Management of Patient with Tracheostomy Maya Govender Practice


- Slides: 36
Management of Patient with Tracheostomy Maya Govender Practice Educator – CTICU Foundations of Critical Care (FCCN) 17 th January 2018
Learning Outcomes • List the indications for a tracheostomy • List the types of different tracheostomy tubes • List the bed side equipment for a tracheostomy tube • Explain how to decannulate a patient from with a tracheotomy tube • Documentation
What is a Tracheostomy? A tracheostomy is an artificial surgically created airway fashion by an hole in the anterior wall of the trachea and the insertion of a tracheostomy tube, which may or may not be permanent
Indications Upper airway obstruction secondary to: trauma, burns corrosive poisoning laryngeal dysfunction foreign body infections, inflammatory conditions obstructive sleep apnoea Access for pulmonary toilet Prolonged ventilation support Airway protection in head injury or comatose patient
Advantages of Tracheostomy Increased patient mobility More secure airway Increased comfort Improved airway suctioning Early transfer of ventilator dependent patients from ITU Enhance communication Assists in weaning from the ventilator Decreased risk of pneumonia
How to create a Tracheostomy Percutaneous Tracheostomy Can be done in the ITU at the bedside Surgical Tracheostomy Cricothyroidotomy For urgent procedures
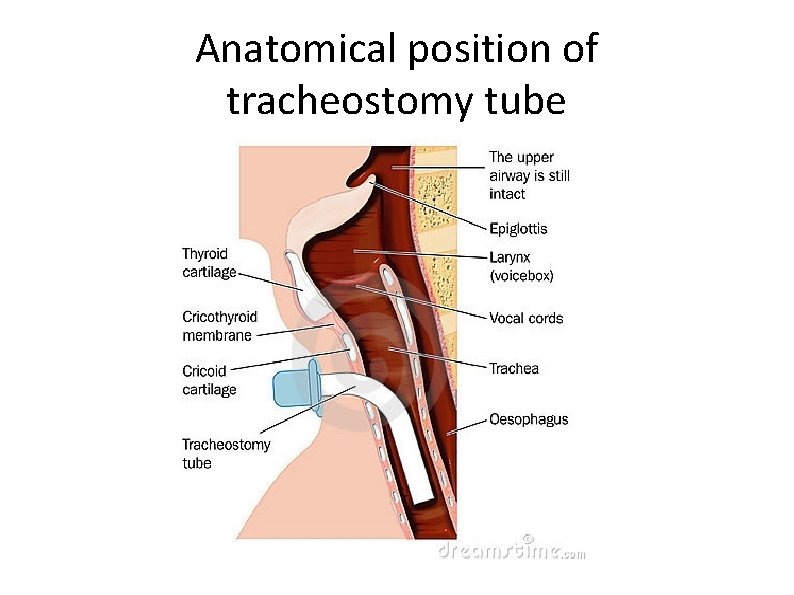
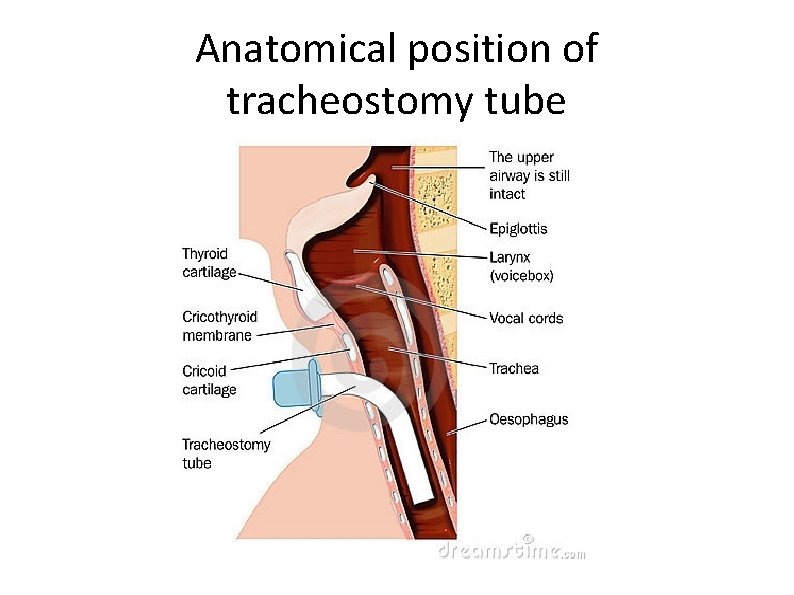
Anatomical position of tracheostomy tube
Types of tracheostomy tube used on the unit • Portex blue line without inner tube • Portex blue line ultra with inner tube • Portex blue line ultra fenestrated tube with fenestrated and clear non fenestrated inner tube • Portex blue line adjustable flange tube
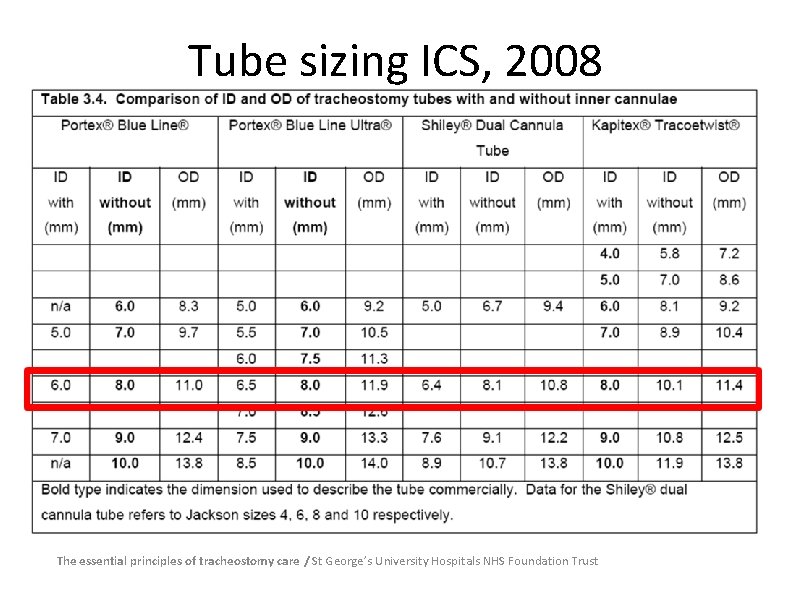
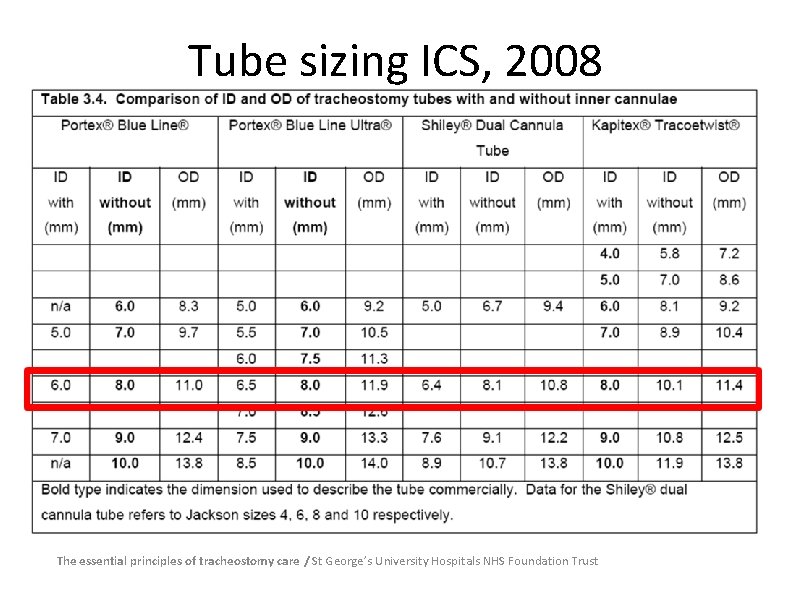
Tube sizing ICS, 2008 The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust

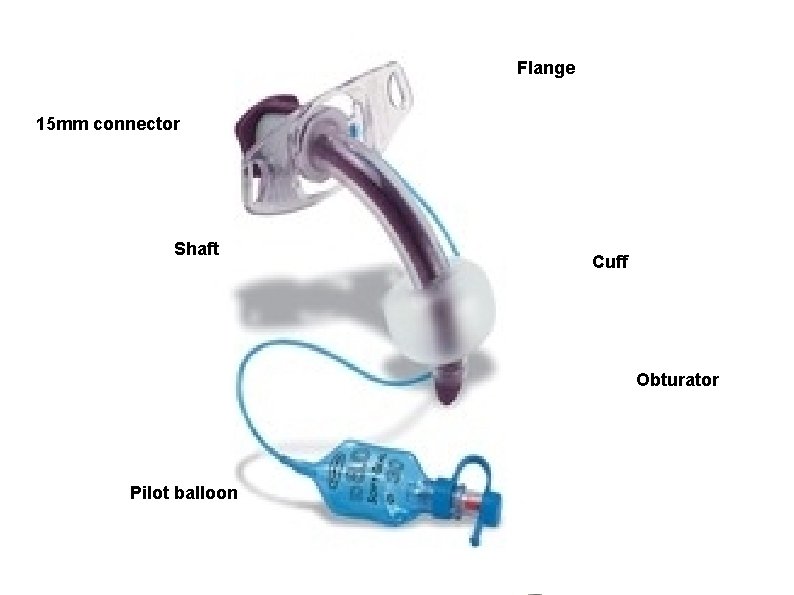
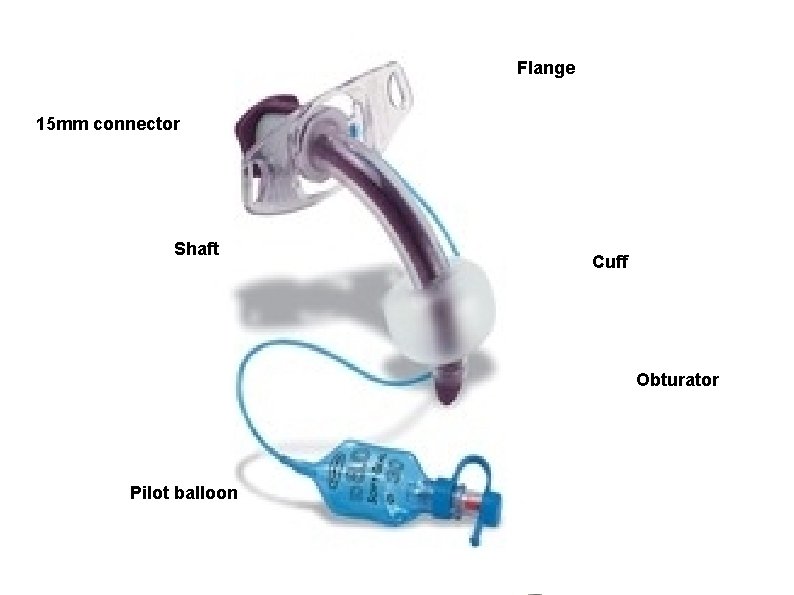
Flange 15 mm connector Shaft Cuff Obturator Pilot balloon
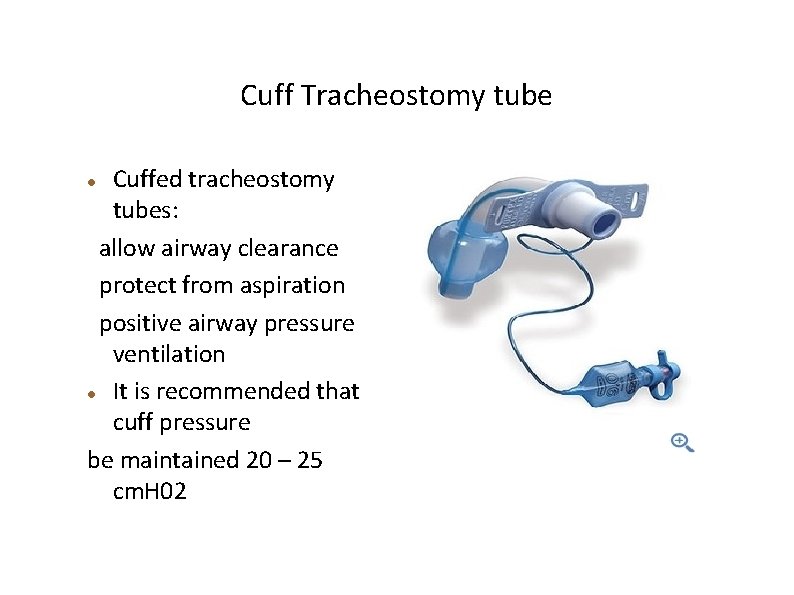
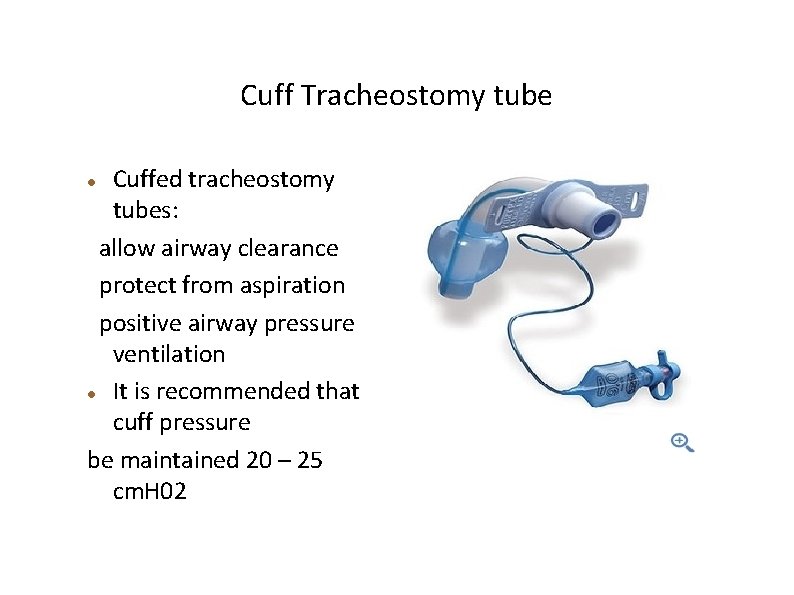
Cuff Tracheostomy tube Cuffed tracheostomy tubes: allow airway clearance protect from aspiration positive airway pressure ventilation It is recommended that cuff pressure be maintained 20 – 25 cm. H 02
Fenestrated Trachesotomy Tube The fenestrated tracheostomy tube is similar to the standard tracheostomy tube with the addition of the opening in the posterior portion of the tube above the cuff
Fenestrated Tubes This allows for assessment of the patient's ability to breath through the normal oral/nasal route Preparing the patient for decannulation Patient can talk with the Fenestrated Tube
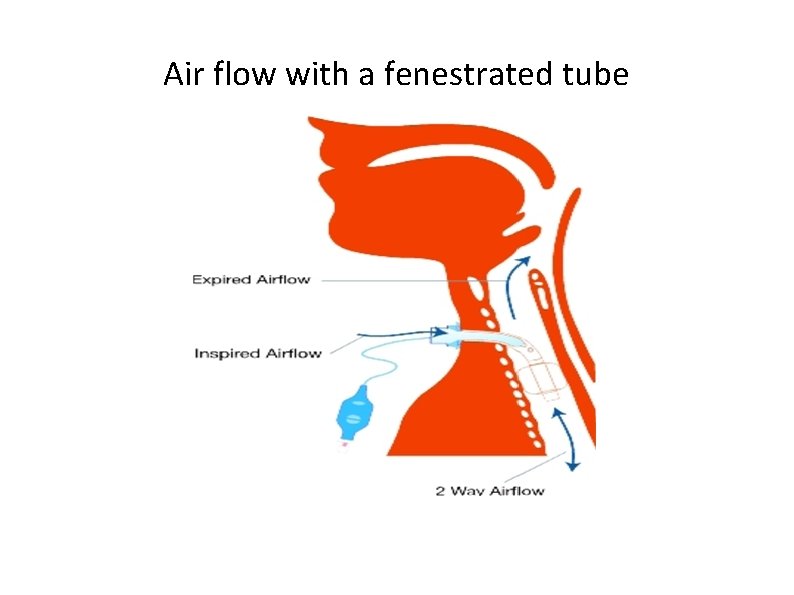
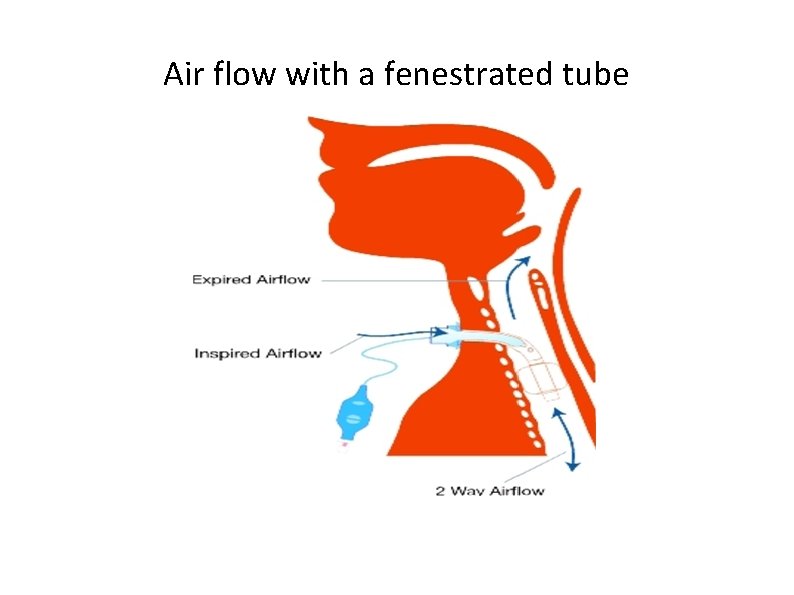
Air flow with a fenestrated tube
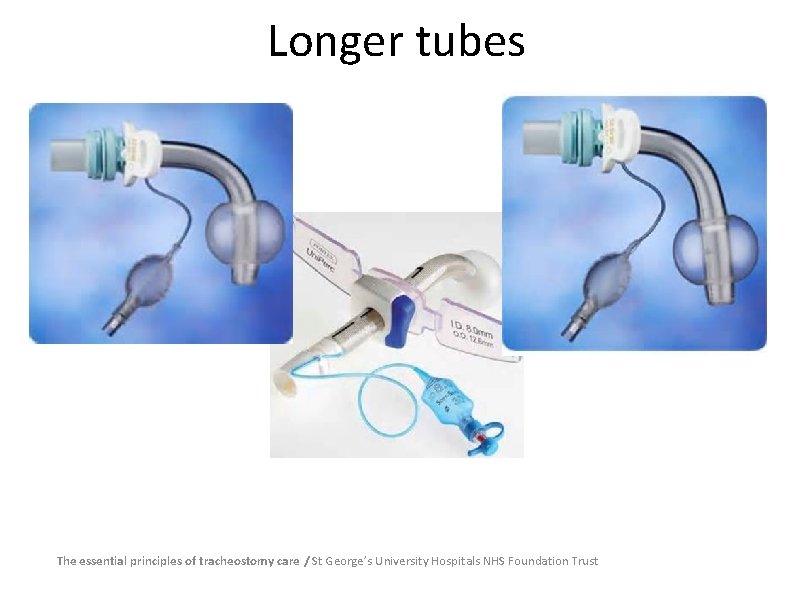
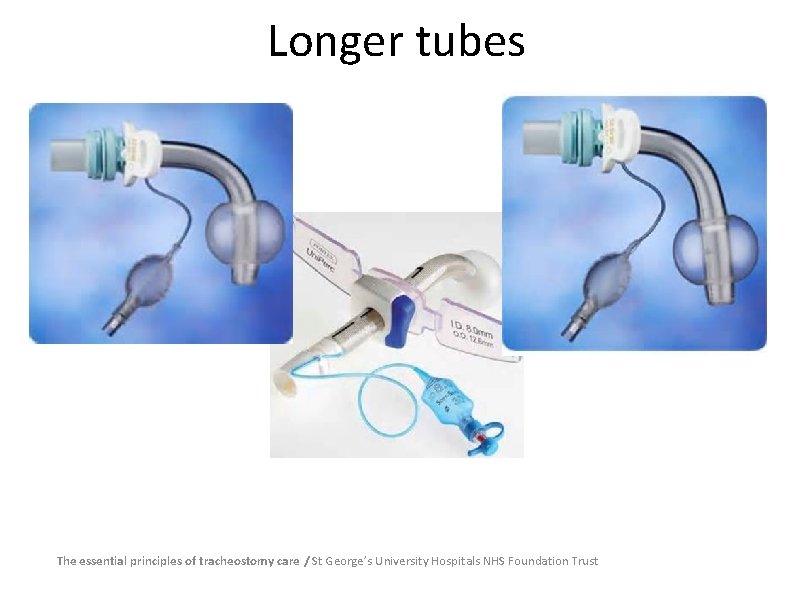
Longer tubes The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
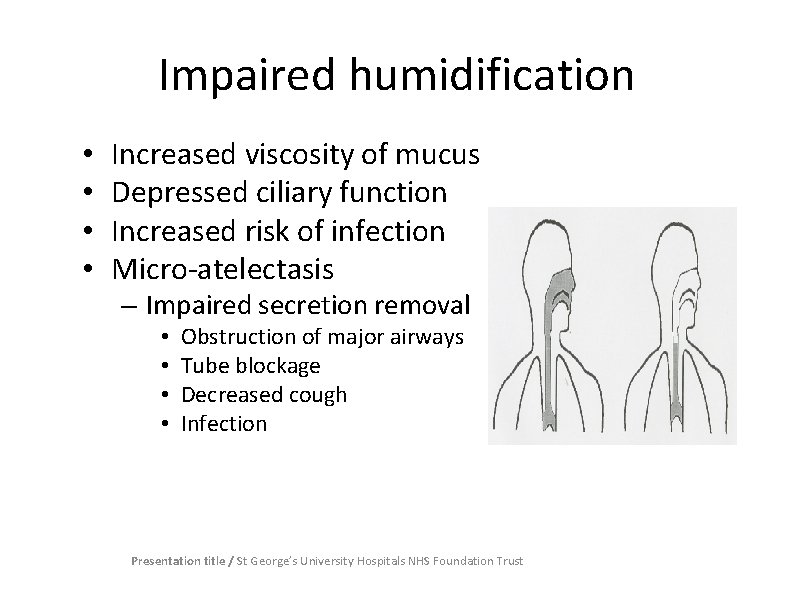
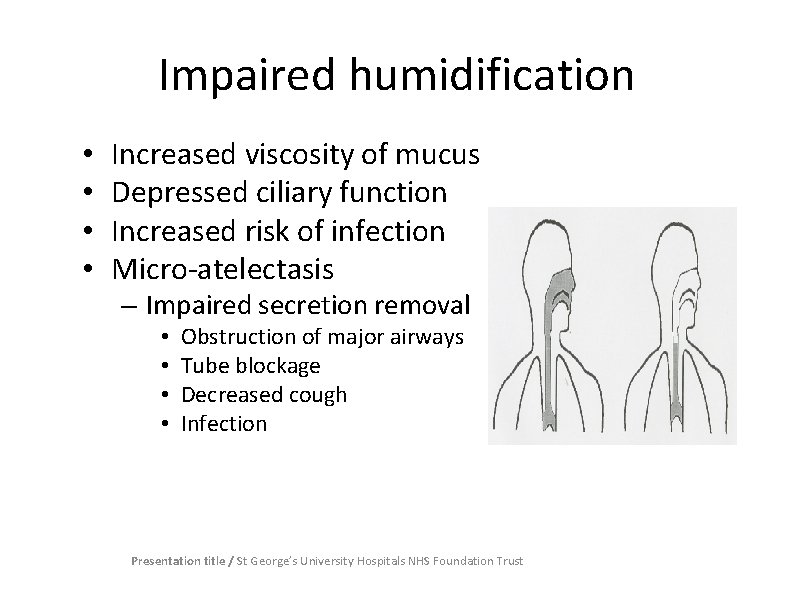
Impaired humidification • • Increased viscosity of mucus Depressed ciliary function Increased risk of infection Micro-atelectasis – Impaired secretion removal • • Obstruction of major airways Tube blockage Decreased cough Infection Presentation title / St George’s University Hospitals NHS Foundation Trust
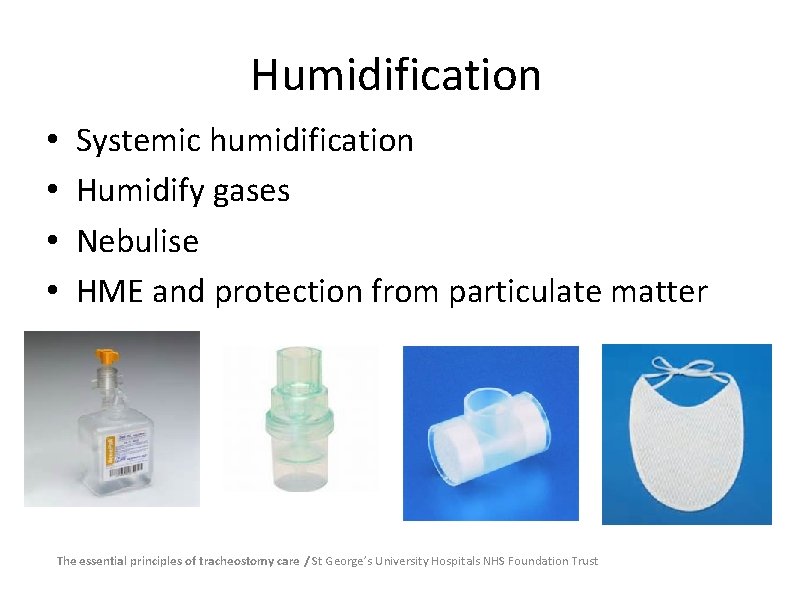
Humidification • • Systemic humidification Humidify gases Nebulise HME and protection from particulate matter The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
Suctioning • Assessment needed • Reserved for patients unable to clear own secretions • Cough yankeur suction • Pre-oxygenate? • 10 -16 k. Pa vacuum • ID mm -2 x 2 • Insert 10 -15 cm, stop if resistance felt and withdraw 2 cm The essential principles of tracheostomy care St George’s University Hospitals NHS Foundation Trust
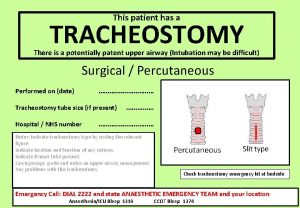
Equipment at the bedside Rebreathe bag, catheter mount, face mask • Ambubag & mask • Working suction, yanker and suction catheters • Tracheal dilators • 2 spare tracheostomy tubes one the same size and one smaller (of the same type of trachy tube in situ) • 10 ml syringe • Clean gloves, aprons and eye protection • Humidification – HME, wet humidification Poster
Care • Inner cannula – Routine use – Inspected four hourly • Cuff – Cuff manometer (20 -25 cm. H 2 O) • Oral hygiene – Acutely ill patients four - six hourly – Oral fluids where possible The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
Procedure for cleaning inner tube Wash hands, apply gloves, apron & eye protection • Remove inner tube and replace with the spare inner tube • Rinse the tube through with the sterile water using the disposable bowl • If necessary remove secretions with swabs and rinse with water • Dry with clean gauze • If the inner tube remains soiled and cleaning is ineffective dispose of this inner tube and replace with a new inner tube.
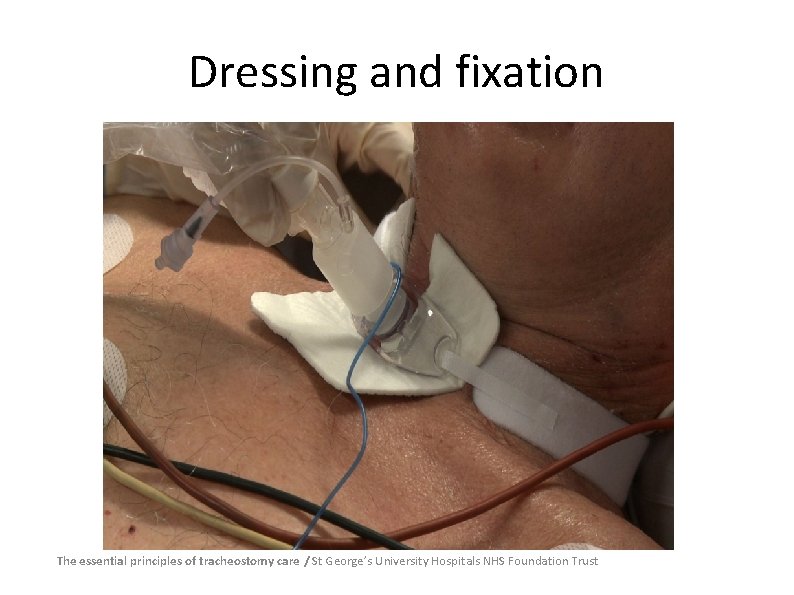
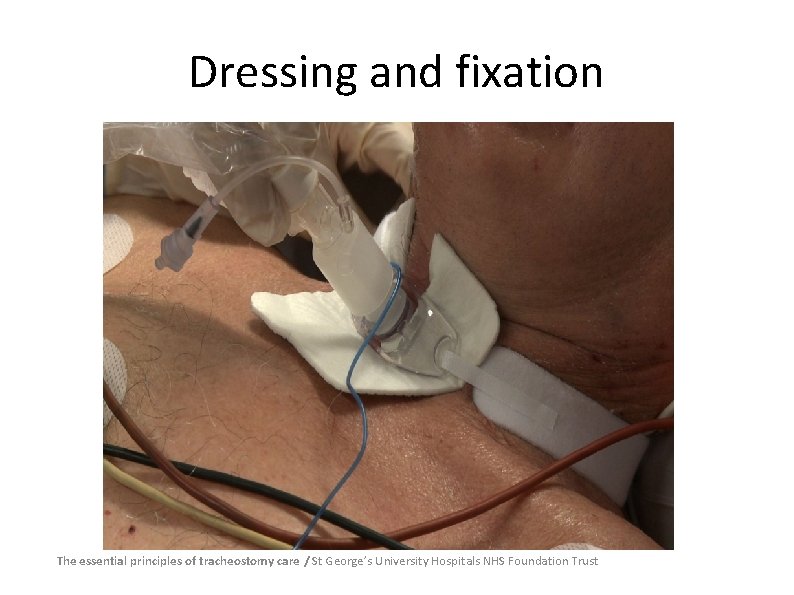
Dressing and fixation The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
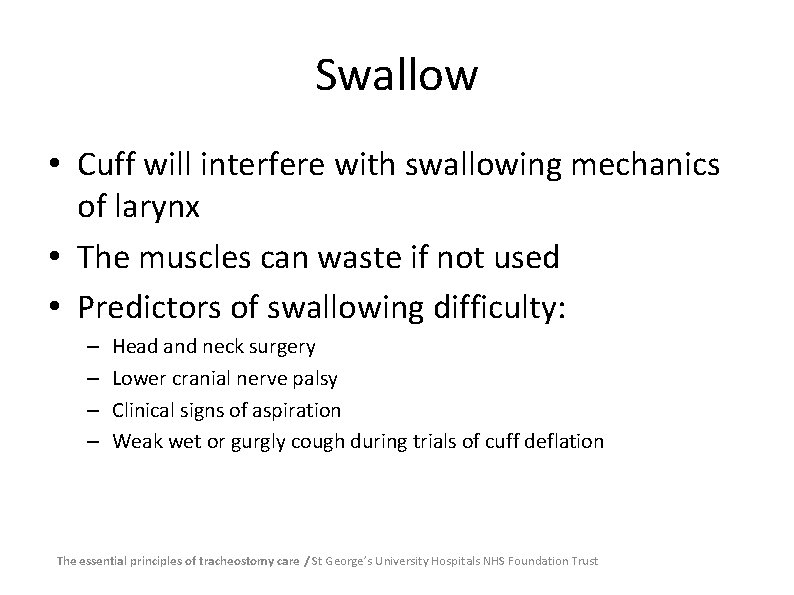
Swallow • Cuff will interfere with swallowing mechanics of larynx • The muscles can waste if not used • Predictors of swallowing difficulty: – – Head and neck surgery Lower cranial nerve palsy Clinical signs of aspiration Weak wet or gurgly cough during trials of cuff deflation The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
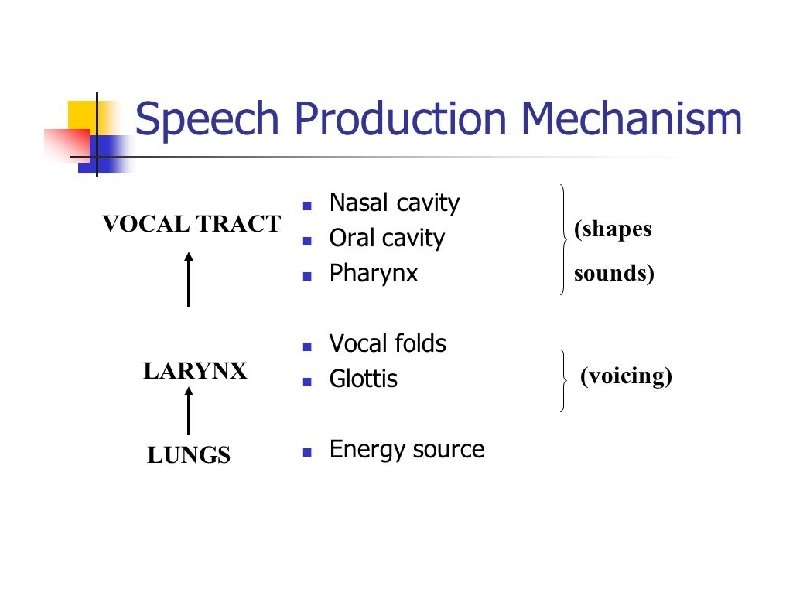
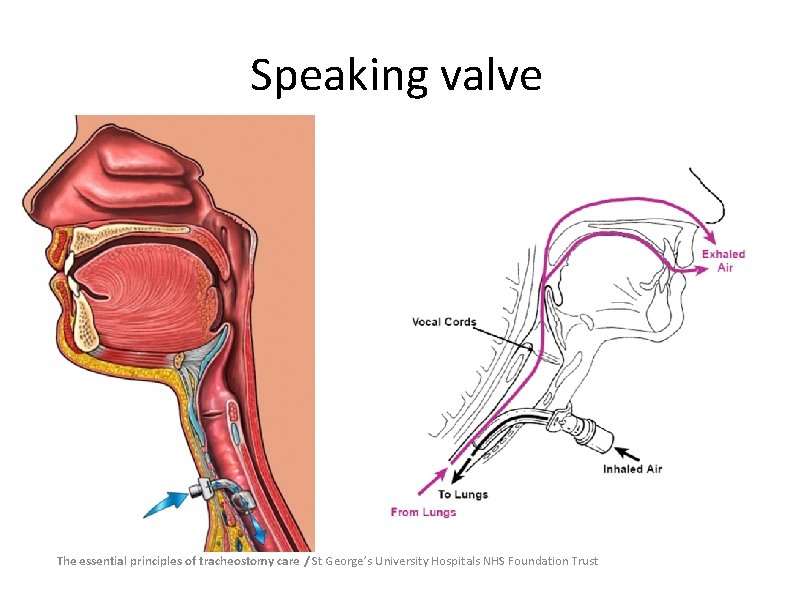
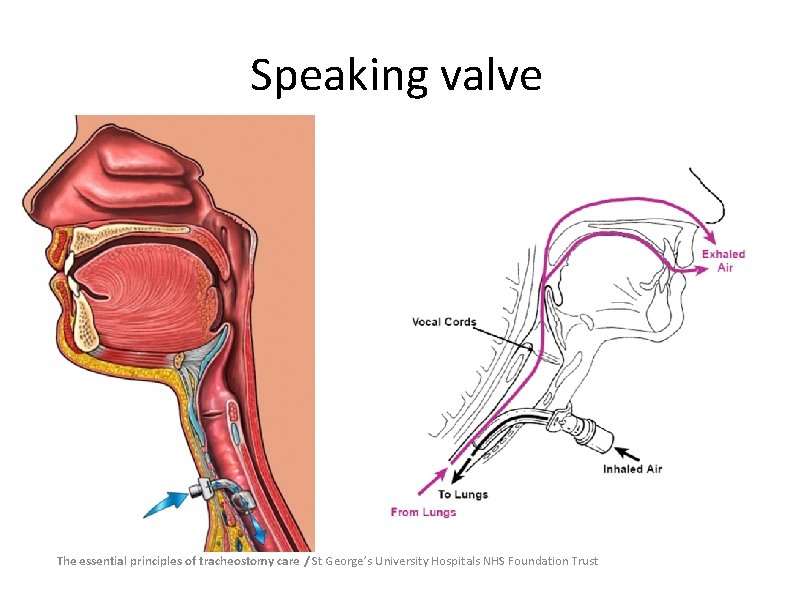
Speaking valve The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
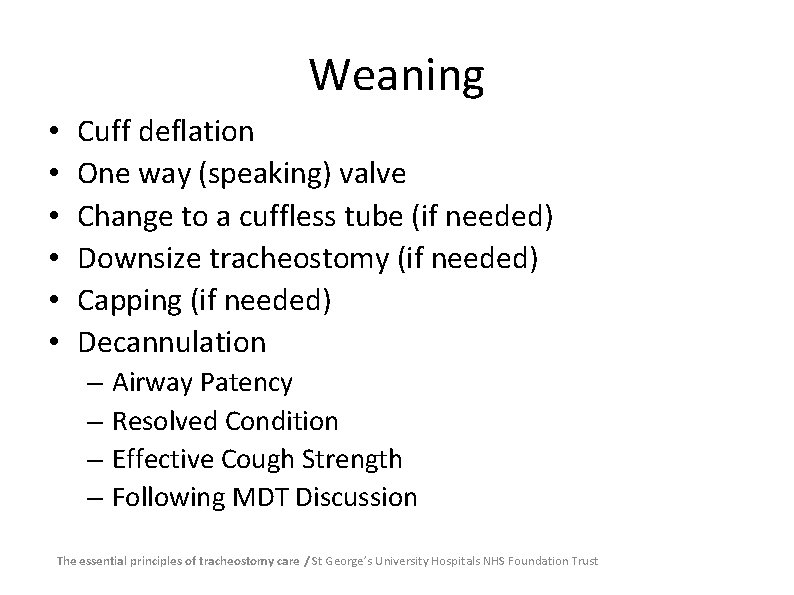
Weaning • • • Cuff deflation One way (speaking) valve Change to a cuffless tube (if needed) Downsize tracheostomy (if needed) Capping (if needed) Decannulation – Airway Patency – Resolved Condition – Effective Cough Strength – Following MDT Discussion The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust
Decannulation of tracheostomy tube Prior to removal patient should: • Be alert and orientated • Have a good cough reflex and managing secretions • Be breathing spontaneously with the cuff deflated • Have a normal respiratory rate, good Spo 2 saturations. Check blood gases • Require less than 40 % oxygen via trachy mask • Have anaesthetic review & decision to remove tube agreed with team
Decannulation of tracheostomy tube Ensure all emergency equipment is at hand: • Rebreathe bag, catheter mount & face mask • Ambu bag & mask • Working suction, yanker and suction catheters • Tracheal dilators, 2 spare tracheostomy tubes one the same size and one smaller (of the same type of trachy tube in situ) • 10 ml syringe, clean gloves, aprons and eye protection face mask and oxygen for use following decannulation
Decannulation of tracheostomy tube – (continued) • Ensure cuff is already deflated before removal of tracheostomy • Have emergency equipment attached and ready for use • Connect humidified facial oxygen mask for use after decannulation • Explain the procedure to the patient • Sit patient upright • Suction the mouth and down the tracheostomy tube
continued • Pre oxygenate the patient for 1 -2 minutes • Re check respiratory rate, colour and saturations • Remove tube • Place occlusive sterile dressing over stoma • Place oxygen mask on patient • Continue monitoring respiratory rate, saturations and patient colour for any changes.
Post Decannulation Observations The patient should be observed for signs of respiratory distress including: • Dyspnoea • Laboured or noisy respiration, stridor • Increased respiratory rate and heart rate • Excess use of accessory muscles • Diaphragmatic respiration • Agitation • Oxygen desaturation
https: //www. stgeorges. nhs. uk/gps-and-clinicians/clinicalresources/tracheostomy-guidelines/
Presentation title / St George’s University Hospitals NHS Foundation Trust
Documentation ICP Type and size of tracheostomy Tracheostomy procedure Patent/non patent upper airway Equipment check Care record inc. inner cannula, cuff and suctioning • Weaning record • • • The essential principles of tracheostomy care / St George’s University Hospitals NHS Foundation Trust

 Nightingale health
Nightingale health Patient 2 patient
Patient 2 patient Suction types
Suction types Tracheostomy complications
Tracheostomy complications Feeding cuff
Feeding cuff St george tracheostomy
St george tracheostomy Indications for tracheostomy
Indications for tracheostomy Tracheostomy care
Tracheostomy care Tracheostomy
Tracheostomy Tracheostomy stoma
Tracheostomy stoma Tracheostomy care
Tracheostomy care Trakeostoma
Trakeostoma Perawatan ett adalah
Perawatan ett adalah Tracheostomy downsizing protocol
Tracheostomy downsizing protocol Tracheostomy oxygen delivery
Tracheostomy oxygen delivery Tracheostomy
Tracheostomy Dope mnemonic emt
Dope mnemonic emt Tracheostomy stoma
Tracheostomy stoma Summary of tracheostomy care
Summary of tracheostomy care Sap patient management
Sap patient management Treatment of ocd
Treatment of ocd Chapter 20 patient collections and financial management
Chapter 20 patient collections and financial management Resource patient management system
Resource patient management system Care plan of cataract
Care plan of cataract Patient management problem
Patient management problem Patient blood management definition
Patient blood management definition Nursing diagnosis of meningitis slideshare
Nursing diagnosis of meningitis slideshare Hospital web application
Hospital web application Safety incident management system
Safety incident management system Bivalve cast
Bivalve cast Myeplg
Myeplg Scientific management
Scientific management Top management middle management first line management
Top management middle management first line management Top management and middle management
Top management and middle management Maya angelou pronunciation
Maya angelou pronunciation Turing tumble simulator
Turing tumble simulator Streamsc
Streamsc