Feeding Tracheostomy Patients with the Cuff Inflated What
- Slides: 30
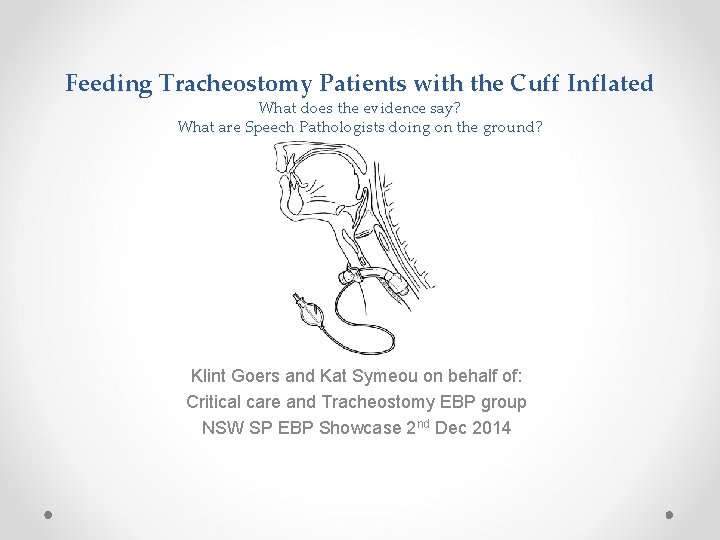
Feeding Tracheostomy Patients with the Cuff Inflated What does the evidence say? What are Speech Pathologists doing on the ground? Klint Goers and Kat Symeou on behalf of: Critical care and Tracheostomy EBP group NSW SP EBP Showcase 2 nd Dec 2014
Overview • • • Anatomy refresher Tracheostomy – does it cause dysphagia? Cuff status and potential impact on swallow Why did we want to look at this area? What did we already know? 2014 clinical question 2014 clinical bottom line Survey of speech pathologists across Australia and their clinical practice Summary and where to from here Acknowledgements
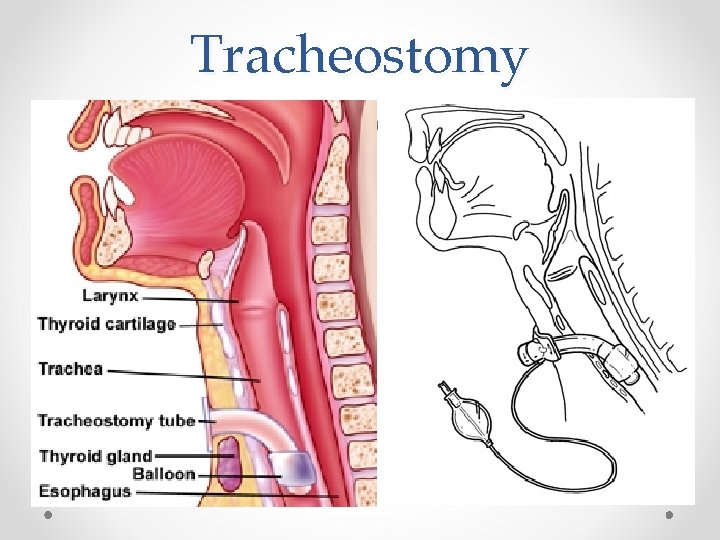
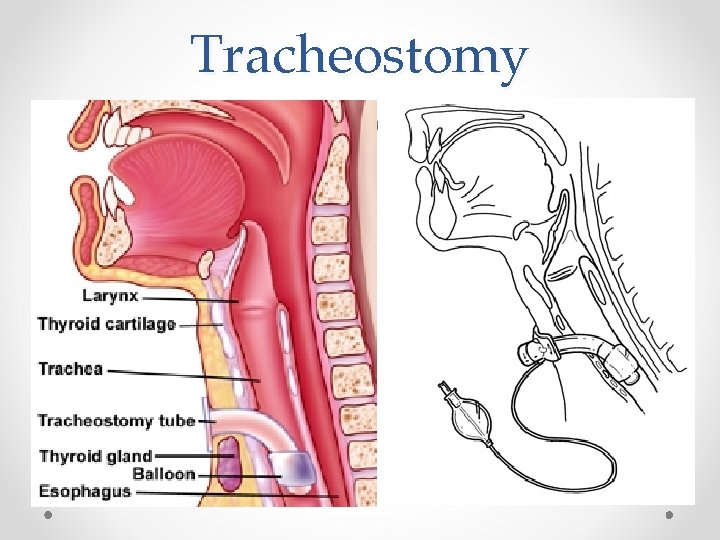
Tracheostomy
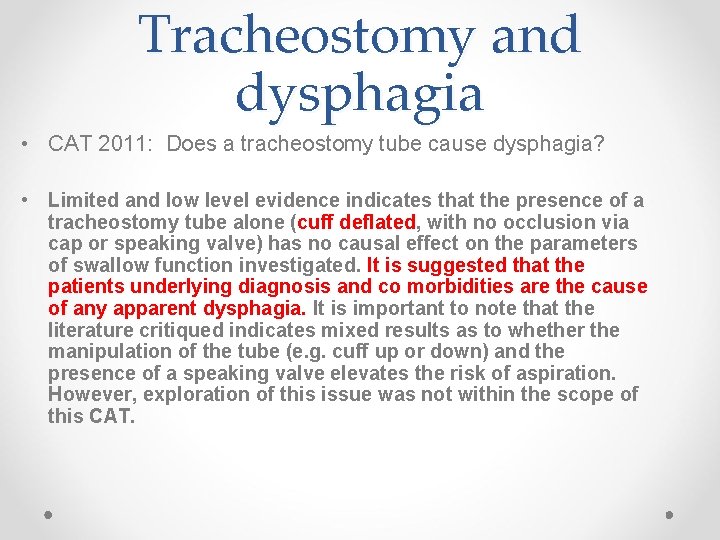
Tracheostomy and dysphagia • CAT 2011: Does a tracheostomy tube cause dysphagia? • Limited and low level evidence indicates that the presence of a tracheostomy tube alone (cuff deflated, with no occlusion via cap or speaking valve) has no causal effect on the parameters of swallow function investigated. It is suggested that the patients underlying diagnosis and co morbidities are the cause of any apparent dysphagia. It is important to note that the literature critiqued indicates mixed results as to whether the manipulation of the tube (e. g. cuff up or down) and the presence of a speaking valve elevates the risk of aspiration. However, exploration of this issue was not within the scope of this CAT.
What about feeding patients with the cuff inflated? The oral pharyngeal swallow may be impacted when a patient is fed with an inflated cuff • Anchoring of the larynx on tracheal wall affecting hyoid movement • Changes to airflow through the upper airway therefore may impact sensation and/or swallow • Reduced effectiveness of cough Why therapists may be reluctant to feed with the cuff up: Previous case reports of perforation of the oesophagus when patient’s fed with high pressure inflated cuffs
What about feeding patients with the cuff inflated? Why did we want to look at this? • Differences in practice across members/sites in relation to feeding patients with the cuff up • Speech Pathologists recognising the importance of early intervention (i. e. when the patients are still ventilated) in order to improve QOL, potentially prevent disuse and atrophy • Acknowledgement that this is a contentious issue • 2013 Trache ACI CPG reported the results for cuff up feeding and aspiration were mixed. All these factors combined meant that we needed to review the evidence as a group
What about feeding patients with the cuff inflated? What did we already know? This topic was last looked at in this group in 2002 via 2 x CAP’s. The clinical question was: Does an inflated cuff exacerbate/increase aspiration at the level of the vocal folds? Study 1. Davis 2002: Non ventilated respiratory patients. Level IV Old clinical bottom line: Cuff inflation may exacerbate/increase aspiration at the level of the vocal folds and an MBS should be pursued for further detail.
2014 clinical question In patients with a tracheostomy (+/- mechanical ventilation), does an inflated cuff exacerbate / increase aspiration of food or fluids at the level of the vocal folds compared to a deflated cuff? • Search last 15 years via Google scholar and Medline • 6 articles identified • Inclusion criteria: Used instrumental assessment to compare the same patient with cuff up/cuff down feeding and evaluate aspiration as an outcome • 2 met criteria for inclusion
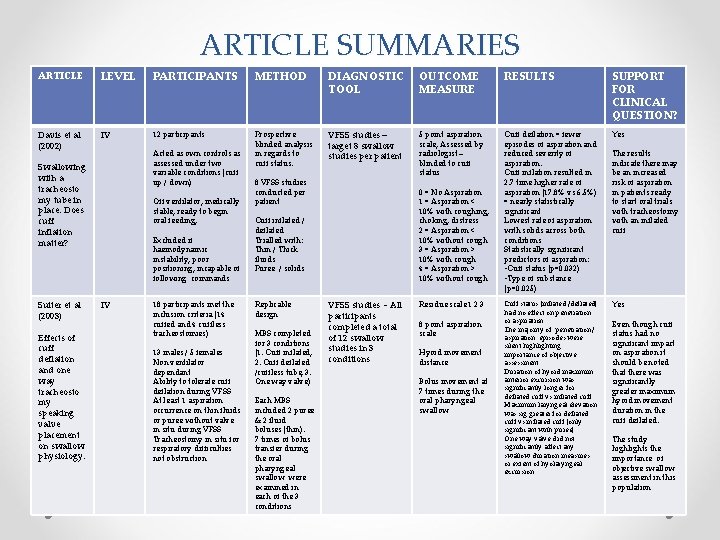
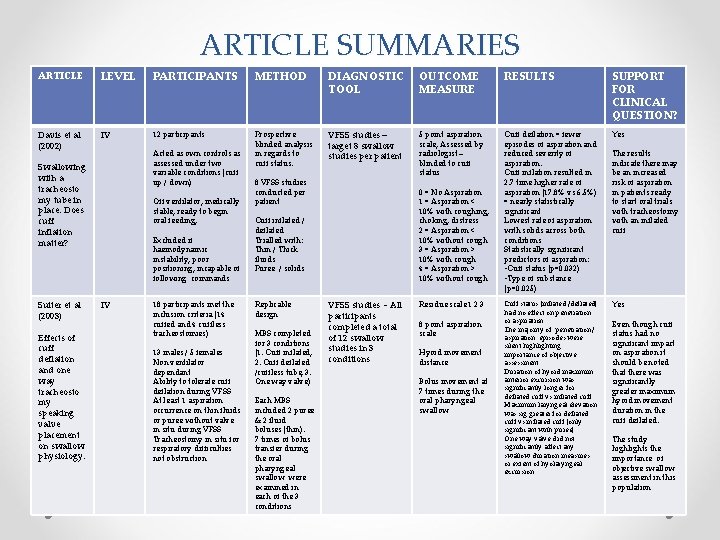
ARTICLE SUMMARIES ARTICLE LEVEL PARTICIPANTS METHOD DIAGNOSTIC TOOL OUTCOME MEASURE RESULTS SUPPORT FOR CLINICAL QUESTION? Davis et al (2002) IV 12 participants Prospective blinded analysis in regards to cuff status. VFSS studies – target 8 swallow studies per patient 5 point aspiration scale, Assessed by radiologist – blinded to cuff status Cuff deflation = fewer episodes of aspiration and reduced severity of aspiration. Cuff inflation resulted in 2. 7 time higher rate of aspiration (17. 8% vs 6. 5%) = nearly statistically significant Lowest rate of aspiration with solids across both conditions Statistically significant predictors of aspiration: • Cuff status (p=0. 032) • Type of substance (p=0. 025) Yes Cuff status (inflated /deflated) had no effect on penetration or aspiration. The majority of penetration / aspiration episodes were silent highlighting importance of objective assessment. Duration of hyoid maximum anterior excursion was significantly longer for deflated cuff vs inflated cuff. Maximum laryngeal elevation was sig greater for deflated cuff vs inflated cuff (only significant with puree) One way valve did not significantly affect any swallow duration measures or extent of hyolaryngeal excursion Yes Acted as own controls as assessed under two variable conditions (cuff up / down) Swallowing with a tracheosto my tube in place: Does cuff inflation matter? Suiter et al (2003) Effects of cuff deflation and one way tracheosto my speaking valve placement on swallow physiology. Off ventilator, medically stable, ready to begin oral feeding, Excluded if haemodynamic instability, poor positioning, incapable of following commands IV 18 participants met the inclusion criteria (14 cuffed and 4 cuffless tracheostomies) 13 males / 5 females Non ventilator dependant Ability to tolerate cuff deflation during VFSS At least 1 aspiration occurrence on thin fluids or puree without valve in situ during VFSS Tracheostomy in situ for respiratory difficulties not obstruction 8 VFSS studies conducted per patient 0 = No Aspiration 1 = Aspiration < 10% with coughing, choking, distress 2 = Aspiration < 10% without cough 3 = Aspiration > 10% with cough 4 = Aspiration > 10% without cough Cuff inflated / deflated Trialled with: Thin / Thick fluids Puree / solids Replicable design MBS completed for 3 conditions (1. Cuff inflated, 2. Cuff deflated /cuffless tube, 3. One way valve) Each MBS included 2 puree & 2 fluid boluses (thin). 7 times of bolus transfer during the oral pharyngeal swallow were examined in each of the 3 conditions VFSS studies - All participants completed a total of 12 swallow studies in 3 conditions Residue scale 1 2 3 8 point aspiration scale Hyoid movement distance Bolus movement at 7 times during the oral pharyngeal swallow The results indicate there may be an increased risk of aspiration in patients ready to start oral trials with tracheostomy with an inflated cuff Even though cuff status had no significant impact on aspiration it should be noted that there was significantly greater maximum hyoid movement duration in the cuff deflated. The study highlights the importance of objective swallow assessment in this population
New CAT 2014: clinical bottom line • In non-ventilated respiratory patients with tracheostomy, there are mixed results on whether aspiration of food or fluid is exacerbated or increased by the presence of an inflated cuff. There were no studies in mechanically ventilated patients that answered the clinical question. In the nonventilated cohort two small studies were identified, one suggested an increased risk, the other reported no increased risk in aspiration with cuff up when evaluated on MBS. We are not able to conclusively report either way on whether cuff status increases the risk of aspiration. • Davis 2002, Suiter 2003
So the results are mixed Wonder what's happening out there? How can we investigate this ? A survey
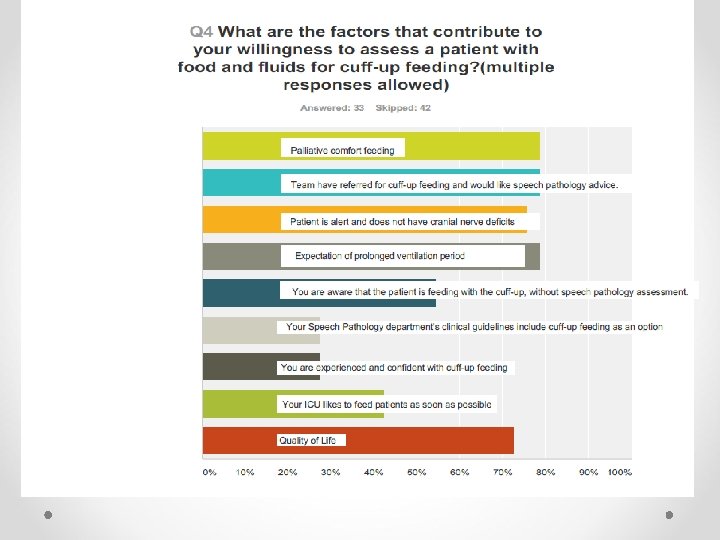
Aim of Survey • How much of this evidence do therapists know ? • How widespread is feeding with the cuff up practiced in Australia? • How are speech pathologists interpreting the evidence? • What are the factors that make a therapist more likely to feed or not feed a patient with the cuff up.
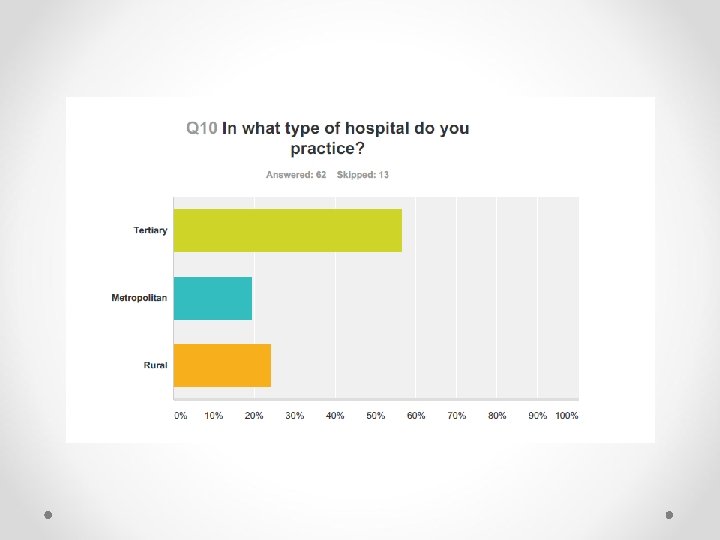
Survey Design • 75 respondents • Available for 3 weeks on Survey Monkey • Distributed via Critical Care and Tracheostomy EBP google group/list serve (200 members) and the H&N google list serve ~ 200 members • Also sent out via SPAN (NSW SP managers across NSW) • Lengthy survey, unable to capture all of it today but please email Klint if you want a copy • A note about bias. Potentially therapists who feed with the cuff up more likely to have responded
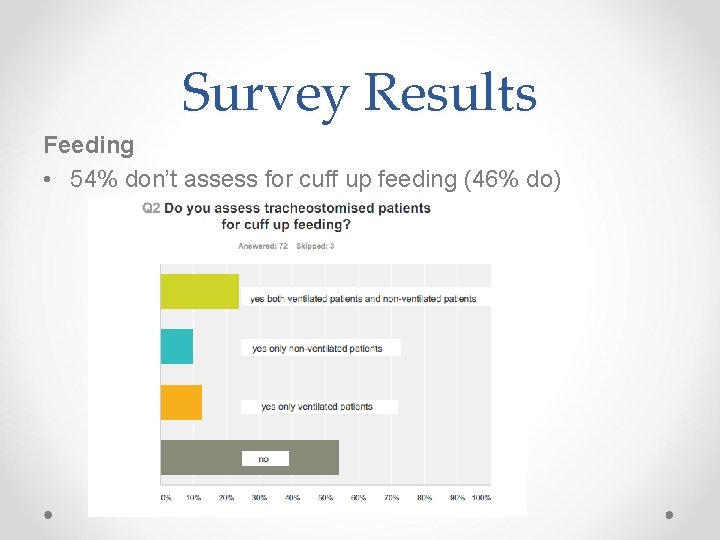
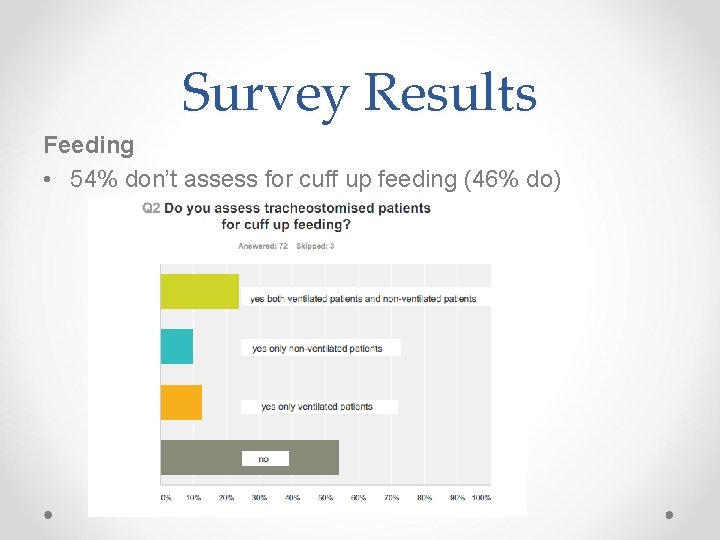
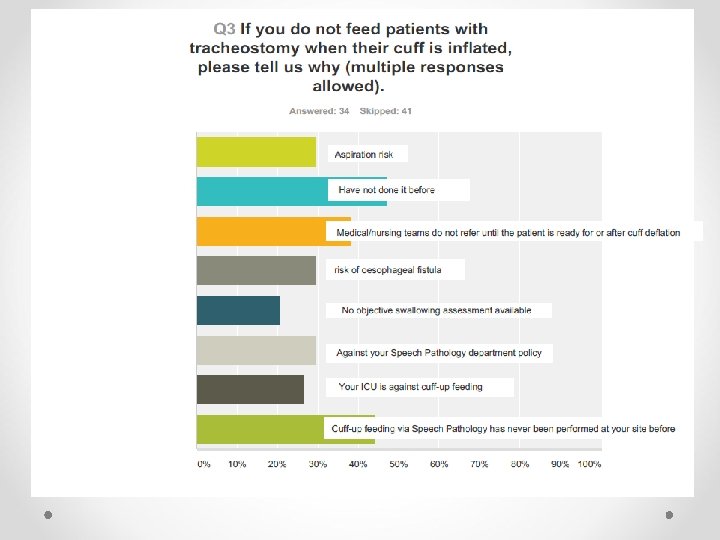
Survey Results Feeding • 54% don’t assess for cuff up feeding (46% do)
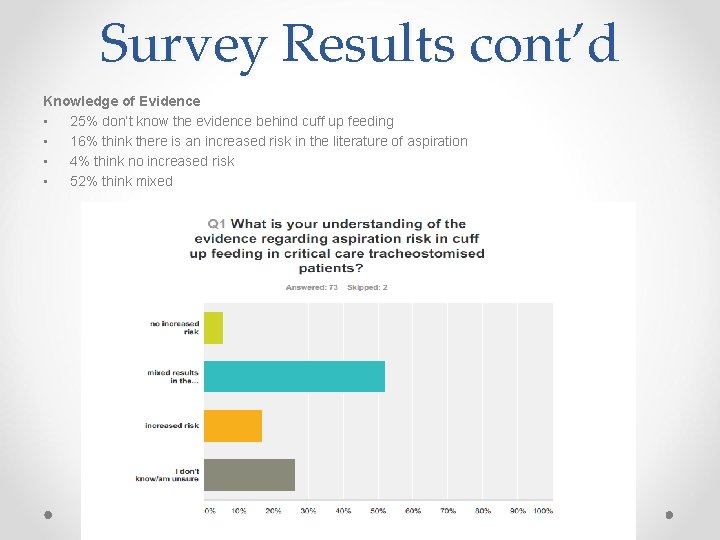
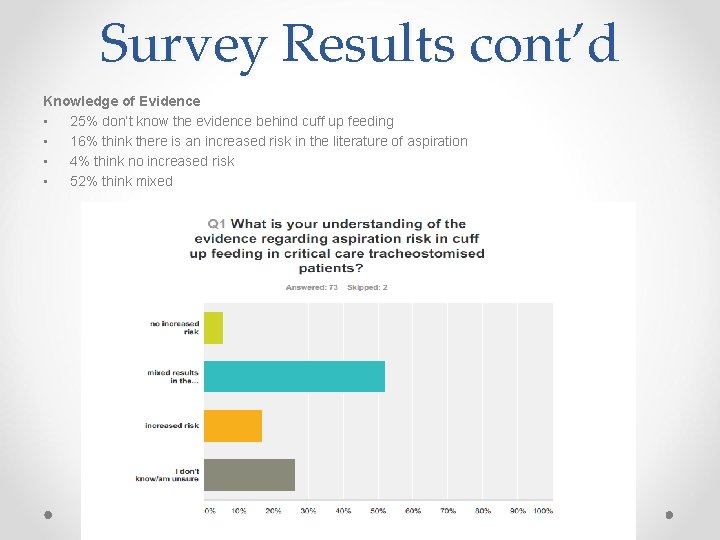
Survey Results cont’d Knowledge of Evidence • 25% don’t know the evidence behind cuff up feeding • 16% think there is an increased risk in the literature of aspiration • 4% think no increased risk • 52% think mixed
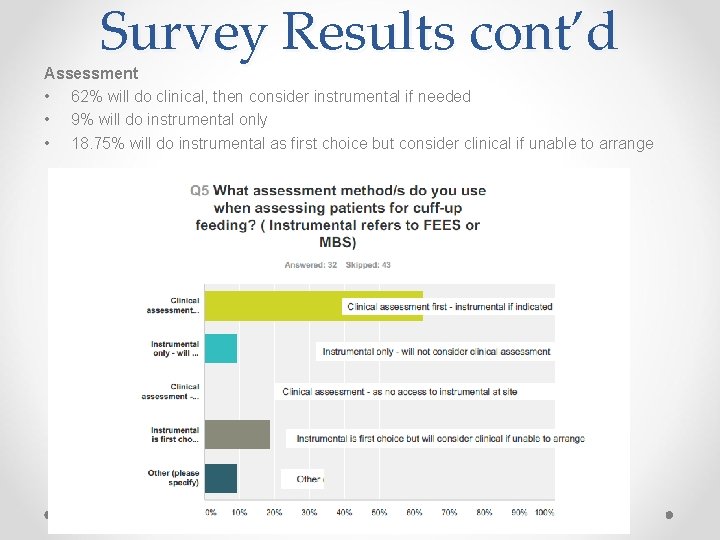
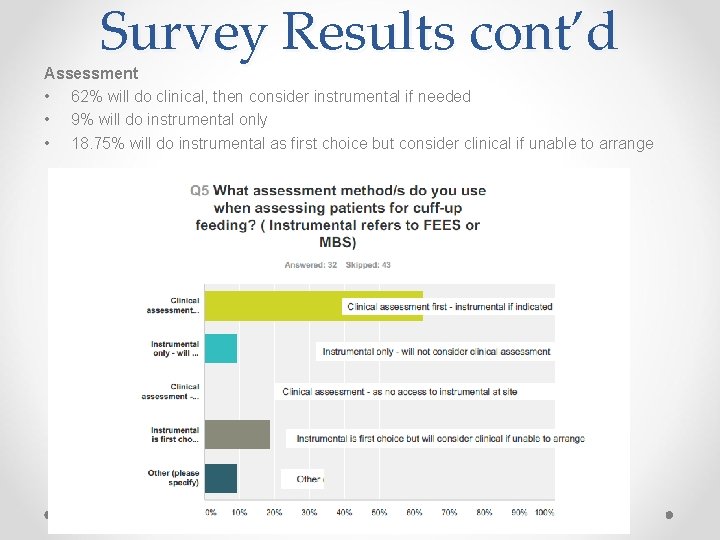
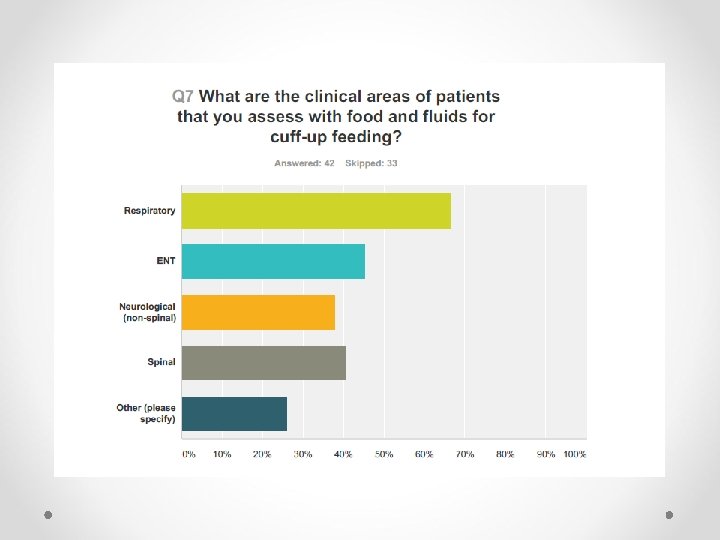
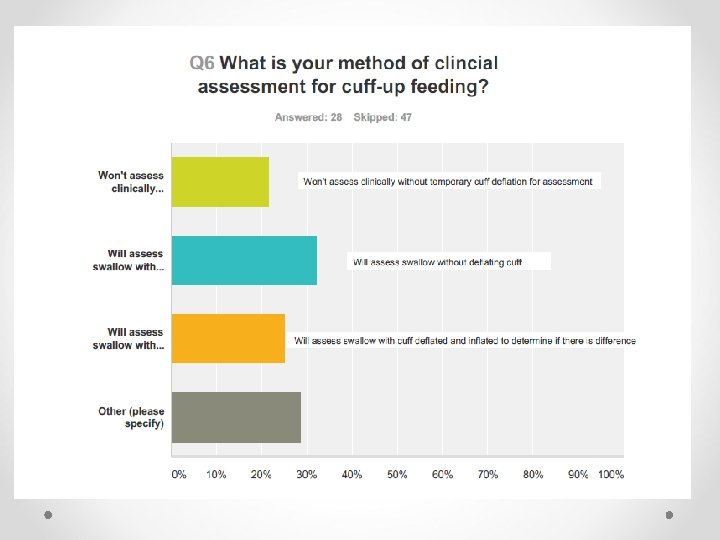
Survey Results cont’d Assessment • 62% will do clinical, then consider instrumental if needed • 9% will do instrumental only • 18. 75% will do instrumental as first choice but consider clinical if unable to arrange
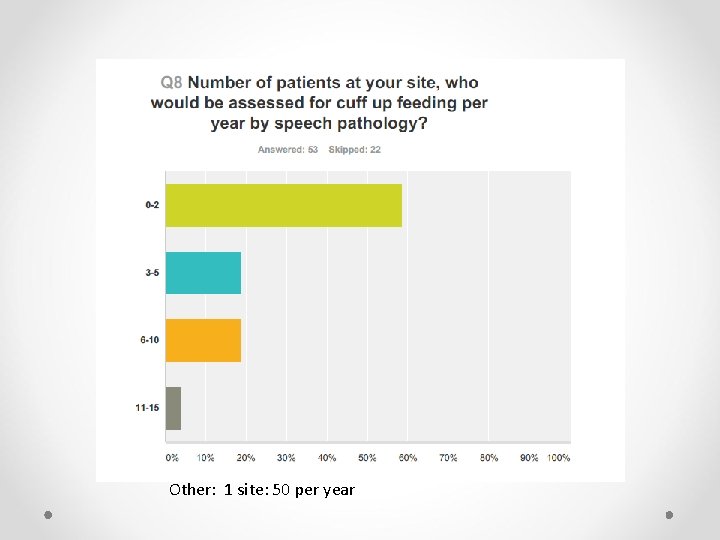
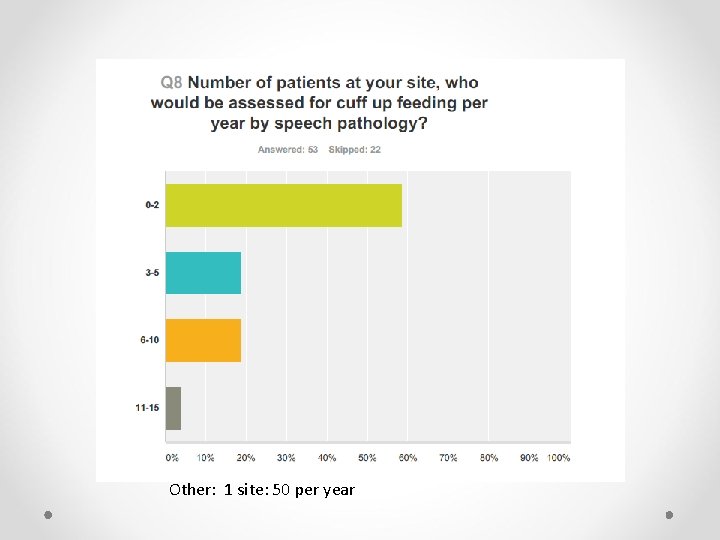
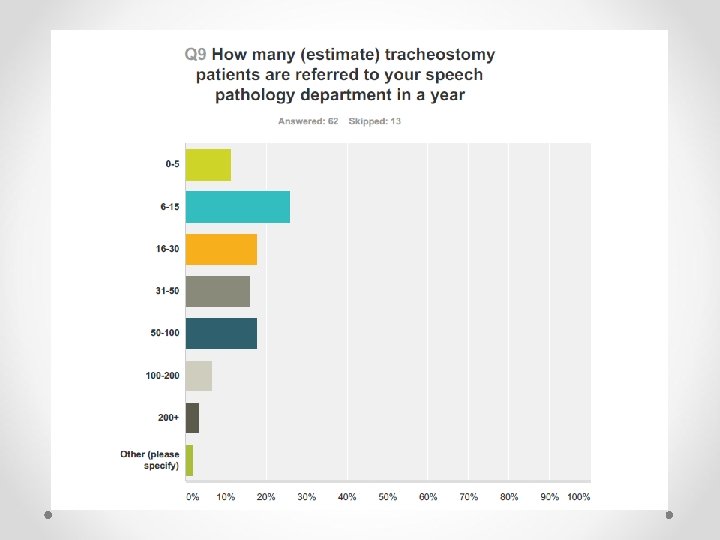
Other: 1 site: 50 per year
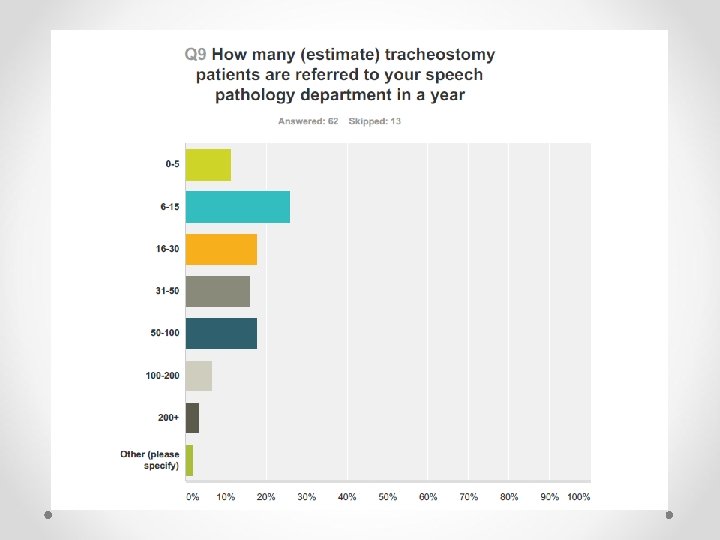
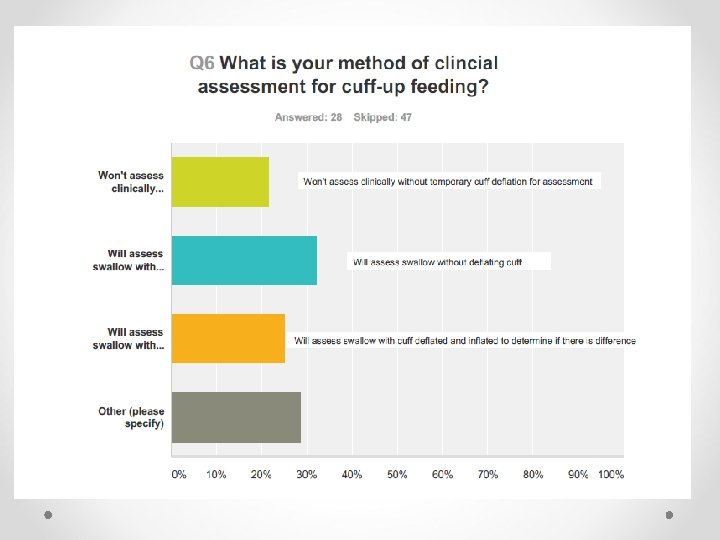
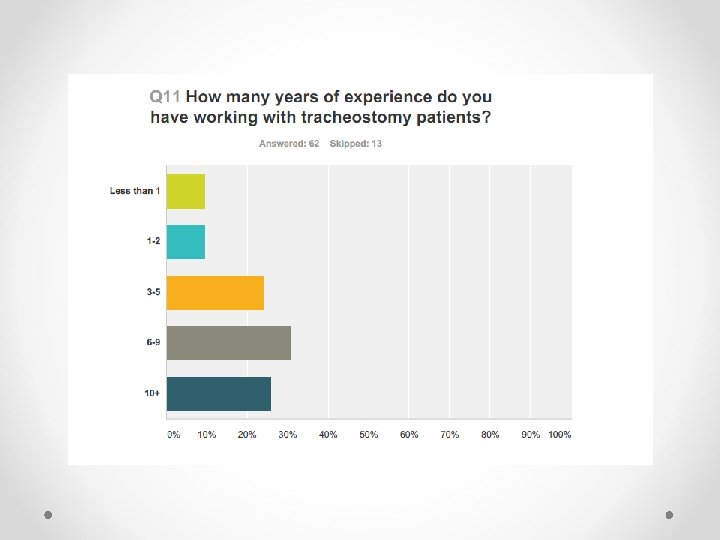
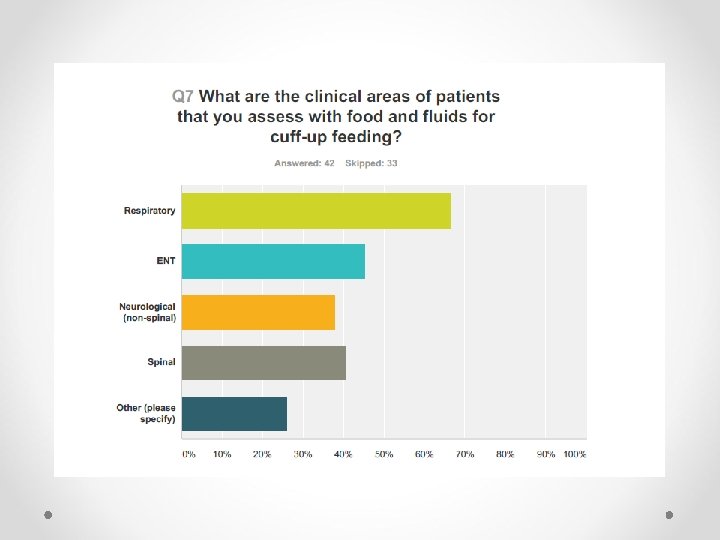
Survey Results cont’d Differences in Clinical Assessment • 21% won’t assess without cuff down • 32% will assess without cuff deflation • 25% will contrast up and down swallow status • Most sites do fewer than 2 cuff up assessments per year • One site does > 50 p/year • Sites that receive greater than 30 SP referrals per year for tracheostomy are more likely to practice cuff up feeding • 70% of sites with > than 30 per year referrals are doing this practice
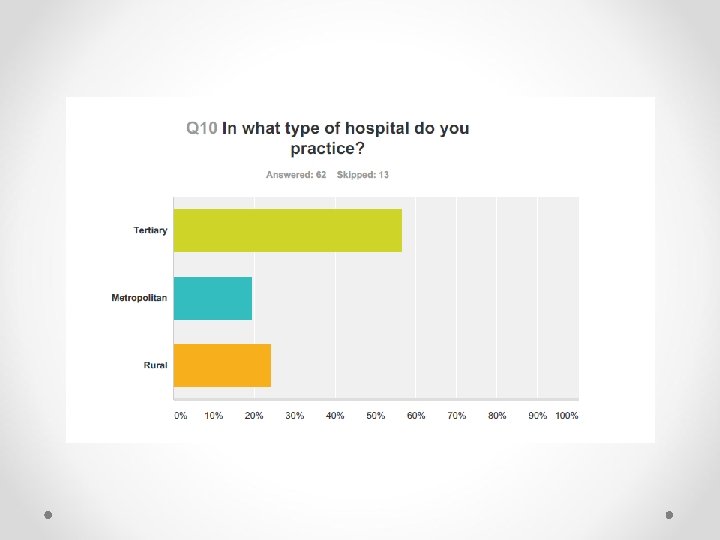
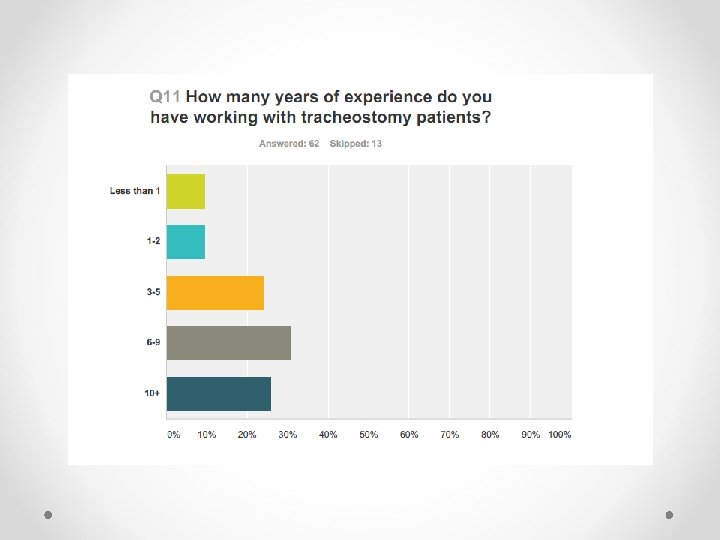
Survey Results cont’d Demographic data comparison: Location • • Therapists who responded from tertiary hospitals seemed to have more awareness that the evidence is mixed Cuff up feeding assessment was practiced more by therapists at tertiary hospitals (% of respondents who feed at each site: tertiary = 67, metro = 33, rural =13) Demographic data: Years of Experience • • • Increased years of experience = increased knowledge of evidence Increased years of experience = increased cuff up feeding practice Years of experience did not determine a preference for clinical vs instrumental assessment Other: • People that said they don’t feed patients with the cuff up worked at sites with less than 30 trache referrals per year
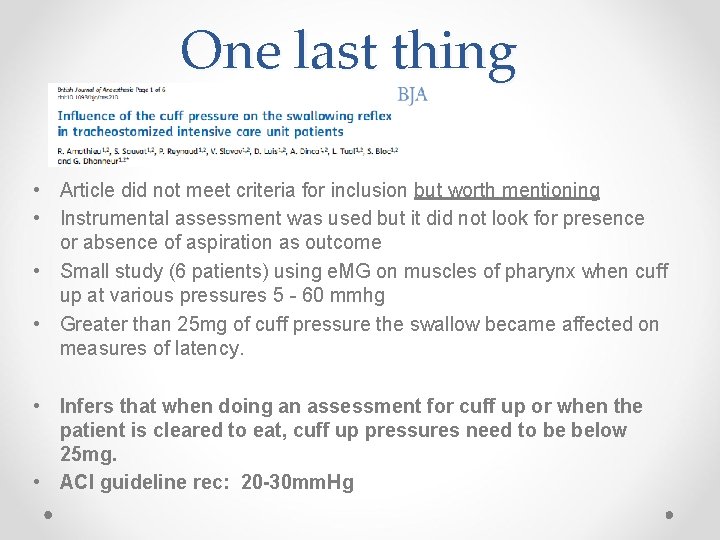
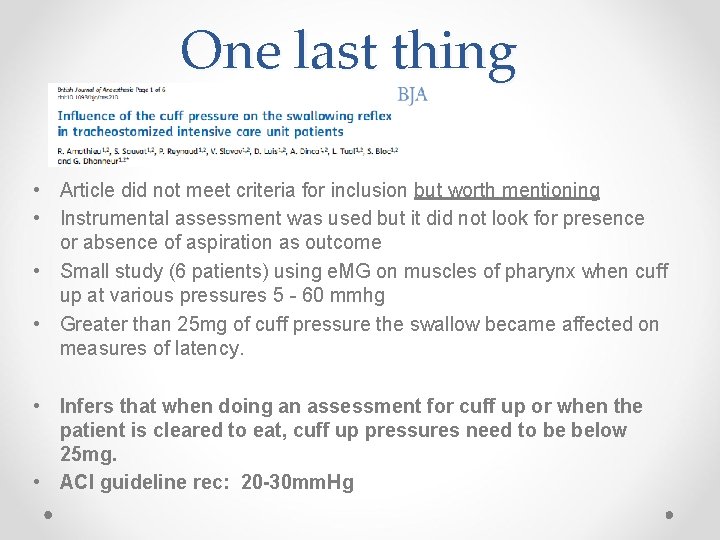
One last thing • Article did not meet criteria for inclusion but worth mentioning • Instrumental assessment was used but it did not look for presence or absence of aspiration as outcome • Small study (6 patients) using e. MG on muscles of pharynx when cuff up at various pressures 5 - 60 mmhg • Greater than 25 mg of cuff pressure the swallow became affected on measures of latency. • Infers that when doing an assessment for cuff up or when the patient is cleared to eat, cuff up pressures need to be below 25 mg. • ACI guideline rec: 20 -30 mm. Hg
Summary • The evidence is inconclusive as to whether an inflated cuff exacerbates / increases aspiration of food or fluids at the level of the vocal folds • Based on the survey findings different clinical assessment of swallowing is occurring i. e. , bedside, instrumental • The survey shows cuff inflated swallow assessment / feeding differs from site to site. This appears to be due to a number of factors e. g. No of referrals / hospital size / late or early referral / policies and procedures / experience of speech pathologists in this area etc…
Where to ? Should clinicians be considering cuff up feeding where we didn’t before with careful assessment, medical support given the potential benefits? Other factors to consider may also include Quality of life approach for patients who are unable to have the cuff deflated. Currently there is no evidence which indicates best practice for swallow assessment in tracheostomy with an inflated cuff. However, instrumental assessment is considered the gold standard for dysphagia management therefore it should be considered in this patient population.
Acknowledgements Cuff up working group: Klint Goers, Rachelle Robinson, Katherine Symeou, Elise Hamilton-Foster, Karen Mc. Barron, Christian Wiley Trache and critical care group members: Rebecca Black; Lindsay Wagner; Katherine Watson; Katherine Symeou; Laura O'Carrigan; Kelly Richardson; Pip Taylor; Shaun Deery, Thanks to Rebecca Black and Shaun Deery (retiring after 2 years) as leaders. New leaders in 2014: Kate Watson and Kelly Richardson
 Cuff inflated tracheostomy
Cuff inflated tracheostomy Shiley trach sizes chart
Shiley trach sizes chart Enteral parenteral beslenme
Enteral parenteral beslenme Air inflated pneumatic structures
Air inflated pneumatic structures What causes a balloon to remain inflated? *
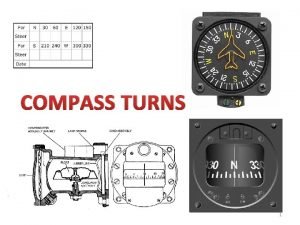
What causes a balloon to remain inflated? * Compass turn
Compass turn Friction is ______ if your tires are under-inflated
Friction is ______ if your tires are under-inflated Examples of inflated language
Examples of inflated language Proper blood pressure cuff placement
Proper blood pressure cuff placement Shoulder girdle muscles
Shoulder girdle muscles Rotator cuff examination
Rotator cuff examination Rotatro cuff
Rotatro cuff Rotator cuff tendinitis
Rotator cuff tendinitis Paul cuff
Paul cuff Pediatric cuff size
Pediatric cuff size Rotator cuff anatomy
Rotator cuff anatomy Sleeve styles
Sleeve styles Subscapularis action
Subscapularis action Skulder anatomi muskler
Skulder anatomi muskler Rotator cuff innervation
Rotator cuff innervation Calf cuff
Calf cuff Inverted champagne bottle sign
Inverted champagne bottle sign Cuff your hands
Cuff your hands Sits rotator cuff
Sits rotator cuff Acromion resectie
Acromion resectie Ray nimmo
Ray nimmo Ligament huméral transverse
Ligament huméral transverse Cuff bladder length
Cuff bladder length Rotator cuff kasları
Rotator cuff kasları Universal cuff
Universal cuff Empty-can test
Empty-can test