Principles of Pediatric Dermatological Diagnosis and Therapy References



- Slides: 59

Principles of Pediatric Dermatological Diagnosis and Therapy 高雄長庚紀念醫院暨兒童醫院 皮膚科 黃柏翰醫師
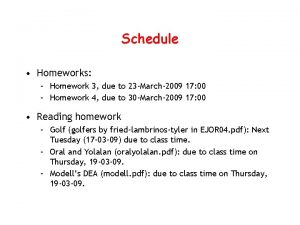
References n n n Principles of Diagnosis in Pediatric Dermatology, Moise L Levy, 1996 Principles of Treatment in Pediatric Dermatology, Elaine Siegfried, 1996 Principles of Pediatric Dermatological Therapy, Dennis P. West and Giuseppe Micali, 2001
Principles of Diagnosis n n An initial careful history: A description of the condition under evaluation in the patient’s or parent’s words Observation of individual lesions: u morphology of skin lesions, color, and distribution Diagnostic aids: u microscopy, lab. Newer methods: u dermatoscopy, PCR
History: newborn or infancy (birth to 1 year) n n Prenatal history reviewed on neonate’s chart and obstetric sheet and obtained from parents u Maternal condition u Delivery difficulty u Infection: herpes simplex, syphilis u Family history Must establish a positive relationship with all concerned individuals
History: toddlers and preschool-aged children (1 to 4 years) n n n Prenatal history and development during the first year obtained from parents and caretakers. Physicians: be seated and attempt eye contact with children at their level. Non-threatening body language: No loud voice, threatening looks, or touching before with a level of confidence with the physician. Allow to play with toys. Some aged 2 or 3 may be able to participate in the historic review.
History: school-age child (5 to 10 years) n n n Children will be able to participate directly in the review. Talk to any patient using language understandable to the child. No laughing or trying to be humorous only when you are well known to the child. Parents or caretakers will also be relied on heavily.

History: highlights n n n Physician’s relationship with each parent Parents have anxiety and guilt about possible contributions to the child’s problem. Open-ended question are non-threatening and leave options that may help clarify the chief complaint.
Physical Examination n Never separate the kid from the parents and allow to stay close to the parents or even in their lap. Do not jump out of the chair or move about in a quick manner. Allow to play with toys
Communication n “Find it and fix it” is not enough in medicine? Essential skills in empathic communication Currently, (1) physicians have the empathy but lack the skills to convey; (2) the techniques of empathic communication are simple and learnable.
Tip 1 n How to begin the discussion with a new patient? u It sounds like you’ve been through a lot. t Try to shut up and express respect and concern t Give the family a chance to tell the part of their story that is most important to them u In Taiwan, we often end with “just listen to me!”
Tip 2 n Repeating to the patient the story that we’ve just heard u Let me see if i have this right t Also a way of showing that we have been listening and paying attention u In Taiwan, the history taking is always not enough.
Tip 3 n Handling emotions u You seem frustrated. Most people in your situation would find this very frustrating u I can tell you are worried. I can easily understand that you would be worried. t Comments of this sore allow us to move into a different and more empathic conversation with our patients and their families. u In Taiwan, handling emotions is not always a issue.
Tip 4 n Praise opportunity u You’re doing a great job. u I know that doing these treatments at home has been a lot of work. t Express legitimate and deserved respect for the work they are doing to cope with difficult health problems. u In Taiwan, patients or families to do best is obligated and not deserved respect.
Tip 5 n When things haven’t gone well or when we are faced with a problem that is difficult or impossible to treat effectively. u “I am sorry that…” can easily be confused and be misconstrued as an apology. u I wish things were different. u I wish there were better treatments available. t Express empathy and lets the patient know that you share their disappointment and concern. u In Taiwan, the patients always felt disappointed to the medical system or doctors.
Tip 6 n How to advise to the very touchy issues, e. g. lifestyle or parenting u Would it be ok if i give you some advise about this? u Would it be ok if i share some things i’ve learned from other patients/families who have dealt with this problem? u In Taiwan, physicians seems like a know-it-all.
Tip 7 n How to conclude in a way that is graceful and never perceived as abrupt or uncaring u Is there anything else you would like to tell me t To make sure the patient’s concerns have been addressed. t Allow to participate in the decision to conclude the visit. u In Taiwan, visits are always ended abruptly.
Principles of Medical Treatment n n Monitoring for the growth parameter: u Children treated with prolonged course of steroids, cytotoxic or immunomodulating drugs. Screening for the developmental delay: u Early language development and problemsolving skills. u Metabolic abnormality, dysmorphic features, phakomatosis, or genodermatois.
Therapeutics Appropriate for Age and Family n n The form and taste of a medication u Dicloxacillin: bitter and poorly tolerated t Better choice: Erythromycin, Baktar, Keflex u Smaller volume per dose To allow adolescents to choose medication will improve the compliance Do not blame the patient or parents immediately though poor compliance. Design the most acceptable regimens
Therapeutics Appropriate for Age and Family n n n If no uniform safe and effective therapy, start with inexpensive, safe, and painless ones. If benign and self-limited, nontherapeutic approach is appropriate. The parents’ concern might be different from the patient’s symptoms and signs.
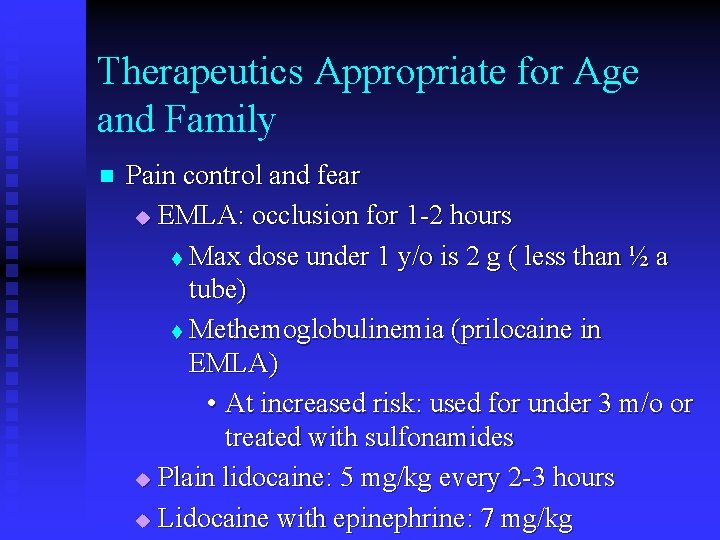
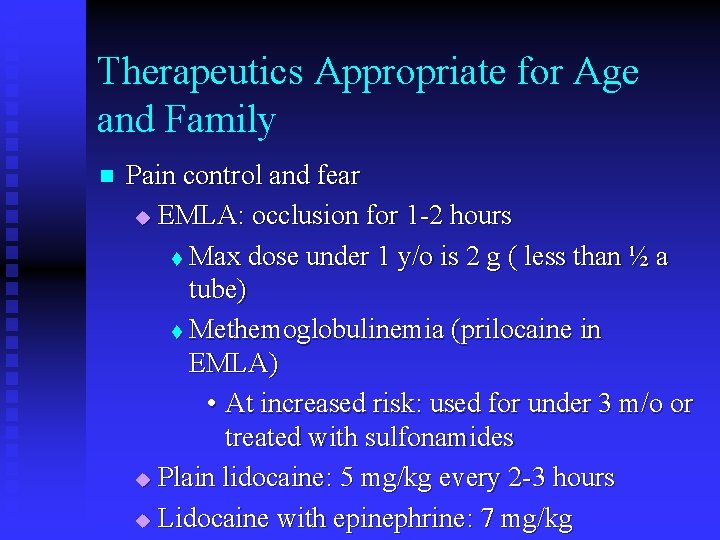
Therapeutics Appropriate for Age and Family n Pain control and fear u EMLA: occlusion for 1 -2 hours t Max dose under 1 y/o is 2 g ( less than ½ a tube) t Methemoglobulinemia (prilocaine in EMLA) • At increased risk: used for under 3 m/o or treated with sulfonamides u Plain lidocaine: 5 mg/kg every 2 -3 hours u Lidocaine with epinephrine: 7 mg/kg
NEONATAL SKIN CARE AND SELECTED NEONATAL SKIN DISORDERS
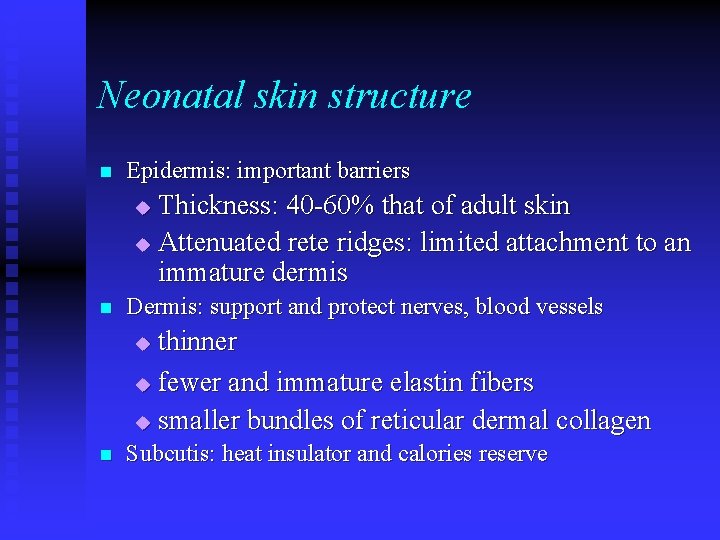
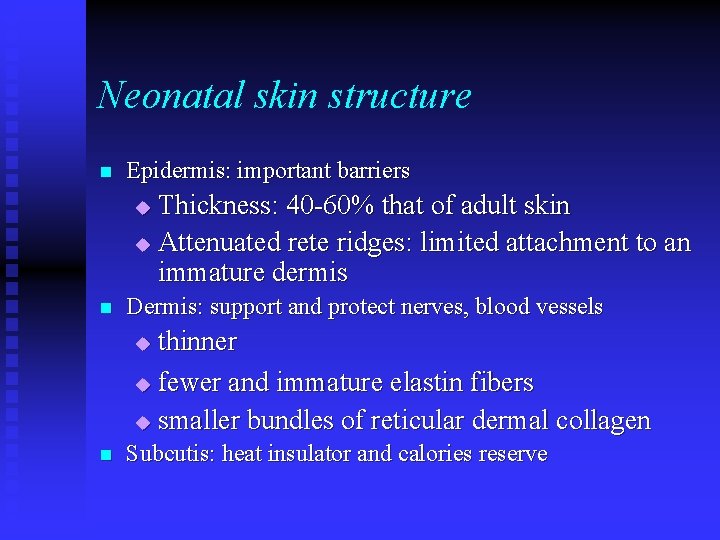
Neonatal skin structure n Epidermis: important barriers Thickness: 40 -60% that of adult skin u Attenuated rete ridges: limited attachment to an immature dermis u n Dermis: support and protect nerves, blood vessels thinner u fewer and immature elastin fibers u smaller bundles of reticular dermal collagen u n Subcutis: heat insulator and calories reserve
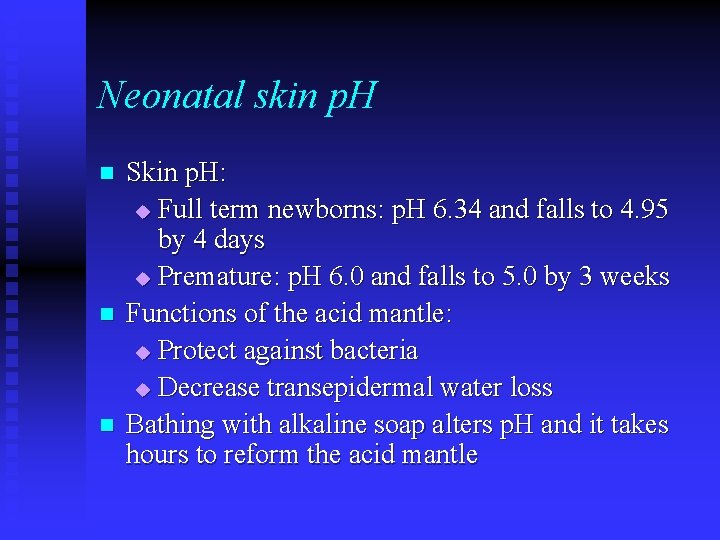
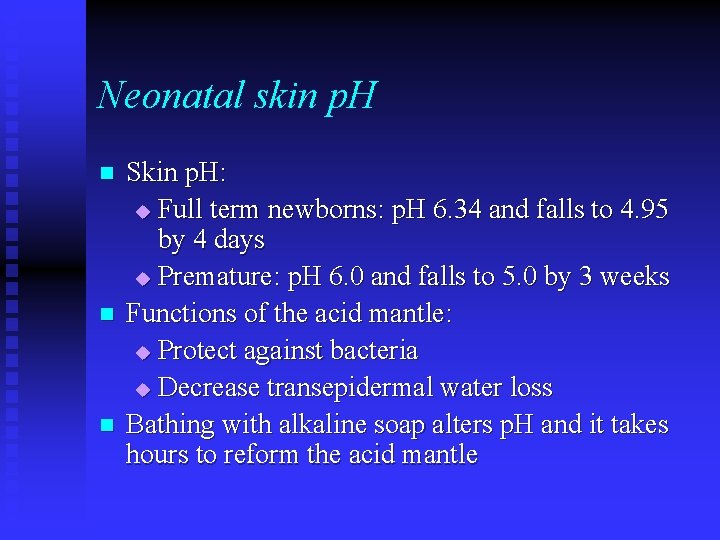
Neonatal skin p. H n n n Skin p. H: u Full term newborns: p. H 6. 34 and falls to 4. 95 by 4 days u Premature: p. H 6. 0 and falls to 5. 0 by 3 weeks Functions of the acid mantle: u Protect against bacteria u Decrease transepidermal water loss Bathing with alkaline soap alters p. H and it takes hours to reform the acid mantle
Transepidermal water loss (TEWL) n n n Premature: 15 times higher in 1 day old infants born at 25 weeks gestation Very low birth weight infants: 30% of total body weight in 24 hours Traditional resolution: fluid replacement has a lag time and may result in sodium and glucose overload
Skin injury n Clinically occult skin injury accompanies routine care. u Skin stripping u Local application of pressure or thermal heat. u UV light burns due to white light (UVA and infrared heat included) phototherapy for jaundice.

Skin care practices n n n n Bathing Diapering Emollients Skin Antisepsis Adhesive Application and Removal Care of Cord Care of Broken Skin Control of Transepidermal Water Loss
Murphy’s Law: Whatever can go wrong, will.
Bathing n n No antimicrobial cleansing agents for routine bathing with clearly demonstrable benefits for infants: reduced colonization for 4 hours only. Mild cleansing products work or hurt? Little difference among them. Burns after immersion in hot water tested only by touch. Cloth diaper: avoid laundered with phenolic compounds (pentachlorophenol)
Bathing n n Bathing only after the temperature has established, often from 2 -4 hours later. Leave the vernix on as long as possible. u u n n providing added skin barrier protection: hydrophobic and bactericidal regulating postnatal surface adhesion properties, heat flux, and surface electrical property Robbing is avoided. Baths should be on alternate day.
Diapering n n n The first disposable diapers, Pampers, were marketed in 1963. Its absorbent core is cellulose fluff. In the mid-1980’s, the superabsorbent core, a cross-linked sodium polyacrylate, in all disposable diapers. Urine output monitoring by weighing diapers: u Greater evaporative loss from a regular fluff-type u Pseudoanuria: inability to feel moisture on a superabsorbent diaper
Emollients and diaper rash products n n Potential percutaneous toxicities, especially the diaper area due to occlusion. u Commercially available ingredients used with caution in the newborn: Triclosan, Propylene glycol, Benzethonium chloride, Glycerin, Ammonium lactate, and Coal tar. Contact sensitization: thimerosal, nickel, Kathon CG, fragrances, neomycin, and wool alcohol. The safest and best effective emollient: white petrolatum The best initial choice for diaper dermatitis is zinc oxide ointment
Adhesive application and removal n n n Hydrogel (vigilon) or hydrocolloid ( Deo. Derm Extra Thin) is favored to replace conventional adhesive products, especially for patients with epidermolysis bullosa (EB). Cotton bandages work well, too. Prevention of skin trauma from adhesive removal: smaller pieces of adhesive, backing the adhesive with cotton gauze, delaying removal, and reducing frequency. Warm water is safest to facilitate removal, but not oil.
Care of broken skin n Etiology: adhesive removal, infection, friction, pressure sores, wiping skin when diarrhea and diaper dermatitis, etc. n Care: u frequent irrigation with sterile water and covered with opsite, hydrogel, or hydrocolloid u keeping a moist surface speeds healing u Antifungal and antibacterial ointment preferred because of improved coating and healing by facilitating migration of epithelial cells
Control of transepidermal water loss I n White petroleum is regarded as the gold standard. Oils, creams, and lotions provides a much less effective moisture barrier. u Formulation requires the addition of several potentially irritating, sensitizing or toxic ingredients. u Aquaphor: TEWL after 30 minutes is 67% decrease but only 34% decrease after 6 hours. 6 hour application interval is needed. u
Control of transepidermal water loss II n Stable skin surface temperature, and no evidence of hyperthermia or burn following application of petrolatum-based ointment under infrared warmer.
Proposed Recommendations for Basic Skin Care of the Premature Newborn n n n Use adhesive sparingly Limit bathing be aware of the composition and quantity of all topically applied agents Ensure adequate intake of protein, essential fatty acid, zinc, biotin, and vitamins A, D, and B’s Apply an ointment emollient every 6 -8 hours Guard against excessive thermal and UV exposure Protect sites of cutaneous injury with the appropriate occlusive dressing
Diaper rashes update in pathomechanism I n n Occlusion and moisture: edema of stratum corneum Friction: wet skin more susceptible Urine and ammonia: ammonia DOES NOT produce primary irritation, but can be a secondary irritant when skin is injured Feces: protease and lipase; breastfeeding babies have lower fecal p. H, lower protease and lipase activities, fewer urea-splitting bacteria (less urease)
Diaper rashes update in pathomechanism II n n n Candida albicans: keratolytic activity, activating complement Bacteria: colonization by S. aureus Other risk factors: washed with detergent soaps
Diaper rashes update in therapy I n n n Reduce moisture and friction: frequent diaper changes (at least every 2 hours), superabsorbant diapers, no tight fitting diapers, and occlusive pants, disposable diaper with cloth-like covering Protect diaper area: barrier ointment with diaper change Minimize washing of diaper area: for urine, blot dry, DO NOT need wipes; for stool, avoid water, consider soap-free cleanser
Diaper rashes update in therapy II n n n Decrease skin inflammation: HC 1% ointment, No halogenated steroids, including Betamethasone and Triamcinolone. Treat candida: satellite lesions, or if rash present for more than 3 days Antibacterial therapy: use if crusting; topical; systemic
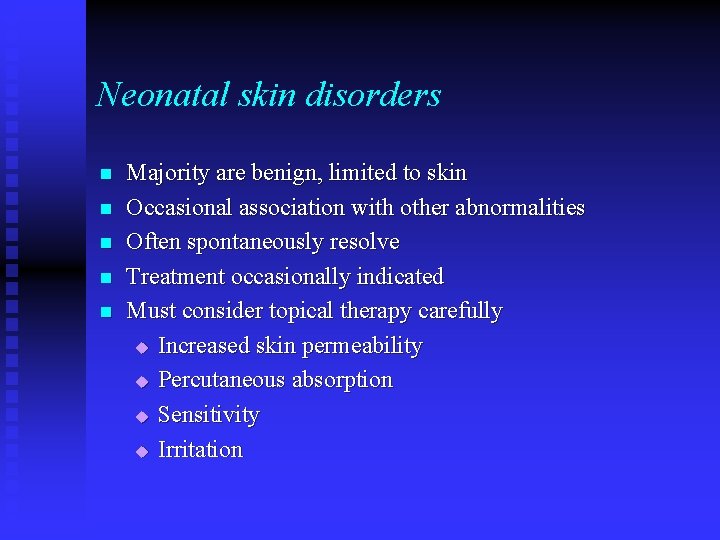
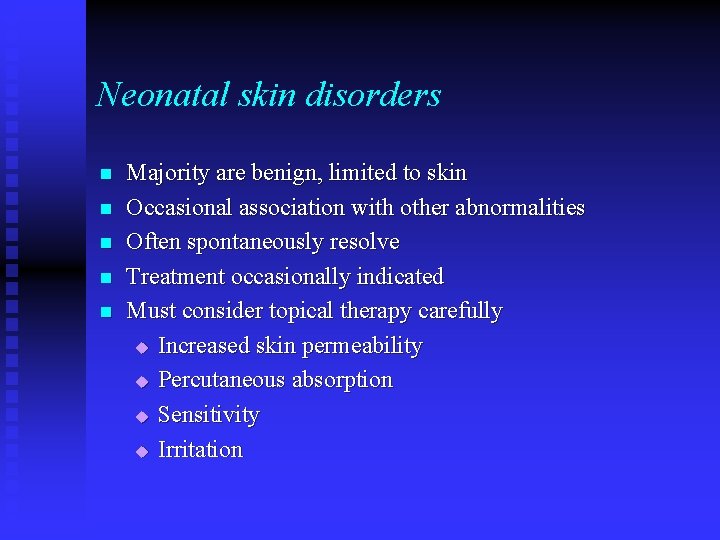
Neonatal skin disorders n n n Majority are benign, limited to skin Occasional association with other abnormalities Often spontaneously resolve Treatment occasionally indicated Must consider topical therapy carefully u Increased skin permeability u Percutaneous absorption u Sensitivity u Irritation
Ultimately, clinicians learned that they were not limited by glucocorticoid efficacy, but rather by the side effects.
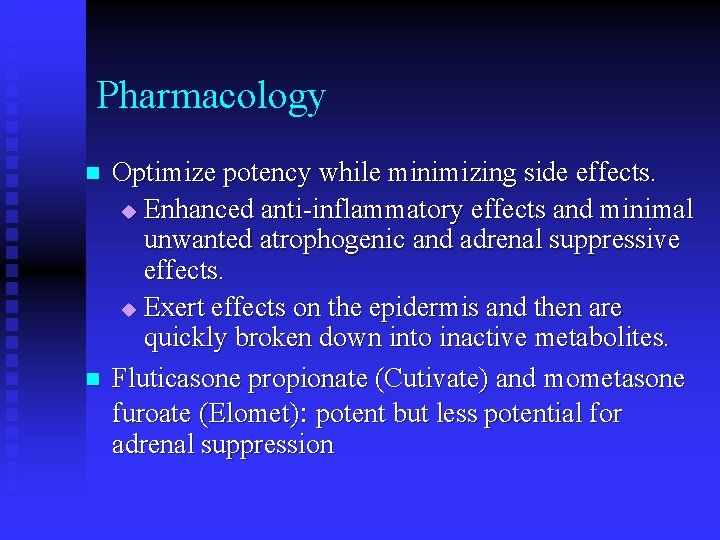
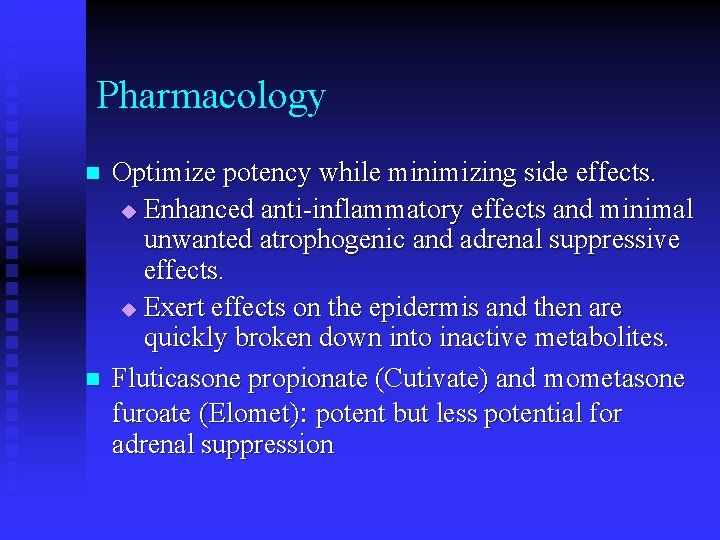
Pharmacology n n Optimize potency while minimizing side effects. u Enhanced anti-inflammatory effects and minimal unwanted atrophogenic and adrenal suppressive effects. u Exert effects on the epidermis and then are quickly broken down into inactive metabolites. Fluticasone propionate (Cutivate) and mometasone furoate (Elomet): potent but less potential for adrenal suppression
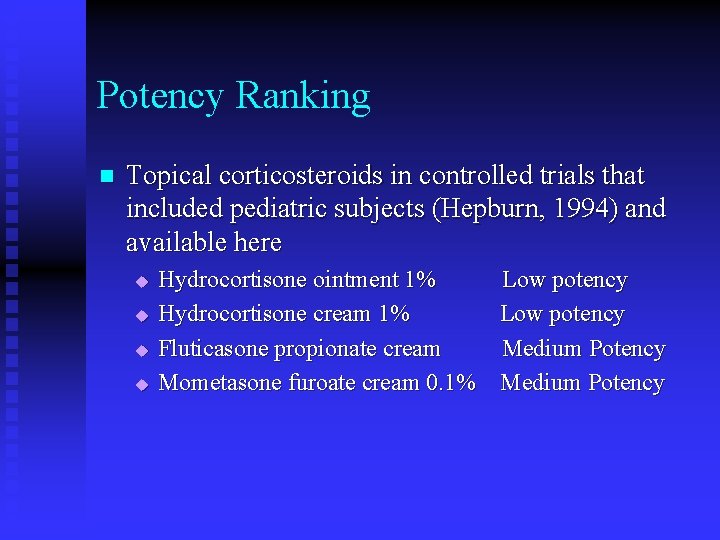
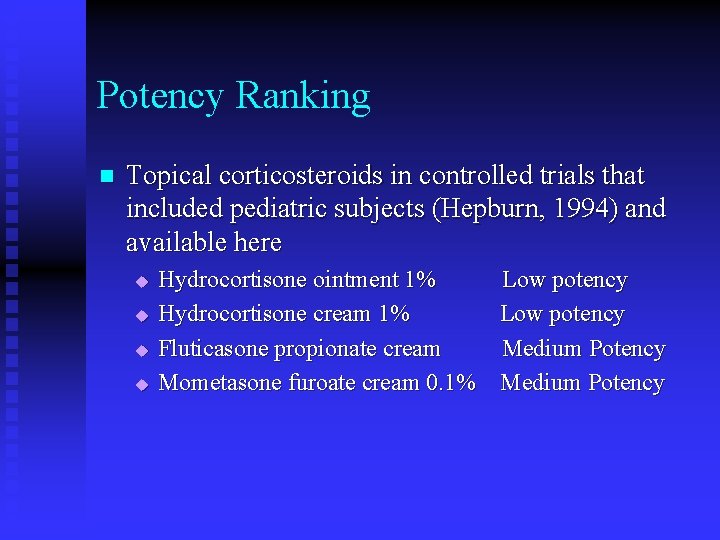
Potency Ranking n Topical corticosteroids in controlled trials that included pediatric subjects (Hepburn, 1994) and available here u u Hydrocortisone ointment 1% Low potency Hydrocortisone cream 1% Low potency Fluticasone propionate cream Medium Potency Mometasone furoate cream 0. 1% Medium Potency
Local side-effects n n n More common but not life threatening Insidious in onset and troublesome Steroid phobia due to overuse of topical steroids for atopic dermatitis in Japan (Yamamoto, 1989). Same in Taiwan.
Local side-effects n n n Atrophy, striae, purpura and telaniectasia u Medium potency on the face and in the intertriginous areas: 4 weeks u Potent or superpotent agent without occlusion for other sites: 2 weeks; if under occlusion: 7 days. Rosacea, and granuloma gluteale infantum Tinea, scabies, and impetigo will initially improve. Flare of acne Hirsutism and hypertrichosis Hypopigmentation
Tinea incognito, masking of fungal infection Reduced redness and eliminated scales. Tinea continues to spread!
Systemic side-effects n n Due to a greater surface to body ratio and less able to metabolize potent steroids quickly, infants and toddlers are at high risk. Greater than 1/3 of applied dose is systemically absorbed in infants with active atopic dermatitis.
Systemic side-effects n n HPA axis suppression (adrenocortical function is decreased in the 2 nd post-tx day in 75% of infants using fluorinated steroids), failure to thrive, overt Cushing’s syndrome, glaucoma (more than 10 day -use), and benign cephalic hypertension. Be ware of amount, extent, frequency, length, potency and occlusion or not.
How to Use Smartly and Safely
Diagnosis is the Key to Success.
Regional Differences in Activity n n n Choose the potency and dosage form according to the anatomic area being treated Napkin area, all intertriginous areas u Thin, moist, occluded u Low-potency is recommended Trunk and extremities u Moderate potency with greater safety
Choice of Vehicles n n Ointments are favored in atopic patients with dryness though cosmetically not acceptable. Creams are far less greasy and much easier to spread. Emollient creams have more petrolatum like derivatives. It’s sometimes more irritating. Lotions have water, alcohol, and various exotic agents. Gels, which have alcohol and acetone, cause the most problems.
Brief Periods n n In infants and children, twice or once a day and duration of 7 -14 days is usually sufficient. Steroid holiday: After 7 -14 days of treatment, stop topical steroids and substitutes emollients for a few weeks.
Minimizing Occlusion n Occlusion enhances skin absorption u Supersaturated in upper layers of stratum corneum Diffuses slowly inward and provide a steady flux to the dermis u Detectable for many days or even a few weeks Skin atrophy can be produced within 7 days by superpotent topical steroids under occlusion
Do Not Forget Emollients!
Practical Use for Kids in CGMH n n Hydrocortisone ointment 1% (Cort-S) Low potency u Diaper dermatitis and intertriginous dermatitis u Ateatotic dermatitis, esp. in winter u Extensive use is safe but too greasy. Hydrocortisone cream 1% (Tropoderm) Low potency u Be ware of possible allergy to neomycin and other unnecessary ingredients u Use in winter is not preferable (Not a good emollient)
Practical Use for Kids in CGMH n Fluticasone propionate cream (Cutivate) Medium Potency u Good and suitable for most eczematous dermatitis in kids. u Should avoid putting on diaper areas.
Practical Use for Kids in CGMH n Mometasone furoate cream 0. 1% (Elomet) Medium Potency u Never use for intertriginous areas u No long term use u More effective than Cutivate but also more irritating u The most potent topical steroids before referral to pediatric dermatologists
 Nursing diagnosis
Nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnoses
Types of nursing diagnoses Pediatric physical therapy outcome measures
Pediatric physical therapy outcome measures Pathways pediatric therapy
Pathways pediatric therapy Pediatric occupational therapy frames of reference
Pediatric occupational therapy frames of reference Simplesetpro
Simplesetpro Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system price
Bioness integrated therapy system price Humanistic therapy aims to
Humanistic therapy aims to Automotive technology principles diagnosis and service
Automotive technology principles diagnosis and service Five core principles of money and banking
Five core principles of money and banking Difference between bibliography and references
Difference between bibliography and references Difference between bibliography and references
Difference between bibliography and references Contextual criticism art
Contextual criticism art 8 figure grid reference example
8 figure grid reference example (acv-s03) homework - addresses and references
(acv-s03) homework - addresses and references Java pointers and references
Java pointers and references Types of references and examples
Types of references and examples Java pointers and references
Java pointers and references Wubbolding
Wubbolding Double rope in suspension therapy
Double rope in suspension therapy Neurodevelopmental therapy principles
Neurodevelopmental therapy principles Principles of topical therapy in dermatology
Principles of topical therapy in dermatology Cv reference
Cv reference Contoh term of reference proyek
Contoh term of reference proyek Ucas reference examples for teachers
Ucas reference examples for teachers Risk management reference list
Risk management reference list References apa format
References apa format How to put references on a poster
How to put references on a poster Examples of intertext
Examples of intertext Vague pronoun examples
Vague pronoun examples Waste management references
Waste management references Ibm iseries external storage
Ibm iseries external storage How many references for 1000 words
How many references for 1000 words Grid references
Grid references Contextual reference meaning
Contextual reference meaning Contextual reference
Contextual reference Dejobbing
Dejobbing Performance appraisal reference books
Performance appraisal reference books Reference construction
Reference construction Ic design references
Ic design references Allusion in f451
Allusion in f451 Bibliography vs references
Bibliography vs references Grid references
Grid references Intertextual references in riptide
Intertextual references in riptide Abstract apa format
Abstract apa format Dear red if you're reading this
Dear red if you're reading this Swedbank internetbanka ieiet
Swedbank internetbanka ieiet Chubby references
Chubby references Ventral cavity
Ventral cavity Water conservation references
Water conservation references Understanding grid references
Understanding grid references References of solar energy
References of solar energy Hypothesis example in qualitative research
Hypothesis example in qualitative research Sop references
Sop references Malaria references
Malaria references Criteria for evaluation of reference sources
Criteria for evaluation of reference sources