Adult Respiratory Distress Syndrome Gail Lupica Ph D
- Slides: 22
Adult Respiratory Distress Syndrome Gail Lupica Ph. D, RN, CNE Nurs 211
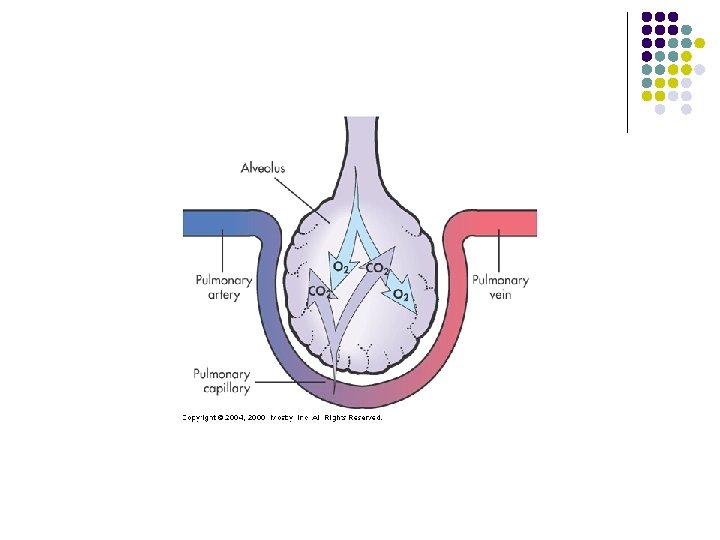
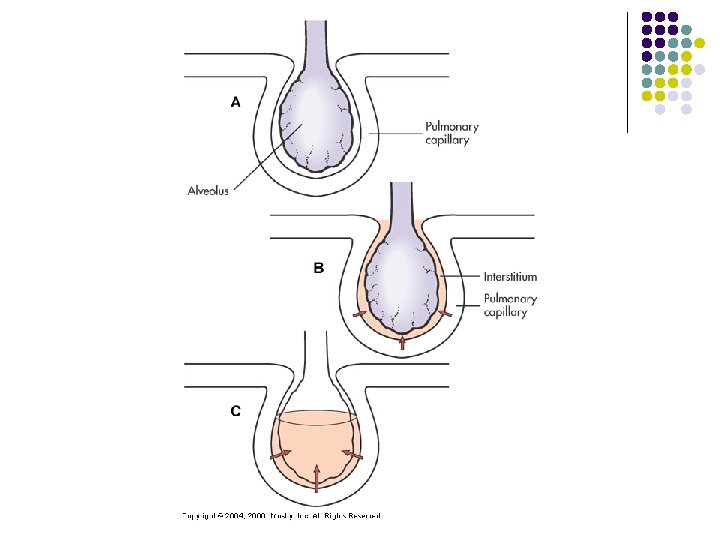
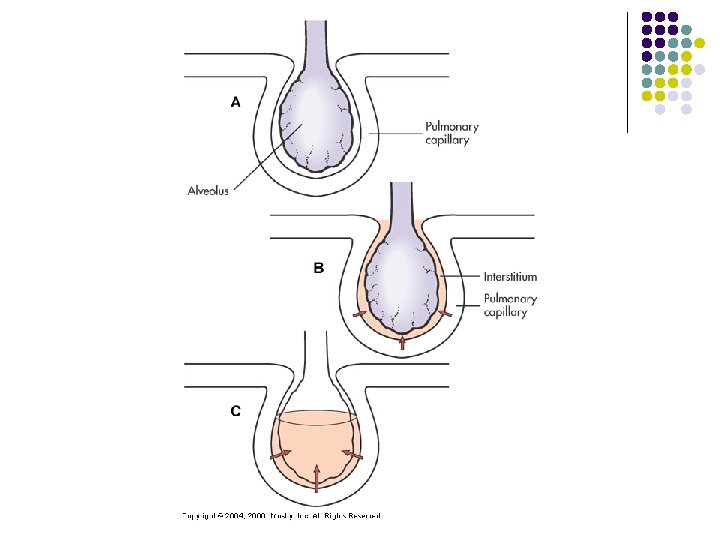
ARDS simply stated, is pulmonary edema. We are familiar with pulmonary edema due to cardiogenic causes. You learned when a patient’s heart fails, they have “CHF”. Fluid is forced backward into their pulmonary veins and capillaries.
l l ARDS is pulmonary edema that is non-cardiac in origin. Either the alveoli get damaged directly due to some trauma (near drowning or smoke inhalation or contusion), or indirectly from the blood passing through the pulmonary capillary bed filled that is filled with some toxic substance that damages the capillaries/vessels.
l An inflammatory response is triggered. When an inflammatory response occurs it changes the permeability of the involved tissue.
l Once alveoli are filled with fluid, not only is there an inability for gas exchange to occur, but also there is a blockage of surfactant production. Surfactant production is inadequate from a fluid filled alveoli. What is surfactant?
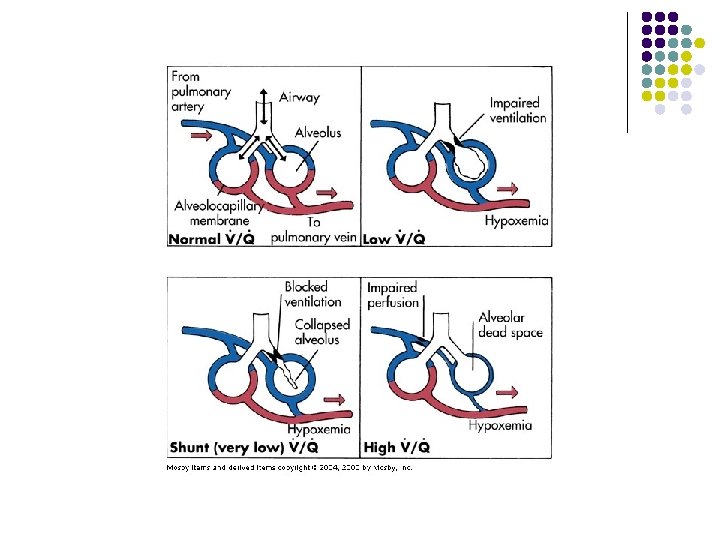
Initially, the patient’s response to this acute hypoxemia is to increase their respiratory rate. Their compensatory mechanisms kick in to try to correct the hypoxemia. l What do you think their ABG will look like? l
l Mechanical Ventilation is needed! Because their alveoli are filled with fluid their need for higher levels of supplemental oxygen increases. But, the alveoli are collapsed and adequate gas exchange cannot occur.
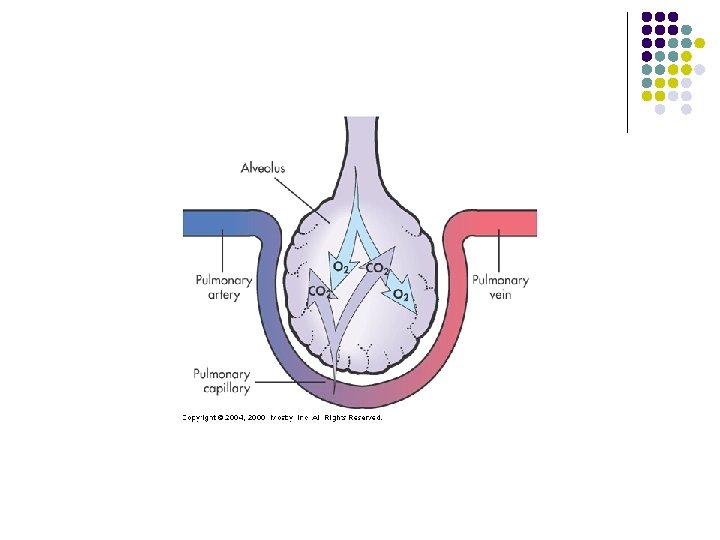
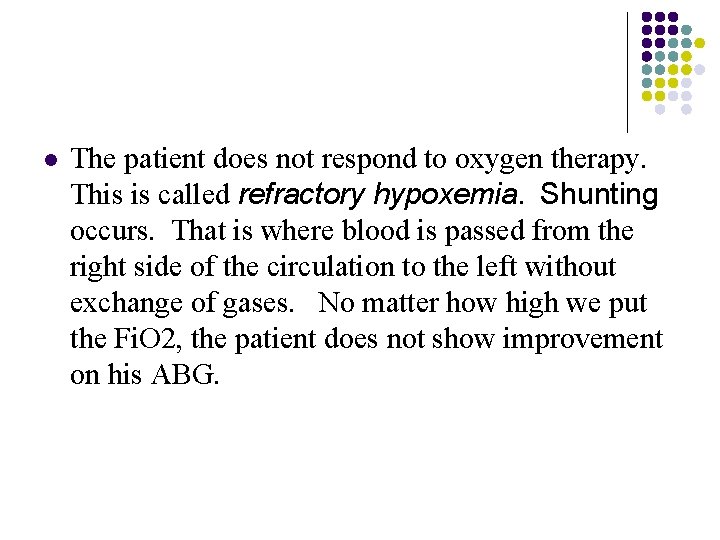
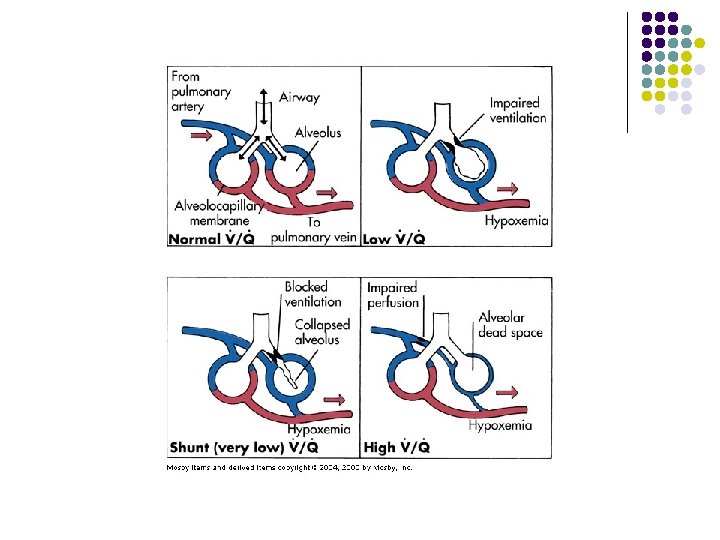
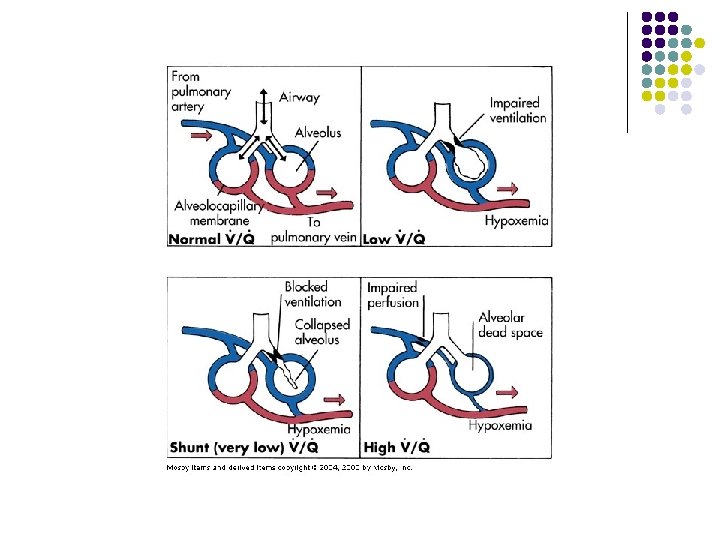
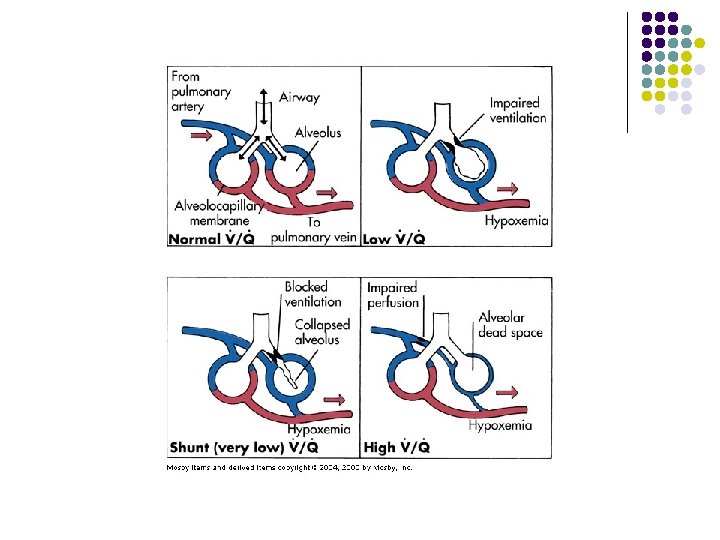
l The patient does not respond to oxygen therapy. This is called refractory hypoxemia. Shunting occurs. That is where blood is passed from the right side of the circulation to the left without exchange of gases. No matter how high we put the Fi. O 2, the patient does not show improvement on his ABG.
l Should we give the patient more and more oxygen? Why/Why not? l What is oxygen toxicity? How/When does it occur?
PEEP l A treatment that’s commonly used for this is Positive End Expiratory Pressure (PEEP). PEEP is something we can dial in on the vent. It is a pressure that we set that is left in our alveoli at the end of exhalation. In other words, our alveoli are “forced” to stay open with the pressure that is set.
PEEP l The higher we go with the PEEP, the greater the expansion of our alveoli. This is a good thing when we are not responding to oxygen therapy because when we inflate our alveoli, it allows a greater surface area for gas exchange. We can get better gas exchange with a comparable Fi. O 2.
PEEP l What happens when the patient gets too much PEEP?
l l Always keep in mind that your overall goal for the ARDS patient is to maintain functional vital organs while this underlying pathology resolves. Nutrition is extremely important. Parenteral nutrition that is high in protein and calories will prevent catabolism of the muscles of ventilation due to increased metabolic needs. Why not high in carbohydrates?
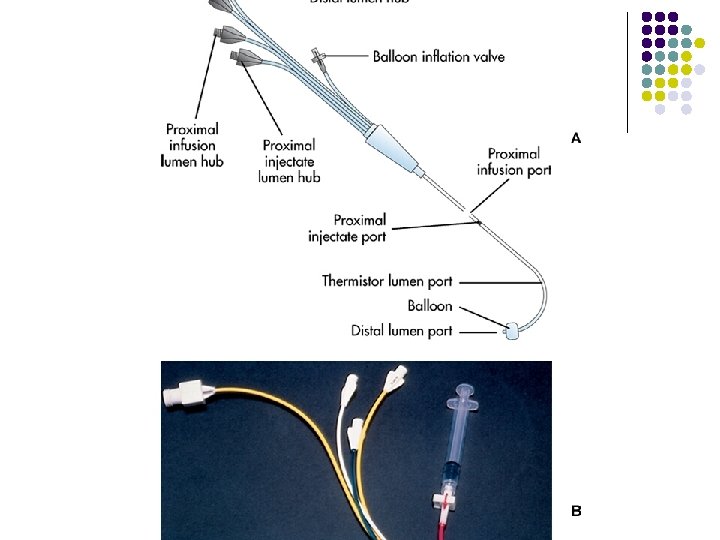
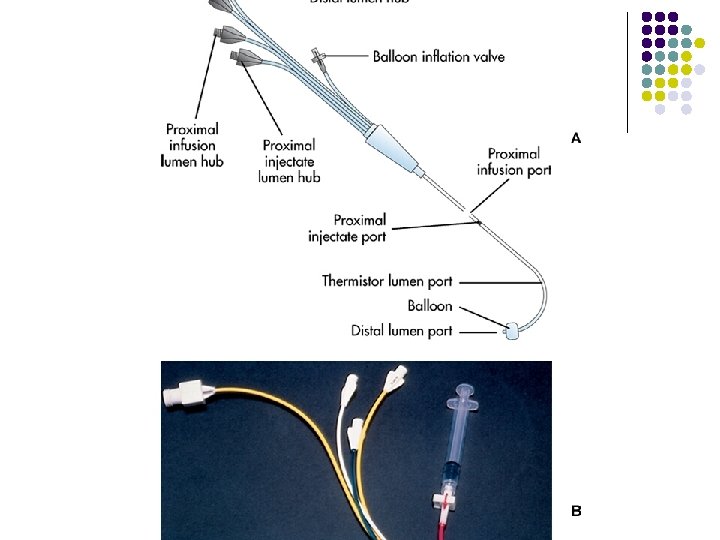
ARDS l l Sedation or paralysis Why? Fluid resuscitation is tricky Why? Carefully monitor your hourly urine outputs. Why? Invasive hemodynamic monitoring with a Swan Ganz catheter can give you the most precise information regarding fluid volume status, and cardiac function.
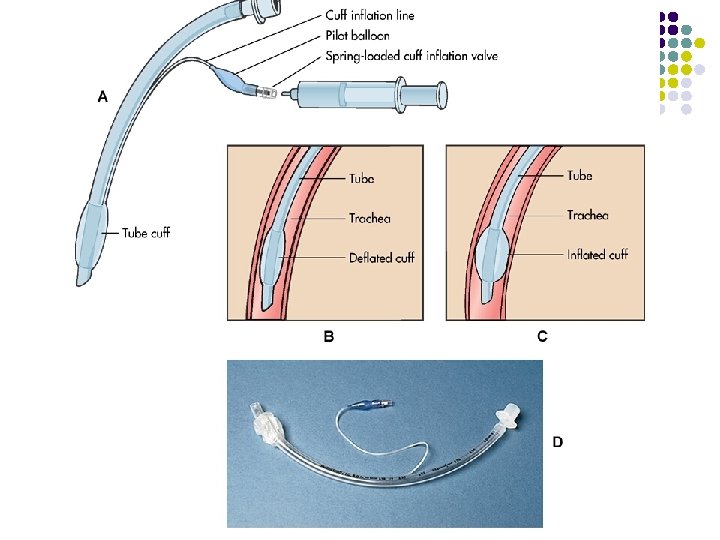
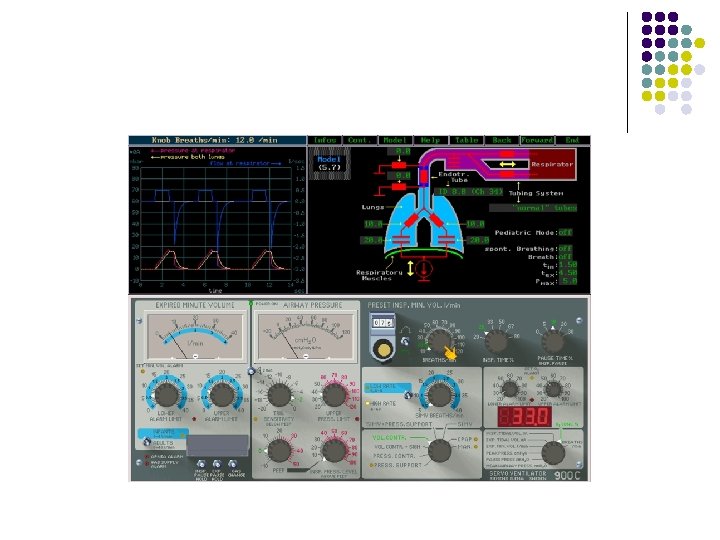
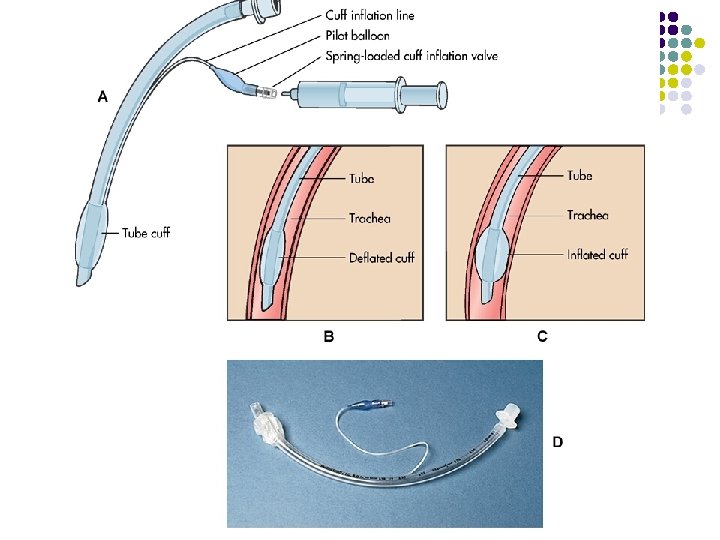
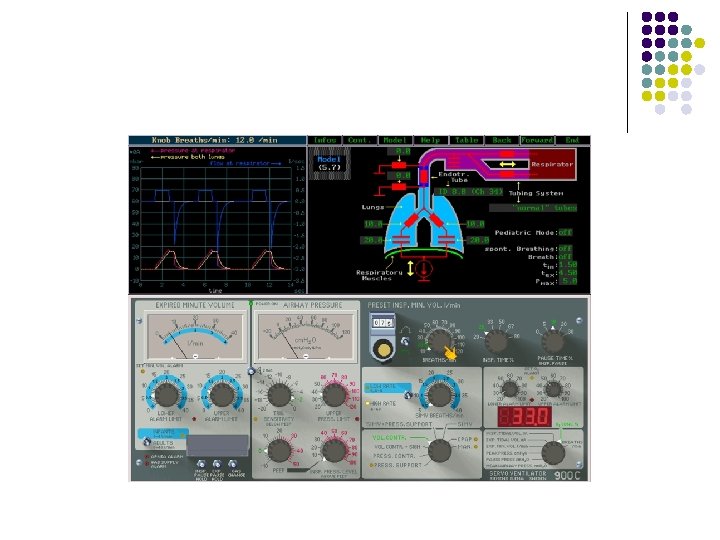
Mechanical Ventilation l Lets review the ventilator.