RESPIRATORY SYSTEM FUNCTIONAL ANATOMY AND PHYSIOLOGY Lungs occupy



- Slides: 81
RESPIRATORY SYSTEM
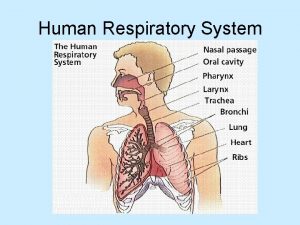
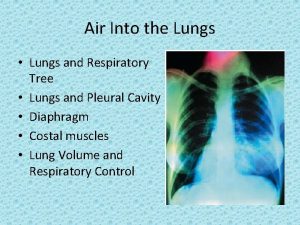
FUNCTIONAL ANATOMY AND PHYSIOLOGY �Lungs occupy upper two thirds bony thorax �Inspiration involves downward contraction of diaphragm outward & upward movement of the ribs at costovertebral joints caused by external intercostal muscles
�Expiration is passive due to elastic recoil of lungs
Lung mechanics �Healthy alveolar walls contain a fine network of elastin and collagen fibres �The volume of the lungs at the end of breath out is called the functional residual capacity (FRC)
�At this volume the inward elastic recoil of the lungs (resulting from elastin fibres and the surface tension in the alveoli) is balanced by the resistance of the chest wall to inward distortion, causing negative pressure in the pleural space
�Elastin fibres allow the lungs to be easily distended but collagen fibres restrict expansion �So in health, the maximum inspiratory volume is limited by the lung (rather than chest wall)
�Elastin fibres in the alveolar walls maintains small airway patency by radial traction on the airway walls �During normal breathing, small airways narrow during expiration because of surrounding high alveolar pressure, but are prevented from collapsing by radial traction
�So the volume that can be exhaled is thus limited purely by capacity of expiratory muscles to distort chest wall inwards. �In emphysema loss of alveolar walls, leaves the small airways unsupported and their collapse on expiration causes air trapping and high end expiratory volume
Control of breathing �Respiratory motor neurons in the medulla are the origin of the respiratory cycle �Their activity is modulated by multiple external inputs in health and in disease � Central chemoreceptors in the ventrolateral medulla sense the p. H of the cerebrospinal fluid (CSF) and are indirectly stimulated by a rise in arterial. PCO 2
�The carotid bodies sense hypoxaemia & are activated by arterial PO 2 values below 8 KPa(60 mm. Hg). �Cortical(volitional) and limbic(emotional) influences can override the automatic control of breathing
� The lungs are designed for gaseous exchange (oxygen uptake and carbon dioxide elimination) through the process of ventilation and molecular diffusion �To maintain health, purified air must be presented to the alveolar epithelial surface to aerate pulmonary capillary blood
�Ambient air, which contains environmental debris, microbes, and possibly solubilized toxins must be cleaned �Cleaning is done by system of host defenses that usually removes these contaminants
�Mechanically (by sneezing, rhinorrhea, coughing, and mucociliary clearance) �Innate (natural) immunity or adaptive (acquired) immunity �This immunity is compromised by systemic illness or the side effects of other medical therapy
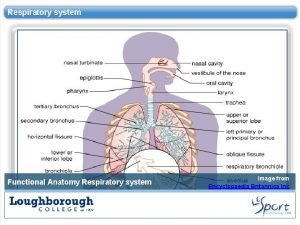
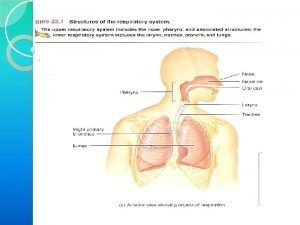
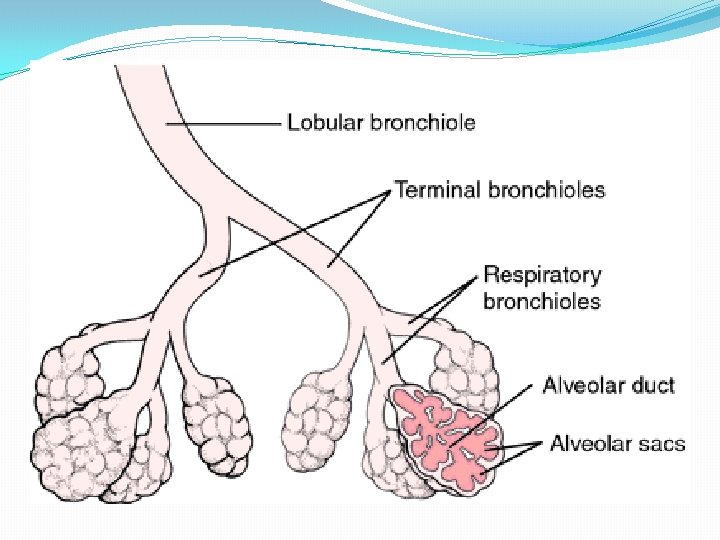
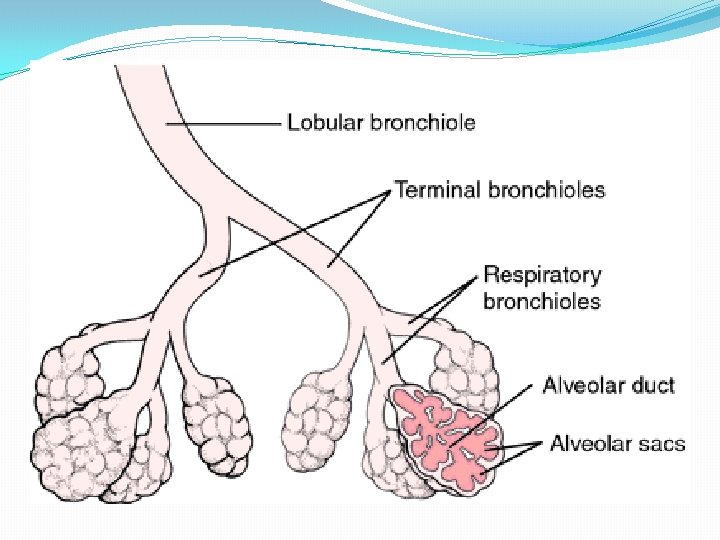
�Although the respiratory tract is a unit of branching tubes leading to the air exchange– alveolar surface, it functionally has distinct anatomic segments �Naso-oropharynx or upper airways �Conducting airways (larynx, trachea, and bronchi that branch to terminal bronchioles) �Respiratory bronchioles, alveolar ducts and alveoli
�Vascular and neural structures are integral to each segment �Lymphatic channels begin at the level of respiratory bronchioles and flow upward into the hilar nods
�The airways and their accompanying blood supply develop from the foregut and primitive esophagus �The conducting airway system has approximately 14 generations of branches, which are extended by another 10 branches within the acinar airways, finally ending as alveolar sacs
�Later developments in the foetus initiate progressive thinning of the mucosal epithelial layer in distal bronchi and then the respiratory bronchioles to a single cell surface
�Because this mucosal surface that lines the airways down to the respiratory bronchioles is in breath-to-breath contact with the external environment, mechanisms to clean inspired air are dispersed along the entire tract
�Deglutition and respiration are coordinated exquisitely by the epiglottis and laryngeal musculature to direct fluids and food into the esophagus and air into the subglottic trachea �Control is not perfect, aspiration can occur in normal persons during sleep causing cough and asthma
�The surface of the nasal mucosa is similar to that in the lower conducting airways with respect to ciliary function and immunologic components �Mucociliary clearance declines with age, causing more frequent occurrence of respiratory infections in the elderly
�The conducting airways begin with the trachea, 10 cm in length �At the carina, it divides into two major bronchi, and then multiple smaller bronchial branches �Branching reduces resistance to airflow and reduces the speed of air as it prepares to enter the acinar ducts and alveolar sacs
�Here any 0. 5 - to 3 -μm particulates settle out if present by the slower movement the air �The thickness of the mucosal surface attenuates as the pseudostratified cell layer flattens to become a single cell layer in the terminal bronchioles
�Here the less protected surface may become more vulnerable to injury from inhaled toxins and microbes producing chronic inflammation (bronchiolitis)

�The respiratory bronchioles, which are positioned between the distal conducting airways and the alveolized air exchange surface, functionally separate the upper and lower respiratory tracts
�This segment is a bottleneck for airflow and a last surface to capture small particles and microbial or antigenic debris before the alveolar space as the immune responses can be initiated here
�The respiratory bronchioles can be the site of airway obstruction �Inflammation typical of bronchiolitis obliterans, chronic graft rejection after lung transplantation and lung involvement by collagen vascular diseases
�In this transition segment, several changes occur �Single-layer cuboidal epithelial surface further differentiates into alveolar type I cells that cover the alveolar lining surface & type II cells(pneumocytes)
�Type II pneumocytes produce surfactant that reduces surface tension and counteracts tendency of alvevoli to collapse under surface tension
�Pulmonary brush cells with microvilli are dense in this area and may be involved with chemosensing or trapping of inhaled particles and pollutants as well as with regulation of fluid and solute absorption
�Surface host defenses change from mucociliary clearance to macrophage phagocytes, inflammatory cells (neutrophils or eosinophils), and opsonins �Finally, the changeover is made from the bronchial arterial blood supply for the conducting airways to the pulmonary artery –pulmonary capillary blood
�The air exchange compartment, or the alveolar space, is composed of about 480 million alveoli supported by a fibrous scaffolding and intertwined with a meshwork of pulmonary artery capillaries that permit air-blood contact(distance is < 0. 4 micron)
VENTILATION & PERFUSION �Gravity determines the distribution of ventilation and blood flow in the lungs �Most ventilation and perfusion goes to dependent zones �Locally, hypoxia constricts pulmonary arterioles and airway CO 2 dilates bronchi
�Diseases which impair ventilation locally result in desaturated and CO 2 -laden blood entering the pulmonary veins, causing arterial hypoxaemia
�Increased ventilation of remaining normal lung units increase CO 2 excretion, correcting arterial CO 2 to normal, but cannot augment oxygen uptake or correct hypoxaemia, because maximal oxygen uptake in these normal lung units is limited by the capacity of haemoglobin
�The resulting pattern of blood gas abnormality is hypoxia with normocapnia, which is termed 'type I respiratory failure
�Hypoxia with hypercapnia is termed type II respiratory failure �It is seen if there is severe generalised ventilation-perfusion mismatch (insufficient normal lung to correct CO 2) or a disease which reduces total ventilation
�Ventilation is reduced by diseases of the lung or chest wall & also diseases affecting any part of the neuromuscular mechanism of ventilation like, � brain injury � narcotic poisoning � polyneuropathies � myopathies
�The pulmonary circulation in health operates at low pressure (approximately 24/9 mm. Hg), and can accommodate large increases in flow (e. g. during exercise) without much rise in pressure
�Pulmonary hypertension may result when pulmonary vessels are destroyed by emphysema, obstructed by thrombus or involved in interstitial inflammation or fibrosis
INVESTIGATIONS �A detailed history, thorough examination and basic haematological and biochemical tests usually suggest the likely diagnosis
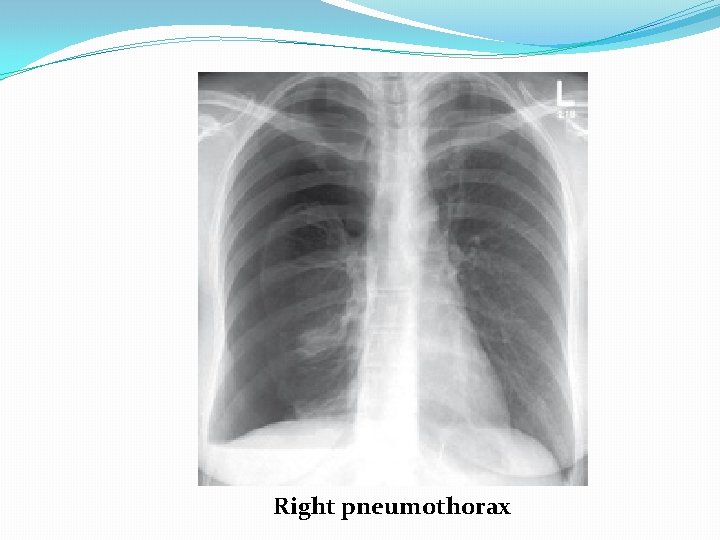
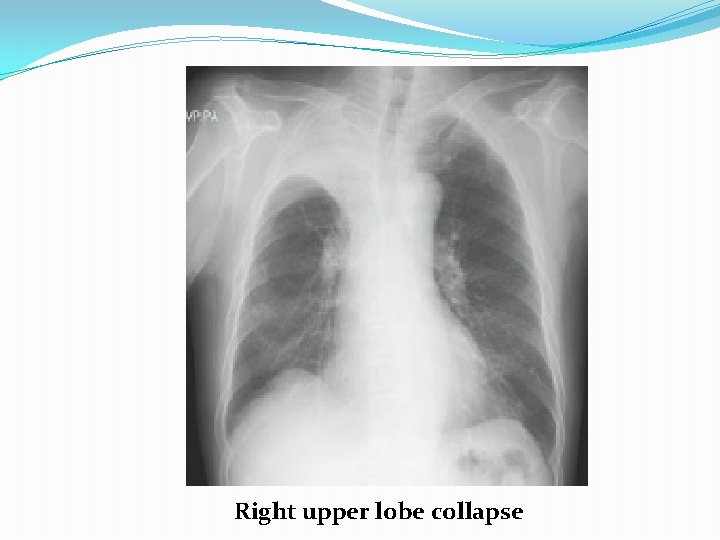
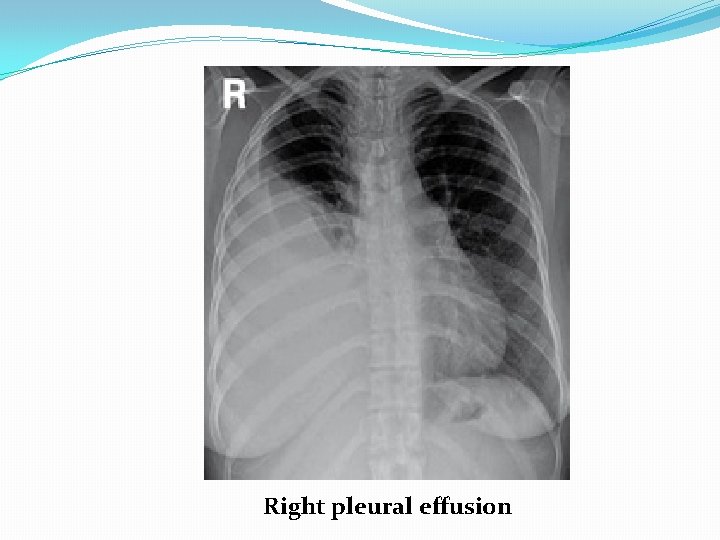
Chest X-RAY �Performed on the majority of patients �A postero-anterior (PA) film provides information on the lung fields, heart, mediastinum, vascular structures and the thoracic cage
�Lateral film, is requested if pathology is suspected behind the heart shadow or deep in the diaphragmatic sulci �Increased shadowing may represent accumulation of fluid, lobar collapse or consolidation
�Consolidation does not change the position of the mediastinum �Presence of an air bronchogram means that proximal bronchi are patent �Collapse (implying obstruction of the proximal bronchus) is accompanied by loss of volume and displacement of the mediastinum towards the affected side
�Ring shadows (diseased bronchi seen endon), tramline shadows (diseased bronchi side-on) or tubular shadows (bronchi filled with secretions) suggests bronchiectasis �Pleural fluid is suggested by a shadow which, in the erect patient, ascends towards the axilla

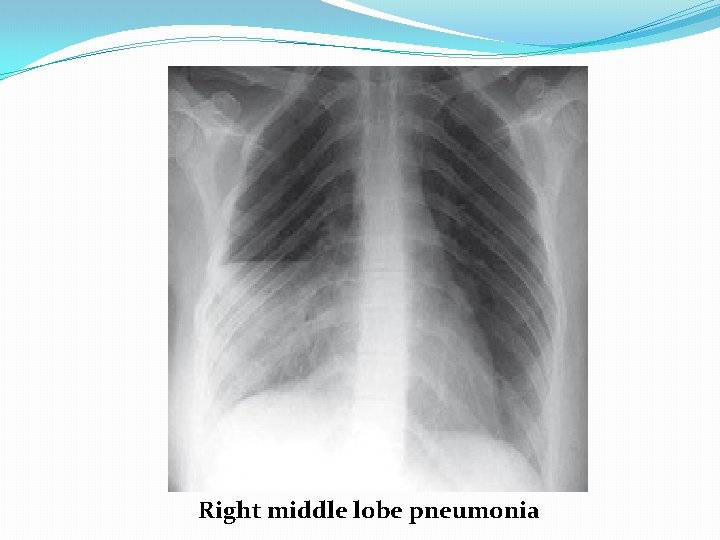
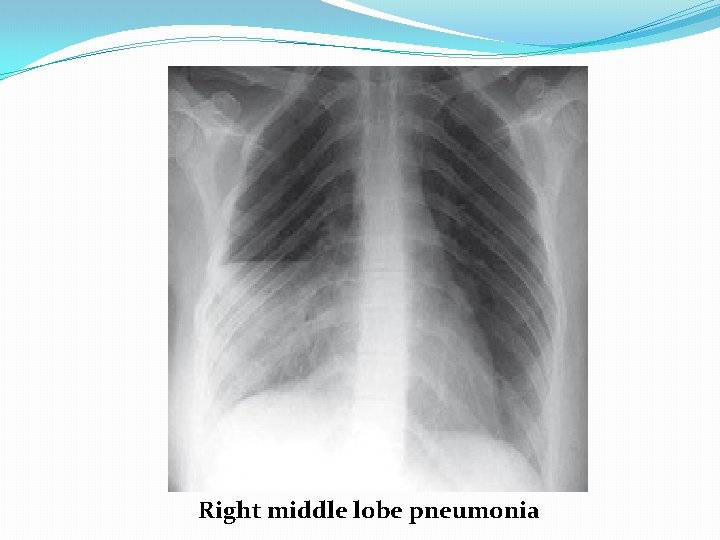
Right middle lobe pneumonia
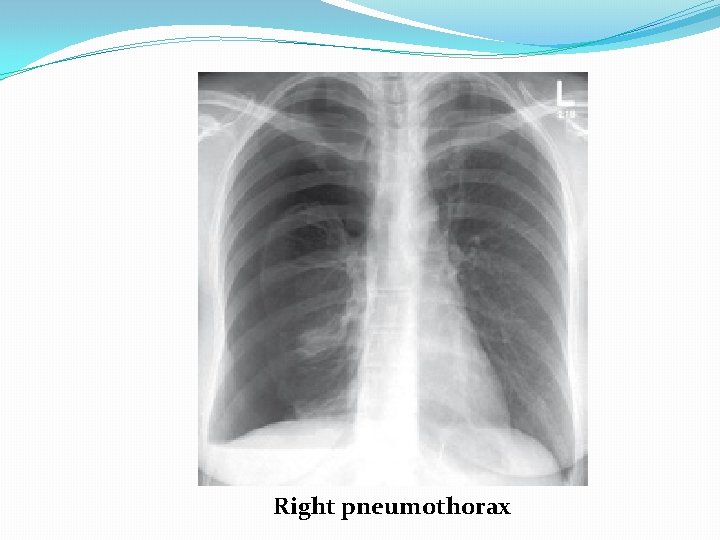
Right pneumothorax
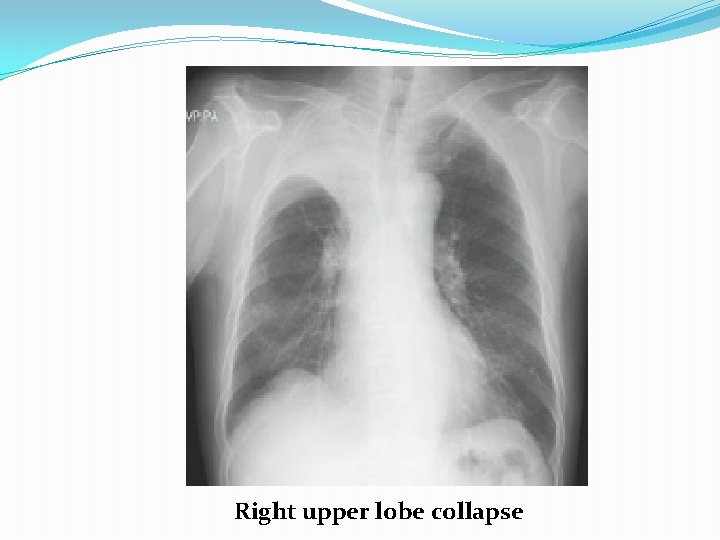
Right upper lobe collapse
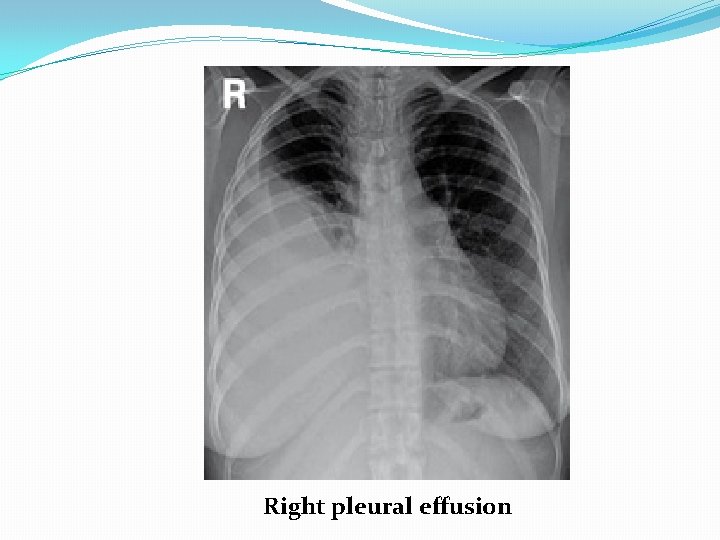
Right pleural effusion
Computed tomography (CT) �CT provides detailed images of the pulmonary parenchyma, mediastinum, pleura and bony structures �CT is superior to chest X ray in determining the position and size of a pulmonary lesion and whether calcification or cavitation is present
�It is now routinely used in the assessment of patients with suspected lung cancer and facilitates guided percutaneous needle biopsy
�High-resolution CT (HRCT) uses thin sections to provide detailed images of the pulmonary parenchyma and is particularly useful in assessing diffuse parenchymal lung disease, e. g. Bronchiectasis, emphysema �CT pulmonary angiography (CTPA) is used in the diagnosis of pulmonary thrombo embolism
Ultrasound �Ultrasound is sensitive at detecting pleural fluid �Helps in pleural biopsy �Endobronchial ultrasound is now possible using specialised bronchoscopes, and is used for imaging and sampling peribronchial lymph nodes
Ventilation–perfusion imaging �Lungs are imaged using a gamma camera that is able to distinguish two isotopes, inhaled 133 Xe (yielding ventilation images) and injected macro aggregates of 99 m. Tcalbumin (yielding perfusion images) �Pulmonary emboli appear as perfusion defects with preserved ventilation
Positron emission tomography (PET) �PET scanners exploit the avid ability of malignant tissue to absorb and metabolise glucose �The radiotracer 18 F-fluorodeoxyglucose (FDG) is administered and rapidly taken up by malignant tissue
�It is then phosphorylated but cannot be metabolised further, being ‘trapped’ in the cell �PET is useful in the investigation of pulmonary nodules, and in staging mediastinal lymph nodes and distal metastatic disease in patients with lung cancer
Pulmonary angiography �Images taken with contrast medium in the main pulmonary artery �Rarely used, because now CTPA is widely available

Endoscopic examination �Laryngoscopy �The larynx may be inspected indirectly with a mirror or directly with a laryngoscope � Fibreoptic instruments allow a magnified view
Bronchoscopy �The trachea and larger bronchi may be inspected using either a flexible or a rigid bronchoscope �Flexible bronchoscopy may be performed under local anaesthesia with sedation on an outpatient basis
�Structural changes can be seen �Abnormal tissue in the bronchial lumen or wall can be biopsied �Bronchial brushings, washings or aspirates can be taken for cytological or bacteriological examination
�Small biopsy specimens of lung tissue, can be taken by forceps passed through the bronchial wall (transbronchial biopsies) �Transbronchial needle aspiration(TBNA) may be used to sample mediastinal lymph nodes and in the staging of lung cancer
�Endobronchial ultrasound (EBUS) using a specialised bronchoscope allows directed needle aspiration from peribronchial nodes
Assessment of the mediastinum �Lymph nodes down to the main carina can be sampled using a mediastinoscope passed through a small incision at the suprasternal notch under GA
�Lymph nodes in the lower mediastinum may be biopsied via the oesophagus using endoscopic ultrasound (EUS), an oesophageal endoscope equipped with an ultrasound transducer and biopsy needle
Microbiological investigations �Sputum, pleural fluid, throat swabs, blood and bronchial washings and aspirates can be examined for bacteria and fungi
Histopathological examination �Histopathological examination of biopsy material obtained from pleura, lymph node or lung is done to make a ‘tissue diagnosis’ in lung malignancy or ILD
Cytological examination of exfoliated cells in sputum, pleural fluid or bronchial brushings and washings can support diagnosis of malignancy
Skin tests �The tuberculin test is used in the diagnosis of tuberculosis. �Skin hypersensitivity tests are useful in the investigation of allergic diseases
Respiratory function testing �Lung function tests are essential to measure a person's objective ability to move the ventilatory apparatus in comparison with normal subjects, adjusted for sex, height, ethnicity, and age �Used to aid diagnosis, assess functional impairment, and monitor treatment or progression of disease
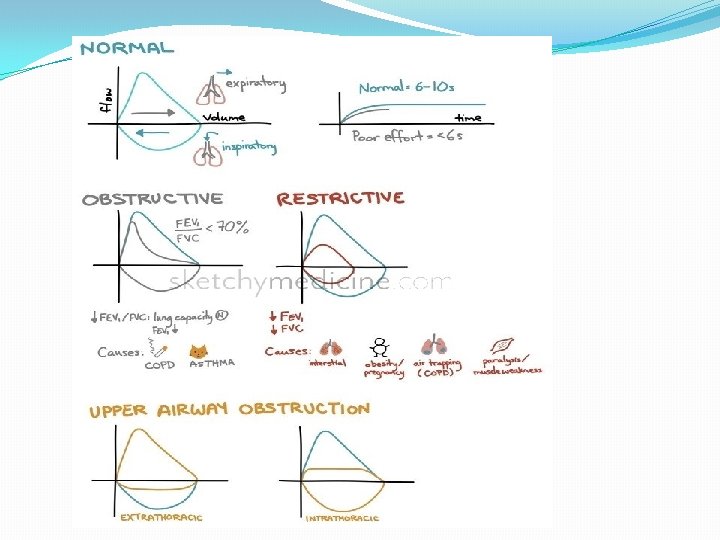
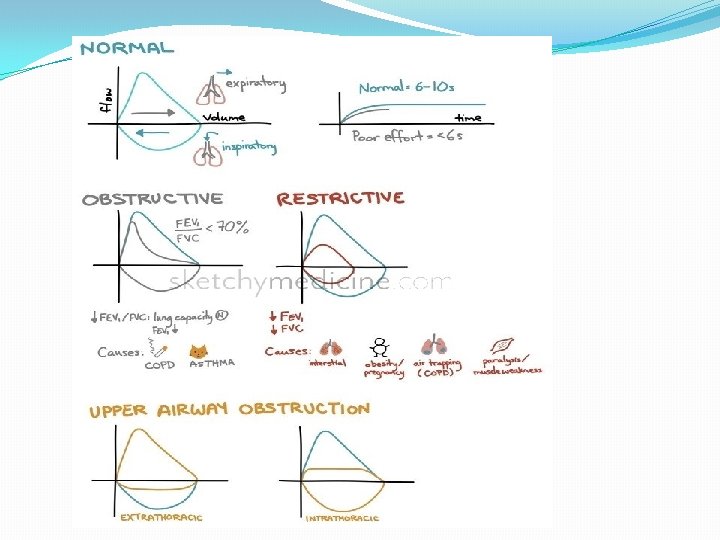
�Basic tests for preliminary assessment and for monitoring disease progression include spirometry �Spirometry is a record of exhaled volume versus time during a forced exhalation �Determination of the response to an inhaled bronchodilator for possible reversible airflow done in asthama
�Obstructive defect: In diseases characterised by airway narrowing (e. g. asthma, bronchitis and emphysema), maximum expiratory flow is limited by dynamic compression of small intrathoracic airways, limiting the volume which can be expired in first minute �FVC is preserved, but the time of exhalation is prolonged
�FEV 1 is disproportionately reduced, resulting in FEV 1/FVC ratios of less than 70% �After the administration of bronchodilators, the FEV 1 and FVC may increase by 10 to 15%, especially in asthma indicating reversibility of airway obstruction
�Restrictive defect: spirometry with symmetric decreases in FEV 1 & FVC �Requires further testing, including lung volume measurement and the diffusion capacity of the lung for carbon monoxide (DLCO)
�A total lung capacity (TLC) less than 80% of the predicted value for a patient's age, race, gender, and height defines restrictive pathophysiology
�Restriction can result from parenchymal disease, neuromuscular weakness, or chest wall or pleural diseases �Restriction with impaired gas exchange (decreased DLCO) suggests parenchymal lung disease
Flow/volume loops �To distinguish large airway narrowing (e. g. Tracheal stenosis or compression) from small airway narrowing, flow/volume loops are recorded using spirometry Lung volumes �Tidal volume and vital capacity (VC) can be measured by spirometry.
�Diffusion capacity measures the transfer of carbon monoxide to indicate how well inspired gases cross the alveolar-interstitialcapillary endothelial interface into blood �Measured by using mixture of 0. 3% carbon monoxide
Thank you
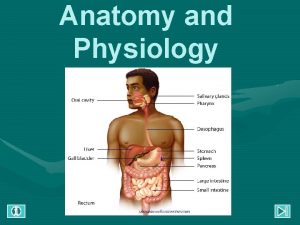
 Respiratory system in man
Respiratory system in man Functional anatomy of the respiratory system
Functional anatomy of the respiratory system Upper respiratory tract
Upper respiratory tract Bronchial tree
Bronchial tree Conducting zone and respiratory zone
Conducting zone and respiratory zone Anatomy and physiology unit 7 cardiovascular system
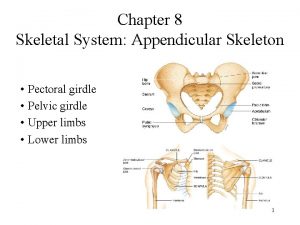
Anatomy and physiology unit 7 cardiovascular system Male vs female skeleton pelvis
Male vs female skeleton pelvis Respiratory digestive and circulatory system
Respiratory digestive and circulatory system Gross anatomy of the lungs
Gross anatomy of the lungs Lesson 9.1 the anatomy of the lungs
Lesson 9.1 the anatomy of the lungs Minute respiratory volume
Minute respiratory volume Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Imperfect flowers examples
Imperfect flowers examples Bone anatomy and physiology
Bone anatomy and physiology Stomach ulcer
Stomach ulcer Segmental anatomy of the liver
Segmental anatomy of the liver Hypogastric region
Hypogastric region Wpigastric region
Wpigastric region Google com
Google com The central sulcus divides which two lobes? (figure 14-13)
The central sulcus divides which two lobes? (figure 14-13) 3 layers of muscle
3 layers of muscle Http://anatomy and physiology
Http://anatomy and physiology Waistline
Waistline Anatomy and physiology of appendix
Anatomy and physiology of appendix Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomical planes
Anatomical planes Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Teks anatomy and physiology
Teks anatomy and physiology Science olympiad forensics cheat sheet
Science olympiad forensics cheat sheet Chapter 2 basic chemistry anatomy and physiology
Chapter 2 basic chemistry anatomy and physiology Stomach anatomy and physiology ppt
Stomach anatomy and physiology ppt Pancreas anatomy and physiology
Pancreas anatomy and physiology Chapter 7 anatomy and physiology
Chapter 7 anatomy and physiology Anatomy and physiology coloring workbook chapter 14
Anatomy and physiology coloring workbook chapter 14 Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Necessary life functions anatomy and physiology
Necessary life functions anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Gi tract histology
Gi tract histology Anatomy and physiology
Anatomy and physiology Chapter 1 introduction to anatomy and physiology
Chapter 1 introduction to anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Cranial cephalic
Cranial cephalic Anatomy and physiology exam 1
Anatomy and physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Anatomy and physiology of the foot
Anatomy and physiology of the foot Skin cancer
Skin cancer Pancreas histology slide
Pancreas histology slide Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Organ orientation
Organ orientation Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 10-1 blood
Figure 10-1 blood Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Human anatomy and physiology 10th edition
Human anatomy and physiology 10th edition Label o
Label o Anatomy and physiology of eye
Anatomy and physiology of eye Cranial nuclei
Cranial nuclei Irn.org anatomy and physiology
Irn.org anatomy and physiology Anatomy and physiology body parts
Anatomy and physiology body parts Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Figure 14-1 anatomy and physiology
Figure 14-1 anatomy and physiology Anatomy and physiology of the retina
Anatomy and physiology of the retina Anatomy and physiology
Anatomy and physiology