Pneumonia Pneumonia Definition Acute infectious inflammation of the






- Slides: 41
Pneumonia
Pneumonia • Definition: Acute infectious inflammation of the distal lung paranchyme (Distal to terminal bronchioles) with clinical and radiological signs of consolidation • Pneumonitis: Noninfectious inflammation
Classifications – Community Acquired – Nosocomial (Hospital acquired) – Pneumonia in immuncompromised host • Anatomic – Lober – Bronchopneumonia – Interstitial pneumonia • Etiologic – Bacterial – Viral – Fungal
• The microorganism reaches the lungs by: – Inhalation or aspiration – Hematogenious way – Direct invasion from the neighbouring tissues • The amount of the organism inoculated, the virulance factors and the immunity of the host are important factors
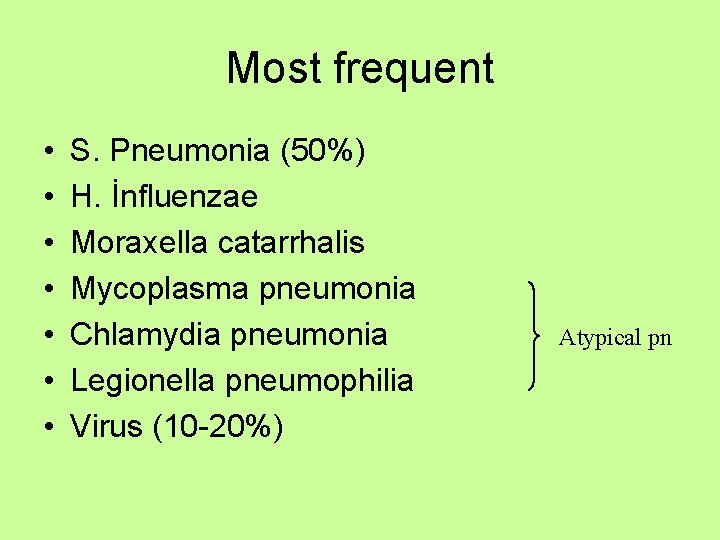
Most frequent • • S. Pneumonia (50%) H. İnfluenzae Moraxella catarrhalis Mycoplasma pneumonia Chlamydia pneumonia Legionella pneumophilia Virus (10 -20%) Atypical pn
Community acquired pneumonia • The symptoms of pneumonia are usually nonspecific but generaly include: – Fever (chills) – Cough – Sputum production (purulent) – Thoracic pain – Dyspnea
• Typical pneumonia is characterised by abrubt onset high fever, chills, productive cough, thoracic pain, focal clinical signs, lobar or segmental radiographic findings, leukocytosis – Strep. Pneumonia • Rusty colored sputum • Labial herpes lesions • Lober infiltration – H. influenzae
Different presentation • Confusion, tachypnea, hypotermia can be the presenting symptom in old age groups • Unusual presentation can be seen in immunocompromised patients
• Atypical pneumonias are characterised by progressive onset, fever without chills, a cough without sputum, headache, myalgia, diffuse crackles, modest leukocytosis, interstitial infiltrates on chest radiographs. – Mycoplasma pneumonia – Legionella (bradicardia, hyponatremia) – Chlamydia
Physical examination • High fever, tachicardia, tachypnea, hypotension, confusion, drowsiness, altered mental status • Respiratory system: • Inspection: – – Usually normal Ortopnea Cyanosis Respiratory disstress • Palpation – İncreased Vibration thoracic (lober pneumonia) – Decreased hemithoracal movement
• Percution – Normal sonority – Dullness (Matite) • Oscultation – End inspiratory fine crackles – Local diminished breath sounds – Bronchial voice
Diagnosis • • • History and symptoms Physical examination PA Chest x-ray Microbiologic examination Routine laboratory tests – CBC, ESR, CRP, Hepatic enzymes, Renal functions • Blood gas
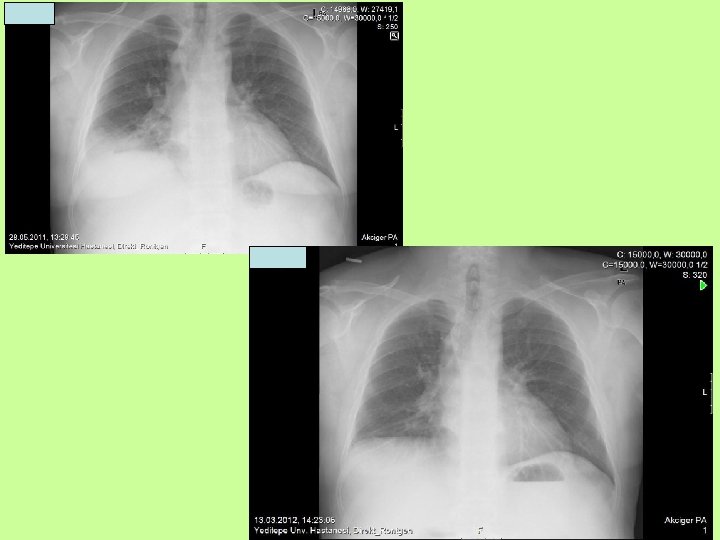
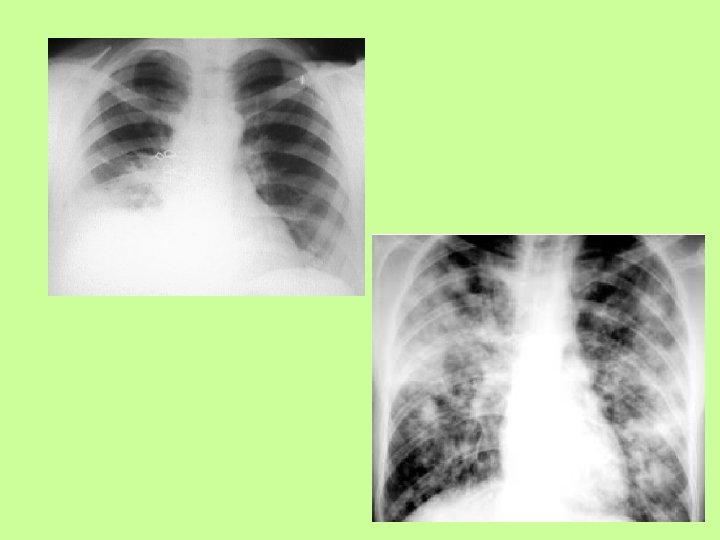
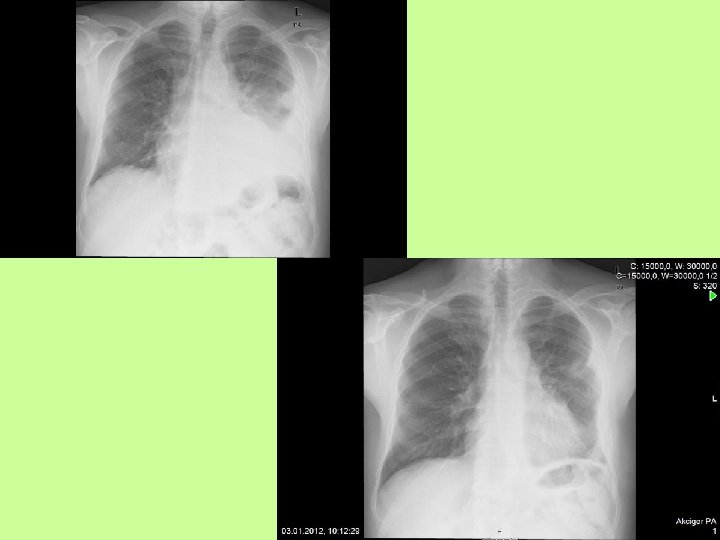
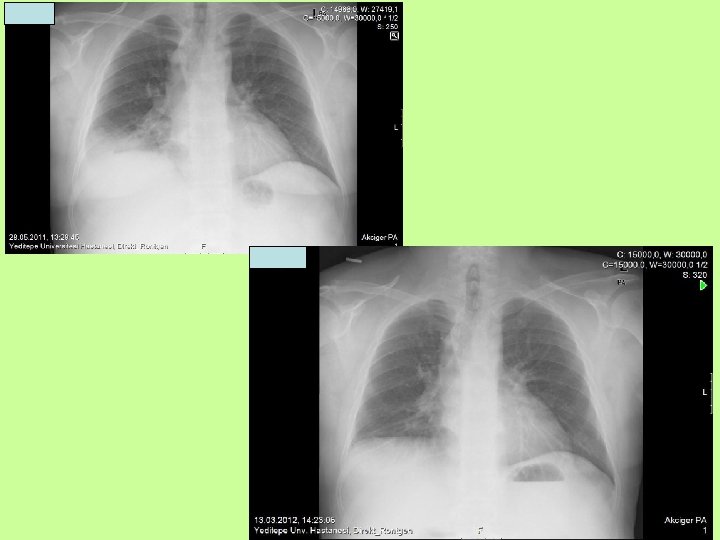
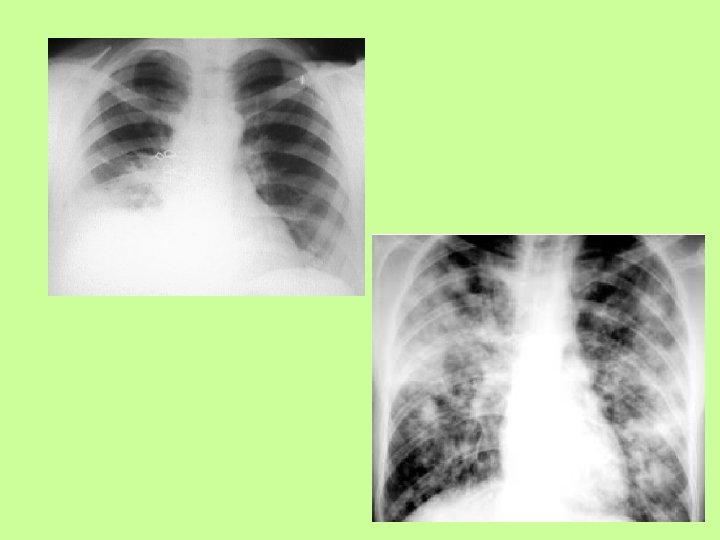
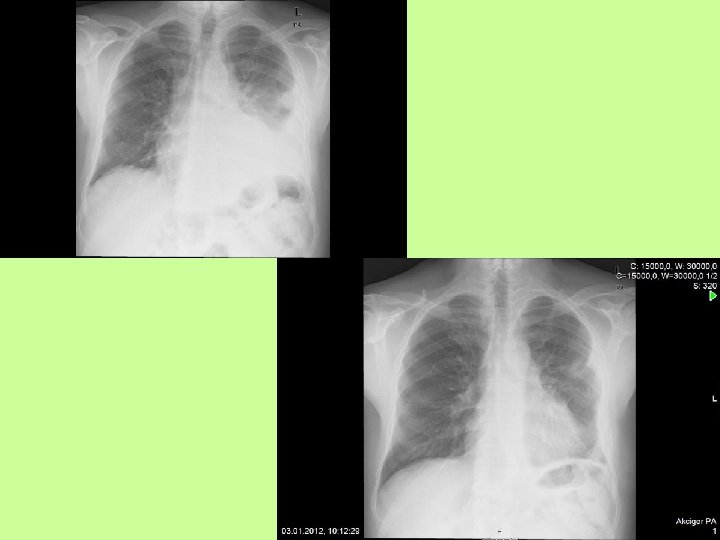
PA Chest x-ray • Consolidation – Lobar or patchy nonhomogenious infiltrations – Air bronchogram – Round opacity – Fine reticular density • Complications – – – Pleural effusion Cavitation Abscess Pneumatocell Pneumothorax





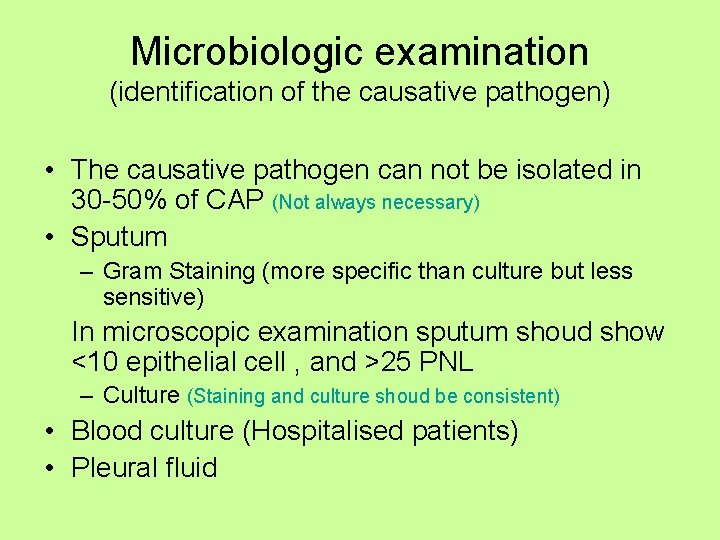
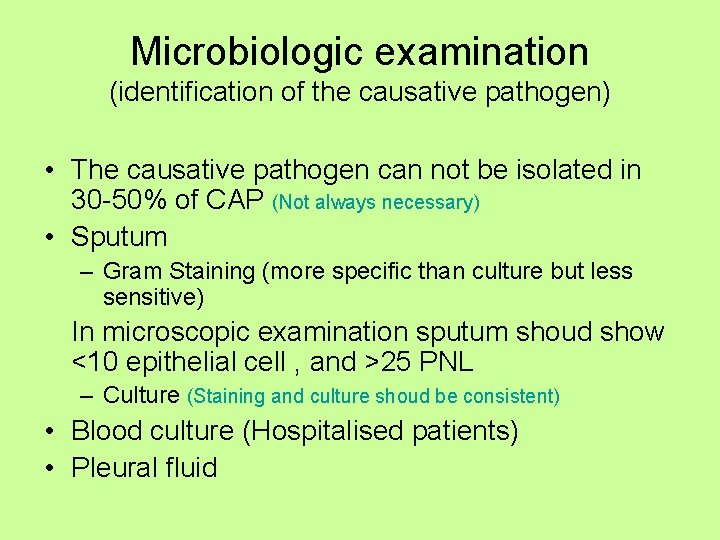
Microbiologic examination (identification of the causative pathogen) • The causative pathogen can not be isolated in 30 -50% of CAP (Not always necessary) • Sputum – Gram Staining (more specific than culture but less sensitive) In microscopic examination sputum shoud show <10 epithelial cell , and >25 PNL – Culture (Staining and culture shoud be consistent) • Blood culture (Hospitalised patients) • Pleural fluid
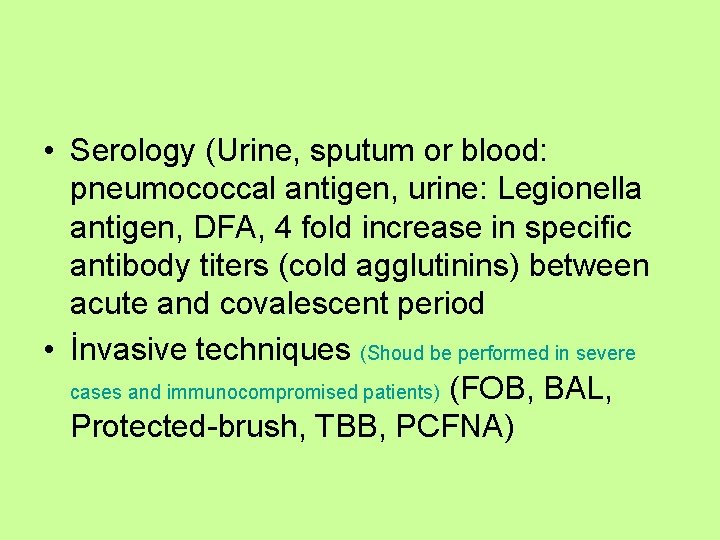
• Serology (Urine, sputum or blood: pneumococcal antigen, urine: Legionella antigen, DFA, 4 fold increase in specific antibody titers (cold agglutinins) between acute and covalescent period • İnvasive techniques (Shoud be performed in severe cases and immunocompromised patients) (FOB, BAL, Protected-brush, TBB, PCFNA)
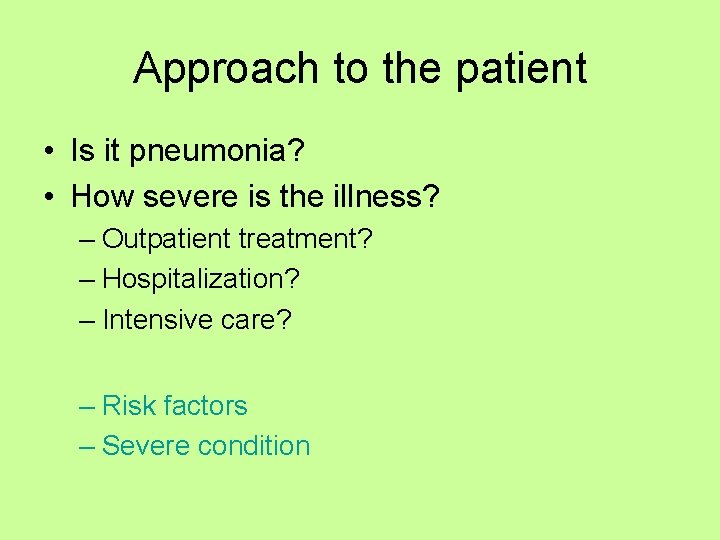
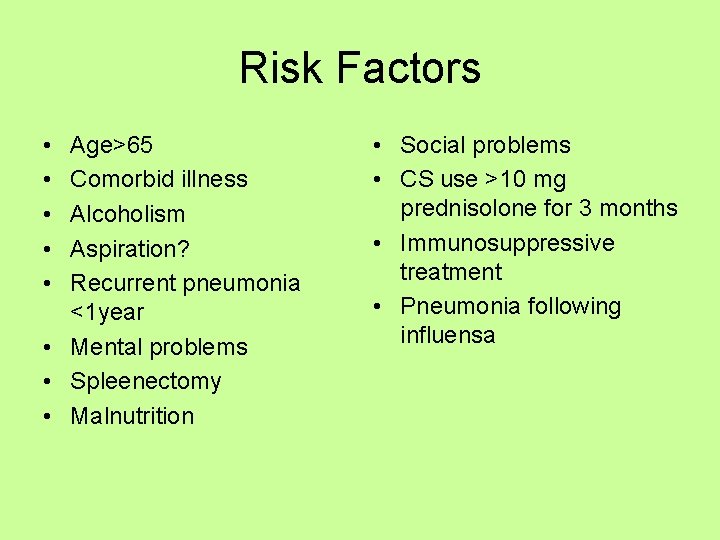
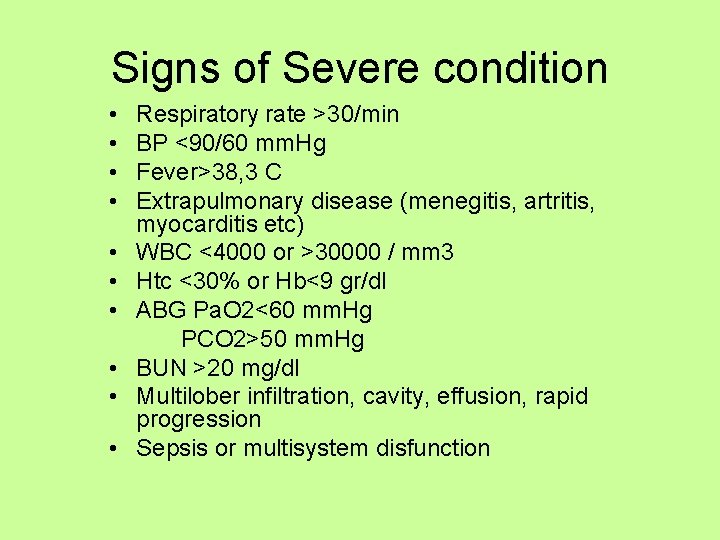
Approach to the patient • Is it pneumonia? • How severe is the illness? – Outpatient treatment? – Hospitalization? – Intensive care? – Risk factors – Severe condition
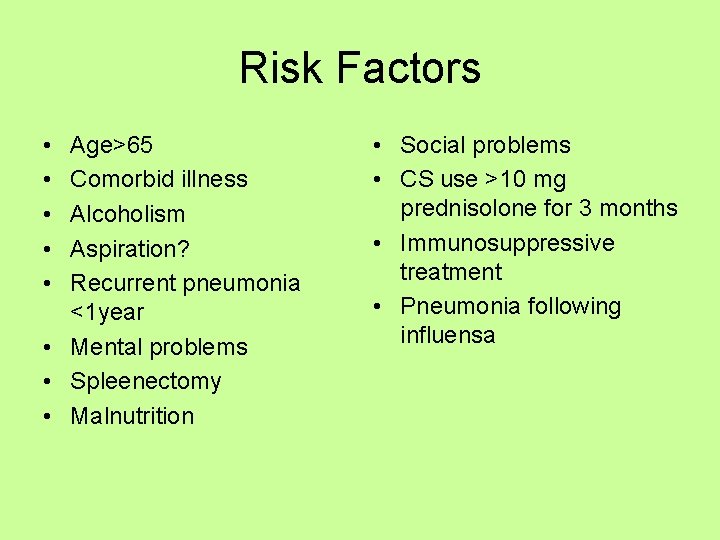
Risk Factors • • • Age>65 Comorbid illness Alcoholism Aspiration? Recurrent pneumonia <1 year • Mental problems • Spleenectomy • Malnutrition • Social problems • CS use >10 mg prednisolone for 3 months • Immunosuppressive treatment • Pneumonia following influensa
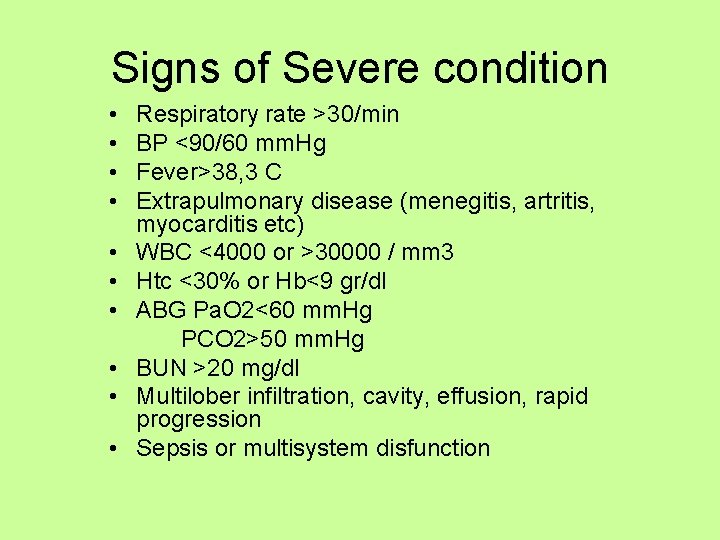
Signs of Severe condition • • • Respiratory rate >30/min BP <90/60 mm. Hg Fever>38, 3 C Extrapulmonary disease (menegitis, artritis, myocarditis etc) WBC <4000 or >30000 / mm 3 Htc <30% or Hb<9 gr/dl ABG Pa. O 2<60 mm. Hg PCO 2>50 mm. Hg BUN >20 mg/dl Multilober infiltration, cavity, effusion, rapid progression Sepsis or multisystem disfunction
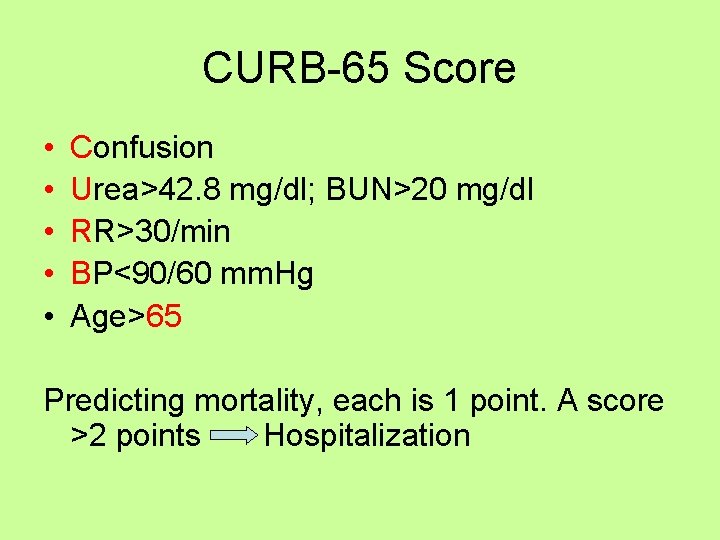
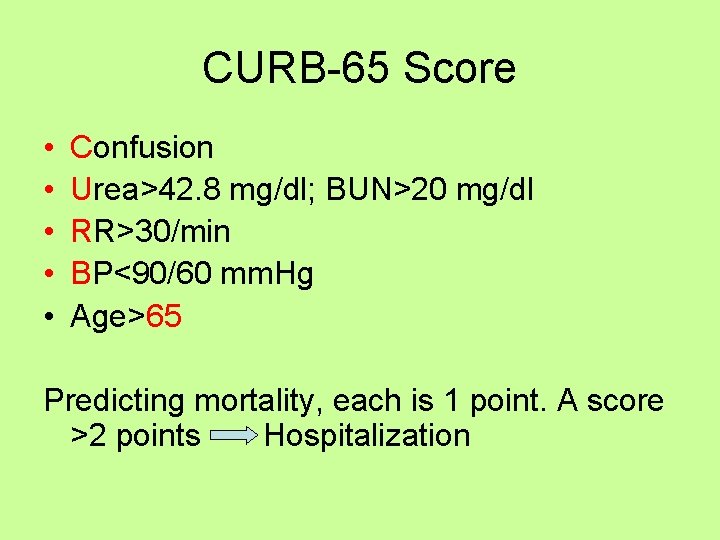
CURB-65 Score • • • Confusion Urea>42. 8 mg/dl; BUN>20 mg/dl RR>30/min BP<90/60 mm. Hg Age>65 Predicting mortality, each is 1 point. A score >2 points Hospitalization
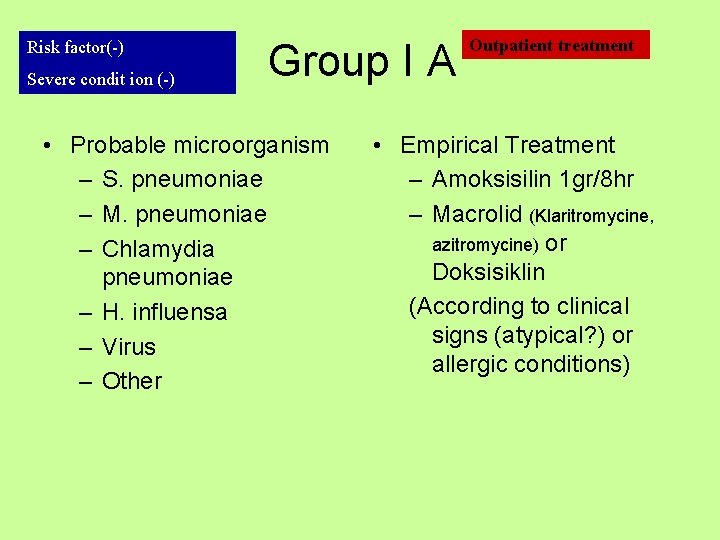
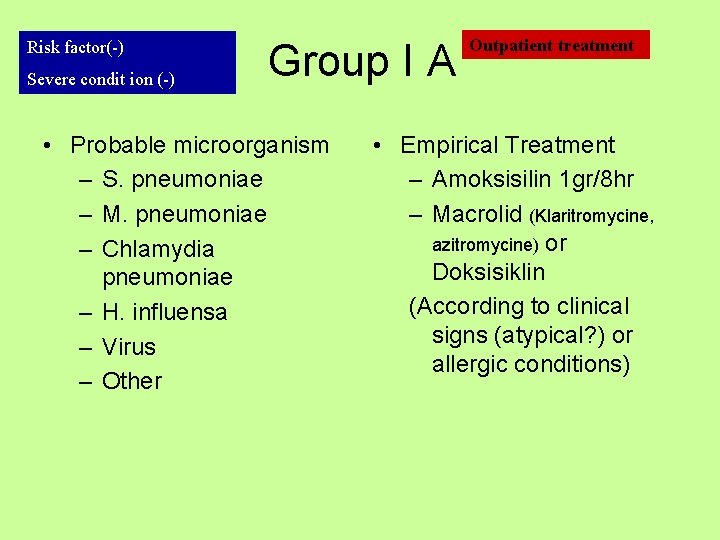
Risk factor(-) Severe condit ion (-) Group I A • Probable microorganism – S. pneumoniae – M. pneumoniae – Chlamydia pneumoniae – H. influensa – Virus – Other Outpatient treatment • Empirical Treatment – Amoksisilin 1 gr/8 hr – Macrolid (Klaritromycine, azitromycine) or Doksisiklin (According to clinical signs (atypical? ) or allergic conditions)
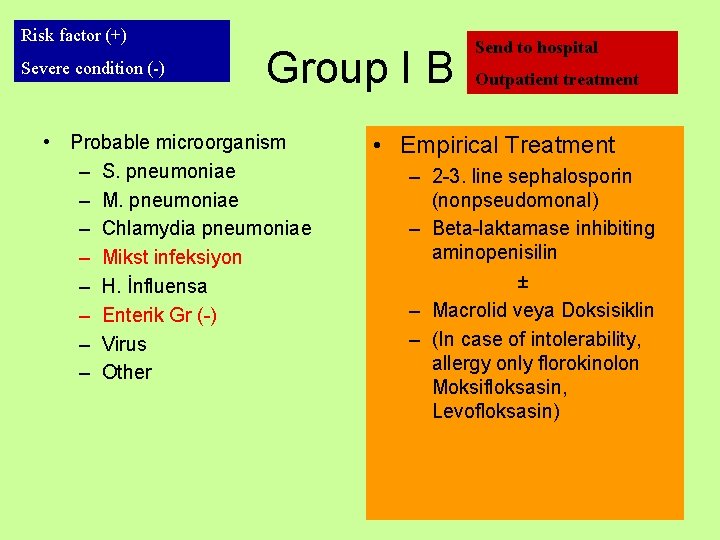
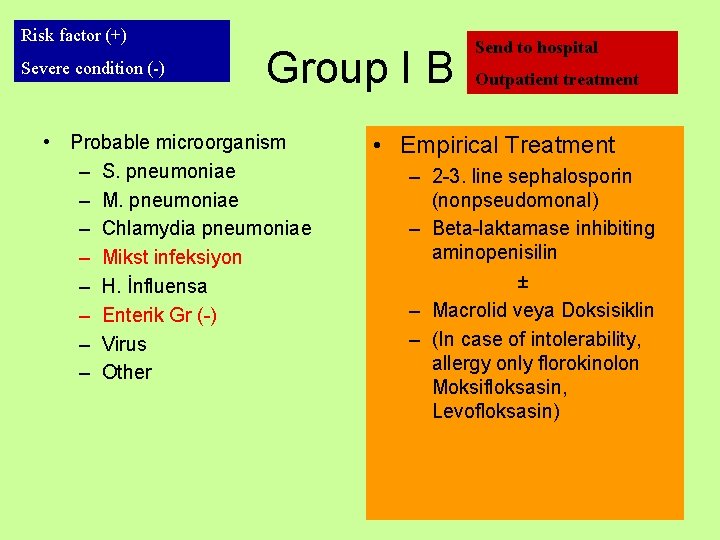
Risk factor (+) Severe condition (-) Group I B • Probable microorganism – S. pneumoniae – M. pneumoniae – Chlamydia pneumoniae – Mikst infeksiyon – H. İnfluensa – Enterik Gr (-) – Virus – Other Send to hospital Outpatient treatment • Empirical Treatment – 2 -3. line sephalosporin (nonpseudomonal) – Beta-laktamase inhibiting aminopenisilin ± – Macrolid veya Doksisiklin – (In case of intolerability, allergy only florokinolon Moksifloksasin, Levofloksasin)
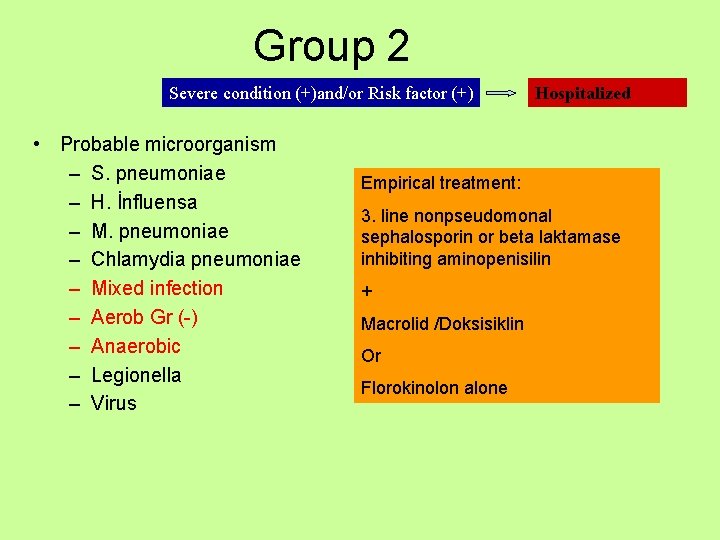
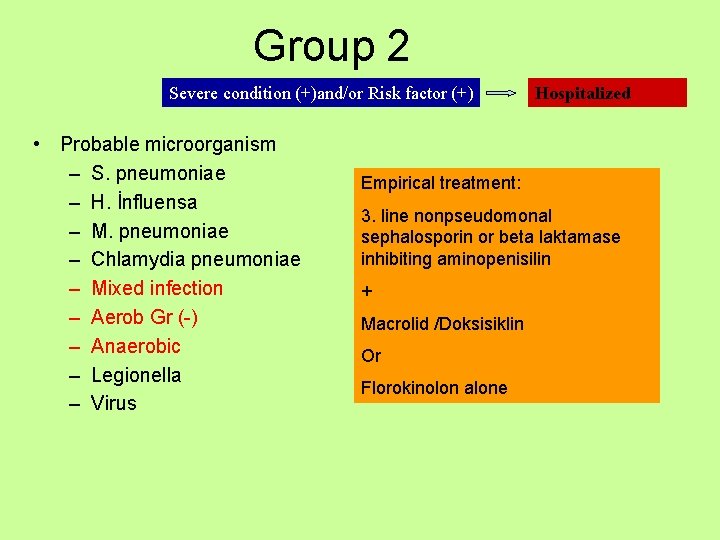
Group 2 Severe condition (+)and/or Risk factor (+) • Probable microorganism – S. pneumoniae – H. İnfluensa – M. pneumoniae – Chlamydia pneumoniae – Mixed infection – Aerob Gr (-) – Anaerobic – Legionella – Virus Hospitalized Empirical treatment: 3. line nonpseudomonal sephalosporin or beta laktamase inhibiting aminopenisilin + Macrolid /Doksisiklin Or Florokinolon alone
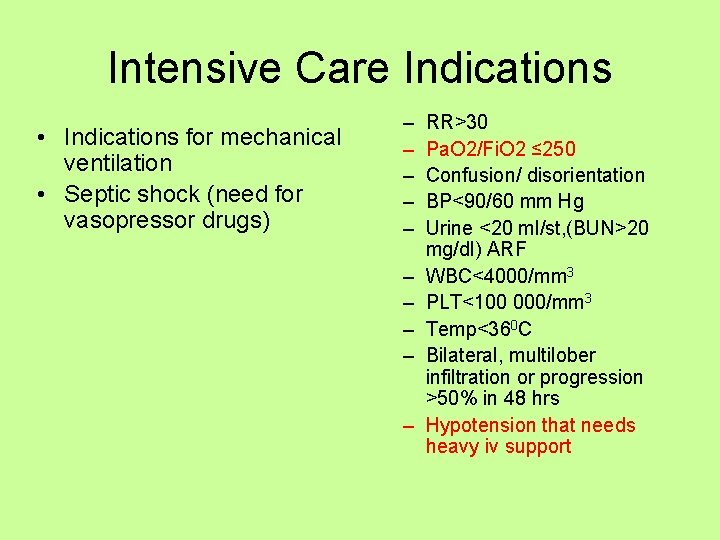
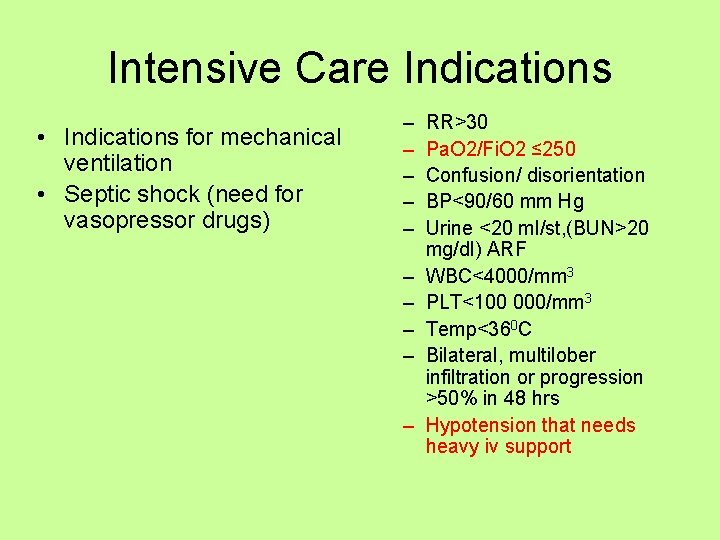
Intensive Care Indications • Indications for mechanical ventilation • Septic shock (need for vasopressor drugs) – – – – – RR>30 Pa. O 2/Fi. O 2 ≤ 250 Confusion/ disorientation BP<90/60 mm Hg Urine <20 ml/st, (BUN>20 mg/dl) ARF WBC<4000/mm 3 PLT<100 000/mm 3 Temp<360 C Bilateral, multilober infiltration or progression >50% in 48 hrs Hypotension that needs heavy iv support
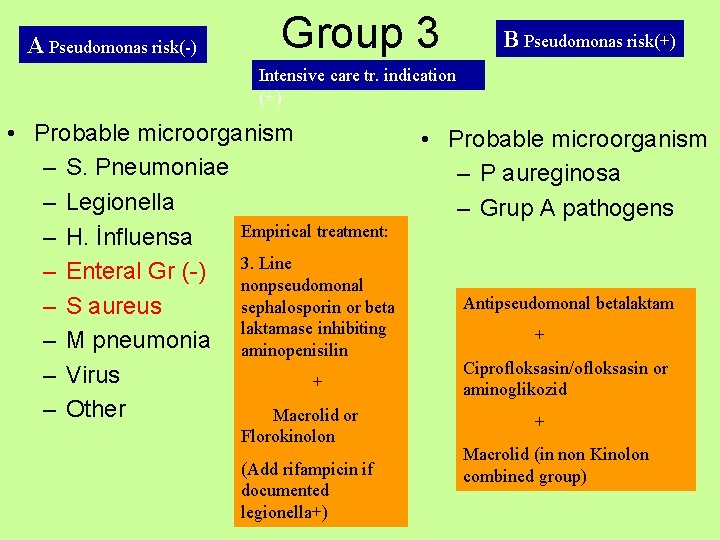
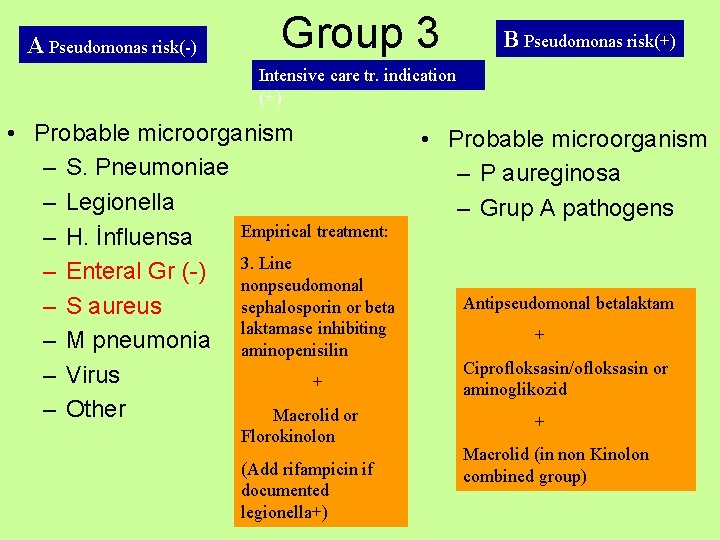
A Pseudomonas risk(-) Group 3 B Pseudomonas risk(+) Intensive care tr. indication (+) • Probable microorganism – S. Pneumoniae – Legionella Empirical treatment: – H. İnfluensa Line – Enteral Gr (-) 3. nonpseudomonal sephalosporin or beta – S aureus laktamase inhibiting – M pneumonia aminopenisilin – Virus + – Other Macrolid or Florokinolon (Add rifampicin if documented legionella+) • Probable microorganism – P aureginosa – Grup A pathogens Antipseudomonal betalaktam + Ciprofloksasin/ofloksasin or aminoglikozid + Macrolid (in non Kinolon combined group)
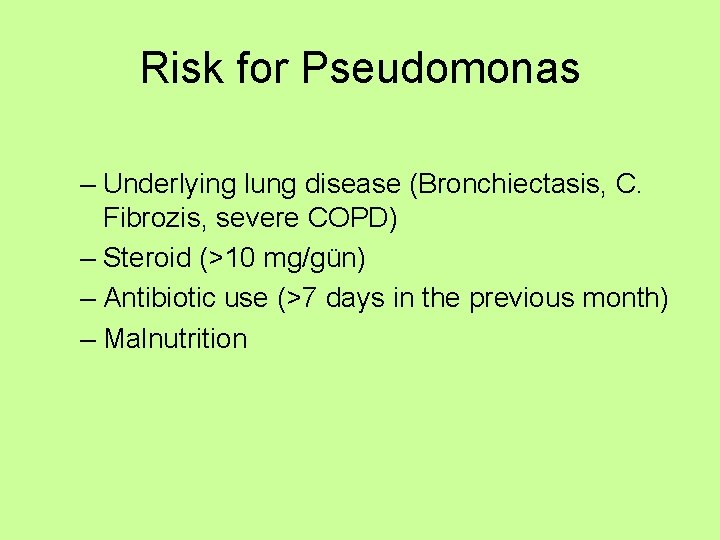
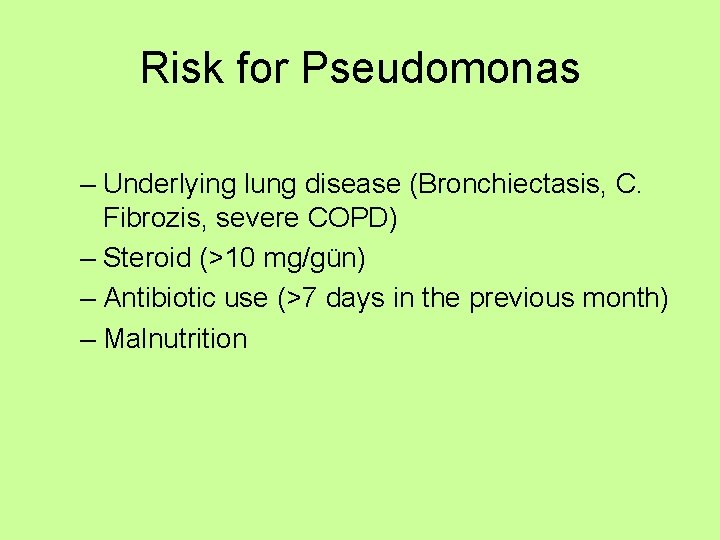
Risk for Pseudomonas – Underlying lung disease (Bronchiectasis, C. Fibrozis, severe COPD) – Steroid (>10 mg/gün) – Antibiotic use (>7 days in the previous month) – Malnutrition
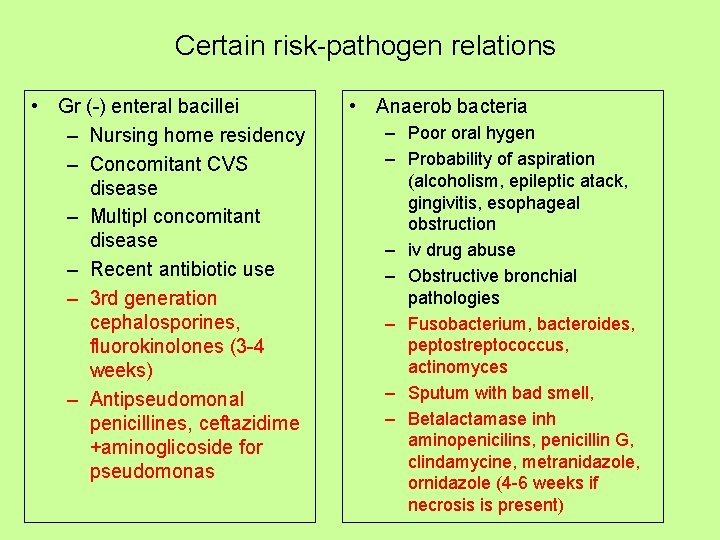
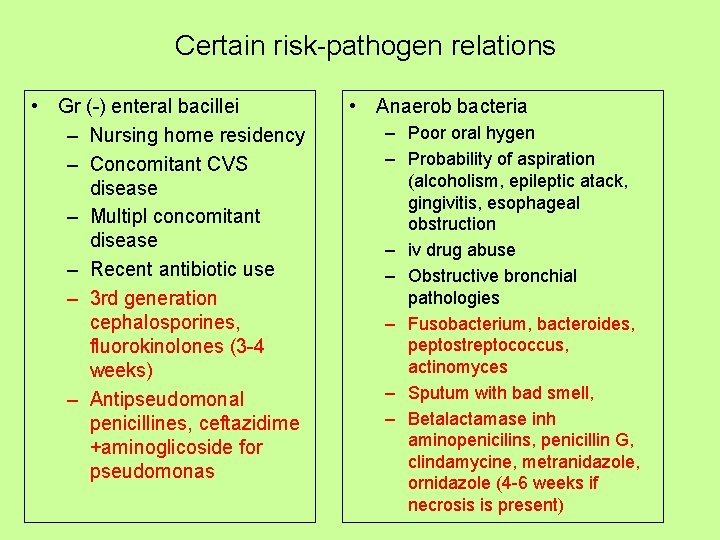
Certain risk-pathogen relations • Gr (-) enteral bacillei – Nursing home residency – Concomitant CVS disease – Multipl concomitant disease – Recent antibiotic use – 3 rd generation cephalosporines, fluorokinolones (3 -4 weeks) – Antipseudomonal penicillines, ceftazidime +aminoglicoside for pseudomonas • Anaerob bacteria – Poor oral hygen – Probability of aspiration (alcoholism, epileptic atack, gingivitis, esophageal obstruction – iv drug abuse – Obstructive bronchial pathologies – Fusobacterium, bacteroides, peptostreptococcus, actinomyces – Sputum with bad smell, – Betalactamase inh aminopenicilins, penicillin G, clindamycine, metranidazole, ornidazole (4 -6 weeks if necrosis is present)
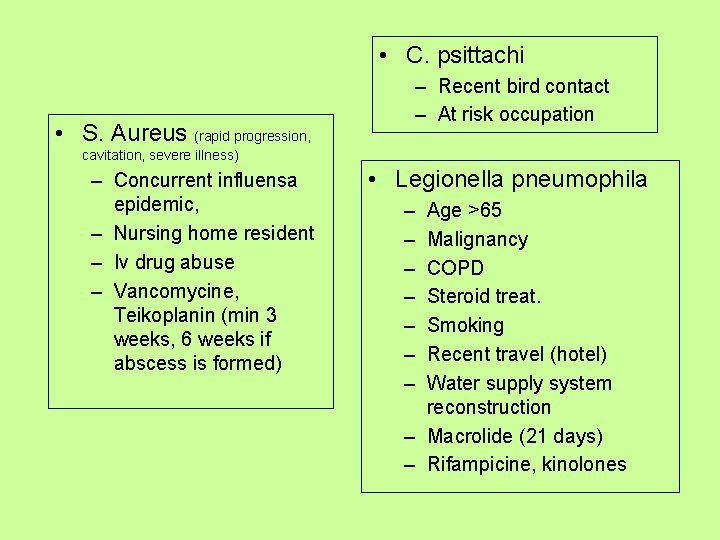
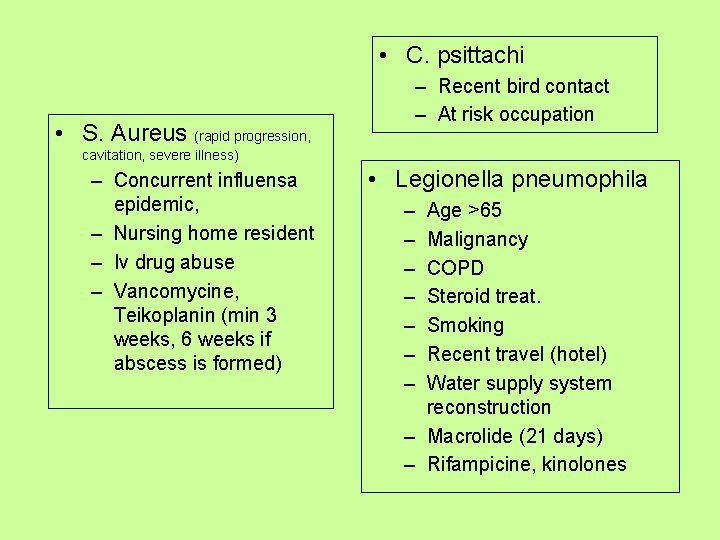
• C. psittachi • S. Aureus (rapid progression, – Recent bird contact – At risk occupation cavitation, severe illness) – Concurrent influensa epidemic, – Nursing home resident – Iv drug abuse – Vancomycine, Teikoplanin (min 3 weeks, 6 weeks if abscess is formed) • Legionella pneumophila – – – – Age >65 Malignancy COPD Steroid treat. Smoking Recent travel (hotel) Water supply system reconstruction – Macrolide (21 days) – Rifampicine, kinolones
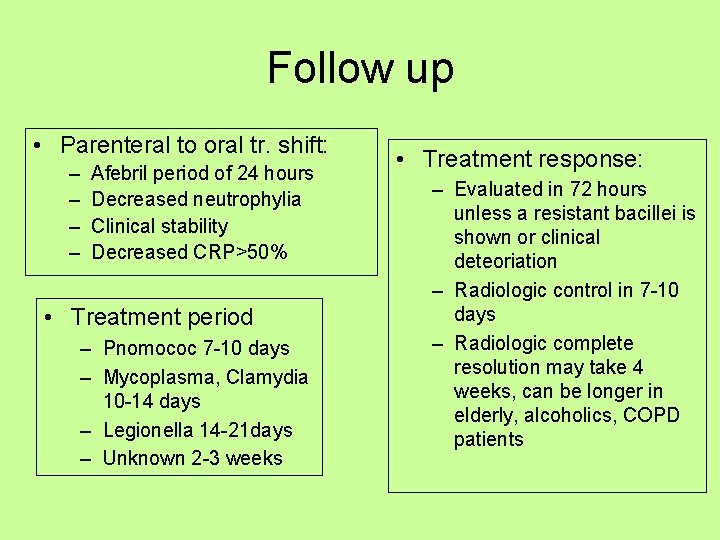
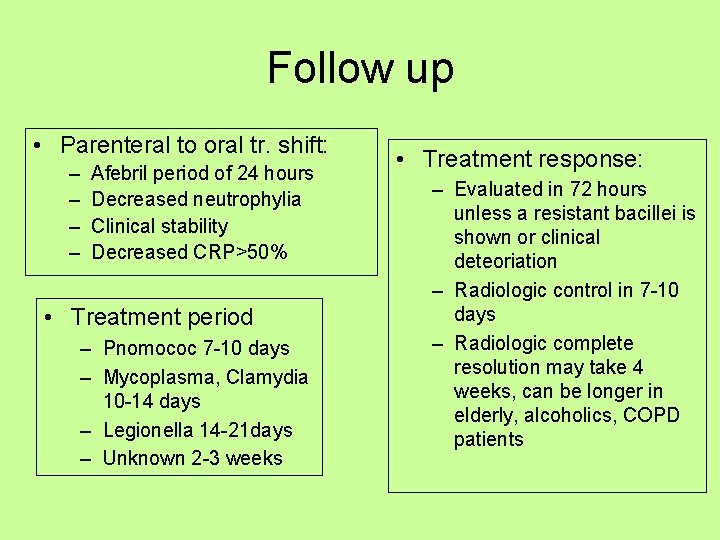
Follow up • Parenteral to oral tr. shift: – – Afebril period of 24 hours Decreased neutrophylia Clinical stability Decreased CRP>50% • Treatment period – Pnomococ 7 -10 days – Mycoplasma, Clamydia 10 -14 days – Legionella 14 -21 days – Unknown 2 -3 weeks • Treatment response: – Evaluated in 72 hours unless a resistant bacillei is shown or clinical deteoriation – Radiologic control in 7 -10 days – Radiologic complete resolution may take 4 weeks, can be longer in elderly, alcoholics, COPD patients
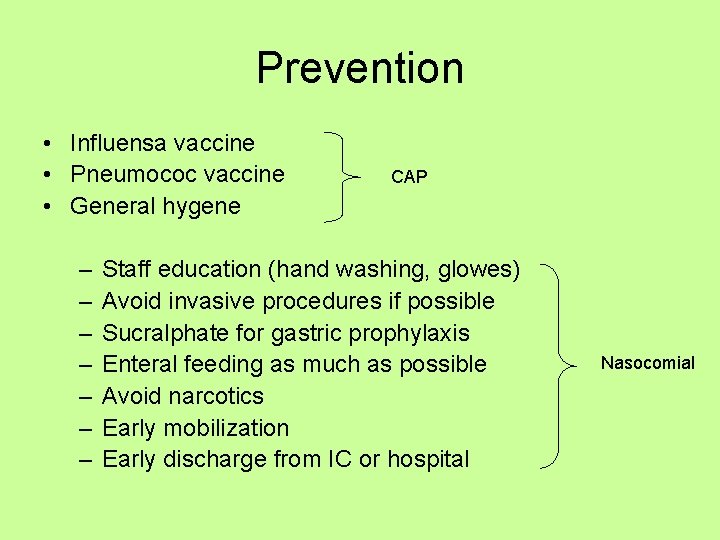
Prevention • Influensa vaccine • Pneumococ vaccine • General hygene – – – – CAP Staff education (hand washing, glowes) Avoid invasive procedures if possible Sucralphate for gastric prophylaxis Enteral feeding as much as possible Avoid narcotics Early mobilization Early discharge from IC or hospital Nasocomial
Certain Definitions • Recurrent pneumonia: A second pneumonia that occurs after the complete healing of a first attack (>1 month). At least 2 times a year. • Late resolution: A pneumonia that resolves <50% in 2 weeks or incomplete regression in 4 weeks • Nasocomial Pneumonia: Pneumonia seen after 48 hours of hospitalization or within 48 hours after being discharged from hospital
Risk factors for late resolution: – – – – Age COPD Alcoholism Smoking D mellitus Malignancy Renal or cardiac failure CS use – – S pneumonia Legionella Viral H influensae
Complications of pneumonia • • • Pleural effusion (parapneumonic) Emphyema Bronchopleural fistule Mediastinitis, pericarditis, chest wall infection Necrosis, cavitation Pneumatocel Pneumothorax ARDS Fibrosis Bronchiectasis Late resolution or recurrens

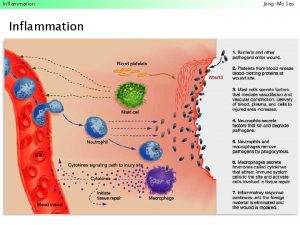
 Acute inflammation definition
Acute inflammation definition Acute inflammation definition
Acute inflammation definition Cellular events of inflammation
Cellular events of inflammation Cardinal sign of inflammation
Cardinal sign of inflammation Acute inflammation
Acute inflammation Morphological pattern of acute inflammation slideshare
Morphological pattern of acute inflammation slideshare Cellular events of acute inflammation
Cellular events of acute inflammation Cardinal sign of inflammation
Cardinal sign of inflammation Vascular response in acute inflammation
Vascular response in acute inflammation Cellular events of acute inflammation
Cellular events of acute inflammation Morphological pattern of inflammation
Morphological pattern of inflammation Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Acute inflammation
Acute inflammation Morphologic patterns of acute inflammation
Morphologic patterns of acute inflammation Acute inflammation
Acute inflammation Waste management definition
Waste management definition Infectious disease quality controls
Infectious disease quality controls Periods of infectious disease
Periods of infectious disease Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Stages of infectious disease
Stages of infectious disease Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease board review
Infectious disease board review Certain infectious and parasitic diseases
Certain infectious and parasitic diseases What is the smallest infectious agent
What is the smallest infectious agent Papillomitosis
Papillomitosis Infectious nucleic acid
Infectious nucleic acid University of washington
University of washington Infectious disease
Infectious disease Ebv
Ebv Hennepin county infectious disease manual
Hennepin county infectious disease manual Epidemiological triad of malaria
Epidemiological triad of malaria Hhps symbols
Hhps symbols Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Infectious stunting syndrome
Infectious stunting syndrome Prof. dr. bilun gemicioğlu
Prof. dr. bilun gemicioğlu Verminous pneumonia
Verminous pneumonia Pathophysiology of appendicitis
Pathophysiology of appendicitis Cardiac output trained vs untrained
Cardiac output trained vs untrained Periodontitis apicalis chronica
Periodontitis apicalis chronica Bell clapper deformity pictures
Bell clapper deformity pictures Acute angle definition
Acute angle definition Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể