April 21 2017 Chicago Airway Management Workshop Advanced


- Slides: 49
April 21, 2017 Chicago Airway Management Workshop – Advanced Catherine Hart, MD Updated 2/08/2017
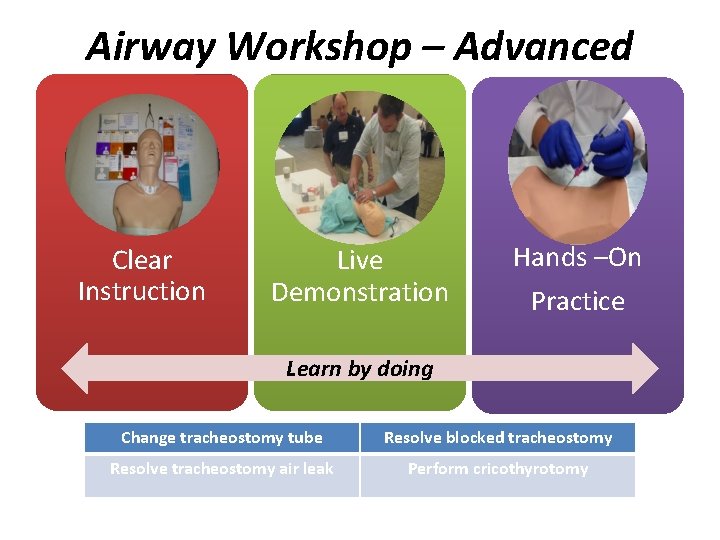
Airway Workshop – Advanced Clear Instruction Live Demonstration Hands –On Practice Learn by doing Change tracheostomy tube Resolve blocked tracheostomy Resolve tracheostomy air leak Perform cricothyrotomy
Introduction There are multiple methods and techniques available to successfully complete all the topics presented in this workshop. Some are based on patient request, available equipment or supervising physician’s preference. The goal of this workshop is to correctly demonstrate the most common methods and give participants time for hands on training.
Learning Objectives Learning objectives • Discuss and practice tracheostomy care techniques. • Discuss and practice management for tracheostomy airway obstruction. • Discuss and practice management for tracheostomy airway leaks. • Discuss and practice manament for tracheostomy bleeding. • Discuss indications for and practice cricothyrotomy.
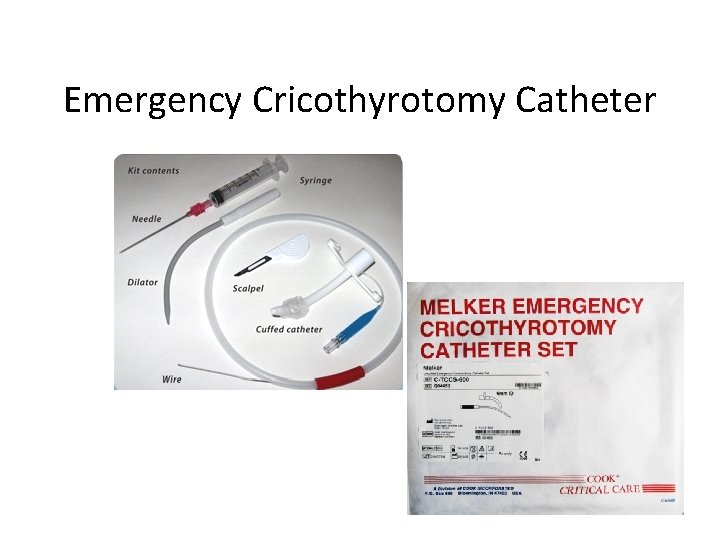
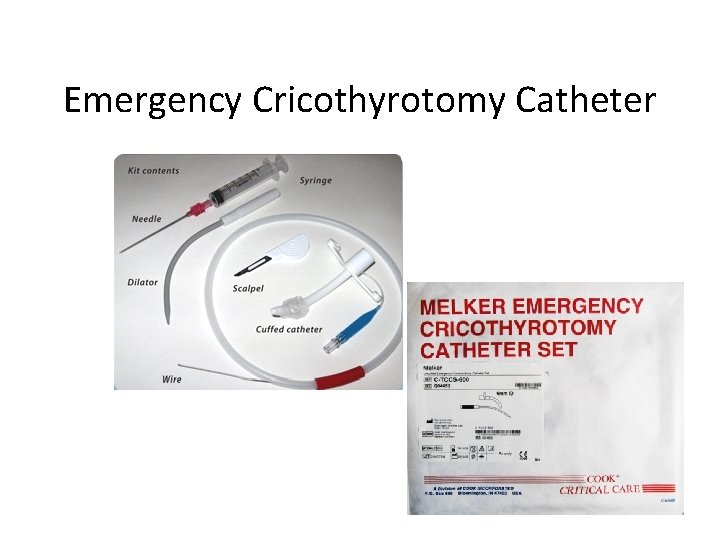
Emergency Cricothyrotomy Catheter
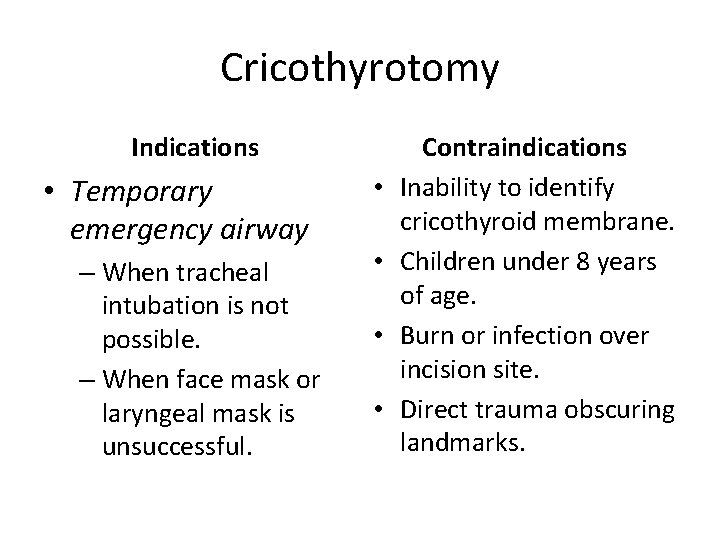
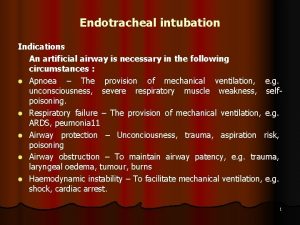
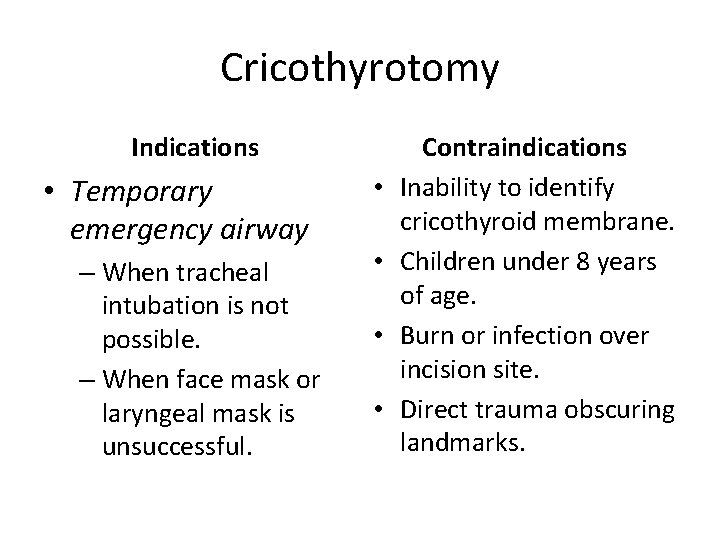
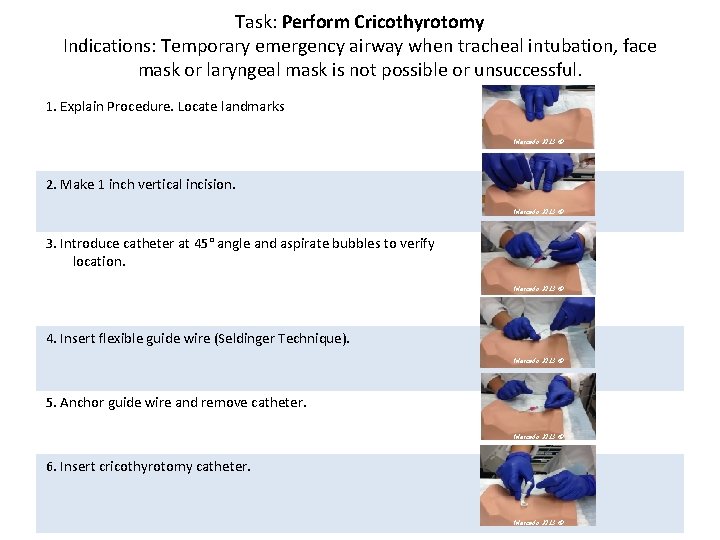
Cricothyrotomy Indications • Temporary emergency airway – When tracheal intubation is not possible. – When face mask or laryngeal mask is unsuccessful. • • Contraindications Inability to identify cricothyroid membrane. Children under 8 years of age. Burn or infection over incision site. Direct trauma obscuring landmarks.
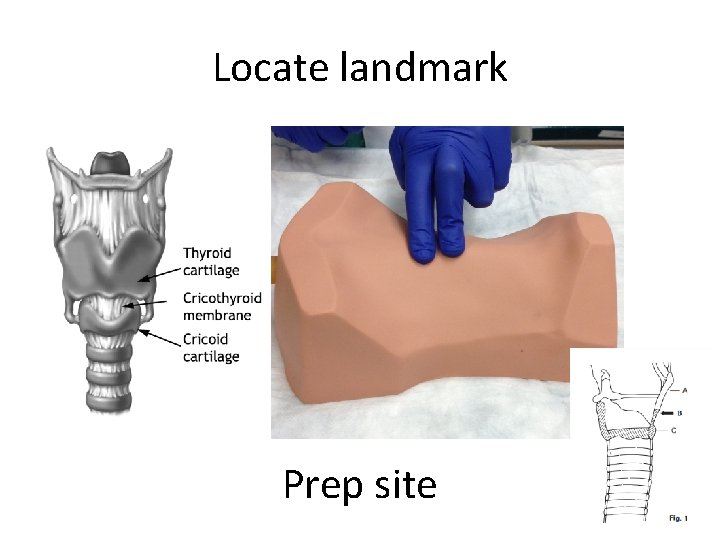
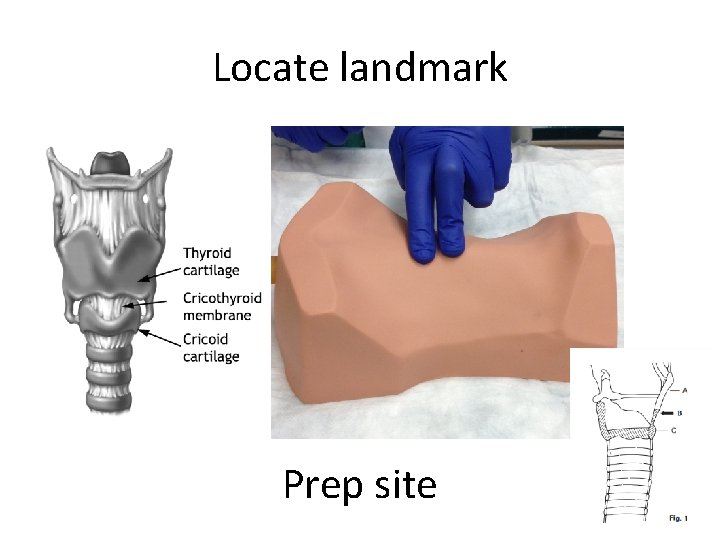
Locate landmark Prep site
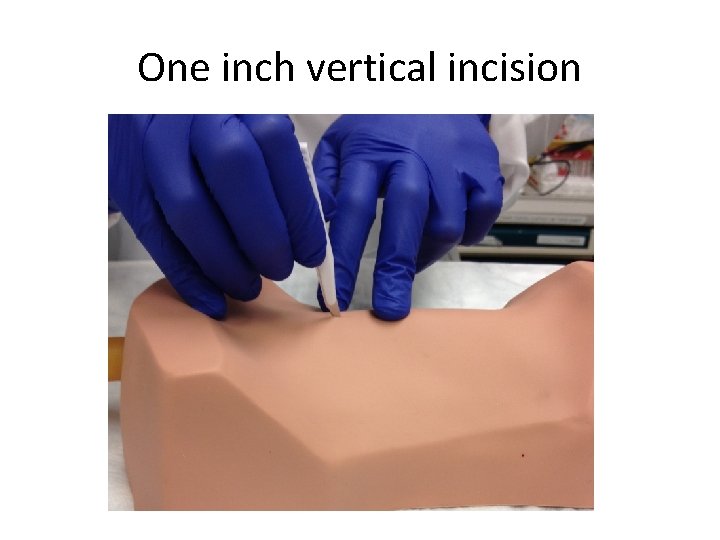
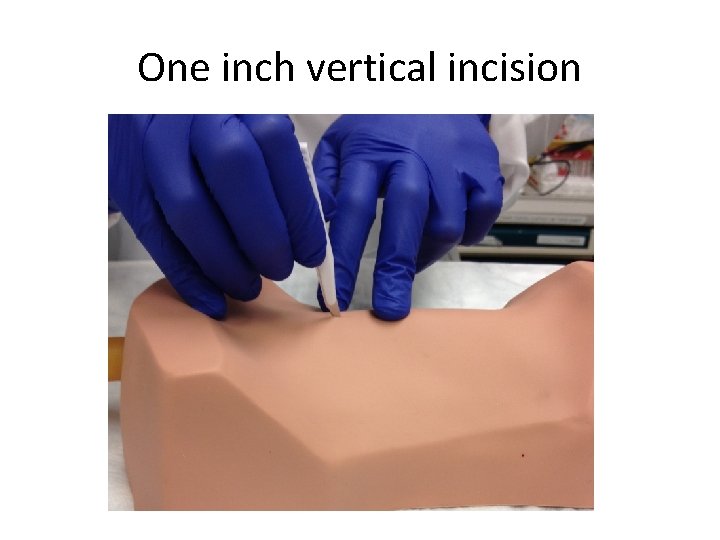
One inch vertical incision
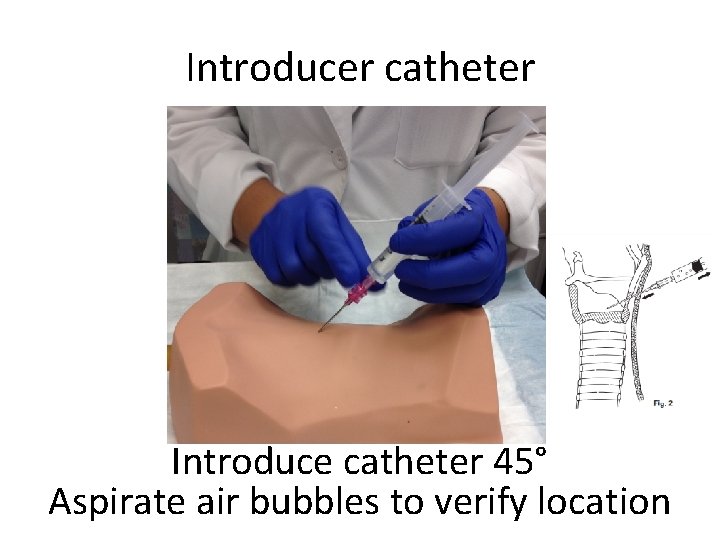
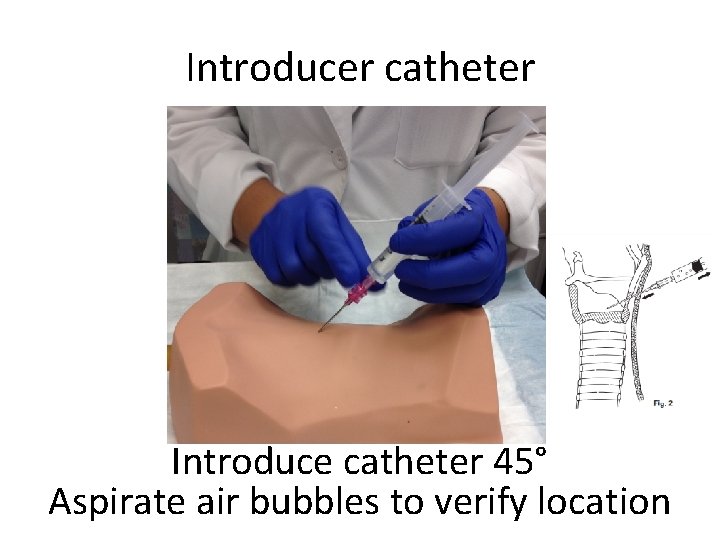
Introducer catheter Introduce catheter 45° Aspirate air bubbles to verify location
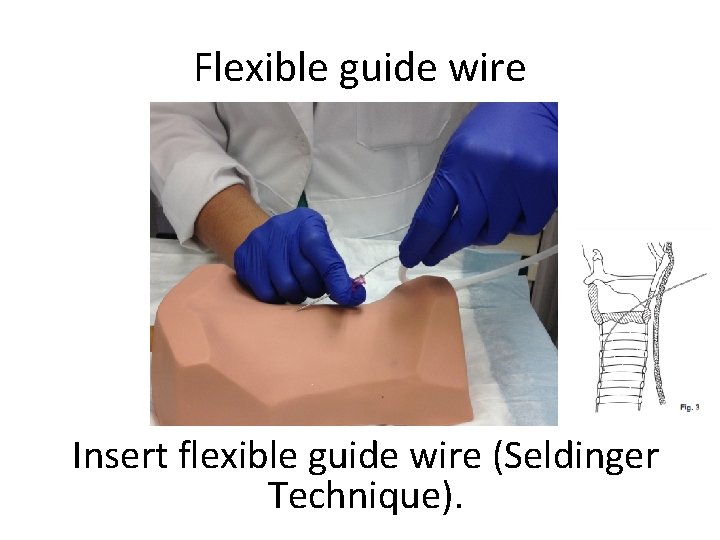
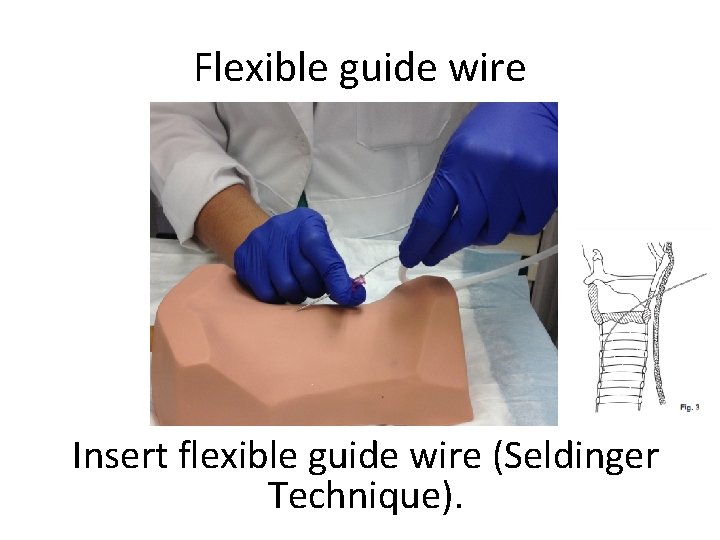
Flexible guide wire Insert flexible guide wire (Seldinger Technique).
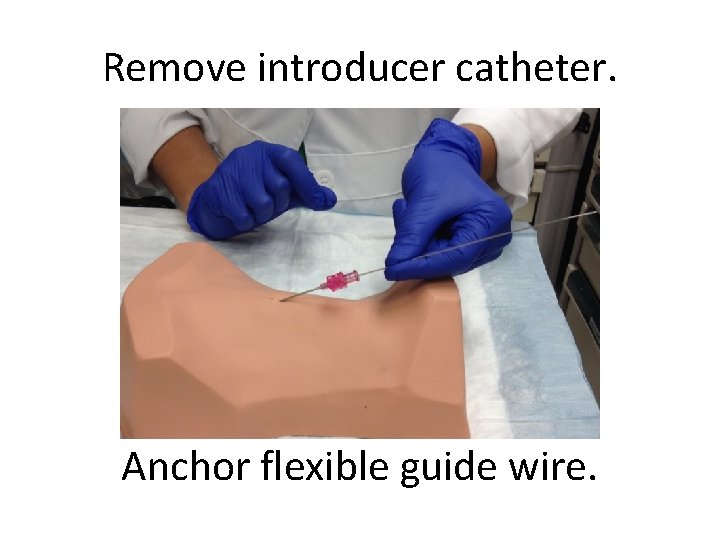
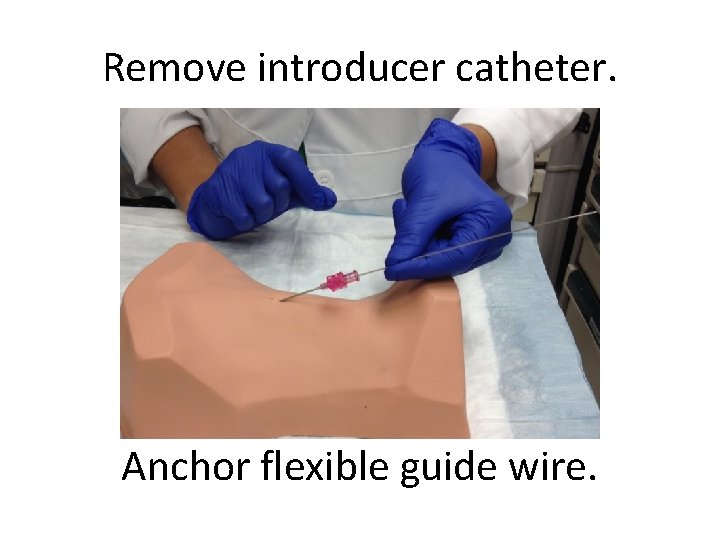
Remove introducer catheter. Anchor flexible guide wire.
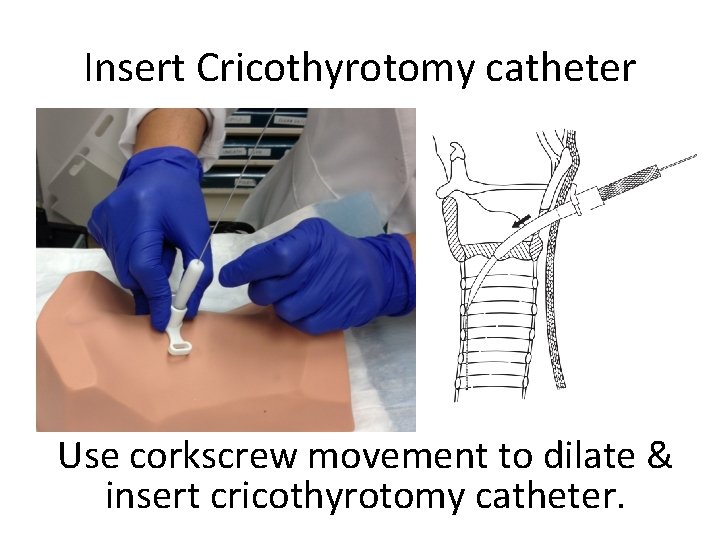
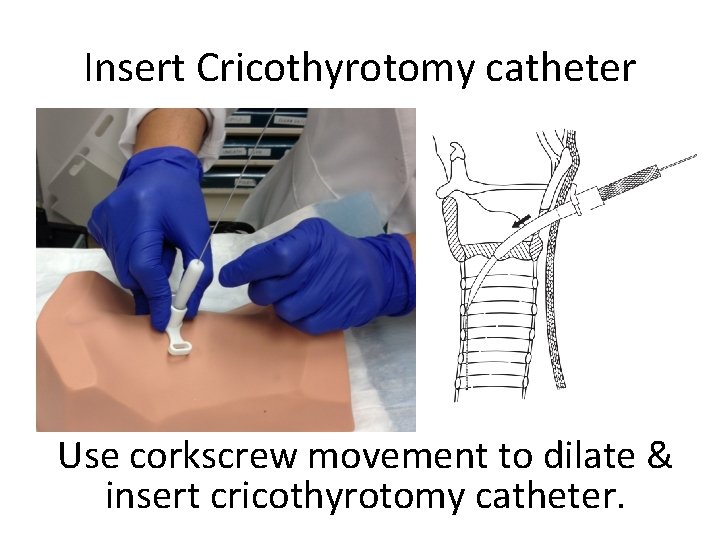
Insert Cricothyrotomy catheter Use corkscrew movement to dilate & insert cricothyrotomy catheter.
Technical tip Always visualize proximal end of the wire during airway insertion to prevent inadvertent loss into trachea.
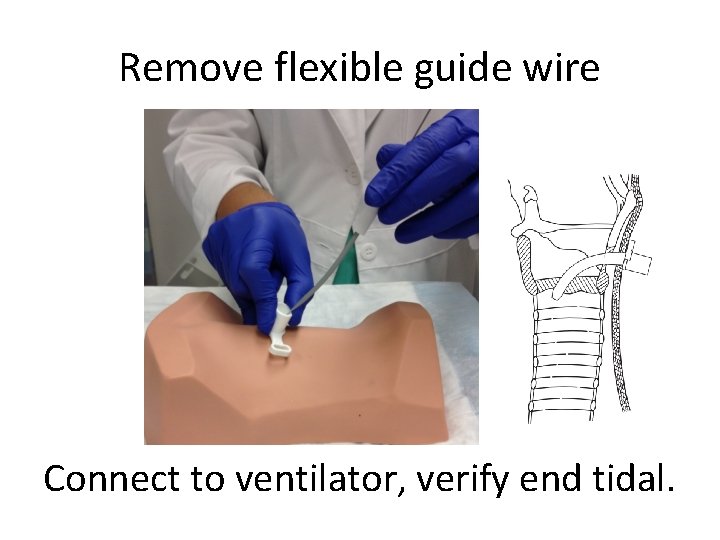
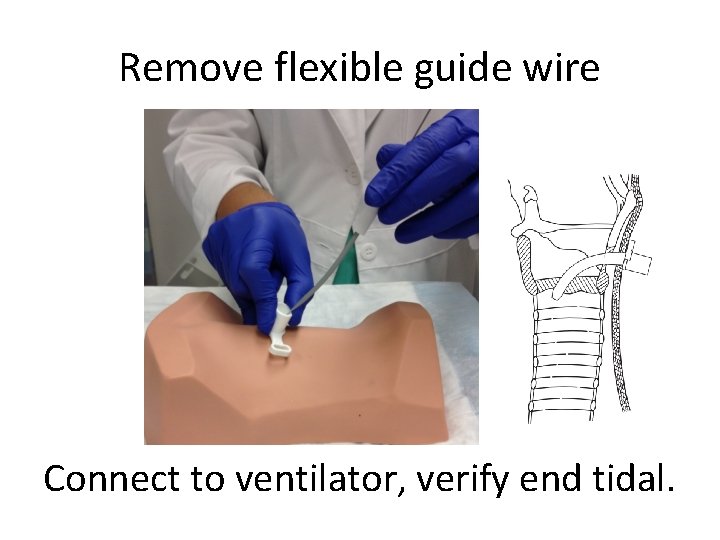
Remove flexible guide wire Connect to ventilator, verify end tidal.
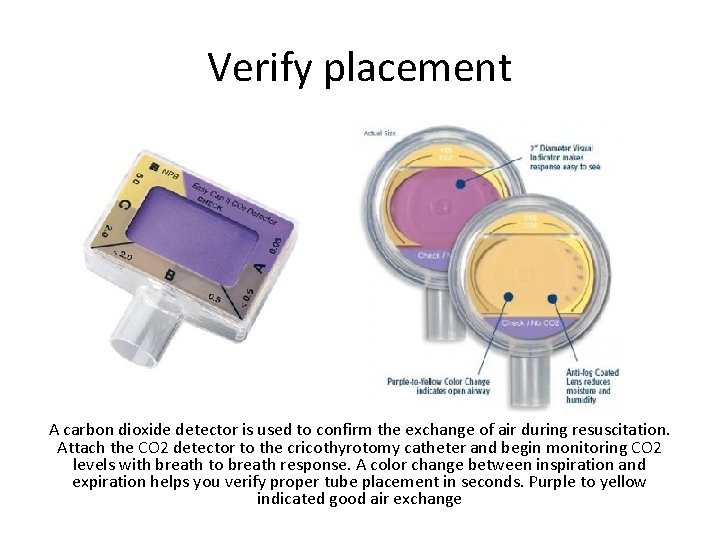
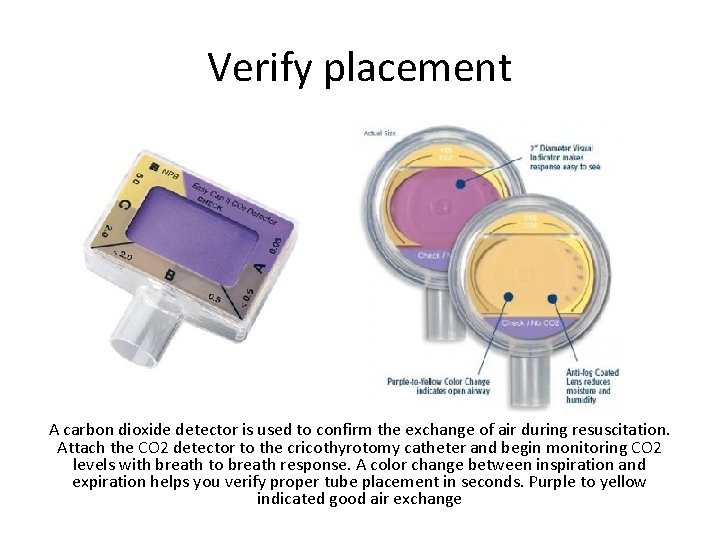
Verify placement A carbon dioxide detector is used to confirm the exchange of air during resuscitation. Attach the CO 2 detector to the cricothyrotomy catheter and begin monitoring CO 2 levels with breath to breath response. A color change between inspiration and expiration helps you verify proper tube placement in seconds. Purple to yellow indicated good air exchange
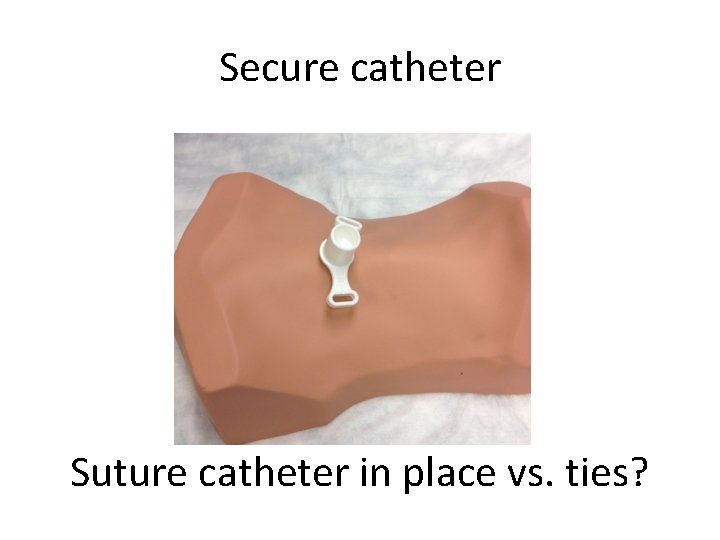
Secure catheter Suture catheter in place vs. ties?
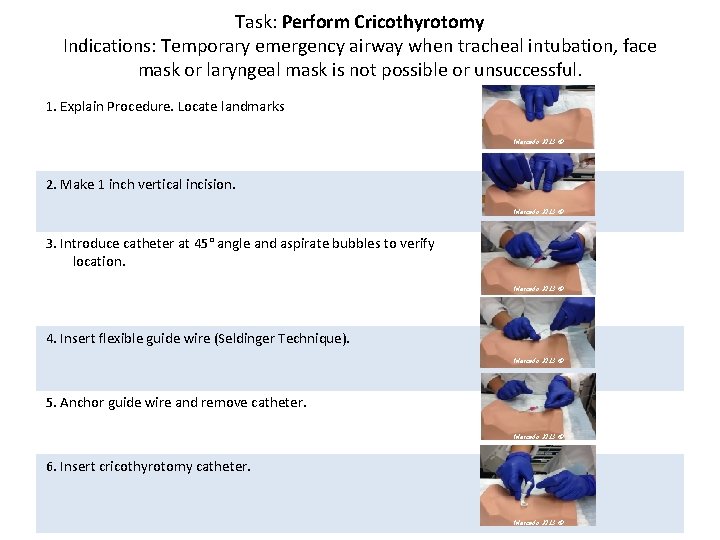
Task: Perform Cricothyrotomy Indications: Temporary emergency airway when tracheal intubation, face mask or laryngeal mask is not possible or unsuccessful. 1. Explain Procedure. Locate landmarks Mercado 2013 © 2. Make 1 inch vertical incision. Mercado 2013 © 3. Introduce catheter at 45° angle and aspirate bubbles to verify location. Mercado 2013 © 4. Insert flexible guide wire (Seldinger Technique). Mercado 2013 © 5. Anchor guide wire and remove catheter. Mercado 2013 © 6. Insert cricothyrotomy catheter. Mercado 2013 ©
Tracheostomy Care
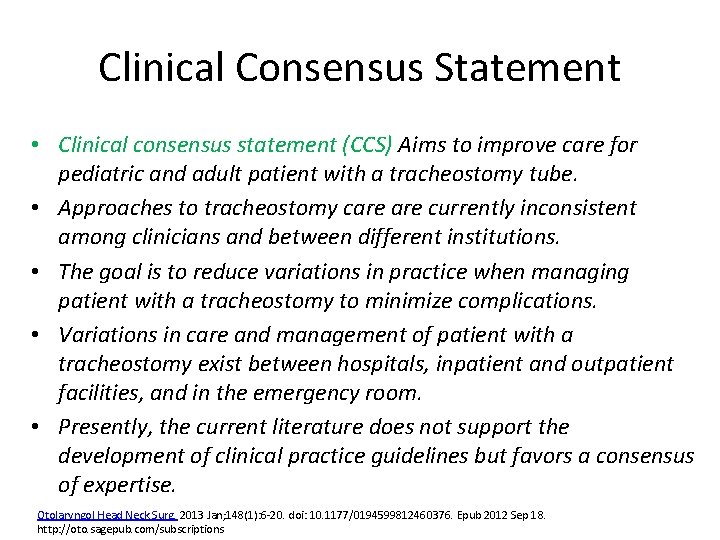
Clinical Consensus Statement • Clinical consensus statement (CCS) Aims to improve care for pediatric and adult patient with a tracheostomy tube. • Approaches to tracheostomy care currently inconsistent among clinicians and between different institutions. • The goal is to reduce variations in practice when managing patient with a tracheostomy to minimize complications. • Variations in care and management of patient with a tracheostomy exist between hospitals, inpatient and outpatient facilities, and in the emergency room. • Presently, the current literature does not support the development of clinical practice guidelines but favors a consensus of expertise. Otolaryngol Head Neck Surg. 2013 Jan; 148(1): 6 -20. doi: 10. 1177/0194599812460376. Epub 2012 Sep 18. http: //oto. sagepub. com/subscriptions

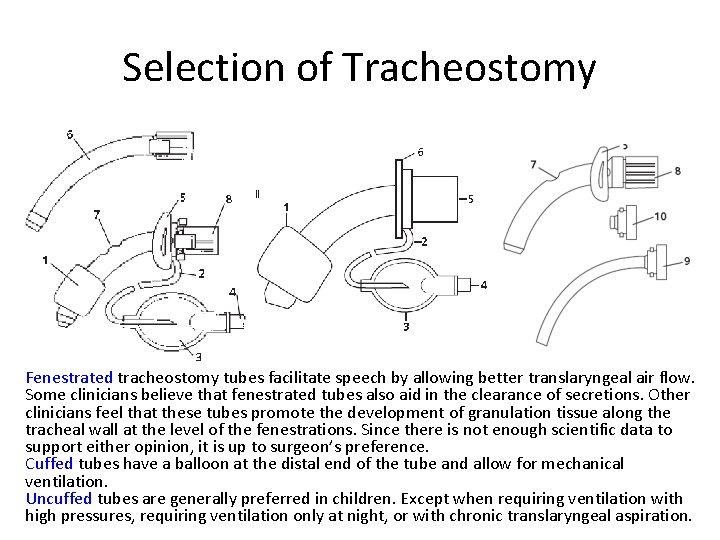
Selection of Tracheostomy tubes come in different sizes and different materials. Two types of tracheostomy tubes commonly used are Polyvinyl chloride tracheostomy tubes (Shiley) and Silicone (Bivona). Shiley tubes are slightly flexible and Bivona are the most flexible. Both Shiley and Bivona tubes come standard with a universal adapter for ventilation. In double cannula tubes, the inner cannula is inserted and locked in place after the obturator is removed. The inner cannula can be removed briefly for cleaning. The outer tube is secured to the patient. Single cannula tubes are often used in children and do not have an inner cannula.
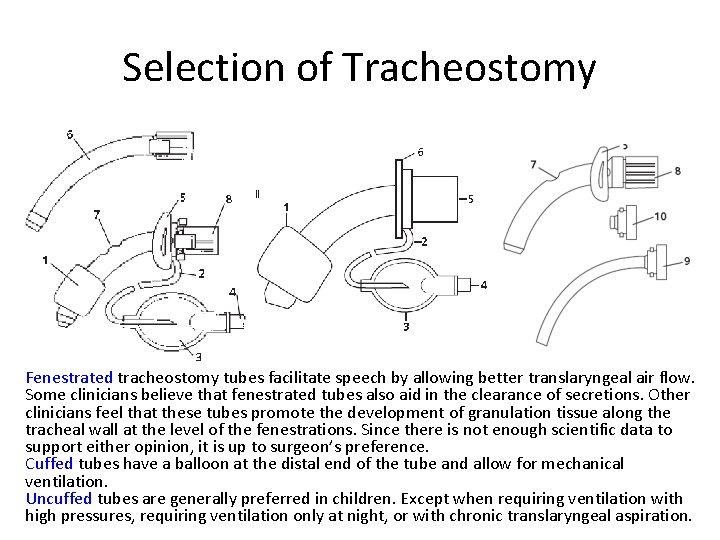
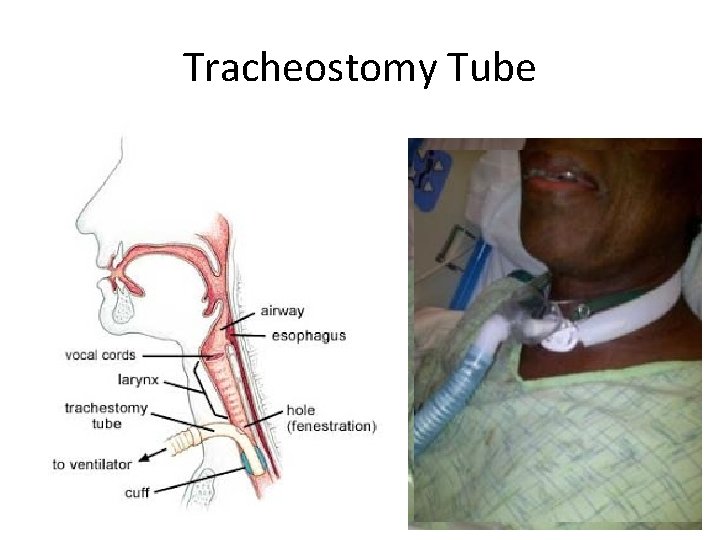
Selection of Tracheostomy Fenestrated tracheostomy tubes facilitate speech by allowing better translaryngeal air flow. Some clinicians believe that fenestrated tubes also aid in the clearance of secretions. Other clinicians feel that these tubes promote the development of granulation tissue along the tracheal wall at the level of the fenestrations. Since there is not enough scientific data to support either opinion, it is up to surgeon’s preference. Cuffed tubes have a balloon at the distal end of the tube and allow for mechanical ventilation. Uncuffed tubes are generally preferred in children. Except when requiring ventilation with high pressures, requiring ventilation only at night, or with chronic translaryngeal aspiration.
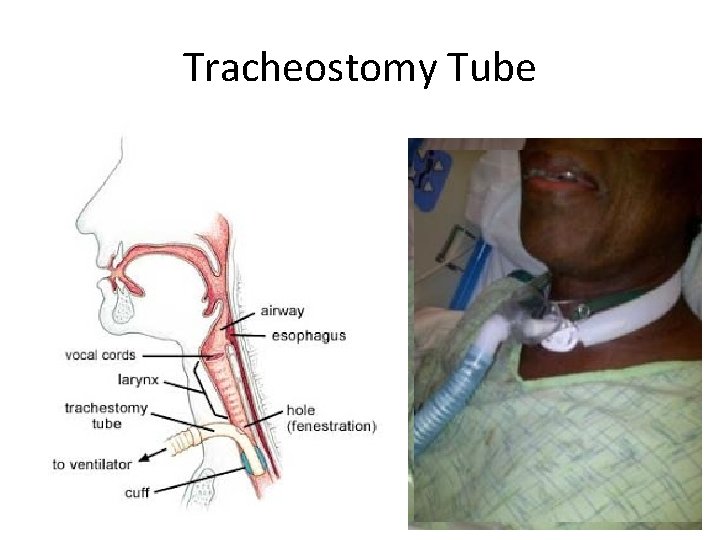
Tracheostomy Tube Mercado 2011 ©
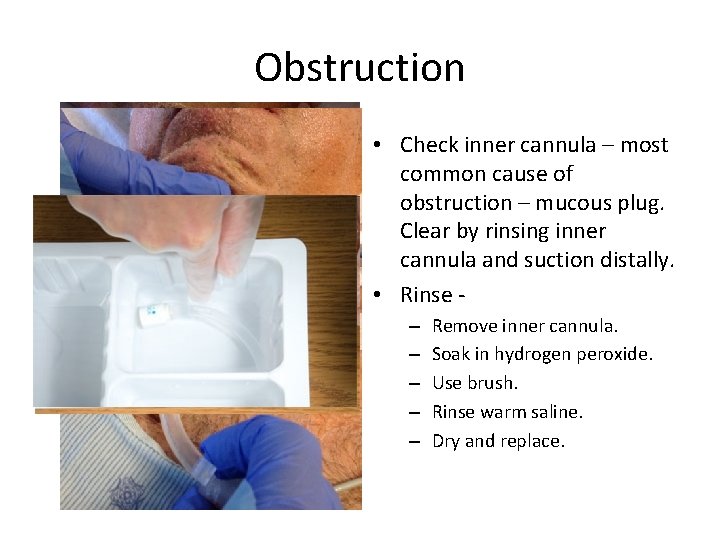
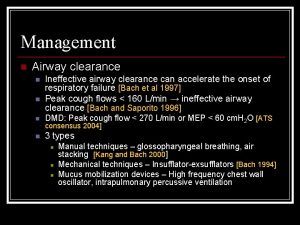
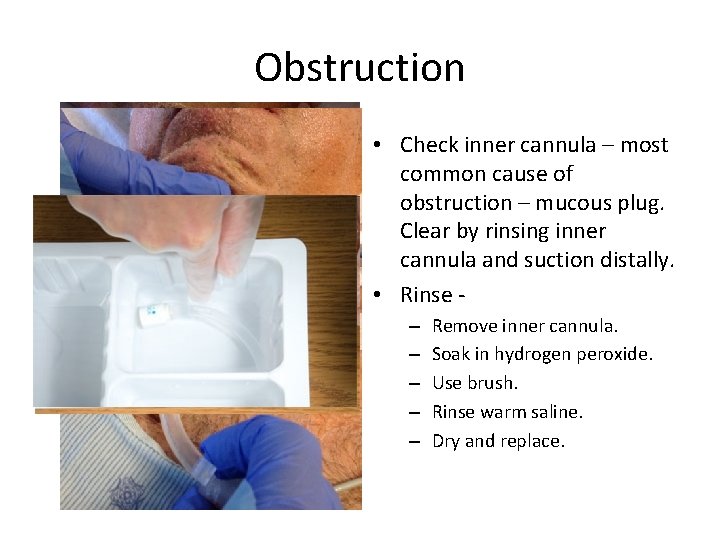
Obstruction • Check inner cannula – most common cause of obstruction – mucous plug. Clear by rinsing inner cannula and suction distally. • Rinse – – – Remove inner cannula. Soak in hydrogen peroxide. Use brush. Rinse warm saline. Dry and replace.
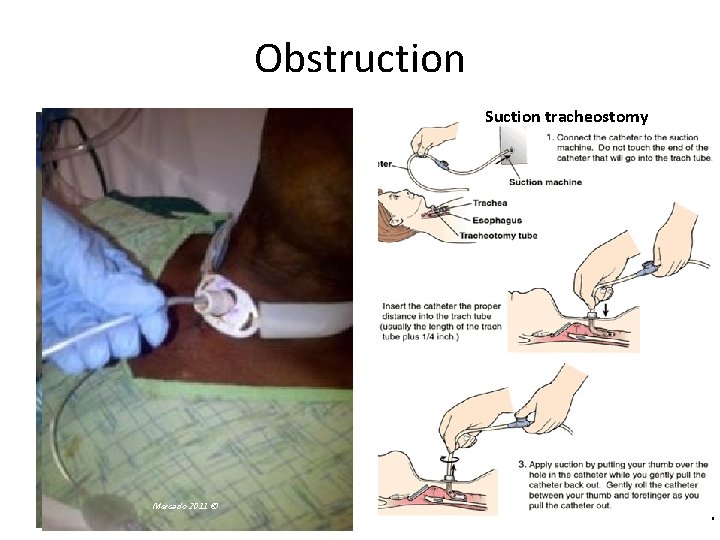
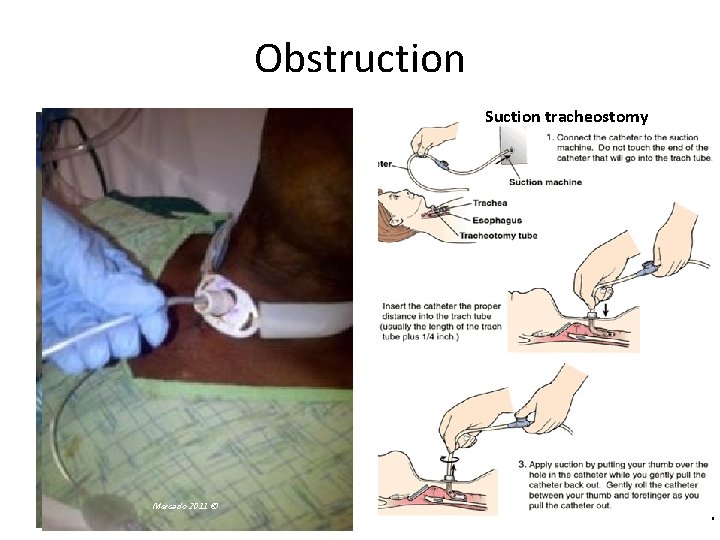
Obstruction Suction tracheostomy Mercado © Mercado 2011 ©
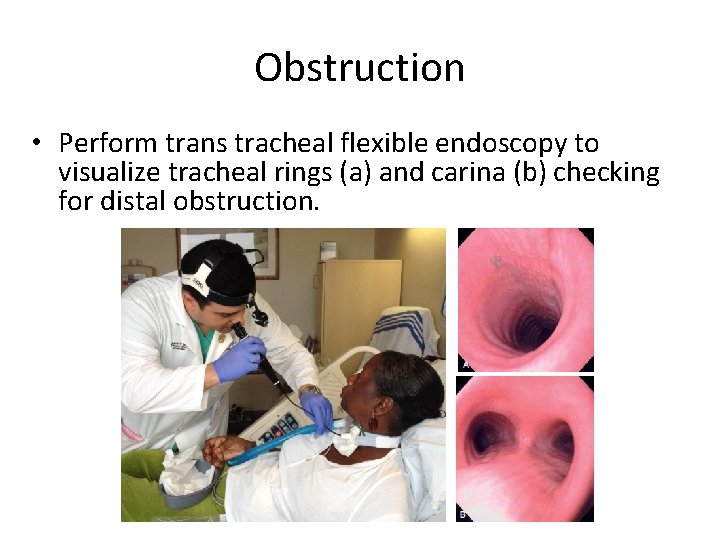
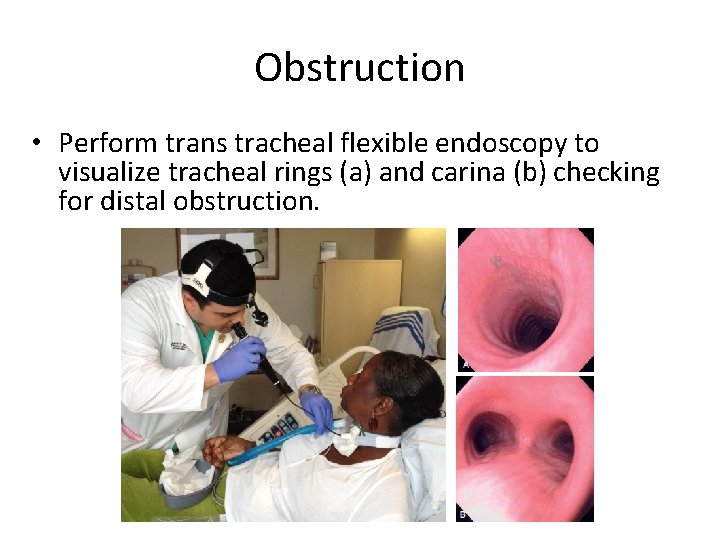
Obstruction • Perform trans tracheal flexible endoscopy to visualize tracheal rings (a) and carina (b) checking for distal obstruction. Mercado 2011 ©
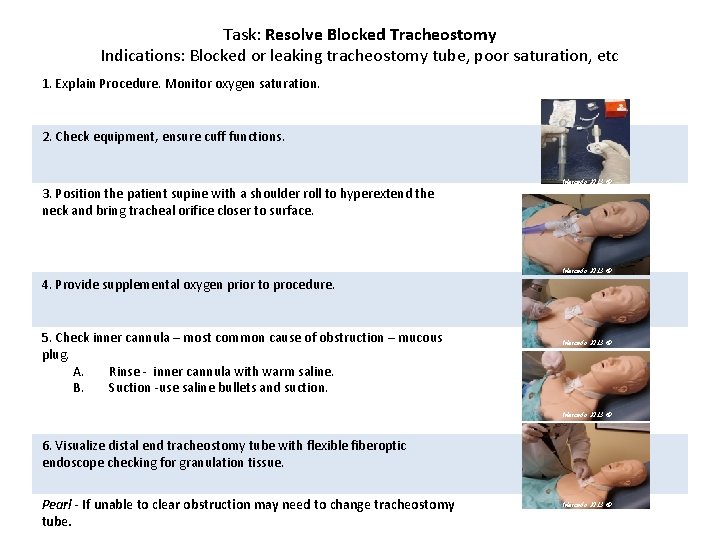
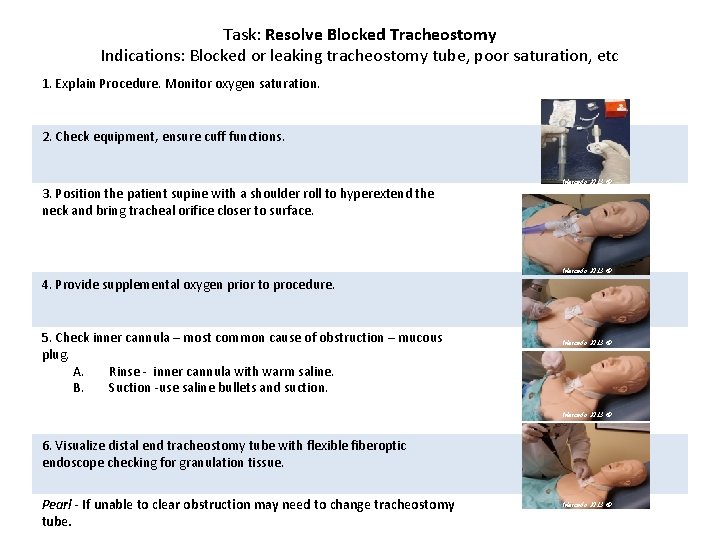
Task: Resolve Blocked Tracheostomy Indications: Blocked or leaking tracheostomy tube, poor saturation, etc 1. Explain Procedure. Monitor oxygen saturation. 2. Check equipment, ensure cuff functions. 3. Position the patient supine with a shoulder roll to hyperextend the neck and bring tracheal orifice closer to surface. Mercado 2013 © 4. Provide supplemental oxygen prior to procedure. 5. Check inner cannula – most common cause of obstruction – mucous plug. A. Rinse - inner cannula with warm saline. B. Suction -use saline bullets and suction. Mercado 2013 © 6. Visualize distal end tracheostomy tube with flexible fiberoptic endoscope checking for granulation tissue. Pearl - If unable to clear obstruction may need to change tracheostomy tube. Mercado 2013 ©
Tracheostomy Change Indications: for tracheostomy change include minimizing risk of postoperative infection and granulation tissue formation, verifying formation of a stable tract for ancillary support staff, and downsizing the tracheostomy tube if the patient is clinically improving. Contraindications: Changing a tracheostomy tube too soon after operation (generally < 5 d) before tract has healed adequately, which increases the likelihood of entry into a false passage, Inadequate lighting, exposure, and equipment. Performer inexperience and unavailability of staff versed in airway management. Extremely high ventilator settings, which increases the risk of decannulation. Patient noncooperation without ancillary support
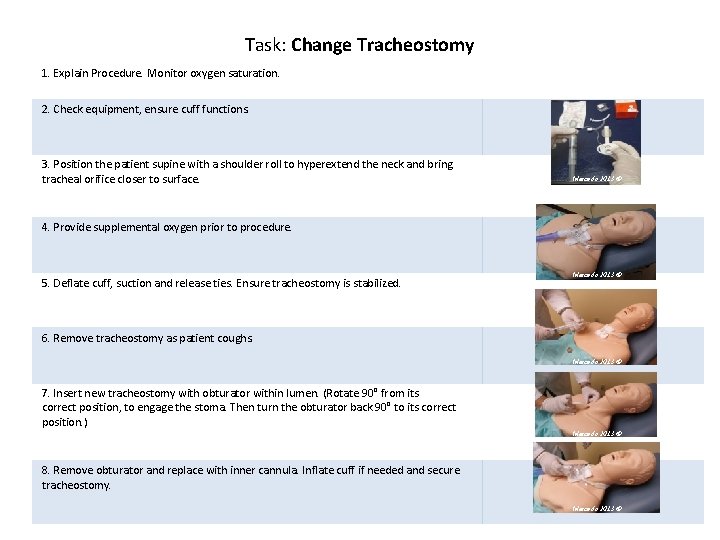
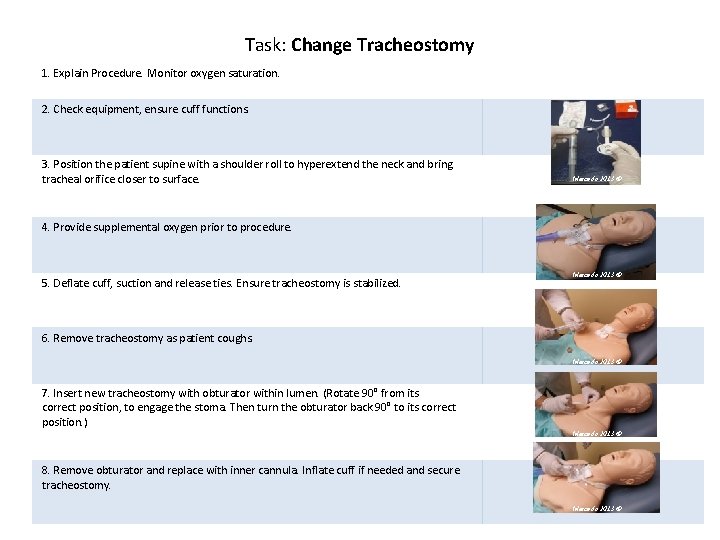
Task: Change Tracheostomy 1. Explain Procedure. Monitor oxygen saturation. 2. Check equipment, ensure cuff functions. 3. Position the patient supine with a shoulder roll to hyperextend the neck and bring tracheal orifice closer to surface. Mercado 2013 © 4. Provide supplemental oxygen prior to procedure. 5. Deflate cuff, suction and release ties. Ensure tracheostomy is stabilized. Mercado 2013 © 6. Remove tracheostomy as patient coughs. Mercado 2013 © 7. Insert new tracheostomy with obturator within lumen. (Rotate 90° from its correct position, to engage the stoma. Then turn the obturator back 90° to its correct position. ) Mercado 2013 © 8. Remove obturator and replace with inner cannula. Inflate cuff if needed and secure tracheostomy. Mercado 2013 ©
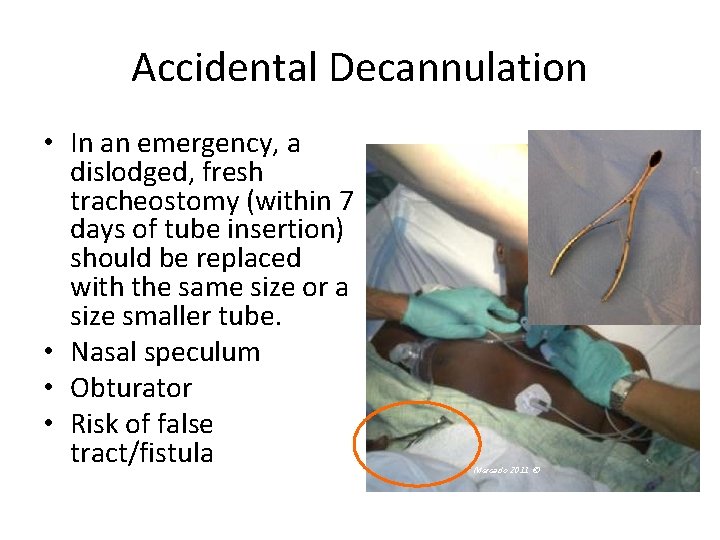
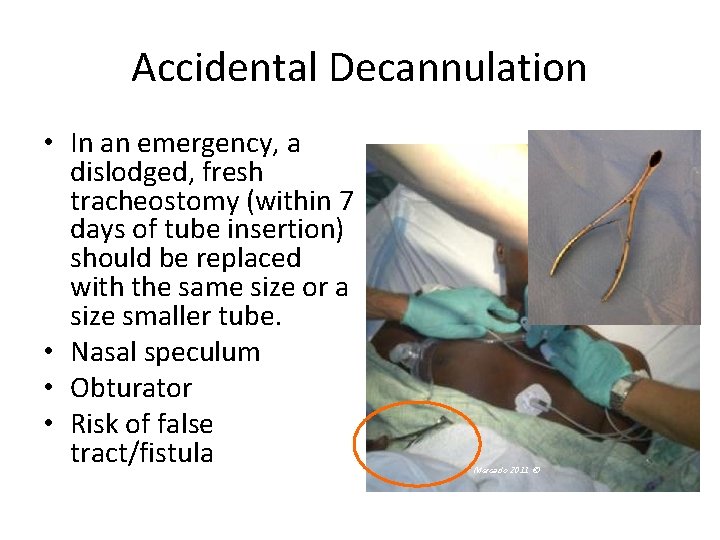
Accidental Decannulation • In an emergency, a dislodged, fresh tracheostomy (within 7 days of tube insertion) should be replaced with the same size or a size smaller tube. • Nasal speculum • Obturator • Risk of false tract/fistula Mercado 2011 ©
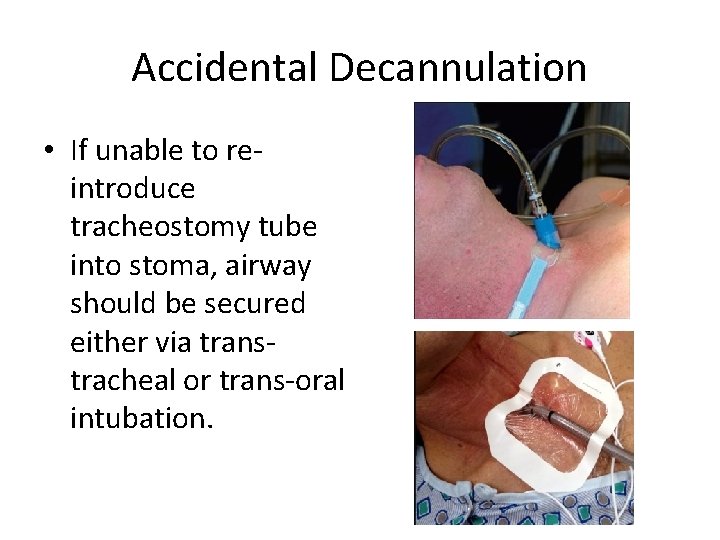
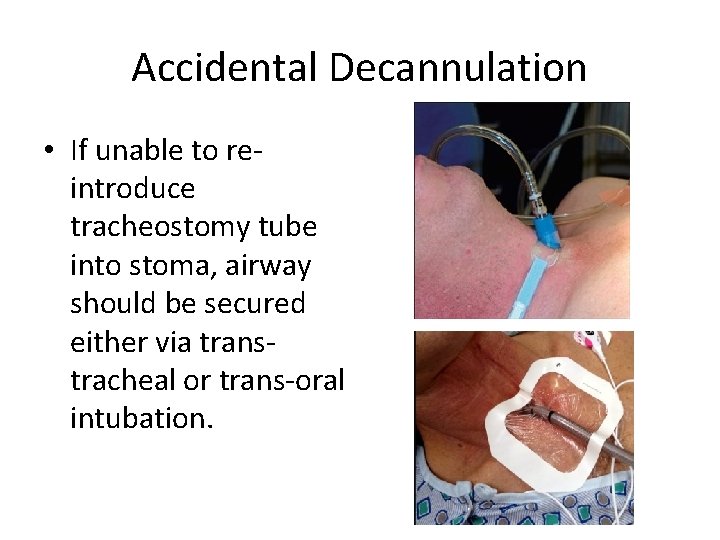
Accidental Decannulation • If unable to reintroduce tracheostomy tube into stoma, airway should be secured either via transtracheal or trans-oral intubation.
Complications Although tracheostomy tube changes are routinely performed, the procedure is not without complications. Minimize complications by understanding and practicing procedure as well as anticipating potential problems. In addition to oxygen, pulse oximeter and suction, have basic emergency equipment at bedside, such as a manual ventilator bag, 2 extra tracheostomy tubes (same size as the trach and one smaller), and an obturator The consequences of tracheostomy tube displacement can be dire and can include loss of adequate airway and death. Occasionally, displacement occurs at the time of the first tube change, resulting from creation of a false tract in the pretracheal or peristomal region. This may present insidiously with respiratory failure and subcutaneous emphysema. Confirmation of placement following the procedure with passage of a flexible suction catheter and/or direct visualization with flexible endoscopy will reduce incidence. Resistance met with this maneuver may represent improper placement.
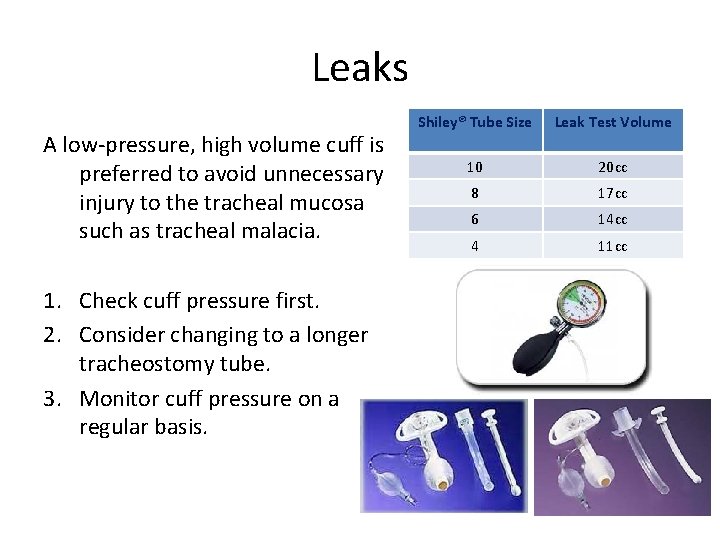
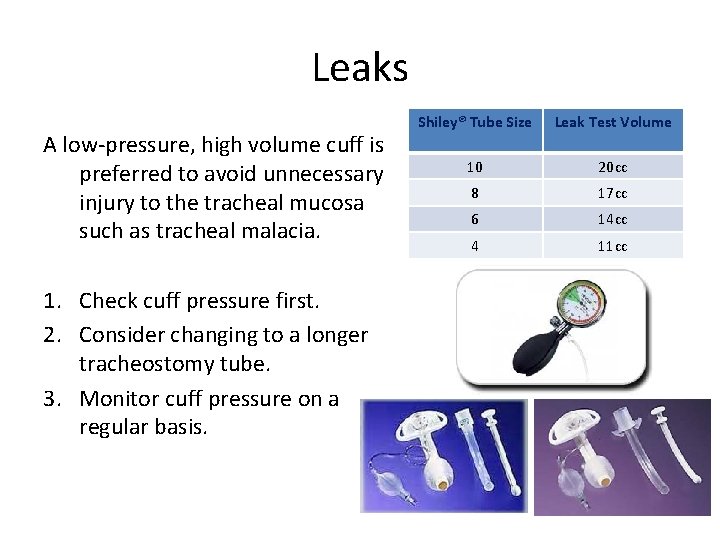
Leaks A low-pressure, high volume cuff is preferred to avoid unnecessary injury to the tracheal mucosa such as tracheal malacia. 1. Check cuff pressure first. 2. Consider changing to a longer tracheostomy tube. 3. Monitor cuff pressure on a regular basis. Shiley® Tube Size Leak Test Volume 10 20 cc 8 17 cc 6 14 cc 4 11 cc
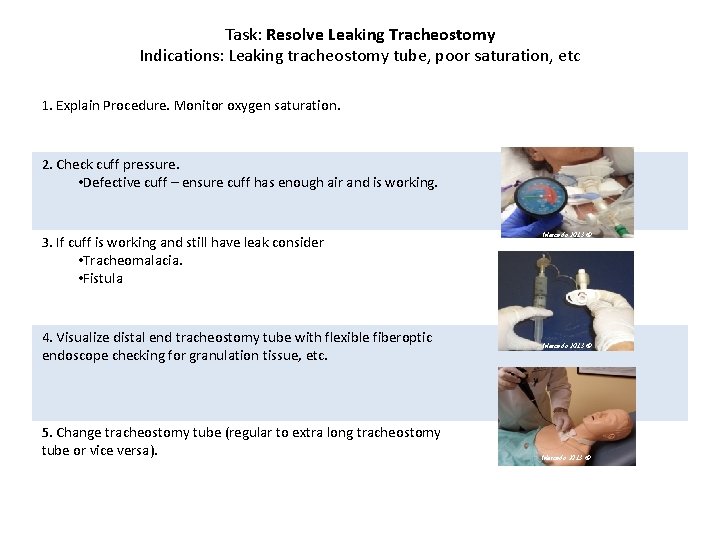
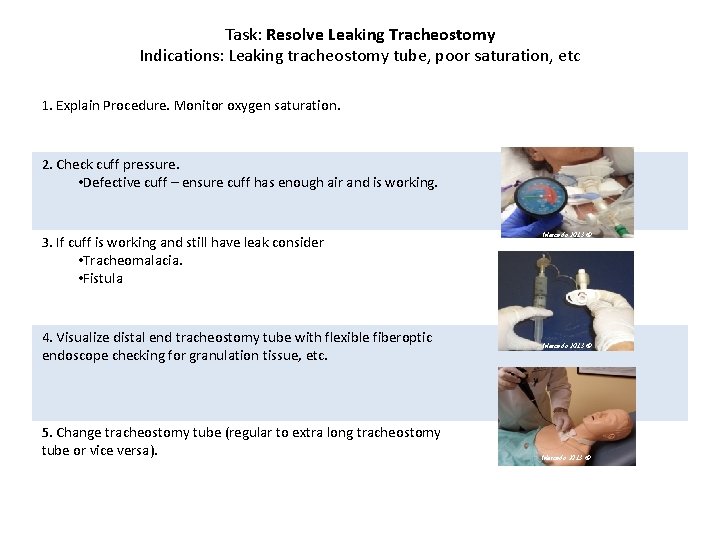
Task: Resolve Leaking Tracheostomy Indications: Leaking tracheostomy tube, poor saturation, etc 1. Explain Procedure. Monitor oxygen saturation. 2. Check cuff pressure. • Defective cuff – ensure cuff has enough air and is working. 3. If cuff is working and still have leak consider • Tracheomalacia. • Fistula 4. Visualize distal end tracheostomy tube with flexible fiberoptic endoscope checking for granulation tissue, etc. 5. Change tracheostomy tube (regular to extra long tracheostomy tube or vice versa). Mercado 2013 ©
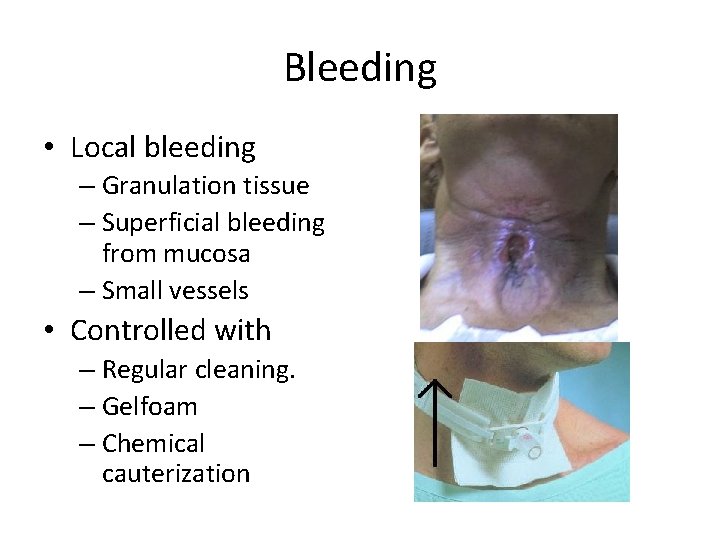
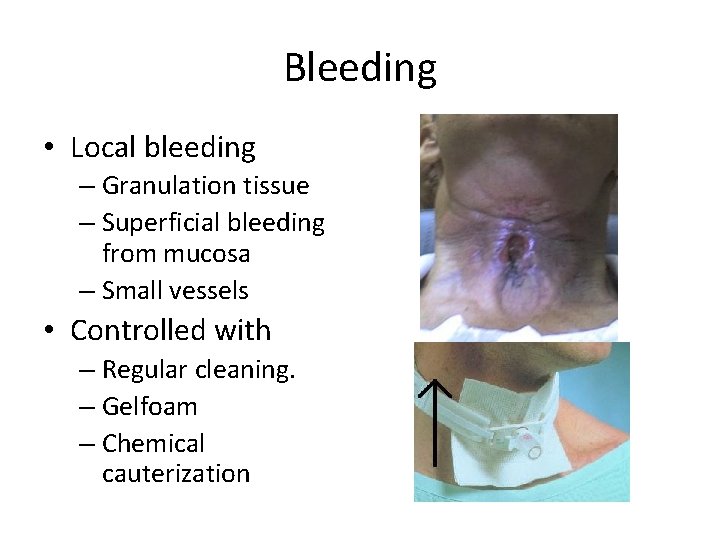
Bleeding • Local bleeding – Granulation tissue – Superficial bleeding from mucosa – Small vessels • Controlled with – Regular cleaning. – Gelfoam – Chemical cauterization
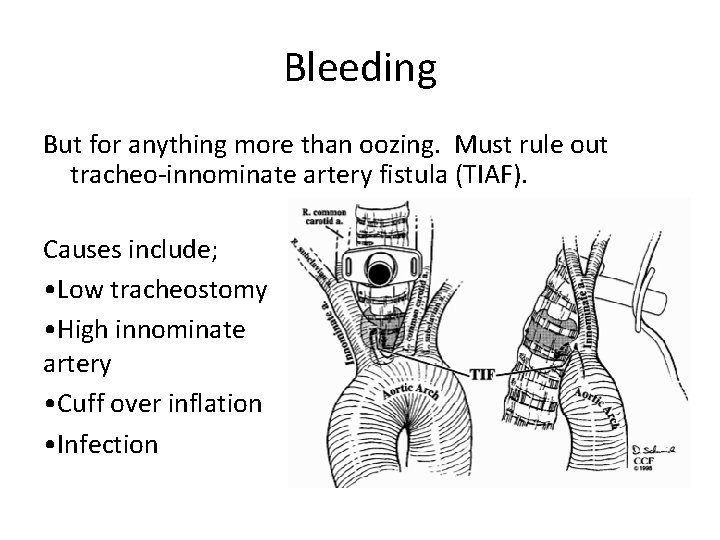
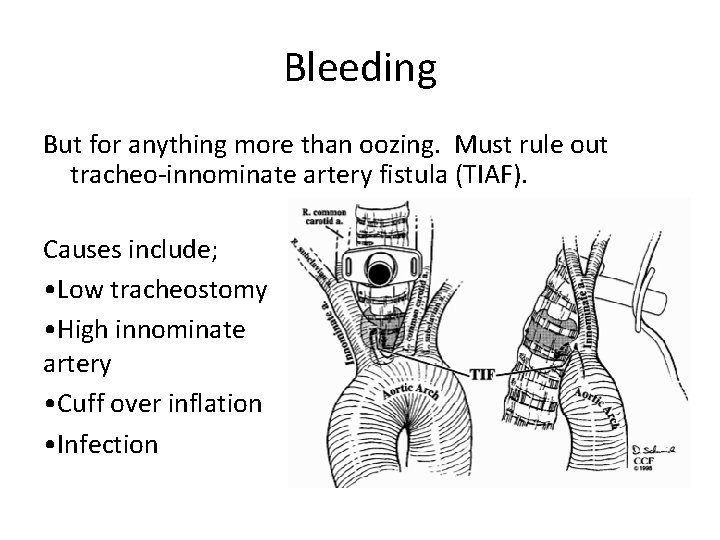
Bleeding But for anything more than oozing. Must rule out tracheo-innominate artery fistula (TIAF). Causes include; • Low tracheostomy • High innominate artery • Cuff over inflation • Infection
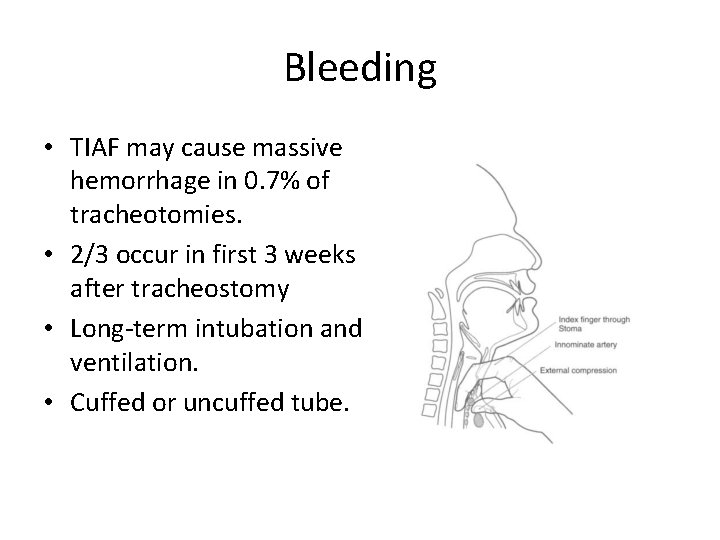
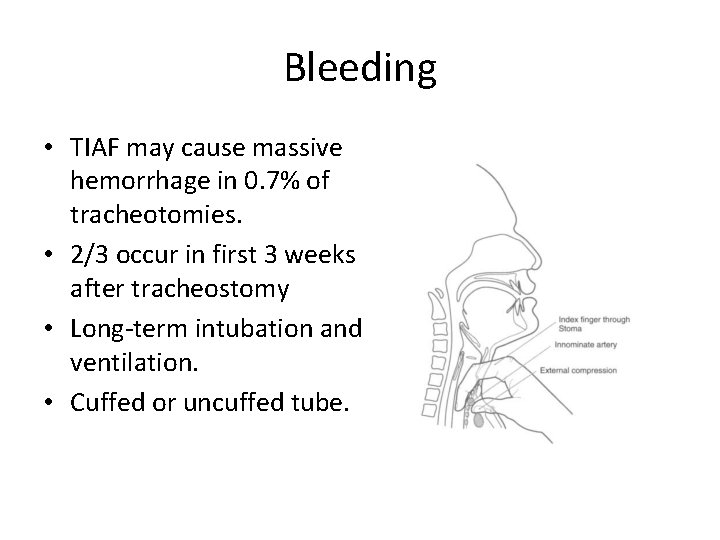
Bleeding • TIAF may cause massive hemorrhage in 0. 7% of tracheotomies. • 2/3 occur in first 3 weeks after tracheostomy • Long-term intubation and ventilation. • Cuffed or uncuffed tube.
Decannulation When the adult patient is in the hospital and; 1. Does not require mechanical ventilation 2. Indication for tracheotomy has resolved 3. Patient tolerates breathing through the tracheotomy tube with the cuff deflated. 4. Breathing with a cuffless #6 Shiley tube is checked (smaller patients, a cuffless #4 Shiley tube is placed) 5. Patient tolerates tracheostomy capped with a red button. 6. If the patient is stable (normal oxygen and CO 2) for 24 – 48 hours with the trach plugged, the tube will be removed by a qualified physician or mid-level provider, and the stoma will be allowed to close. Downsizing, capping and decannulation

Decannulation Downsizing, capping and decannulation
Decannulation When the patient succeeds at decannulation sequence, 1. Wound margins should heal by secondary intention, with initial wound co-apting in 5 to 7 days (unless wound was created with a fenestration technique) 2. New epithelial cells grow across wound in 7 to 10 days. No leak of air from the wound at this time. 3. If wound does not heal, then wound may be closed surgically, by separating trachea from the skin, and closing the wounds in layers. 4. If scar appearance is not acceptable, wound may be closed in a transverse incision across the lower neck with a plastic closure.
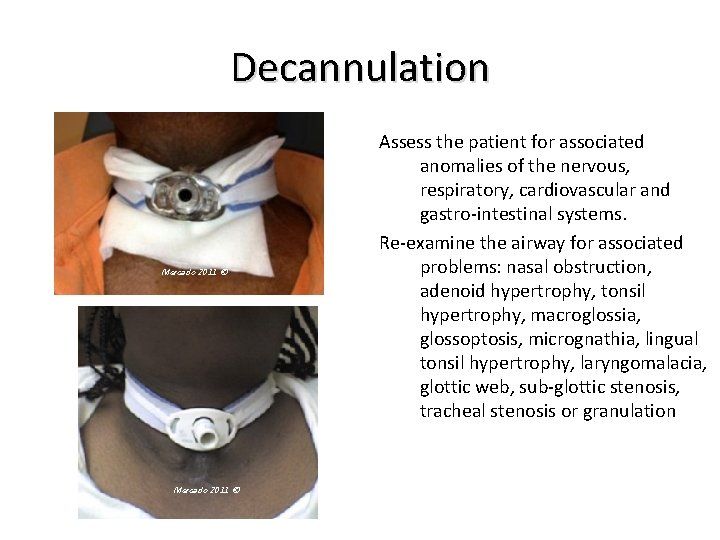
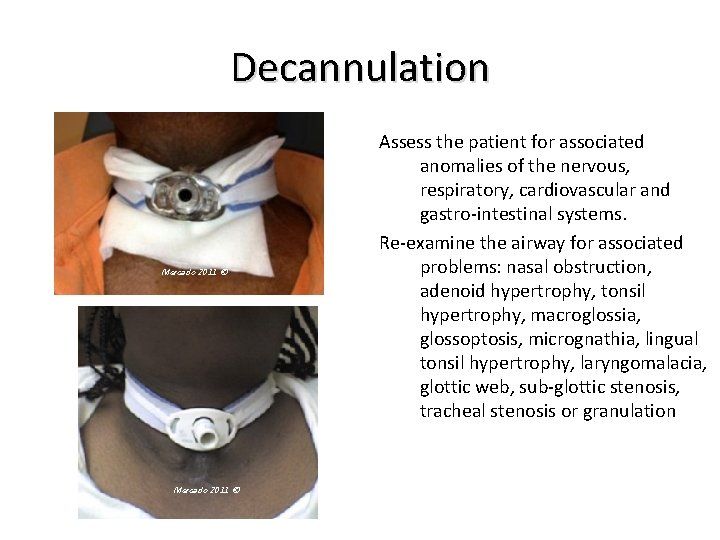
Decannulation Mercado 2011 © Assess the patient for associated anomalies of the nervous, respiratory, cardiovascular and gastro-intestinal systems. Re-examine the airway for associated problems: nasal obstruction, adenoid hypertrophy, tonsil hypertrophy, macroglossia, glossoptosis, micrognathia, lingual tonsil hypertrophy, laryngomalacia, glottic web, sub-glottic stenosis, tracheal stenosis or granulation
Clinical Consensus Summary • In the absence of aspiration, tracheostomy tube cuffs should be deflated when the patient no longer requires mechanical ventilation. • A patient initial tracheostomy tube should normally be replaced within 10 -14 days. • The Panel agreed an experienced physician should ideally be present for the first tube change, although there are was recognition that in some facilities, this may not be feasible and thus performed by an experienced advanced practice provider (APP) with immediate physician backup available. • In an emergency, a dislodged, mature tracheostomy tube should be replaced with the same size or a size smaller tracheostomy tube. If those are not available for could not be inserted, then an appropriately sized endotracheal tube should be placed through the wound into the trachea. In a patient in whom a tube could not be replaced, resulting in hypoxia or concern for eventual loss of airway, they should undergo oral tracheal intubation or immediate surgical revision tracheostomy.
Clinical Consensus Summary • Tracheostomy tube should be changed using a clean technique. A sterile technique is not necessary and does not lead to a reduction in impaction. • Plastic tracheostomy tube should be used among pediatric and adult patients for initial tube placement. • Tracheostomy tube ties should be used unless the patient recently underwent local or free flap reconstructive surgery or other major neck surgery. • No patient should be discharged with tracheostomy tube sutured in place. Any suture securing a tracheostomy should be removed during first tube change. • Stoma and tracheostomy tube should be suctioned when there is evidence of visual or audible secretions in the airway, suspected airway obstruction, and whether tube is changed or deflated.
Tracheotomy- Summary 1. Identify source of leaking and bleeding. 2. If unable to safely change tracheostomy at bedside consider revision tracheostomy in OR. 3. Care of the tracheostomy tube and the wound require planning and communication. 4. Do only as much as you have been trained to, feel comfortable doing and is within your scope of practice.
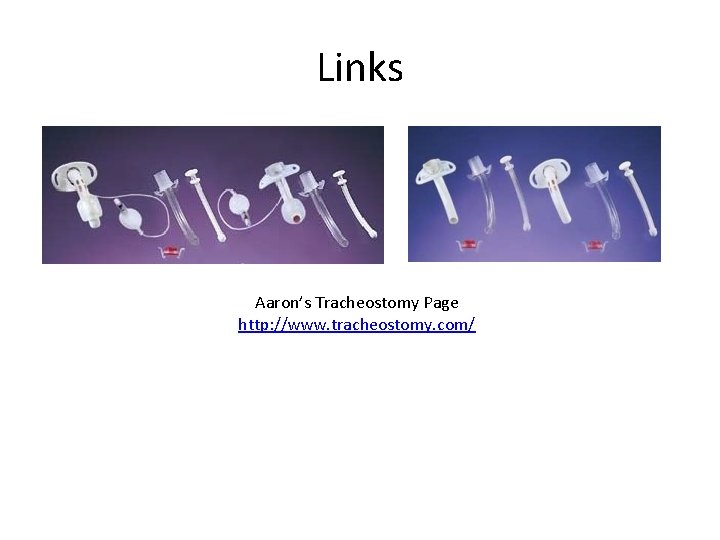
Links Aaron’s Tracheostomy Page http: //www. tracheostomy. com/
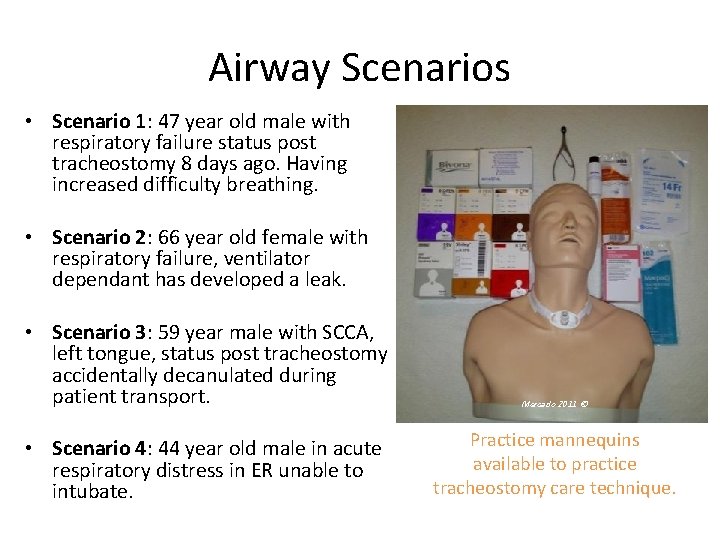
Airway Scenarios • Scenario 1: 47 year old male with respiratory failure status post tracheostomy 8 days ago. Having increased difficulty breathing. • Scenario 2: 66 year old female with respiratory failure, ventilator dependant has developed a leak. • Scenario 3: 59 year male with SCCA, left tongue, status post tracheostomy accidentally decanulated during patient transport. • Scenario 4: 44 year old male in acute respiratory distress in ER unable to intubate. Mercado 2011 © Practice mannequins available to practice tracheostomy care technique.
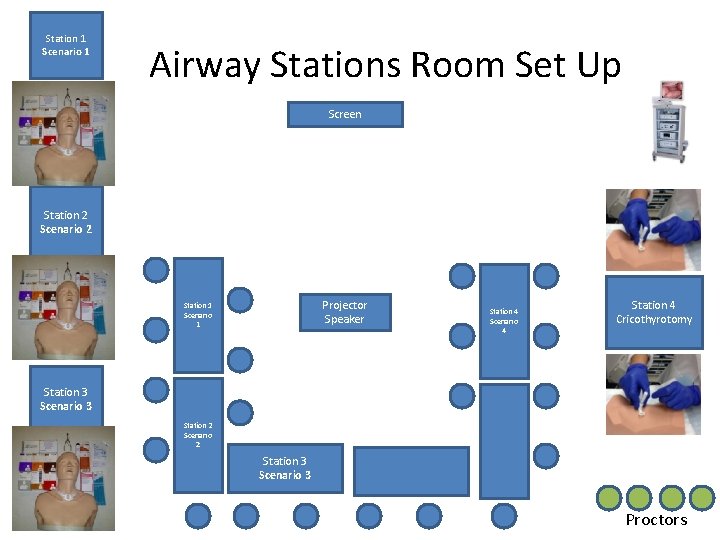
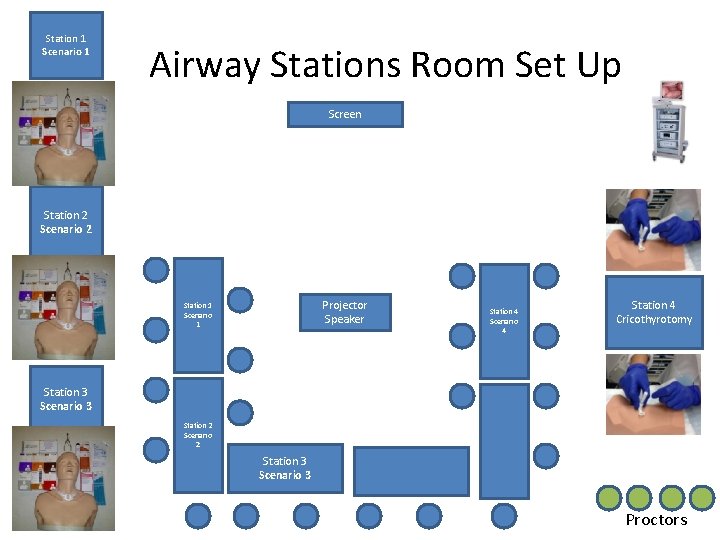
Station 1 Scenario 1 Airway Stations Room Set Up Screen Station 2 Scenario 2 Projector Speaker Station 1 Scenario 1 Station 4 Scenario 4 Station 4 Cricothyrotomy Station 3 Scenario 3 Station 2 Scenario 2 Station 3 Scenario 3 Proctors
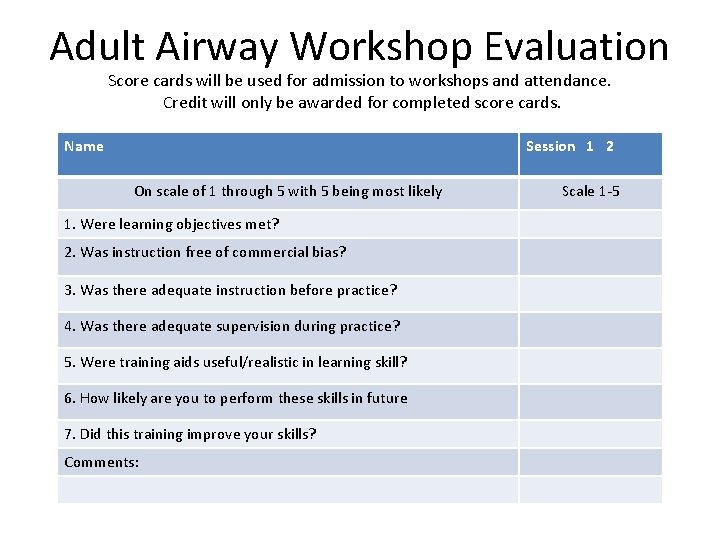
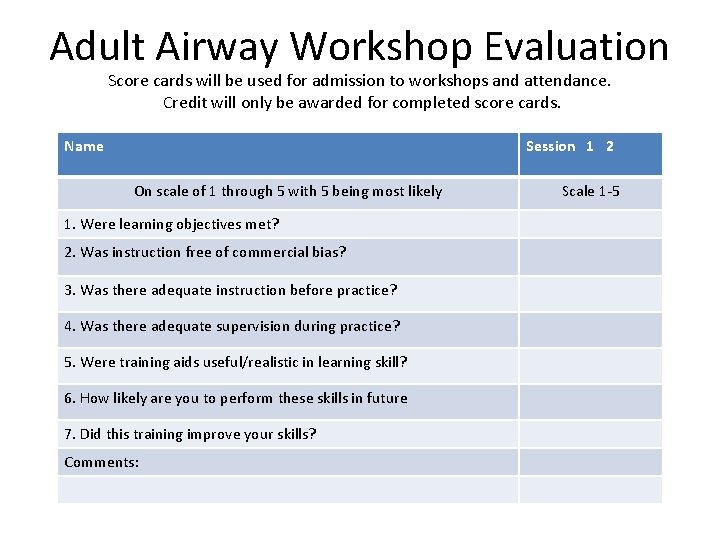
Adult Airway Workshop Evaluation Score cards will be used for admission to workshops and attendance. Credit will only be awarded for completed score cards. Name Session 1 2 On scale of 1 through 5 with 5 being most likely 1. Were learning objectives met? 2. Was instruction free of commercial bias? 3. Was there adequate instruction before practice? 4. Was there adequate supervision during practice? 5. Were training aids useful/realistic in learning skill? 6. How likely are you to perform these skills in future 7. Did this training improve your skills? Comments: Scale 1 -5
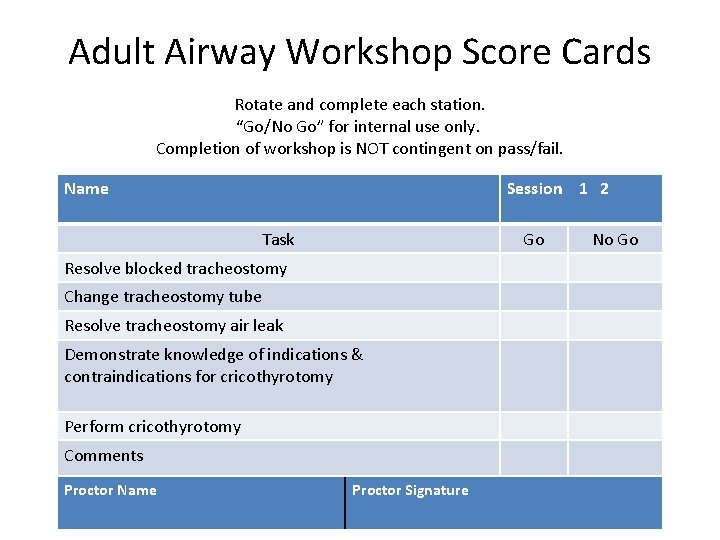
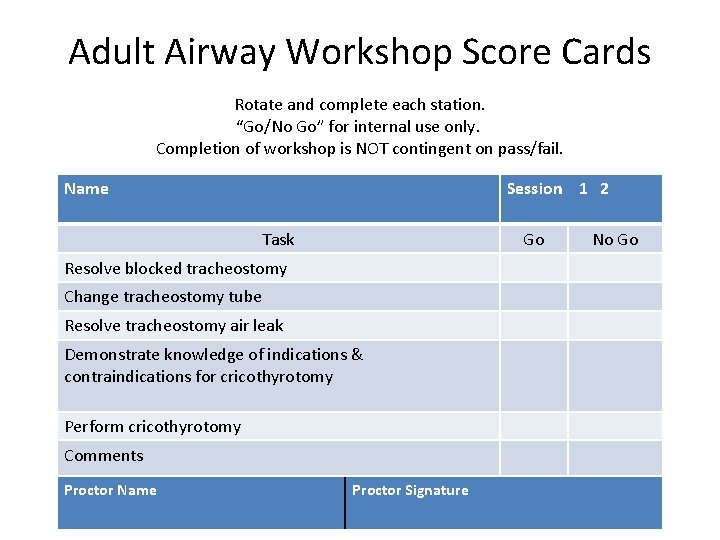
Adult Airway Workshop Score Cards Rotate and complete each station. “Go/No Go” for internal use only. Completion of workshop is NOT contingent on pass/fail. Name Session 1 2 Task Go Resolve blocked tracheostomy Change tracheostomy tube Resolve tracheostomy air leak Demonstrate knowledge of indications & contraindications for cricothyrotomy Perform cricothyrotomy Comments Proctor Name Proctor Signature No Go
 Laryngoscopy view grades
Laryngoscopy view grades Airway management acls
Airway management acls Tracheostomy stoma
Tracheostomy stoma Airway ladder
Airway ladder Npa measurement
Npa measurement Technique abcde
Technique abcde Sandwich manuver adalah
Sandwich manuver adalah Stepwise airway management
Stepwise airway management Smx advanced 2017 slides
Smx advanced 2017 slides Network management chicago
Network management chicago Chicago management training seminar
Chicago management training seminar Lemon anaesthesia
Lemon anaesthesia Lower respiratory tract
Lower respiratory tract Mechanism of respiration
Mechanism of respiration Respiratory airway secretary
Respiratory airway secretary Intubation airway anatomy
Intubation airway anatomy Cormack lehane
Cormack lehane Log roll
Log roll Mean airway pressure
Mean airway pressure Macintosh blade placement
Macintosh blade placement Mean airway pressure
Mean airway pressure Sellick manevrası
Sellick manevrası Vareculla
Vareculla Intubating lma
Intubating lma Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Mean airway pressure formula
Mean airway pressure formula Automatic positive airway pressure
Automatic positive airway pressure Asp medical
Asp medical Airway numaraları
Airway numaraları Asa airway classification
Asa airway classification Aprv
Aprv What is this picture from
What is this picture from Pharyngo-tracheal lumen airway
Pharyngo-tracheal lumen airway Rae
Rae Intubation anatomy
Intubation anatomy Seeking consensual validation
Seeking consensual validation Indications for artificial airway
Indications for artificial airway Emergency action step
Emergency action step Airway gym app
Airway gym app Airway breathing c
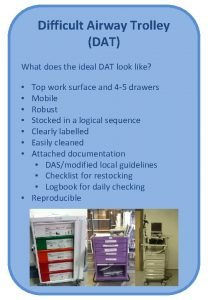
Airway breathing c Difficult airway trolley
Difficult airway trolley Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Moans airway
Moans airway Fire risk assessment surgery
Fire risk assessment surgery Generations of supraglottic airway devices
Generations of supraglottic airway devices Nasopharyngeal airway
Nasopharyngeal airway Nasopharyngeal airway
Nasopharyngeal airway Blood air barrier cells
Blood air barrier cells Asa difficult airway algorithm
Asa difficult airway algorithm Mouth gag airway
Mouth gag airway