SHOCK NURS 211 GAIL L LUPICA PHD RN
![CICULATORY SHOCK A life-threatening condition that occurs due to inadequate oxygen. [2] CICULATORY SHOCK A life-threatening condition that occurs due to inadequate oxygen. [2]](https://slidetodoc.com/presentation_image_h2/044fde0ed3cea909aceb67869882d3ad/image-9.jpg)





- Slides: 36
SHOCK NURS 211 GAIL L LUPICA PHD, RN, CNE
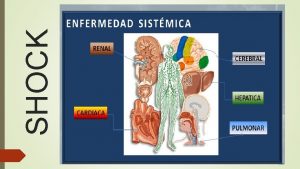
SHOCK FAILURE OF THE CIRCULATORY SYSTEM TO MAINTAIN ADEQUATE PERFUSION OF VITAL ORGANS.
PERFUSION WHAT’S PERFUSION ANYWAY?
PERFUSION YES! BLOOD FLOW! SO IN THE SHOCK STATE THERE IS NOT DELIVERY OF THE OXYGEN, ELECTROLYTES, PROTEINS, FLUIDS, AND HORMONES…. T H A T Y O U R CELLS NEED
NO PERFUSION? キ Without adequate perfusion, oxygenation is compromised, and anaerobic metabolism will take place.
METABOLIC ACIDOSIS The by-product of anaerobic metabolism is lactic acid. A metabolic acidosis ensues. Also, when there is inadequate tissue perfusion, waste products of cellular metabolism accumulate (CO 2).
7. 35 -7. 45 Remember what ph our body cells function best at? 7. 35 - 7. 45
ACIDOSIS LEADS TO CELL DEATH. When acidosis occurs, and ph level fall below 7. 35 for an extended period. Cell & then organ death occur.
![CICULATORY SHOCK A lifethreatening condition that occurs due to inadequate oxygen 2 CICULATORY SHOCK A life-threatening condition that occurs due to inadequate oxygen. [2]](https://slidetodoc.com/presentation_image_h2/044fde0ed3cea909aceb67869882d3ad/image-9.jpg)
CICULATORY SHOCK A life-threatening condition that occurs due to inadequate oxygen. [2]
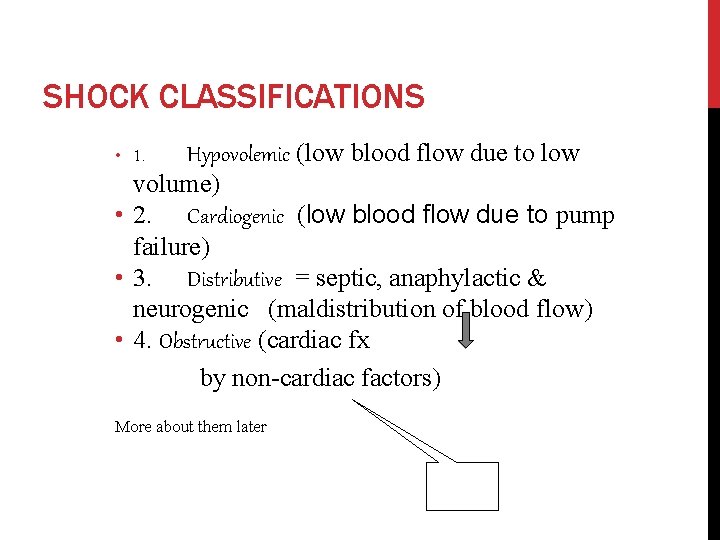
SHOCK CLASSIFICATIONS Shock can be divided into four major classifications:
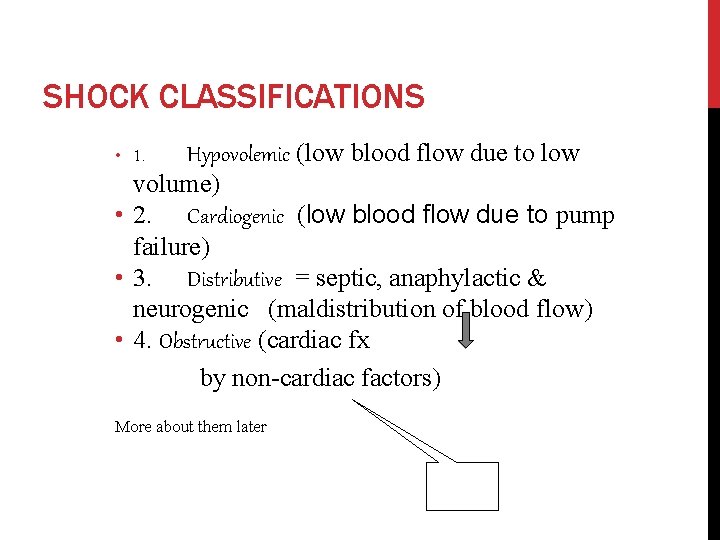
SHOCK CLASSIFICATIONS Hypovolemic (low blood flow due to low volume) • 2. Cardiogenic (low blood flow due to pump failure) • 3. Distributive = septic, anaphylactic & neurogenic (maldistribution of blood flow) • 4. Obstructive (cardiac fx by non-cardiac factors) • 1. More about them later
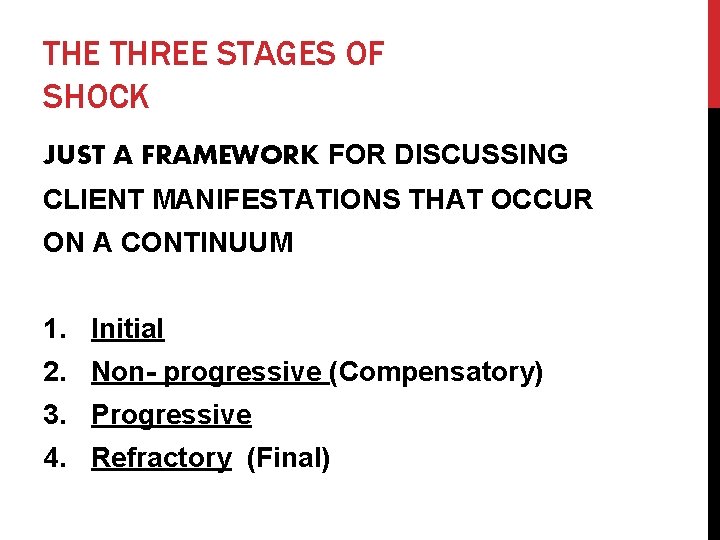
THE THREE STAGES OF SHOCK JUST A FRAMEWORK FOR DISCUSSING CLIENT MANIFESTATIONS THAT OCCUR ON A CONTINUUM 1. Initial 2. Non- progressive (Compensatory) 3. Progressive 4. Refractory (Final)
INITIAL STAGE Patient may NOT have any clinical manifestations of. Tissue perfusion. Lack of oxygen is occurring at the cellular level May have a HR will . in MAP. 5 -10 mm. HG
NON- PROGRESSIVE STAGE (COMPENSATORY) • Compensatory mechanisms kick in to maintain BP and perfusion. (A diminishing CO sets this in motion. ) • MAP falls 10 -15 mm. Hg • HOW is that done? – 2 systems
NON- PROGRESSIVE STAGE (COMPENSATORY) • 1. Autonomic Nervous System (ANS) • 2. Renin Angiotensin Aldosterone System (RAA)
NON- PROGRESSIVE STAGE (COMPENSATORY) Autonomic Nervous System “presso receptors” in the carotids and aortic arch sense a falling BP. Signals are sent (from hypoth) to adrenal medulla in order to release norepinephrine & epinephrine. Signals are sent (from hypoth) to adrenal cortex to release cortisol. .
NON- PROGRESSIVE STAGE (COMPENSATORY) Autonomic Nervous System What effect will these catecholamines have on: vasculature? HR? Contractility? Blood flow to the myocardium and the brain?
NON- PROGRESSIVE STAGE (COMPENSATORY) Autonomic Nervous System A decrease in ph (due to lactic acidosis & (hypoventilation)) is sensed by “chemo receptors” (chemo=chemical receptors) in the carotids and aortic arch. Signals are transmitted to the Respiratory center in the medulla. What effect does this have?

NON- PROGRESSIVE STAGE (COMPENSATORY) Renin Angiotensin Aldosterone System
NON- PROGRESSIVE STAGE (COMPENSATORY) Decreased blood flow to the kidney is sensed by the juxtaglomerular receptor. In turn renin (a hormone) is released. Renin reacts with Angiotensinogen (from the liver) and produces Angiotensin I is converted to Angiotensin II (by a converting enzyme in the lung) Angiotensin II is a potent vasoconstrictor. BP is raised!
NON- PROGRESSIVE STAGE (COMPENSATORY) Renin Angiotensin Aldosterone System It also stimulates Aldosterone release from the Adrenal cortex (which causes reabsorption of Na+ and water. This will increase circulating fluid volume, and therefore raise blood pressure) • In addition ADH is released from posterior pituitary because of signals received from hypothalamus to hold on to body water (to maintain BP)
CRITICAL THINKING ? ? ? ? ? ? NON- PROGRESSIVE STAGE (COMPENSATORY)? ?
? ? ? ? NON- PROGRESSIVE STAGE (COMPENSATORY)? ? Will his respiratory rate be increased or decreased? Why? What effect will this response have on the ABG initially? Will he be hypotensive, normotensive, or hypertensive? Why? Will his urine output be maintained? Why or why not?
? ? ? NON- PROGRESSIVE STAGE (COMPENSATORY)? ? ? ? What will the appearance of his skin be? Why? Will his blood sugar be affected? Why, Why not?

PROGRESSIVE • Compensatory Mechanisms are no longer able to compensate for decreased cardiac output. MAP falls > 20 -mm. Hg Massive organ hypoperfusion develops. What would that look like?
PROGRESSIVE How are organ systems adversely affected? • Respiratory system. • Hypoperfusion to pulmonary capillary bed caused alveolar cells to become ischemic & unable to produce surfactant. • Cardiovascular system • (Heme) Disseminated Intravascular Coagulation

PROGRESSIVE How are organ systems adversely affected? Renal System. (acute tubular necrosis Hepatic System o An impaired ability to detoxify Neurological System GI System. *****************
REFRACTORY (FINAL) • Body is refractory to all therapeutic measures. • It is irreversible Death is imminent.
LET’S TAKE A LOOK BG is a 62 year old woman who came through the ER c/o “not feeling well”. SHe has a medical history of COPD and very recent surgical history of “small bowel obstruction/lysis of adhesions”. What are your immediate interventions? You find that his BP is 112/60, HR 90, RR 24, temp 100. 4. Pulse ox is 94% on room air. What are your thoughts here? You apply oxygen at 3 l/min via nasal cannula. You start 2 IV s (one in left arm and one in right antecubital) and begin infusion of. 9% Normal Saline at 100 ml/hr. Continuous EKG monitoring is in place, as is a continuous pulse ox and NBP set for every 10 minutes. CBC and CMP are sent.

BG
40 MINUTES LATER… BG is becoming dyspneic. Her BP is alarming and coming up at 100/40, HR 100, RR 30. Pulse ox is at 90% on 3 l/min nasal cannula. What are your thoughts? What should be done? SHe pt is place on a NRB mask at 100% while RT is being paged. Blood cultures, and ABGs are sent. Foley is inserted to down drain. A CVP monitor is inserted via the right IJ. Her pulse ox begins to drop to 84% and the decision is made to intubate. Her BP is 88/38. What is going on here?
ANOTHER 40 MINUTES LATER
WHAT IS BG’S PICTURE? Now BG is intubated and being mechanically ventilated on assist control. SHe has propofol at 4. 7 mcg/kg/min (20 ml/hr), Fentanyl at 10 mcg/hr (1 ml/hr), Tobramycin at 100 ml/hour in a 50 ml bag, Levophed at 30 mcg/kg/hr. LR at 150/hr. Her BP is 82/40, HR 114, RR 10/8, T 101. 2. You see little purplish bruises on her. Left forearm, that looks like pethechia. Her ABG ph- 7. 03 CO 2 - 58 Pa. O 2 -48 HCO 3 - -18 lactate level 9 mmom/l. WBC- 14. CVP -2 Give the rationale for each of the pt’s gtts. What is her MAP? Where should her CVP be? Interpret her ABG. Where will you look to see if the pt is getting adequate perfusion to her tissues/organs? What labs will you check? ?
45 MINUTES AFTER THAT The decision was made to begin a vasopressin infusion at 0. 04 u/min in addition to the Levophed still at 30 mcg/kg/min. LR infusion was increased to 200 ml/hour and a Zosyn infusion was begun. The pt was transferred to the MICU. What report will you give the nurse accepting the pt in the MICU.

BG TO MICU NOW!!!
 Gail lupica
Gail lupica Cne
Cne Gail lupica
Gail lupica Choleycystitis
Choleycystitis Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Cauda equina vs conus medullaris
Cauda equina vs conus medullaris Subacute combined degeneration of the cord
Subacute combined degeneration of the cord Shock normovolemico
Shock normovolemico Nurs 425
Nurs 425 Nurs 425
Nurs 425 Nurs 200
Nurs 200 Nefritis lupica clasificacion
Nefritis lupica clasificacion Anemia lupica
Anemia lupica Percusion renal
Percusion renal Re starter
Re starter Dr gail busby
Dr gail busby Gail herrine
Gail herrine Gail howard
Gail howard Gail cheramie
Gail cheramie Parsons gail model
Parsons gail model Macro vs micro sociology
Macro vs micro sociology Gail billingsley
Gail billingsley Shattering glass gail giles summary
Shattering glass gail giles summary Gail rankin
Gail rankin Gail khan
Gail khan Mara runs faster than gail
Mara runs faster than gail Gail langellotto
Gail langellotto Gail cheramie
Gail cheramie Gail's voucher
Gail's voucher Barbara gail montero
Barbara gail montero Small ideas big impact
Small ideas big impact Gail van tatenhove
Gail van tatenhove Organic analogy parsons
Organic analogy parsons Gail knudson
Gail knudson The planets by gail gibbons
The planets by gail gibbons Gail palmer
Gail palmer