Respiratory system Functional Anatomy of respiratory system Mechanics
- Slides: 28
Respiratory system
• Functional Anatomy of respiratory system • Mechanics of breathing • Muscles of inspiration and expiration • pressure changes during respiratory cycle • Work of breathing • Compliance • Surfactant • Dead space • Lung volume and capacities • static and dynamic lung volumes • Pulmonary function tests.
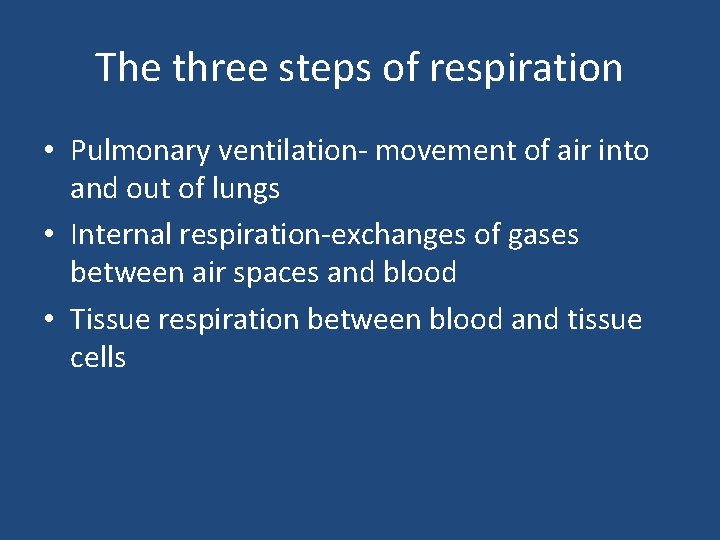
• • • Types of respiration External respiration Internal respiration Phases of respiration Inspiration Expiration
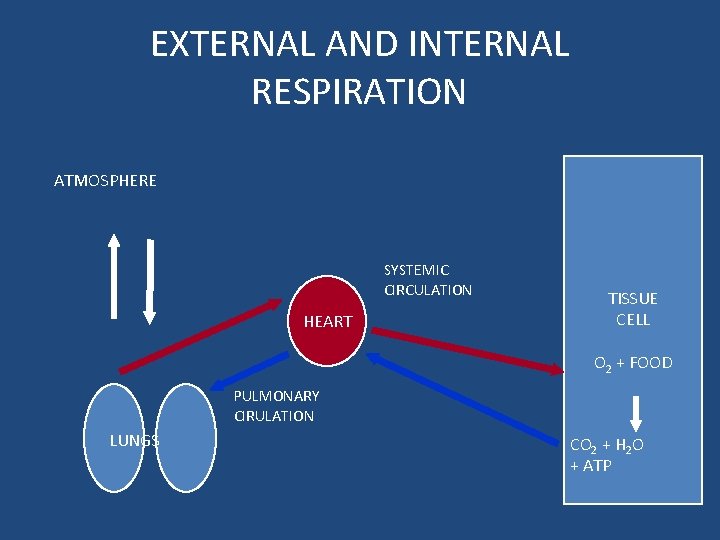
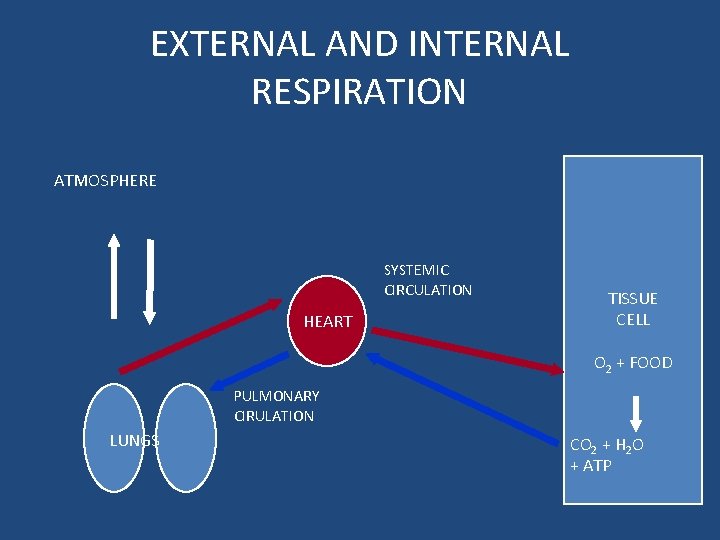
EXTERNAL AND INTERNAL RESPIRATION ATMOSPHERE SYSTEMIC CIRCULATION HEART TISSUE CELL O 2 + FOOD PULMONARY CIRULATION LUNGS CO 2 + H 2 O + ATP
• External respiration • Transport of gases • Internal respiration.
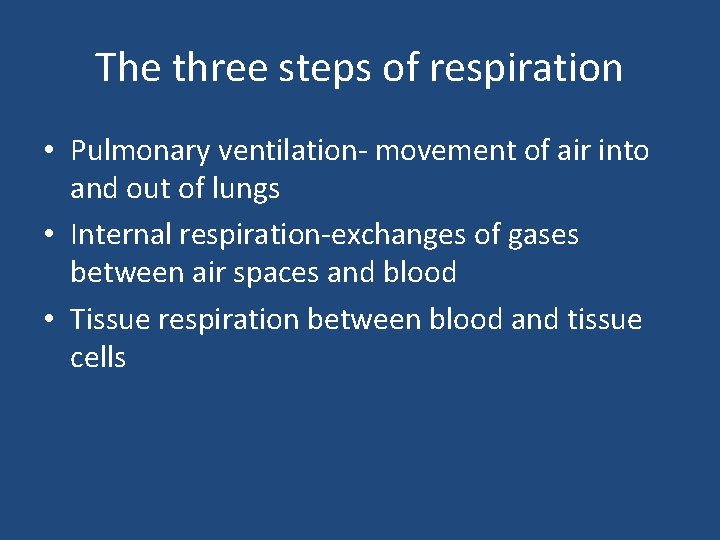
The three steps of respiration • Pulmonary ventilation- movement of air into and out of lungs • Internal respiration-exchanges of gases between air spaces and blood • Tissue respiration between blood and tissue cells
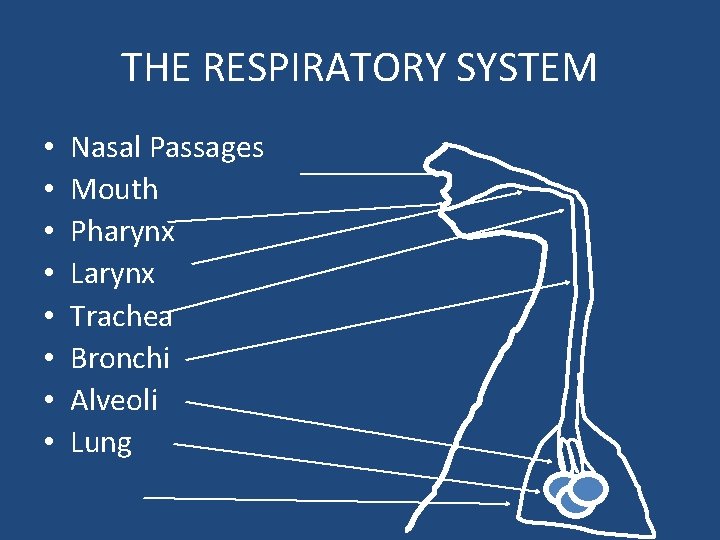
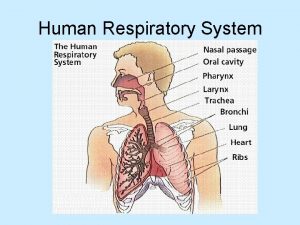
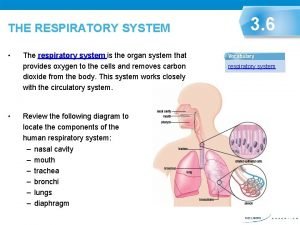
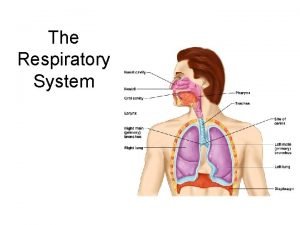
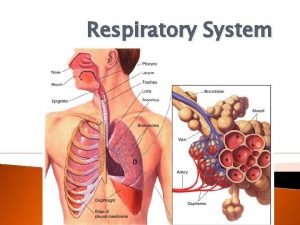
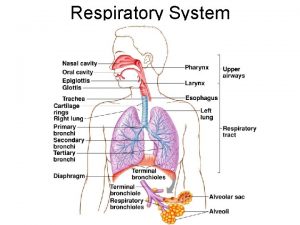
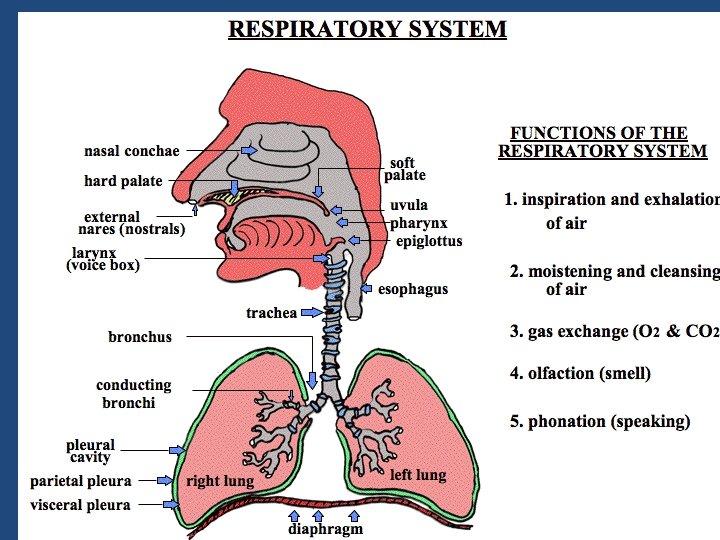
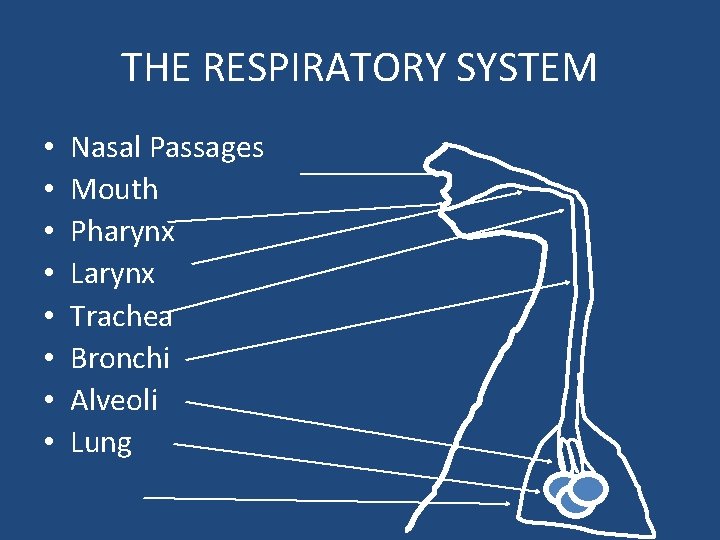
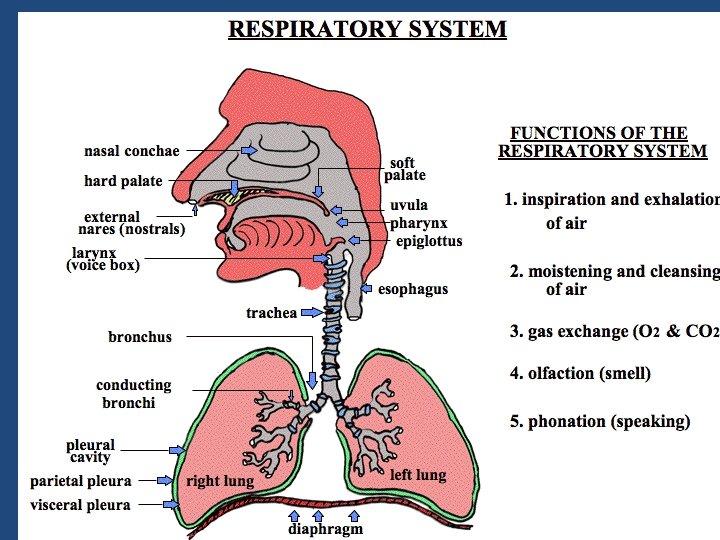
THE RESPIRATORY SYSTEM • • Nasal Passages Mouth Pharynx Larynx Trachea Bronchi Alveoli Lung
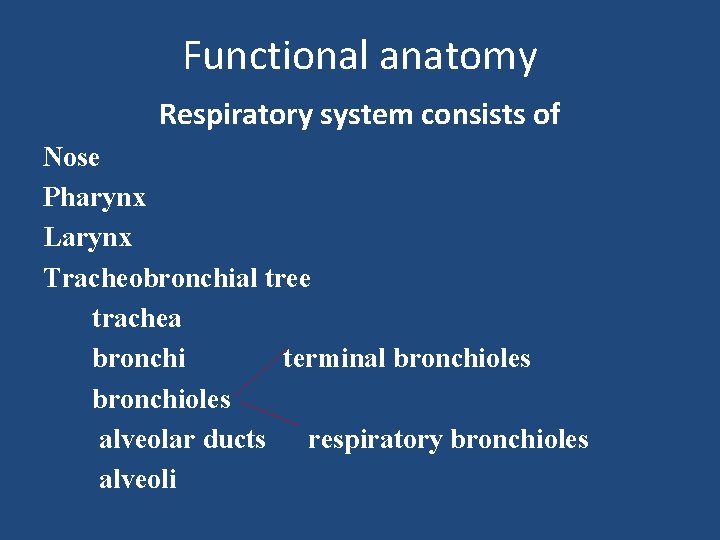
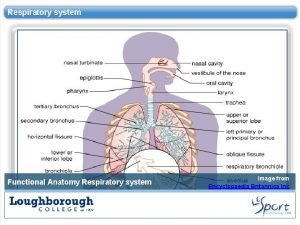
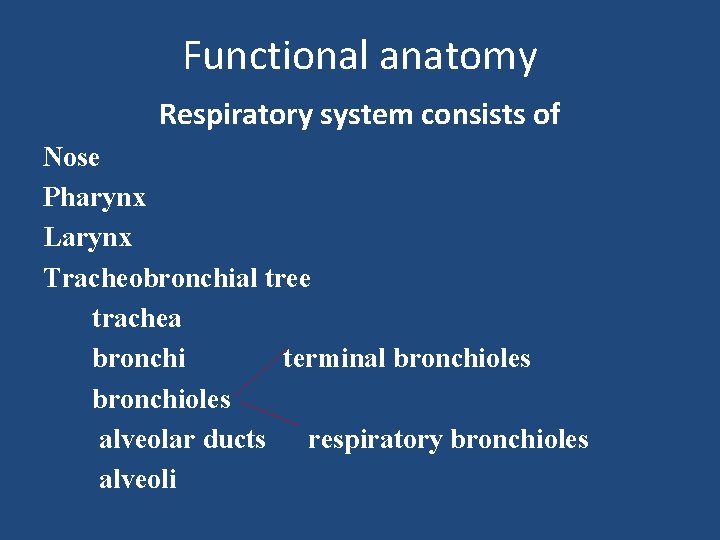
Functional anatomy Respiratory system consists of Nose Pharynx Larynx Tracheobronchial tree trachea bronchi terminal bronchioles alveolar ducts respiratory bronchioles alveoli
• Pleura • Each lung is surrounded by a bilayered serous membrane. • Pleura • Has two layers-visceral and parietal • Visceral layer is attached to the surface of the lungs • At hilum it continuous with parietal layer which is attached to wall of the thoracic cavity.
• • Pleural cavity Narrow space between two layers of pleura Intrapleural fluid Contain thin flim of serous fluid called intrapleural fluid. Functions of intrapleural fluid. Functions as lubricant Creates negative pressure. Pneumothorax
• Nose – made of cartilage and bone and is designed to warm, moisten, and filter air as it comes into the system • Pharynx – (throat) conducts food and air; exchanges air with Eustachian tube to equalize pressure • Larynx – (voice box) connects the pharynx and the trachea; made of cartilage; contains vocal cords • Trachea – (windpipe) tubular passage way for air; carries air to the lungs, C-shaped cartilage rings, divides at end • Bronchi-The bronchi, or bronchial tree, is a set of branching tubes. The bronchial tree starts at the trachea as one tube then splits into two, which continue to split into smaller tubes called bronchioles, which go into the lungs
Anatomy of lungs Regions of the Respiratory Tract • The upper airway. • The conducting airway. • The alveolar airway
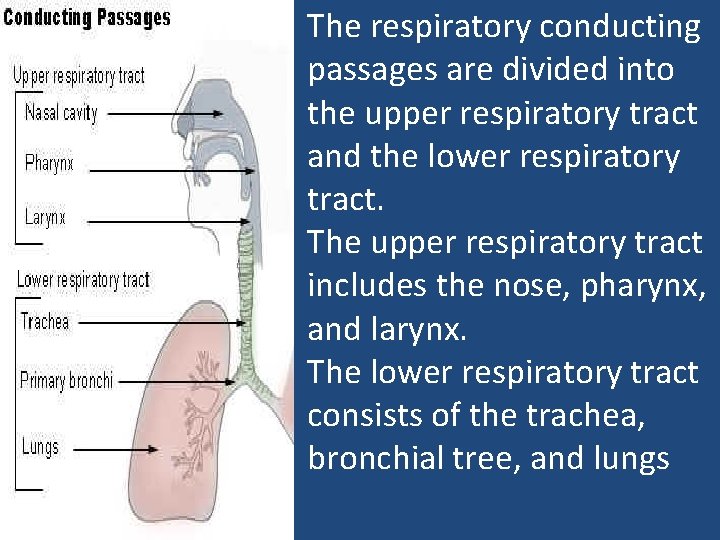
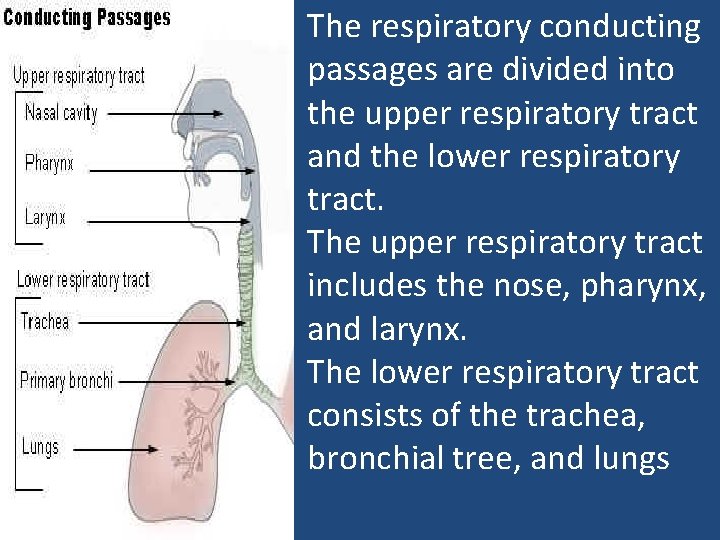
The respiratory conducting passages are divided into the upper respiratory tract and the lower respiratory tract. The upper respiratory tract includes the nose, pharynx, and larynx. The lower respiratory tract consists of the trachea, bronchial tree, and lungs
Functions of upper airway • Filtering out large particulates (30– 50 μm) to prevent them from reaching the conducting and alveolar airways. • Serving to warm and humidify air as it enters the body. • Olfaction.
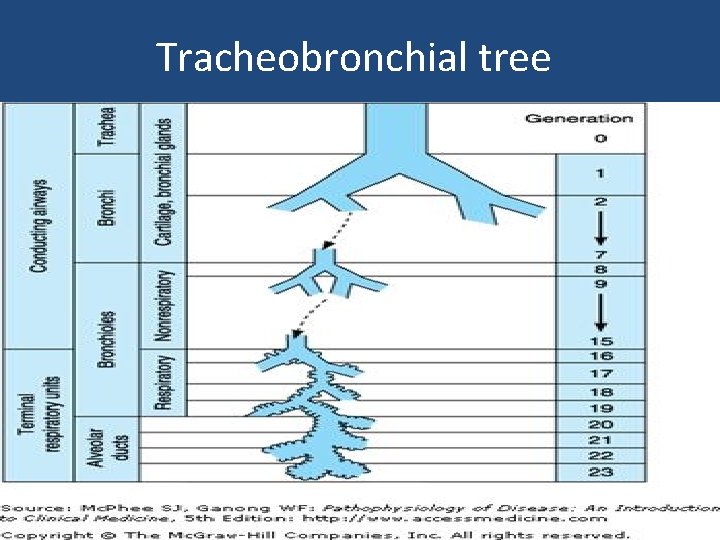
Conducting airway • The conducting airway begins at the trachea and branches greatly expand the surface area of the tissue in the lung. • The first 16 generations of passages form the conducting zone of the airways that transports gas from and to the upper airway. • Branches are made up of bronchi, bronchioles, and terminal bronchioles.
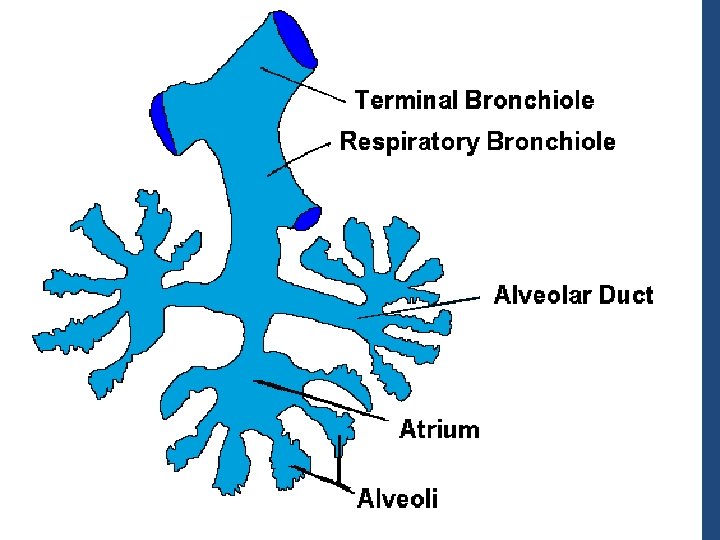
Alveolar Airway • Between the trachea and the alveolar sacs, the airways divide 23 times. • The last seven generations form the transitional and respiratory zones where gas exchange occurs. • Transitional and respiratory bronchioles, alveolar ducts and alveoli. • Total cross-sectional area of the airways increase from 2. 5 cm 2 (trachea) to 11, 800 cm 2 (alveoli)
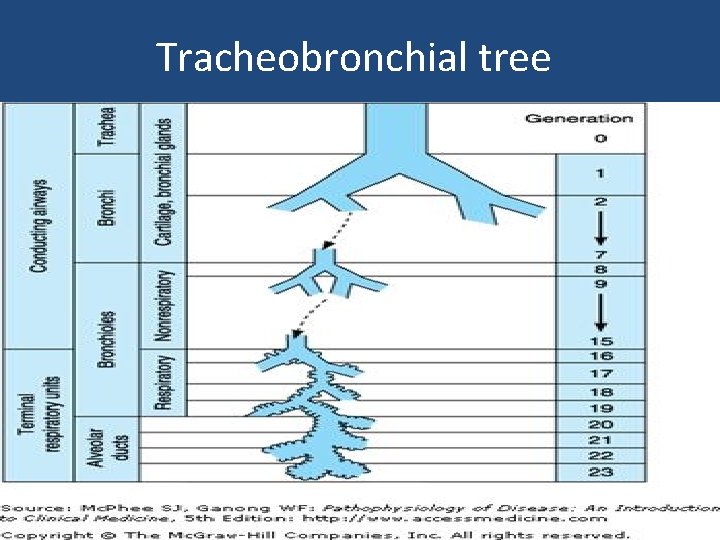
Tracheobronchial tree
The Components of the Respiratory System • Conducting Zone. • Respiratory Zone
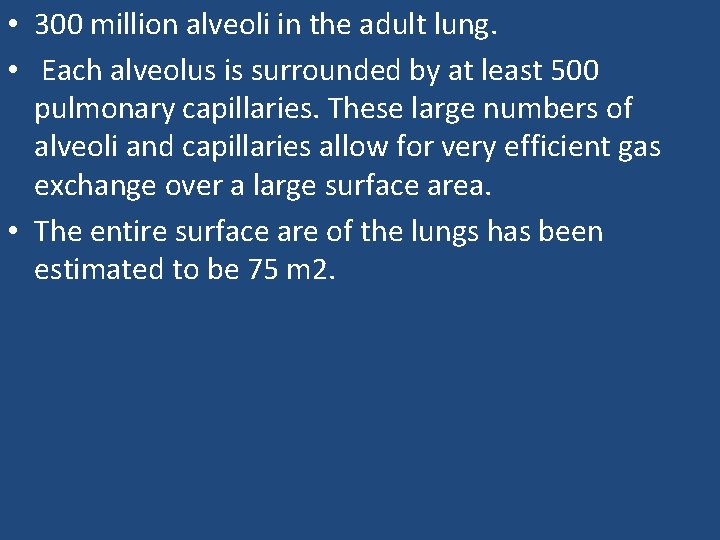
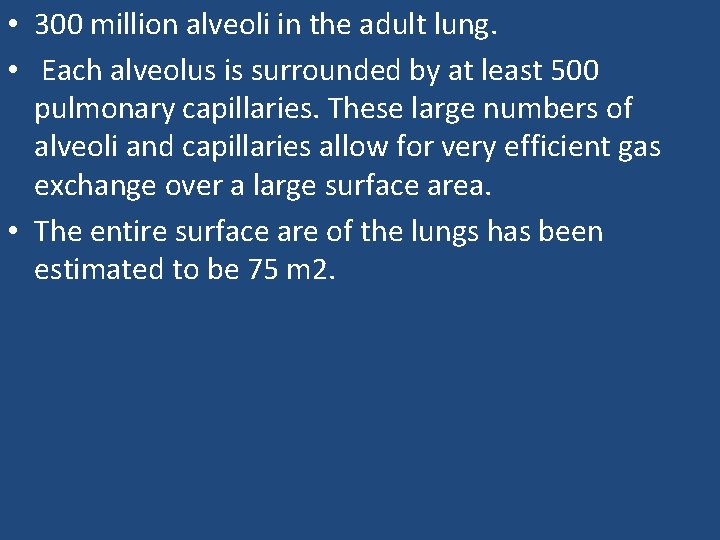
• 300 million alveoli in the adult lung. • Each alveolus is surrounded by at least 500 pulmonary capillaries. These large numbers of alveoli and capillaries allow for very efficient gas exchange over a large surface area. • The entire surface are of the lungs has been estimated to be 75 m 2.
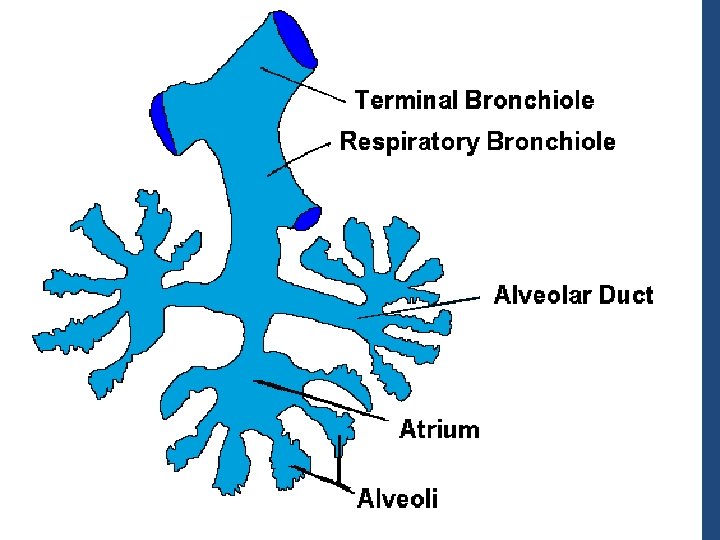
Respiratory unit • • • Respiratory unit Respiratory bronchioles Alveolar ducts Alveolar sacs alveoli
• The alveoli are lined by two types of epithelial cells. • Type I cells – Flat cells with large cytoplasmic extensions. – Primary lining cells of the alveoli ( 95%). – • Type II cells (granular pneumocytes) – Thicker and contain numerous lamellar inclusion bodies. – 5% of the surface area of alveoli.
Type II cells are important in • Alveolar repair • Production of surfactant • Typical lamellar bodies (LB), membrane-bound organelles containing whorls of phospholipid, are formed in these cells. • LB secreted by exocytosis into the fluid lining the alveoli. • The released LB material is converted to tubular myelin (TM). • TM is the source of the phospholipid surface film (SF), lines alveoli.
• This surfactant layer plays an important role in maintaining alveolar structure by reducing surface tension. • Surface tension is inversely proportional to the surfactant concentration per unit area. • The surfactant molecules move further apart as the alveoli enlarge during inspiration, and surface tension increases. • It decreases when they move closer together during expiration.
• The alveoli also contain other specialized cells, including pulmonary alveolar macrophages (PAMs, or AMs), lymphocytes, plasma cells, neuroendocrine cells, and mast cells. • PAMs are an important component of the pulmonary defense system. • PAMs are actively phagocytic and ingest small particles that evade the mucociliary escalator and reach the alveoli.
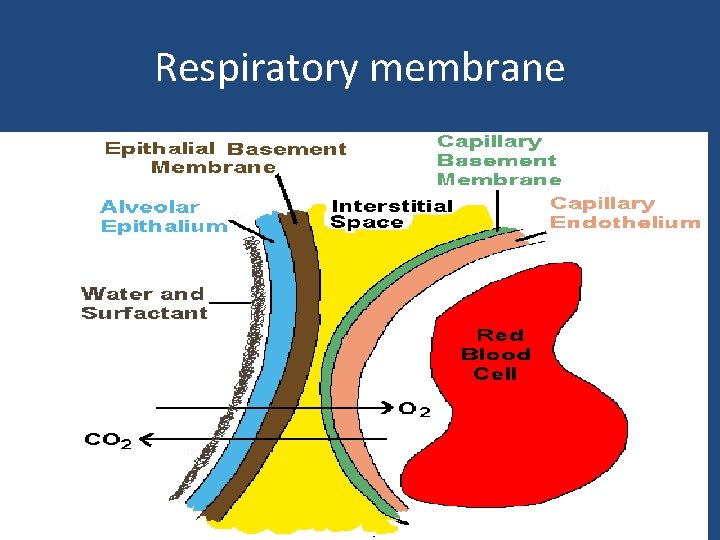
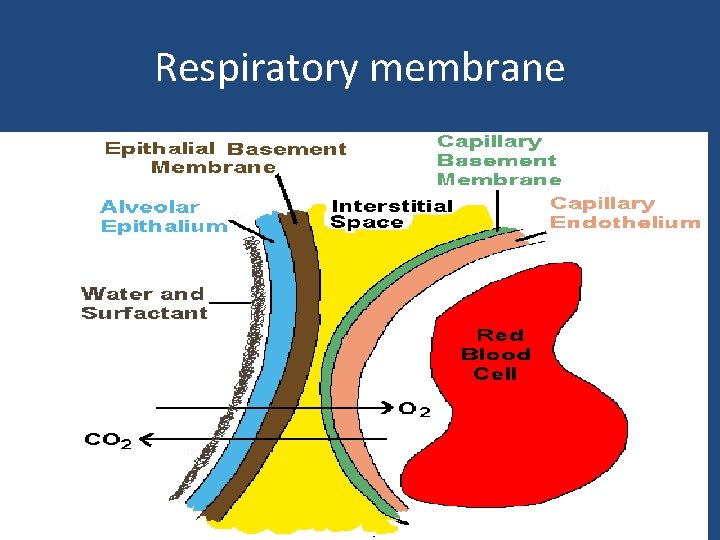
Respiratory membrane
Respiratory Membrane • This air-blood barrier is composed of: – Alveolar and capillary walls – Their fused basal laminas • Alveolar walls: – Are a single layer of type I epithelial cells – Permit gas exchange by simple diffusion – Secrete angiotensin converting enzyme (ACE) • Type II cells secrete surfactant
 Functional anatomy of the respiratory system
Functional anatomy of the respiratory system Respiratory zone of the respiratory system
Respiratory zone of the respiratory system Bronchopulmonary segment
Bronchopulmonary segment Respiratory system in man
Respiratory system in man Functional anatomy of the digestive system
Functional anatomy of the digestive system Transpalatal arch space maintainer
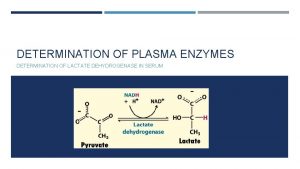
Transpalatal arch space maintainer Non functional plasma enzyme
Non functional plasma enzyme Plasma enzyme
Plasma enzyme Functional and non functional
Functional and non functional Site:slidetodoc.com
Site:slidetodoc.com Physiology of respiration
Physiology of respiration Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Structure of the upper respiratory system
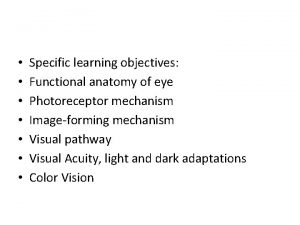
Structure of the upper respiratory system Cyanopsin color
Cyanopsin color Functional anatomy of prokaryotic and eukaryotic cells
Functional anatomy of prokaryotic and eukaryotic cells Tiny air sacs at the end of the bronchioles
Tiny air sacs at the end of the bronchioles Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Simplest equivalent of concurrent force system is
Simplest equivalent of concurrent force system is Force system in mechanics
Force system in mechanics Bozeman respiratory system
Bozeman respiratory system Unit 9 respiratory system
Unit 9 respiratory system Diagnostic test of respiratory system
Diagnostic test of respiratory system Respiratory system
Respiratory system What is larynx
What is larynx Respiratory system coloring page
Respiratory system coloring page Respiratory system purpose
Respiratory system purpose Conclusion respiratory system
Conclusion respiratory system The energy-releasing process that is fueled by oxygen
The energy-releasing process that is fueled by oxygen Chapter 7:10 respitory system
Chapter 7:10 respitory system