Scoutmaster and Assistant Scoutmaster Outdoor Skills Training First







- Slides: 80

Scoutmaster and Assistant Scoutmaster Outdoor Skills Training First Aid
Goals By the end of this session, participants will be able to: • Shape their attitudes and approach to first-aid situations • Define first aid and explain what a first aid plan is • Describe a systematic approach to first aid • Assemble a first-aid kit that includes items for specific injuries • Explain the considerations for first aid in pre-trip planning
Disclaimer I acknowledge: 1. Many of you have had first aid training 2. There may be different ways to do things But…. . We’re going to go over what BSA wants us to teach our Scouts

What is First Aid? The first help given to a victim of an accident or other health emergency. First Aid should: • Stop life-threatening dangers • Protect an injured or ill person from further harm • Get proper medical help for the victim
Systematic Approach to Teaching First Aid • As the Scouts work on the requirements for Tenderfoot, Second Class, and then First Class we build upon their first aid skills • This is not necessarily the way we approach a victim, but it is a good way to build the skills of the Scout
Tenderfoot Requirements Requirement 11 Identify local poisonous plants; tell how to treat exposure to them Requirement 12 a. Show to care for someone who is choking
Tenderfoot Requirements Requirement 12 b. Show first aid for the following: • • Simple cuts and scrapes Blisters on the hand foot Minor (thermal/heat) burns or scalds Bites or stings of insects and ticks Venomous snakebite Nosebleed Frostbite and sunburn
Poisonous Plants • Oily sap from the plant causes a reaction on the skin • It usually takes 10 – 20 minutes on the skin to cause the rash • Prevention—wash the skin with soap and water if you have a known exposure • Don’t forget the sap can be on clothes and shoes
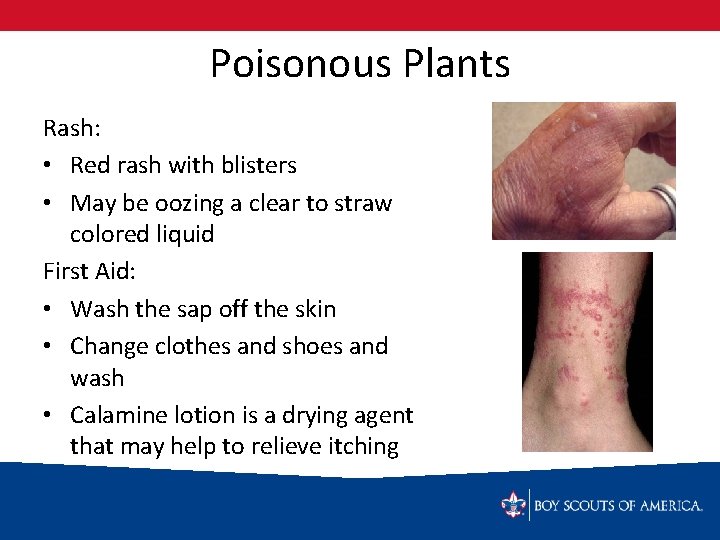
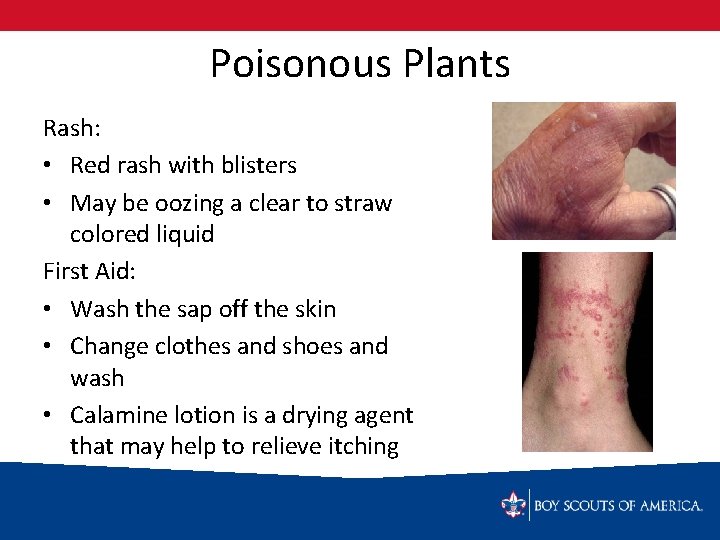
Poisonous Plants Rash: • Red rash with blisters • May be oozing a clear to straw colored liquid First Aid: • Wash the sap off the skin • Change clothes and shoes and wash • Calamine lotion is a drying agent that may help to relieve itching
Choking Universal symbol for choking: First Aid: 1. Ask, “Are you choking? ” 2. If the person can speak, cough, or breathe: – Encourage them to keep coughing and trying to get the object up – Have someone call for help
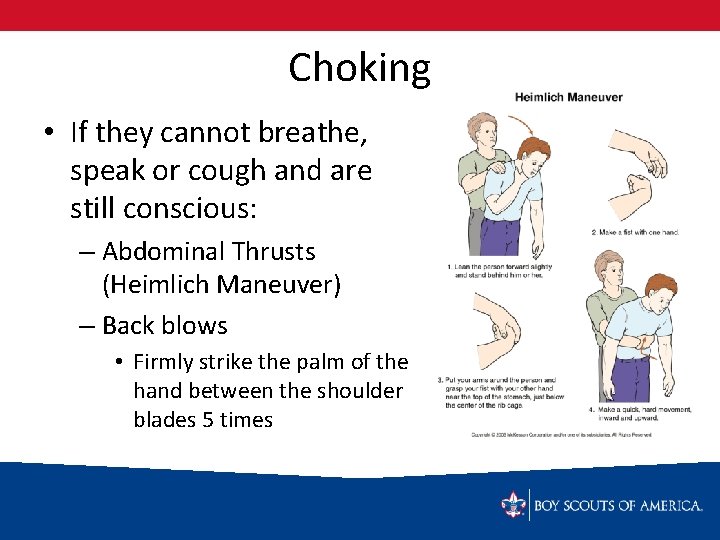
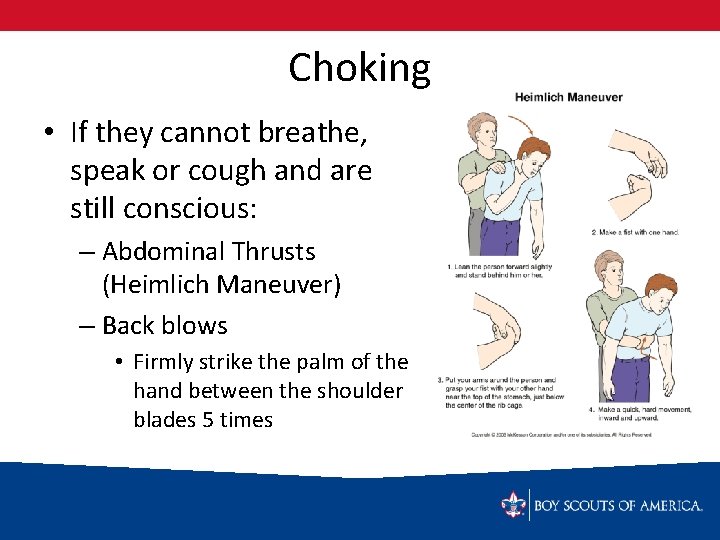
Choking • If they cannot breathe, speak or cough and are still conscious: – Abdominal Thrusts (Heimlich Maneuver) – Back blows • Firmly strike the palm of the hand between the shoulder blades 5 times
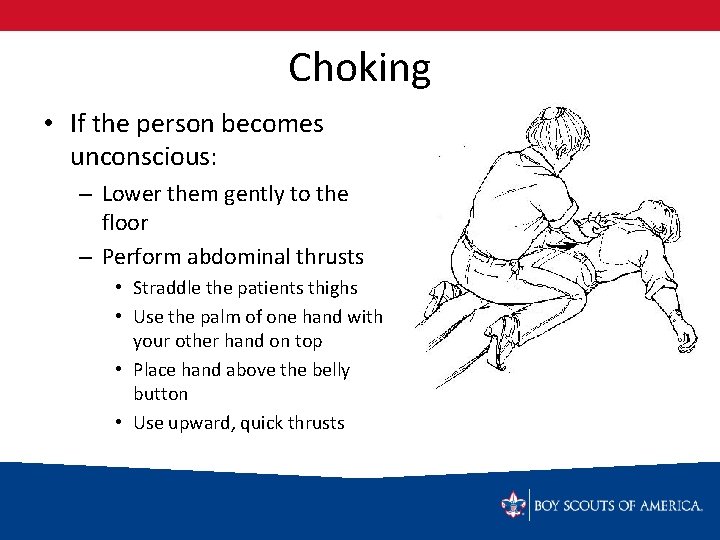
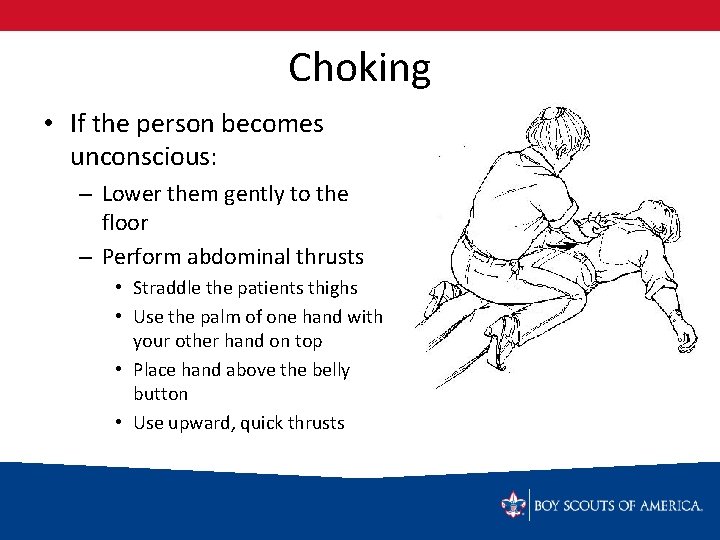
Choking • If the person becomes unconscious: – Lower them gently to the floor – Perform abdominal thrusts • Straddle the patients thighs • Use the palm of one hand with your other hand on top • Place hand above the belly button • Use upward, quick thrusts
Simple Cuts & Scratches • Wash with soap and water • Apply antiseptic to prevent infection • Keep the wound clean with an adhesive bandage (Band-aid) • Clean and rebandage small wound daily

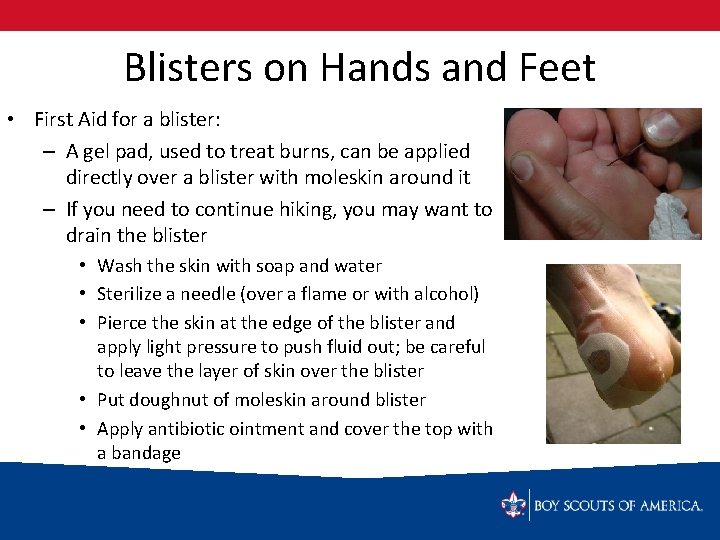
Blisters on Hands and Feet • Pockets of fluid that form as a defense against friction on the skin • Prevention: – Wear work gloves (community service projects, when using saw, ax, etc. ) – Wear proper fitting shoes or boots – Change socks when they become sweaty or wet – Pay attention to warnings (hot spots)
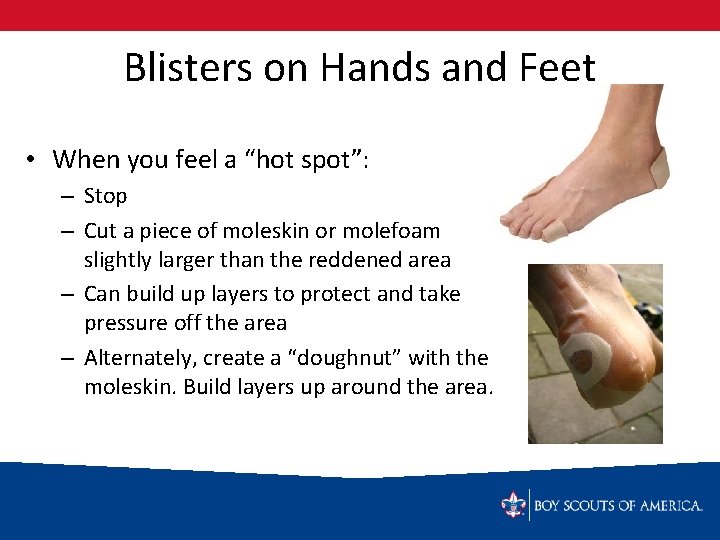
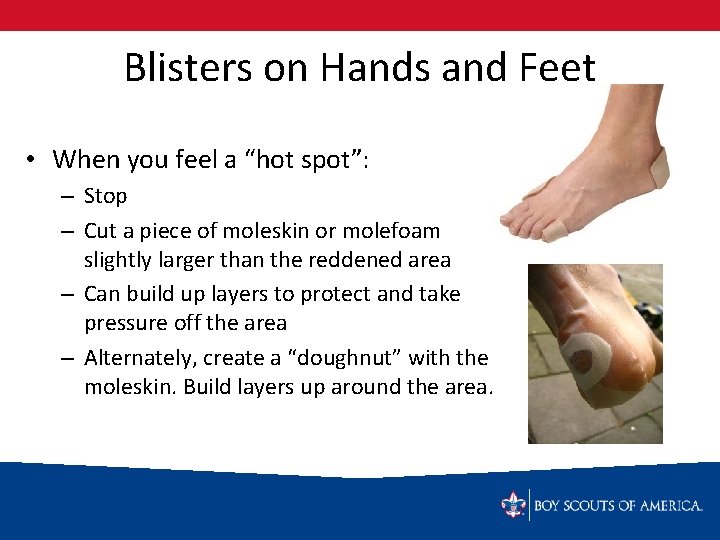
Blisters on Hands and Feet • When you feel a “hot spot”: – Stop – Cut a piece of moleskin or molefoam slightly larger than the reddened area – Can build up layers to protect and take pressure off the area – Alternately, create a “doughnut” with the moleskin. Build layers up around the area.
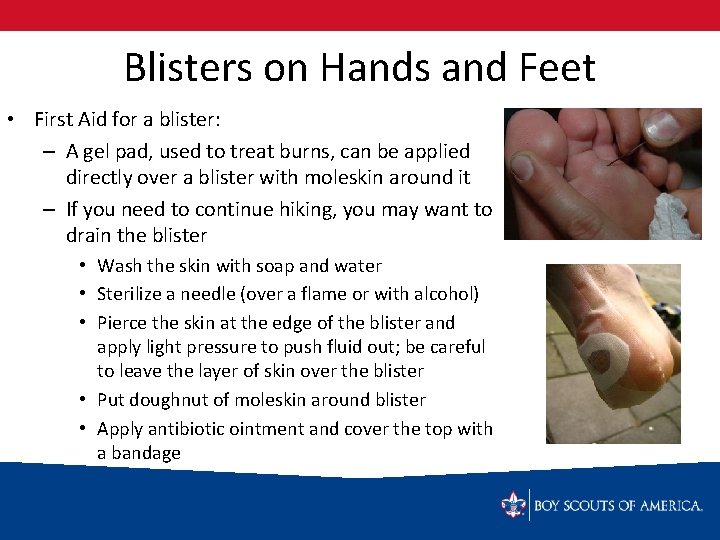
Blisters on Hands and Feet • First Aid for a blister: – A gel pad, used to treat burns, can be applied directly over a blister with moleskin around it – If you need to continue hiking, you may want to drain the blister • Wash the skin with soap and water • Sterilize a needle (over a flame or with alcohol) • Pierce the skin at the edge of the blister and apply light pressure to push fluid out; be careful to leave the layer of skin over the blister • Put doughnut of moleskin around blister • Apply antibiotic ointment and cover the top with a bandage
Minor Burns/Scalds (1 st degree) First Aid – Remove the heat source – Run under cool water or apply cool compresses Prevention of sunburn: – – Apply sunscreen Reapply if sweating or swimming Wide brimmed hat Long sleeves/long pants
Bee and Wasp Stings • Scrape away stinger with edge of credit card or knife • Apply an ice pack • Know whether or not the person is allergic to bee stings
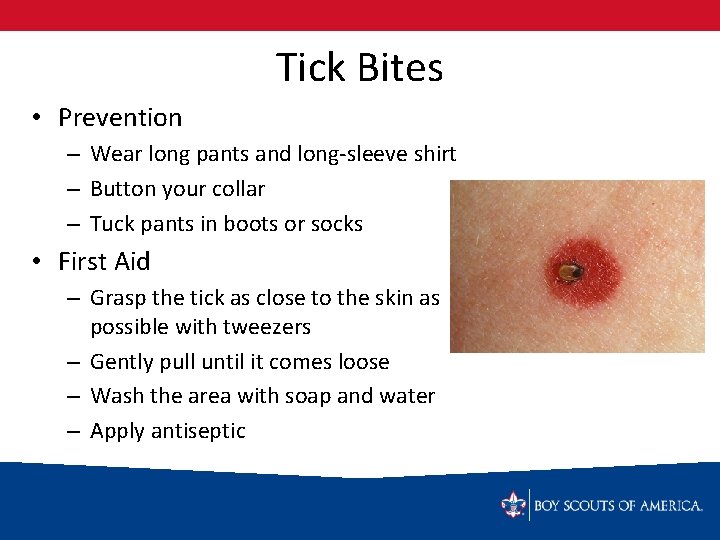
Tick Bites • Prevention – Wear long pants and long-sleeve shirt – Button your collar – Tuck pants in boots or socks • First Aid – Grasp the tick as close to the skin as possible with tweezers – Gently pull until it comes loose – Wash the area with soap and water – Apply antiseptic
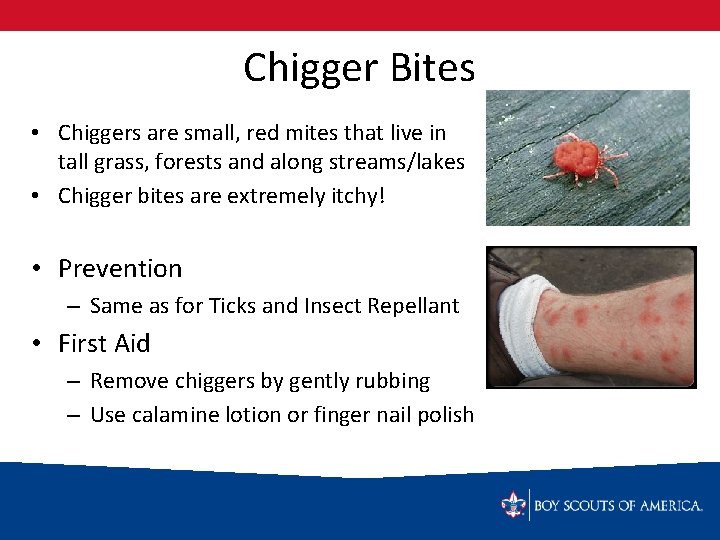
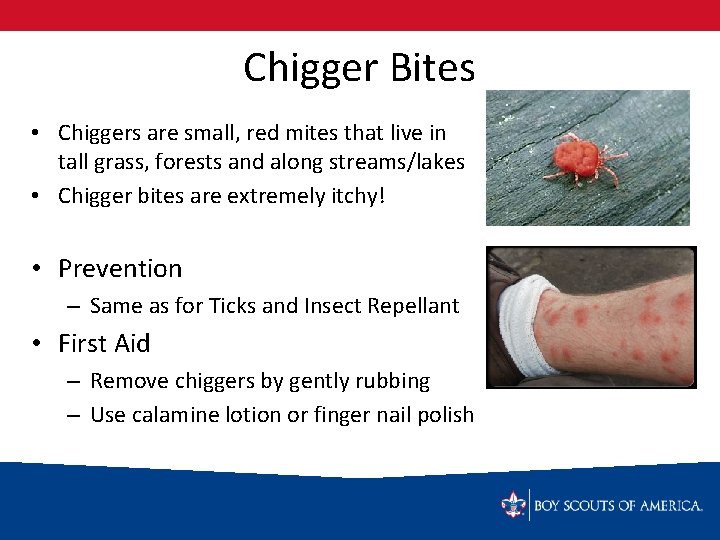
Chigger Bites • Chiggers are small, red mites that live in tall grass, forests and along streams/lakes • Chigger bites are extremely itchy! • Prevention – Same as for Ticks and Insect Repellant • First Aid – Remove chiggers by gently rubbing – Use calamine lotion or finger nail polish
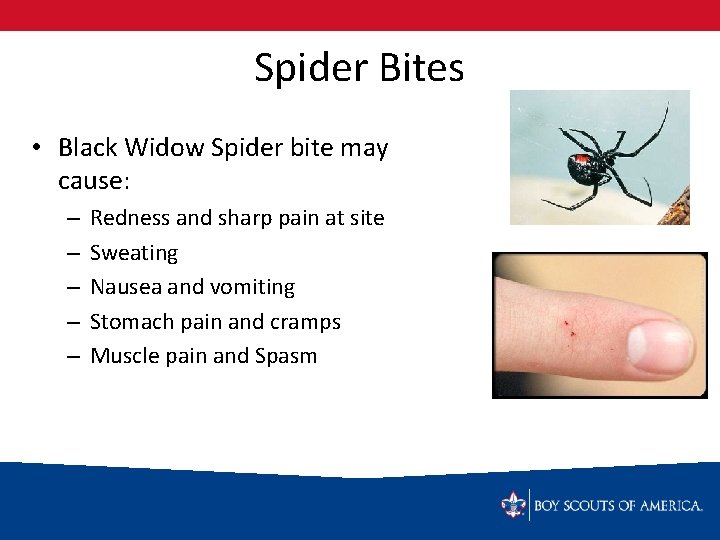
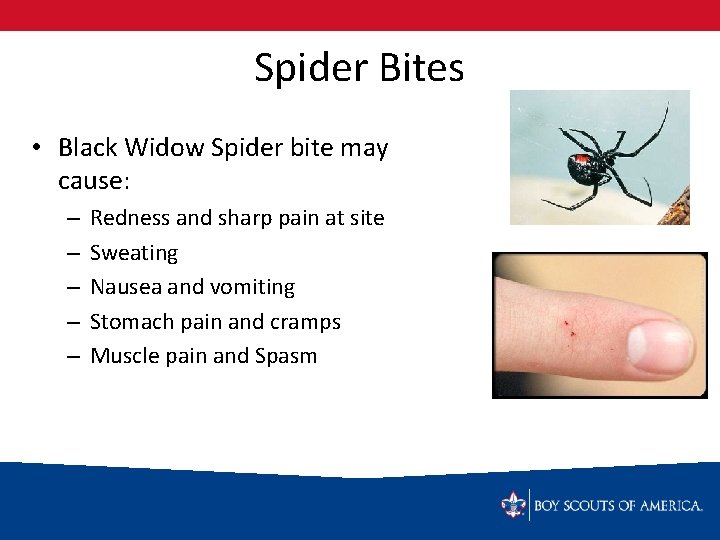
Spider Bites • Black Widow Spider bite may cause: – – – Redness and sharp pain at site Sweating Nausea and vomiting Stomach pain and cramps Muscle pain and Spasm

Spider Bites • Brown Recluse Spider may cause: – Pain, redness and swelling in 2 -8 hours (usually not right away) – An open sore will likely develop – Fever – Chills – Nausea and vomiting – Joint pain – Faint rash
Spider Bites • First Aid for all spider bites: – Wash the area with soap and water – Apply cold pack – Seek medical attention
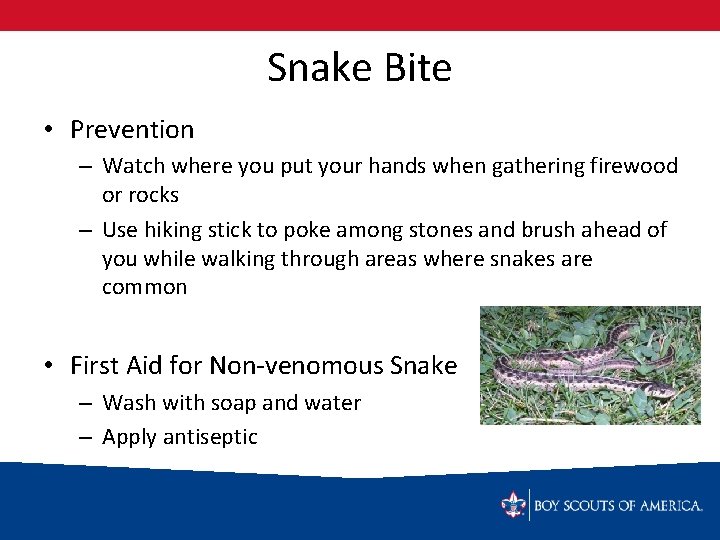
Snake Bite • Prevention – Watch where you put your hands when gathering firewood or rocks – Use hiking stick to poke among stones and brush ahead of you while walking through areas where snakes are common • First Aid for Non-venomous Snake – Wash with soap and water – Apply antiseptic
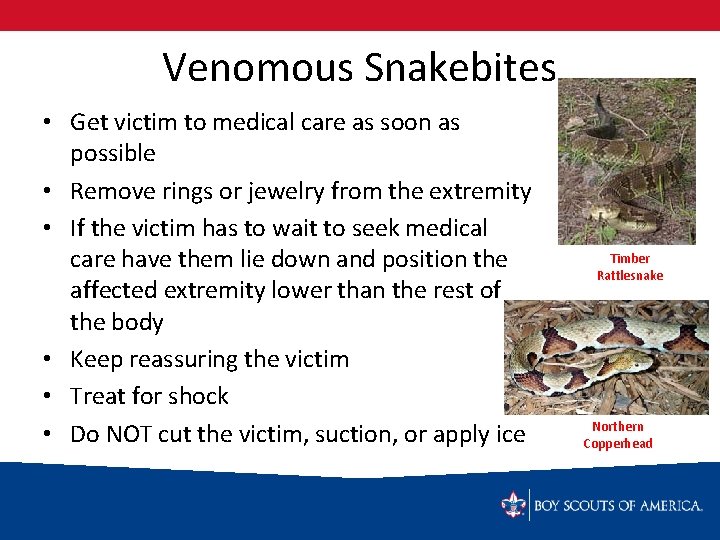
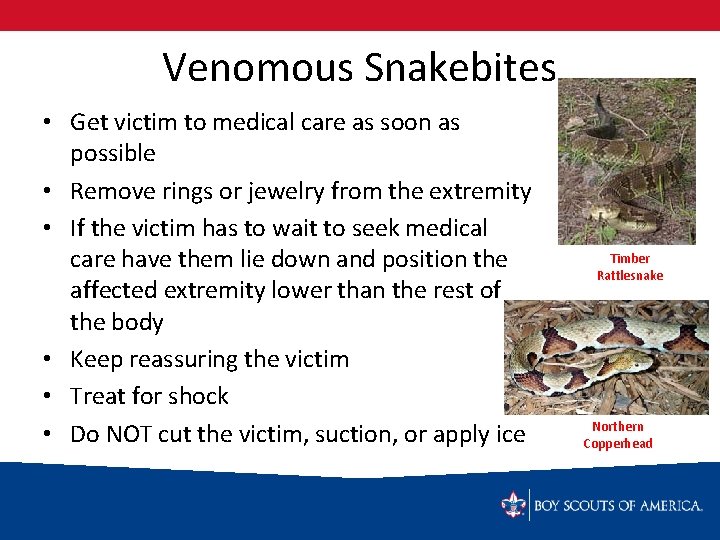
Venomous Snakebites • Get victim to medical care as soon as possible • Remove rings or jewelry from the extremity • If the victim has to wait to seek medical care have them lie down and position the affected extremity lower than the rest of the body • Keep reassuring the victim • Treat for shock • Do NOT cut the victim, suction, or apply ice Timber Rattlesnake Northern Copperhead
Nosebleed • Have the victim sit up and lean forward • Pinch the nostril shut • Apply a cool, wet cloth over the bridge of the nose • If severe: – Treat for shock – Seek medical attention
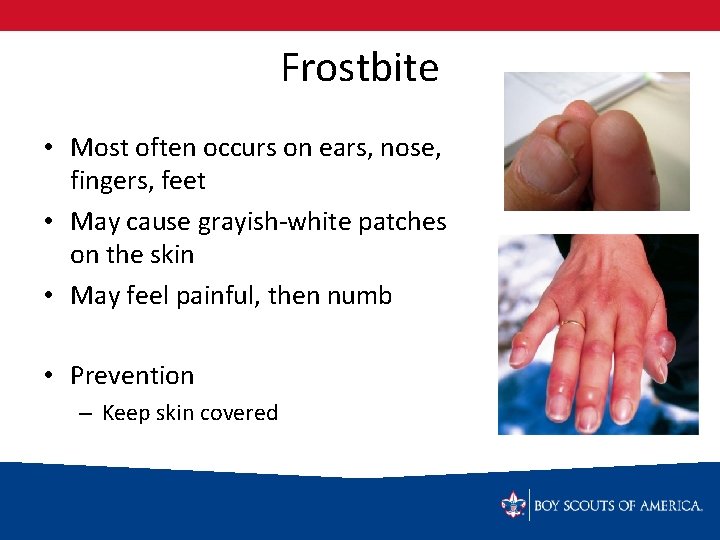
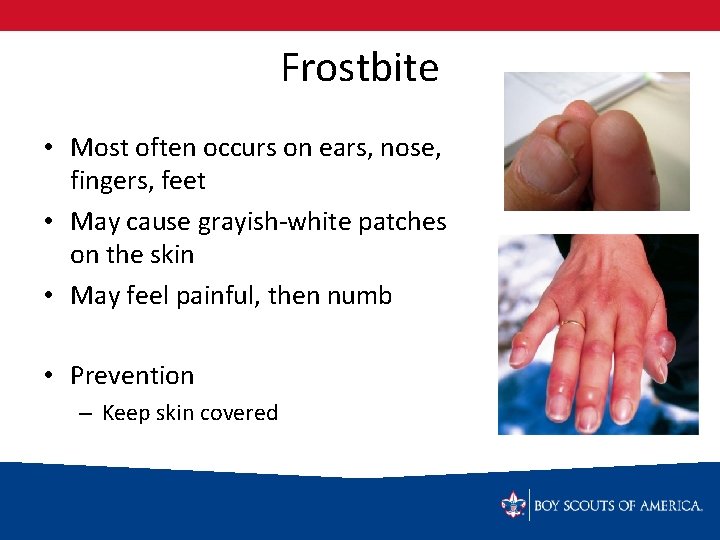
Frostbite • Most often occurs on ears, nose, fingers, feet • May cause grayish-white patches on the skin • May feel painful, then numb • Prevention – Keep skin covered
Frostbite • First Aid – – – – Get victim indoors, if possible Place palm of hand over ear or cheek Place fingers under clothing in armpit Place victim’s feet on skin of your abdomen DO NOT RUB the skin Can run the affected area under warm (not hot) water Have the victim exercise affected fingers or toes Seek medical attention
Second Class Requirement 6 a Show what to do for “hurry” cases of stopped breathing, serious bleeding, and ingested poisoning Requirement 6 b Prepare a personal first aid kit to take with you on a hike
Second Class Requirement 6 c Demonstrate first aid for the following: – Object in the eye – Bite of a suspected rapid animal – Puncture wound from a splinter, nail, and fishhook – Serious burns – Heat exhaustion – Shock – Heat stroke, dehydration, hypothermia, and hyperventilation
Hurry Cases What is a “hurry” case? A “hurry” case is when a victim suffers from an immediate threat to their life. Action must be taken within minutes to save the victim.
Hurry Cases What are the “hurry” cases? 1. 2. 3. 4. Stopped breathing Severe bleeding Ingested poisoning Stopped heartbeat (First Class Requirement)
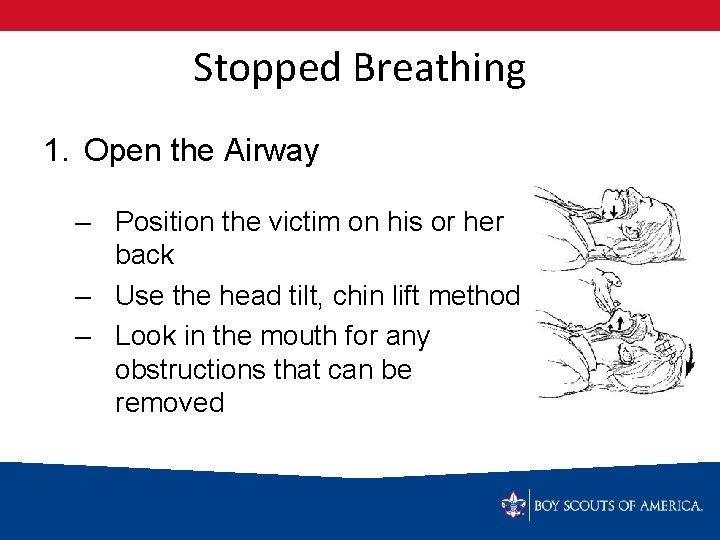
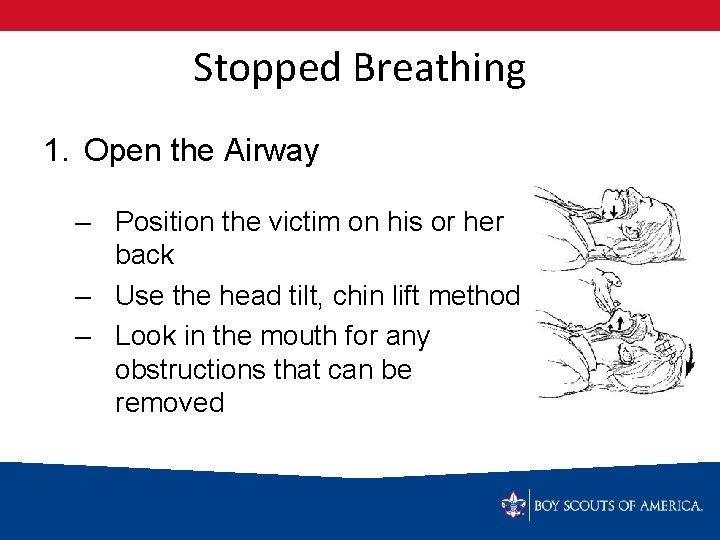
Stopped Breathing 1. Open the Airway – Position the victim on his or her back – Use the head tilt, chin lift method – Look in the mouth for any obstructions that can be removed
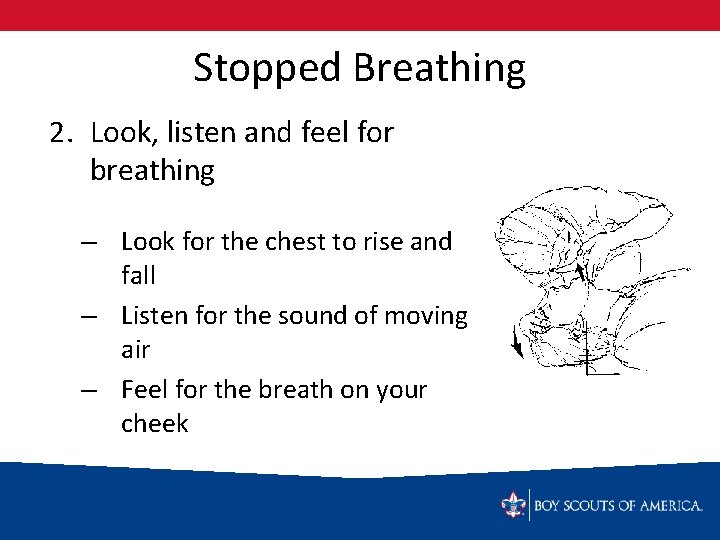
Stopped Breathing 2. Look, listen and feel for breathing – Look for the chest to rise and fall – Listen for the sound of moving air – Feel for the breath on your cheek
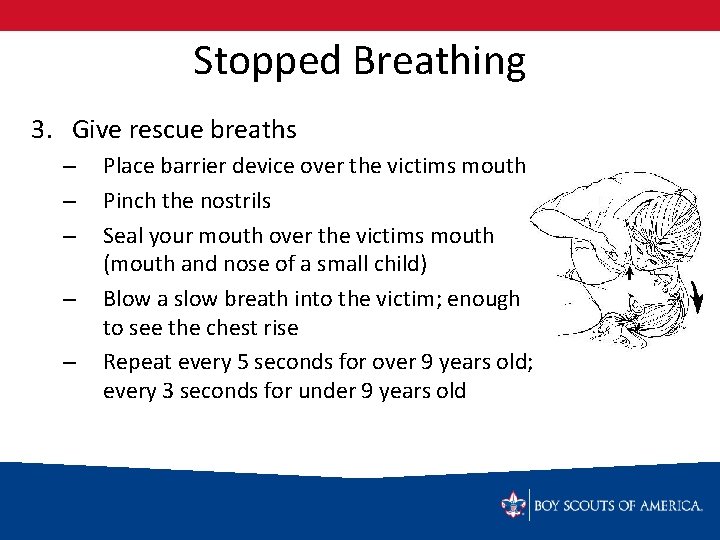
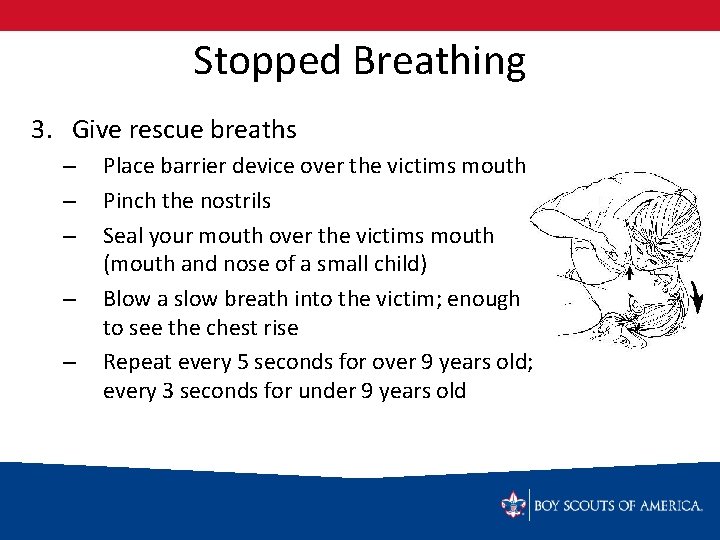
Stopped Breathing 3. Give rescue breaths – – – Place barrier device over the victims mouth Pinch the nostrils Seal your mouth over the victims mouth (mouth and nose of a small child) Blow a slow breath into the victim; enough to see the chest rise Repeat every 5 seconds for over 9 years old; every 3 seconds for under 9 years old
Stopped Breathing 4. If the chest doesn’t rise and fall – – Reposition the head Check again for any obstructions Try the breaths again If still not able to make the chest rise, begin abdominal thrusts – Continue rescue breathing until the victims breathes on their own, help arrives, or you are too physically exhausted to continue
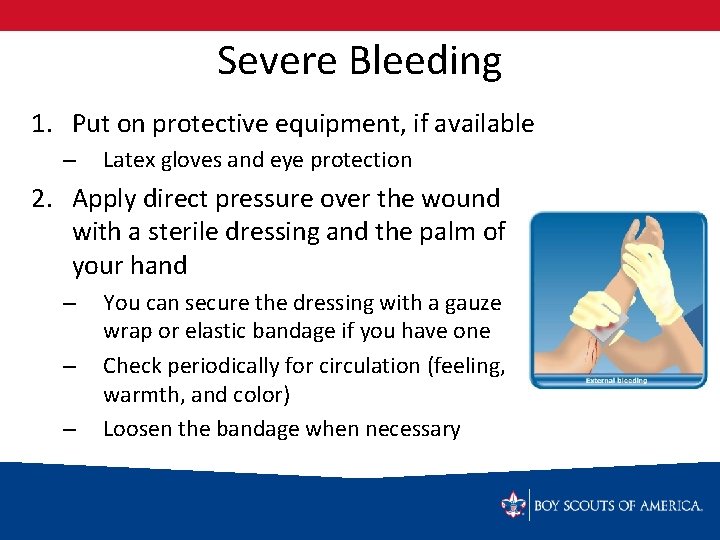
Severe Bleeding 1. Put on protective equipment, if available – Latex gloves and eye protection 2. Apply direct pressure over the wound with a sterile dressing and the palm of your hand – – – You can secure the dressing with a gauze wrap or elastic bandage if you have one Check periodically for circulation (feeling, warmth, and color) Loosen the bandage when necessary
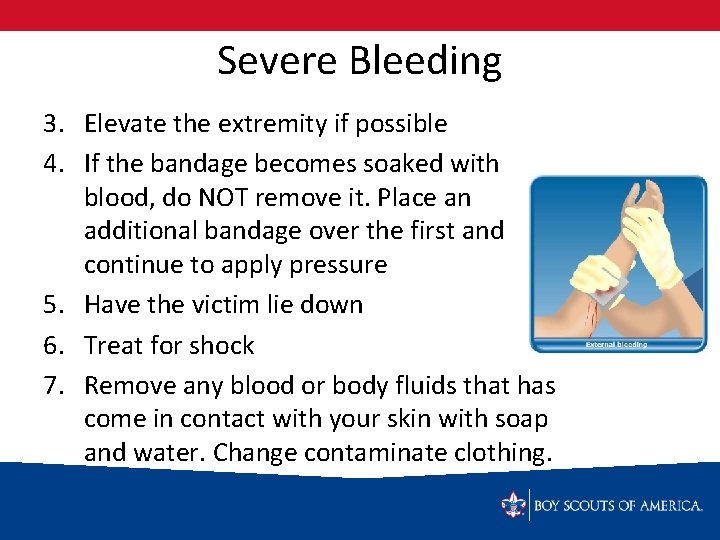
Severe Bleeding 3. Elevate the extremity if possible 4. If the bandage becomes soaked with blood, do NOT remove it. Place an additional bandage over the first and continue to apply pressure 5. Have the victim lie down 6. Treat for shock 7. Remove any blood or body fluids that has come in contact with your skin with soap and water. Change contaminate clothing.
Ingested Poisoning 1. Victim will be sick, maybe unconscious 2. Most clues will be found at the scene – – Gather empty bottles/containers Estimate how much may have been ingested 3. Call Poison Control Center and 911. 4. Do not give victim anything by mouth or induce vomiting unless told to do so by Poison Control 5. Treat victim for shock 6. Monitor Breathing
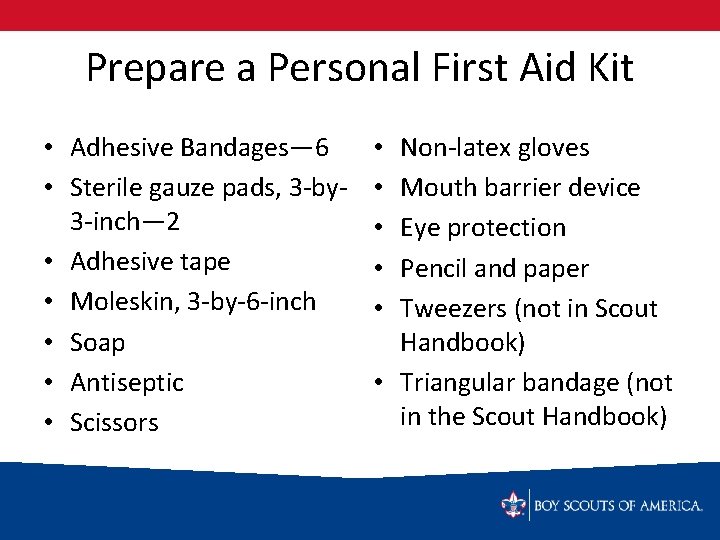
Prepare a Personal First Aid Kit • Adhesive Bandages— 6 • Sterile gauze pads, 3 -by 3 -inch— 2 • Adhesive tape • Moleskin, 3 -by-6 -inch • Soap • Antiseptic • Scissors Non-latex gloves Mouth barrier device Eye protection Pencil and paper Tweezers (not in Scout Handbook) • Triangular bandage (not in the Scout Handbook) • • •
Personal First Aid Kit • Make it practical for the Scout • Encourage them to bring their personal first aid kits on all outdoor scout activities (and any others where they may have a day pack or fanny pack) • Periodically review the contents of their first aid kits when appropriate for the event to which you are going
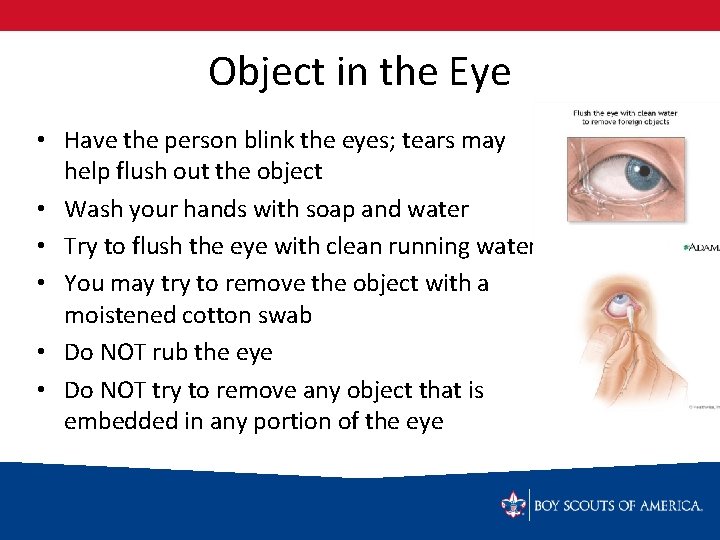
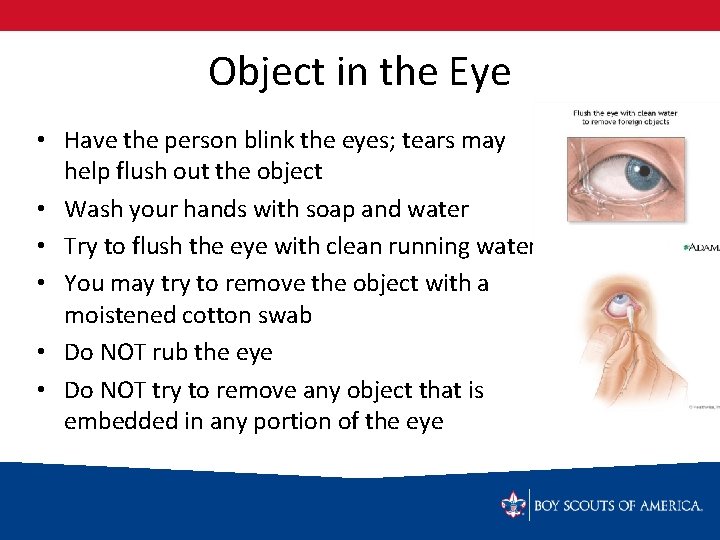
Object in the Eye • Have the person blink the eyes; tears may help flush out the object • Wash your hands with soap and water • Try to flush the eye with clean running water • You may try to remove the object with a moistened cotton swab • Do NOT rub the eye • Do NOT try to remove any object that is embedded in any portion of the eye
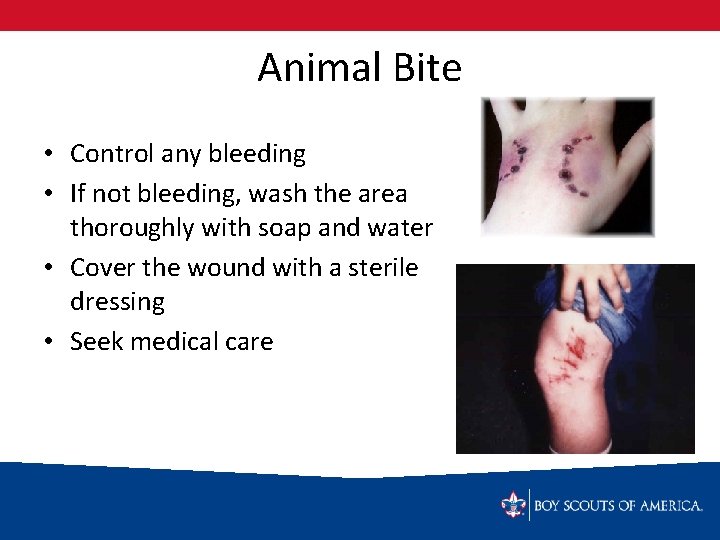
Animal Bite • Control any bleeding • If not bleeding, wash the area thoroughly with soap and water • Cover the wound with a sterile dressing • Seek medical care
Animal Bite • Suspect rabies in any animal, especially if they are acting uncharacteristically • Try to get a description of the animal and note when the animal was last seen • Do NOT put yourself at risk for injury by trying to capture the animal • Notify police, animal control, or rangers about the animal
Splinters • Remove splinters with tweezers sterilized over a flame or in boiling water • May also use a sterilized needle if necessary • Wash the area with soap and water • Apply antiseptic • Apply adhesive bandage
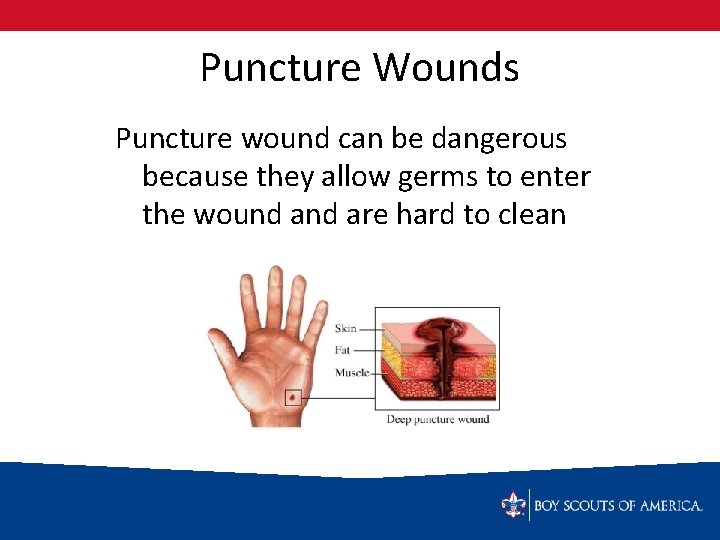
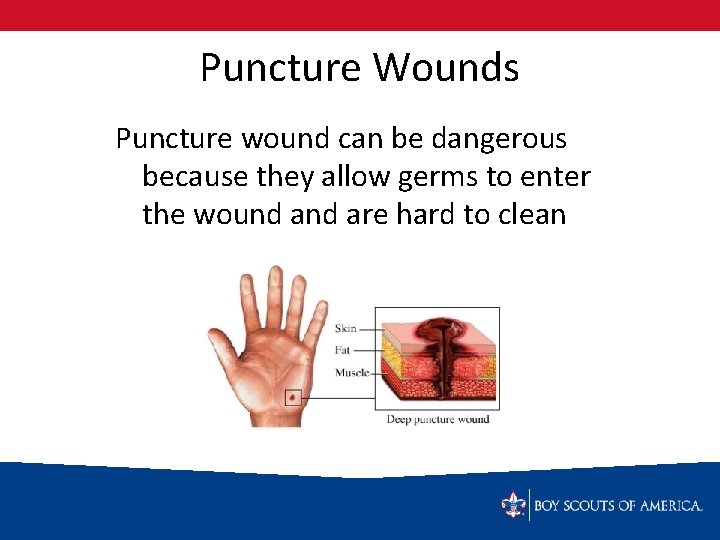
Puncture Wounds Puncture wound can be dangerous because they allow germs to enter the wound are hard to clean
Puncture Wounds • Remove bits of glass or other objects you can see with tweezers sterilized over a flame or in boiling water • Wash the area with soap and water • Apply antiseptic • Apply sterile bandages • Seek medical attention
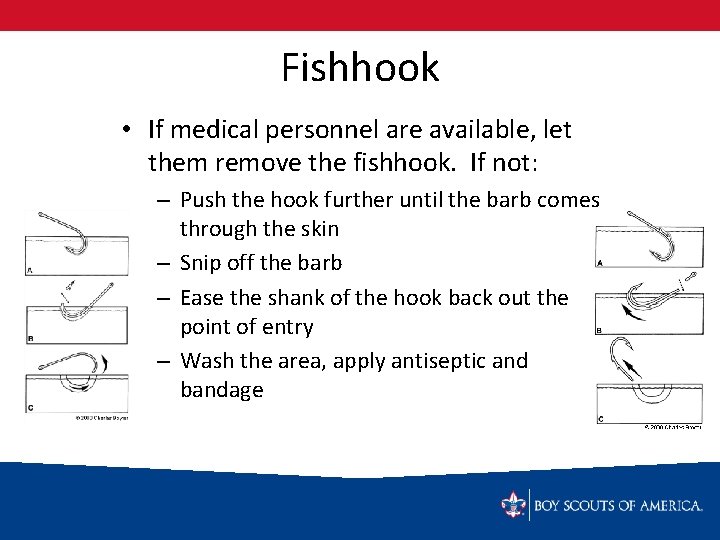
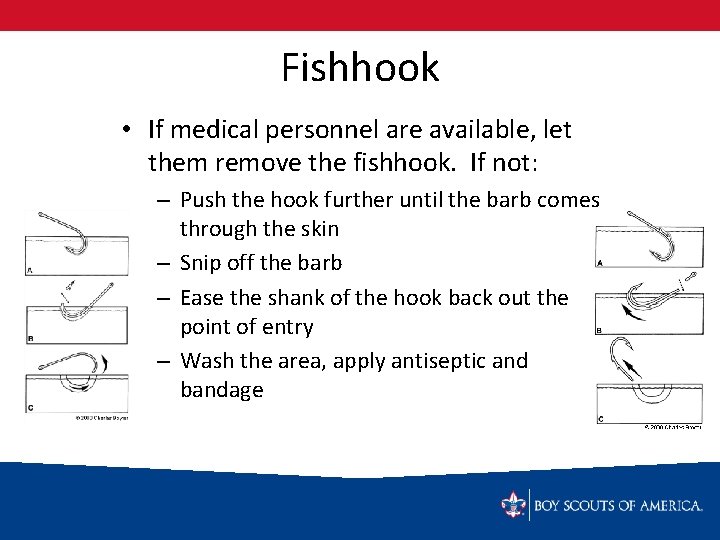
Fishhook • If medical personnel are available, let them remove the fishhook. If not: – Push the hook further until the barb comes through the skin – Snip off the barb – Ease the shank of the hook back out the point of entry – Wash the area, apply antiseptic and bandage

Second-Degree Burns When blisters form, there is deeper damage to the skin Remove heat source Run under cool water or use cool compresses Dry area and protect with a sterile bandage Do NOT pop blisters Do NOT apply butter, cream, ointments or sprays • Seek medical care • • •
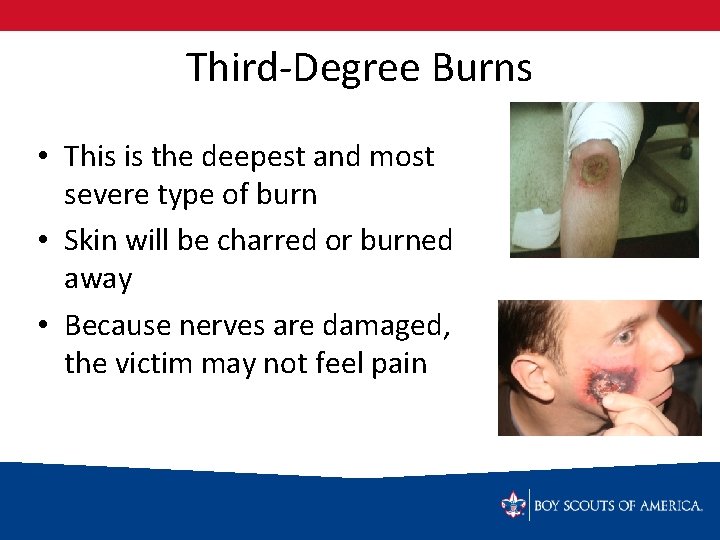
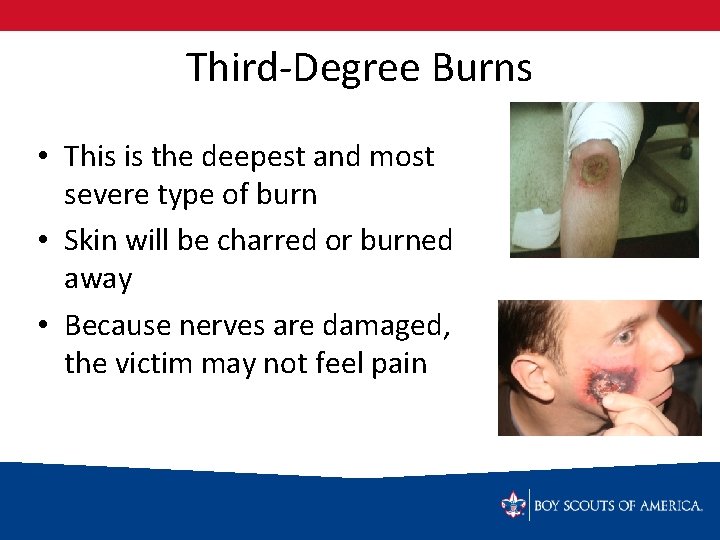
Third-Degree Burns • This is the deepest and most severe type of burn • Skin will be charred or burned away • Because nerves are damaged, the victim may not feel pain
Third-Degree Burns • Stop the burning process! May use cool compresses but do not immerse large areas in cool water (may cause shock) • Do NOT try to remove clothing that is sticking to the area • Do NOT apply creams, ointments or sprays • Cover the area with a sterile gauze or clean sheet if the area is large • Treat for shock • Seek immediate medical attention
Shock What is shock? – When the circulatory system is unable to provide enough blood to all parts of the body When does it occur? – May occur with any injury or stress to the body
Symptoms of Shock • Restlessness or irritability • Weakness • Confusion or fear • Dizziness • Moist, clammy, cool, and/or pale skin • Quick, weak pulse • Shallow, rapid, and irregular breathing • Nausea • Vomiting • Extreme thirst
Shock • Treat every victim for shock! – Most victims have some degree of shock but symptoms are not always apparent early – Sometimes early first aid for an injury may prevent shock – Sometimes early treatment for shock will prevent shock

Shock • Eliminate the causes of shock by restoring breathing and circulation, controlling bleeding, relieving severe pain, and treating wounds • Call for emergency aid • Have the victim lie down • Raise the victim’s legs about 12 inches (only if you don’t suspect head, neck, back, hip or leg injuries) • Keep the victim warm with blankets, coats or sleeping bags
Shock • Do not leave the victim alone • Continue to reassure the victim in a calm voice (fear and uncertainty make shock worse) • A person who appears to be unconscious may still be able to hear you—keep letting them know you are there and you are getting help
Heat Related Injuries Prevention – Drink plenty of fluids – Rest in the shade when you feel too warm or get muscle cramps – Do the heaviest physical activity in the morning or evening – Wear loose, light-colored clothing – Shade your head with a hat
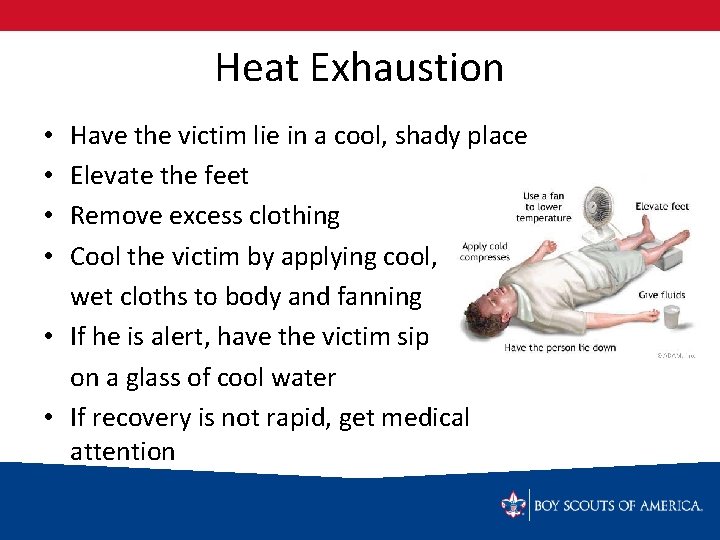
Heat Exhaustion Occurs when the body’s cooling system becomes overworked. Symptoms – – – – Pale skin that is clammy from heavy sweating Nausea Fatigue/weakness Dizziness/lightheadedness Headache Muscle cramps Rapid Pulse
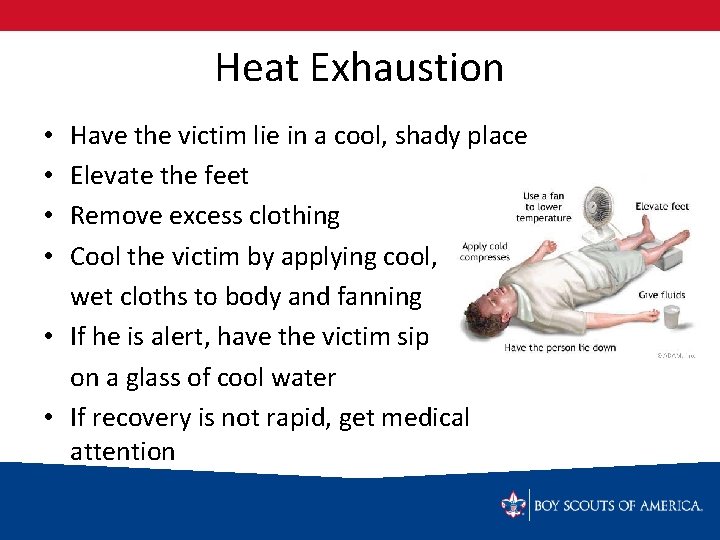
Heat Exhaustion Have the victim lie in a cool, shady place Elevate the feet Remove excess clothing Cool the victim by applying cool, wet cloths to body and fanning • If he is alert, have the victim sip on a glass of cool water • If recovery is not rapid, get medical attention • •
Heat Stroke Occurs when the body’s cooling system is overworked and stops functioning. The victims body temperature will soar to a life-threatening level
Heat Stroke • Symptoms – Very hot skin – Red skin, can be dry or a little damp from sweat – Rapid pulse – Noisy breathing – Confusion, irritability, unwillingness to accept treatment – Unconsciousness
Heat Stroke • Call for medical help immediately! • Move the victim to a shady or air-conditioned area • Cool the victim any way you can – Remove outer clothing – Cover with cool wet towels, clothing, etc. and fan – Place in a steam, bathtub of cool water, or in front of an air conditioner in house or car – Wrap icepacks with a thin barrier and place in armpits, along neck, and in groin
Heat Stroke • Keep the victim lying down and comfortable • Raise the victims head and shoulders a little • If the person is able to drink, give small amounts of cool water • Monitor the victim closely – They may vomit – They may require rescue breathing
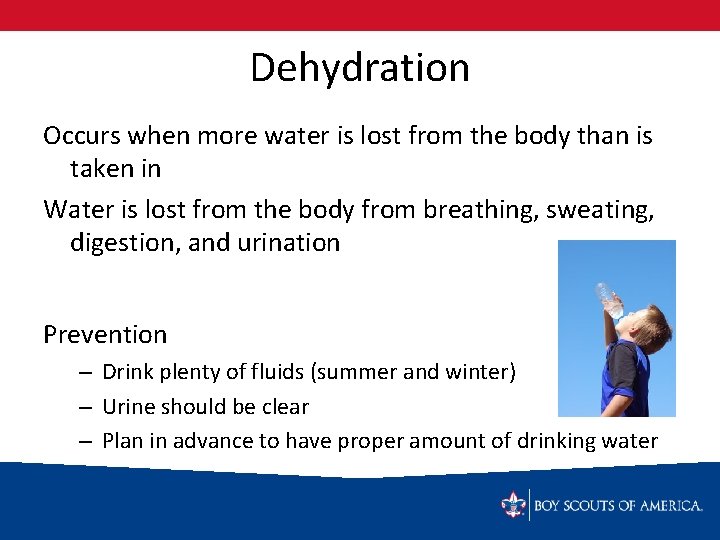
Dehydration Occurs when more water is lost from the body than is taken in Water is lost from the body from breathing, sweating, digestion, and urination Prevention – Drink plenty of fluids (summer and winter) – Urine should be clear – Plan in advance to have proper amount of drinking water
Dehydration Symptoms – – – Increased thirst Dry lips Headache Body aches, muscle cramps Dark urine Heat exhaustion, heat stroke, and hypothermia can all be caused in part by dehydration
Hypothermia Occurs when more body heat is lost than can be generated. Wind, precipitation, hunger, dehydration, and exhaustion all increase the risk Prevention – – Wear proper clothing for the weather Don’t forget the hat! Eat proper food for energy Drink plenty of fluids
Symptoms of Hypothermia • • • Feeling cold and numb • Confusion, making bad decisions Fatigue • Irritability Anxiety Uncontrollable shivering • Stumbling and/or falling down Slurred speech • Loss of consciousness
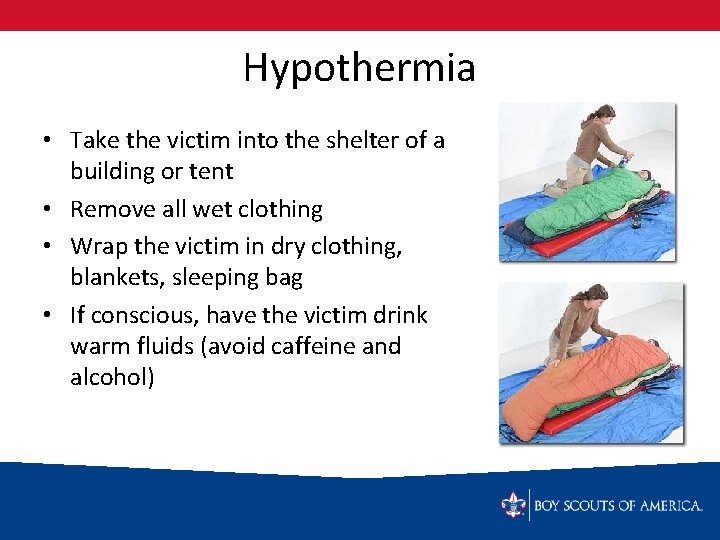
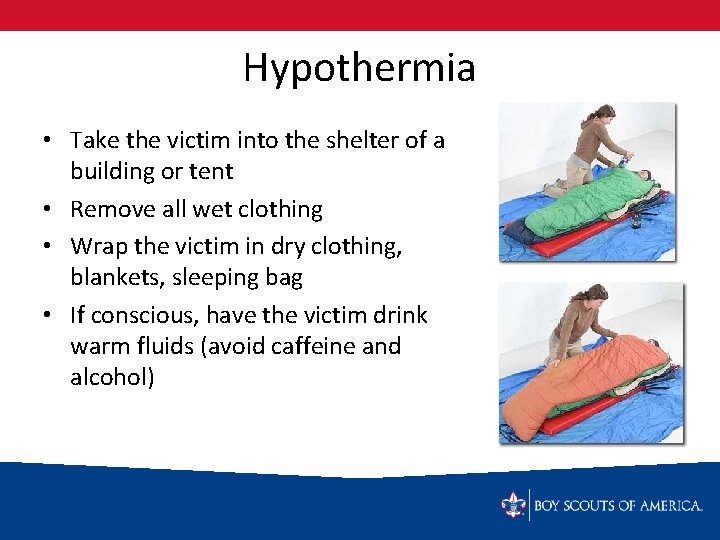
Hypothermia • Take the victim into the shelter of a building or tent • Remove all wet clothing • Wrap the victim in dry clothing, blankets, sleeping bag • If conscious, have the victim drink warm fluids (avoid caffeine and alcohol)
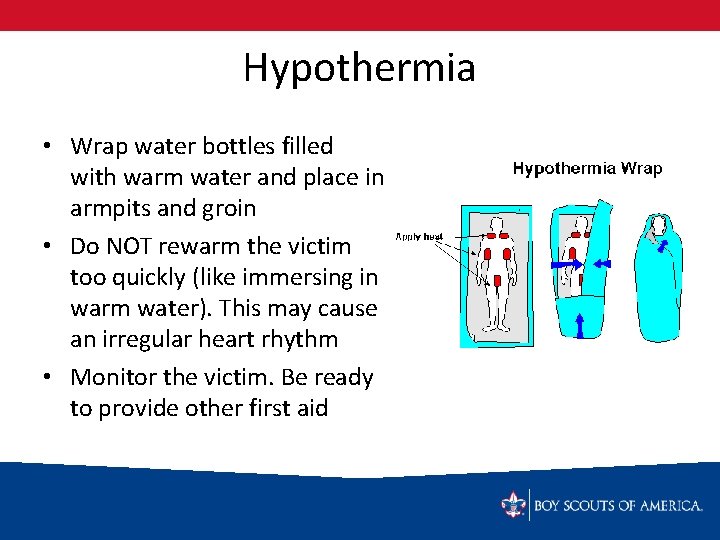
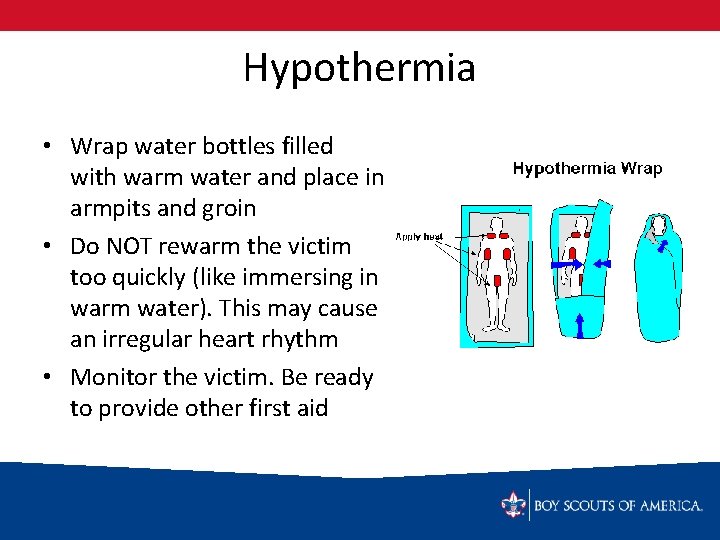
Hypothermia • Wrap water bottles filled with warm water and place in armpits and groin • Do NOT rewarm the victim too quickly (like immersing in warm water). This may cause an irregular heart rhythm • Monitor the victim. Be ready to provide other first aid
Hyperventilation Occurs when breathing is too rapid and too much carbon dioxide is removed from the bloodstream Symptoms – – – Victim feels like he or she is suffocating Dizziness Disoriented Increasingly fearful Tingling in fingers, toes, lips
Hyperventilation • Talk quietly to the victim • Encourage the victim to calm down and breath slowly • Have the patient take some slow breaths in a paper bag • Seek medical care—breathing fast may be a sign of other conditions (asthma, diabetes, etc. )
First Class Requirement 8 a Demonstrate bandages for a sprained ankle and for injuries of the head, the upper arm, and the collarbone. Requirement 8 b Show to transport by yourself, and with another person, a person – From a smoke-filled room – With a sprained ankle, for at least 25 yards
First Class Requirement 8 d Tell the five most common signals of a heart attack. Explain the steps (procedures) in cardiopulmonary resuscitation (CPR)
Bandages Sprained Ankle Head Upper Arm Collarbone
Rescue from a Smoke-Filled Room • Must be done quickly • Cannot put yourself at risk • How to move a victim in that environment: – Grab the victim by their clothing and drag them toward you – Roll the victim onto a coat, blanket, tablecloth, etc. and drag them out – Get behind the victim, reach under his arms, grab his wrists and drag him out
Transport a Victim with Sprained Ankle • • Walking Assist One-Person Carry Four-handed Seat Carry Two-person Carry
Heart Attack 5 Most Common Symptoms 1. Uncomfortable pressure, squeezing, fullness in the chest • 2. 3. 4. 5. May spread to shoulders, arms, and neck Unusual Sweating Nausea Shortness of Breath A feeling of Weakness
CPR for Heart Attack 1. Check for Response – Tap the victim on the shoulder – Are you OK? 2. Activate the Emergency Response System and get an AED

CPR for Heart Attack 3. Open the Airway – – – Head tilt--chin lift Look, listen and feel for 5 -10 secs If not adequate breathing, give 2 rescue breaths Watch for the chest to rise and fall If chest doesn’t rise, reposition the head (airway) and attempt 2 more breaths
CPR for Heart Attack 4. Begin Chest Compressions – 30 compressions, then 2 breaths – Rate of 100 per minute – Keep interruptions to 10 seconds or less – Continue until: • • • Scene is unsafe More qualified help arrives Cannot physically continue