Stroke and TIA Evaluations in Neurologically Underserved Regions
- Slides: 32
Stroke and TIA Evaluations in Neurologically Underserved Regions Ganesh Asaithambi, MD John Nasseff Neuroscience Specialty Clinic 11/8/18
Disclosures No relevant financial or competing interests
Objectives • Discuss current burden of stroke and TIA • Review acute evaluations for patients presenting with acute stroke symptoms • Identify methods of evaluation for stroke and TIA patients for secondary prevention
What is a stroke?
What is a transient ischemic attack (TIA)?
Background 795, 000 people in US have a stroke each year A stroke occurs every 40 seconds in the US Every 4 minutes a stroke-related death occurs Women between ages of 45 -54 are twice as likely to have and die from a stroke than breast cancer • Fifth leading cause of death in US • Leading cause of disability • • Benjamin EJ et al. Circulation 2018; 137: e 67 -e 492.
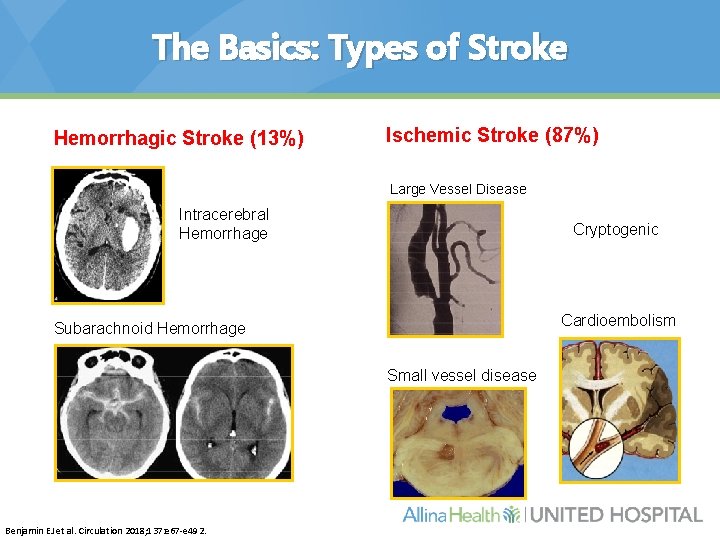
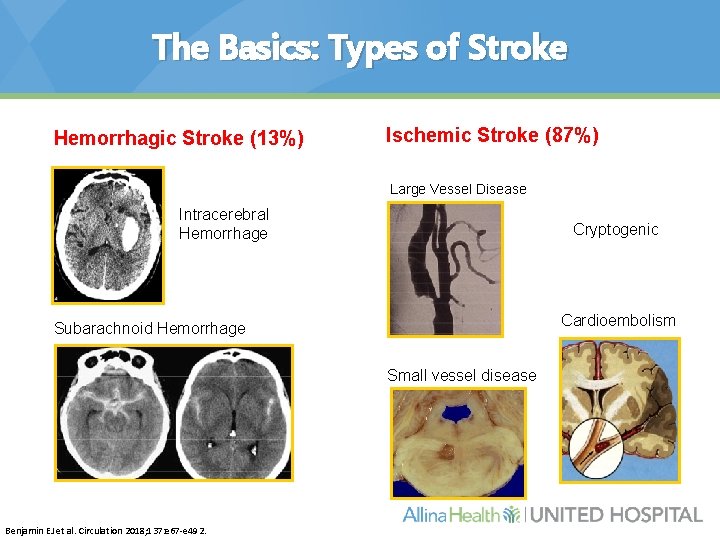
The Basics: Types of Stroke Hemorrhagic Stroke (13%) Ischemic Stroke (87%) Large Vessel Disease Intracerebral Hemorrhage Cryptogenic Cardioembolism Subarachnoid Hemorrhage Small vessel disease Benjamin EJ et al. Circulation 2018; 137: e 67 -e 492.
Stroke in Minnesota (2016) • ~2. 5% of adults in Minnesota reported ever having had a stroke in their lifetime – More than 100, 000 people • More than 5% of all deaths in Minnesota are due to stroke (2, 197 deaths in 2016) – Fifth-leading cause of death in the state • More than 11, 000 hospitalizations for acute stroke events • Ranked 11 th lowest for overall stroke mortality among states and District of Columbia • From 2010 -2016, stroke death rate is 26% higher in African. Americans and Asians compared to whites Minnesota Department of Health
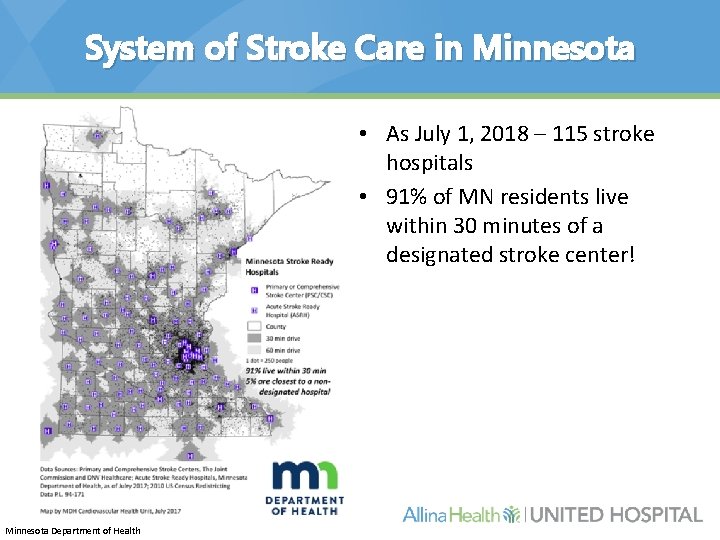
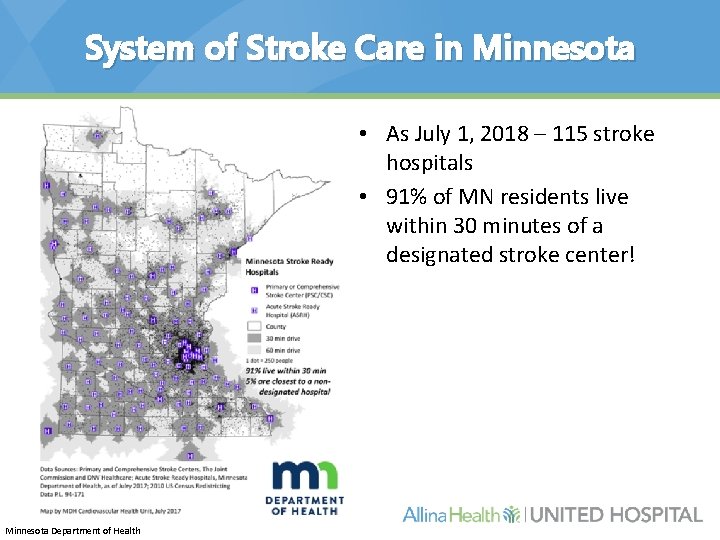
System of Stroke Care in Minnesota • As July 1, 2018 – 115 stroke hospitals • 91% of MN residents live within 30 minutes of a designated stroke center! Minnesota Department of Health
Transient Ischemic Attacks (TIAs) • • “Warning strokes” that can happen before a major stroke ~5 million Americans will experience a TIA Almost 10 times more likely to have a stroke Get a good history, rule out possible mimics – – – Seizure Hypo/hyperglycemia Migraine Conversion disorder/reaction Hypertensive encephalopathy Drug toxicity Benjamin EJ et al. Circulation 2018; 137: e 67 -e 492.
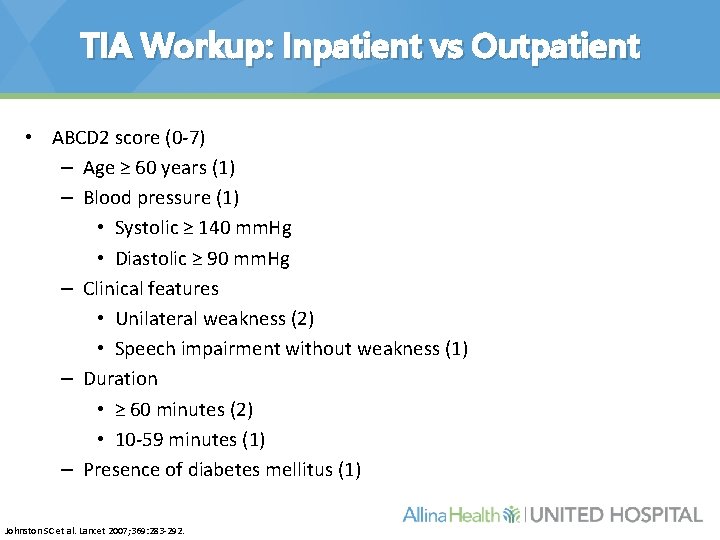
TIA Workup: Inpatient vs Outpatient • ABCD 2 score (0 -7) – Age ≥ 60 years (1) – Blood pressure (1) • Systolic ≥ 140 mm. Hg • Diastolic ≥ 90 mm. Hg – Clinical features • Unilateral weakness (2) • Speech impairment without weakness (1) – Duration • ≥ 60 minutes (2) • 10 -59 minutes (1) – Presence of diabetes mellitus (1) Johnston SC et al. Lancet 2007; 369: 283 -292.
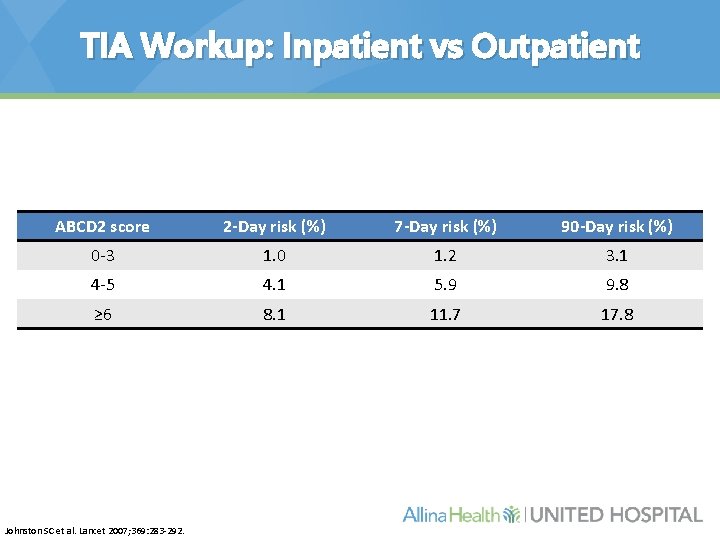
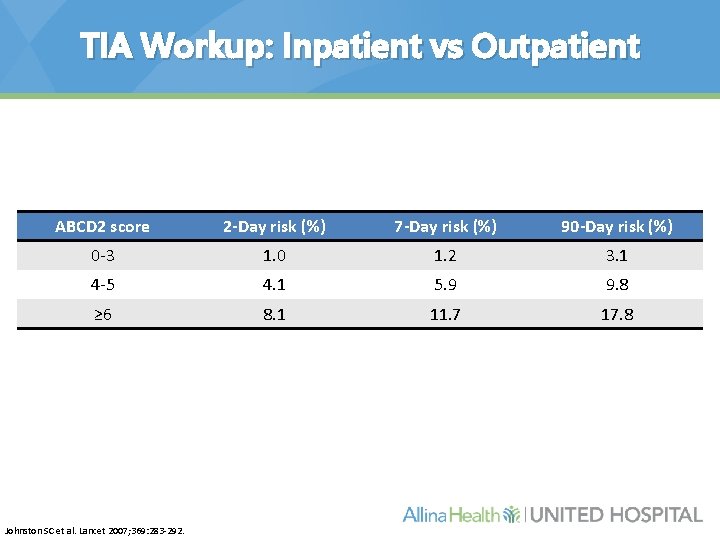
TIA Workup: Inpatient vs Outpatient ABCD 2 score 2 -Day risk (%) 7 -Day risk (%) 90 -Day risk (%) 0 -3 1. 0 1. 2 3. 1 4 -5 4. 1 5. 9 9. 8 ≥ 6 8. 1 11. 7 17. 8 Johnston SC et al. Lancet 2007; 369: 283 -292.
But first…
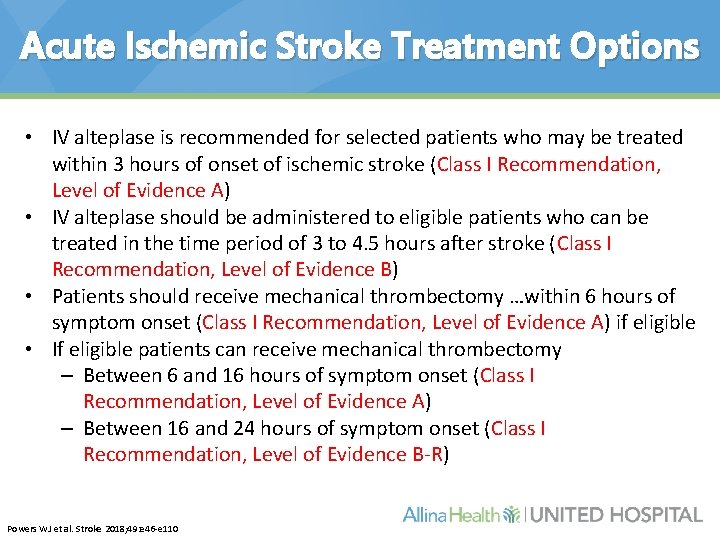
Acute Ischemic Stroke Treatment Options • IV alteplase is recommended for selected patients who may be treated within 3 hours of onset of ischemic stroke (Class I Recommendation, Level of Evidence A) • IV alteplase should be administered to eligible patients who can be treated in the time period of 3 to 4. 5 hours after stroke (Class I Recommendation, Level of Evidence B) • Patients should receive mechanical thrombectomy …within 6 hours of symptom onset (Class I Recommendation, Level of Evidence A) if eligible • If eligible patients can receive mechanical thrombectomy – Between 6 and 16 hours of symptom onset (Class I Recommendation, Level of Evidence A) – Between 16 and 24 hours of symptom onset (Class I Recommendation, Level of Evidence B-R) Powers WJ et al. Stroke 2018; 49: e 46 -e 110
Acute Ischemic Stroke Treatment Options • Because time from onset of symptoms to treatment has such a powerful impact on outcomes, treatment with IV alteplase should not be delayed to monitor further improvement (Class III Recommendation, Level of Evidence C-EO) Powers WJ et al. Stroke 2018; 49: e 46 -e 110
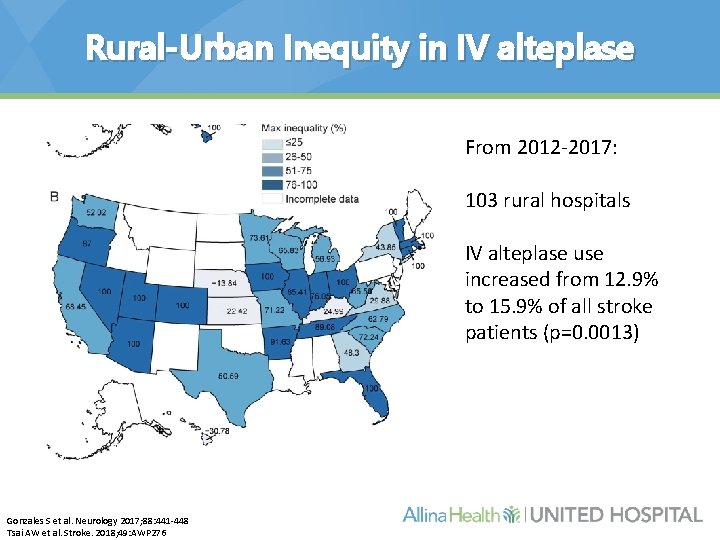
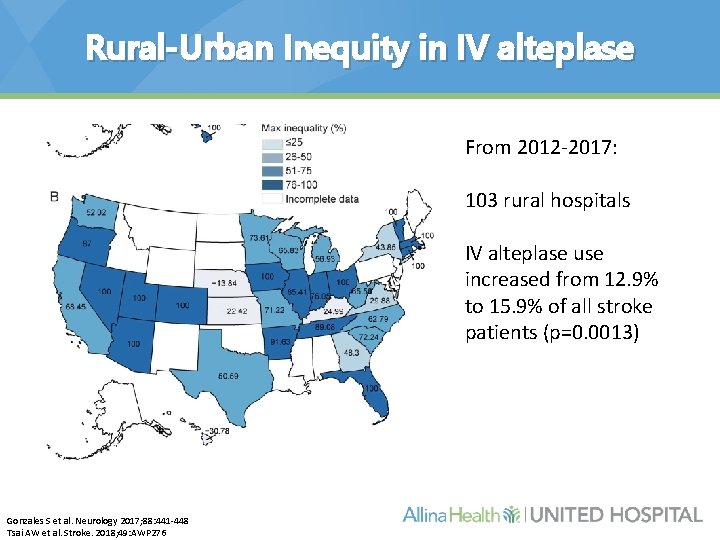
Rural-Urban Inequity in IV alteplase From 2012 -2017: 103 rural hospitals IV alteplase use increased from 12. 9% to 15. 9% of all stroke patients (p=0. 0013) Gonzales S et al. Neurology 2017; 88: 441 -448 Tsai AW et al. Stroke. 2018; 49: AWP 276
Work Up for the Stroke/TIA Patient
Cranial Imaging • Computed tomography (CT) head – Hemorrhage? – Can be negative in the first few hours with increased sensitivity several hours later – Early CT signs of ischemia confers worse prognosis Wardlaw JM et al. Radiology 2005; 235: 444 -453.
Cranial Imaging • Magnetic Resonance Imaging (MRI) – More sensitive that CT – Not as generalizable • Do you need to transfer the patient?
Vessel Imaging • Carotid Dopplers • MRA/CTA – Extra- and intracranial vasculature • Digital subtracted angiography – Gold standard
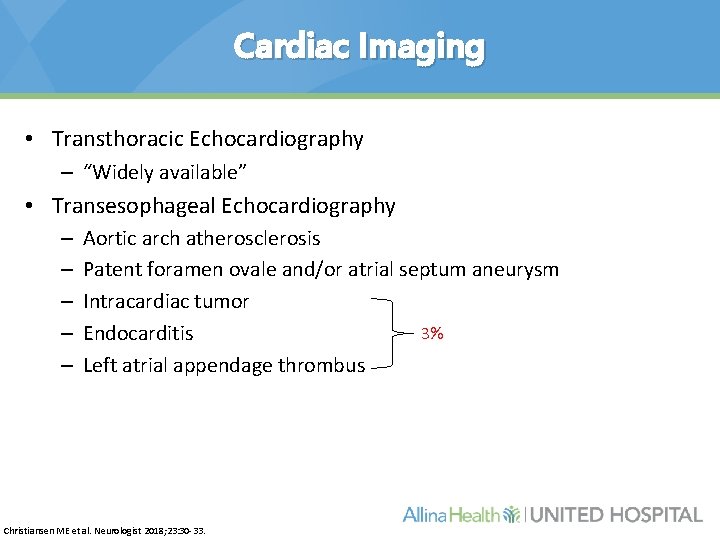
Cardiac Imaging • Transthoracic Echocardiography – “Widely available” • Transesophageal Echocardiography – – – Aortic arch atherosclerosis Patent foramen ovale and/or atrial septum aneurysm Intracardiac tumor 3% Endocarditis Left atrial appendage thrombus Christiansen ME et al. Neurologist 2018; 23: 30 -33.
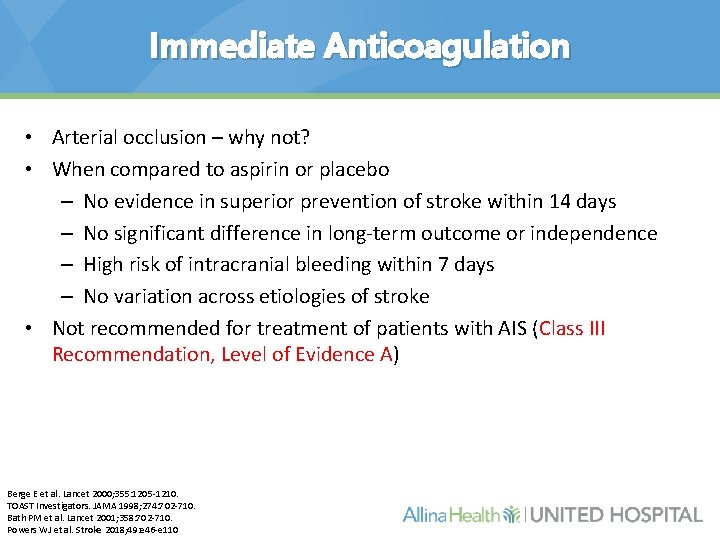
Immediate Anticoagulation • Arterial occlusion – why not? • When compared to aspirin or placebo – No evidence in superior prevention of stroke within 14 days – No significant difference in long-term outcome or independence – High risk of intracranial bleeding within 7 days – No variation across etiologies of stroke • Not recommended for treatment of patients with AIS (Class III Recommendation, Level of Evidence A) Berge E et al. Lancet 2000; 355: 1205 -1210. TOAST Investigators. JAMA 1998; 274: 702 -710. Bath PM et al. Lancet 2001; 358: 702 -710. Powers WJ et al. Stroke 2018; 49: e 46 -e 110
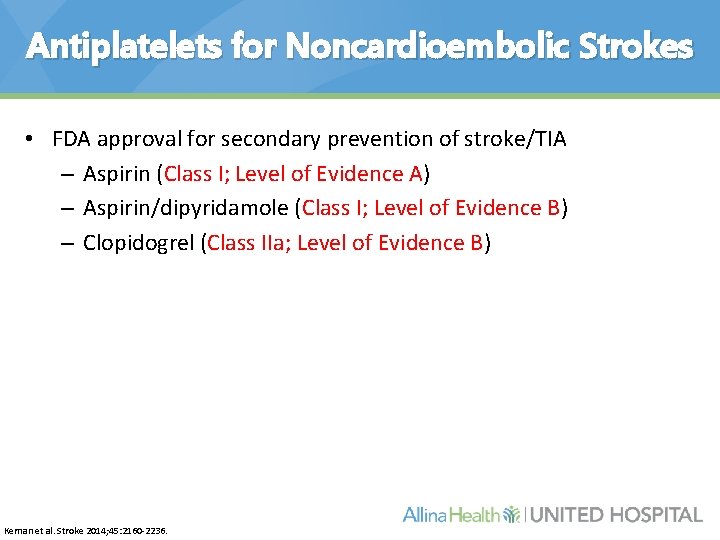
Antiplatelets for Noncardioembolic Strokes • FDA approval for secondary prevention of stroke/TIA – Aspirin (Class I; Level of Evidence A) – Aspirin/dipyridamole (Class I; Level of Evidence B) – Clopidogrel (Class IIa; Level of Evidence B) Kernan et al. Stroke 2014; 45: 2160 -2236.
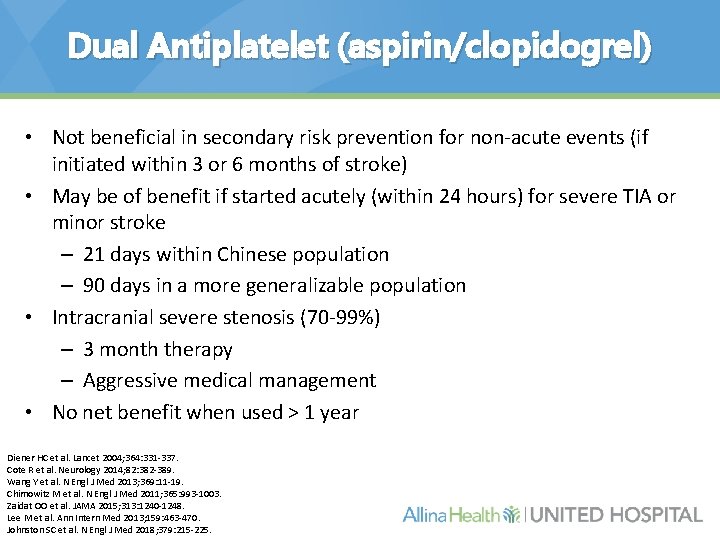
Dual Antiplatelet (aspirin/clopidogrel) • Not beneficial in secondary risk prevention for non-acute events (if initiated within 3 or 6 months of stroke) • May be of benefit if started acutely (within 24 hours) for severe TIA or minor stroke – 21 days within Chinese population – 90 days in a more generalizable population • Intracranial severe stenosis (70 -99%) – 3 month therapy – Aggressive medical management • No net benefit when used > 1 year Diener HC et al. Lancet 2004; 364: 331 -337. Cote R et al. Neurology 2014; 82: 382 -389. Wang Y et al. N Engl J Med 2013; 369: 11 -19. Chimowitz M et al. N Engl J Med 2011; 365: 993 -1003. Zaidat OO et al. JAMA 2015; 313: 1240 -1248. Lee M et al. Ann Intern Med 2013; 159: 463 -470. Johnston SC et al. N Engl J Med 2018; 379: 215 -225.
Long-term Anticoagulation • Warfarin – Atrial fibrillation (Class I; Level of Evidence A) – Mechanical aortic or mitral valve (Class I; Level of Evidence B/C) – Intracardiac thrombus (Class I; Level of Evidence C) – Left ventricular assist device (Class IIa; Level of Evidence C) – Cardiomyopathy with ejection fraction < 35% (Class IIb; Level of Evidence B) – Rheumatic mitral valve disease (Class IIb; Level of Evidence C) Kernan et al. Stroke 2014; 45: 2160 -2236.
Direct Oral Anticoagulants • Nonvalvular atrial fibrillation – Apixaban – Rivaroxaban – Dabigatran – Edoxaban
Outpatient Arrhythmia Monitoring • Current duration of outpatient monitoring is undetermined – At least 24 hours upon admission for stroke • External monitors – 7 -, 14 -, 28 -, and 30 -day monitors • Insertable monitors – Up to 3 years Jauch E et al. Stroke 2013; 44: 870 -947.
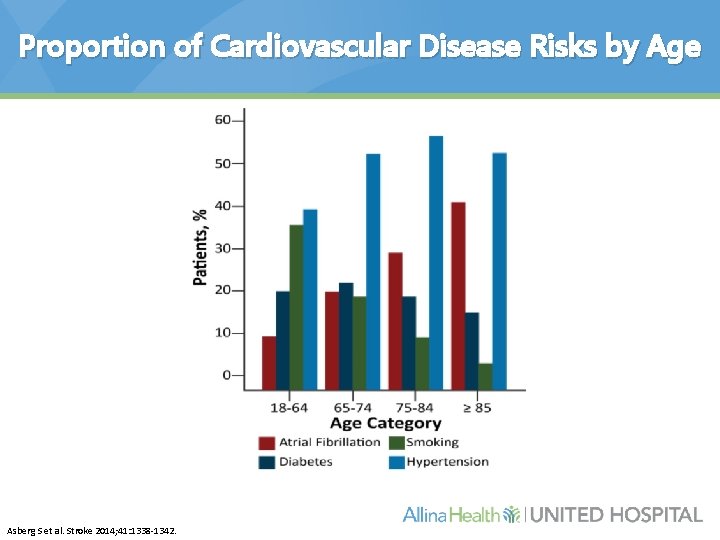
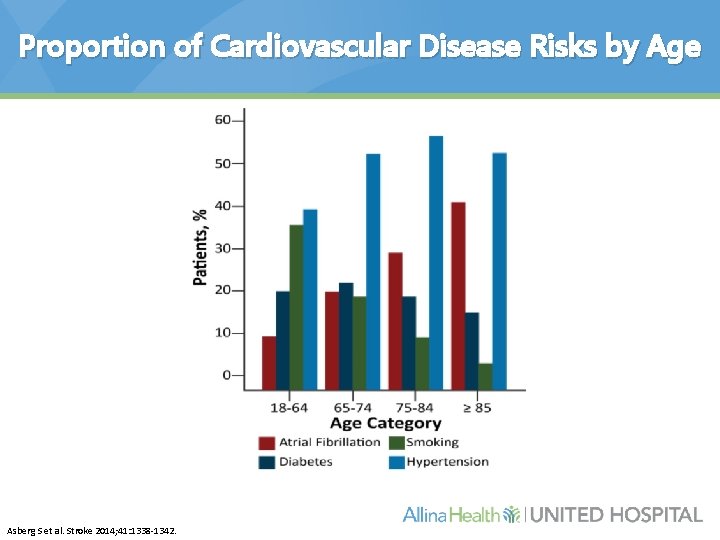
Proportion of Cardiovascular Disease Risks by Age Asberg S et al. Stroke 2014; 41: 1338 -1342.
Lipid Management • High dose atorvastatin – Prior stroke or TIA – Reduction in recurrent stroke completed with placebo SPARCL Investigators. N Engl J Med 2006; 355: 549 -559.
Blood Pressure Control
“Basic Work Up” • • CT head Carotid Dopplers TTE Lipids Hemoglobin A 1 c Screening labs (PT/INR) Electrocardiogram
Conclusions • Not all patients need to be transferred to a “larger” hospital for stroke/TIA work up • Confer with a neurologist when you can – Strokes are not all the same • Patients presenting with acute stroke symptoms to the emergency department should still be considered for acute stroke treatments