TRACHEOSTOMY CARE AND EMERGENCIES Indications for tracheostomy Airway




- Slides: 13
TRACHEOSTOMY CARE AND EMERGENCIES
Indications for tracheostomy Airway Severe Facial Trauma, Head and neck cancers / tumours Acute Angioedema and Inflammation of the head and neck. Ventilation Respiratory wean / tracheal toilet – ICU setting (performed in 8 -24% of ICU patients) Need for long-term mechanical ventilation – often neurological indication Obstructive Sleep Apnoea seen in patients intolerant of Continuous Positive Airway Pressure (CPAP) therapy. Emergencies Failed orotracheal or nasotracheal intubation, either tracheotomy or cricothyroidotomy may be performed.
ICU Tracheostomies ITU indications: Prevents laryngeal / upper airway damage from prolonged translaryngeal intubation. Access to the lower airway for suctioning Stable airway for long-term weaning Vs ETT reduces resistive and elastic work of breathing Easier mouth care Earlier entral feeding and mobilisation Improved comfort and reduced sedative usage Complications: Bleeding, infection, stenosis, death Need to identify patients early: Avoid tracheostomy in patients who can be weaned quickly Perform tracheostomy early in patients who will need long-term mechanical ventilation / slow weaning
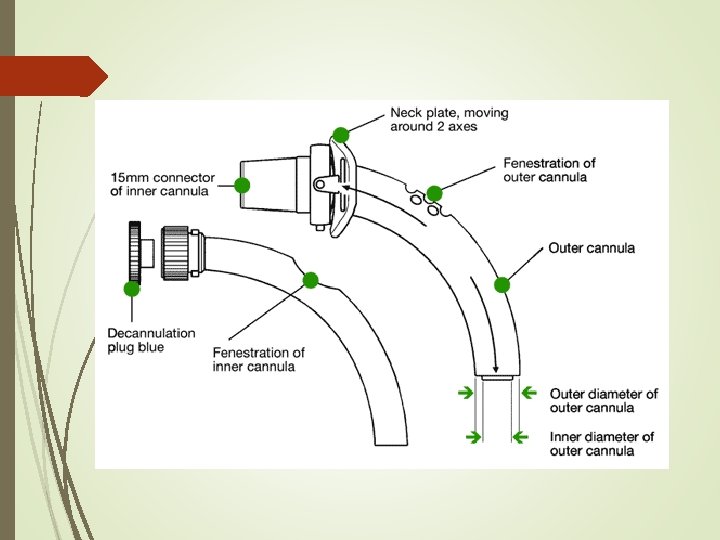
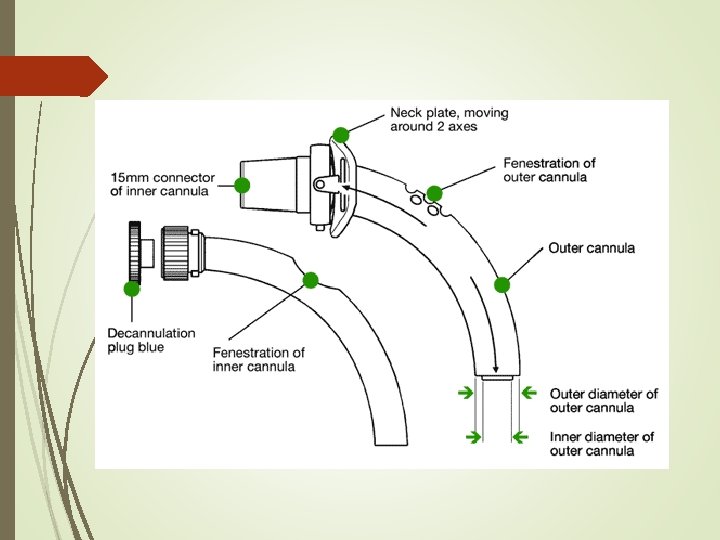
Tracheostomy Tube Types Single or double lumen Double lumen – removable inner tube for cleaning – considered safer Uncuffed Air can flow through the tracheostomy or the oropharynx Cuffed Allows for IPPV Prevents aspiration Fenestrated tubes Allows increased airflow through the upper airway giving the patient the ability to speak and cough Can be blocked by using and un-fenestrated inner tube to allow IPPV and prevent aspiration.


Anaesthesia for a surgical tracheostomy Pre-op Consider using ICU vent and TIVA STOP NG feed Correct coagulopathy Peri-op Head ring, neck extension and head elevation Tape tube and keep pilot balloon available Aspirate NGT and oropharynx Preoxygenate prior to tube change ! RISK OF AIRWAY FIRE! Prior to incision of trachea either withdraw or advance tube to avoid damage to cuff. Surgeon will direct withdrawal of ETT under direct vision to allow insertion of tracheostomy, don’t complete withdraw until surgeon confirms position within trachea Attach circuit to tracheostomy and confirm position / ability to ventilate.
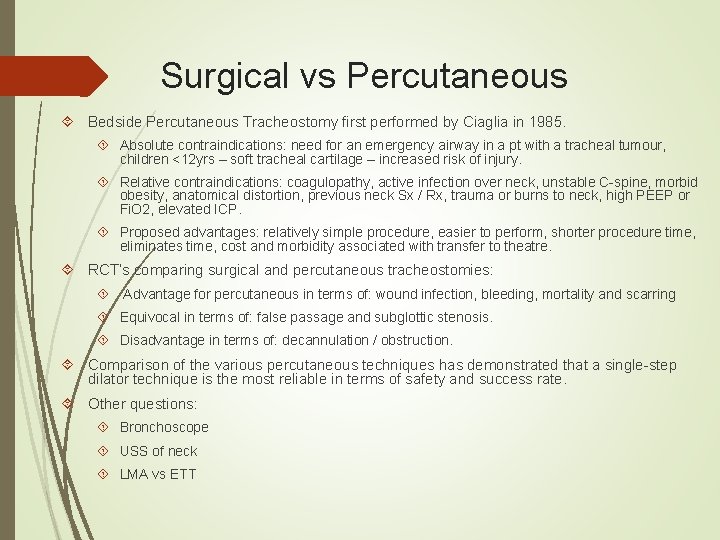
Surgical vs Percutaneous Bedside Percutaneous Tracheostomy first performed by Ciaglia in 1985. Absolute contraindications: need for an emergency airway in a pt with a tracheal tumour, children <12 yrs – soft tracheal cartilage – increased risk of injury. Relative contraindications: coagulopathy, active infection over neck, unstable C-spine, morbid obesity, anatomical distortion, previous neck Sx / Rx, trauma or burns to neck, high PEEP or Fi. O 2, elevated ICP. Proposed advantages: relatively simple procedure, easier to perform, shorter procedure time, eliminates time, cost and morbidity associated with transfer to theatre. RCT’s comparing surgical and percutaneous tracheostomies: Advantage for percutaneous in terms of: wound infection, bleeding, mortality and scarring Equivocal in terms of: false passage and subglottic stenosis. Disadvantage in terms of: decannulation / obstruction. Comparison of the various percutaneous techniques has demonstrated that a single-step dilator technique is the most reliable in terms of safety and success rate. Other questions: Bronchoscope USS of neck LMA vs ETT

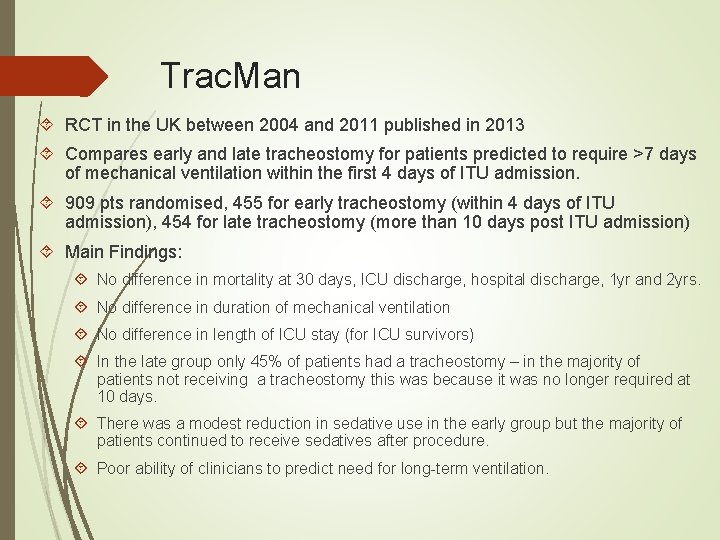
Trac. Man RCT in the UK between 2004 and 2011 published in 2013 Compares early and late tracheostomy for patients predicted to require >7 days of mechanical ventilation within the first 4 days of ITU admission. 909 pts randomised, 455 for early tracheostomy (within 4 days of ITU admission), 454 for late tracheostomy (more than 10 days post ITU admission) Main Findings: No difference in mortality at 30 days, ICU discharge, hospital discharge, 1 yr and 2 yrs. No difference in duration of mechanical ventilation No difference in length of ICU stay (for ICU survivors) In the late group only 45% of patients had a tracheostomy – in the majority of patients not receiving a tracheostomy this was because it was no longer required at 10 days. There was a modest reduction in sedative use in the early group but the majority of patients continued to receive sedatives after procedure. Poor ability of clinicians to predict need for long-term ventilation.

1. The ventilator liberation process: update on technique, timing, and termination of tracheostomy. Respiratory Care October 1, 2012 vol. 57 no. 10 1626 -1634 2. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the Trac. Man randomized trial. JAMA. 2013; 309(20): 2121 -2129 3. Tracheostomy management Contin Educ Anaesth Crit Care Pain (2008) 8 (1): 31 -35.
 Upper airway and lower airway
Upper airway and lower airway Indications for artificial airway
Indications for artificial airway Site:slidetodoc.com
Site:slidetodoc.com Tracheostomy indication and contraindication
Tracheostomy indication and contraindication Tracheostomy care
Tracheostomy care Tracheostomy care
Tracheostomy care Tracheostomy care
Tracheostomy care Summary of tracheostomy care
Summary of tracheostomy care Tracheostomy care
Tracheostomy care Contraindications for vaginal delivery
Contraindications for vaginal delivery Primary care secondary care tertiary care
Primary care secondary care tertiary care Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies