Treatment complications drug interactions and drug resistance Dr











- Slides: 39

Treatment complications, drug interactions and drug resistance Dr Sarah Mungall Avon Tuberculosis Clinic 1 st March 2018
Aim of talk • Drug toxicity • Drug interactions • Drug resistance • Anti TNF • HIV

Drug toxicity may be related to: 1. Side effects of TB medication (counsel carefully when starting treatment) 2. Drug interactions 3. Drug doses (consider this when deciding whether to prescribe Rifater and ethambutol or Voractiv)

Drug Interactions • • Antiretroviral therapy Warfarin Steroids Methadone Anticonvulsants Sulphonylureas Hormonal Contraception Cardiac medication

Side effects Rifampicin Hepatotoxicity, rash, fever, blood disorders Isoniazid Hepatotoxicity, peripheral neuropathy, rash, fever, blood disorders Pyrazinamide Hepatotoxicity, rash, fever, arthralgia, blood disorders Ethambutol Optic neuritis, rash (rarely)

1. 2. 3. 4. Hepatotoxicity Rash and red man syndrome Optic neuritis Peripheral neuropathy
1. Hepatotoxicity stop all TB treatment if: a) ALT >5 x upper limit of normal or b) bilirubin or ALP >2 x upper limit of normal or c) ALT 3 -5 times upper limit of normal and symptoms
Risk factors for hepatotoxicity 1. Hepatitis B or C infection 2. Heavy alcohol use 3. Malnutrition or low serum albumin at baseline 4. Cirrhosis or any other chronic liver disease 5. Other concurrent potentially hepatotoxic medication 6. Elderly 7. During pregnancy or up to 3 months post partum
Hepatitis C and Latent TB infection • 29% HCV have LTBI • 26% LTBI have HCV Aldridge RW, Hayward AC, Hemming S, et al High prevalence of latent tuberculosis and bloodborne virus infection in a homeless population Thorax Published Online First: 29 January 2018. doi: 10. 1136/thoraxjnl-2016 -209579
Re-introduction after drug induced liver injury (DILI) If well and not infectious wait for liver function to return to normal / <twice upper limit of normal if unwell or infectious or immunocompromised give ethambutol and injectable +/- moxifloxacin until liver function settles Isoniazid has a short half life, risk of drug resistance if given as monotherapy for >5 days
Re-introduction after drug induced liver injury (DILI) Two schools of thought: Slow re-introduction (BTS) Fast re-introduction (ATS)

What is the risk of hepatotoxicity with reintroduction of standard TB treatment? Three Different Regimens for Reintroduction of Anti-Tuberculosis Drugs. 11% developed recurrence of DILI, low pre treatment albumin only risk factor No significant difference between 3 arms Surendra K. Sharma et al. Clin Infect Dis. 2010; 50: 833 -839 © 2010 by the Infectious Diseases Society of America
The jury is still out. . . risk of drug resistance with slow reintroduction risk of hepatotoxicity with fast reintroduction (may not be as much as originally thought)
What I do 1. Always check baseline LFTs and Hepatitis B and C 2. Recheck LFTs only if symptoms or abnormal at baseline 3. If ALT >5 x stop all TB treatment and admit if symptomatic 4. Ultrasound liver, full liver blood screen and synthetic function 5. Consider hepatology opinion 6. Slower reintroduction if symptomatic/comorbidities ( cover with ethambutol and injectable/quinolone) 7. Faster if asymptomatic 8. Faster if inpatient 9. Think about weekends and blood tests 10. Do as an inpatient if patient is unwell or not reliable (low threshold)
Case 1 • • • 46 year old male Background of diabetes Commenced on treatment for pulmonary and pleural TB Baseline LFTs Developed symptoms of hepatotoxicity 1 month later
Case 1 • All treatment stopped and admitted to hospital • Unwell with extensive disease and immunocompromised due to diabetes • Liver function took a long time to settle
Case 1 • Treated with intramuscular capreomycin and ethambutol • Found to have isoniazid and streptomycin resistance • Liver function improving therefore treatment reintroduced

Started TB treatment Stopped TB treatment Treatment reintroduced, E, R, P (slow)
Case 1 principles of treatment burden of disease and immunocompetence of host risk of side effects with drug regimen

Rash • Cetirizine 10 mg od and titrate dose up (high doses of 20 mg bd often needed) • Check LFTs Red man syndrome • due to rifampicin • use rifampicin resistant regiment
Peripheral neuropathy • age and dose related • tolerated well in children Risks increased by: • age • renal failure • alcohol • diabetes • nutritional status

Peripheral neuropathy • Pyridoxine as prophylaxis • Titration of pyridoxine dose above 20 mg if symptoms of peripheral neuropathy does not work in my experience • Needs to be changed to isoniazid resistant regimen if peripheral neuropathy develops ( get nerve conduction studies)
Optic neuritis • Baseline Ishihara and visual acuity • Cumulative dose is important • Reporting of symptoms most important • Ask and document about blurred vision or change in colour vision at every appointment • Follow up Ishihara and visual acuity if on long term ethambutol (isoniazid resistant regimen)
Drug Resistance Need to send samples to get information on drug resistance
Case 2 • • 30 year old Somali lady Presented with back pain and weight loss MRI spine performed – consistent with TB Commenced on standard TB treatment with Voractiv
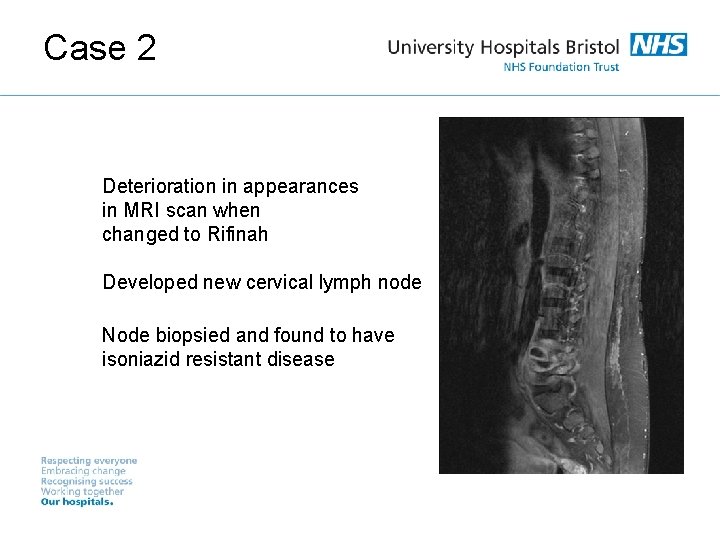
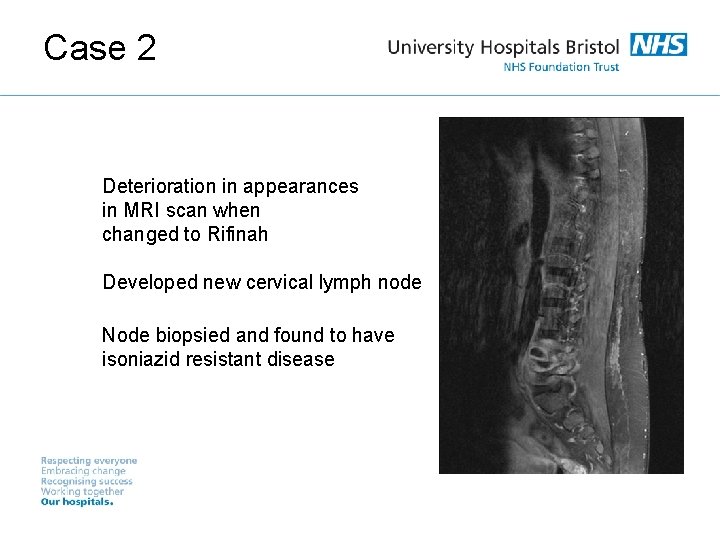
Case 2 Deterioration in appearances in MRI scan when changed to Rifinah Developed new cervical lymph node Node biopsied and found to have isoniazid resistant disease
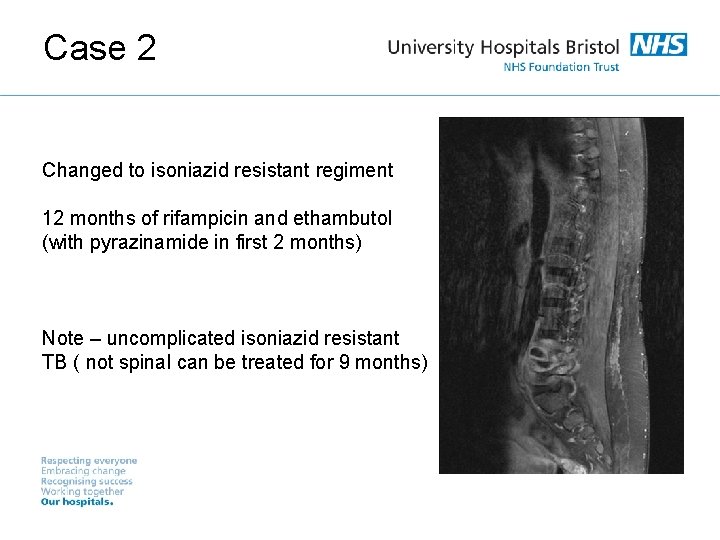
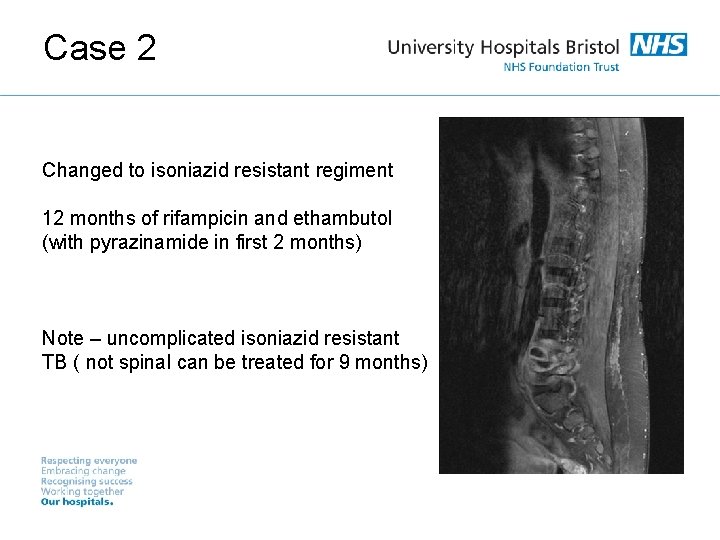
Case 2 Changed to isoniazid resistant regiment 12 months of rifampicin and ethambutol (with pyrazinamide in first 2 months) Note – uncomplicated isoniazid resistant TB ( not spinal can be treated for 9 months)
Drug Resistance What increases the risk of drug resistance? • Previous TB treatment • Born in area with high rates of drug resistance • HIV co infection • Living in London • Aged 25 -44 • Male
Pyrazinamide resistance • M Bovis • Resistant to pyrazinamide • Needs 9 months of treatment

Proportion of TB cases with isoniazid resistance or MDR-TB, UK, 2004 -2013 Source: Enhance Tuberculosis Surveillance (ETS), Enhanced Surveillance of Mycobacterial Infections (ESMI) Data as at: May 2014. Prepared by: TB Section, Centre for Infectious Disease Surveillance and Control, Public Health England Tuberculosis in the UK: 2014 report 30
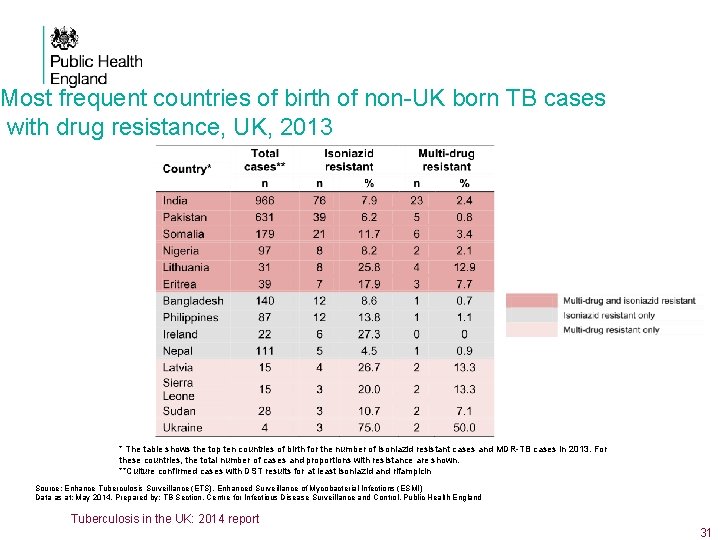
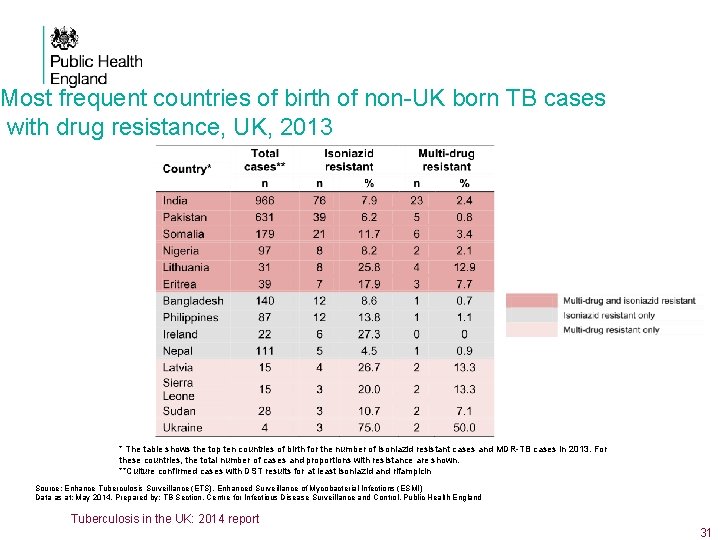
Most frequent countries of birth of non-UK born TB cases with drug resistance, UK, 2013 * The table shows the top ten countries of birth for the number of isoniazid resistant cases and MDR-TB cases in 2013. For these countries, the total number of cases and proportions with resistance are shown. **Culture confirmed cases with DST results for at least isoniazid and rifampicin Source: Enhance Tuberculosis Surveillance (ETS), Enhanced Surveillance of Mycobacterial Infections (ESMI) Data as at: May 2014. Prepared by: TB Section, Centre for Infectious Disease Surveillance and Control, Public Health England Tuberculosis in the UK: 2014 report 31
TB reactivation with anti TNF • 2001 Post marketing surveillance (FDA Adverse events reporting) in USA on Infliximab 1998 -May 2001 revealed 70 cases of reactivated TB with infliximab (1) with 4 of 12 deaths directly attributed to TB (121, 000 patients) • 56% extra pulmonary and 24% disseminated disease • Patients also at risk of primary infection • For infliximab, majority of cases occurred within 3 cycles of treatment at a median of 12 weeks from starting treatment and for adalimumab within 8 months • Fivefold increase in reactivation 32
• HIV and TB if new diagnosis of HIV at time of starting TB treatment aim to start ART within 8 -12 weeks if CD 4 count <50 aim to start within 2 weeks British HIV Association guidelines for the management of TB/HIV co-infection in adults 2017 (draft)
TB and steroids evidence is in CNS and pericardial disease sometimes used in pleural disease ( no evidence) used in IRIS
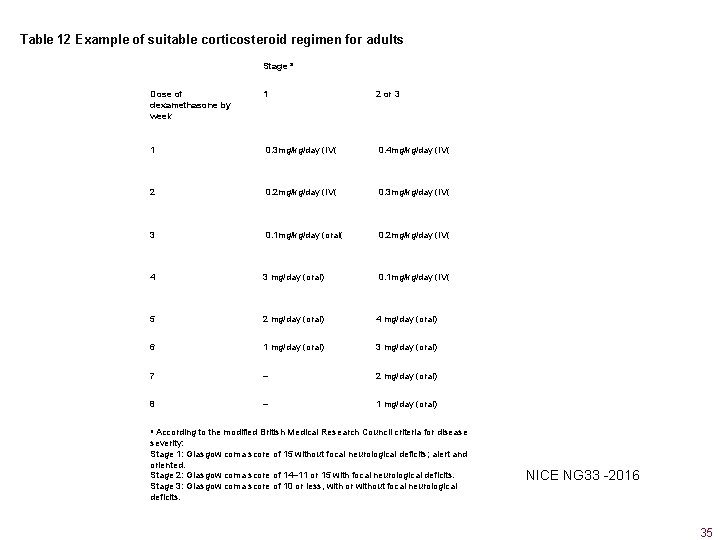
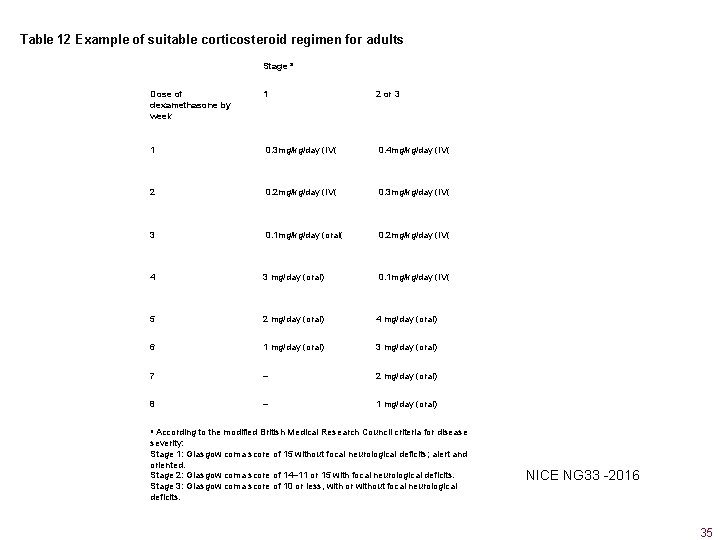
Table 12 Example of suitable corticosteroid regimen for adults Stage a Dose of dexamethasone by week 1 2 or 3 1 0. 3 mg/kg/day (IV( 0. 4 mg/kg/day (IV( 2 0. 2 mg/kg/day (IV( 0. 3 mg/kg/day (IV( 3 0. 1 mg/kg/day (oral( 0. 2 mg/kg/day (IV( 4 3 mg/day (oral) 0. 1 mg/kg/day (IV( 5 2 mg/day (oral) 4 mg/day (oral) 6 1 mg/day (oral) 3 mg/day (oral) 7 – 2 mg/day (oral) 8 – 1 mg/day (oral) a According to the modified British Medical Research Council criteria for disease severity: Stage 1: Glasgow coma score of 15 without focal neurological deficits; alert and oriented. Stage 2: Glasgow coma score of 14– 11 or 15 with focal neurological deficits. Stage 3: Glasgow coma score of 10 or less, with or without focal neurological deficits. NICE NG 33 -2016 35
Pericardial TB 1. 3. 7. 20 At the start of an anti‑TB treatment regimen, offer adults with active pericardial TB oral prednisolone at a starting dose of 60 mg/day, gradually withdrawing it 2– 3 weeks after starting treatment. [2016] NICE NG 33 -2016 36
Immune Reconstitution Syndrome/Paradoxical Reaction ( IRIS) • More common in HIV positive individuals • Mimics active TB • Diagnosis of exclusion • Treat with tapered steroids over 4 -6/52 37
Conclusions 1. Always do baseline tests 2. Think about interactions 3. Counsel carefully regarding side effects 4. Need samples for culture to get information on drug resistance 5. Liaise with microbiology lab 6. Drug reintroduction after toxicity should be done on a case by case basis with advice from experts 7. Specialist input if HIV co infection

 Complications of insulin resistance
Complications of insulin resistance Felodapine
Felodapine Ppi omeprazole
Ppi omeprazole Ppi drug interactions
Ppi drug interactions Beri beri
Beri beri Crpc
Crpc Filter press equation
Filter press equation What is a force that opposes motion through direct contact
What is a force that opposes motion through direct contact Natural selection and drug resistance
Natural selection and drug resistance Natural selection
Natural selection Drug resistance training
Drug resistance training Drug resistance training
Drug resistance training Compulsory drug treatment correctional centre
Compulsory drug treatment correctional centre Drug reaction treatment
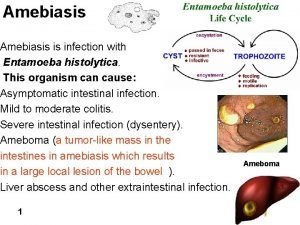
Drug reaction treatment Drug of choice for the treatment of extraluminal amebiasis
Drug of choice for the treatment of extraluminal amebiasis Drug of choice for the treatment of extraluminal amebiasis
Drug of choice for the treatment of extraluminal amebiasis Principles effective addiction treatment
Principles effective addiction treatment Interactions between ais and internal and external parties
Interactions between ais and internal and external parties Example of substitution with exhausted drug is
Example of substitution with exhausted drug is Complications of blood transfusion
Complications of blood transfusion Early and late complications of blood transfusion
Early and late complications of blood transfusion Define a short story
Define a short story Elements of the setting
Elements of the setting Words images objects qualitative or quantitative
Words images objects qualitative or quantitative Unit 5 macroeconomics lesson 2 activity 45 answer key
Unit 5 macroeconomics lesson 2 activity 45 answer key The properties and interactions of magnets are called
The properties and interactions of magnets are called What are sphere interactions?
What are sphere interactions? 6.1 habitats niches and species interactions answer key
6.1 habitats niches and species interactions answer key Integral architecture example
Integral architecture example 4 factors facilitating communication
4 factors facilitating communication Symbiosis and species interactions keystone webquest
Symbiosis and species interactions keystone webquest Naive bayes pays attention to complex interactions and
Naive bayes pays attention to complex interactions and Modular vs integral product architecture example
Modular vs integral product architecture example Niches and community interactions
Niches and community interactions Regional and transregional interactions
Regional and transregional interactions Fundamental particles and interactions
Fundamental particles and interactions Regional and transregional interactions
Regional and transregional interactions Causes of primary hypothyroidism
Causes of primary hypothyroidism Eswl complications
Eswl complications Complications c section
Complications c section