Pathology of inflammation LEC 1 Overview of Inflammation






- Slides: 38
Pathology of inflammation LEC 1 ﺩ ﻫﺒﺔ ﺍﺣﻤﺪ ﻏﻴﺪﺍﻥ
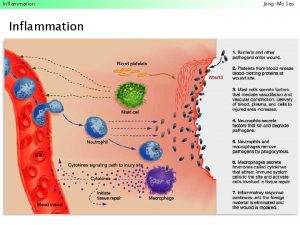
Overview of Inflammation: • Inflammation is a protective response of vascularized living tissue to injury. • It may be evoked by microbial infections, physical agents, chemicals, necrotic tissue, or immune reactions. • The goals of Inflammation are to contain and isolate injury, to destroy invading microorganisms , inactivate toxins, and to prepare the tissue for healing and repair. • However, the benefits of inflammation, It can also be harmful, for example, by causing life-threatening hypersensitivity reactions or progressive organ damage from chronic inflammation and subsequent fibrosis.
Inflammation can be divided into two basic types; • Acute inflammation : • Chronic inflammation:

1 - Acute inflammation : • Early onset (i. e. , seconds to minutes). short duration (i. e. , minutes to days), involving fluid exudation (edema) and polymorphonuclear cell (neutrophil) emigration. • The suffix (itis) add to the name of organs signifying acute inflammation, but with some exceptions e. g. colitis, appendicitis
2 - Chronic inflammation: • Later onset (i. e. , days) and longer duration (i. e. , weeks to years), involving lymphocytes and macrophages, with blood vessel proliferation and fibrosis. • The suffix (osis) add to the name of organs signifying chronic inflammation, e. g. dermatosis
Classical (cardinal) clinical sings of inflammation: There are five cardinal signs of inflammation (most prominent in acute inflammation): 1. Warmth (Latin: calor) due to vascular dilation 2. Erythema (Latin: rubor) due to vascular dilation and congestion 3. Edema (Latin: tumor) due to increased vascular permeability 4. Pain (Latin: dolor) due to mediator release 5. Loss of function (Latin: functio laesa) due to pain, edema, tissue injury, and/or scar
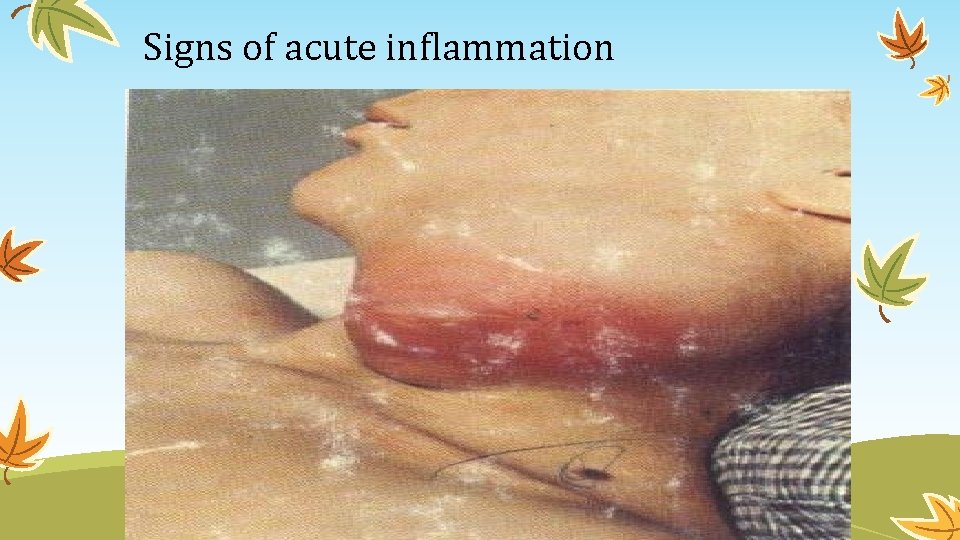
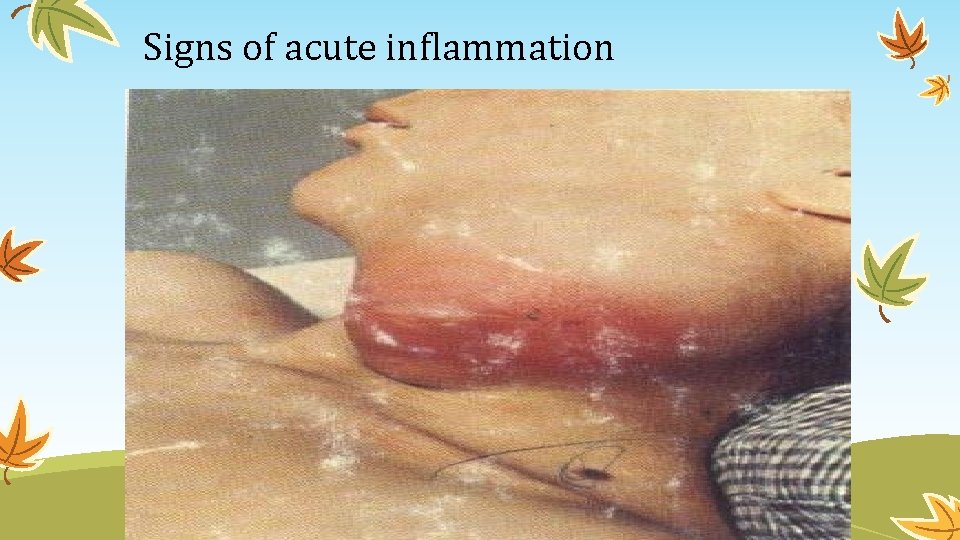
Signs of acute inflammation
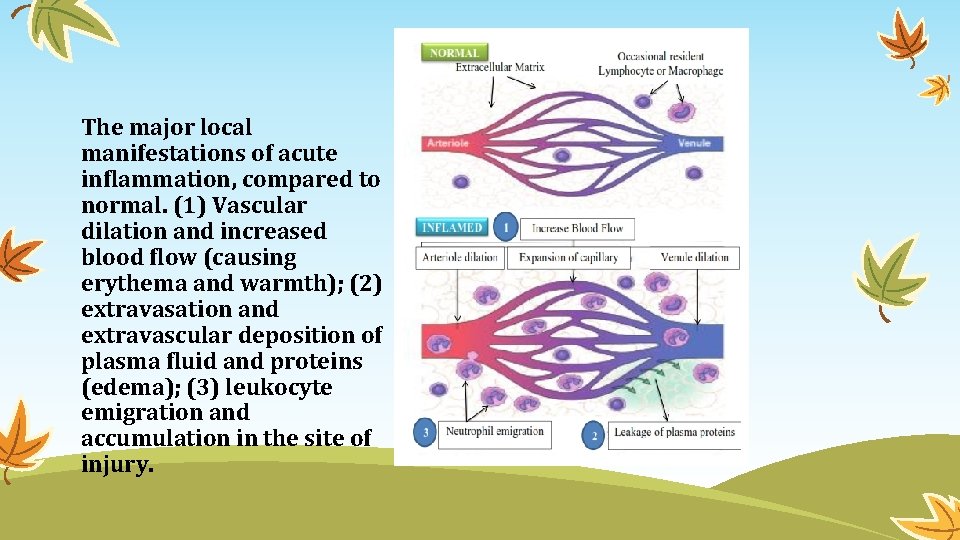
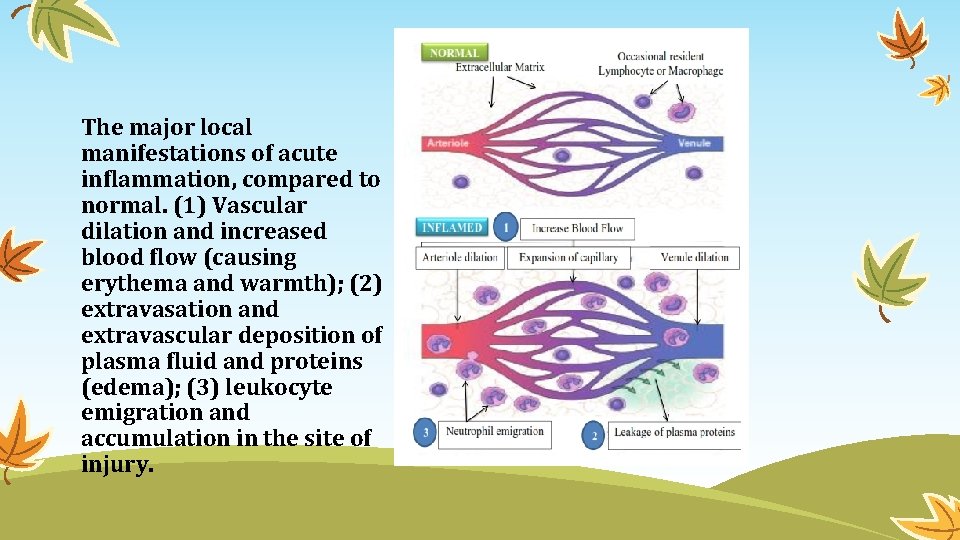
The major local manifestations of acute inflammation, compared to normal. (1) Vascular dilation and increased blood flow (causing erythema and warmth); (2) extravasation and extravascular deposition of plasma fluid and proteins (edema); (3) leukocyte emigration and accumulation in the site of injury.
Acute Inflammation Acute inflammation is a rapid host response that serves to deliver leukocytes and plasma proteins to sites of infection or tissue injury.
Stimuli of acute inflammation Acute inflammatory reactions are triggered by a variety of stimuli that include: 1. Infections: bacterial, viral, parasitic and microbial toxins 2. Physical and chemical agents (trauma, thermal injuries, irradiation, toxins, strong acids, etc. ) 3. Tissue necrosis (of any from or cause) 4. Foreign bodies (splinters, dirt, sutures) 5. Immune reactions (hypersensitivity and autoimmune reactions)
Acute inflammation has three major components: (1) alterations in vascular caliber that lead to an increase in blood flow. (2) structural changes in the microvasculature that permit plasma proteins and leukocytes to leave the circulation. (3) emigration of the leukocytes from the microcirculation, their accumulation in the focus of injury, and their activation to eliminate the offending agent. 1 and 2 3 ( vascular changes ) (cellular changes)

Reactions of Blood Vessels in Acute Inflammation : Normal fluid exchange in vascular beds depends on an intact endothelium and is modulated by two opposing forces: • Hydrostatic pressure causes fluid to move out of the circulation. • Plasma colloid osmotic pressure causes fluid to move into the capillaries.
DEFINITIONS Edema is excess fluid in interstitial tissue or body cavities and can be either an exudate or a transudate. Exudate is an inflammatory, extravascular fluid with cellular debris and high protein concentration (specific gravity of 1. 020 or more), . Occurred due to increase permeability of capillaries Transudate is excess, extravascular fluid with low protein content (specific gravity of 1. 012 or less); it is essentially an ultrafiltrate of blood plasma resulting from increase hydrostatic pressure or diminished plasma osmotic forces. Pus is a purulent inflammatory exudate rich in neutrophils and cell debris.
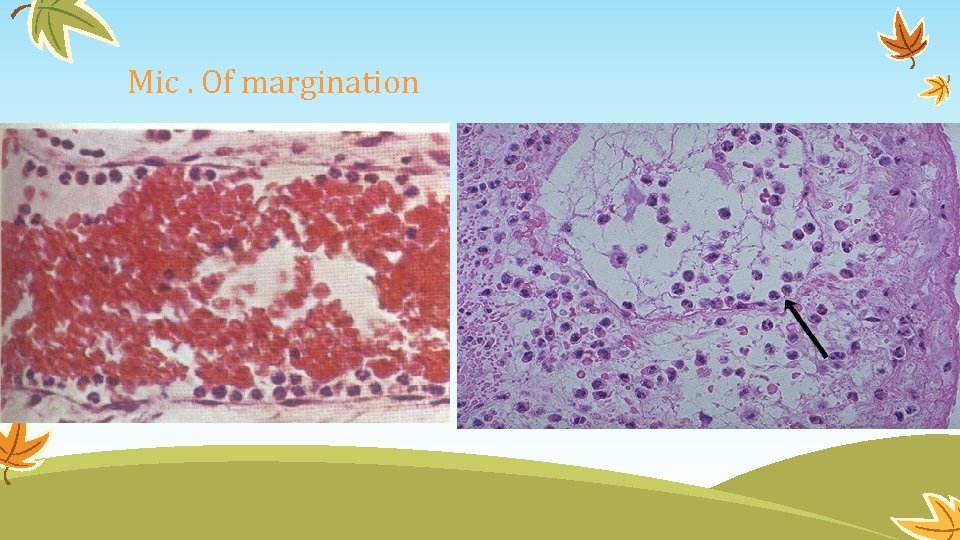
Changes in Vascular Flow and Caliber: 1. After transient seconds from cell injury, there is vasoconstriction. 2. Then there is arteriolar vasodilatation, which result in increase local blood flow to capillary bed (this responsible for hotness & redness of area). 3. Movement of protein rich fluid into extravascular areas, this movement of fluid will leave the blood concentrated by RBCs (increase viscosity & slowing the circulation) & this called Stasis. Mic. Dilated small vessels packed with RBCs. 4. After stasis leukocytes (Neutrophils) change their normal flow in vessels, & begin to accumulate along the vascular endothelial surface (Margination).
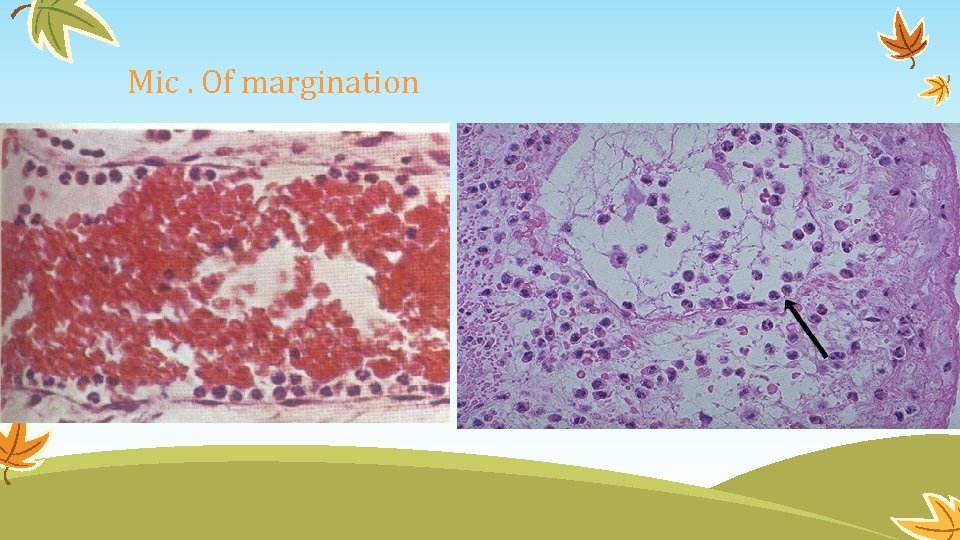
Mic. Of margination
Increased vascular permeability: q This increase in permeability is occurred as a result of arteriolar vasodilatation & increase blood flow into the capillary bed which results in increased hydrostatic pressure & movement of fluid from capillaries, this fluid is called Transudate. q. Transudate should differentiate from Exudates, which occur due to increased vascular permeability & persistence the cause of cell injury. q. As a result of exudates, there is decrease in intravascular osmotic pressure & increase interstitial osmotic pressure, which result in escape of water & ions into interstitium which is called Edema.
Mechanisms of increased vascular permeability: 1. Endothelial cell contraction leads to intercellular gaps in the venules: 2. Endothelial cell retraction: 3. Direct endothelial injury: is either I. Immediate sustained response: Characterized by: II. delayed prolonged leakage: 4. Leukocyte dependent endothelial injury: 5. leakage from newly formed blood vessels: 6. Increased transcytosis:
1. Endothelial cell contraction leads to intercellular gaps in the venules: • Reversible process. • Only occur in the endothelial cells of postcapillary venules. • Induced by chemical mediators (histamine, bradykinin) • It is immediate transient response (15 – 30 minutes).
2. Endothelial cell retraction: • Reversible mechanism. • Induced by TNF(tumor necrotic factor ) & interlukin 1(IL-1). • Takes place within 4 -6 hr & last for up to 24 hrs. • There is structural reorganization of endothelial cells cytoskeleton which result in disruption of cells junctions.
3. Direct endothelial injury: is either I. Immediate sustained response: Characterized by: • Endothelial cells necrosis & detachment……. platelets adhesion & thrombosis. • Seen in severe injuries (burns, infections). • Begins immediately after injury persists for hrs-days (immediate sustained response) & affects venules, capillaries & arterioles. II. delayed prolonged leakage: • Begins after a delay of 2 -12 hrs. • affect venules & capillaries only. • seen in mild to moderate injury like in bacterial toxins injury, X-ray & ultraviolet injury.
4. Leukocyte dependent endothelial injury: • Inflammatory leukocyte induced endothelial injury by secretion of free radicals & proteolytic enzymes. • Seen in vascular organs mainly in pulmonary venules & capillaries. 5. leakage from newly formed blood vessels: new blood vessels formation during tissue repair after inflammation, these vessels are leaky till mature endothelial cells & intercellular junction area formed. 6. Increased transcytosis: • Increased venular permeability due to induction by (VEGF) through intracellular channels.
Cellular changes of acute inflammation: • A critical function of inflammation is to deliver leukocytes to sites of injury, especially those cells capable of phagocytosing microbes and necrotic debris (e. g. , neutrophils and macrophages). • After recruitment, the cells must recognize microbes and dead material and effect their removal. • The type of leukocyte that ultimately migrates into a site of injury depends on the age of the inflammatory response and the original stimulus.
• In most forms of acute inflammation, neutrophils predominate during the first 6 to 24 hours and are then replaced by monocytes after 24 to 48 hours. • There are several reasons for this sequence:

• neutrophils are more numerous in blood than monocytes, they respond more rapidly to chemokines, and they attach more firmly to the particular adhesion molecules that are induced on endothelial cells at early time points. • After migration, neutrophils are also short-lived; they undergo apoptosis after 24 to 48 hours, whereas monocytes survive longer.

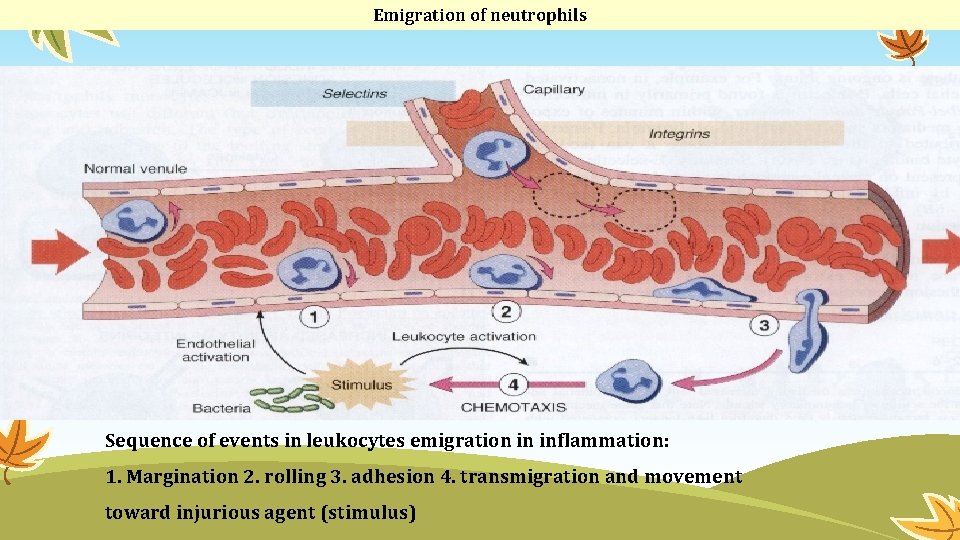
The process of getting cells from vessel lumen to tissue interstitium is called extravasation and is divided into 4 steps: 1. Margination & Rolling 2. Adhesion & Transmigratiuon: 3. Chemotaxis & Activation: 4. Phagocytosis & Degranulation of leukocytes
Cellular events
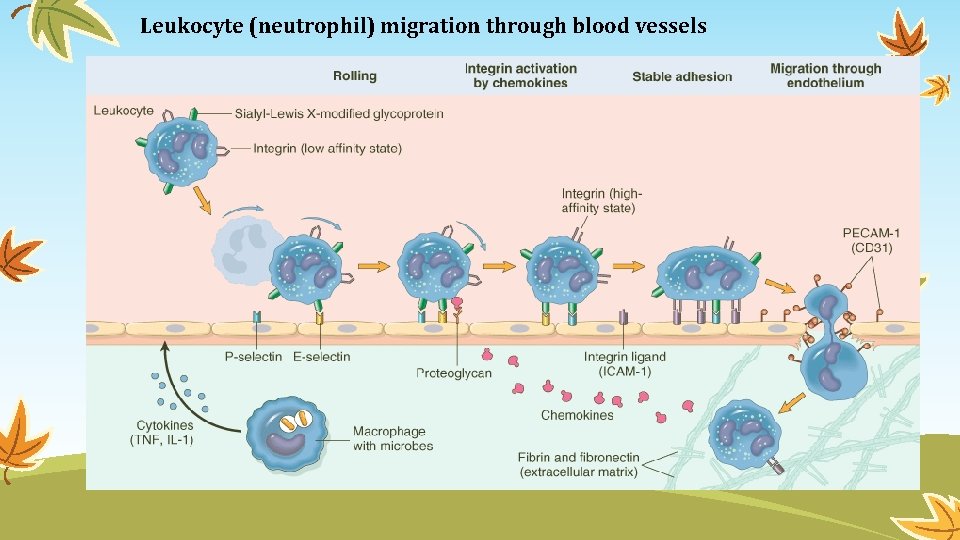
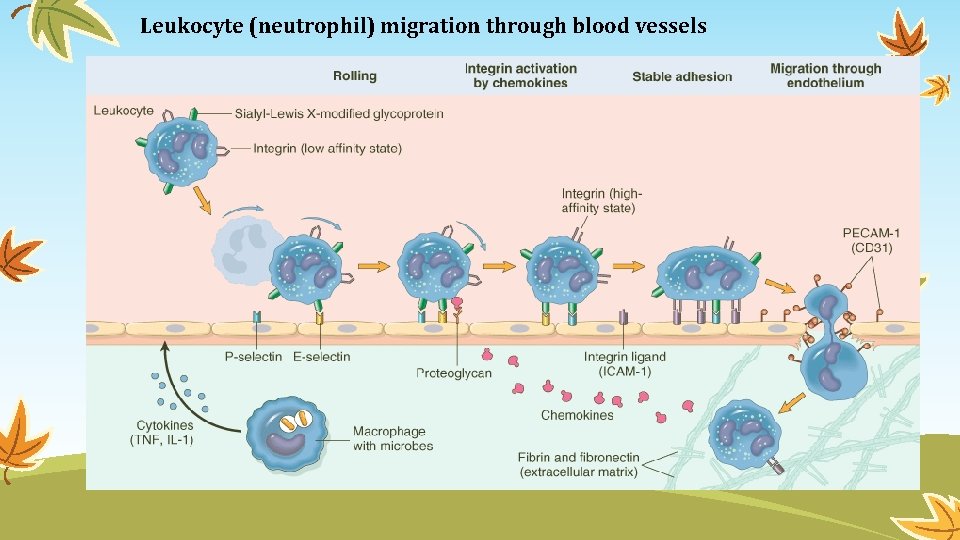
Leukocyte (neutrophil) migration through blood vessels
1. Margination & Rolling: • Under normal condition the flow of blood within capillaries is a laminar flow (plasma, WBC & then RBC) from outside to inside, , , this arrangement make leukocytes more liable to react with endothelial cells of vessels. • As permeability of vessels is increased at early stage of inflammation will result slowness of flow inside the vessels which also increase margination of WBCs. • Subsequently leukocytes tumble on the endothelial cell surface, which is called Rolling of WBCs. (Rolling is occurred due to interaction between protein receptors on leukocytes & sugar on the endothelial cells).
2. Adhesion & Transmigratiuon: • WBC stick the surface of endothelial cells, this is called Adhesion, which is achieved by interaction between Immunoglobulin molecules on endothelial cells & integrins on the leukocytes (Adhesive molecules). • Then Crawling of WBCs between endothelial cells & through basement membrane into the extravascular space is called Transmigration & movement of WBC during this process is called Diapedsis.
3. Chemotaxis & Activation: • After extravasation of WBCs; they will migrate toward sites of injury along chemical gradient, this is called Chemotaxis. • Chemical gradient is more at the site of injury. • Movement of WBC during Chemotaxis toward the sites of injury is achieved by pseudopodia (by actin filaments within WBC).
• Chemotactics (these are proteins present at the site of injury attract WBC to this site), like Soluble bacterial proteins, complement system components like C 5 a, Cytokines (IL-8) , leukotriene B 4. • Activation of WBC is stimulated by the above Chemotactics, & include the followings: • I. Degranulation & secretion of lysosomal enzymes. • II. Production of Arachidonic Acid metabolites (chemical mediators). • III. Modulation of leucocytes adhesive molecules (increased or decreased).
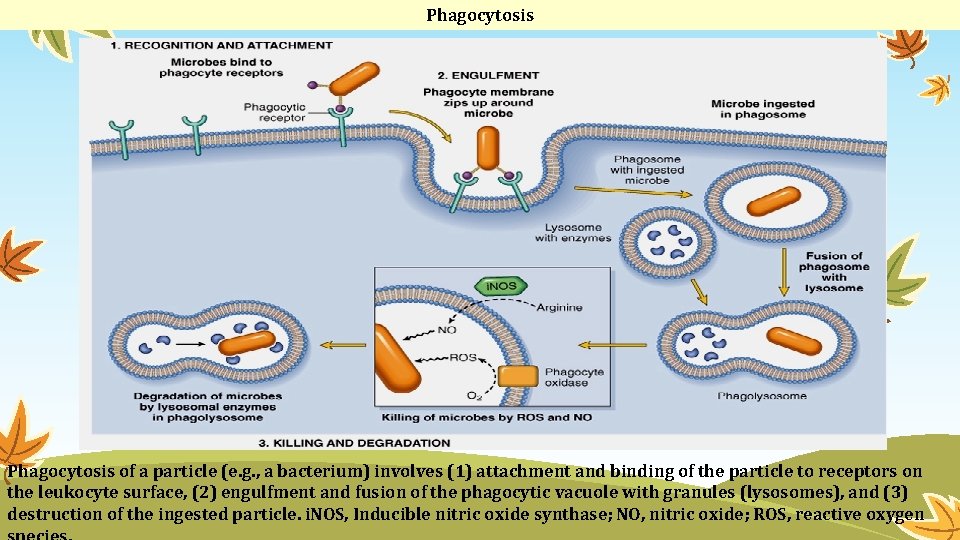
4. Phagocytosis & Degranulation of leukocytes, which include three steps: a. Recognition & attachment of injurious particle to the ingesting leukocytes (by Opsonization) Opsonization is the process by which injurious particles are coated by specific plasma particles that are called opsonins, to facilitate the recognition & attachment of injurious particles to the killer leukocytes. These opsonins are included Ig. G, C 3 b & plasma carbohydrate binding particle called Collectins.
b. Engulfment of injurious particle & formation of phagocytic vacuole by Pseudopods of WBC, & then fusion of these vacuoles with the membrane of lysosomes. C. killing & degradation of injurious particles by production of free radicals.
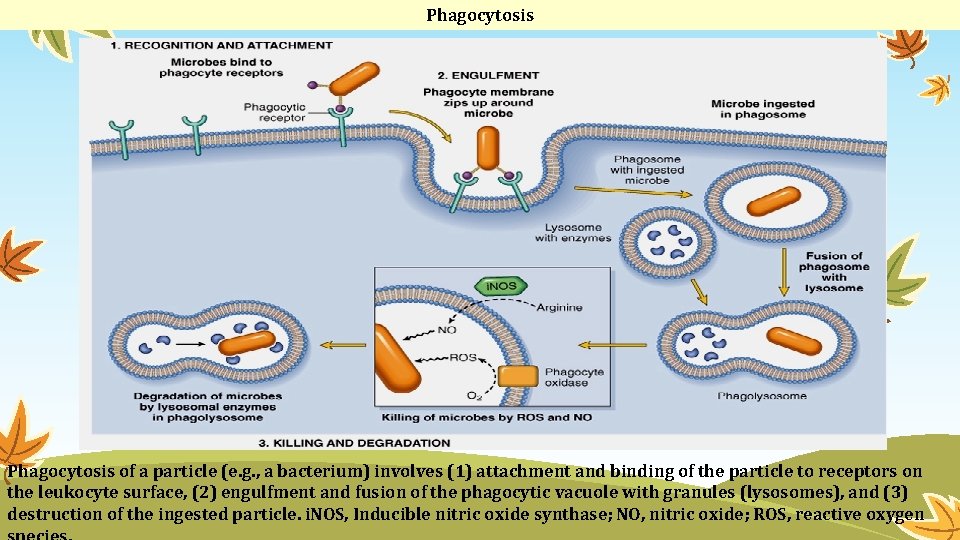
Phagocytosis of a particle (e. g. , a bacterium) involves (1) attachment and binding of the particle to receptors on the leukocyte surface, (2) engulfment and fusion of the phagocytic vacuole with granules (lysosomes), and (3) destruction of the ingested particle. i. NOS, Inducible nitric oxide synthase; NO, nitric oxide; ROS, reactive oxygen
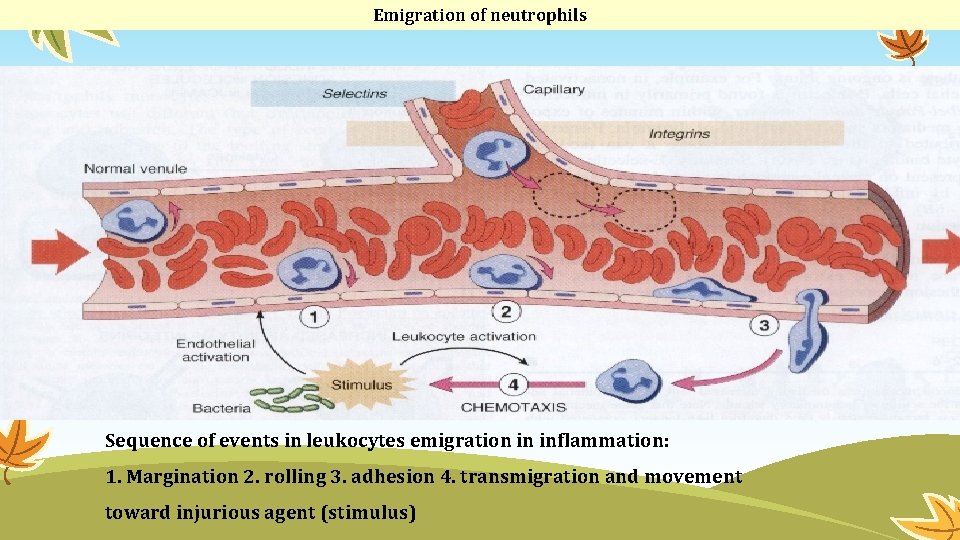
Emigration of neutrophils Sequence of events in leukocytes emigration in inflammation: 1. Margination 2. rolling 3. adhesion 4. transmigration and movement toward injurious agent (stimulus)

Questions?

 132000 lec
132000 lec Lec hardver
Lec hardver 11th chemistry thermodynamics lec 10
11th chemistry thermodynamics lec 10 Lec renal
Lec renal Lec material
Lec material Back work ratio formula
Back work ratio formula Lec ditto
Lec ditto Xrl in 8051
Xrl in 8051 Fenemates
Fenemates Lec element
Lec element Sekisui s-lec america llc
Sekisui s-lec america llc 252 lec
252 lec Art 455 lec
Art 455 lec Lec promotion
Lec promotion Lec scoreboard
Lec scoreboard Tura analítica
Tura analítica Lec barbate
Lec barbate August lec 250
August lec 250 416 lec
416 lec Scoreboard computer architecture
Scoreboard computer architecture Lec
Lec Lec anatomia
Lec anatomia Componentes del lec
Componentes del lec Lec hardver
Lec hardver Lec
Lec Lec 16
Lec 16 11th chemistry thermodynamics lec 13
11th chemistry thermodynamics lec 13 Vegetations in infective endocarditis
Vegetations in infective endocarditis Introduction to cryptology
Introduction to cryptology Pathology
Pathology Albugo eye
Albugo eye National pathology week
National pathology week Ajkd atlas of renal pathology
Ajkd atlas of renal pathology Snomed codes pathology
Snomed codes pathology Clinical pathology laboratories
Clinical pathology laboratories Fraser health authority map
Fraser health authority map Plant pathology
Plant pathology Verrucus
Verrucus Cert 3 in pathology collection
Cert 3 in pathology collection