Tracheostomy and Surgical Airway Management Department of Otolaryngology

- Slides: 28
Tracheostomy and Surgical Airway Management Department of Otolaryngology- Head and Neck Surgery
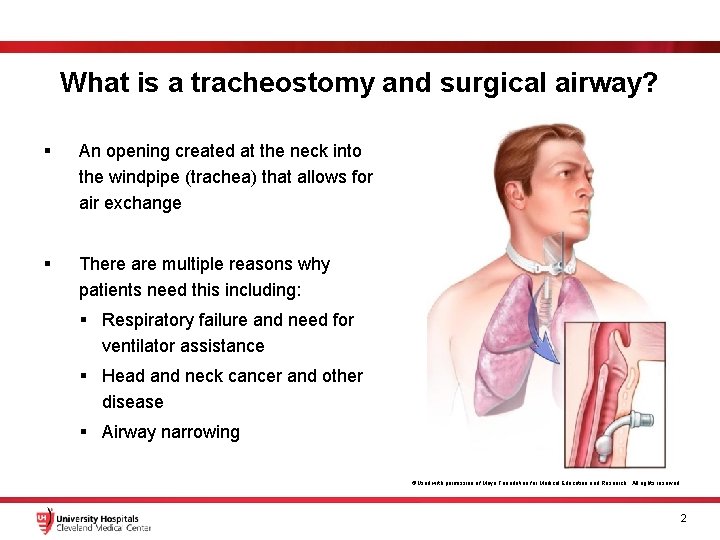
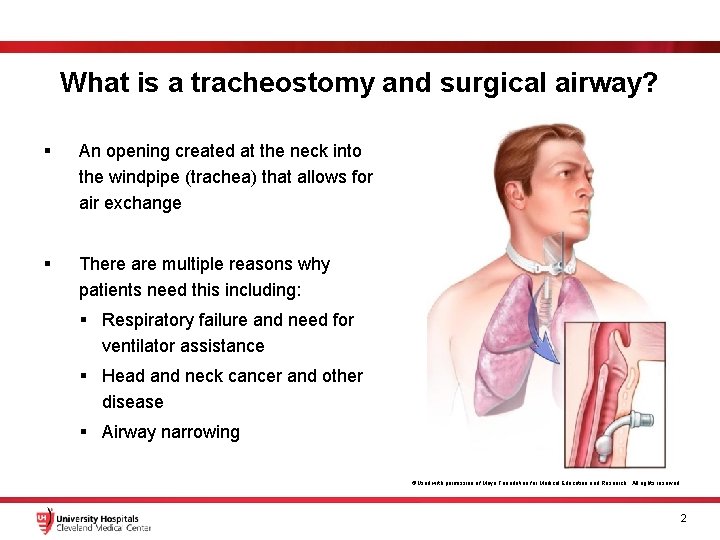
What is a tracheostomy and surgical airway? § An opening created at the neck into the windpipe (trachea) that allows for air exchange § There are multiple reasons why patients need this including: § Respiratory failure and need for ventilator assistance § Head and neck cancer and other disease § Airway narrowing ©Used with permission of Mayo Foundation for Medical Education and Research. All rights reserved 2
What is a tracheostomy and surgical airway? § There are serious consequences of suboptimal care, including death § It is our responsibility as physicians, nurses, therapists, and providers to be educated on how to care for these patients § In this presentation, we will provide an overview on the basics of managing a tracheostomy and surgical airway 3
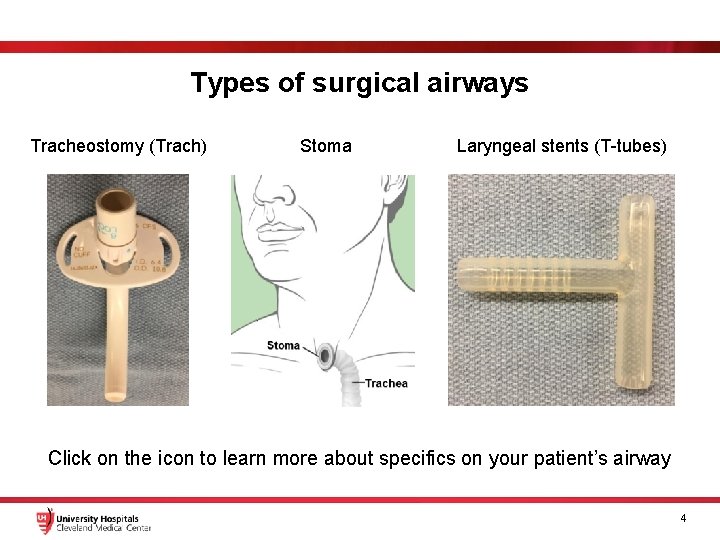
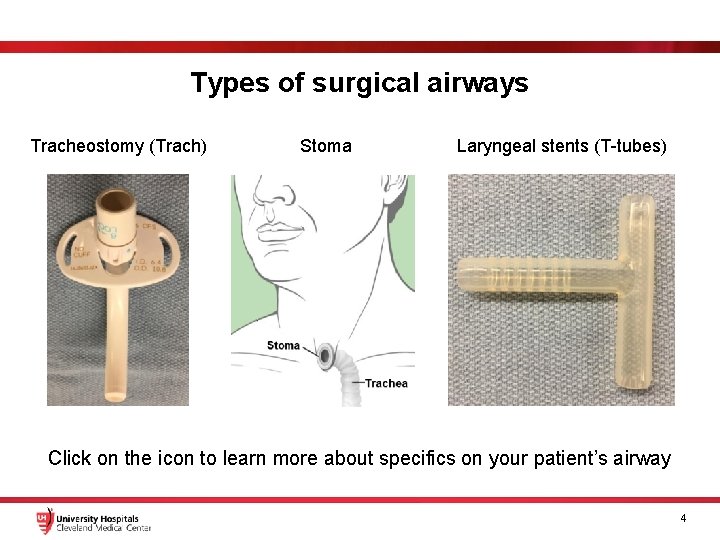
Types of surgical airways Tracheostomy (Trach) Stoma Laryngeal stents (T-tubes) Click on the icon to learn more about specifics on your patient’s airway 4
Tracheostomy 5
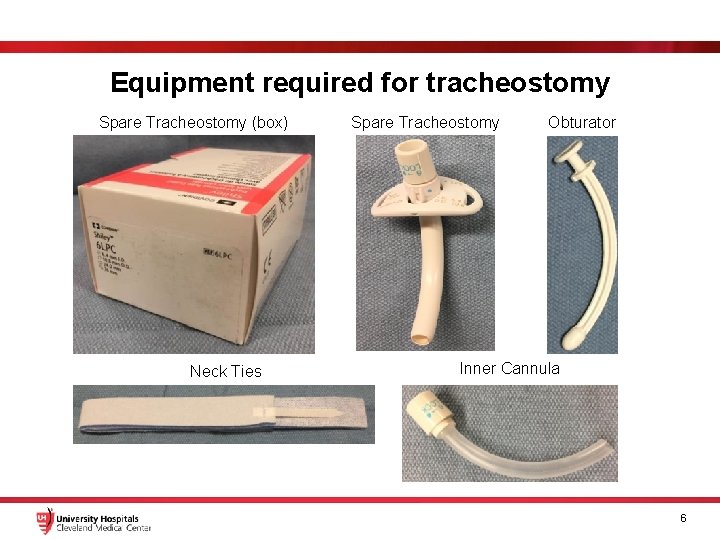
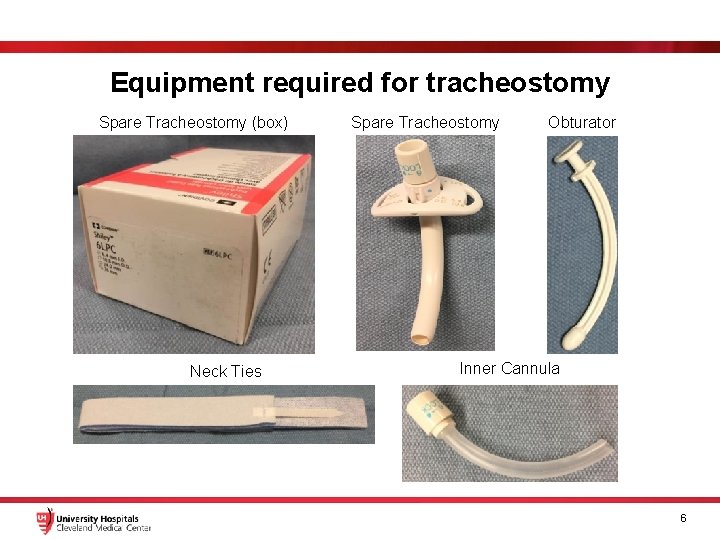
Equipment required for tracheostomy Spare Tracheostomy (box) Neck Ties Spare Tracheostomy Obturator Inner Cannula 6
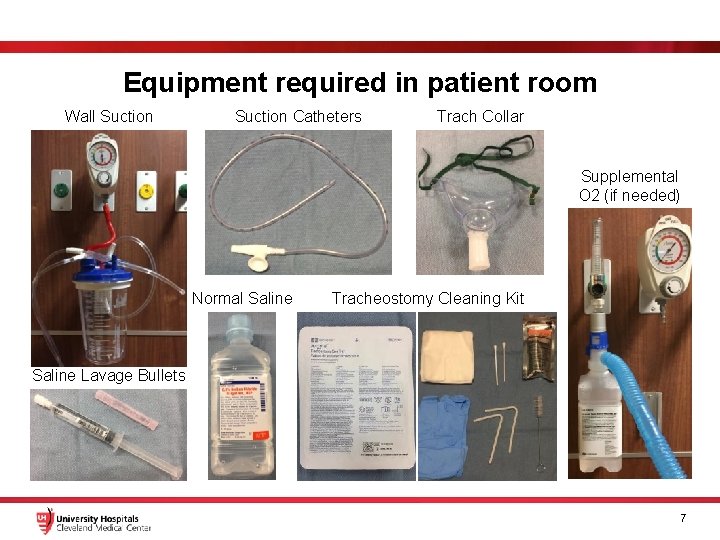
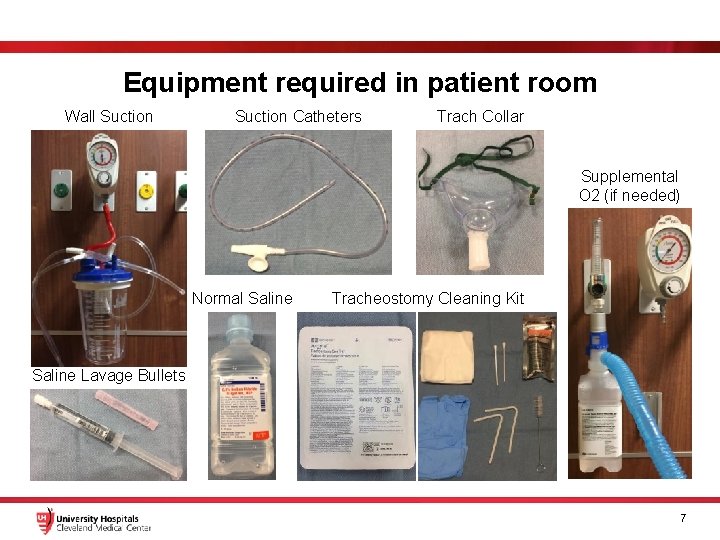
Equipment required in patient room Wall Suction Catheters Trach Collar Supplemental O 2 (if needed) Normal Saline Tracheostomy Cleaning Kit Saline Lavage Bullets 7
Tracheostomy There are different types of tracheostomies You should know the following information about your patients trach: 1. Brand 2. Size 3. Cuffed or cuffless 4. Inner cannula or no inner cannula § Disposable vs non-disposable inner cannula 5. Fenestrated or non-fenestrated 6. How long has the patient had a tracheostomy? 7. Why does the patient have a tracheostomy? 8
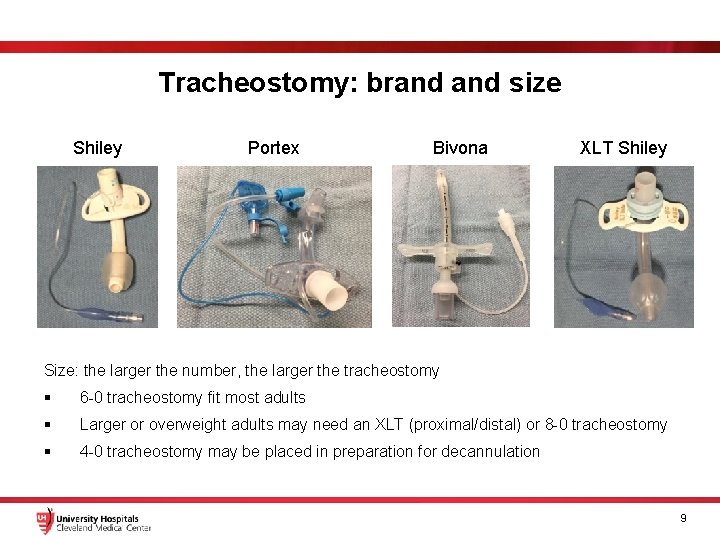
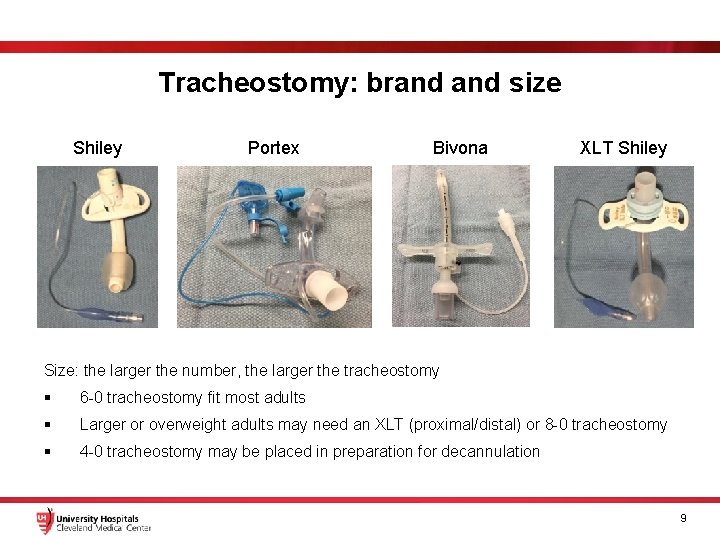
Tracheostomy: brand size Shiley Portex Bivona XLT Shiley Size: the larger the number, the larger the tracheostomy § 6 -0 tracheostomy fit most adults § Larger or overweight adults may need an XLT (proximal/distal) or 8 -0 tracheostomy § 4 -0 tracheostomy may be placed in preparation for decannulation 9
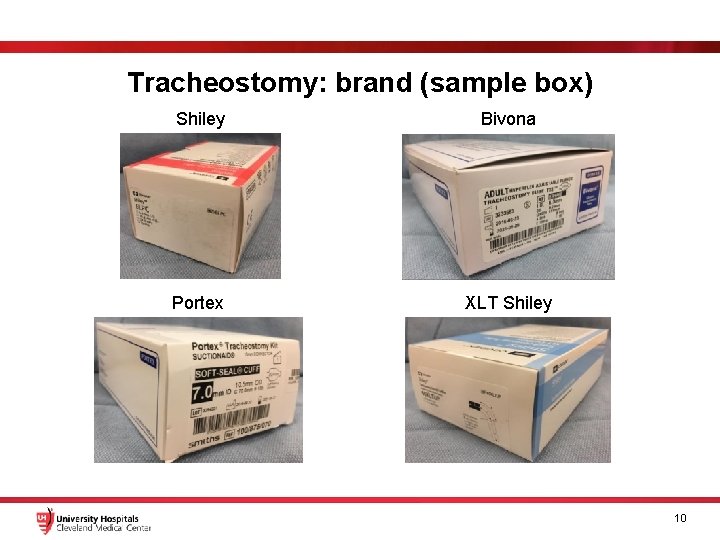
Tracheostomy: brand (sample box) Shiley Bivona Portex XLT Shiley 10
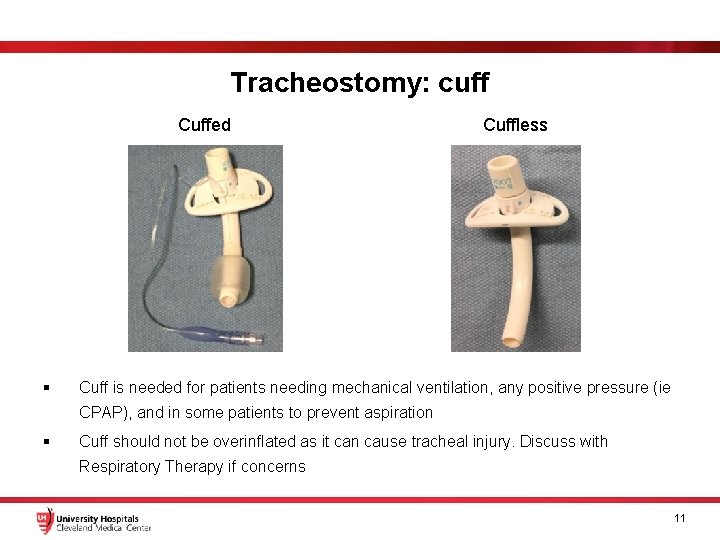
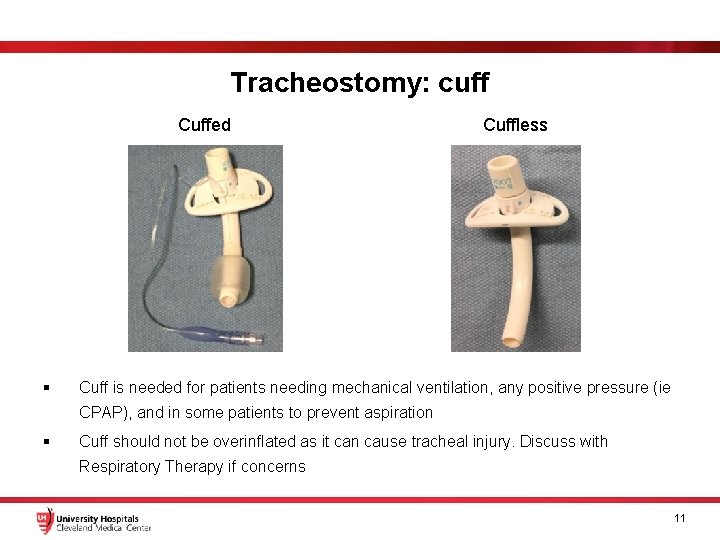
Tracheostomy: cuff Cuffed § Cuffless Cuff is needed for patients needing mechanical ventilation, any positive pressure (ie CPAP), and in some patients to prevent aspiration § Cuff should not be overinflated as it can cause tracheal injury. Discuss with Respiratory Therapy if concerns 11
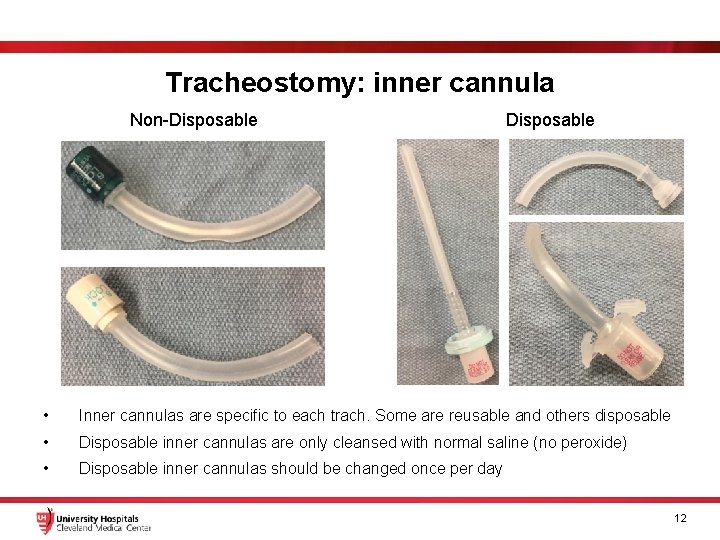
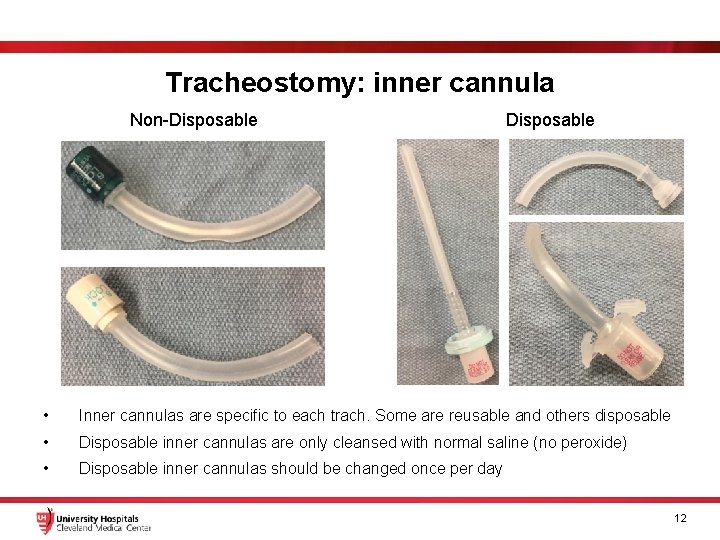
Tracheostomy: inner cannula Non-Disposable • Inner cannulas are specific to each trach. Some are reusable and others disposable • Disposable inner cannulas are only cleansed with normal saline (no peroxide) • Disposable inner cannulas should be changed once per day 12
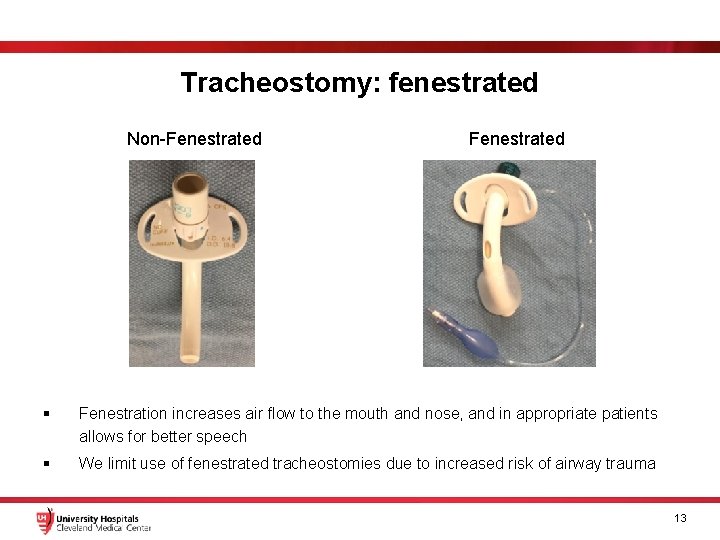
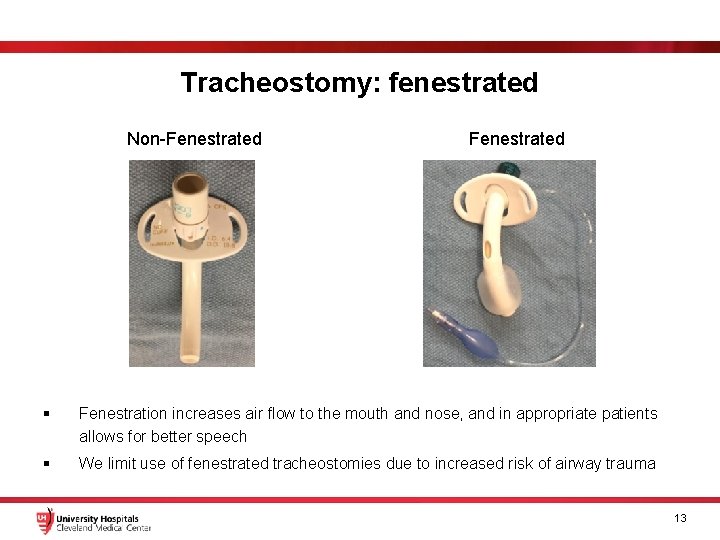
Tracheostomy: fenestrated Non-Fenestrated § Fenestration increases air flow to the mouth and nose, and in appropriate patients allows for better speech § We limit use of fenestrated tracheostomies due to increased risk of airway trauma 13
Tracheostomy: length of time § Knowing the length of time the patient has had a tracheostomy is important § New tracheostomies (within 7 days) need extra care: § Humidification is necessary, as air into the trach is not moistened or warmed by the nose or mouth § Frequent suctioning to help bring up secretions § Bleeding can be seen from the neck incision and secretions may be blood tinged for the first 24 hours § Chronic Tracheostomies § Suctioning can be as needed or only with cleaning 14
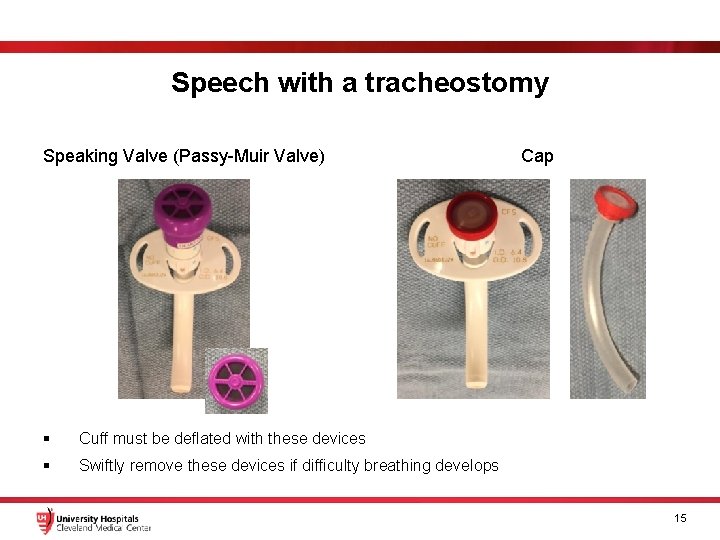
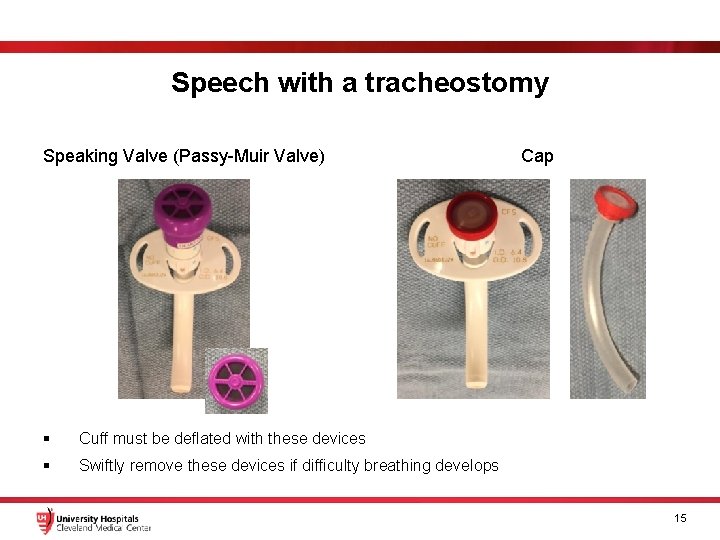
Speech with a tracheostomy Speaking Valve (Passy-Muir Valve) § Cuff must be deflated with these devices § Swiftly remove these devices if difficulty breathing develops Cap 15
Stoma 16
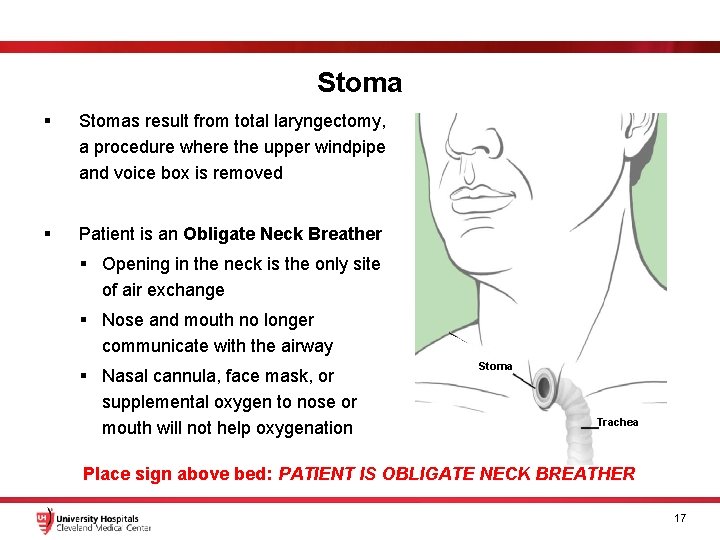
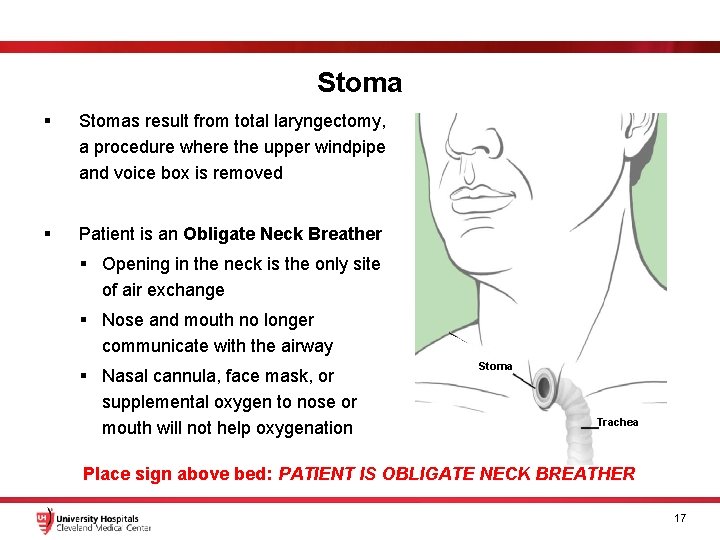
Stoma § Stomas result from total laryngectomy, a procedure where the upper windpipe and voice box is removed § Patient is an Obligate Neck Breather § Opening in the neck is the only site of air exchange § Nose and mouth no longer communicate with the airway § Nasal cannula, face mask, or supplemental oxygen to nose or mouth will not help oxygenation Stoma Trachea Place sign above bed: PATIENT IS OBLIGATE NECK BREATHER 17
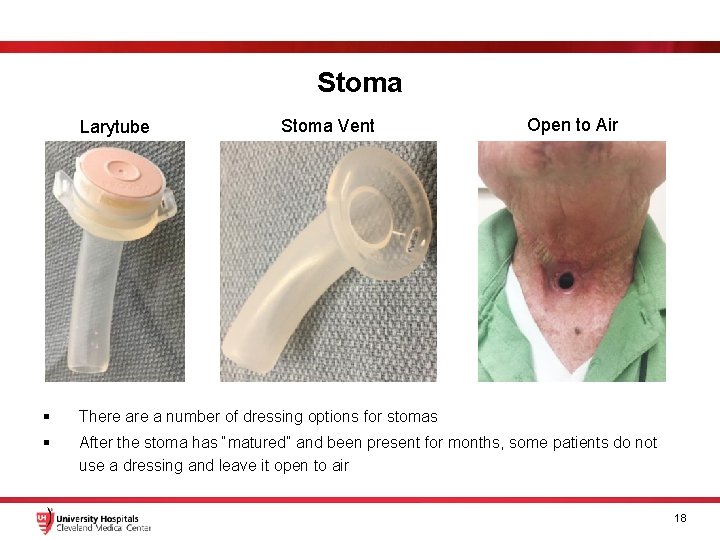
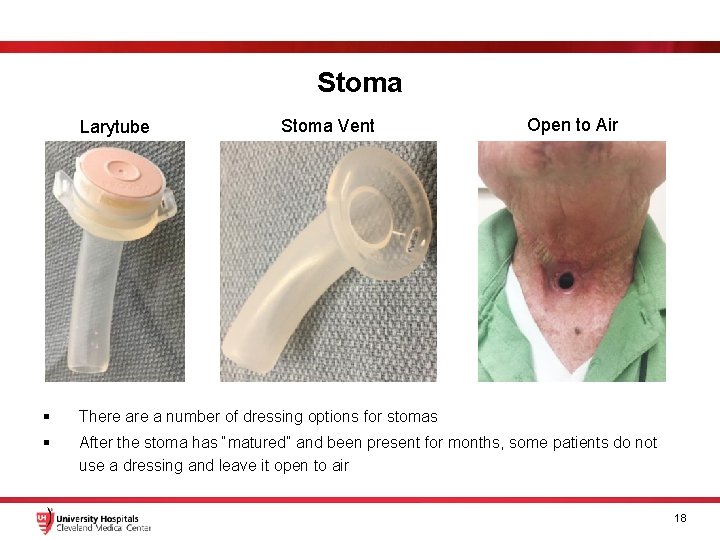
Stoma Larytube Stoma Vent Open to Air § There a number of dressing options for stomas § After the stoma has “matured” and been present for months, some patients do not use a dressing and leave it open to air 18
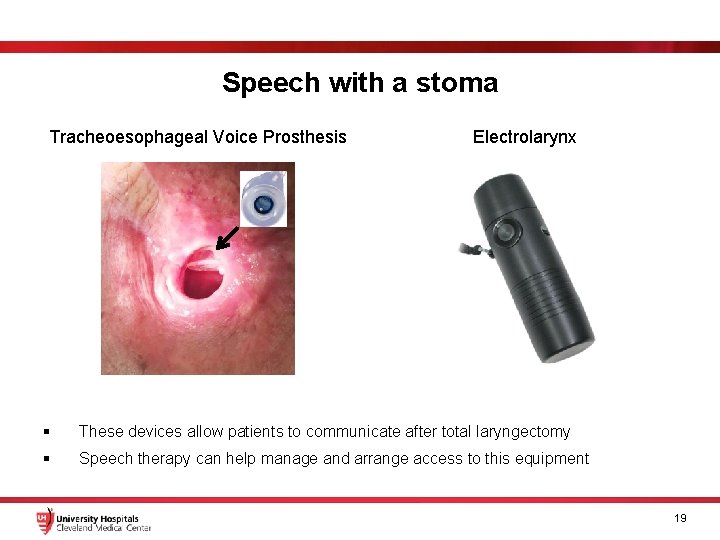
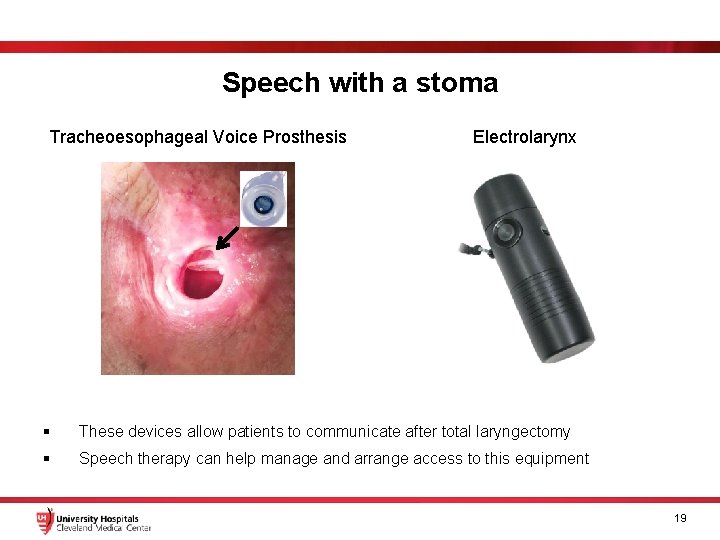
Speech with a stoma Tracheoesophageal Voice Prosthesis Electrolarynx § These devices allow patients to communicate after total laryngectomy § Speech therapy can help manage and arrange access to this equipment 19
T-tube 20
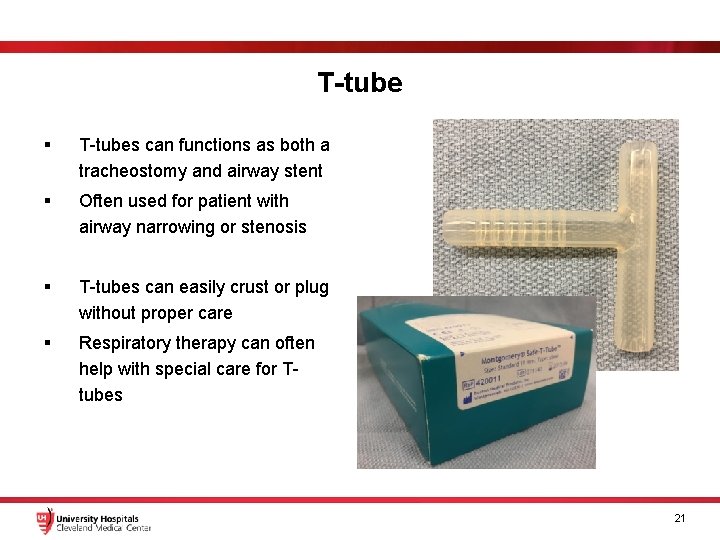
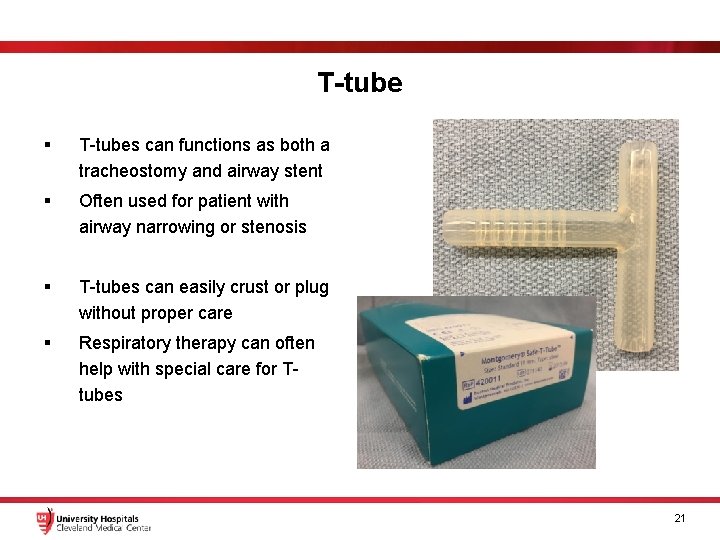
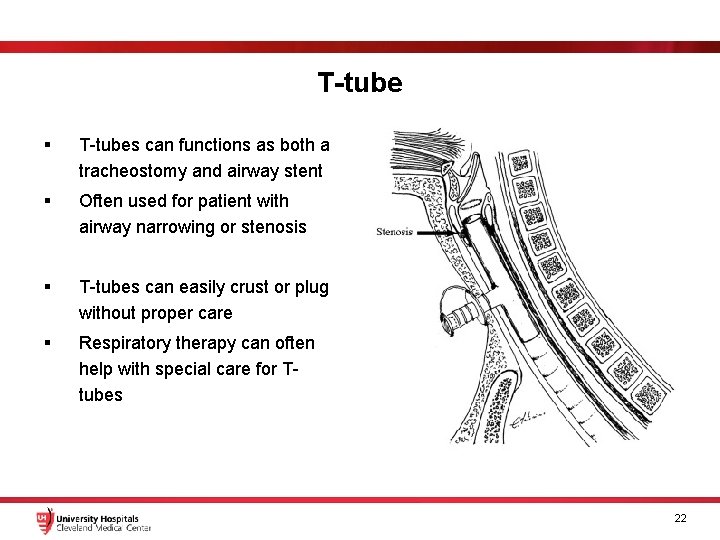
T-tube § T-tubes can functions as both a tracheostomy and airway stent § Often used for patient with airway narrowing or stenosis § T-tubes can easily crust or plug without proper care § Respiratory therapy can often help with special care for Ttubes 21
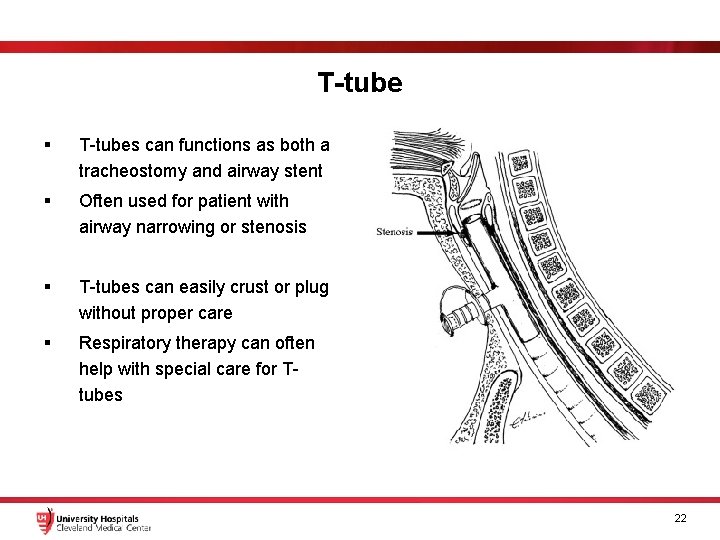
T-tube § T-tubes can functions as both a tracheostomy and airway stent § Often used for patient with airway narrowing or stenosis § T-tubes can easily crust or plug without proper care § Respiratory therapy can often help with special care for Ttubes 22
Emergencies 23
Airway emergencies § Situation: patient has increased work of breathing or SOB § Make sure patient is monitored with central monitor or pulse oximetry § Remove any tracheostomy speaking valve or cap § Mucus plugs and accumulated secretions in the airway is a common problem § Attempt suctioning with a tracheal suction catheter § Try squirting normal saline (2 -3 ml) into the airway to help loosen thick secretions/mucous plugs, then suction the patient § Remove the inner cannula if one is present § Call appropriate codes and CODE ENT 24

Tracheostomy dislodgement § Situation: tracheostomy is accidentally removed and patient cannot breath without tracheostomy in place § You can attempt to replace the tracheostomy. Make sure the obturator (see arrow) is in place § If original tracheostomy cannot be placed, a smaller tracheostomy or endotracheal tube can be temporarily placed § You can attempt intubation from above § Call appropriate codes and CODE ENT 25
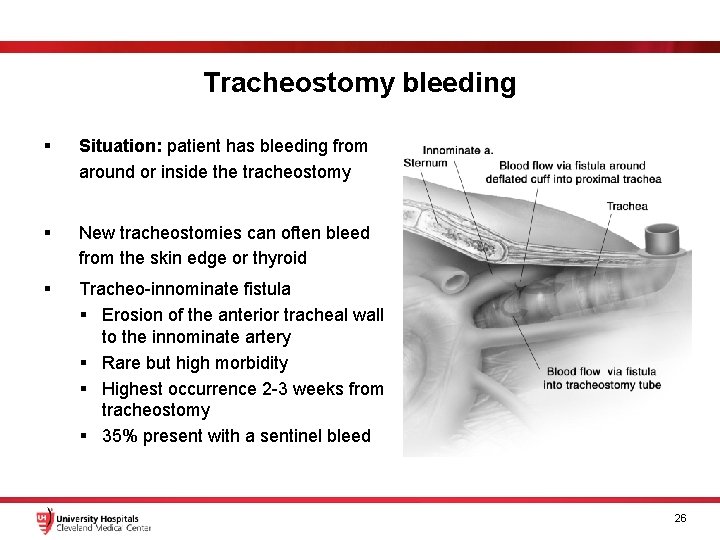
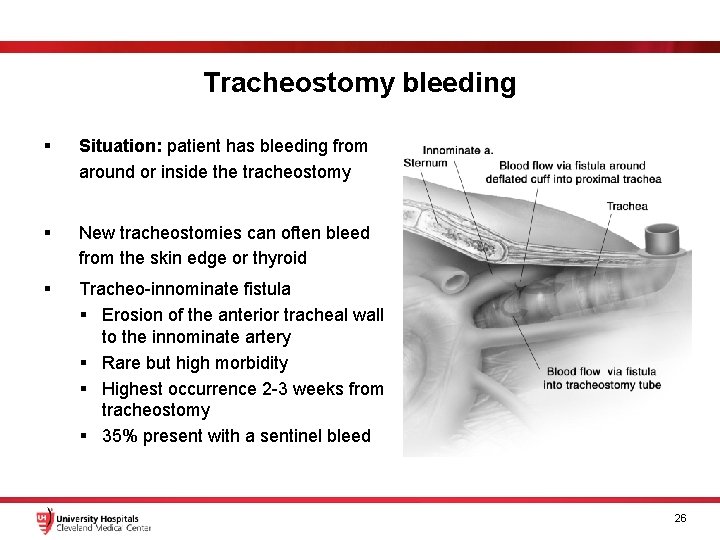
Tracheostomy bleeding § Situation: patient has bleeding from around or inside the tracheostomy § New tracheostomies can often bleed from the skin edge or thyroid § Tracheo-innominate fistula § Erosion of the anterior tracheal wall to the innominate artery § Rare but high morbidity § Highest occurrence 2 -3 weeks from tracheostomy § 35% present with a sentinel bleed 26
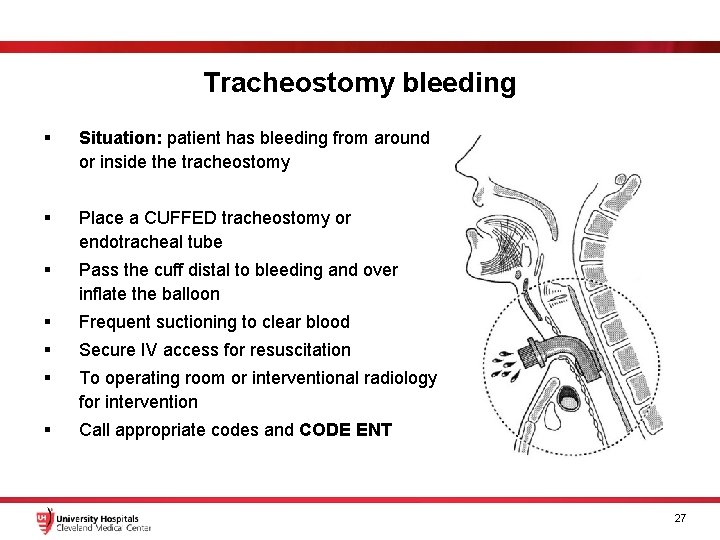
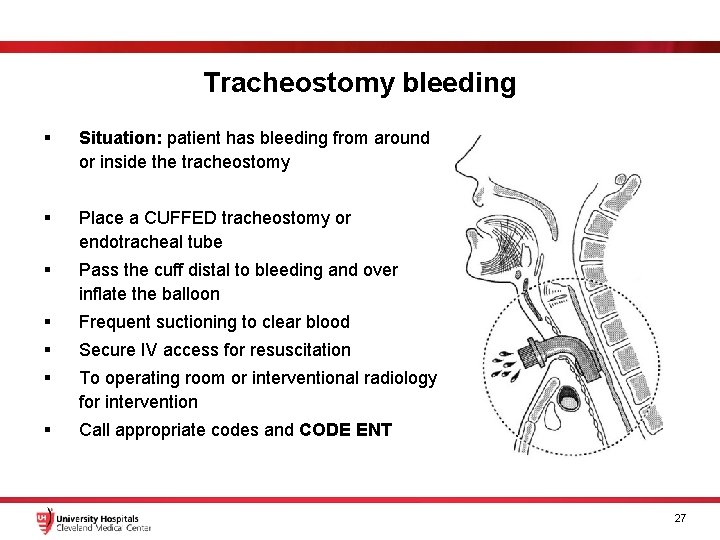
Tracheostomy bleeding § Situation: patient has bleeding from around or inside the tracheostomy § Place a CUFFED tracheostomy or endotracheal tube § Pass the cuff distal to bleeding and over inflate the balloon § Frequent suctioning to clear blood § Secure IV access for resuscitation § To operating room or interventional radiology for intervention § Call appropriate codes and CODE ENT 27
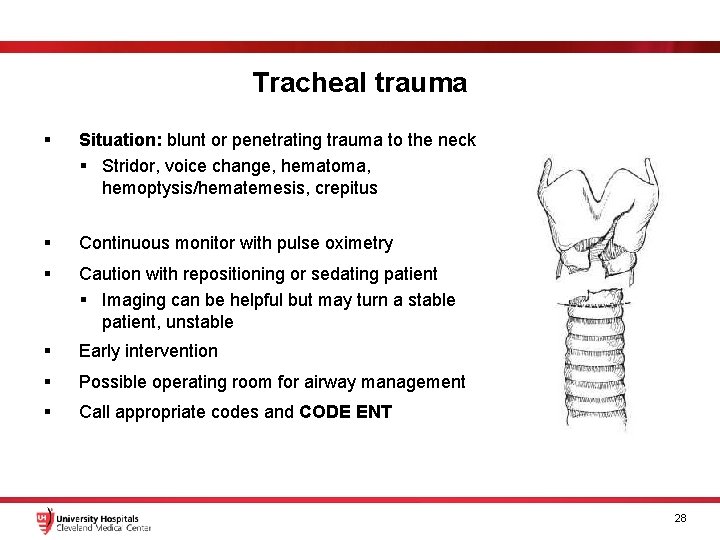
Tracheal trauma § Situation: blunt or penetrating trauma to the neck § Stridor, voice change, hematoma, hemoptysis/hematemesis, crepitus § Continuous monitor with pulse oximetry § Caution with repositioning or sedating patient § Imaging can be helpful but may turn a stable patient, unstable § Early intervention § Possible operating room for airway management § Call appropriate codes and CODE ENT 28
 Airway grade view
Airway grade view Chapter 31 ophthalmology and otolaryngology
Chapter 31 ophthalmology and otolaryngology Tokyo artificial larynx
Tokyo artificial larynx Jennifer baima md
Jennifer baima md Indikasi intubasi
Indikasi intubasi Chapter 10 airway management
Chapter 10 airway management Supraglotal
Supraglotal Chapter 9 airway management
Chapter 9 airway management Technique abcde
Technique abcde Sandwich manuver
Sandwich manuver Stepwise approach to airway management
Stepwise approach to airway management Tracheostomy indication and contraindication
Tracheostomy indication and contraindication Upper respiratory tract organs
Upper respiratory tract organs Suction procedure
Suction procedure Tracheostomy double lumen
Tracheostomy double lumen Feeding cuff
Feeding cuff St george tracheostomy
St george tracheostomy Tracheostomy care
Tracheostomy care Tracheostomy care
Tracheostomy care Tracheostomy care
Tracheostomy care Tracheostomy care
Tracheostomy care Trakeostomi sugning
Trakeostomi sugning Tali tracheostomy
Tali tracheostomy Decannulation of tracheostomy
Decannulation of tracheostomy Tracheostomy oxygen delivery
Tracheostomy oxygen delivery Tracheostomy
Tracheostomy Patients with special challenges
Patients with special challenges Summary of tracheostomy care
Summary of tracheostomy care 332 rule intubation
332 rule intubation