The Role of Atherectomy in the Management of
- Slides: 19
The Role of Atherectomy in the Management of Severely Calcified Lesions Sunil V. Rao MD FSCAI Duke University Health System Durham VA Health System
Disclosures • Institutional research funding • Svelte Inc • Shockwave Medical • Bayer • No consulting RWI • Thanks to Ajay Kirtane for slides
Coronary calcification • Incidence of coronary calcification • Outcomes in patients undergoing PCI of calcified coronary lesions • Atherectomy as an approach to dealing with calcification in the cath lab
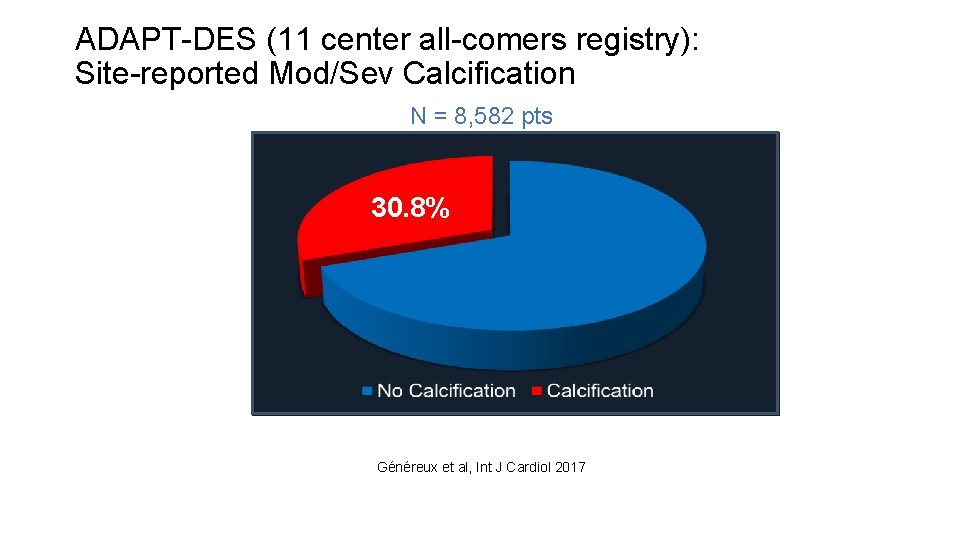
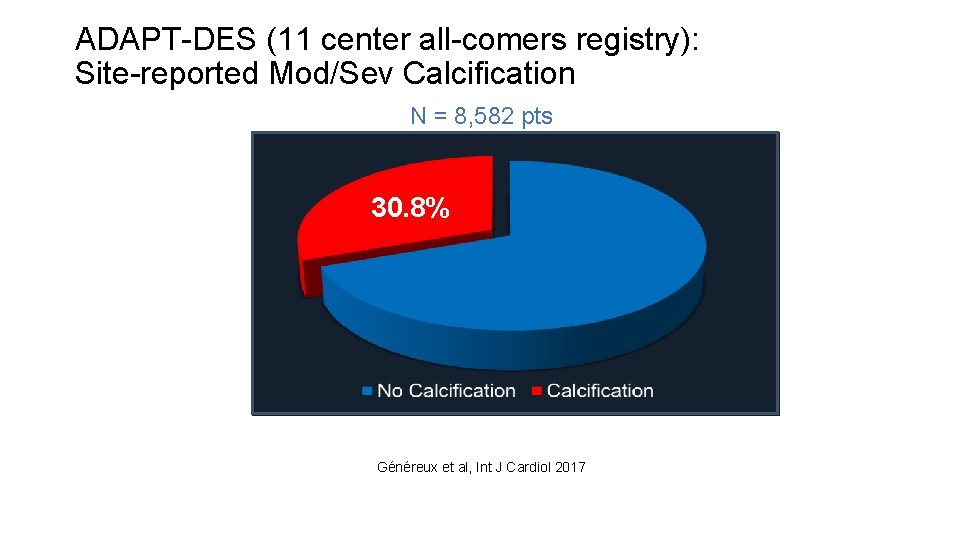
ADAPT-DES (11 center all-comers registry): Site-reported Mod/Sev Calcification N = 8, 582 pts 30. 8% Généreux et al, Int J Cardiol 2017
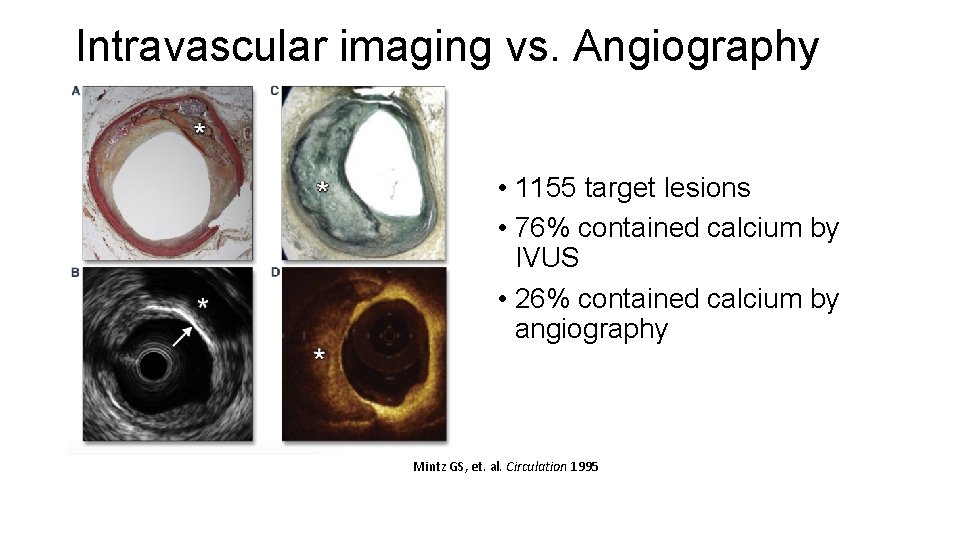
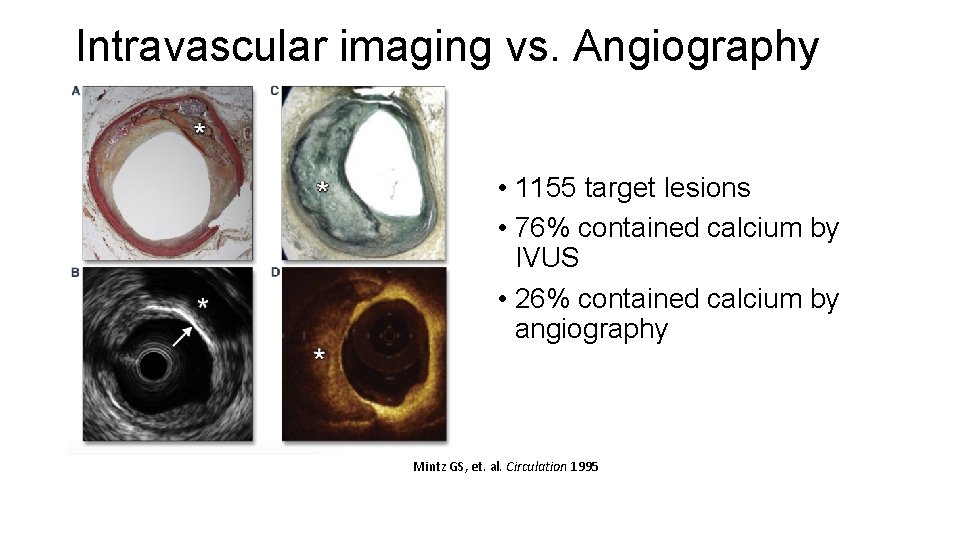
Intravascular imaging vs. Angiography • 1155 target lesions • 76% contained calcium by IVUS • 26% contained calcium by angiography Mintz GS, et. al. Circulation 1995
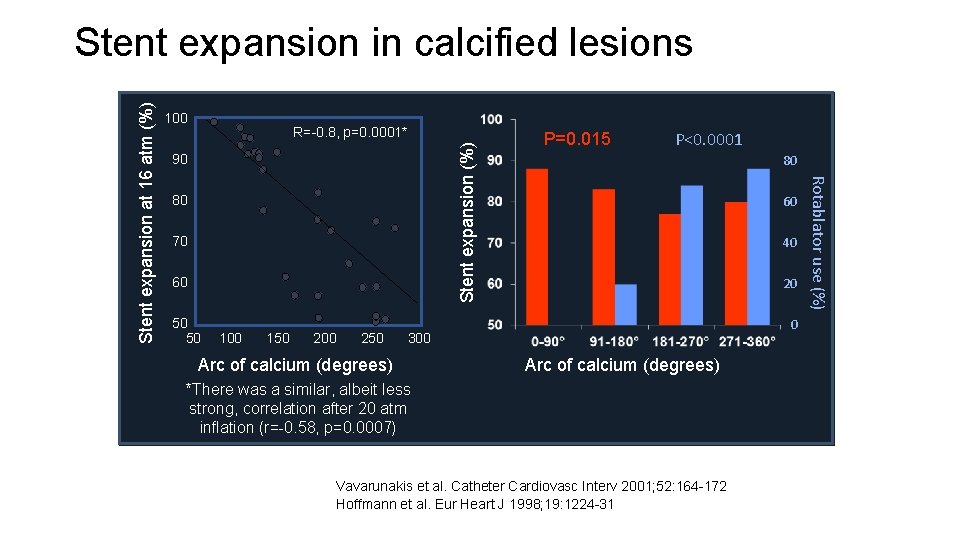
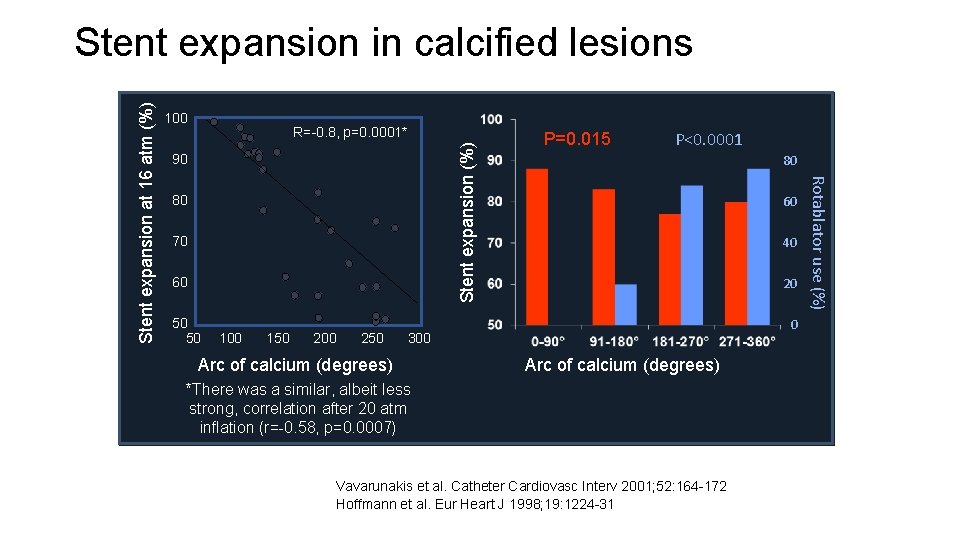
100 Stent expansion (%) R=-0. 8, p=0. 0001* 90 80 70 60 50 50 100 150 200 250 P=0. 015 P<0. 0001 80 60 40 20 0 300 Arc of calcium (degrees) *There was a similar, albeit less strong, correlation after 20 atm inflation (r=-0. 58, p=0. 0007) Vavarunakis et al. Catheter Cardiovasc Interv 2001; 52: 164 -172 Hoffmann et al. Eur Heart J 1998; 19: 1224 -31 Rotablator use (%) Stent expansion at 16 atm (%) Stent expansion in calcified lesions
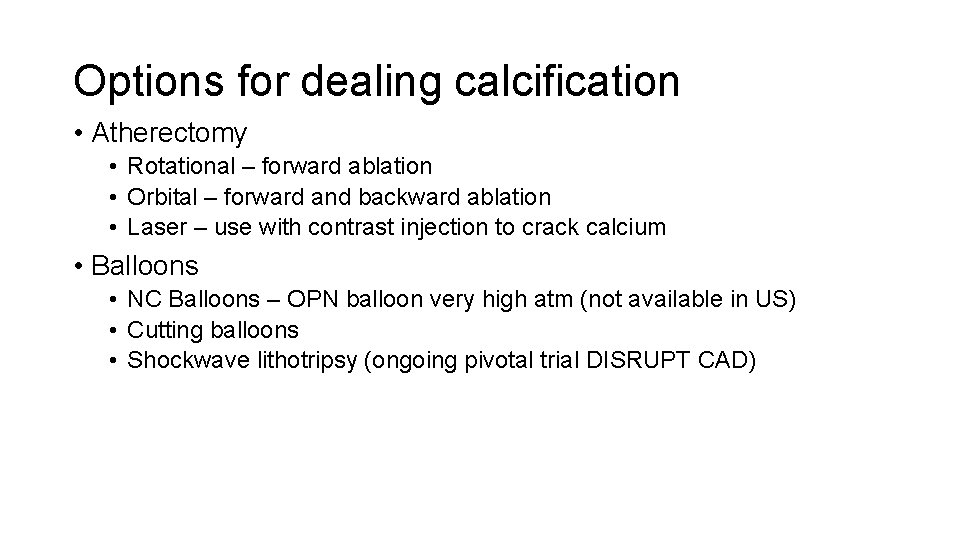
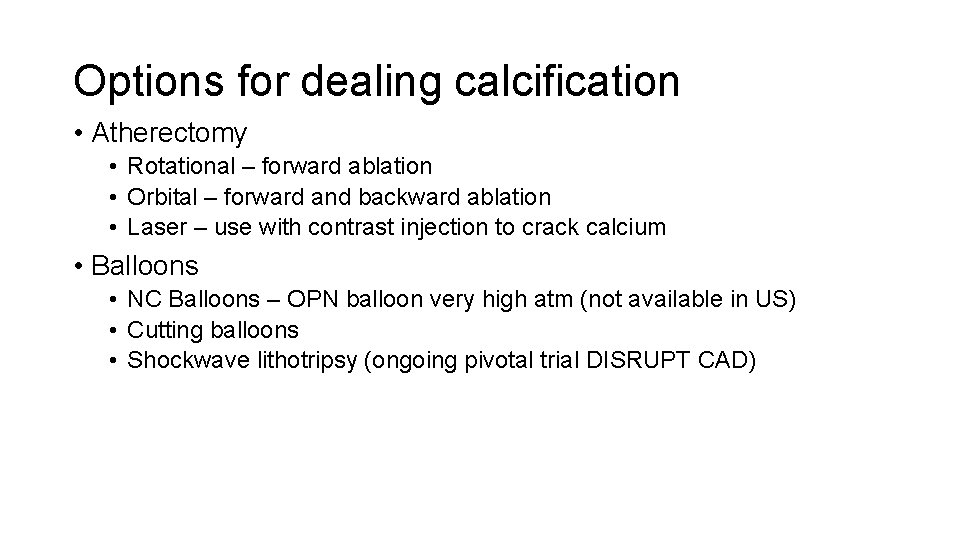
Options for dealing calcification • Atherectomy • Rotational – forward ablation • Orbital – forward and backward ablation • Laser – use with contrast injection to crack calcium • Balloons • NC Balloons – OPN balloon very high atm (not available in US) • Cutting balloons • Shockwave lithotripsy (ongoing pivotal trial DISRUPT CAD)
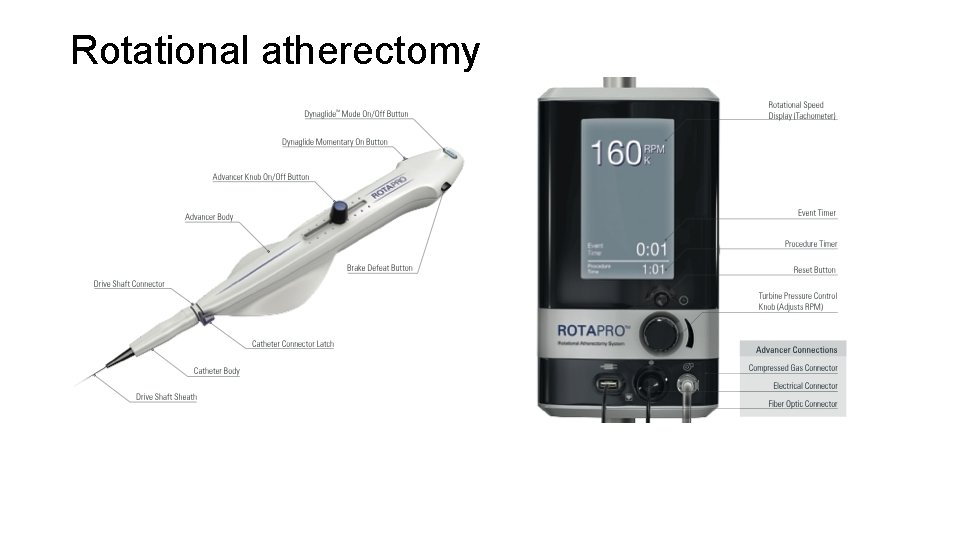
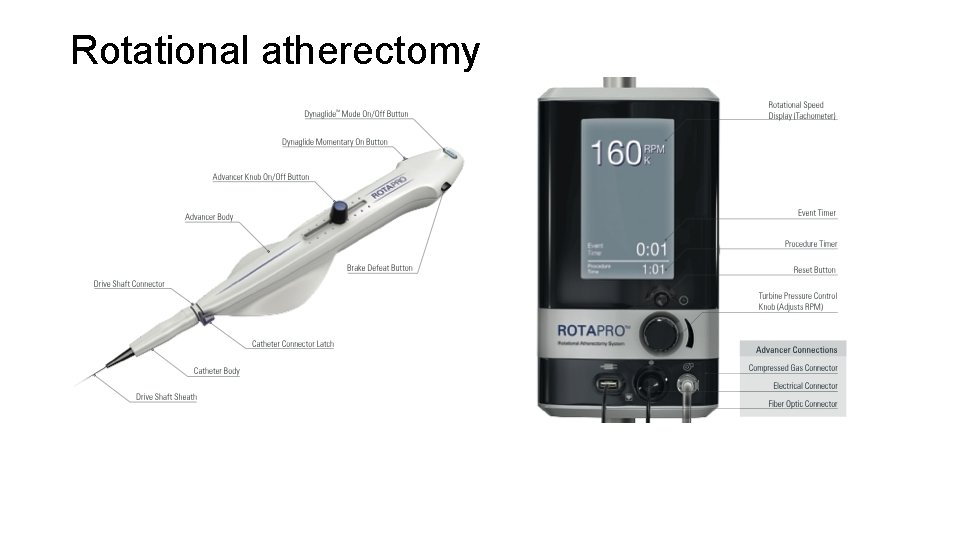
Rotational atherectomy
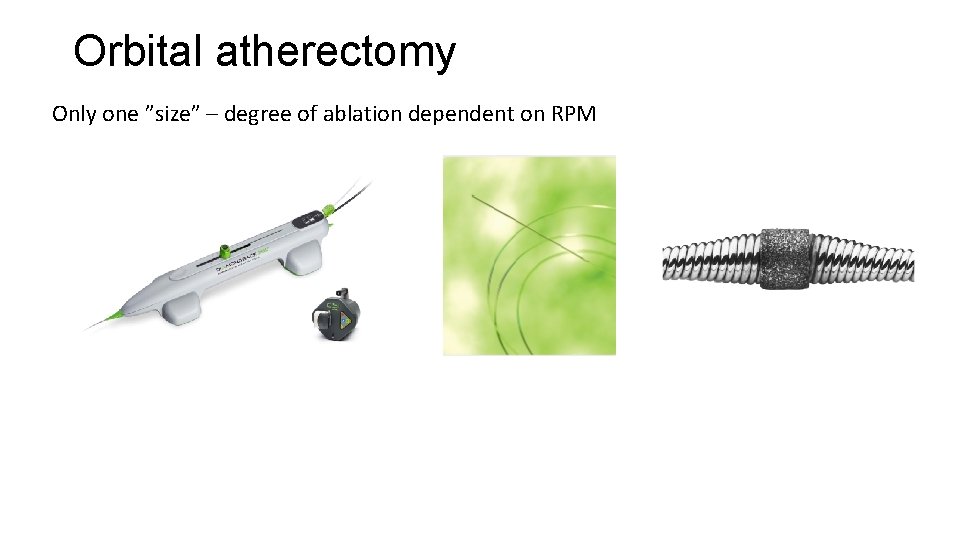
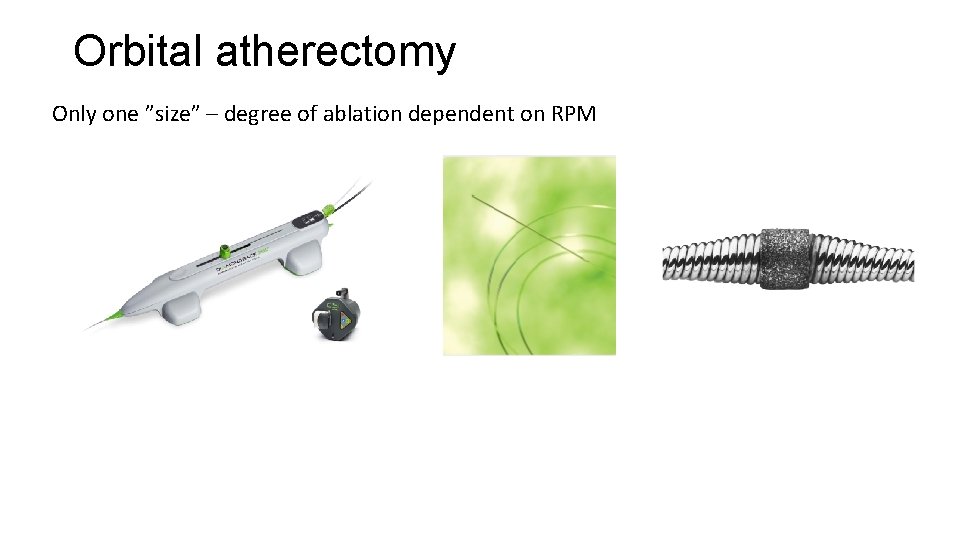
Orbital atherectomy Only one ”size” – degree of ablation dependent on RPM
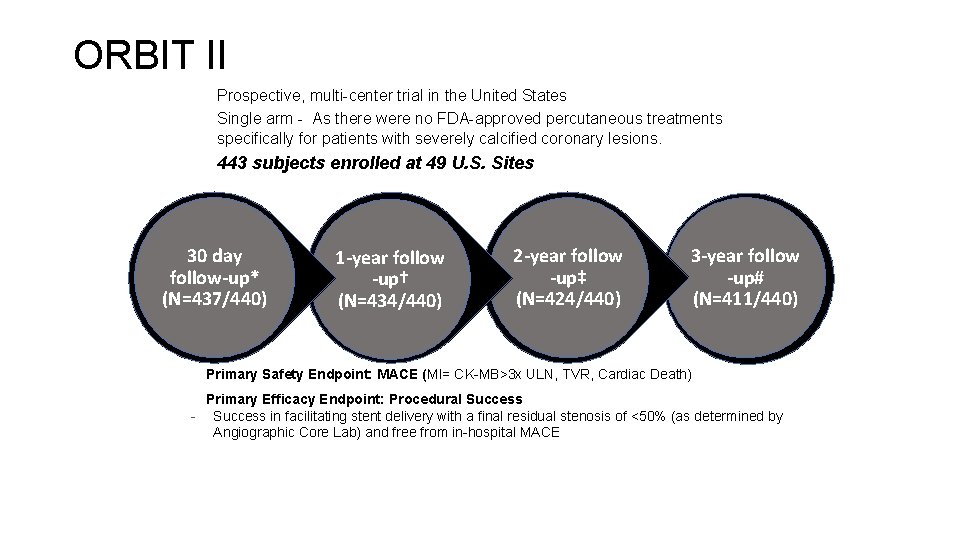
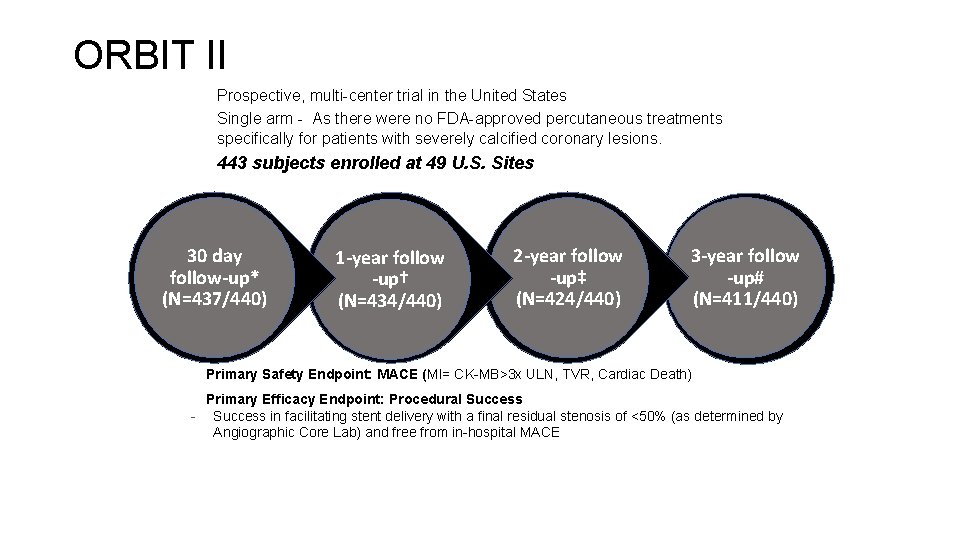
ORBIT II: Study Design ORBIT II – Prospective, multi-center trial in the United States – Single arm - As there were no FDA-approved percutaneous treatments specifically for patients with severely calcified coronary lesions. – 443 subjects enrolled at 49 U. S. Sites 30 day follow-up* (N=437/440) • • 1 -year follow -up† (N=434/440) 2 -year follow -up‡ (N=424/440) 3 -year follow -up# (N=411/440) Primary Safety Endpoint: MACE (MI= CK-MB>3 x ULN, TVR, Cardiac Death) Primary Efficacy Endpoint: Procedural Success - Success in facilitating stent delivery with a final residual stenosis of <50% (as determined by Angiographic Core Lab) and free from in-hospital MACE
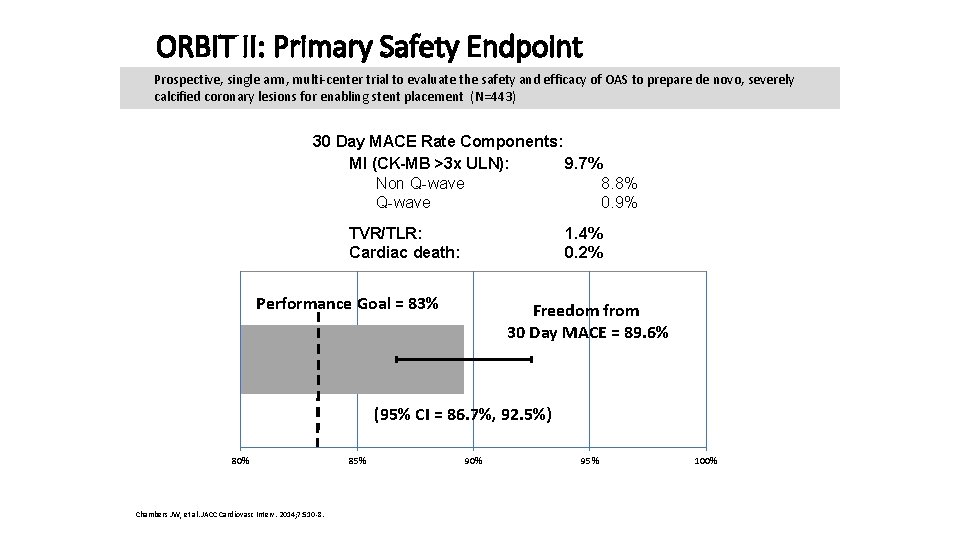
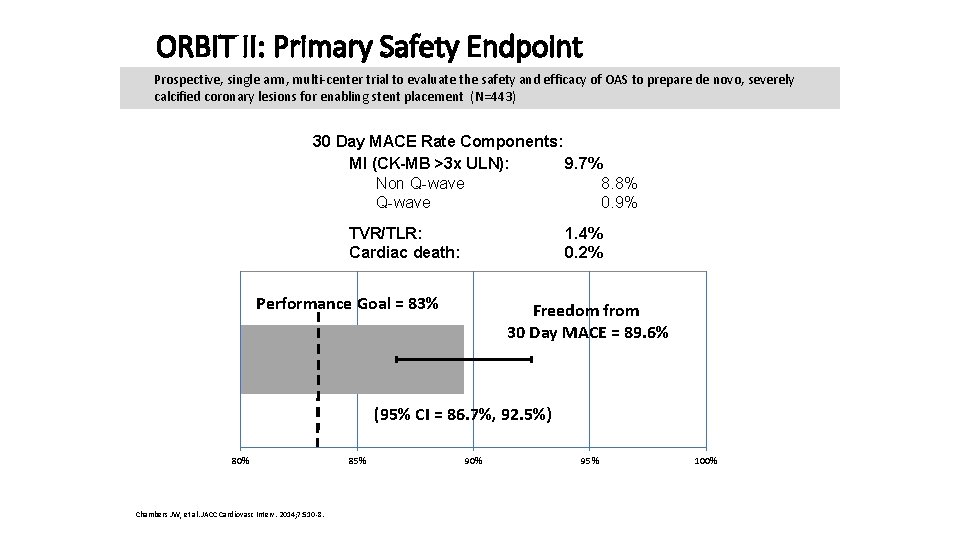
ORBIT II: Primary Safety Endpoint Prospective, single arm, multi-center trial to evaluate the safety and efficacy of OAS to prepare de novo, severely calcified coronary lesions for enabling stent placement (N=443) 30 Day MACE Rate Components: MI (CK-MB >3 x ULN): 9. 7% Non Q-wave 8. 8% Q-wave 0. 9% TVR/TLR: Cardiac death: 1. 4% 0. 2% Performance Goal = 83% Freedom from 30 Day MACE = 89. 6% (95% CI = 86. 7%, 92. 5%) 80% Chambers JW, et al. JACC Cardiovasc Interv. 2014; 7: 510 -8. 85% 90% 95% 100%
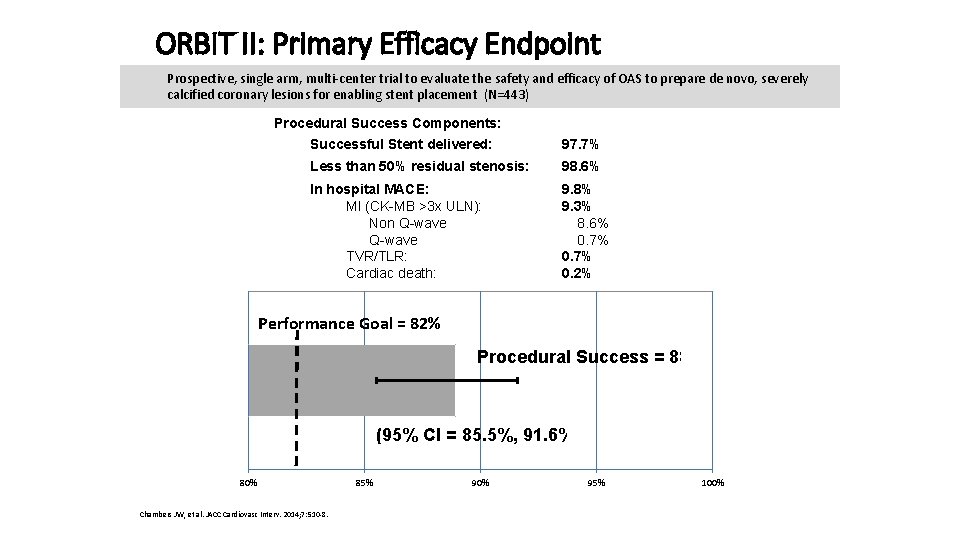
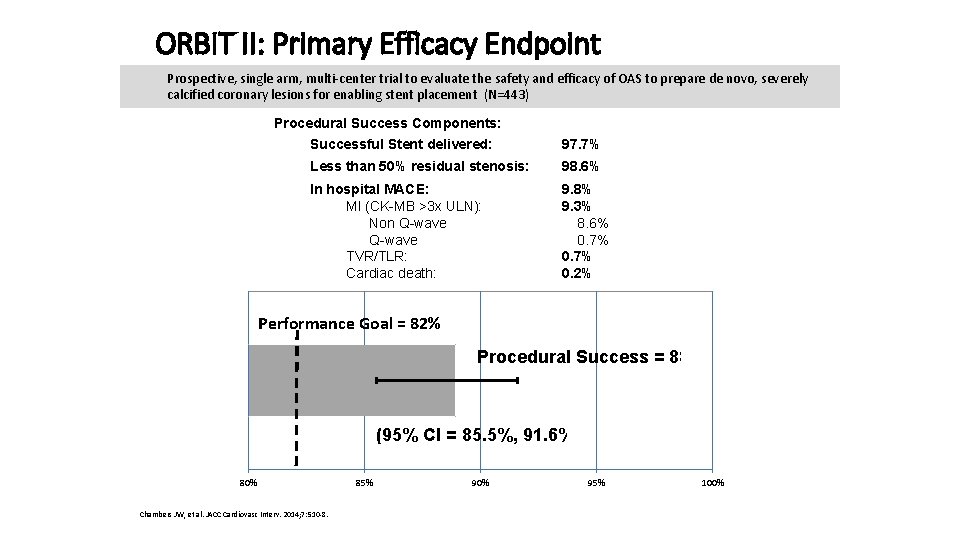
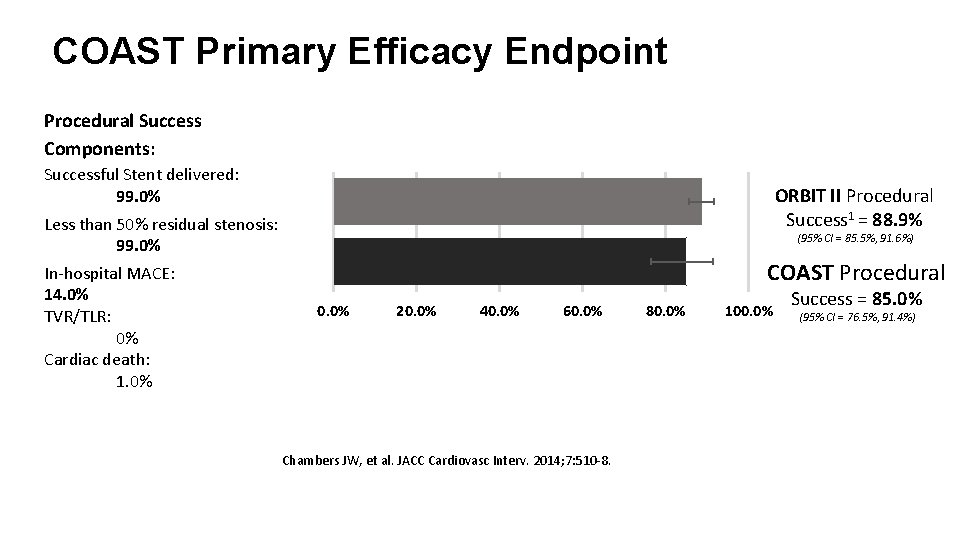
ORBIT II: Primary Efficacy Endpoint Prospective, single arm, multi-center trial to evaluate the safety and efficacy of OAS to prepare de novo, severely calcified coronary lesions for enabling stent placement (N=443) Procedural Success Components: Successful Stent delivered: 97. 7% Less than 50% residual stenosis: 98. 6% In hospital MACE: MI (CK-MB >3 x ULN): Non Q-wave TVR/TLR: Cardiac death: 9. 8% 9. 3% 8. 6% 0. 7% 0. 2% Performance Goal = 82% Procedural Success = 88. 9% (95% CI = 85. 5%, 91. 6%) 80% Chambers JW, et al. JACC Cardiovasc Interv. 2014; 7: 510 -8. 85% 90% 95% 100%
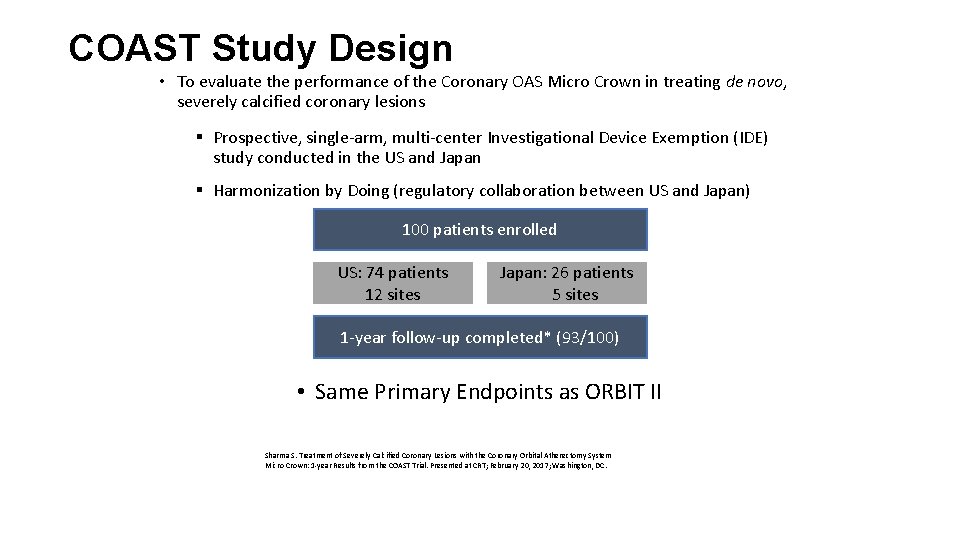
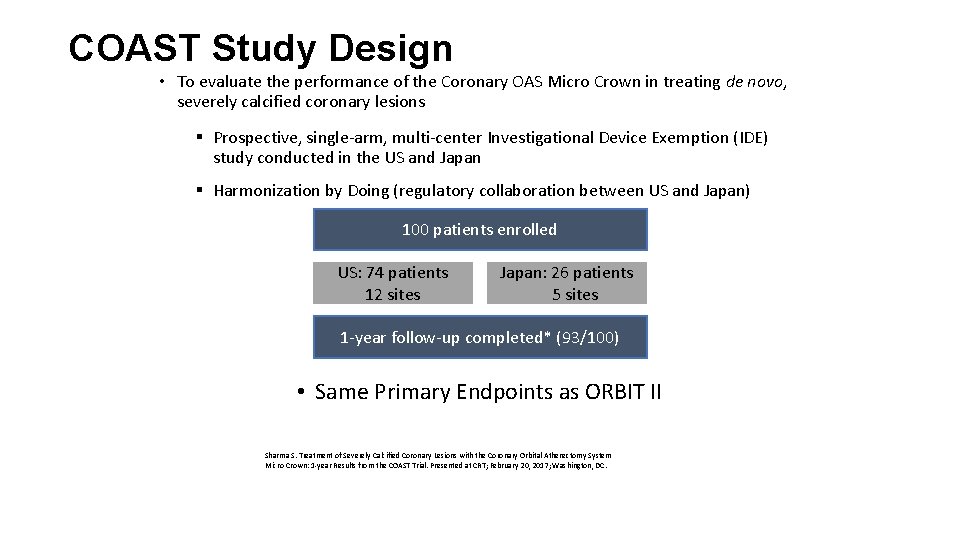
COAST Study Design • To evaluate the performance of the Coronary OAS Micro Crown in treating de novo, severely calcified coronary lesions § Prospective, single-arm, multi-center Investigational Device Exemption (IDE) study conducted in the US and Japan § Harmonization by Doing (regulatory collaboration between US and Japan) 100 patients enrolled US: 74 patients 12 sites Japan: 26 patients 5 sites 1 -year follow-up completed* (93/100) • Same Primary Endpoints as ORBIT II Sharma S. Treatment of Severely Calcified Coronary Lesions with the Coronary Orbital Atherectomy System Micro Crown: 1 -year Results from the COAST Trial. Presented at CRT; February 20, 2017; Washington, DC.
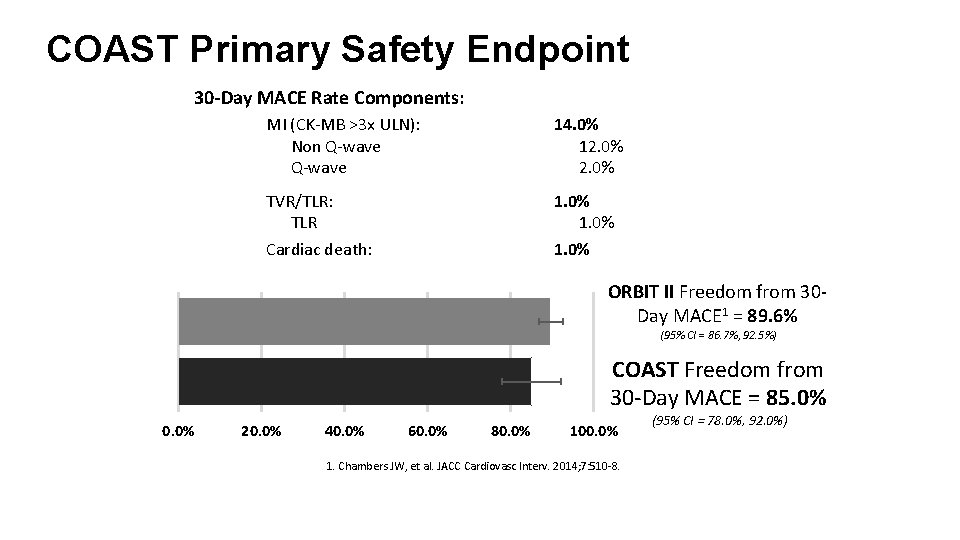
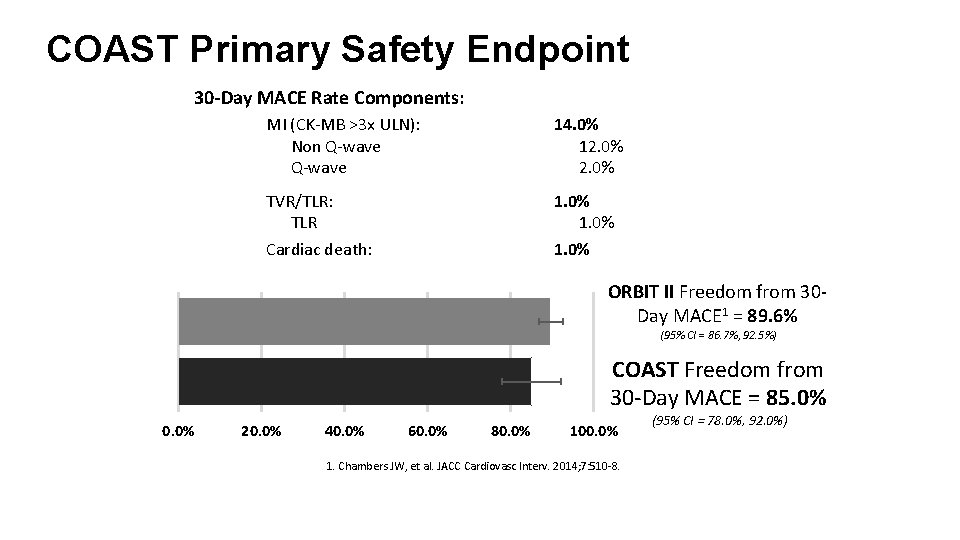
COAST Primary Safety Endpoint 30 -Day MACE Rate Components: MI (CK-MB >3 x ULN): Non Q-wave 14. 0% 12. 0% TVR/TLR: TLR 1. 0% Cardiac death: 1. 0% ORBIT II Freedom from 30 Day MACE 1 = 89. 6% (95% CI = 86. 7%, 92. 5%) COAST Freedom from 30 -Day MACE = 85. 0% 0. 0% 20. 0% 40. 0% 60. 0% 80. 0% 100. 0% 1. Chambers JW, et al. JACC Cardiovasc Interv. 2014; 7: 510 -8. (95% CI = 78. 0%, 92. 0%)
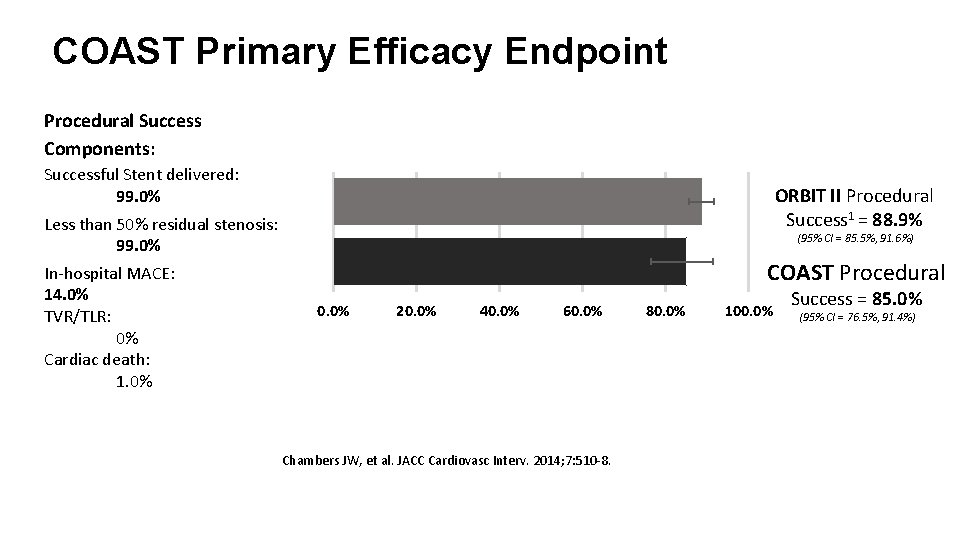
COAST Primary Efficacy Endpoint Procedural Success Components: Successful Stent delivered: 99. 0% ORBIT II Procedural Success 1 = 88. 9% Less than 50% residual stenosis: 99. 0% In-hospital MACE: 14. 0% TVR/TLR: 0% Cardiac death: 1. 0% (95% CI = 85. 5%, 91. 6%) COAST Procedural 0. 0% 20. 0% 40. 0% 60. 0% Chambers JW, et al. JACC Cardiovasc Interv. 2014; 7: 510 -8. 80. 0% 100. 0% Success = 85. 0% (95% CI = 76. 5%, 91. 4%)
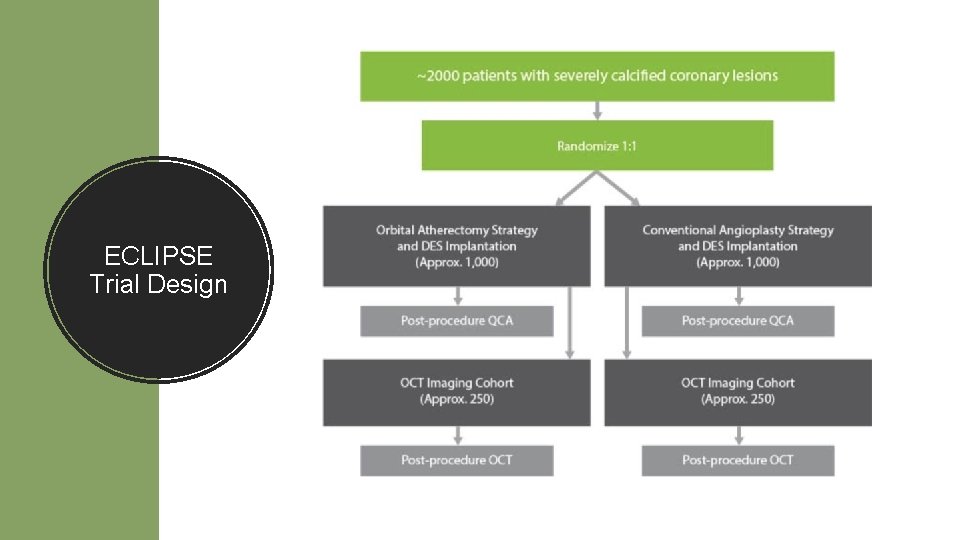
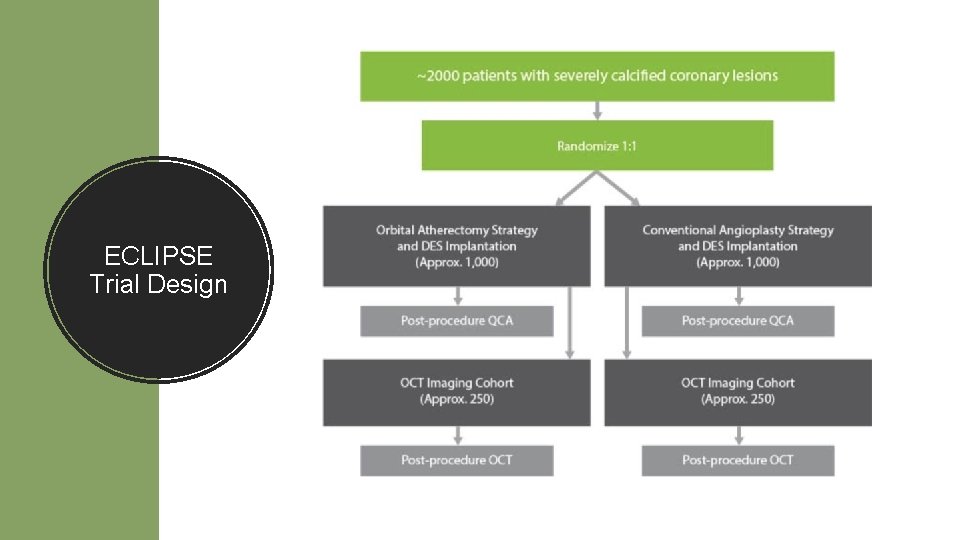
ECLIPSE Trial Design
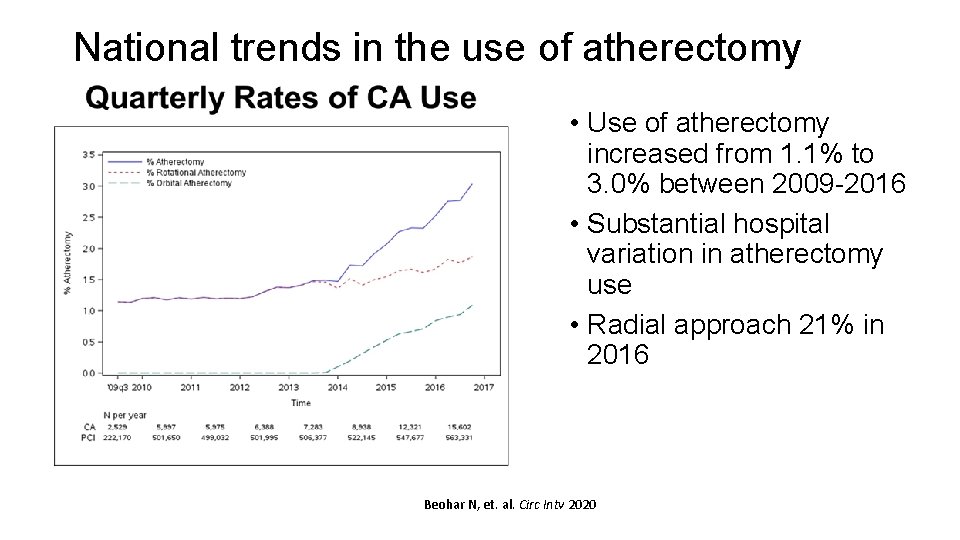
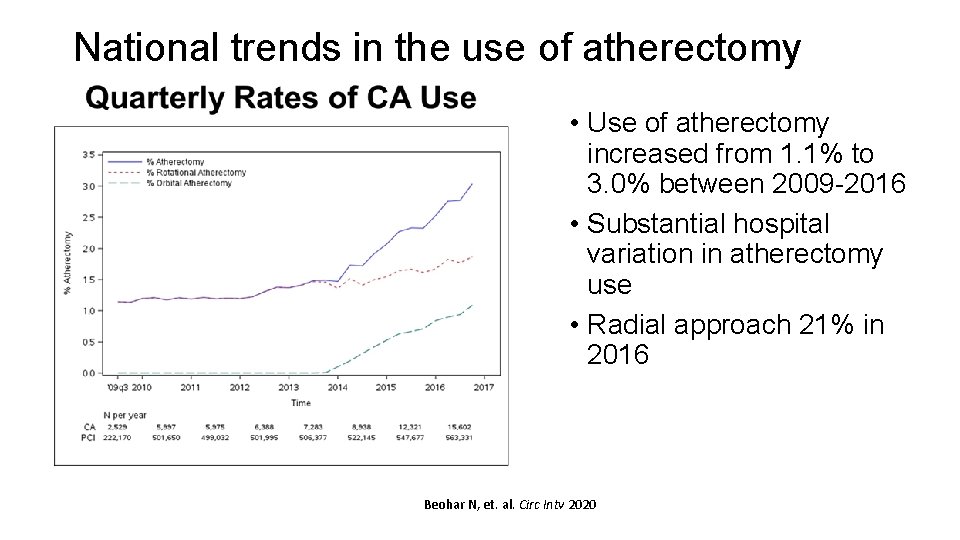
National trends in the use of atherectomy • Use of atherectomy increased from 1. 1% to 3. 0% between 2009 -2016 • Substantial hospital variation in atherectomy use • Radial approach 21% in 2016 Beohar N, et. al. Circ Intv 2020
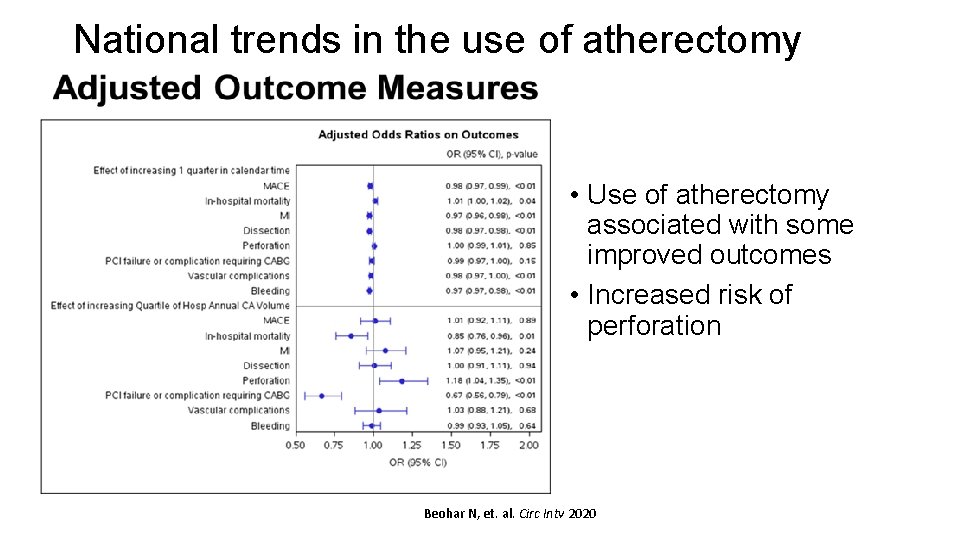
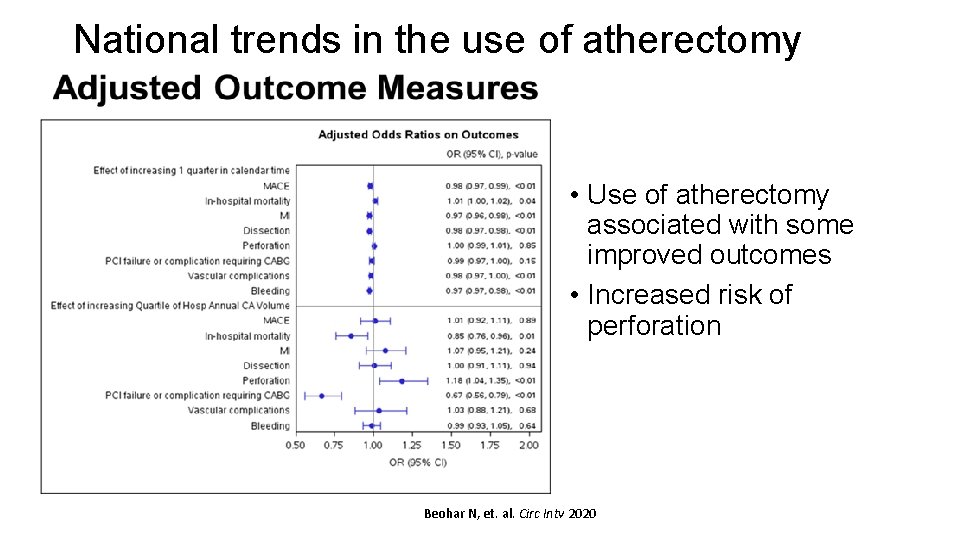
National trends in the use of atherectomy • Use of atherectomy associated with some improved outcomes • Increased risk of perforation Beohar N, et. al. Circ Intv 2020
Summary • Calcification significantly complicates PCI and compromises outcomes • Atherectomy addresses calcification and vessel compliance • Need more randomized data with contemporary DES platforms • Ongoing trials – ECLIPSE – will address the evidence gap • Until those are done, need to gain proficiency with technique to reduce complications
 Csi atherectomy setup
Csi atherectomy setup Web role in azure
Web role in azure Rollendistanz krappmann beispiel
Rollendistanz krappmann beispiel Statuses and their related roles determine
Statuses and their related roles determine Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới