Regional Nodal Radiation Therapy Julia S Wong MD














- Slides: 45


Regional Nodal Radiation Therapy Julia S. Wong MD Department of Radiation Oncology Dana-Farber Cancer Institute Brigham and Women's Hospital
I have no relevant disclosures
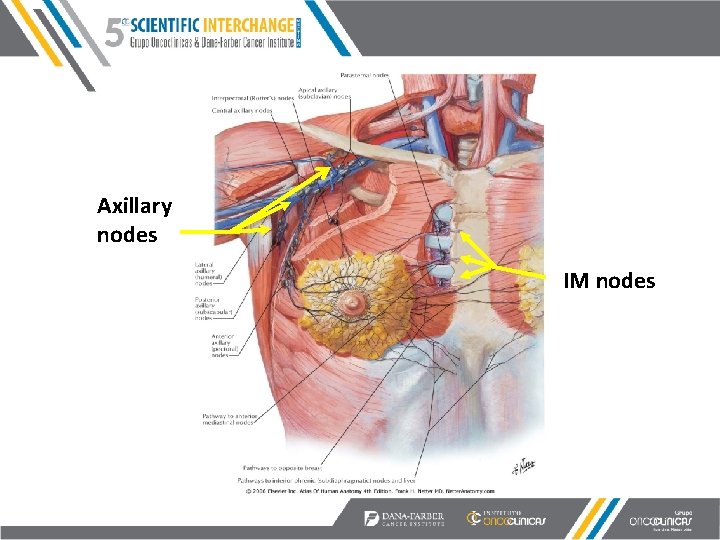
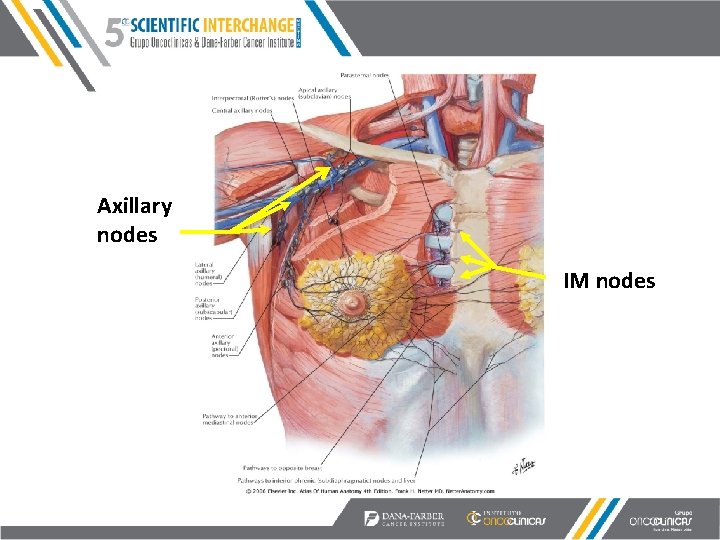
Axillary nodes IM nodes
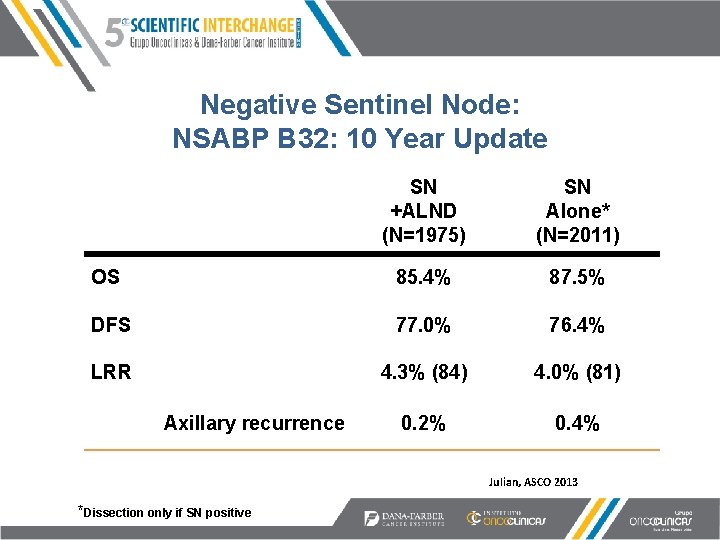
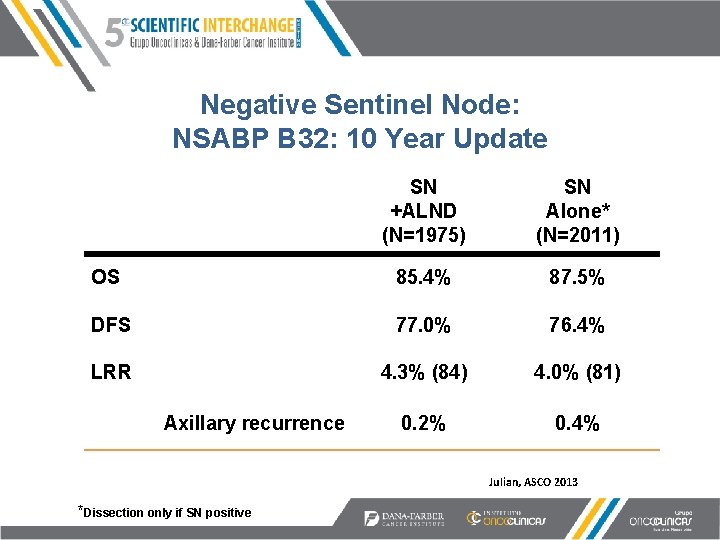
Negative Sentinel Node: NSABP B 32: 10 Year Update SN +ALND (N=1975) SN Alone* (N=2011) OS 85. 4% 87. 5% DFS 77. 0% 76. 4% LRR 4. 3% (84) 4. 0% (81) 0. 2% 0. 4% Axillary recurrence Julian, ASCO 2013 *Dissection only if SN positive
Sentinel Node Positive Patients: Questions • In whom can axillary dissection be safely omitted? • Can RT substitute for completion dissection? • What nodal volume should be irradiated?
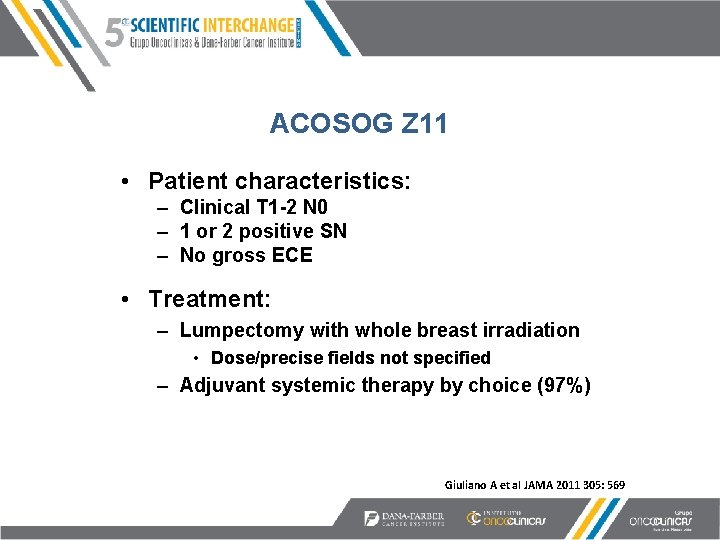
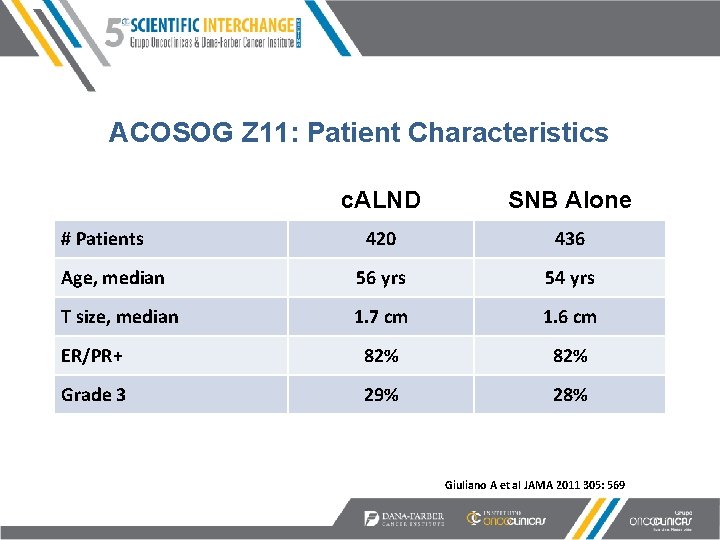
ACOSOG Z 11 • Patient characteristics: – Clinical T 1 -2 N 0 – 1 or 2 positive SN – No gross ECE • Treatment: – Lumpectomy with whole breast irradiation • Dose/precise fields not specified – Adjuvant systemic therapy by choice (97%) Giuliano A et al JAMA 2011 305: 569
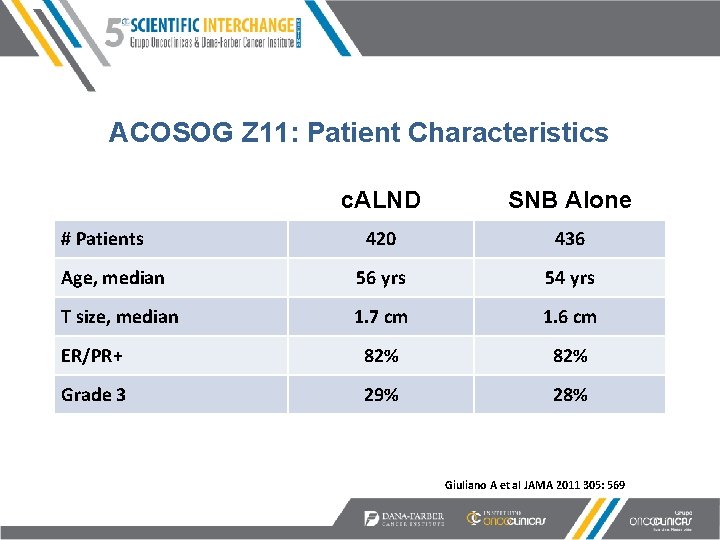
ACOSOG Z 11: Patient Characteristics c. ALND SNB Alone 420 436 Age, median 56 yrs 54 yrs T size, median 1. 7 cm 1. 6 cm ER/PR+ 82% Grade 3 29% 28% # Patients Giuliano A et al JAMA 2011 305: 569
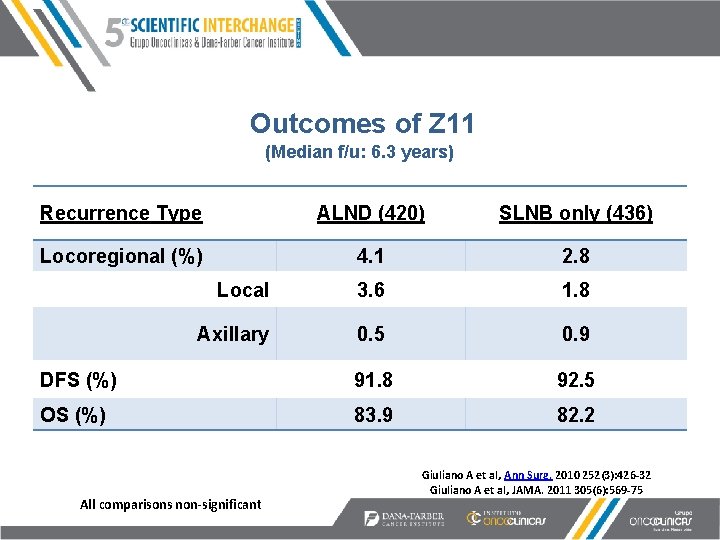
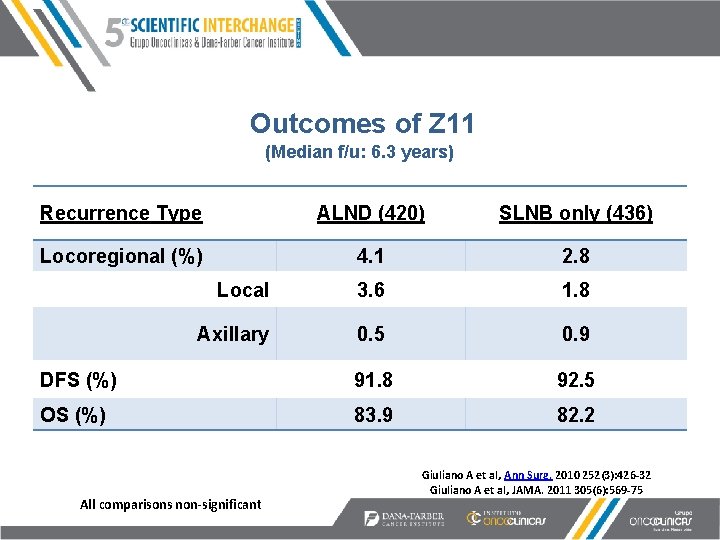
Outcomes of Z 11 (Median f/u: 6. 3 years) Recurrence Type ALND (420) SLNB only (436) Locoregional (%) 4. 1 2. 8 Local 3. 6 1. 8 Axillary 0. 5 0. 9 DFS (%) 91. 8 92. 5 OS (%) 83. 9 82. 2 All comparisons non-significant Giuliano A et al, Ann Surg. 2010 252(3): 426 -32 Giuliano A et al, JAMA. 2011 305(6): 569 -75
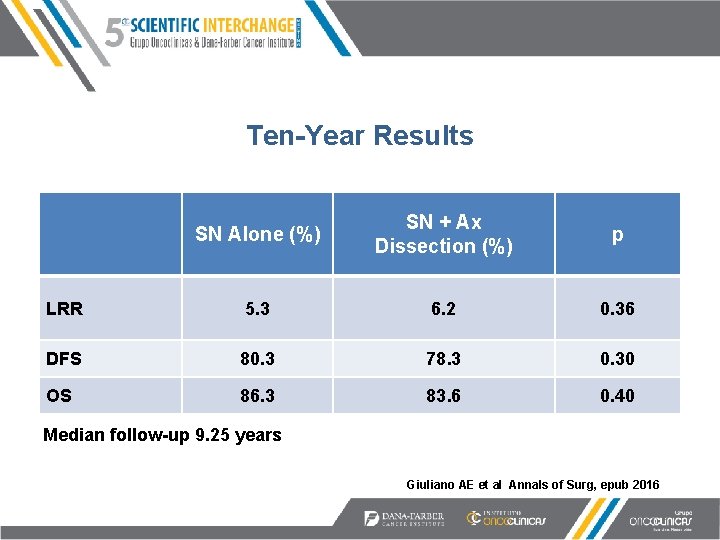
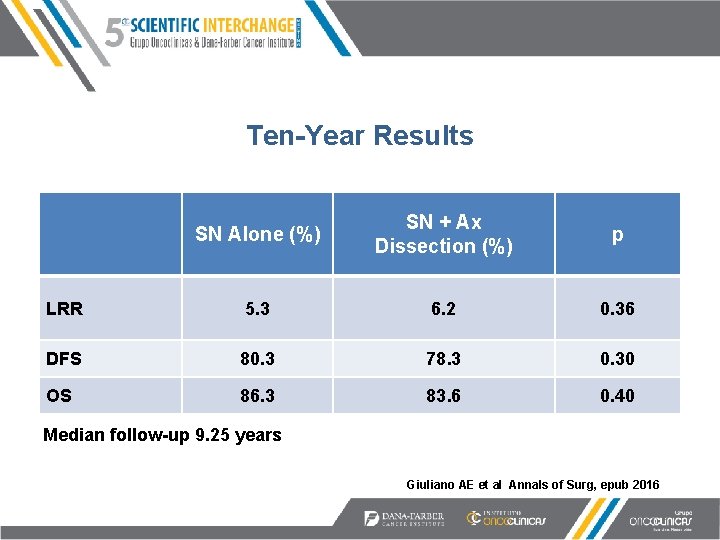
Ten-Year Results SN Alone (%) SN + Ax Dissection (%) p LRR 5. 3 6. 2 0. 36 DFS 80. 3 78. 3 0. 30 OS 86. 3 83. 6 0. 40 Median follow-up 9. 25 years Giuliano AE et al Annals of Surg, epub 2016

Findings on c. ALND in Z 11 • 46% of positive sentinel nodes were micromets • Only 106 (27. 4%) of patients treated with c. ALND had additional positive nodes beyond the SN • This is a highly select group Giuliano A et al JAMA 2011 305: 569
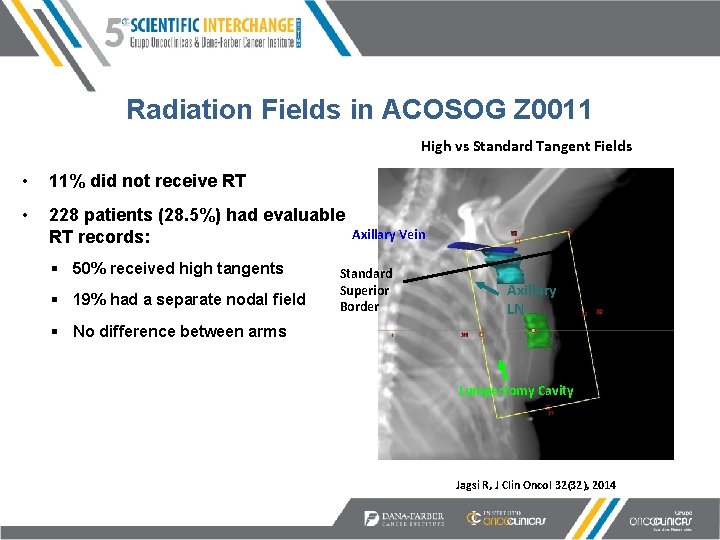
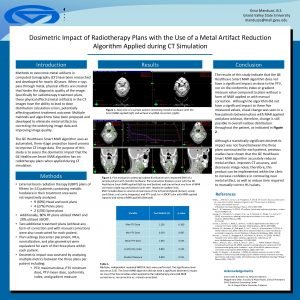
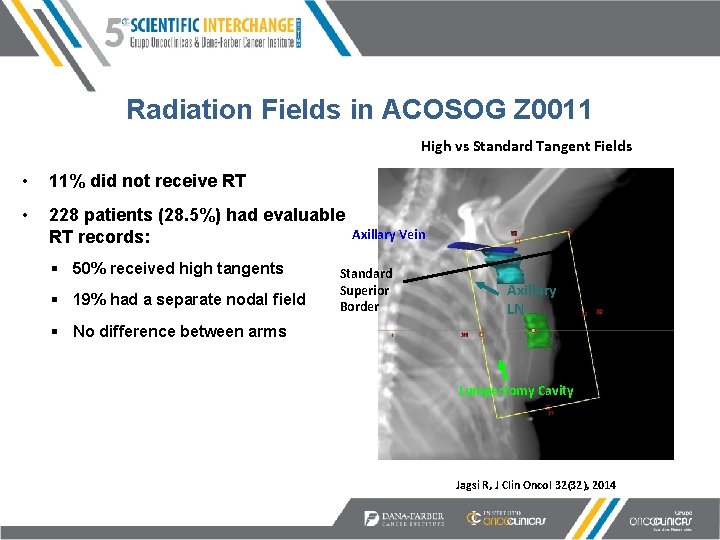
Radiation Fields in ACOSOG Z 0011 High vs Standard Tangent Fields • 11% did not receive RT • 228 patients (28. 5%) had evaluable RT records: § 50% received high tangents § 19% had a separate nodal field Axillary Vein Standard Superior Border Axillary LN § No difference between arms Lumpectomy Cavity Jagsi R, J Clin Oncol 32(32), 2014
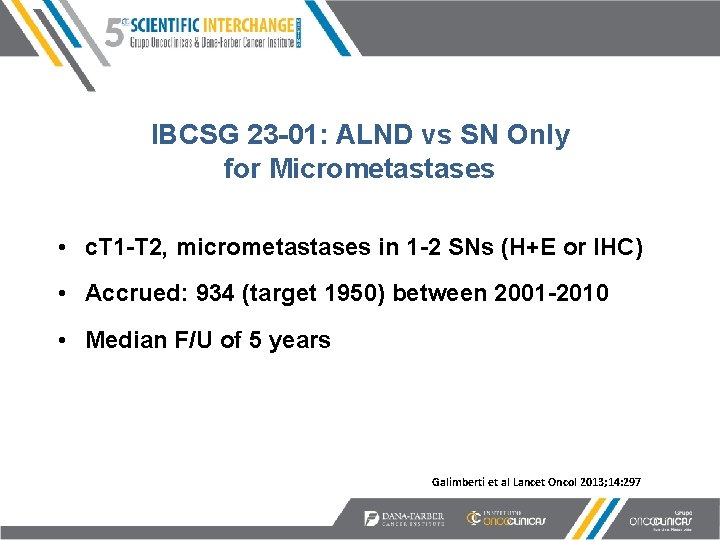
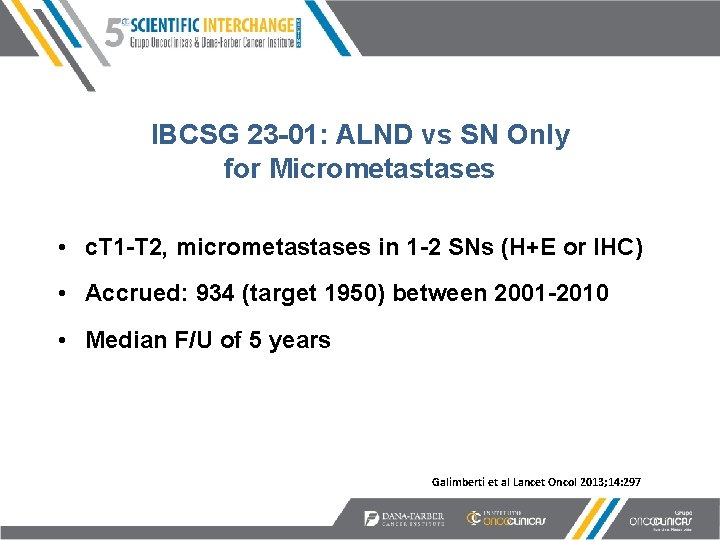
IBCSG 23 -01: ALND vs SN Only for Micrometastases • c. T 1 -T 2, micrometastases in 1 -2 SNs (H+E or IHC) • Accrued: 934 (target 1950) between 2001 -2010 • Median F/U of 5 years Galimberti et al Lancet Oncol 2013; 14: 297

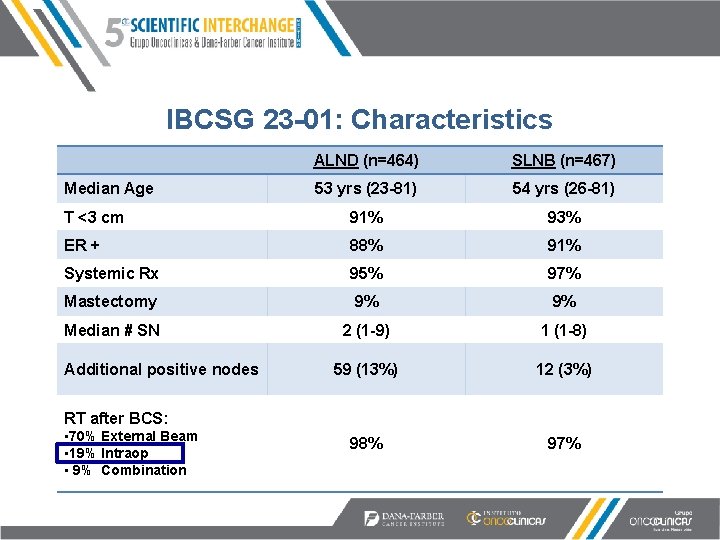
IBCSG 23 -01: Characteristics ALND (n=464) SLNB (n=467) 53 yrs (23 -81) 54 yrs (26 -81) T <3 cm 91% 93% ER + 88% 91% Systemic Rx 95% 97% Mastectomy 9% 9% Median # SN 2 (1 -9) 1 (1 -8) 59 (13%) 12 (3%) 98% 97% Median Age Additional positive nodes RT after BCS: • 70% External Beam • 19% Intraop • 9% Combination
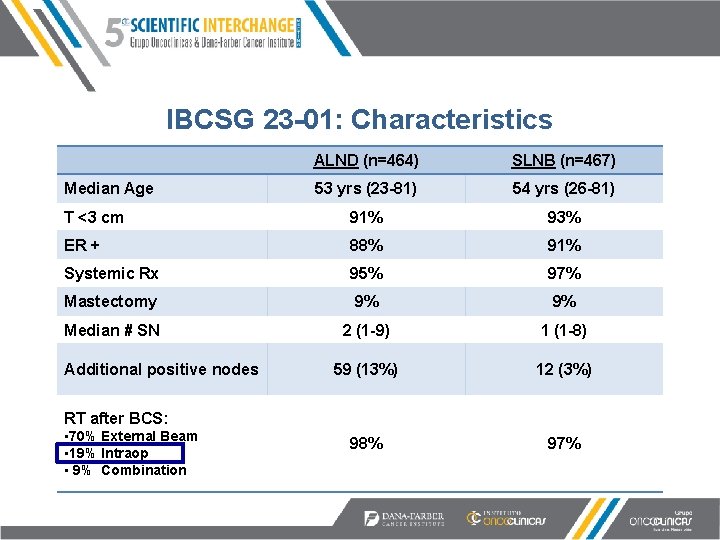
IBCSG 23 -01: Characteristics ALND (n=464) SLNB (n=467) 53 yrs (23 -81) 54 yrs (26 -81) T <3 cm 91% 93% ER + 88% 91% Systemic Rx 95% 97% Mastectomy 9% 9% Median # SN 2 (1 -9) 1 (1 -8) 59 (13%) 12 (3%) 98% 97% Median Age Additional positive nodes RT after BCS: • 70% External Beam • 19% Intraop • 9% Combination
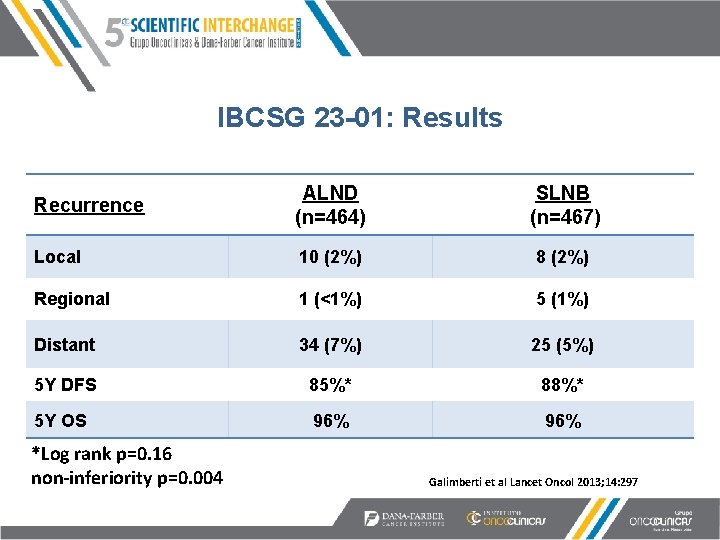
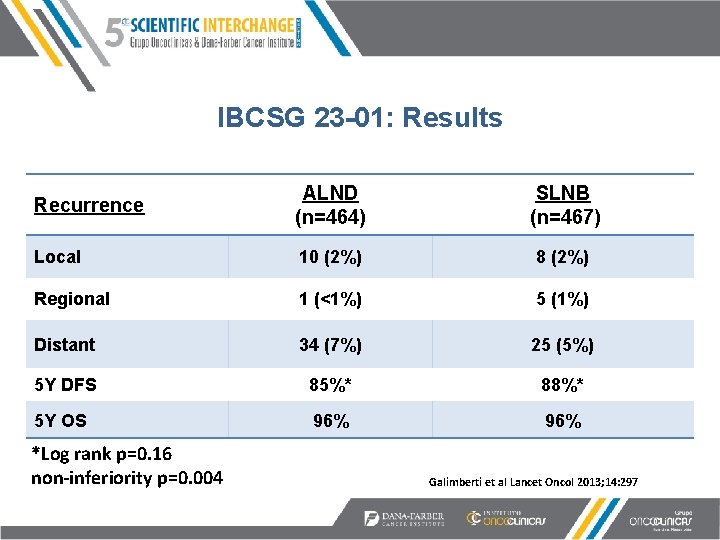
IBCSG 23 -01: Results Recurrence ALND (n=464) SLNB (n=467) Local 10 (2%) 8 (2%) Regional 1 (<1%) 5 (1%) Distant 34 (7%) 25 (5%) 5 Y DFS 85%* 88%* 5 Y OS 96% *Log rank p=0. 16 non-inferiority p=0. 004 Galimberti et al Lancet Oncol 2013; 14: 297
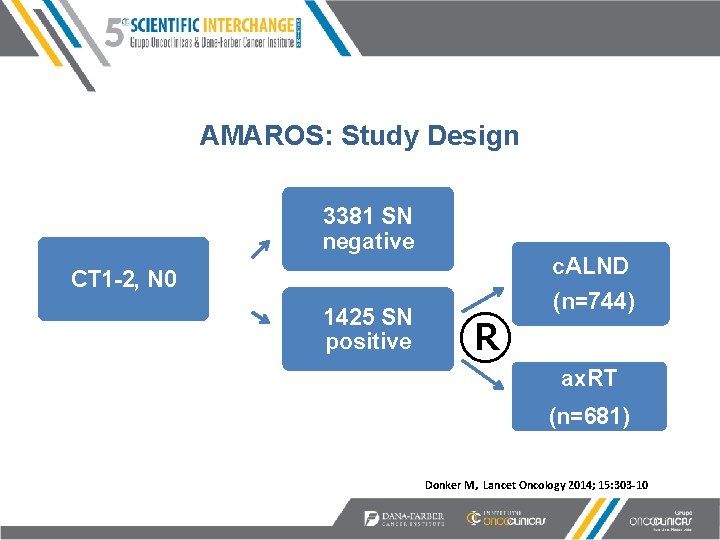
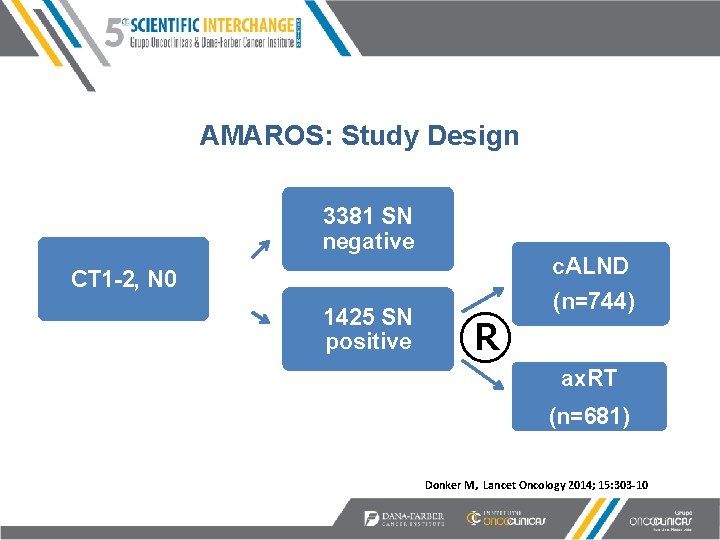
AMAROS: Study Design 3381 SN negative CT 1 -2, N 0 1425 SN positive ® c. ALND (n=744) ax. RT (n=681) Donker M, Lancet Oncology 2014; 15: 303 -10

AMAROS: Patient Characteristics Axillary Dissection (n=744) Axillary RT (n=681) 56 55 0 -2 cm 612 (82%) 533 (78%) 2 -5 cm 132 (18%) 143 (21%) >5 cm 0 1 (<1%) I 179 (24%) 154 (23%) II 356 (48%) 311 (46%) III 192 (26%) 200 (29%) Mastectomy 127 (17%) 121 (18%) Any systemic therapy 666 (90%) 612 (90%) # positive nodes: 1 581 (78%) 512 (75%) 2 127 (17%) 134 (20%) 3 29 (4%) 27 (4%) >3 7 (1%) 8 (1%) Age Tumor size: Grade:
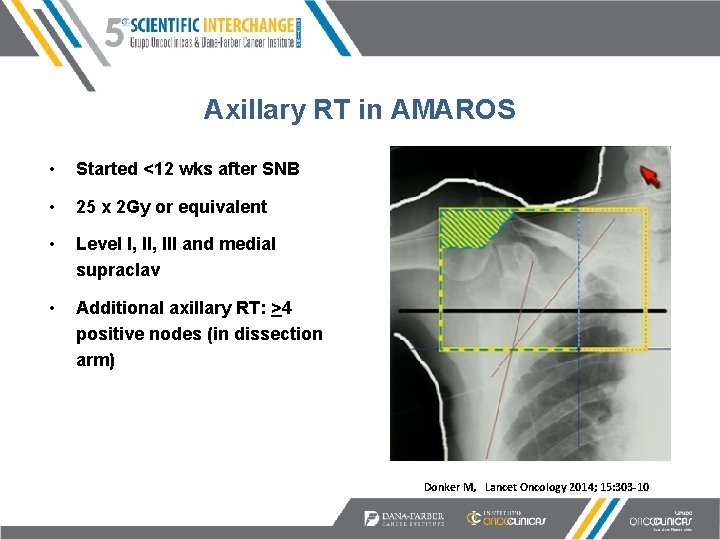
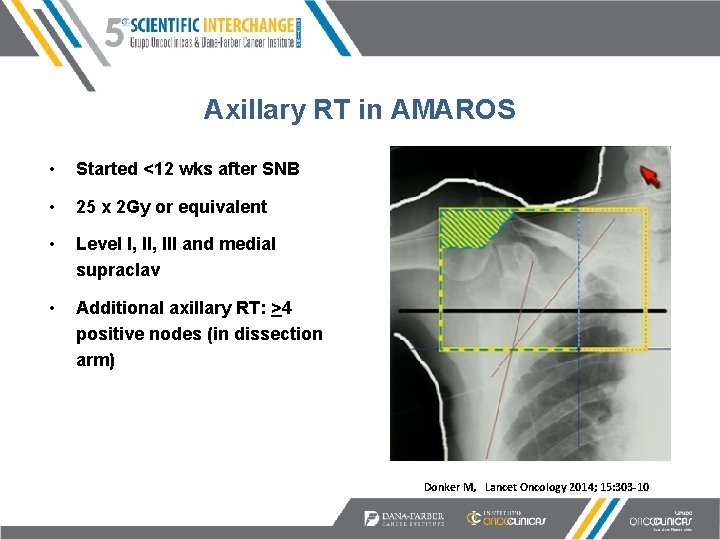
Axillary RT in AMAROS • Started <12 wks after SNB • 25 x 2 Gy or equivalent • Level I, III and medial supraclav • Additional axillary RT: >4 positive nodes (in dissection arm) Figure adapted from Harris, J Donker M, Lancet Oncology 2014; 15: 303 -10

AMAROS Results (Median f/u 6. 1 years) c. ALND n=744 Ax. RT n=681 0. 54% (n=4) 1. 03% (n=7) 5 Y DFS 87% 83% 5 Y OS 94% 5 yr Clinical Lymphedema 23% 11% P<0. 0001 5 -yr Axillary recurrence Donker M, Lancet Oncology 2014; 15: 303 -10
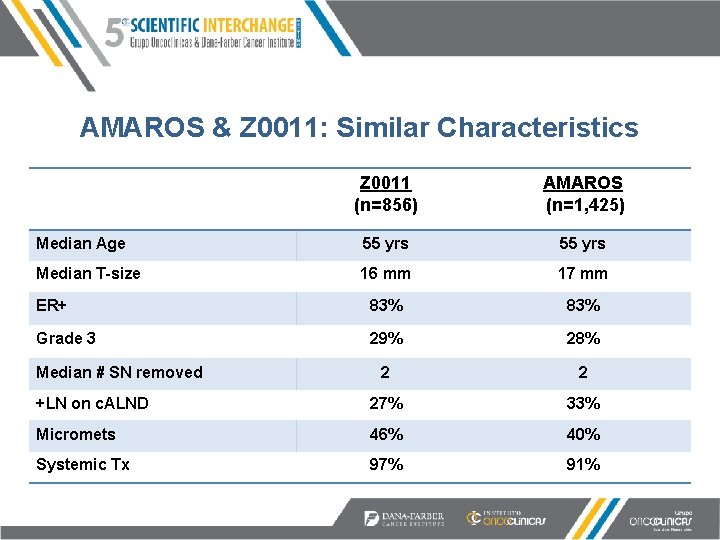
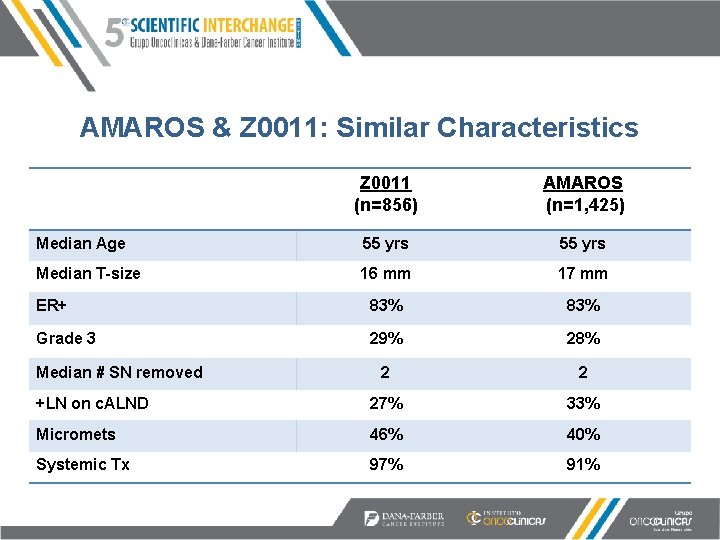
AMAROS & Z 0011: Similar Characteristics Z 0011 (n=856) AMAROS (n=1, 425) Median Age 55 yrs Median T-size 16 mm 17 mm ER+ 83% Grade 3 29% 28% 2 2 +LN on c. ALND 27% 33% Micromets 46% 40% Systemic Tx 97% 91% Median # SN removed
Substituting RT for Surgery • All of these trials indicate RT can substitute for c. ALND – At least in fairly select patients • But what volume to irradiate? – – Tangents alone? High tangents? Supraclav? IMN?
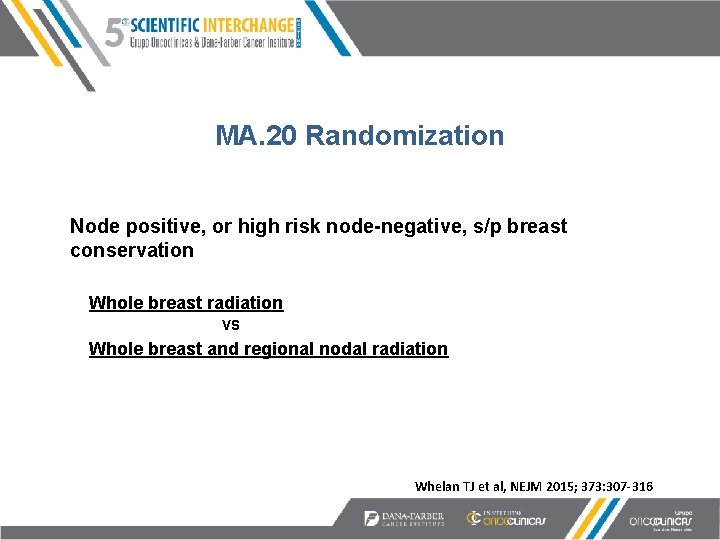
MA. 20 Randomization Node positive, or high risk node-negative, s/p breast conservation Whole breast radiation VS Whole breast and regional nodal radiation Whelan TJ et al, NEJM 2015; 373: 307 -316
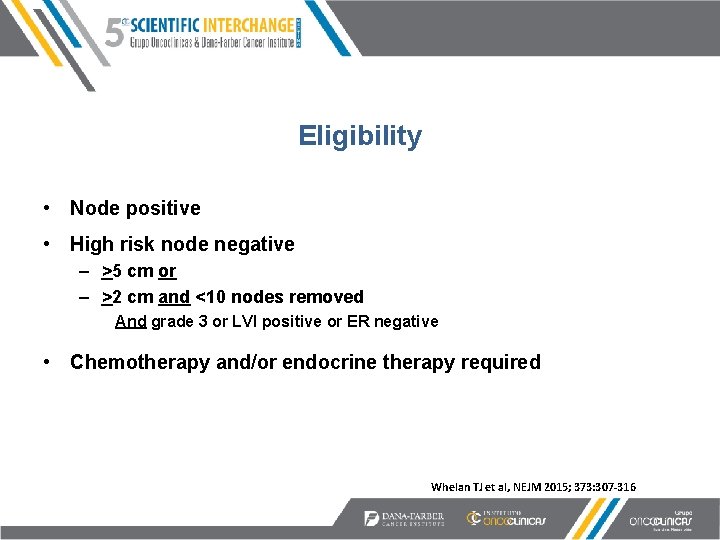
Eligibility • Node positive • High risk node negative – >5 cm or – >2 cm and <10 nodes removed And grade 3 or LVI positive or ER negative • Chemotherapy and/or endocrine therapy required Whelan TJ et al, NEJM 2015; 373: 307 -316
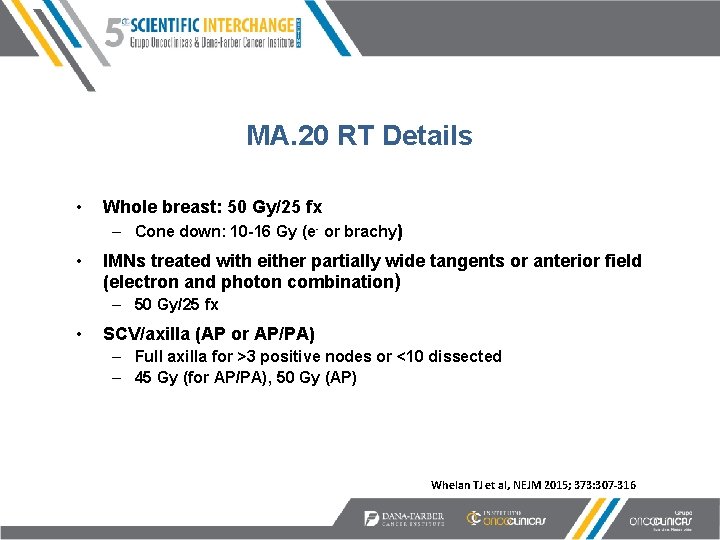
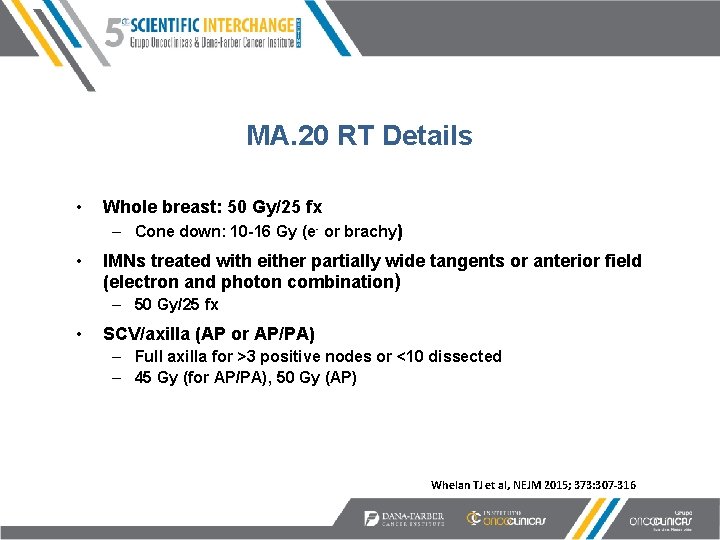
MA. 20 RT Details • Whole breast: 50 Gy/25 fx – Cone down: 10 -16 Gy (e- or brachy) • IMNs treated with either partially wide tangents or anterior field (electron and photon combination) – 50 Gy/25 fx • SCV/axilla (AP or AP/PA) – Full axilla for >3 positive nodes or <10 dissected – 45 Gy (for AP/PA), 50 Gy (AP) Whelan TJ et al, NEJM 2015; 373: 307 -316
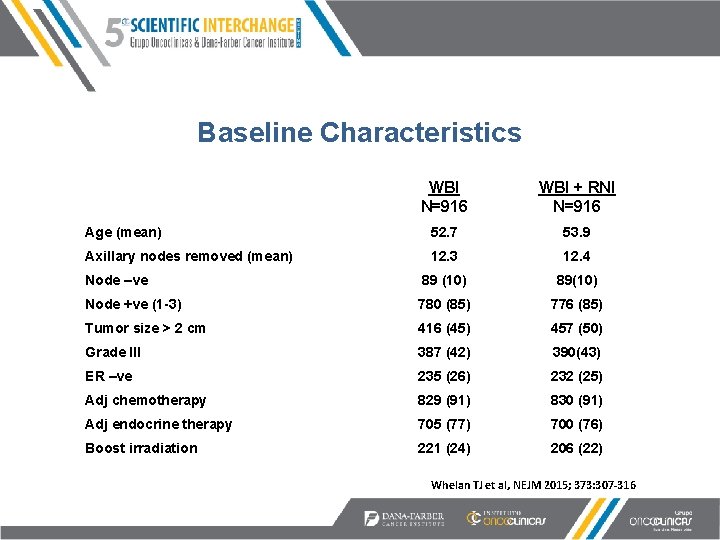
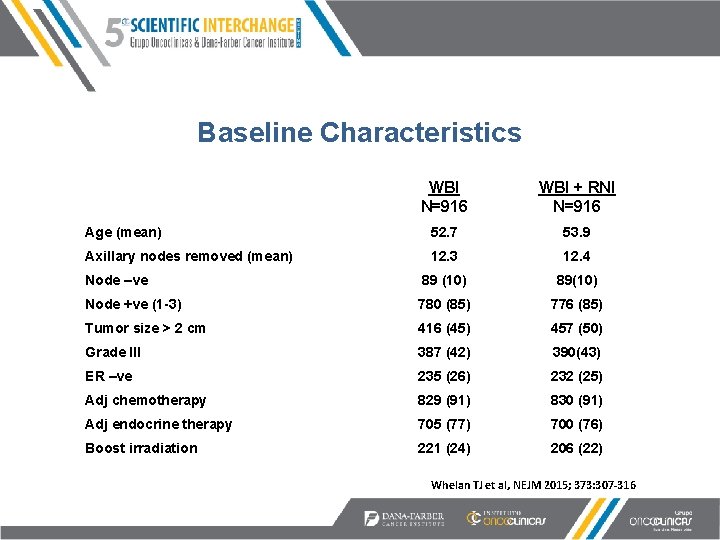
Baseline Characteristics WBI N=916 WBI + RNI N=916 Age (mean) 52. 7 53. 9 Axillary nodes removed (mean) 12. 3 12. 4 Node –ve 89 (10) 89(10) Node +ve (1 -3) 780 (85) 776 (85) Tumor size > 2 cm 416 (45) 457 (50) Grade III 387 (42) 390(43) ER –ve 235 (26) 232 (25) Adj chemotherapy 829 (91) 830 (91) Adj endocrine therapy 705 (77) 700 (76) Boost irradiation 221 (24) 206 (22) in 39% Whelan TJ et al, NEJM 2015; 373: 307 -316

Baseline Characteristics WBI N=916 WBI + RNI N=916 Age (mean) 52. 7 53. 9 Axillary nodes removed (mean) 12. 3 12. 4 Node –ve 89 (10) 89(10) Node +ve (1 -3) 780 (85) 776 (85) Tumor size > 2 cm 416 (45) 457 (50) Grade III 387 (42) 390(43) ER –ve 235 (26) 232 (25) Adj chemotherapy 829 (91) 830 (91) Adj endocrine therapy 705 (77) 700 (76) Boost irradiation 221 (24) 206 (22) in 39% Whelan TJ et al, NEJM 2015; 373: 307 -316

Baseline Characteristics WBI N=916 WBI + RNI N=916 Age (mean) 52. 7 53. 9 Axillary nodes removed (mean) 12. 3 12. 4 Node –ve 89 (10) 89(10) Node +ve (1 -3) 780 (85) 776 (85) Tumor size > 2 cm 416 (45) 457 (50) Grade III 387 (42) 390(43) ER –ve 235 (26) 232 (25) Adj chemotherapy 829 (91) 830 (91) Adj endocrine therapy 705 (77) 700 (76) Boost irradiation 221 (24) 206 (22) in 39% Whelan TJ et al, NEJM 2015; 373: 307 -316
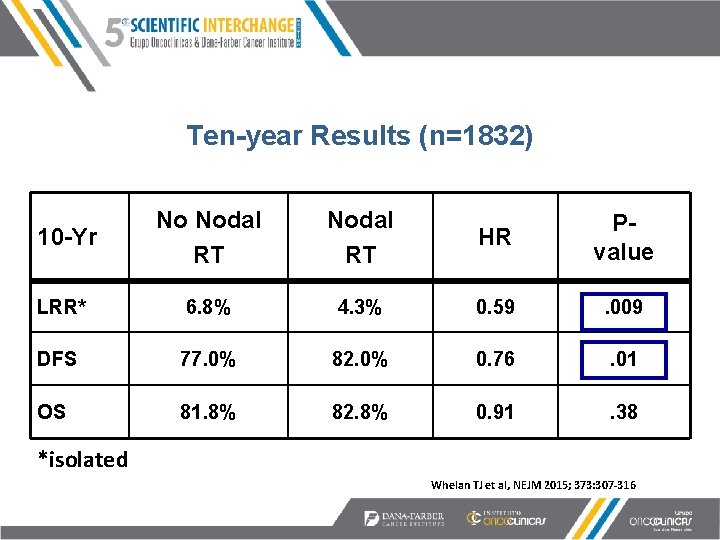
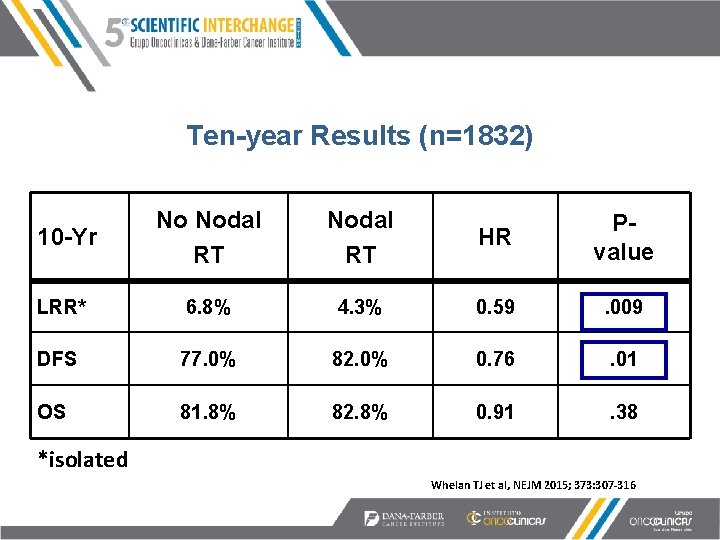
Ten-year Results (n=1832) 10 -Yr No Nodal RT HR Pvalue LRR* 6. 8% 4. 3% 0. 59 . 009 DFS 77. 0% 82. 0% 0. 76 . 01 OS 81. 8% 82. 8% 0. 91 . 38 *isolated Whelan TJ et al, NEJM 2015; 373: 307 -316
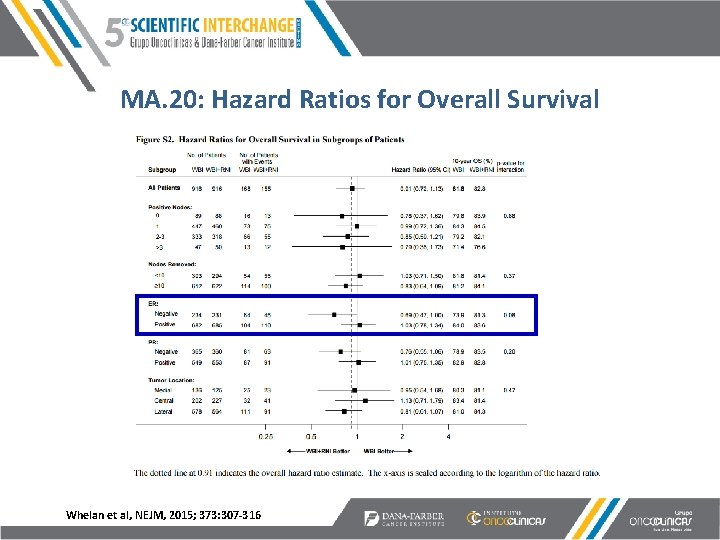
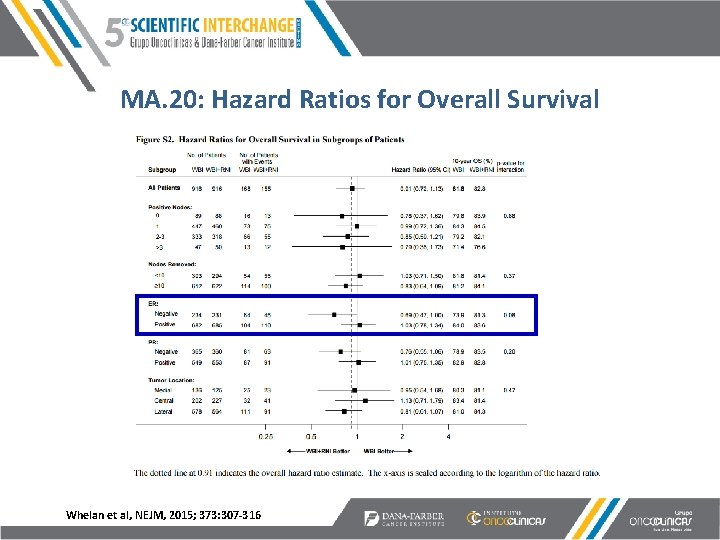
MA. 20: Hazard Ratios for Overall Survival Whelan et al, NEJM, 2015; 373: 307 -316
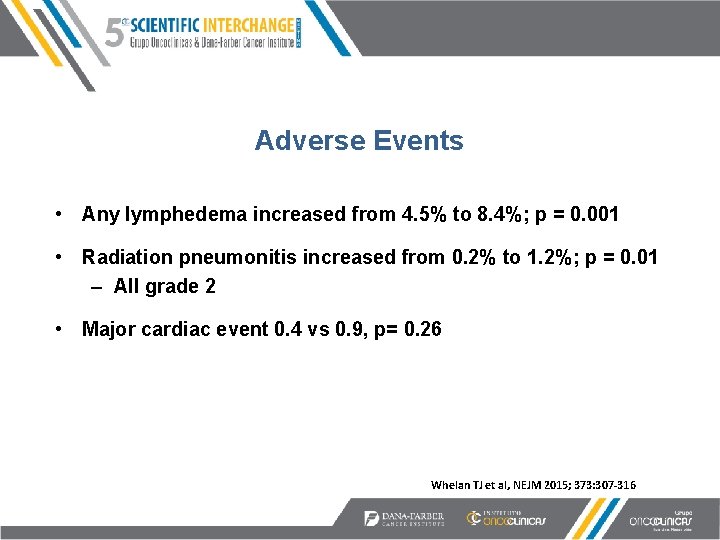
Adverse Events • Any lymphedema increased from 4. 5% to 8. 4%; p = 0. 001 • Radiation pneumonitis increased from 0. 2% to 1. 2%; p = 0. 01 – All grade 2 • Major cardiac event 0. 4 vs 0. 9, p= 0. 26 Whelan TJ et al, NEJM 2015; 373: 307 -316 *NCI – Common toxicity criteria v 2 1998
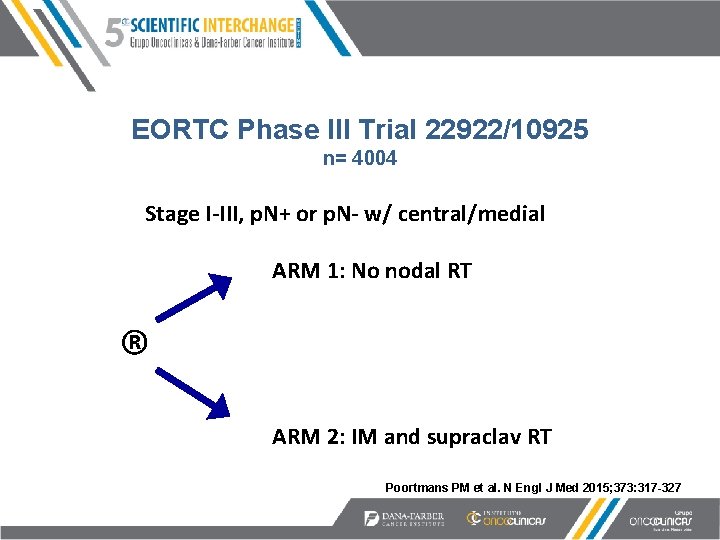
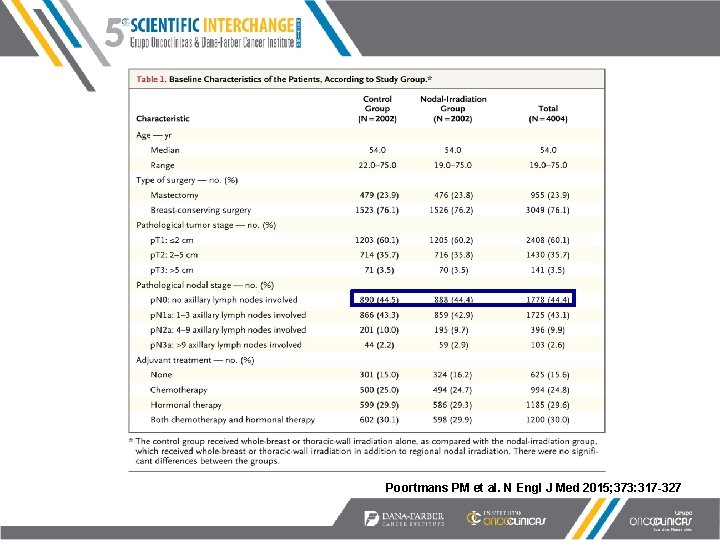
EORTC Phase III Trial 22922/10925 n= 4004 Stage I-III, p. N+ or p. N- w/ central/medial ARM 1: No nodal RT ® ARM 2: IM and supraclav RT Poortmans PM et al. N Engl J Med 2015; 373: 317 -327
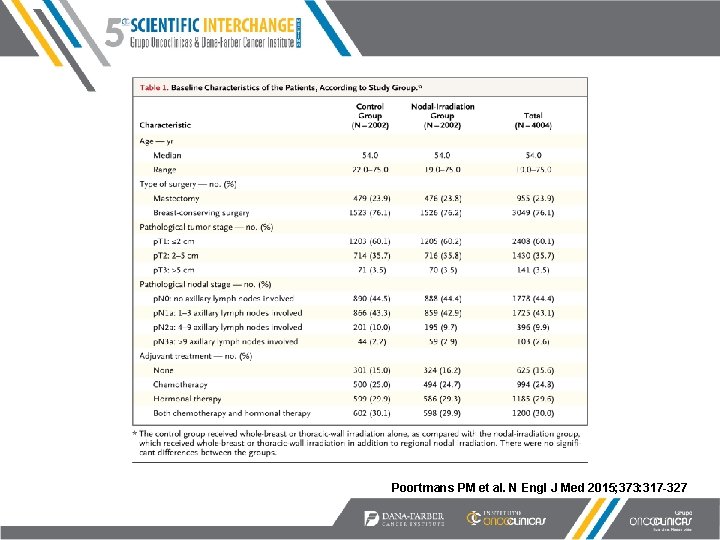
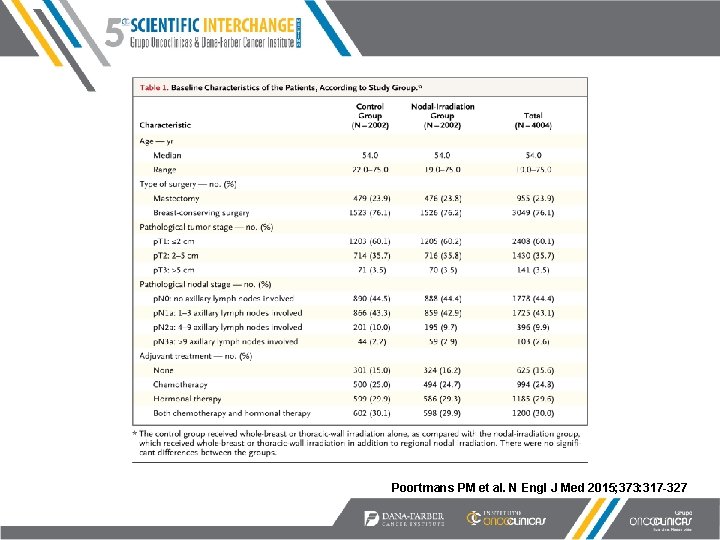
Poortmans PM et al. N Engl J Med 2015; 373: 317 -327
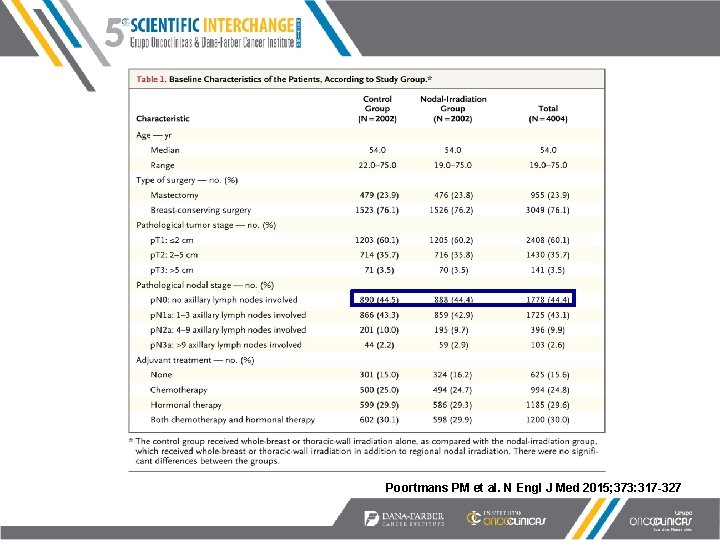
Poortmans PM et al. N Engl J Med 2015; 373: 317 -327

Distant Disease-free and Overall Survival P=0. 02 Median followup: 10. 9 years P=0. 06 Poortmans PM et al. N Engl J Med 2015; 373: 317 -327

Multicenter French Randomized Trial • Randomization: CW, SCV +/- IM • N=1407 • Eligibility: – Mastectomy, larger than 1. 0 cm – Any node positive – Medial/central with or without positive nodes • Technique: First 5 intercostal spaces included, 2/3 rds of the dose with electrons Hennequin et al IJROBP 86(5), 2013
Hennequin: Methods • Powered for a 10% difference in the primary endpoint (OS) • Stratification factors: – Tumor location (medial/central vs lateral) – Axillary lymph node status (p. N 0 vs p. N+) – Adjuvant systemic therapy (chemotherapy vs no chemotherapy) Hennequin et al IJROBP 86(5), 2013

Hennequin: 10 Year Results Outcome No IM RT (%) p OS 59. 3 62. 6 0. 8 DFS 53. 2 49. 9 0. 35 LR as first event 9. 8 9. 2 NS Cardiac Events 2. 2 1. 7 NS Hennequin et al IJROBP 86(5), 2013
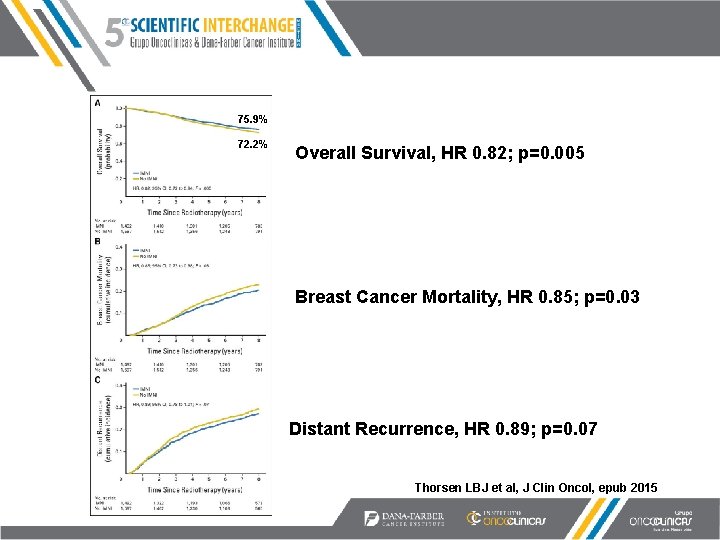
The Danish Experience • Prospective cohort study, 2003 -2007 • Node positive (macroscopic), younger than age 70 • All received periclavicular and chest or breast RT • LT-sided: RT without IMN (n=1586) • RT-sided: RT with IMN (n=1486) Thorsen LBJ et al, J Clin Oncol, epub 2015
Key Patient/Treatment Characteristics (median follow-up 8. 9 years) • Median age 56 • Mastectomy 65%; BCT 35% • ER Positive 80% • Positive axillary nodes: – 1 -3 59% – 4 -9 26% – >10 15% • High grade 28% Thorsen LBJ et al, J Clin Oncol, epub 2015
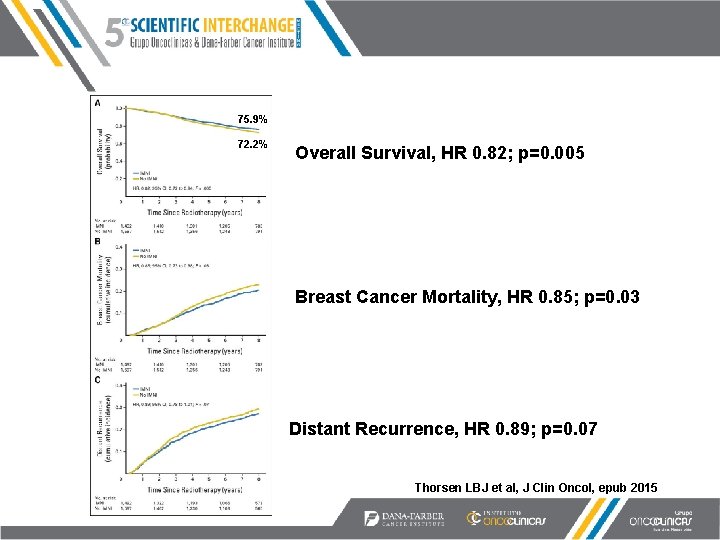
75. 9% 72. 2% Overall Survival, HR 0. 82; p=0. 005 Breast Cancer Mortality, HR 0. 85; p=0. 03 Distant Recurrence, HR 0. 89; p=0. 07 Thorsen LBJ et al, J Clin Oncol, epub 2015

Overall Survival by IMN RT Thorsen LBJ et al, J Clin Oncol, epub 2015

More Questions (few answers) • What is the relative benefit of IM vs supraclav RT – Does it make sense to treat supraclav alone in patients with “difficult” anatomy? – IM alone in patients with medial tumors and negative axillary nodes? • Which subgroups are most likely to benefit – Biologic subtypes? – Limited nodal involvement? • What is the long-term risk of increased lung V 20 and low-dose cardiac RT?
Summary • Nodal RT reasonable alternative to ALND in patients with limited SN involvement • Benefit to regional nodal irradiation (comprehensive? ) • Optimal extent of nodal RT fields remains unclear (inclusion of IMNs at what toxicity cost? ) • Implications for selection of patients for PMRT • Evolving role of RT with improved systemic therapy

 Serat wulangreh kedadeyan saka...pupuh
Serat wulangreh kedadeyan saka...pupuh Julia wong md
Julia wong md Rómeó jellemzése
Rómeó jellemzése Cancer treatment
Cancer treatment Intensity modulated radiation therapy
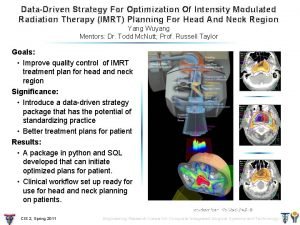
Intensity modulated radiation therapy Gvsu radiation therapy
Gvsu radiation therapy Nhti radiation therapy
Nhti radiation therapy Bioness bits cost
Bioness bits cost Humanistic therapies aim to boost
Humanistic therapies aim to boost Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Wifs tablet colour
Wifs tablet colour Interferencia constructiva
Interferencia constructiva Mesh analysis by inspection
Mesh analysis by inspection Nodal point
Nodal point Mesh analysis
Mesh analysis Nodal and loop analysis
Nodal and loop analysis Nodal analysis
Nodal analysis Nodal analysis
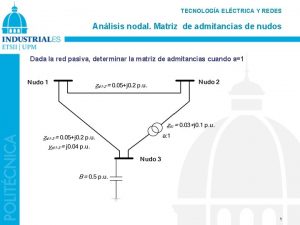
Nodal analysis Sistema por unidad
Sistema por unidad Cardiomyocyte action potential
Cardiomyocyte action potential Nodal analysis
Nodal analysis V(t) = vm sen wt
V(t) = vm sen wt Nodal analysis steps
Nodal analysis steps Strie scalariforme
Strie scalariforme Contoh wilayah nodal
Contoh wilayah nodal Retardo nodal
Retardo nodal Arritmia sinusal con cvp
Arritmia sinusal con cvp Nodal plane and radial node
Nodal plane and radial node Tissu nodal localisation
Tissu nodal localisation Nodal analysis
Nodal analysis Matriz nodal
Matriz nodal Michele casula
Michele casula Find v
Find v Cur 1
Cur 1 Nodal cells
Nodal cells Wilayah indonesia
Wilayah indonesia Advantages of nodal analysis
Advantages of nodal analysis Source transformation circuit analysis
Source transformation circuit analysis Helena wong cityu
Helena wong cityu Input layer
Input layer Dr. terry wong
Dr. terry wong When was new zealand discovered
When was new zealand discovered Robot metaphors
Robot metaphors Daño nervio optico
Daño nervio optico Pawarta iku sipate yoiku
Pawarta iku sipate yoiku Speak up janet wong
Speak up janet wong