Treponema Pallidum UNIT 5 Contents v History v


- Slides: 47
Treponema Pallidum UNIT 5
Contents v History v Introduction v Pathogenicity v Syphilis v Laboratory diagnosis v Treatment v Prophylaxis
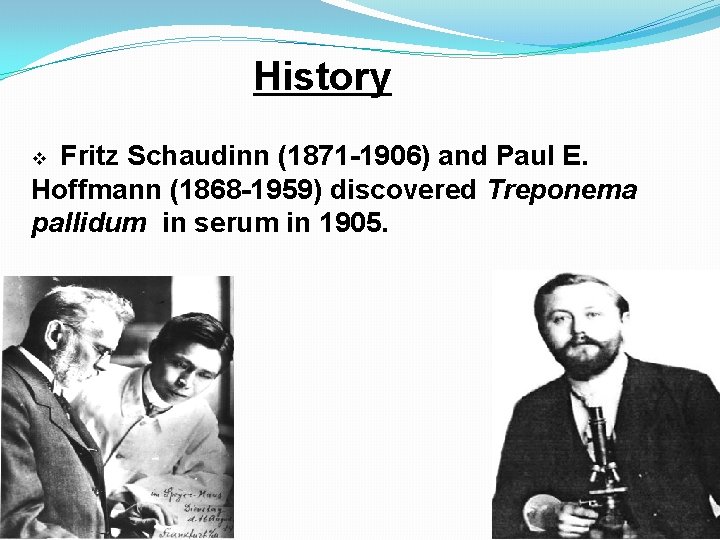
History Fritz Schaudinn (1871 -1906) and Paul E. Hoffmann (1868 -1959) discovered Treponema pallidum in serum in 1905. v
Recent Years v Scientist sequenced the genome of the bacteria Treponema Pallidum in 1998. v From this information scientist hoped to advance their ability to diagnose, treat, and prevent Syphilis
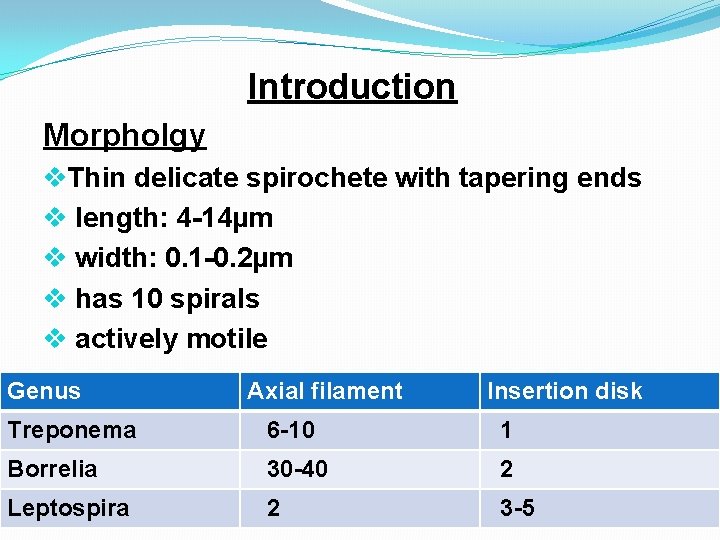
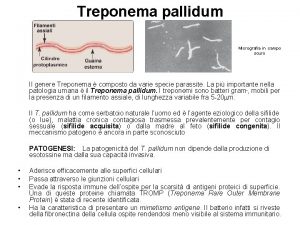
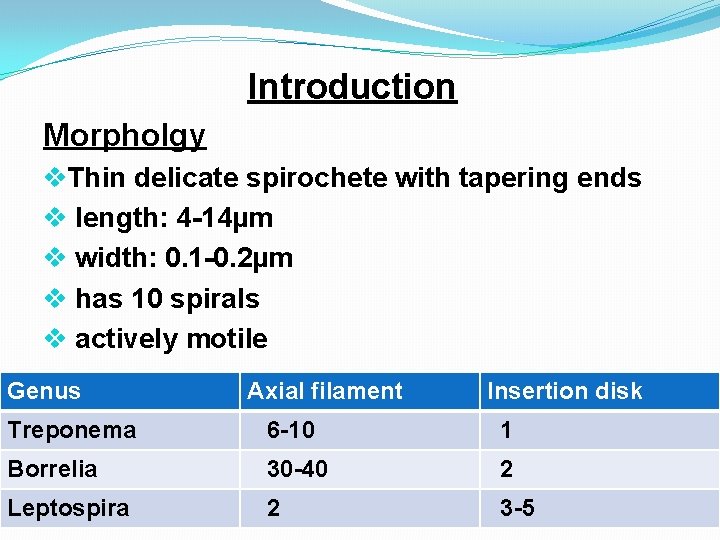
Introduction Morpholgy v. Thin delicate spirochete with tapering ends v length: 4 -14µm v width: 0. 1 -0. 2µm v has 10 spirals v actively motile Genus Axial filament Insertion disk Treponema 6 -10 1 Borrelia 30 -40 2 Leptospira 2 3 -5
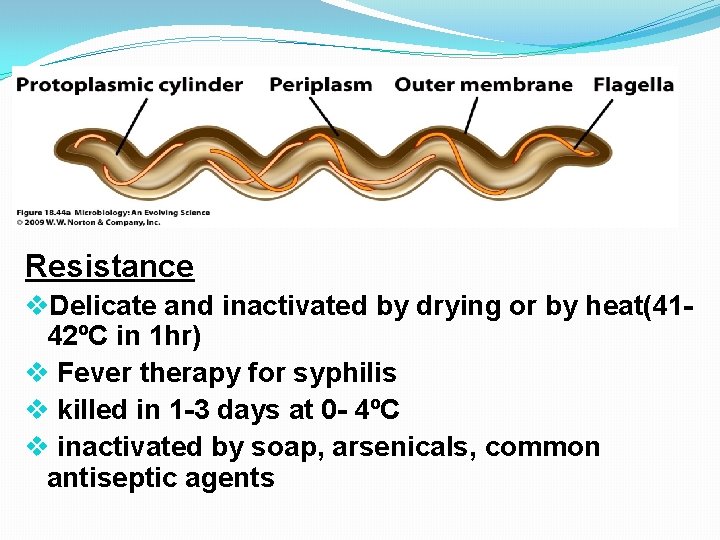
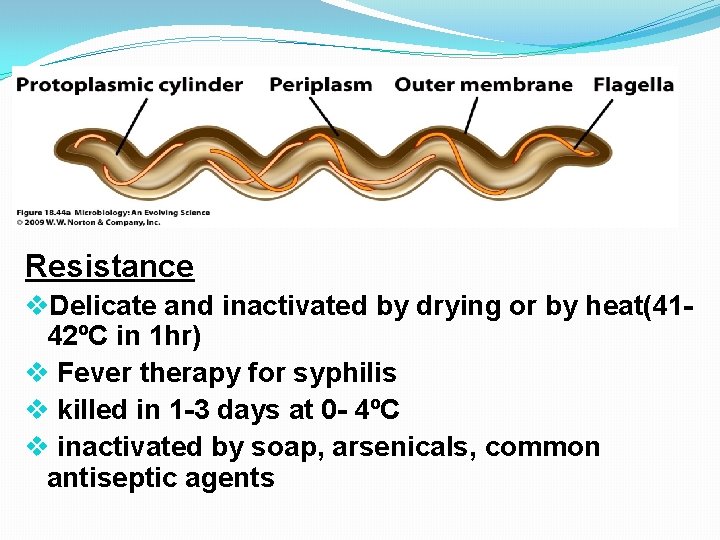
Resistance v. Delicate and inactivated by drying or by heat(4142ºC in 1 hr) v Fever therapy for syphilis v killed in 1 -3 days at 0 - 4ºC v inactivated by soap, arsenicals, common antiseptic agents
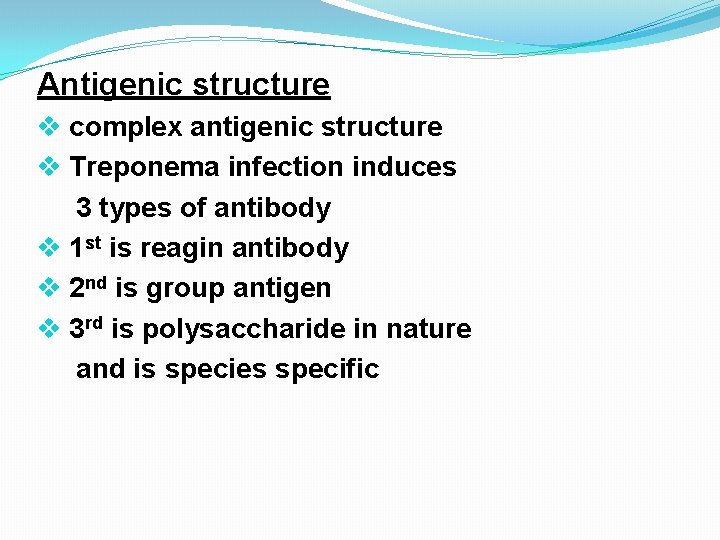
Antigenic structure v complex antigenic structure v Treponema infection induces 3 types of antibody v 1 st is reagin antibody v 2 nd is group antigen v 3 rd is polysaccharide in nature and is species specific
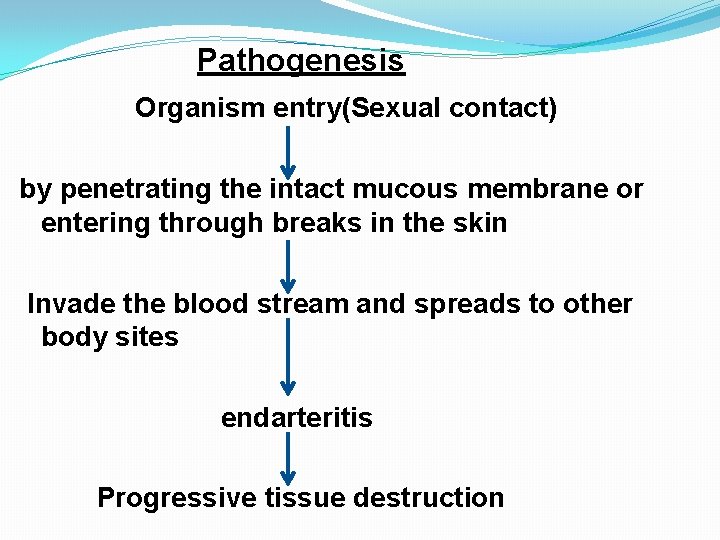
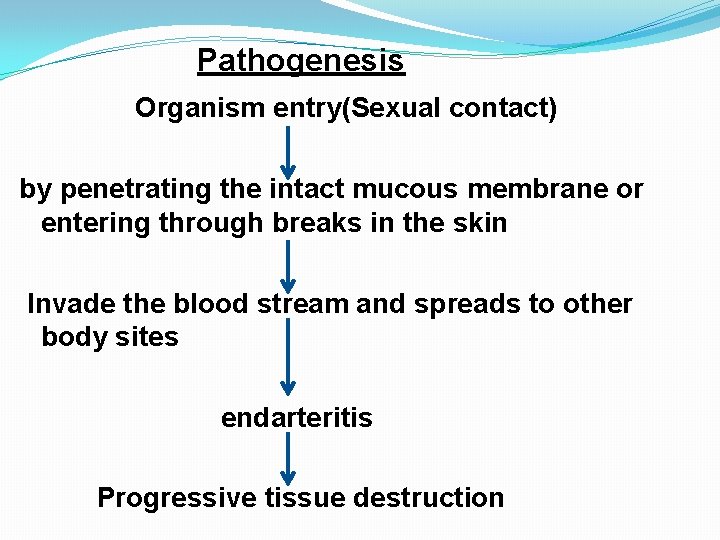
Pathogenesis Organism entry(Sexual contact) by penetrating the intact mucous membrane or entering through breaks in the skin Invade the blood stream and spreads to other body sites endarteritis Progressive tissue destruction
Syphilis v. Origin not definitely known v widely spread disease in Europe in 15 th century Types q Early Syphilis q Late Syphilis Neuro Syphilis Cardiovascular Syphilis Late “Benigin” Syphilis q Congenital Syphilis

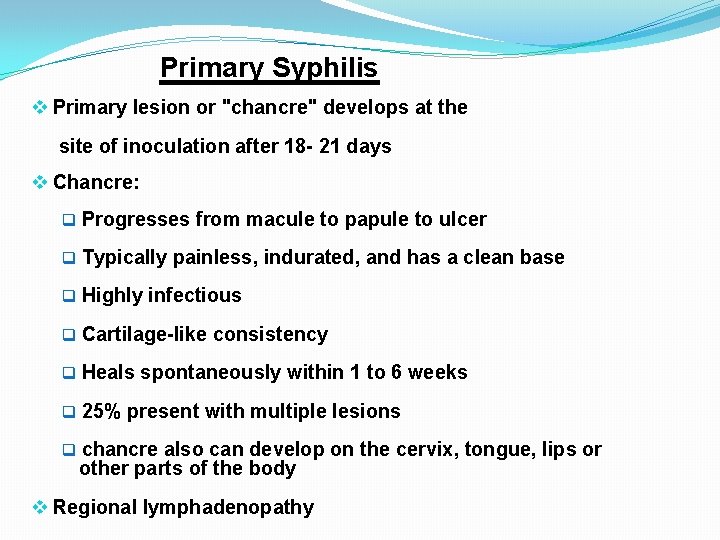
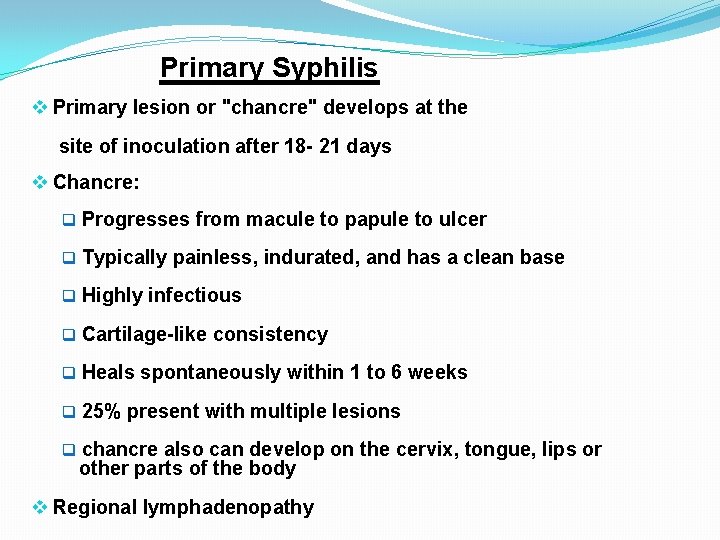
Primary Syphilis v Primary lesion or "chancre" develops at the site of inoculation after 18 - 21 days v Chancre: q Progresses from macule to papule to ulcer q Typically painless, indurated, and has a clean base q Highly infectious q Cartilage-like consistency q Heals spontaneously within 1 to 6 weeks q 25% present with multiple lesions q chancre also can develop on the cervix, tongue, lips or other parts of the body v Regional lymphadenopathy
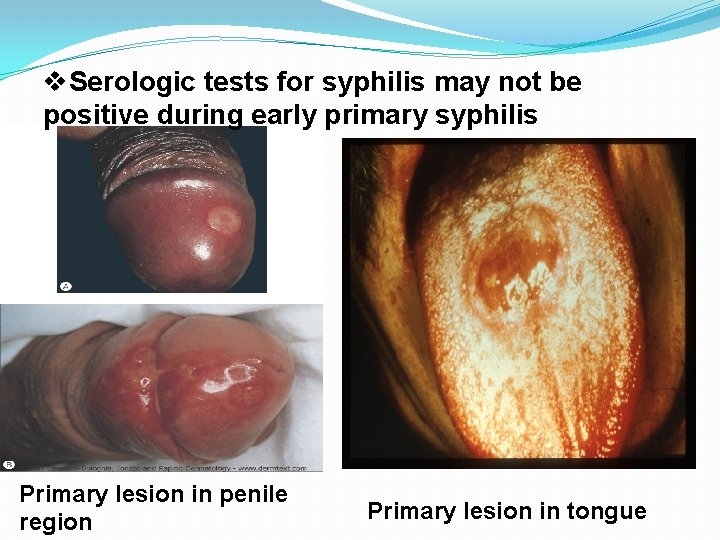
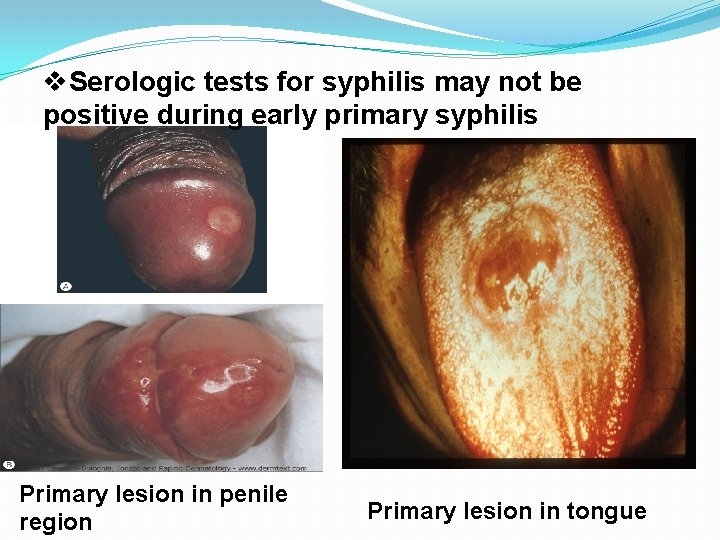
v. Serologic tests for syphilis may not be positive during early primary syphilis Primary lesion in penile region Primary lesion in tongue
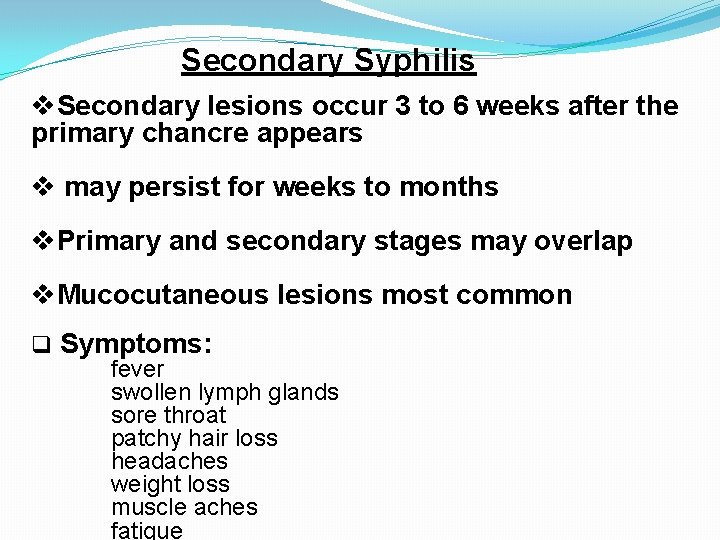
Secondary Syphilis v. Secondary lesions occur 3 to 6 weeks after the primary chancre appears v may persist for weeks to months v. Primary and secondary stages may overlap v. Mucocutaneous lesions most common q Symptoms: fever swollen lymph glands sore throat patchy hair loss headaches weight loss muscle aches fatigue
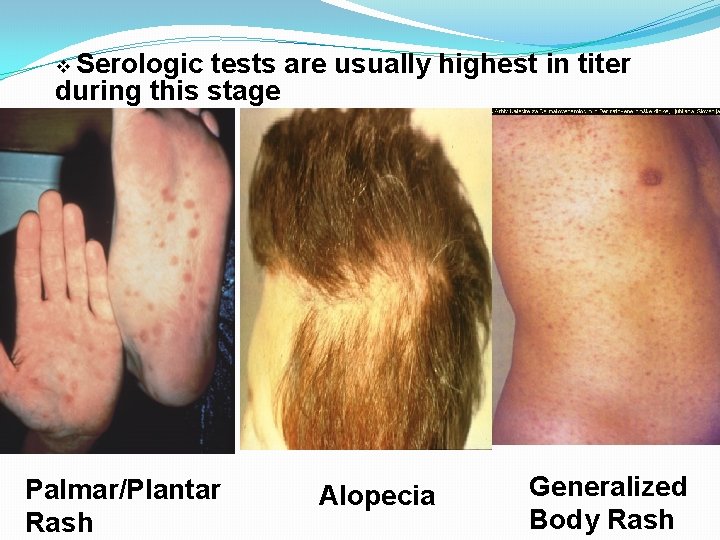
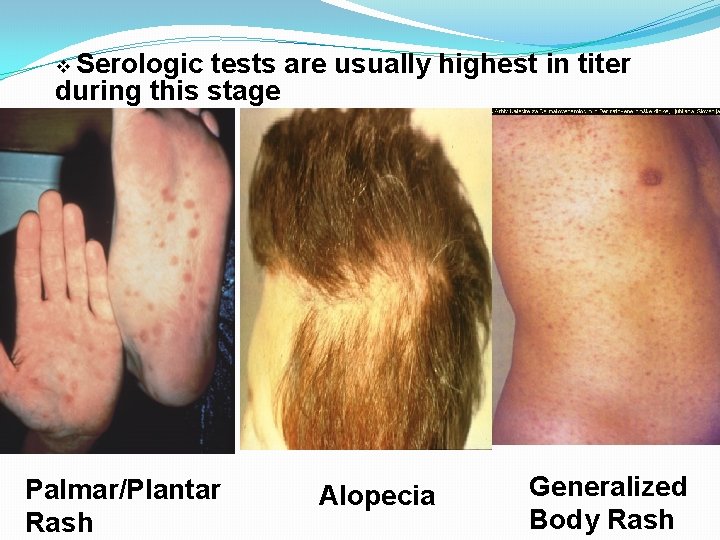
v Serologic tests are usually highest in titer during this stage Palmar/Plantar Rash Alopecia Generalized Body Rash
Latent Syphilis v. Host suppresses infection-no lesions are clinically apparent v. Only evidence is positive serologic test v. May occur between primary and secondary stages secondary relapses after secondary stage �Categories: �Early latent: <1 year duration �Late latent: 1 year duration
Late Syphilis v. Approximately 30% of untreated patients progress to the tertiary stage within 1 to 20 years v. Rare because of the widespread availability and use of antibiotics v. Manifestations �Gummatous lesions �Cardiovascular syphilis � Neurosyphilis
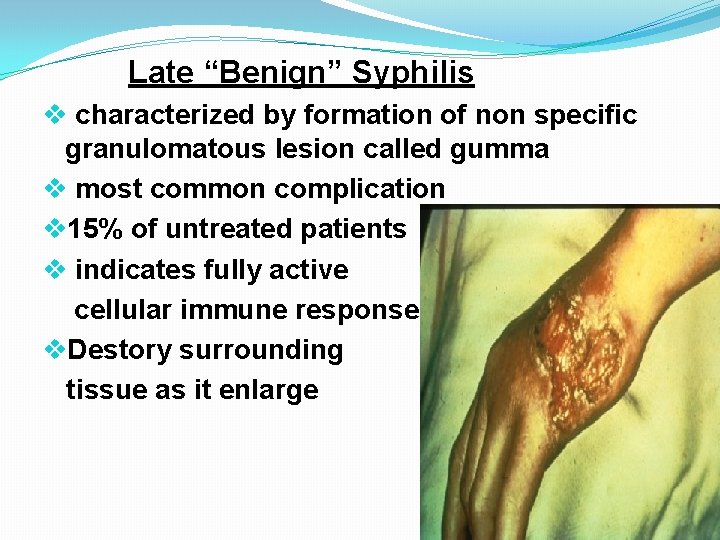
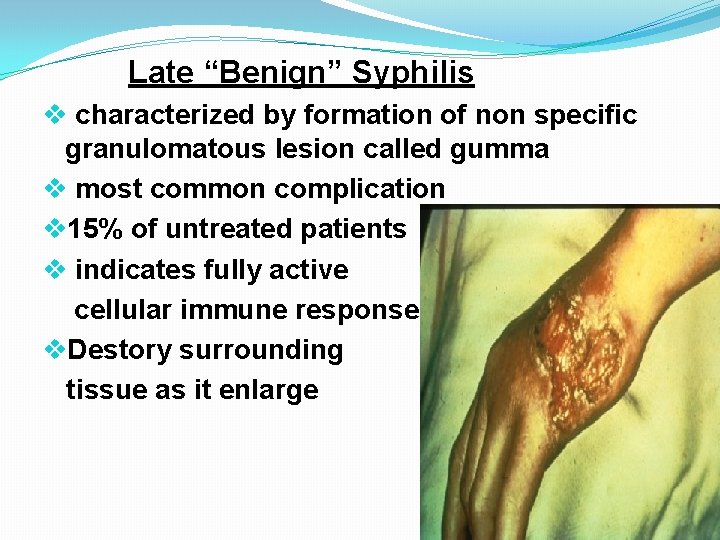
Late “Benign” Syphilis v characterized by formation of non specific granulomatous lesion called gumma v most common complication v 15% of untreated patients v indicates fully active cellular immune response v. Destory surrounding tissue as it enlarge
Cardiovascular Syphilis v 10% of untreated patients v inflammation of the small vessel that feed aorta and affect primarily the ascending aorta v Complications Aortic aneurysm dilation of aortic ring
Neuro Syhilis v May be symptomatic or asymptomatic v asymptomatic disease is characterized by CSF abnormalities v symptomatic infection is either meningovascular or parenchymatous v In meningovascular syphilis any cranial nerve may be inflammed and deafness and visual impairement may occur v Parenchymatous disease may involve the neurons of cerebrum or the spinal cord
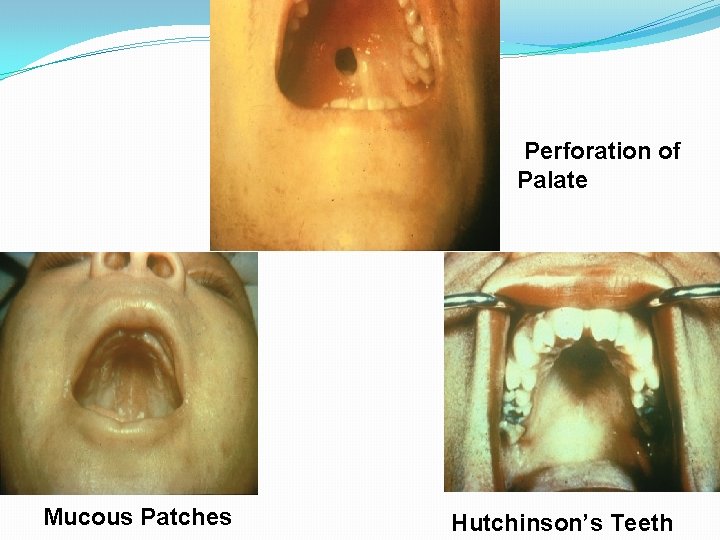
Congenital Syphilis v Occurs when T. pallidum is transmitted from a pregnant woman to her fetus v May lead to stillbirth &neonatal death infant disorders such as deafness neurologic impairment and bone deformities v Transmission can occur during any stage of syphilis v risk is much higher during primary and secondary syphilis v Fetal infection can occur during any trimester of pregnancy
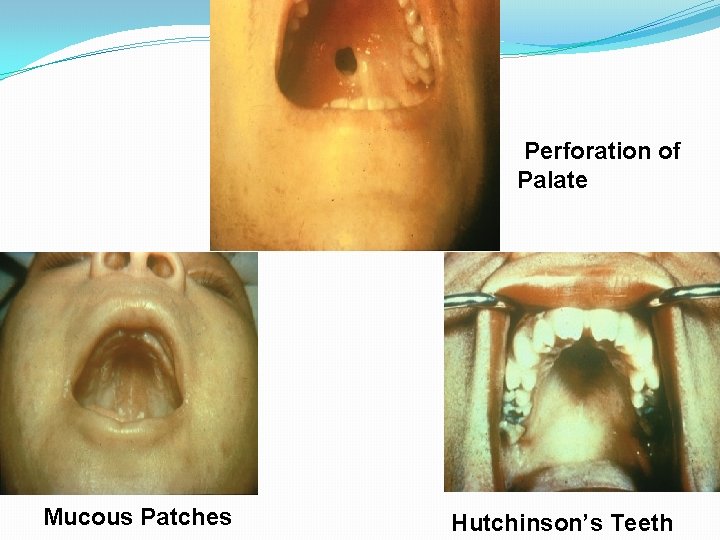
Perforation of Palate Mucous Patches Hutchinson’s Teeth
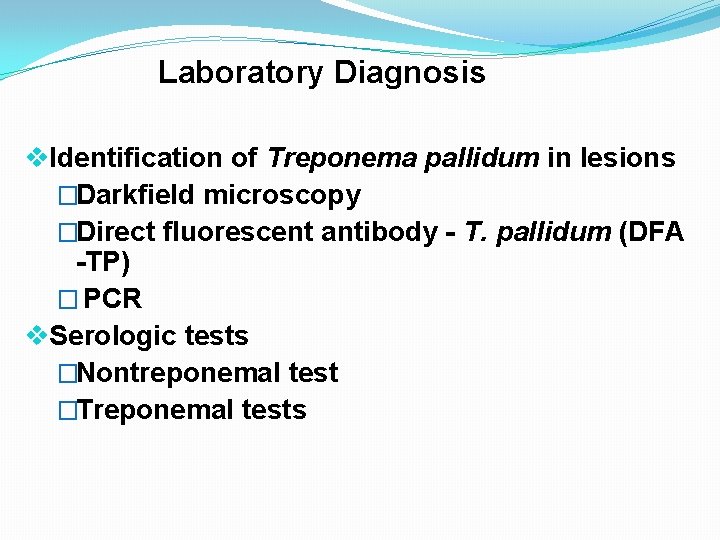
Laboratory Diagnosis v. Identification of Treponema pallidum in lesions �Darkfield microscopy �Direct fluorescent antibody - T. pallidum (DFA -TP) � PCR v. Serologic tests �Nontreponemal test �Treponemal tests
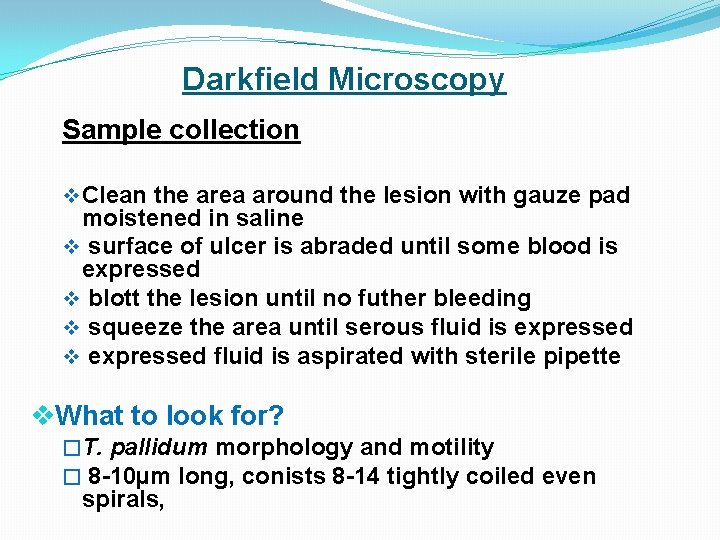
Darkfield Microscopy Sample collection v Clean the area around the lesion with gauze pad moistened in saline v surface of ulcer is abraded until some blood is expressed v blott the lesion until no futher bleeding v squeeze the area until serous fluid is expressed v expressed fluid is aspirated with sterile pipette v. What to look for? �T. pallidum morphology and motility � 8 -10µm long, conists 8 -14 tightly coiled even spirals,
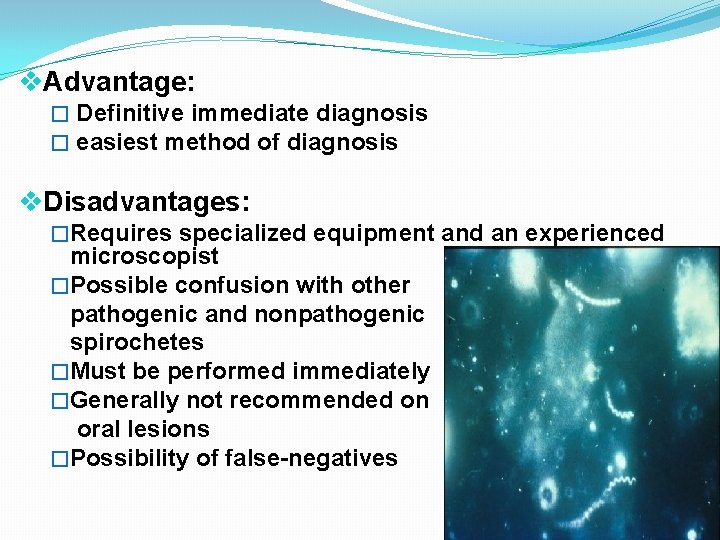
v. Advantage: � Definitive immediate diagnosis � easiest method of diagnosis v. Disadvantages: �Requires specialized equipment and an experienced microscopist �Possible confusion with other pathogenic and nonpathogenic spirochetes �Must be performed immediately �Generally not recommended on oral lesions �Possibility of false-negatives
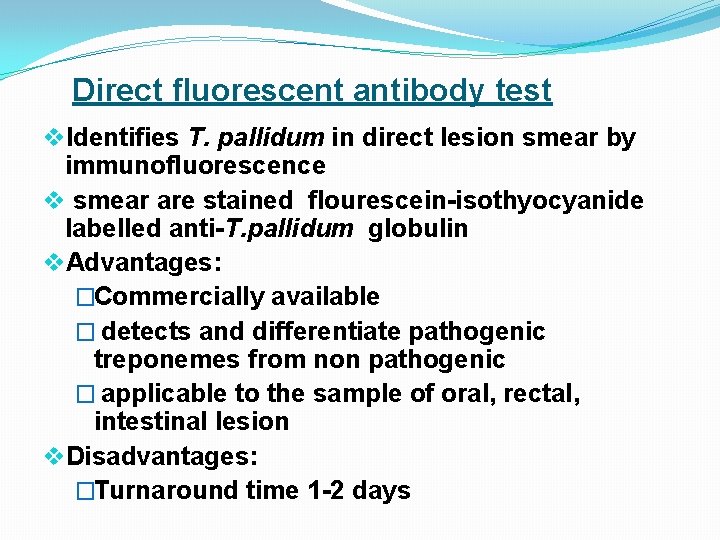
Direct fluorescent antibody test v. Identifies T. pallidum in direct lesion smear by immunofluorescence v smear are stained flourescein-isothyocyanide labelled anti-T. pallidum globulin v. Advantages: �Commercially available � detects and differentiate pathogenic treponemes from non pathogenic � applicable to the sample of oral, rectal, intestinal lesion v. Disadvantages: �Turnaround time 1 -2 days
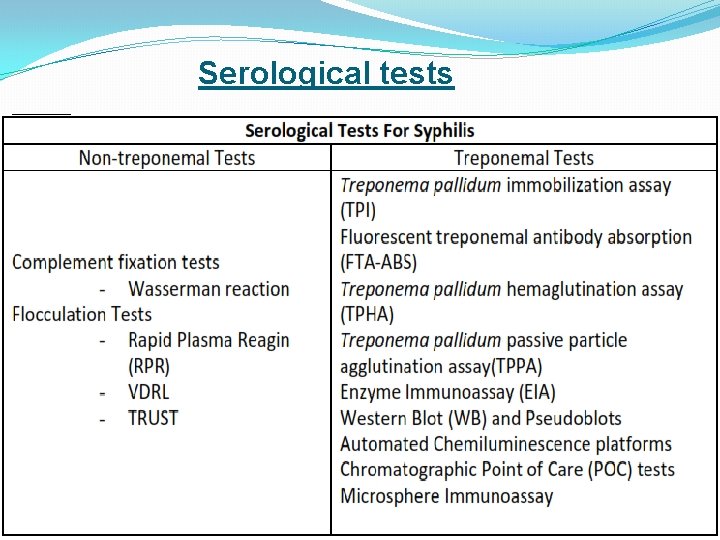
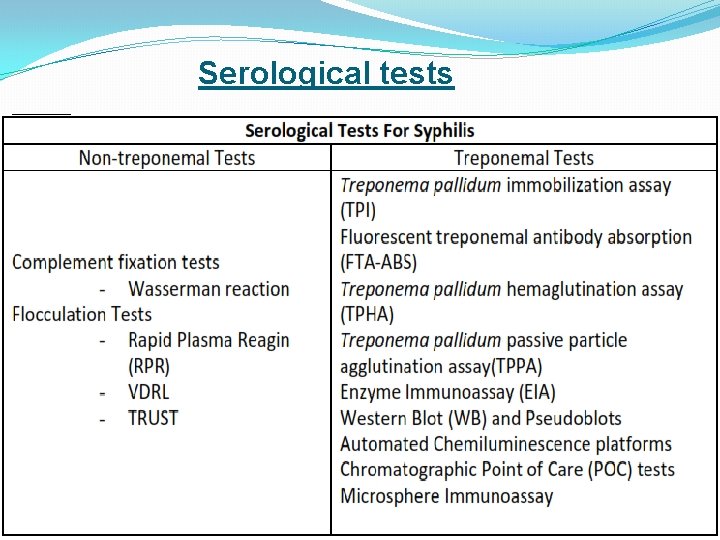
Serological tests

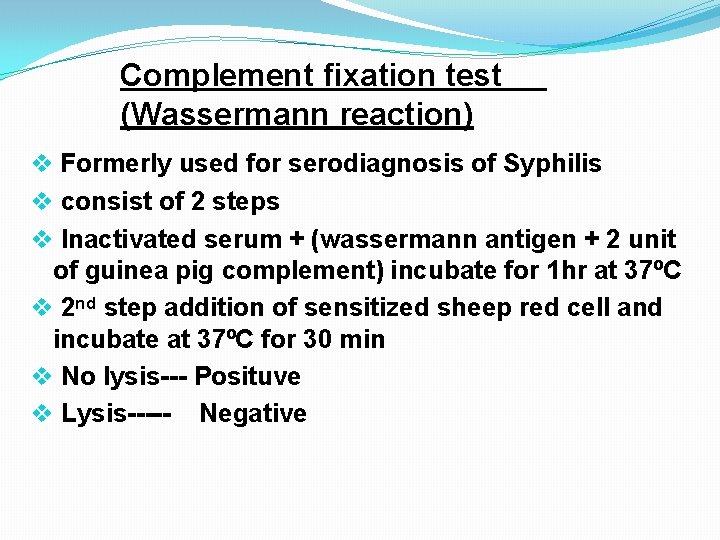
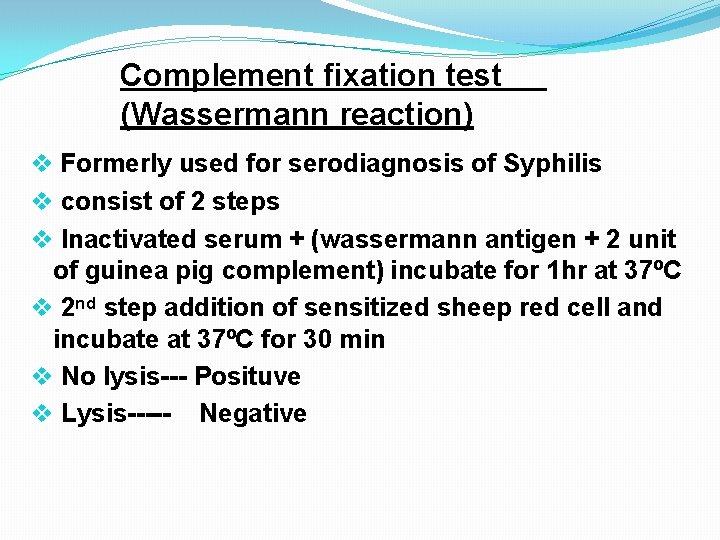
Complement fixation test (Wassermann reaction) v Formerly used for serodiagnosis of Syphilis v consist of 2 steps v Inactivated serum + (wassermann antigen + 2 unit of guinea pig complement) incubate for 1 hr at 37ºC v 2 nd step addition of sensitized sheep red cell and incubate at 37ºC for 30 min v No lysis--- Posituve v Lysis----- Negative
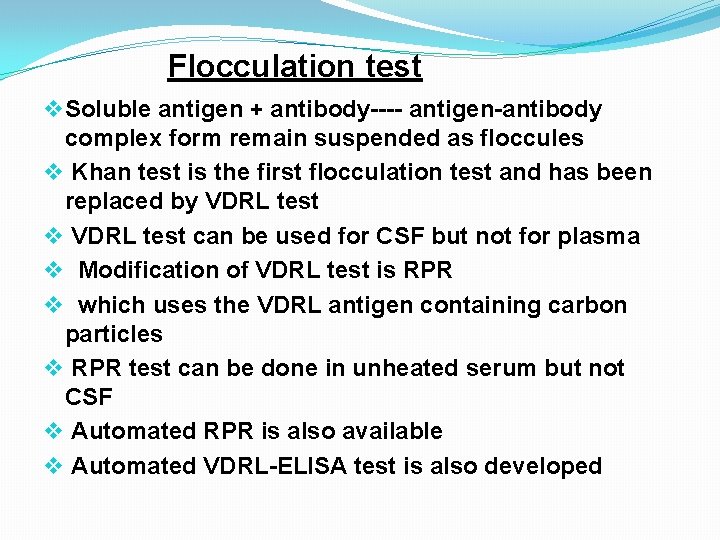
Flocculation test v Soluble antigen + antibody---- antigen-antibody complex form remain suspended as floccules v Khan test is the first flocculation test and has been replaced by VDRL test v VDRL test can be used for CSF but not for plasma v Modification of VDRL test is RPR v which uses the VDRL antigen containing carbon particles v RPR test can be done in unheated serum but not CSF v Automated RPR is also available v Automated VDRL-ELISA test is also developed
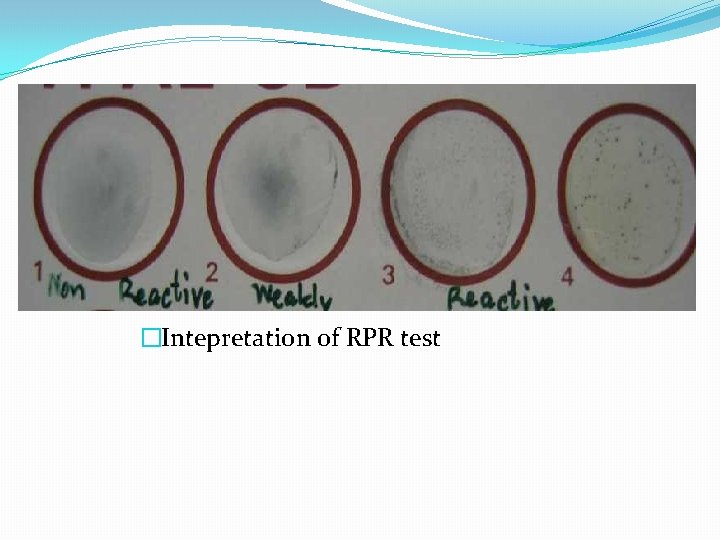
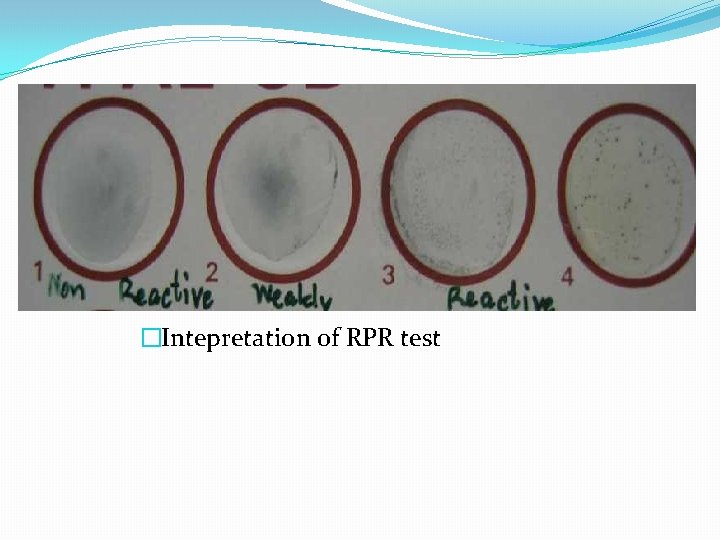
�Intepretation of RPR test
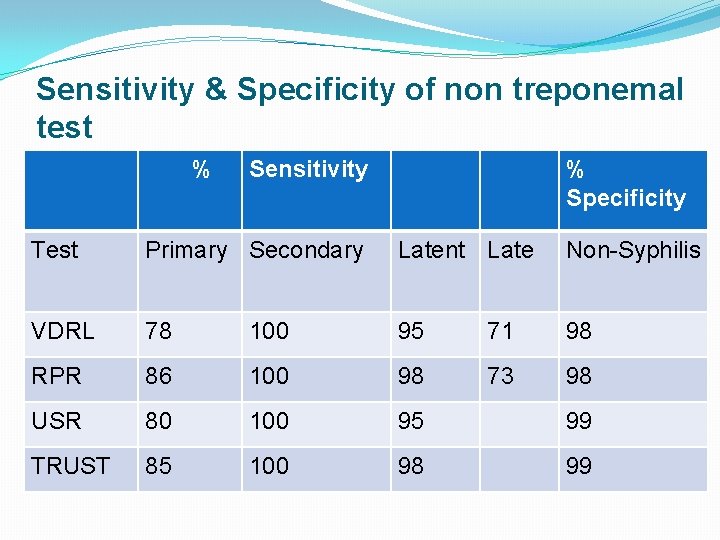
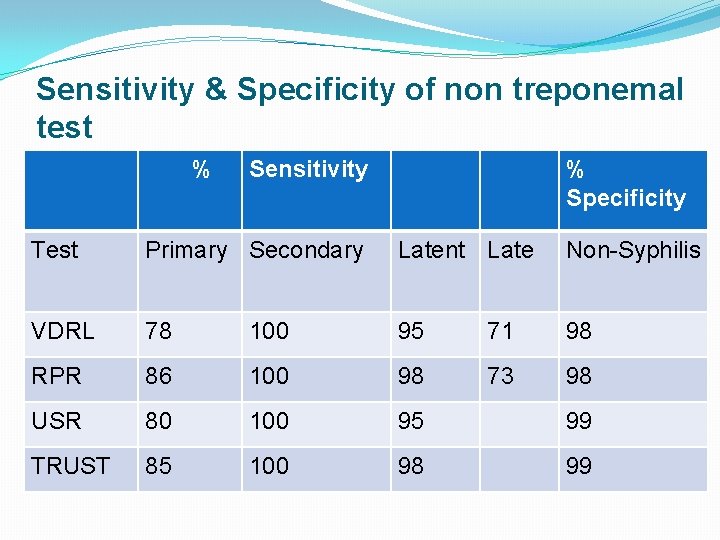
Sensitivity & Specificity of non treponemal test % Sensitivity % Specificity Test Primary Secondary Latent Late Non-Syphilis VDRL 78 100 95 71 98 RPR 86 100 98 73 98 USR 80 100 95 99 TRUST 85 100 98 99
Treponemal tests Treponema pallidum Immoblisation v. Test serum is incubated with complement and T. pallidum maintained in a complex medium anaerobically v If antibody is present the treponemas are immobilized i. e. non-motile when observed under dark ground ilumination v Complex procedure
Fluorescent treponemal antibody v Indirect immunofluorescent test using as antigen, smears prepared on slides with Nichol`s strain v Currently used modification is FTA-absorption (FTA-ABS) v test serum is pre-absorbed with sorbent (heat extract from cultures of non pathogenic Reiter strain) to eliminate group specific reactions v serum is layered on slide to which T. pallidum is fixed v FITC-labelled anti human immunolobulin is added and combine with patient antibodies adhering to T. pallidum, resulting in FITC stained spirochetes
�Modification of FTA-ABS is the FTA-ABS double stain � Conjugate used is rhodamine isothiocyanatelabeled antihuman globulin and counterstain FITClabeled anti T. pallidum conjugate
Hemagglutination methods v TPHA uses tanned erythrocytes sensitised with sonicated extract of T. pallidum as antigen v presence of treponemal antibodies in patient serum was detected by indirect agglutination of sensitized erythocytes v The procedure now employed is MHA-TP which can be automated v simpler to perform than flourescent antibody tests
Particle agglutination methods v MHA test has been modified to use gelatin particles rather than erythocytes as the antigen carrier creating T. pallidum particle agglutination v removal of preabsorption process v procedure similar to MHA-TP v Sensitivity and specificity similar to that of the FTA-ABS test
Latex agglutination methods v In 1985 1 st report of latex agglutination was publish v use cloned T. pallidum antigens bound to latex particles v easy to perform, fast and require less than 30 min for result
Enzyme immunoassay v First applied in 1975 as a serology test for syphilis v 2 types of EIA tests are available one uses sonicated T. pallidum as anitgen one uses cloned antigen v Advantage of EIA are capability to automate the test and run large number of samples in relatively short time
Immunoblotting v Used to detect Ig. G or Ig. M v to prepare the strips for T. pallidum immuno-blotting, intially boiled sodium dodecyl sulphate (SDS) extract of organism is electrophoresed through a gradient gel v After electrophoresis a sheet of nitrocellulose is placed on the top of gel & the protein immunodeterminants are electrophoretically transfer to blot v The blot is cut into strips and incubated with the patient serum v after incubation strips with patient serum are detected using enzyme and substrate lebeled antibody v Ig. M western blot is most sensitive to diagnose the congenital syphilis
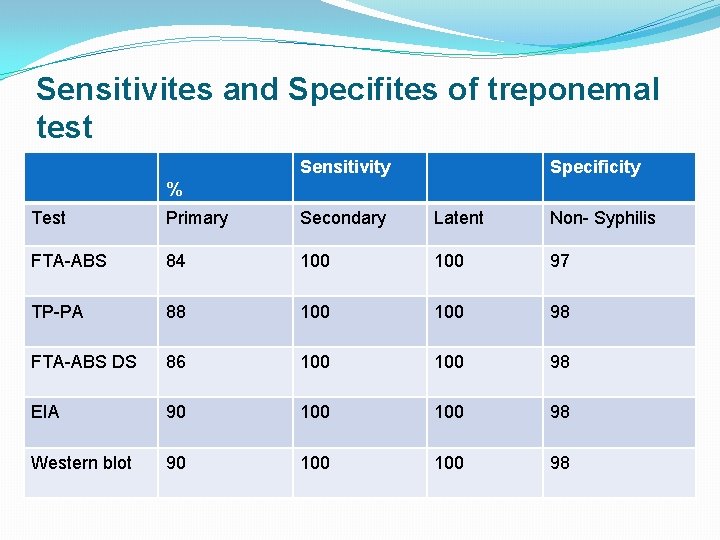
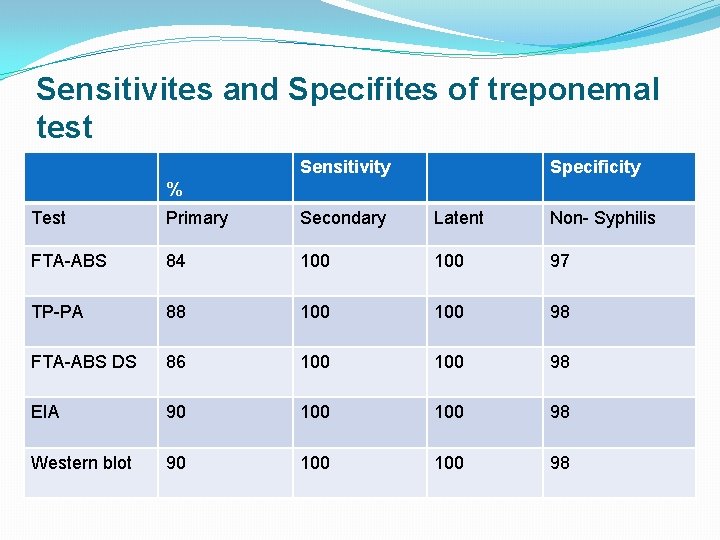
Sensitivites and Specifites of treponemal test Sensitivity Specificity % Test Primary Secondary Latent Non- Syphilis FTA-ABS 84 100 97 TP-PA 88 100 98 FTA-ABS DS 86 100 98 EIA 90 100 98 Western blot 90 100 98
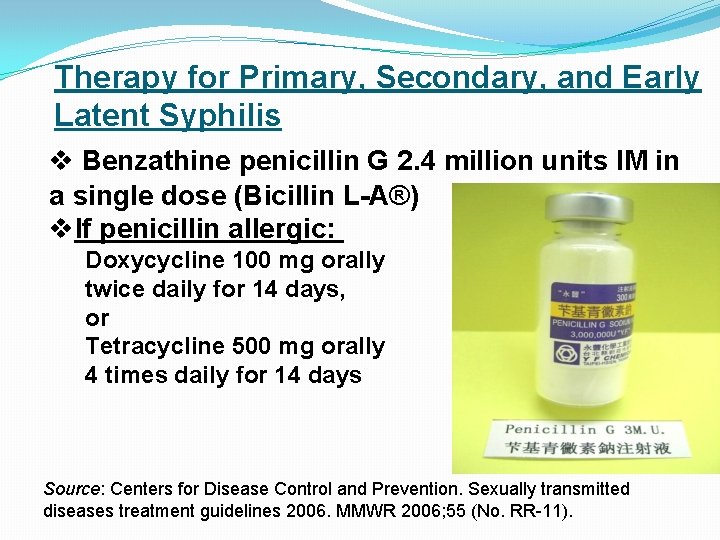
Therapy for Primary, Secondary, and Early Latent Syphilis v Benzathine penicillin G 2. 4 million units IM in a single dose (Bicillin L-A®) v. If penicillin allergic: Doxycycline 100 mg orally twice daily for 14 days, or Tetracycline 500 mg orally 4 times daily for 14 days Source: Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. MMWR 2006; 55 (No. RR-11).
Latent Syphilis of Unknown Duration v Benzathine penicillin G 7. 2 million units total, administered as 3 doses of 2. 4 million units IM each at 1 -week intervals v If penicillin allergic: �Doxycycline 100 mg orally twice daily for 28 days OR �Tetracycline 500 mg orally 4 times daily for 28 days Source: Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. MMWR 2006; 55 (No. RR-11).
Therapy for Neurosyphilis v. Aqueous crystalline penicillin G 18 -24 million units per day, administered as 3 -4 million units IV every 4 hours or continuous infusion for 10 -14 days IV v. Alternative regimen (if compliance can be ensured): Procaine penicillin 2. 4 million units IM once daily PLUS Probenecid 500 mg orally 4 times a day, both for 10 -14 days
Follow-Up v Primary or secondary syphilis �Re-examine at 6 and 12 months �Follow-up titers should be compared to the maximum or baseline nontreponemal titer obtained on day of treatment. v Latent syphilis �Re-examine at 6, 12, 18, and 24 months v HIV-infected patients � 3, 6, 9, and 12 months for primary or secondary syphilis � 6, 12, 18, and 24 months for latent syphilis v Neurosyphilis �Serologic testing as above �Repeat CSF examination at 6 -month intervals until normal
Prevention �Refraining from sexual contact with a individual infected with Syphilis will prevent spreading. �Using a condom will also help prevent transmission
References v Koneman`s Color Atlas and Textbook of Diagnostic Microbiology v Ananthanarayan and Paniker`s Textbook of Microbiology v Bailey & Scott`s Diagnostic Microbiology v Topley`s and Wilson
Thank you
 Espirales o hélices (espiroquetas)
Espirales o hélices (espiroquetas) Treponema pallidum
Treponema pallidum Dark ground microscopy
Dark ground microscopy What disease is caused by treponema pallidum
What disease is caused by treponema pallidum What disease is caused by treponema pallidum
What disease is caused by treponema pallidum Treponema pallidum microbiologia
Treponema pallidum microbiologia Extrapyramidal movements
Extrapyramidal movements Treponema palladium
Treponema palladium Unit 10, unit 10 review tests, unit 10 general test
Unit 10, unit 10 review tests, unit 10 general test Also history physical
Also history physical Introduction for portfolio
Introduction for portfolio Deep perineal pouch contents
Deep perineal pouch contents Febrile non hemolytic transfusion reaction
Febrile non hemolytic transfusion reaction Ffp vs platelets
Ffp vs platelets Mediastinum
Mediastinum Adductor hiatus
Adductor hiatus Horizontal
Horizontal The immortal life of henrietta lacks table of contents
The immortal life of henrietta lacks table of contents Medial lemniscus
Medial lemniscus Teres major origin and insertion
Teres major origin and insertion Ark
Ark Comic book table
Comic book table Falciform ligament
Falciform ligament Mla table of contents
Mla table of contents Contents of stylistic lexis
Contents of stylistic lexis How to make school magazine cover page
How to make school magazine cover page What is methodology
What is methodology Appendix in report
Appendix in report Cryoprecipitate components
Cryoprecipitate components Anterior mediastinum contents
Anterior mediastinum contents Pericardium and mediastinum
Pericardium and mediastinum Abstract vs introduction
Abstract vs introduction Persepolis table of contents
Persepolis table of contents Persepolis table of contents
Persepolis table of contents Interactive notebook table of contents
Interactive notebook table of contents Cryoprecipitate dose
Cryoprecipitate dose Contents of interpeduncular fossa
Contents of interpeduncular fossa Covering of the spermatic cord
Covering of the spermatic cord Greater sciatic foramen
Greater sciatic foramen Event management content
Event management content Contents of the middle mediastinum
Contents of the middle mediastinum Posterior mediastinum contents
Posterior mediastinum contents Contents of carotid sheath
Contents of carotid sheath Triangular space contents
Triangular space contents Curriculum vitaem
Curriculum vitaem Ctd module 3
Ctd module 3 Preparation of cost audit report
Preparation of cost audit report Civics interactive notebook
Civics interactive notebook