There are only two things that drive patients

- Slides: 29
There are only two things that drive patients to doctors: Pain and Fear
�Pain may be defined as an unpleasant sensory or emotional experience associated with actual or potential tissue damage. �Chronic pain is defined as pain still present after three months despite appropriate treatment
NICE � A survey of 975 people in the UK reported that 21% experienced pain every day or on most days. 67% had visited their GP or a walk-in centre, requesting advice about pain relief. � Chronic pain: UK: Approximately 18% (Europe 19%) of the population are currently affected by moderate to severe chronic pain. � Predictors of chronic pain �short education, �poor self-rated health, �high body mass index and �physical strain at work
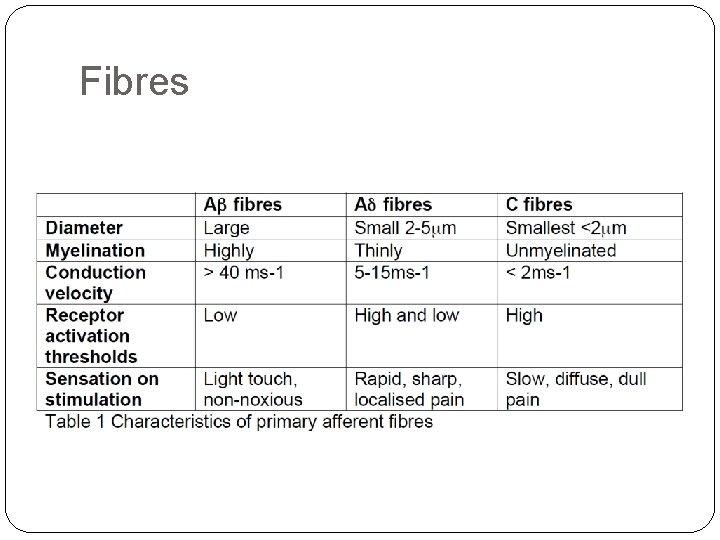
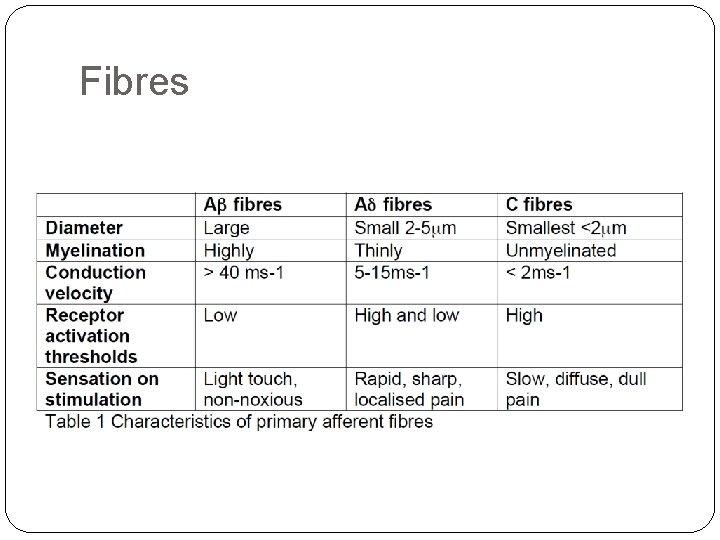
Fibres
�Nociceptors: �Free nerve endings/ sensory receptors �Mechanical/ thermal/chemical activation �Inflammatory mediators �Bradykinin, serotonin, prostaglandins, cytokines, H+ �Directly stimulate �sensitize so they respond abnormally readily �Trasmitters �Glutamate and Substance P �N-methyl-D-aspartate (NMDA) receptors in the postsynaptic area
Connections � Dorsal Horn �Complex connections: �Connect to secondary neurones � ascending spinothalamic (STh) � spinoreticular (SR) ( both decussate slightly higher) �Also connect with � Interneurones (Glycine, GABA) � descending modular pathways � Secondary neurones Thalamus/ hypothalamus �STh – projections to PAG on the way �SR – projections to the brain stem reticular formation on the way � Tertiary neurones project on to: �sensory cortex (localisation) and other areas - ‘Pain Matrix’ � Pain Matrix = EMOTIONAL component of pain experience �(prefrontal, cingulate, insula, parietal; and thereby to
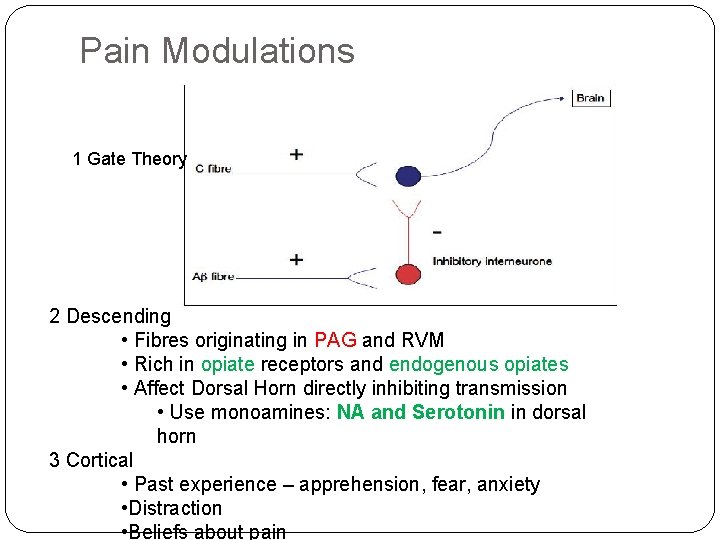
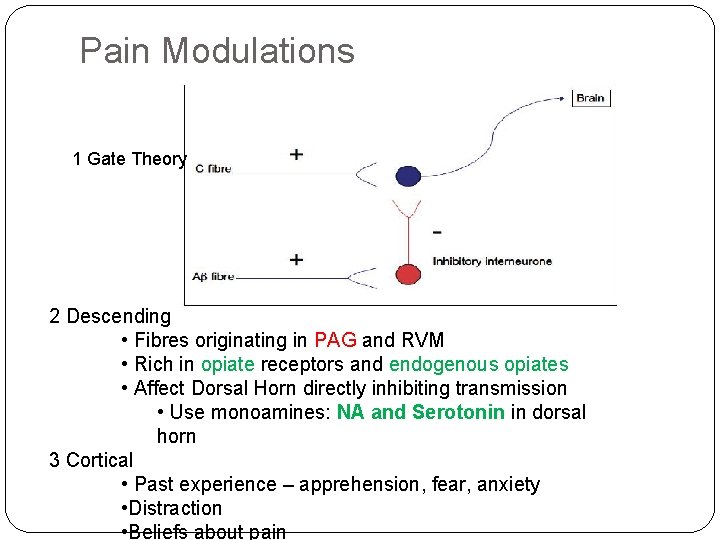
Pain Modulations 1 Gate Theory 2 Descending • Fibres originating in PAG and RVM • Rich in opiate receptors and endogenous opiates • Affect Dorsal Horn directly inhibiting transmission • Use monoamines: NA and Serotonin in dorsal horn 3 Cortical • Past experience – apprehension, fear, anxiety • Distraction • Beliefs about pain
Other factors to bear in mind �Plasticity, in which the central nervous system (CNS) adapts to new situations and 'rewires' itself. �Animal models suggest that developmental plasticity of nociceptive pathways occurring during early experience of pain (ie in the neonatal period) may lay the foundations for an individual's sensitivity to pain in later life. �Emotional, environmental and social factors are becoming increasingly recognised as issues which need to be addressed in the management of chronic pain.
Types of Pain �Somatic pain �Dealt with above – C and Aδ fibres �Sharp/ aching �well localised �Visceral Pain �C fibres - (smooth muscle stretching/ contracting or capsular stretching/ ischaemia/necrosis/ inflammatory chemical stimulation) �slow, deep/ dragging/ dull �autonomic connection – nausea/ sweating/ CVS changes/ strong emotional response �Poor localisation
Types of Pain �Neuropathic Pain �damage to central or peripheral nerves �Cutting/ crushing/chemical damage/ malignancy/radiation/ ischaemia/ infection �Burning or ‘Electric shock’ quality �Dermatomal/ region supplied by affected nerve �Spontaneous �Referred Pain �Pain experienced at a site distant to the source �Convergence of different afferents on the same neurones in the dorsal horn
Definitions �Allodynia: Pain due to a sensory stimulus that does not normally cause pain. �Hyperalgesia: Pain of increased intensity to that normally produced by a painful stimulus. �Sensitisation: Increased responsiveness of nociceptive neurones to their normal input (and/or recruitment of a response to normal sub-threshold inputs)
Pain consultation � Turn to your partner and explain the last patient you saw with moderate to severe pain �What was the pain like? �How would you categorise it? �How was it assessed – was investigation appropriate? � Was the cause identified �Did you think there were any complicating factors? �Did the treatment work? (Why/ why not? ) �Why did they consult about pain �what do they want out of a consultation? �What are your thoughts (reflections) about this?
Yellow flags �Increased risk of progression to long-term distress, disability and pain �Biomedical yellow flags: �severe pain/ increased disability at presentation, �previous significant pain episodes, �multiple site pain, �non-organic signs, �iatrogenic factors �Continuity/ Communication between all involved/ ownership �Over/ under-investigation – both dangerous
Yellow flags �Psychological yellow flags: �belief that pain indicates harm, �expectation that passive rather than active treatments are most helpful, �fear avoidance behaviour, �poor problem solving ability, catastrophic thinking �passive coping strategies, �atypical health beliefs, �psychosomatic presentations, �high levels of distress.
Yellow flags �Social yellow flags: �low expectation of return to work, �lack of confidence in performing work activities, �heavier work, �low levels of control over rate of work, �poor work relationships, �social dysfunction, �medico-legal issues.
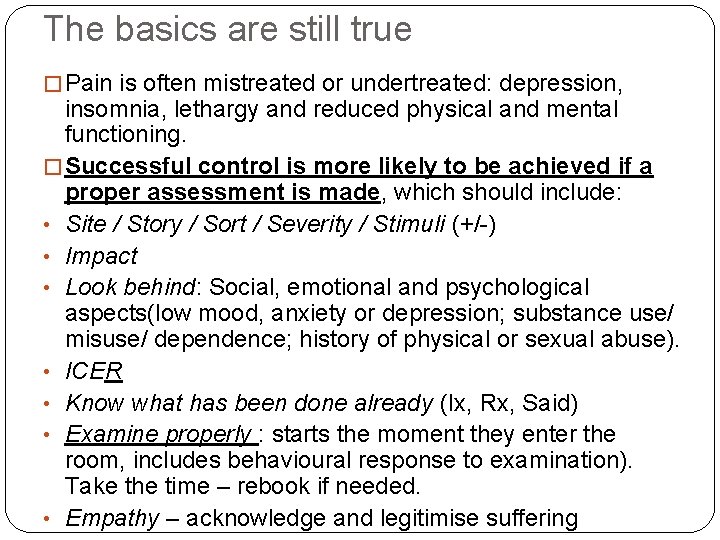
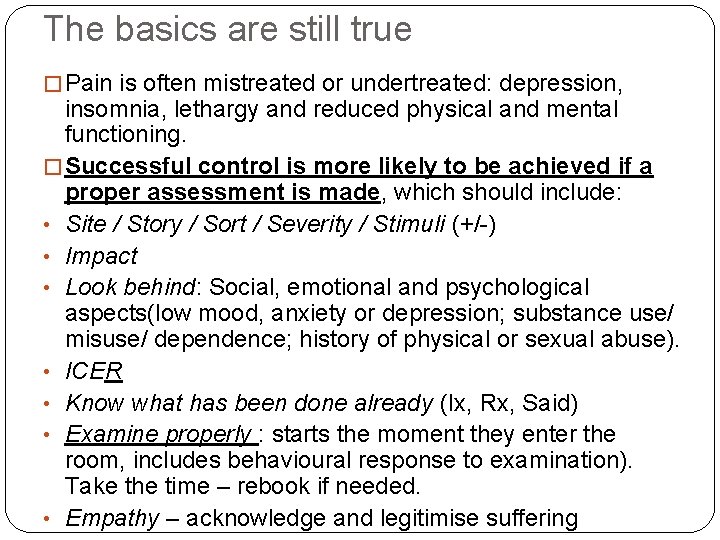
The basics are still true � Pain is often mistreated or undertreated: depression, insomnia, lethargy and reduced physical and mental functioning. � Successful control is more likely to be achieved if a proper assessment is made, which should include: • Site / Story / Sort / Severity / Stimuli (+/-) • Impact • Look behind: Social, emotional and psychological aspects(low mood, anxiety or depression; substance use/ misuse/ dependence; history of physical or sexual abuse). • ICER • Know what has been done already (Ix, Rx, Said) • Examine properly : starts the moment they enter the room, includes behavioural response to examination). Take the time – rebook if needed. • Empathy – acknowledge and legitimise suffering
Low back pain �What causes it. . ? Could you order by prevalence ? �What do we worry about? �What do patients worry about? �What is the role of investigations in low back pain �MRI ? �X ray? �Blood tests?

Red flags for back pain �Thoracic pain �Fever and unexplained weight loss �Bladder or bowel dysfunction �History of carcinoma �Ill health or presence of other medical illness �Progressive neurological deficit �Disturbed gait, saddle anaesthesia �Age of onset <20 years or >55 years
Doctor information �Gordon is a 44 year old man who works for Parcel -Force. He rarely sees the doctor. �It says against the ‘reason for the consultation’ ‘ ? Sick note. Back pain. ’
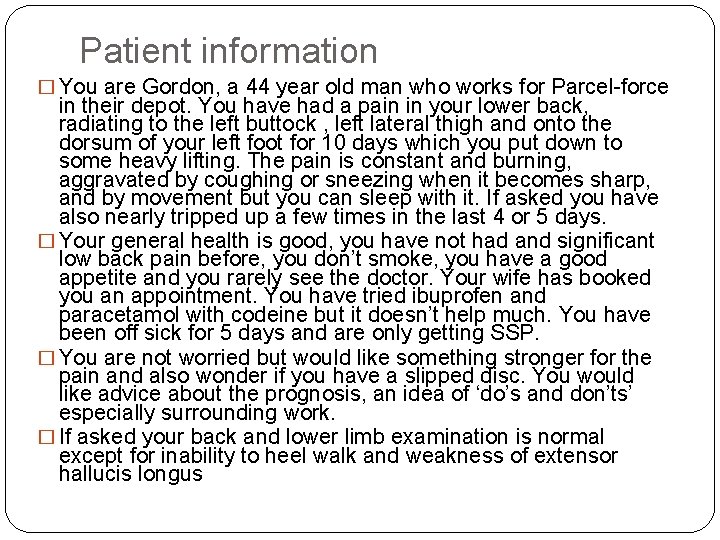
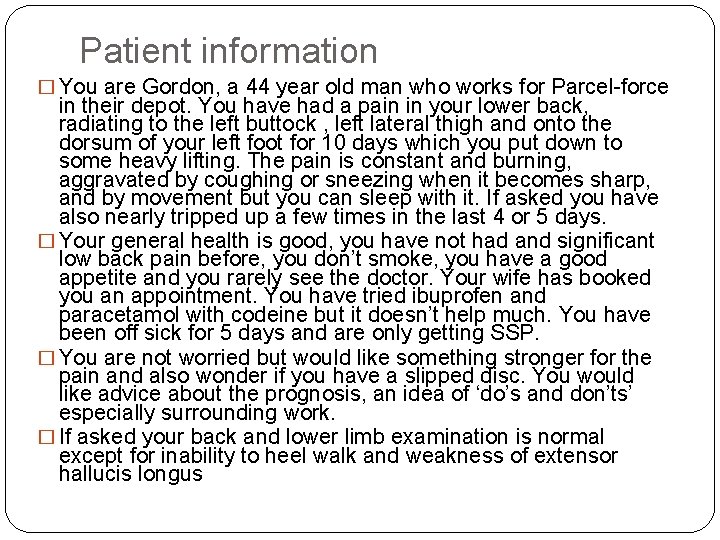
Patient information � You are Gordon, a 44 year old man who works for Parcel-force in their depot. You have had a pain in your lower back, radiating to the left buttock , left lateral thigh and onto the dorsum of your left foot for 10 days which you put down to some heavy lifting. The pain is constant and burning, aggravated by coughing or sneezing when it becomes sharp, and by movement but you can sleep with it. If asked you have also nearly tripped up a few times in the last 4 or 5 days. � Your general health is good, you have not had and significant low back pain before, you don’t smoke, you have a good appetite and you rarely see the doctor. Your wife has booked you an appointment. You have tried ibuprofen and paracetamol with codeine but it doesn’t help much. You have been off sick for 5 days and are only getting SSP. � You are not worried but would like something stronger for the pain and also wonder if you have a slipped disc. You would like advice about the prognosis, an idea of ‘do’s and don’ts’ especially surrounding work. � If asked your back and lower limb examination is normal except for inability to heel walk and weakness of extensor hallucis longus
Low back pain �Mechanical LBP- Lifetime prevalence 50 -70% - Point prevalence 12 -30% �Exercise therapy, back schools, manipulation, behavioural Rx work – and much better and for longer if individualised and delivered with supervision �Corsets, traction, short-wave diathermy, ultrasound and rest don’t
Low back pain �At least 5% LBP caused by disc prolapse �‘Sciatica’ increases likelihood � 50 -90% discs motor/sensory signs �Assessment: �Hip dip (L 3/4) (knee jerk) �Heel Walk (L 5) (ankle jerk) �Tip toe walk (S 1) (ankle jerk) �Sensation – ‘orthopaedic’ - ? bilat / progressive �Sacral/ saddle Anal tone? (-This week) (- Today) (- Now)
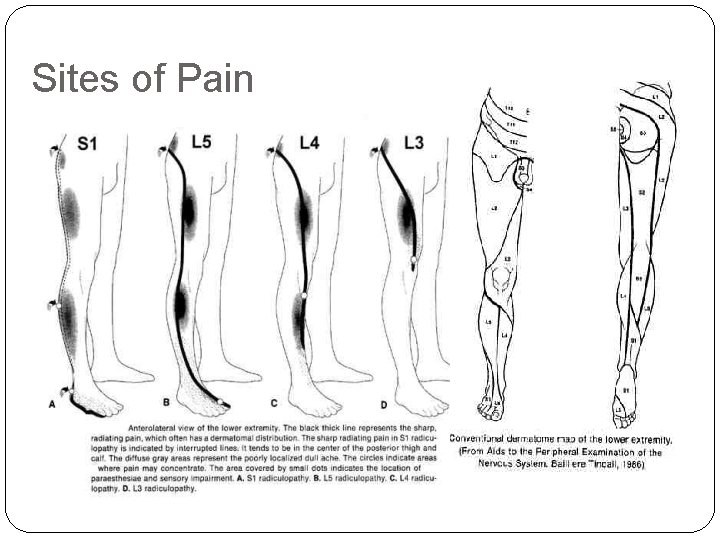
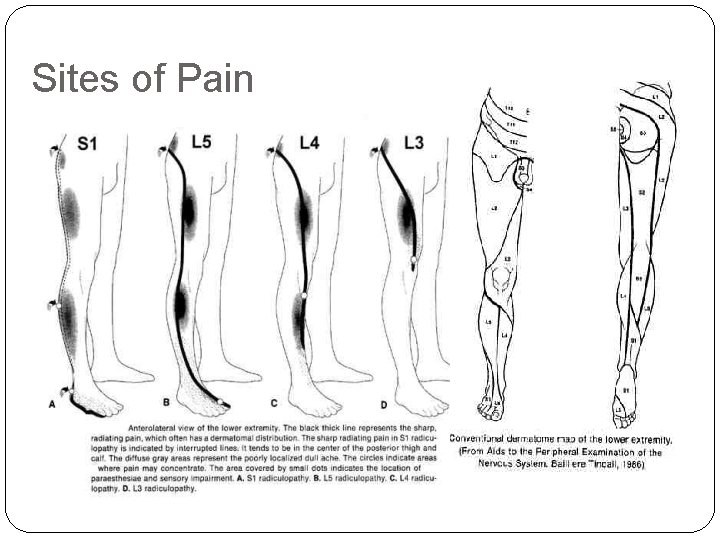
Sites of Pain
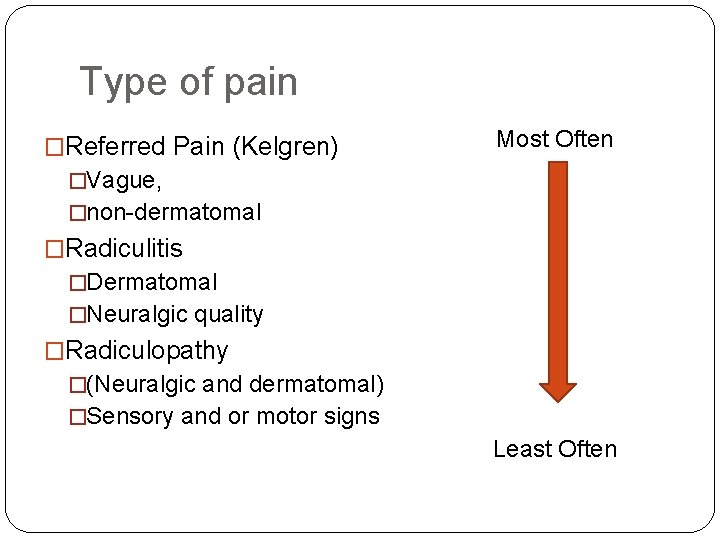
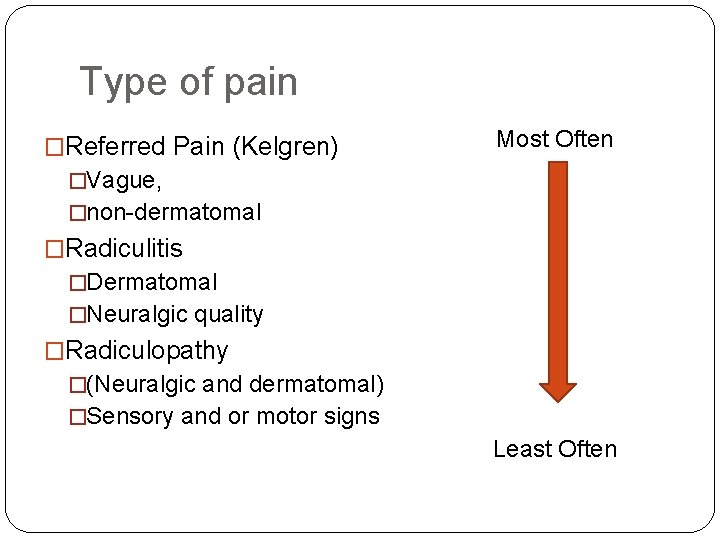
Type of pain �Referred Pain (Kelgren) Most Often �Vague, �non-dermatomal �Radiculitis �Dermatomal �Neuralgic quality �Radiculopathy �(Neuralgic and dermatomal) �Sensory and or motor signs Least Often
Low back pain �Treatment �Discectomy �Microdiscectomy �(Percutaneous discectomy) �(Laser discectomy) �Quicker relief…… �Or…. . .
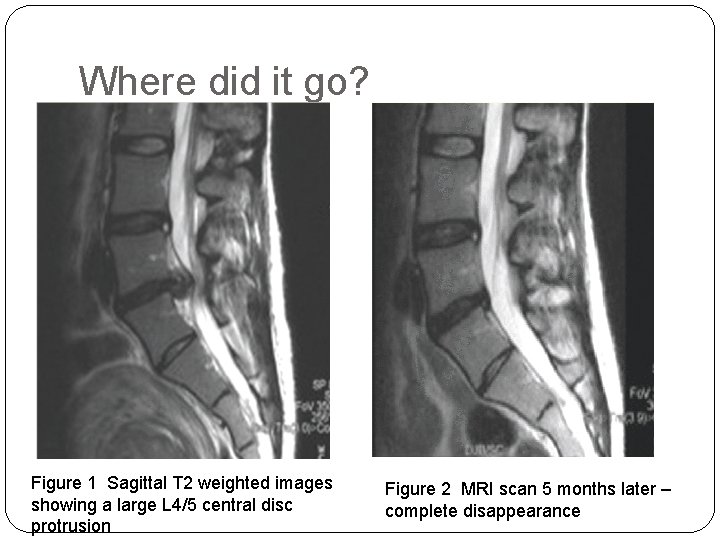
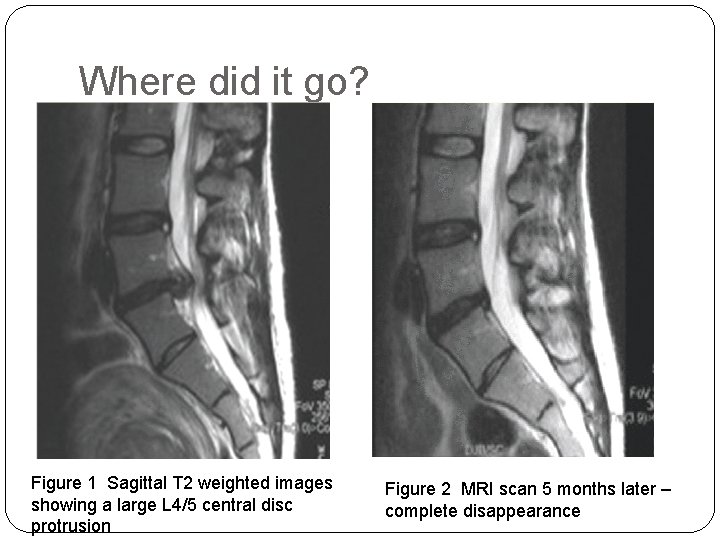
Where did it go? Figure 1 Sagittal T 2 weighted images showing a large L 4/5 central disc protrusion Figure 2 MRI scan 5 months later – complete disappearance
Low back pain �In the absence of above serious sx /signs � 75 -90% experience resolution without surgery: serial MRI’s prove it. (Sequestered fragment even more so)(2) �Mechanism: 1)Neovascularisation 2)Infiltration inflammatory cells (Macrophages, Granulocytes, Lymphocytes) 3)Resorption/ digestion https: //www. youtube. com/watch? v=BOj. Tegn 9 Ru. Y
The basics are still true � Pain is often mistreated or undertreated: depression, insomnia, lethargy and reduced physical and mental functioning. � Successful control is more likely to be achieved if a proper assessment is made, which should include: • Site / Story / Sort / Severity / Stimuli (+/-) • Impact • Look behind: Social, emotional and psychological aspects(low mood, anxiety or depression; substance use/ misuse/ dependence; history of physical or sexual abuse). • ICER • Know what has been done already (Ix, Rx, Said) • Examine properly : starts the moment they enter the room, includes behavioural response to examination). Take the time – rebook if needed. • Empathy – acknowledge and legitimise suffering