CLINICAL CONSENSUS STATEMENT Tracheostomy Care Terri Giordano MSN



- Slides: 56
CLINICAL CONSENSUS STATEMENT Tracheostomy Care Terri Giordano MSN, CRNP, CORLN Division of Otolaryngology The Children’s Hospital of Philadelphia
Clinical Practice Guidelines � Systematically developed statements to assist practitioner and patient decisions about appropriate health care for specific clinical circumstances � Define the role of diagnostic and treatment modalities � Recommendations are evidence-based
Clinical Practice Guidelines � Range of generally accepted approaches for diagnosis, management or prevention � Define practices that meet the needs of most patients in most circumstances
Quality Guidelines � Explicit scope and purpose � Stakeholder � Rigor involvement of development � Clarity of presentation � Applicability � Editorial independence
Clinical Practice Guidelines � Better outcomes � Decreased � Greater ineffective interventions consistency of care
Clinical Practice Guidelines � Improved � Initiate decision making quality improvement � Prioritize � Support research coverage or reimbursement
Clinical Consensus Statement (CCS) � Information opinion � Reflects synthesized from a group of expert views of panel � Examine � Provided and discuss available scientific data for informational and educational purposes only
Expert Review Panel � Synthesize information � Provide clear and accurate answer to the question of interest � Reflect uncertainties, opinions or minority viewpoints � Potential for bias
Clinical Consensus Statement (CCS) � Not intended as a legal document � Findings stated as opinion or suggestions
Consensus Method � Delphi Method � Nominal � The Group Technique Consensus Development Conference
CCS Tracheostomy Care � Aims to improve care for pediatric and adult patients with a tracheostomy tube � Reduce variations in practice and minimize complications
CCS Tracheostomy Care � No controlled studies or peer reviewed papers to guide care or practice � Evidence-based � Lack research is lacking of current literature support

Expert Panel � Pediatric and adult otolaryngology � Advanced practice nursing � Respiratory therapy � Emergency medicine
Literature Search � Cochrane ENT Disorders Group � Clinical practice guidelines, systematic reviews and meta-analyses � Randomized controlled trials, observational studies and case series
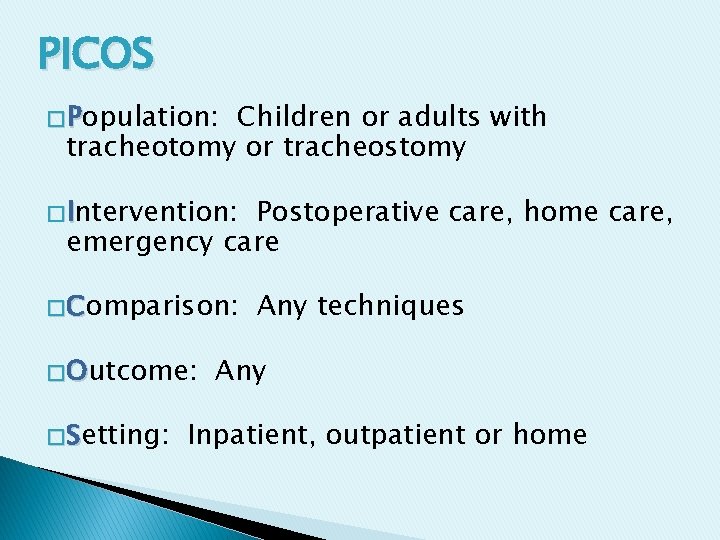
PICOS � Population: Children or adults with tracheotomy or tracheostomy � Intervention: Postoperative care, home care, emergency care � Comparison: � Outcome: � Setting: Any techniques Any Inpatient, outpatient or home
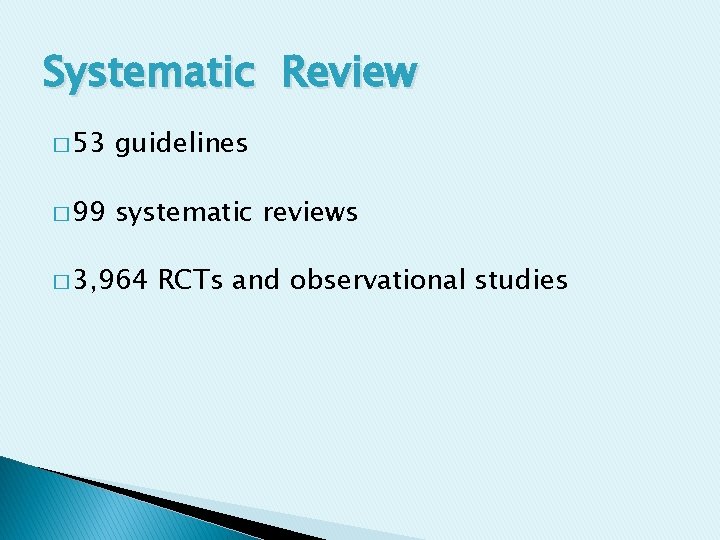
Systematic Review � 53 guidelines � 99 systematic reviews � 3, 964 RCTs and observational studies
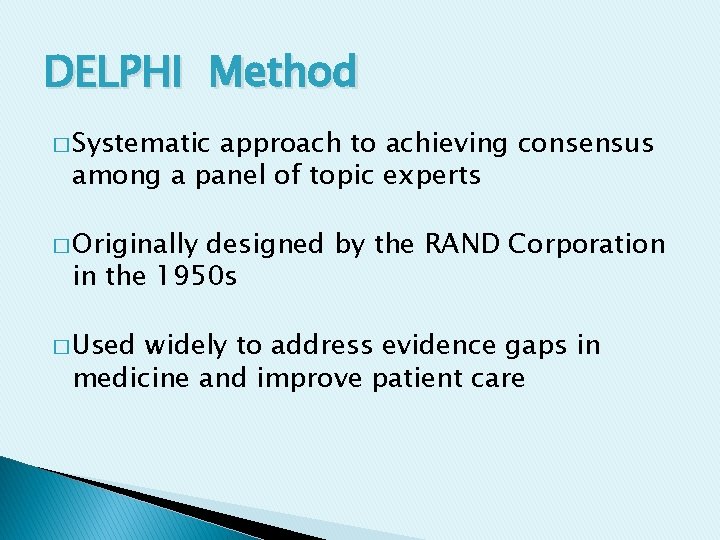
DELPHI Method � Systematic approach to achieving consensus among a panel of topic experts � Originally designed by the RAND Corporation in the 1950 s � Used widely to address evidence gaps in medicine and improve patient care
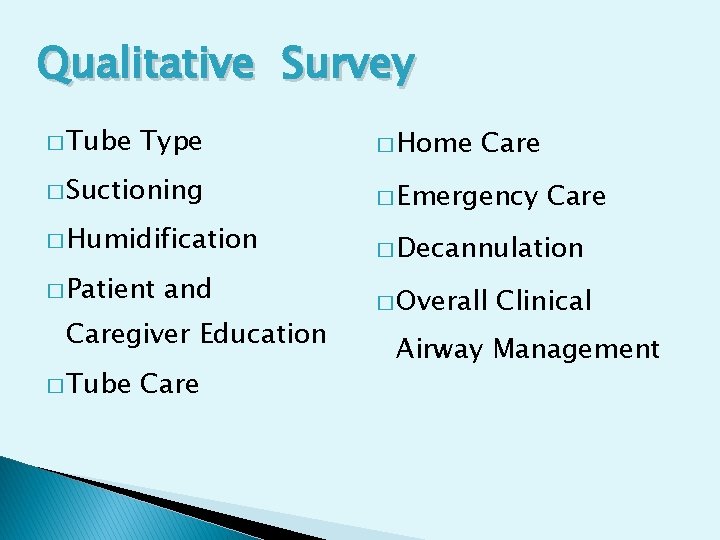
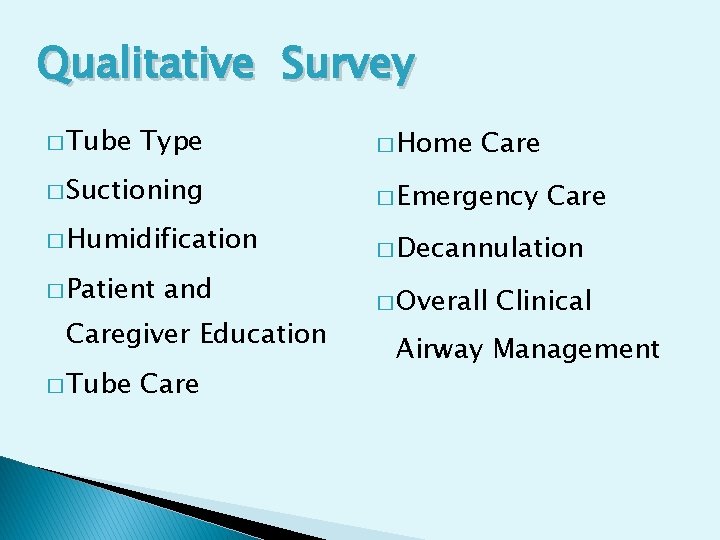
Qualitative Survey � Tube Type � Home Care � Suctioning � Emergency � Humidification � Decannulation � Patient and Caregiver Education � Tube Care � Overall Care Clinical Airway Management
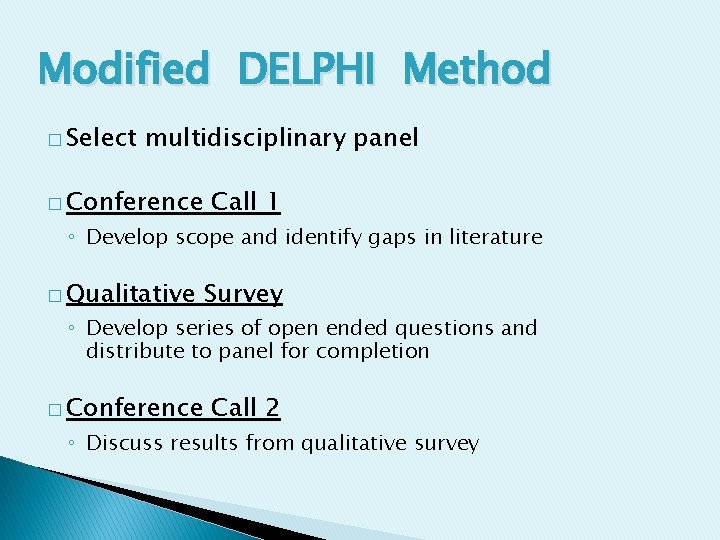
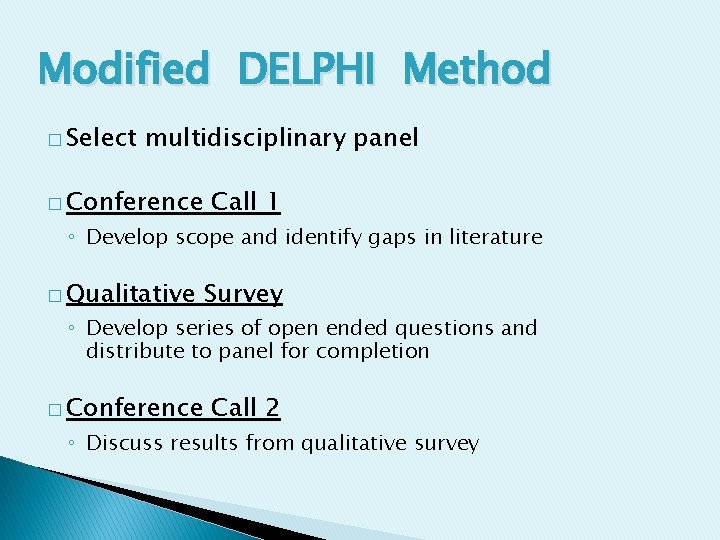
Modified DELPHI Method � Select multidisciplinary panel � Conference Call 1 � Qualitative Survey � Conference Call 2 ◦ Develop scope and identify gaps in literature ◦ Develop series of open ended questions and distribute to panel for completion ◦ Discuss results from qualitative survey
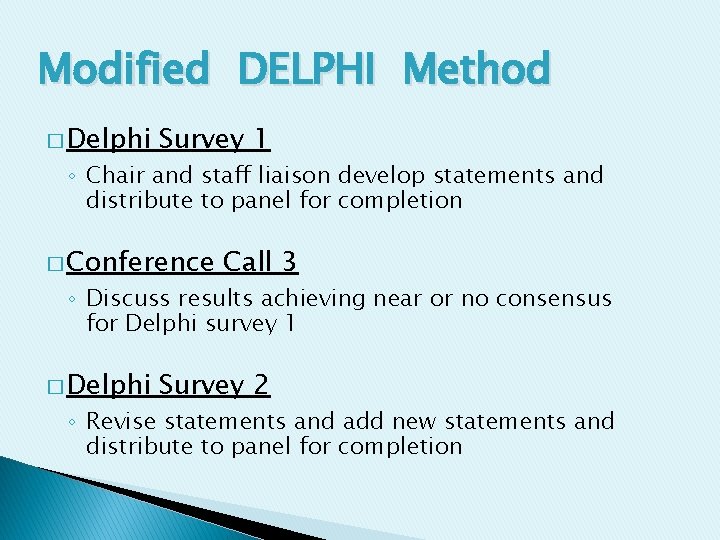
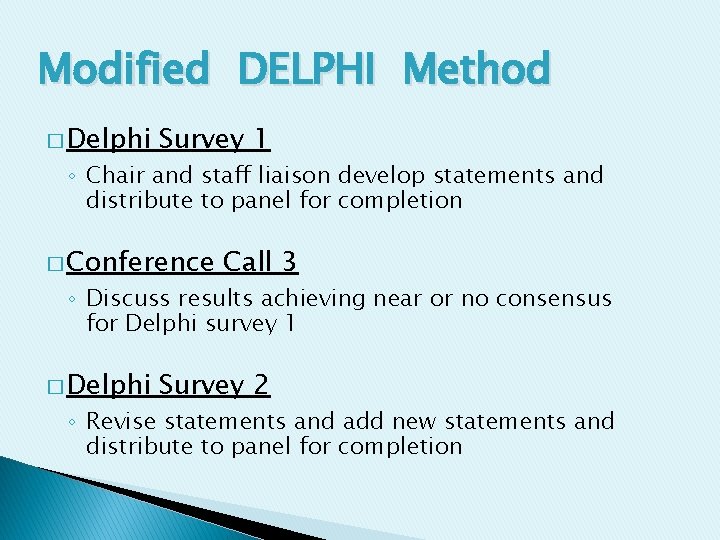
Modified DELPHI Method � Delphi Survey 1 ◦ Chair and staff liaison develop statements and distribute to panel for completion � Conference Call 3 ◦ Discuss results achieving near or no consensus for Delphi survey 1 � Delphi Survey 2 ◦ Revise statements and add new statements and distribute to panel for completion
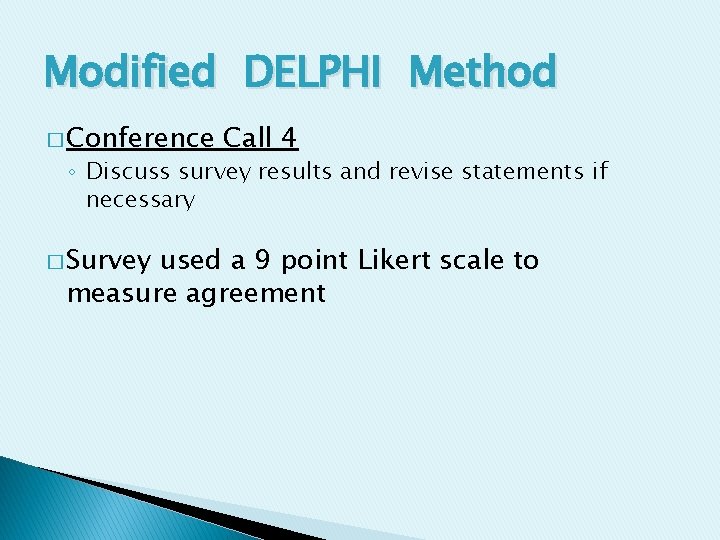
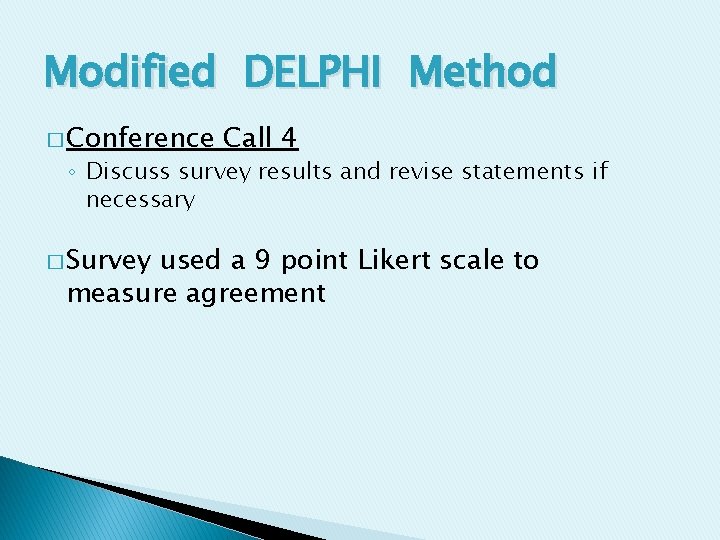
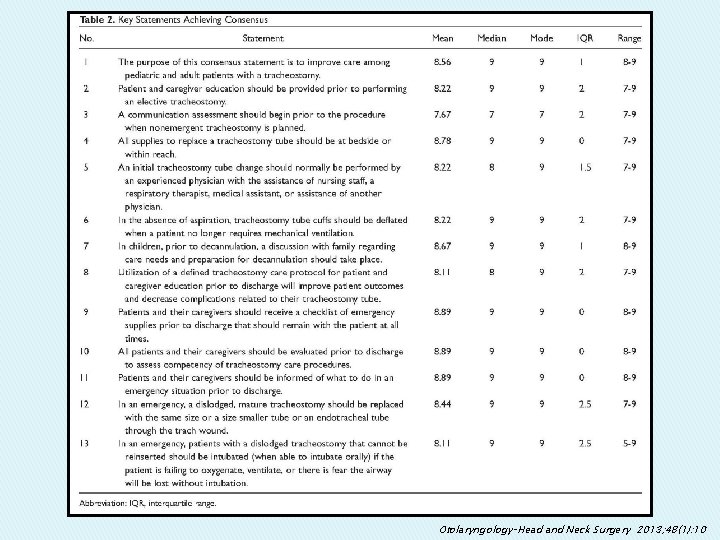
Modified DELPHI Method � Conference Call 4 ◦ Discuss survey results and revise statements if necessary � Survey used a 9 point Likert scale to measure agreement
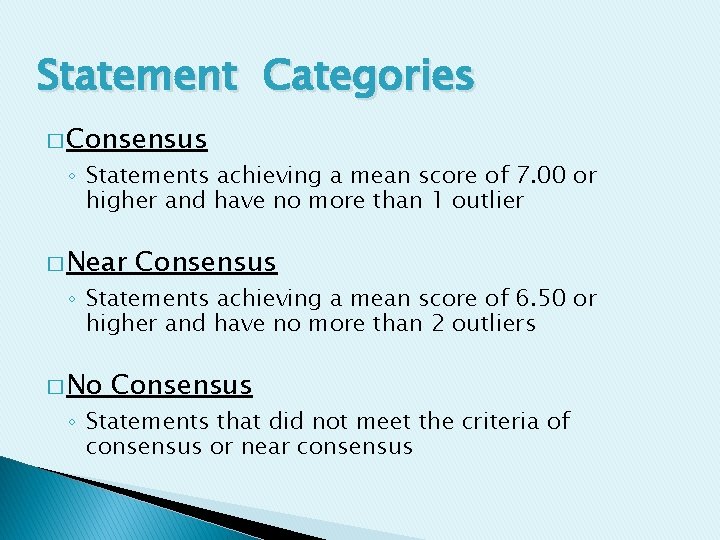
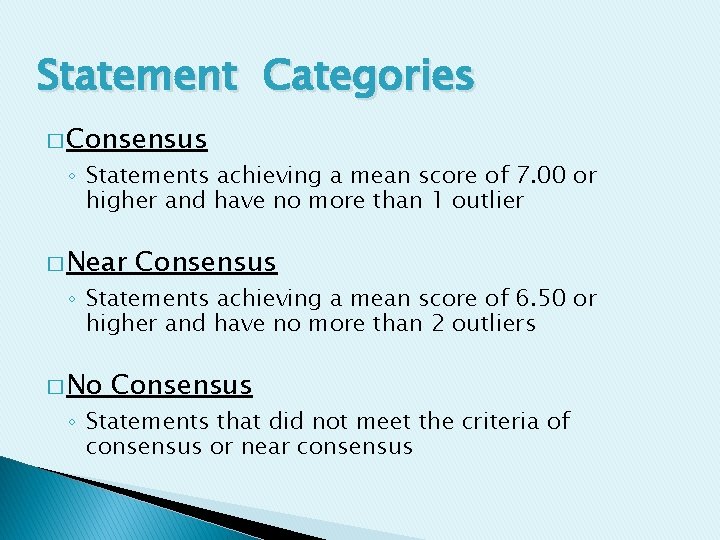
Statement Categories � Consensus ◦ Statements achieving a mean score of 7. 00 or higher and have no more than 1 outlier � Near Consensus ◦ Statements achieving a mean score of 6. 50 or higher and have no more than 2 outliers � No Consensus ◦ Statements that did not meet the criteria of consensus or near consensus
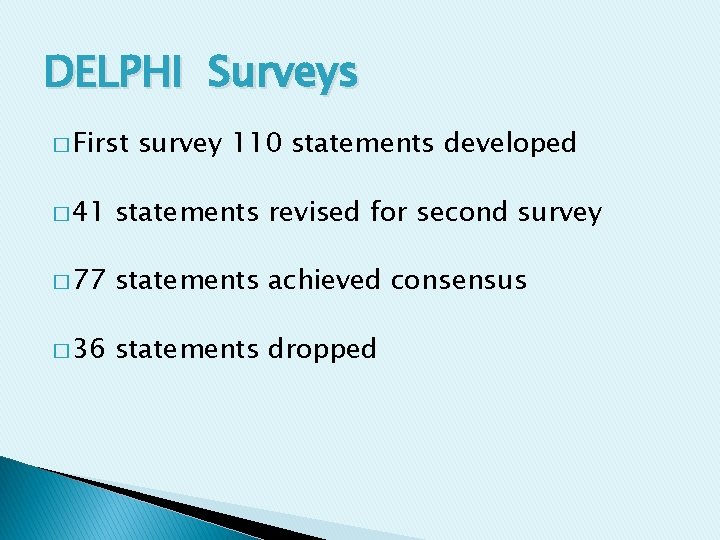
DELPHI Surveys � First survey 110 statements developed � 41 statements revised for second survey � 77 statements achieved consensus � 36 statements dropped
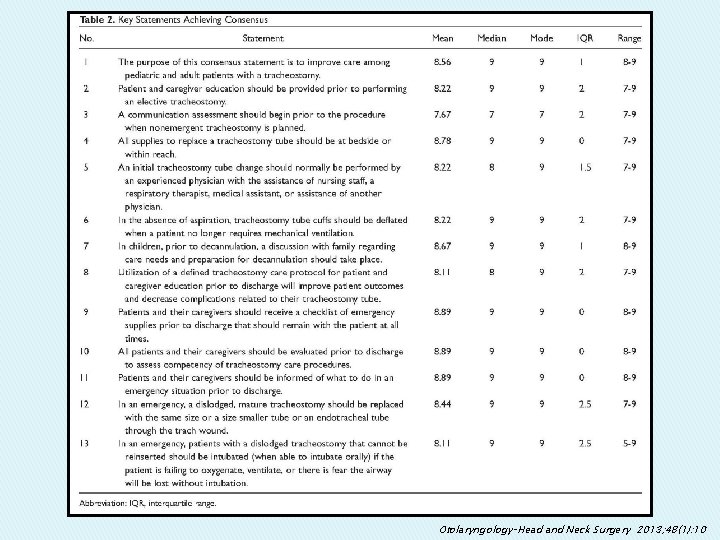
Otolaryngology–Head and Neck Surgery 2013; 48(1): 10
Consensus � Plastic tracheostomy tubes should be used in pediatric and adult patients for initial tube placement. � When determining appropriate diameter, tracheostomy tube, lung mechanics, upper airway resistance and airway clearance should be considered.
Consensus � Tracheostomy tube ties should be used unless the patient recently underwent local or free flap reconstruction surgery or other major neck surgery. �A patient should not be discharged from the hospital with a tracheostomy tube sutured in place.
Consensus � Humidification should be used during the immediate postoperative period and as necessary thereafter. � During hospitalization and at home, the inner cannula should be cleaned regularly. � When at home, the tracheostomy tube should normally be replaced using clean technique.
Consensus � The stoma and tracheostomy tube should be suctioned when there is evidence of visible or audible secretions in the airway. � The stoma and tracheostomy tube should be suctioned before and after the tracheostomy tube is changed.
Consensus �A patient should not use a swallowing or speaking valve while the tracheostomy tube cuff is inflated. � Acute tracheostomy tube occlusion is most likely caused by a mucous plug, obstructing granuloma or insertion of the tube into a false tract.
Consensus � In an emergency, a dislodged fresh tracheostomy (within 7 days of tube insertion) should be replaced with the same size or a size smaller tube and the patient observed for a period of time.
Consensus � In an emergency, a dislodged fresh tracheostomy (within 7 days of tube insertion) should be replaced and the service responsible for inserting the original tube should be contacted.
Consensus �A patient may be turned in bed once tube security has been assessed to avoid accidental decannulation. �A treatment plan should be developed based upon a communication assessment to include possible recommendation of speech or swallowing valve and referral to a speech language pathologist.
Consensus � If a patient and/or their caregivers are incapable of properly caring for the tracheostomy, home nursing care should be considered. �A home care instruction manual for tracheostomy should be given to patients and their caregivers prior to discharge.
Pediatric Consensus �A child’s initial tracheostomy tube should be replaced within 5 -7 days if inserted surgically. � In children, prior to decannulation, a bronchoscopy should be performed within a few months to ensure a patent airway with no occluding suprastomal granulation.
Pediatric Consensus � There should be no documented aspiration events that would preclude decannulation. � In children, prior to decannulation, no ventilator assistance should be needed where a tracheostomy would be required.
Pediatric Consensus � For children, prior to decannulation, the tracheostomy tube should be capped all day and the cap removed at night for several weeks to determine whether the cap can remain on even when the child has a URI.
Pediatric Consensus � Prior to decannulation, children should undergo a daytime capping trial (if they are over the age of 2 years and if the tracheostomy does not occupy so much of the trachea so as to preclude capping). � If they pass, options for decannulation include a capped sleep study, a capped exercise test, or a nighttime capping trial while hospitalized and being observed.
Pediatric Consensus � In a child who is either too young or too small to undergo a successful capping trial, decannulation protocols need to be individualized for the particular patient.
Adult Consensus � Metal or plastic tubes can be used for long term (>1 year) tracheostomy among adults who do not require ventilation. � In adults, prior to decannulation, initial indicators for tracheostomy should be reviewed and reasons for the tracheostomy should have improved or resolved to an appropriate degree.
Adult Consensus � In adults, prior to decannulation, there should be no evidence of gross aspiration based on the fiber-optic laryngoscopy exam or visualizing tolerance of secretions when the cuff is deflated.
Adult Consensus � In adults, prior to decannulation, a physician should confirm that the patient’s level of consciousness and laryngeal-pharyngeal function can protect the tracheobronchial tree from aspiration.
Adult Consensus � In adults, prior to decannulation, if there are concerns regarding airway patency, a bronchoscopy should be performed. � In adults, prior to decannulation, the patient should have an effective cough while the tracheostomy tube is capped.
Near Consensus � Fresh tracheostomies should be replaced using a sterile technique. � Tracheostomy tube cuffs should be used routinely among adult patients requiring mechanical/assisted ventilation. � Caregivers discharge. should know basic CPR prior to
Near Consensus � Tracheostomy tube cuffs should be used among patients experiencing recurrent respiratory infections or aspiration. �A minimal leak test should be used to aid in tracheostomy tube cuff deflation.
Near Consensus � During hospitalization, a nondisposable plastic or metal inner cannula should be cleaned with half-strength hydrogen peroxide and rinsed with sterile normal saline. � Velcro tracheostomy tube ties should be used for children and adults if available.
No Consensus � Following the initial tracheostomy tube change, the tracheostomy tube should be replaced weekly or biweekly based on physician preference and patient circumstances. � If a patient has a compromised airway, a tracheostomy tube should not be replaced until the infection has resolved.
No Consensus � Tracheostomy tube cuffs should be used postoperatively to prevent air leaks and aspiration. � Tracheostomy tube cuffs should be used among patients requiring pulmonary toilet.
No Consensus � The tracheostomy tube should not be suctioned past its tip. � Sutures are necessary in adults to secure the tracheostomy tube. � Sutures are necessary in children to secure the tracheostomy tube. � Tracheostomy tube ties should be used among patients with sutures in place.
No Consensus � In adults, tracheostomy tube cuffs may be inflated with normal saline or water. � In children, water should not be used to inflate tracheostomy cuffs.

Home Care � Signs of respiratory distress � Signs of infection and skin breakdown � Checklist � Contacts of emergency supplies ◦ Health care provider ◦ Health care personnel ◦ Equipment supply company
Home Care � Suctioning � Cleaning � Changing � Using the tracheostomy tube home equipment
Future Research � To define quality metrics related to tracheostomy care that correlate to early hospital discharge � To define important factors in patients with a tracheostomy that may influence the frequency of site infections, accidental tube displacement, emergency room visits and readmission to the hospital

Future Research � Determine whether trained APPs are able to perform initial tracheostomy changes with similar or fewer complication rates compared with experienced physicians
References � Mitchell RB, Hussey HM, Setzen G, Jacobs IN et al. Clinical Consensus Statement: Tracheostomy care. Otolaryngol Head Neck Surg 2013; 148(1): 6 – 20. � http: //www. entnet. org/practice/update/clinical- consensus-statement � http: //nhlbi. nih. gov � Rosenfeld RM, Shiffman RN. Clinical practice guideline development manual: A quality driven approach for translating evidence into action. Otolaryngol Head Neck Surg 2009; 140: S 1 -S 43.