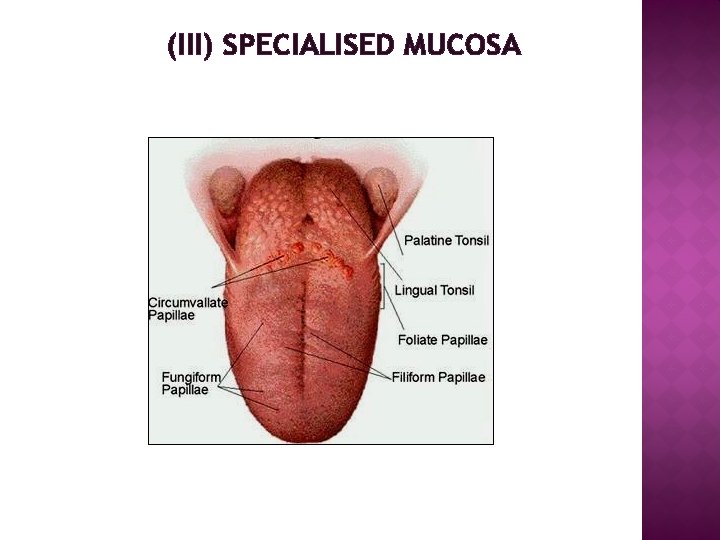
(III) SPECIALISED MUCOSA
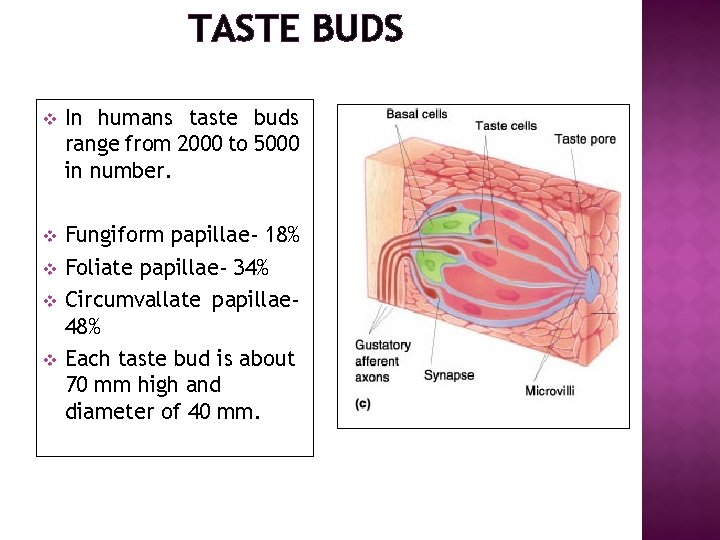
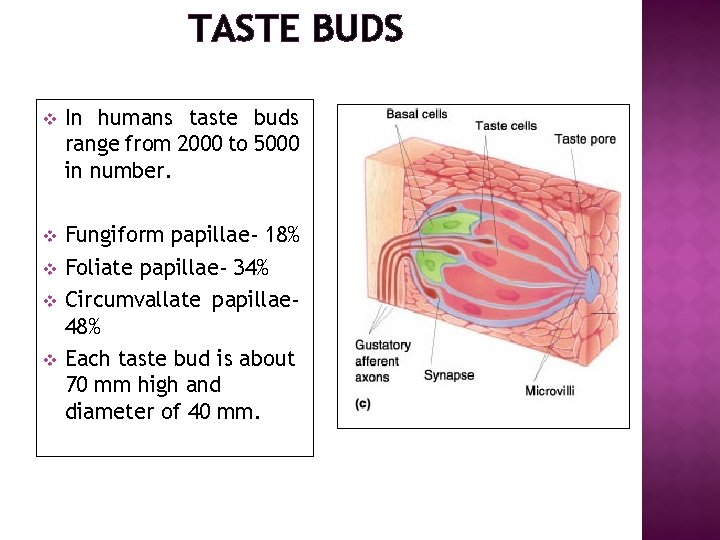
TASTE BUDS v In humans taste buds range from 2000 to 5000 in number. v Fungiform papillae- 18% Foliate papillae- 34% Circumvallate papillae 48% Each taste bud is about 70 mm high and diameter of 40 mm. v v v
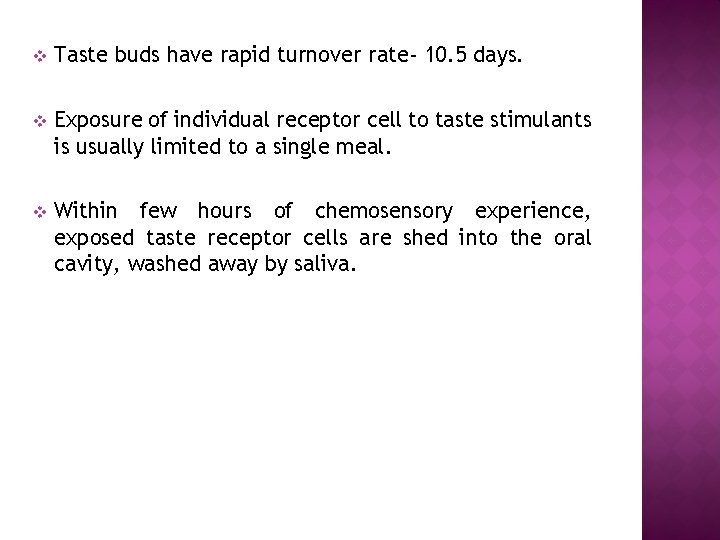
v Taste buds have rapid turnover rate- 10. 5 days. v Exposure of individual receptor cell to taste stimulants is usually limited to a single meal. v Within few hours of chemosensory experience, exposed taste receptor cells are shed into the oral cavity, washed away by saliva.
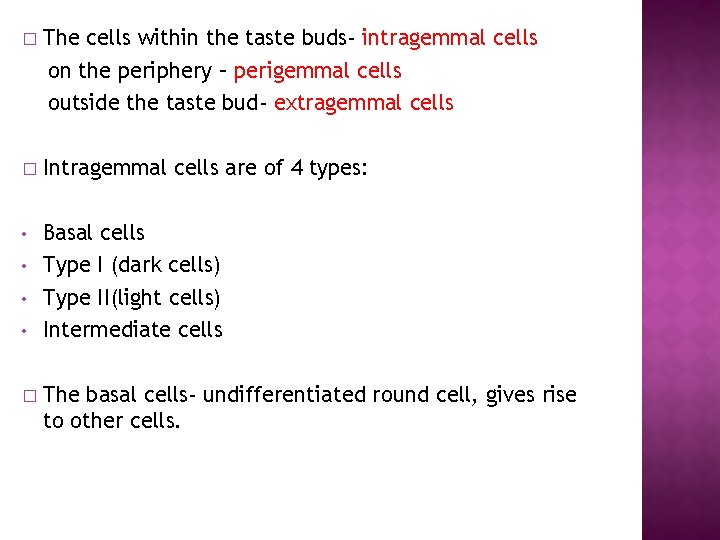
� The cells within the taste buds- intragemmal cells on the periphery – perigemmal cells outside the taste bud- extragemmal cells � Intragemmal cells are of 4 types: • Basal cells Type I (dark cells) Type II(light cells) Intermediate cells • • • � The basal cells- undifferentiated round cell, gives rise to other cells.
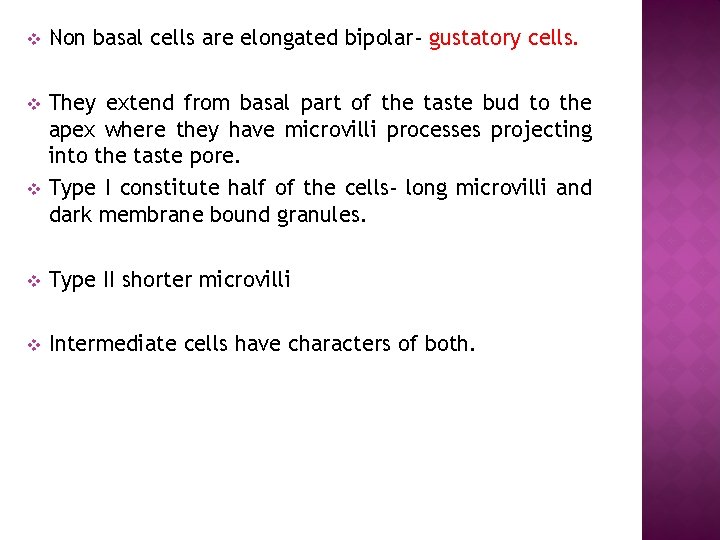
v Non basal cells are elongated bipolar- gustatory cells. v They extend from basal part of the taste bud to the apex where they have microvilli processes projecting into the taste pore. Type I constitute half of the cells- long microvilli and dark membrane bound granules. v v Type II shorter microvilli v Intermediate cells have characters of both.
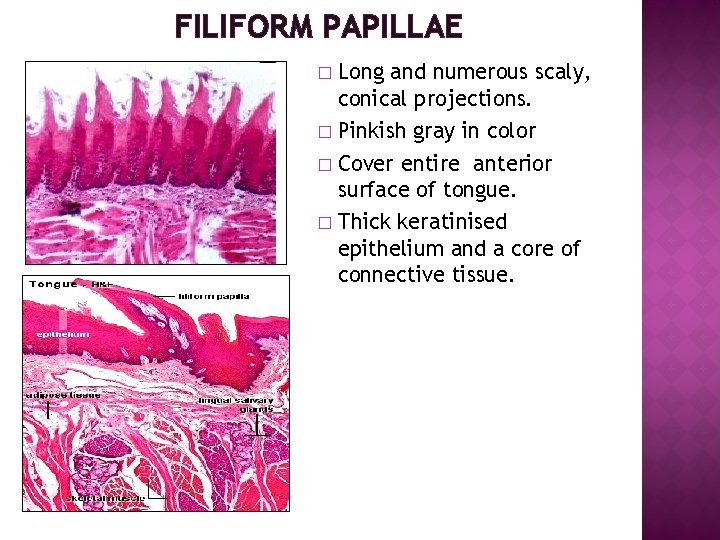
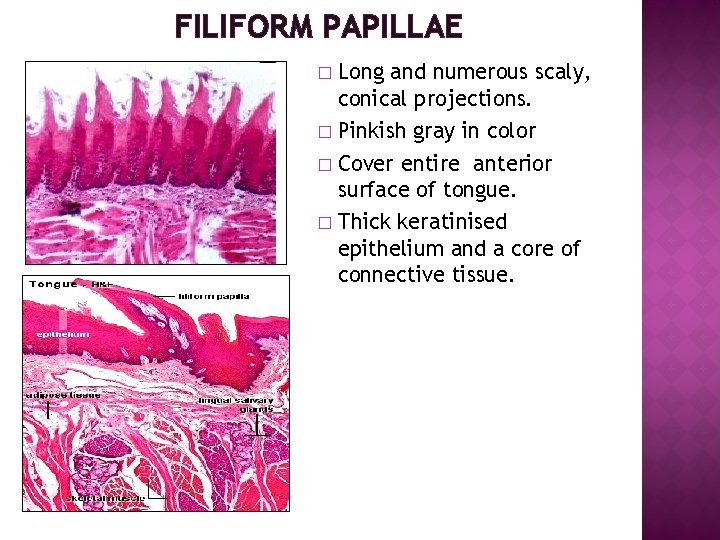
FILIFORM PAPILLAE Long and numerous scaly, conical projections. � Pinkish gray in color � Cover entire anterior surface of tongue. � Thick keratinised epithelium and a core of connective tissue. �
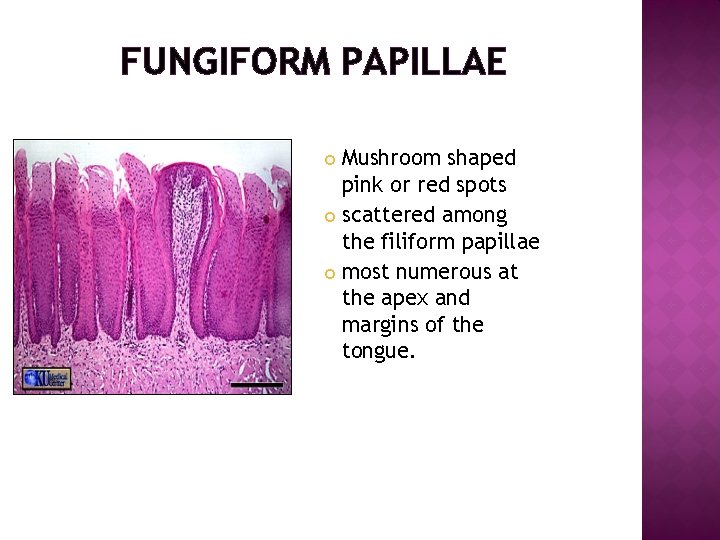
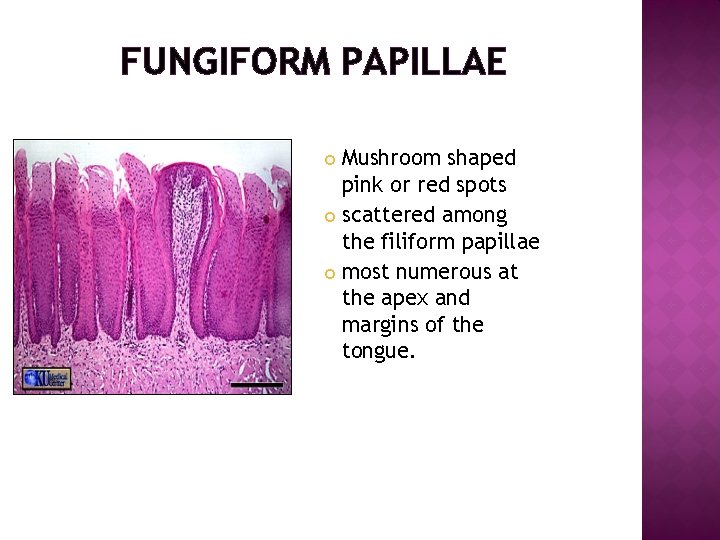
FUNGIFORM PAPILLAE Mushroom shaped pink or red spots scattered among the filiform papillae most numerous at the apex and margins of the tongue.
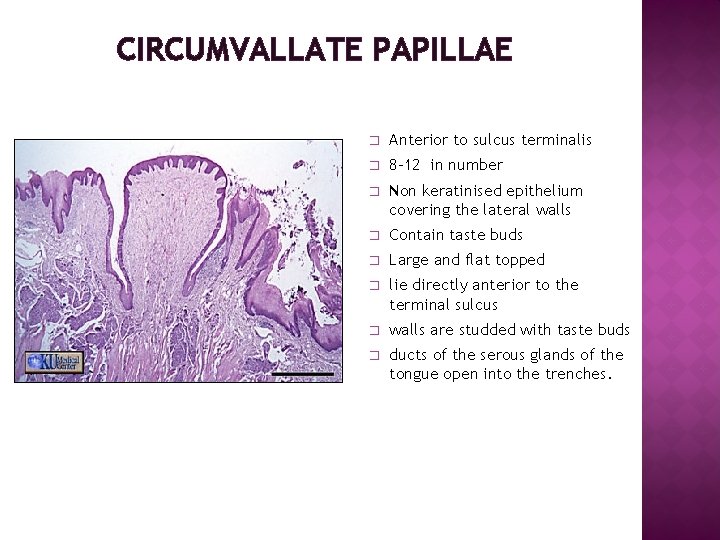
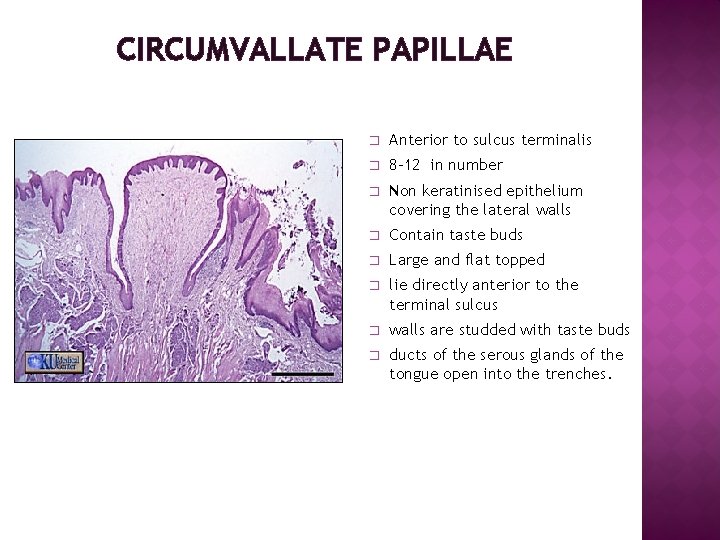
CIRCUMVALLATE PAPILLAE � Anterior to sulcus terminalis � 8 -12 in number � Non keratinised epithelium covering the lateral walls � Contain taste buds � Large and flat topped � lie directly anterior to the terminal sulcus � walls are studded with taste buds � ducts of the serous glands of the tongue open into the trenches.
FOLIATE PAPILLAE � Leaf like, present on lateral and posterior part of tongue. � More frequently seen in mammals than human beings � Contain few taste buds in the epithelium of lateral walls
 Parakeratinised
Parakeratinised Recueil de chant jeunesse adventiste pdf
Recueil de chant jeunesse adventiste pdf Alberts
Alberts Basal lamina and reticular lamina
Basal lamina and reticular lamina Single layer epithelium
Single layer epithelium Stratified squamous non-keratinized epithelium
Stratified squamous non-keratinized epithelium Hemicapsule
Hemicapsule Lining epithelium of soft palate
Lining epithelium of soft palate Non nobis domine non nobis sed nomini tuo ad gloriam
Non nobis domine non nobis sed nomini tuo ad gloriam Bene non escludibile e non rivale
Bene non escludibile e non rivale Non rival adalah
Non rival adalah Non posse non peccare
Non posse non peccare Tratta gli altri come vorresti essere trattato
Tratta gli altri come vorresti essere trattato Contoh pelarut protonik
Contoh pelarut protonik Chi non stima la vita non la merita
Chi non stima la vita non la merita Non nobis domine sed nomini tuo da gloriam
Non nobis domine sed nomini tuo da gloriam Parafrasi 3 canto
Parafrasi 3 canto Kennedy theory value of c for coarse silt
Kennedy theory value of c for coarse silt Non fidarti di chi non chiude gli occhi quando ti bacia
Non fidarti di chi non chiude gli occhi quando ti bacia Behavioral-rational approach to curriculum
Behavioral-rational approach to curriculum Non mihi, non tibi, sed nobis
Non mihi, non tibi, sed nobis No gyro approach
No gyro approach Quia non sunt
Quia non sunt Gli assiomi della comunicazione
Gli assiomi della comunicazione Dù ai nói đông nói tây lòng ta vẫn
Dù ai nói đông nói tây lòng ta vẫn Transpyloric plane
Transpyloric plane Characteristics of squamous epithelium
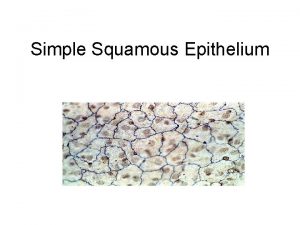
Characteristics of squamous epithelium Domaine apical
Domaine apical Olfactory cortex
Olfactory cortex Cuboidal epithelium tissue function
Cuboidal epithelium tissue function Larynx epithelium
Larynx epithelium Simple columnar epithelial
Simple columnar epithelial Reduced enamel epithelium
Reduced enamel epithelium Transitional epithelium function
Transitional epithelium function Stratified epithelium characteristics
Stratified epithelium characteristics Neural groove
Neural groove Dentoperiosteal fibers
Dentoperiosteal fibers Goblet cells of respiratory epithelium
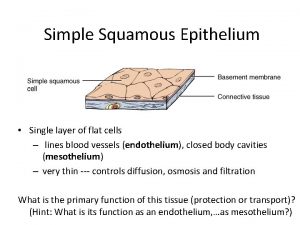
Goblet cells of respiratory epithelium Simple squamous epithelium
Simple squamous epithelium Endocrine histology
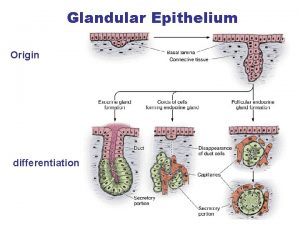
Endocrine histology