Pathologic Spinal Fracture S M Jamalaldini Ortheopadic Spine








- Slides: 56

Pathologic Spinal Fracture S. M. Jamalaldini. Ortheopadic Spine surgeon Medical University of Yazd april 2017
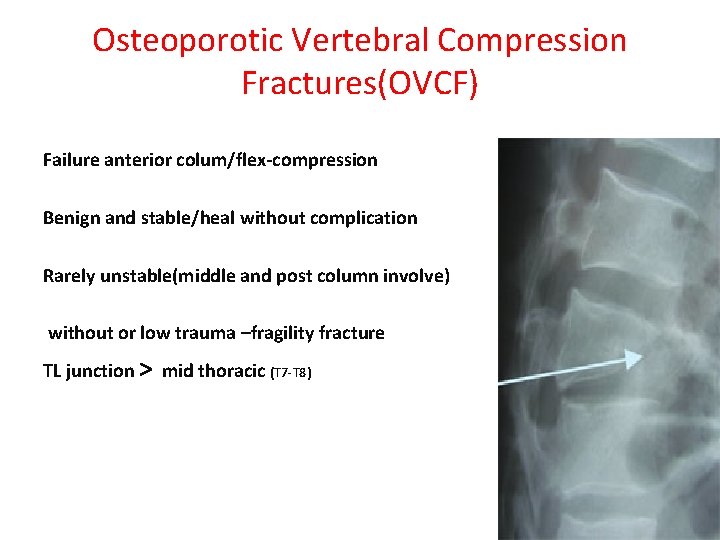
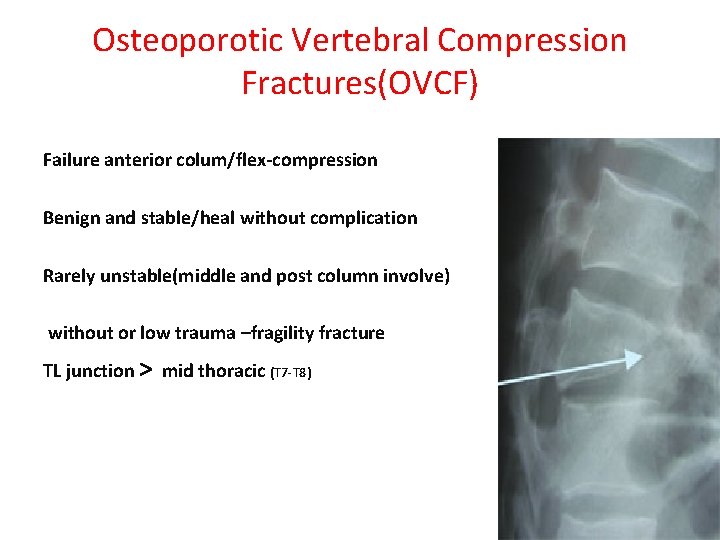
Osteoporotic Vertebral Compression Fractures(OVCF) Failure anterior colum/flex-compression Benign and stable/heal without complication Rarely unstable(middle and post column involve) without or low trauma –fragility fracture TL junction > mid thoracic (T 7 -T 8)
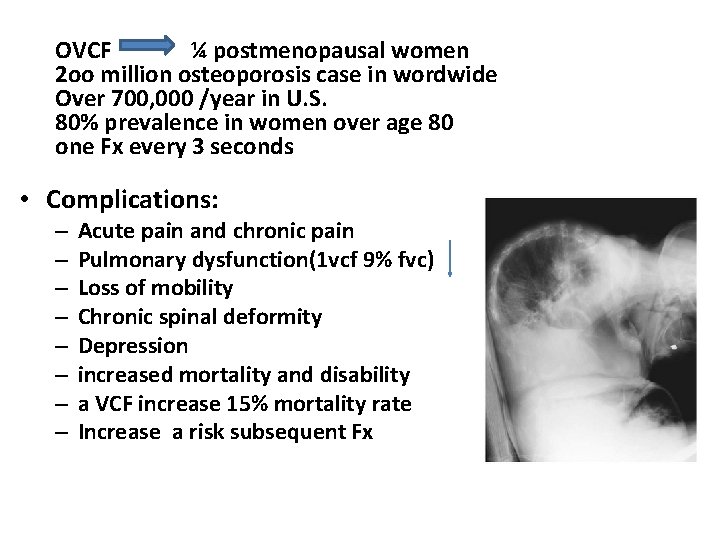
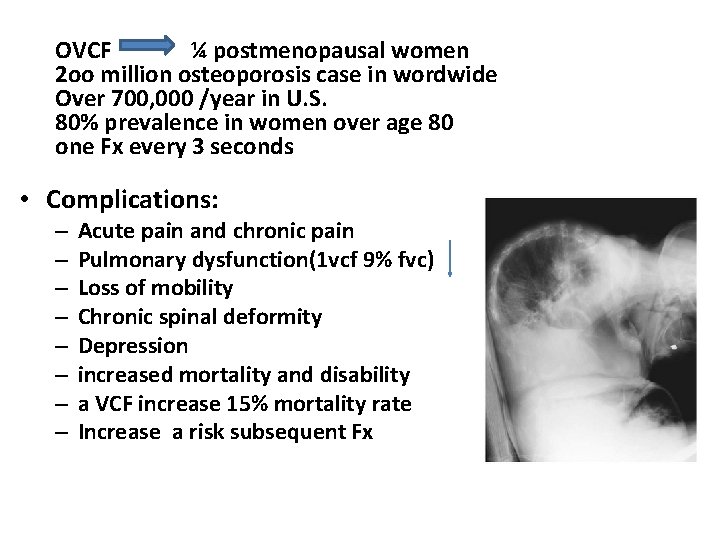
OVCF ¼ postmenopausal women 2 oo million osteoporosis case in wordwide Over 700, 000 /year in U. S. 80% prevalence in women over age 80 one Fx every 3 seconds • Complications: – – – – Acute pain and chronic pain Pulmonary dysfunction(1 vcf 9% fvc) Loss of mobility Chronic spinal deformity Depression increased mortality and disability a VCF increase 15% mortality rate Increase a risk subsequent Fx
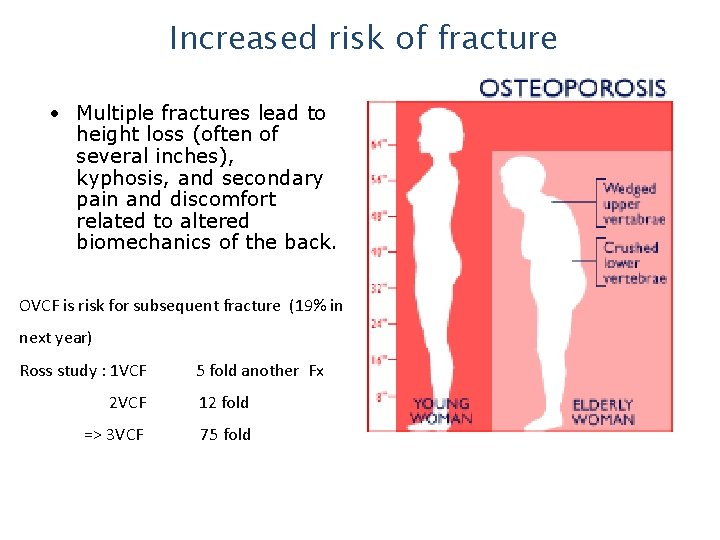
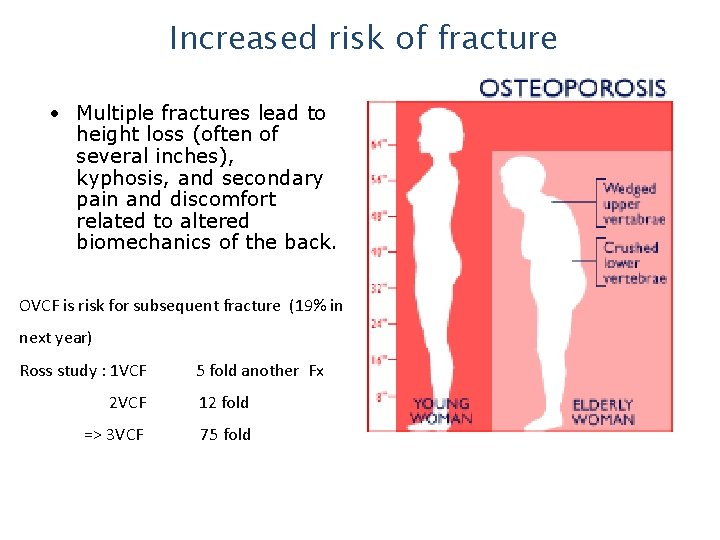
Increased risk of fracture • Multiple fractures lead to height loss (often of several inches), kyphosis, and secondary pain and discomfort related to altered biomechanics of the back. OVCF is risk for subsequent fracture (19% in next year) Ross study : 1 VCF 5 fold another Fx 2 VCF 12 fold => 3 VCF 75 fold
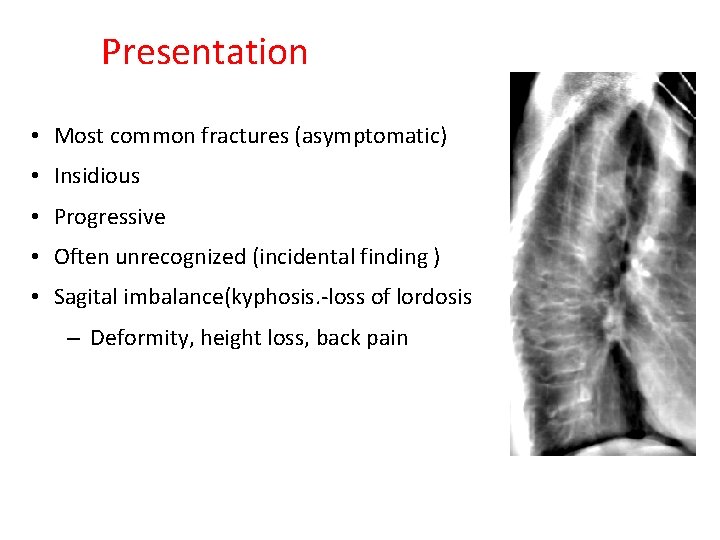
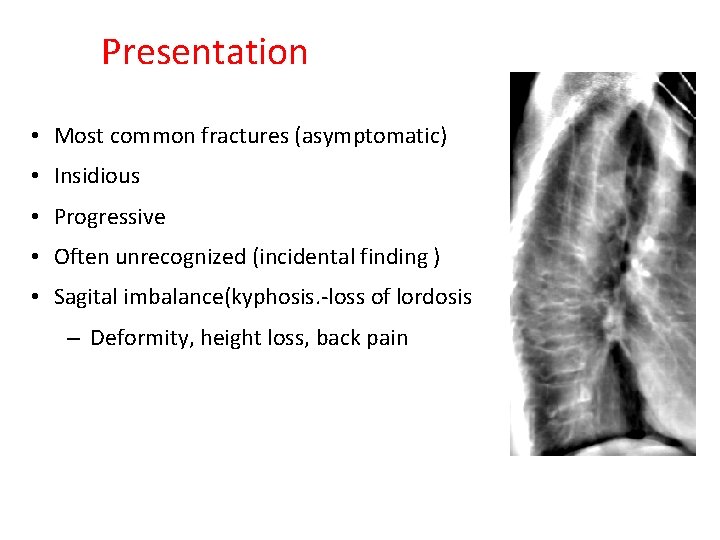
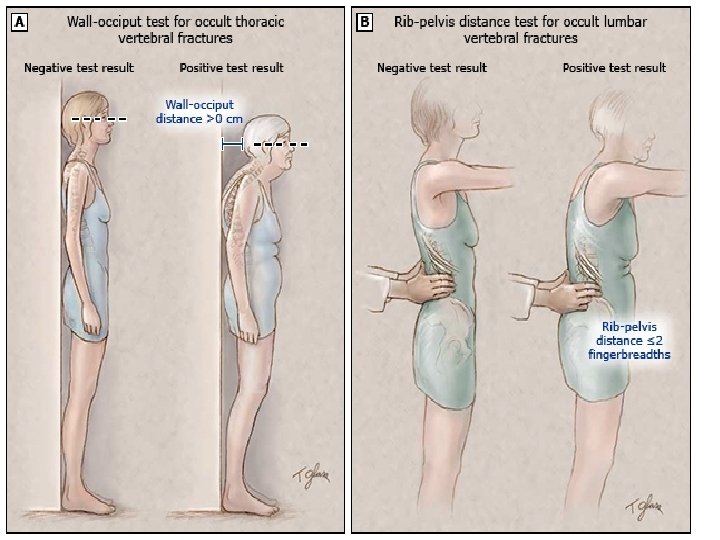
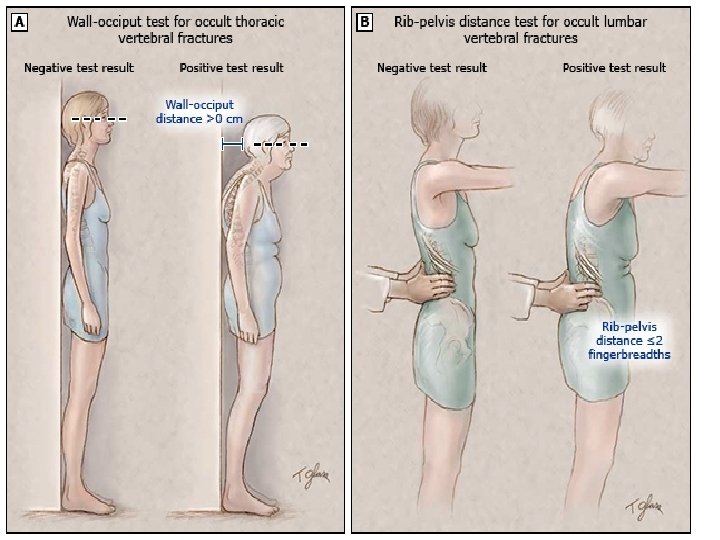
Presentation • Most common fractures (asymptomatic) • Insidious • Progressive • Often unrecognized (incidental finding ) • Sagital imbalance(kyphosis. -loss of lordosis – Deformity, height loss, back pain
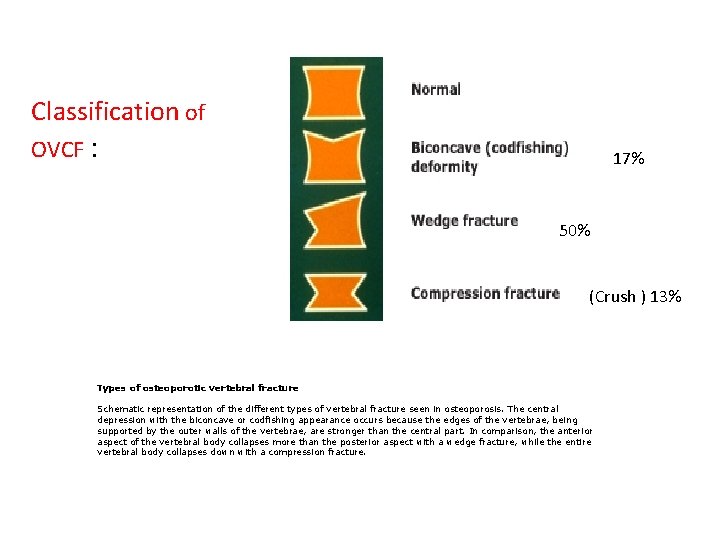
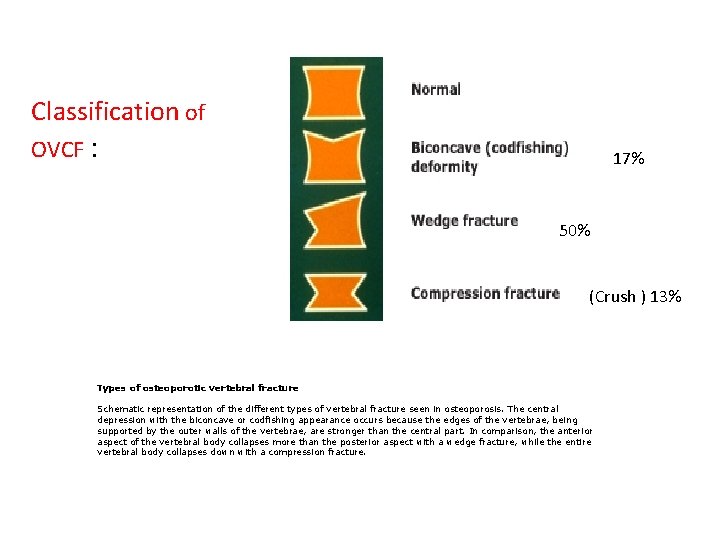
Classification of OVCF : 17% 50% (Crush ) 13% Types of osteoporotic vertebral fracture Schematic representation of the different types of vertebral fracture seen in osteoporosis. The central depression with the biconcave or codfishing appearance occurs because the edges of the vertebrae, being supported by the outer walls of the vertebrae, are stronger than the central part. In comparison, the anterior aspect of the vertebral body collapses more than the posterior aspect with a wedge fracture, while the entire vertebral body collapses down with a compression fracture.
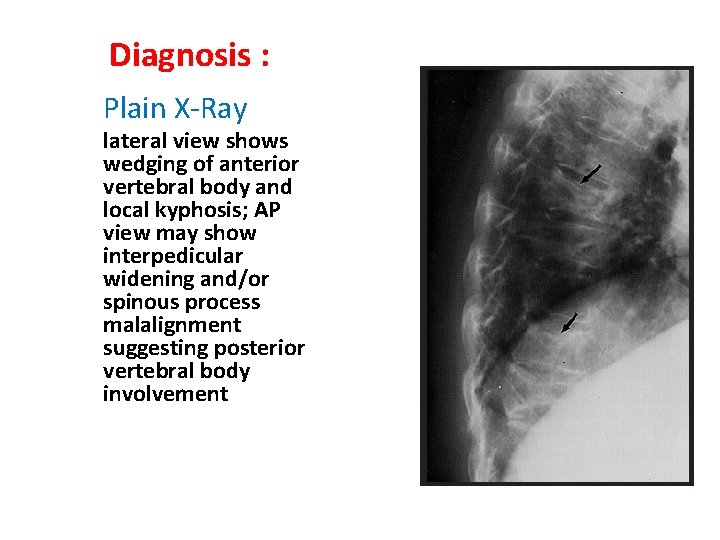
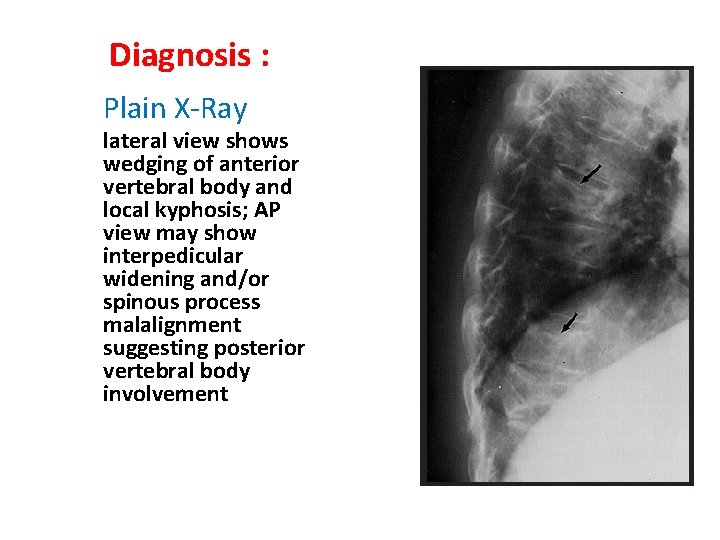
Diagnosis : Plain X-Ray lateral view shows wedging of anterior vertebral body and local kyphosis; AP view may show interpedicular widening and/or spinous process malalignment suggesting posterior vertebral body involvement
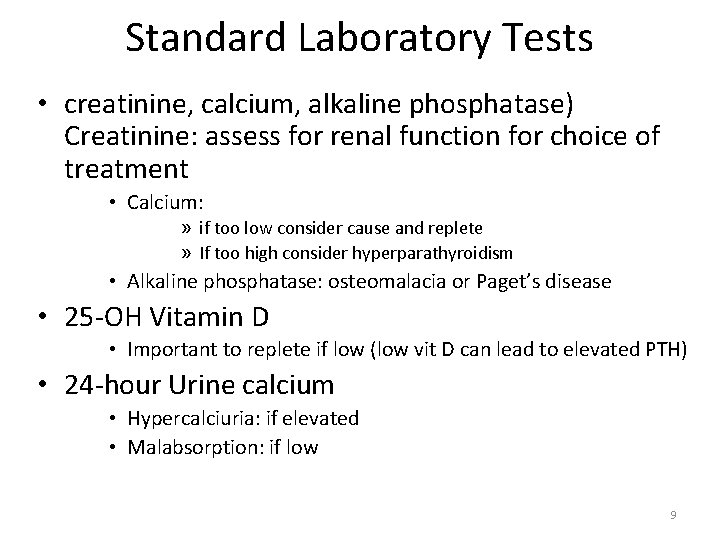
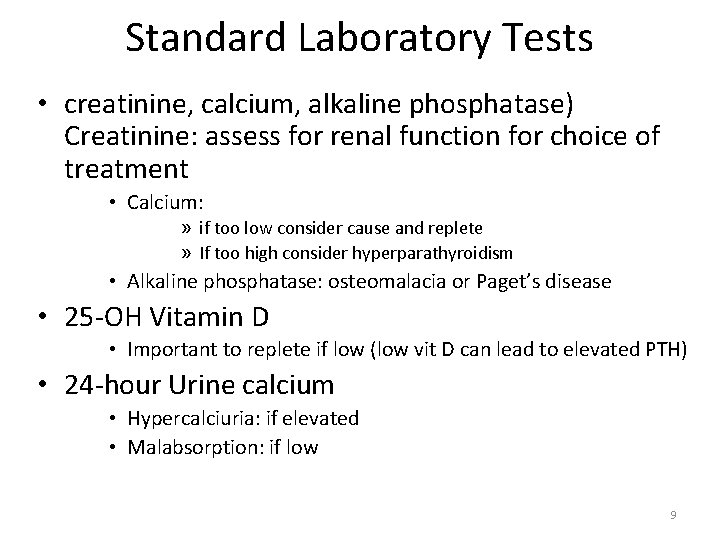
Standard Laboratory Tests • creatinine, calcium, alkaline phosphatase) Creatinine: assess for renal function for choice of treatment • Calcium: » if too low consider cause and replete » If too high consider hyperparathyroidism • Alkaline phosphatase: osteomalacia or Paget’s disease • 25 -OH Vitamin D • Important to replete if low (low vit D can lead to elevated PTH) • 24 -hour Urine calcium • Hypercalciuria: if elevated • Malabsorption: if low 9
Additional Laboratory Tests • PTH (with calcium) • If calcium is elevated • If considering using teriperatide (Forteo) • Patients with ESRD • Testosterone • In men with osteoporosis • 24 hour urine cortisol • In patients with cushingoid features and unexpected osteoporosis 10
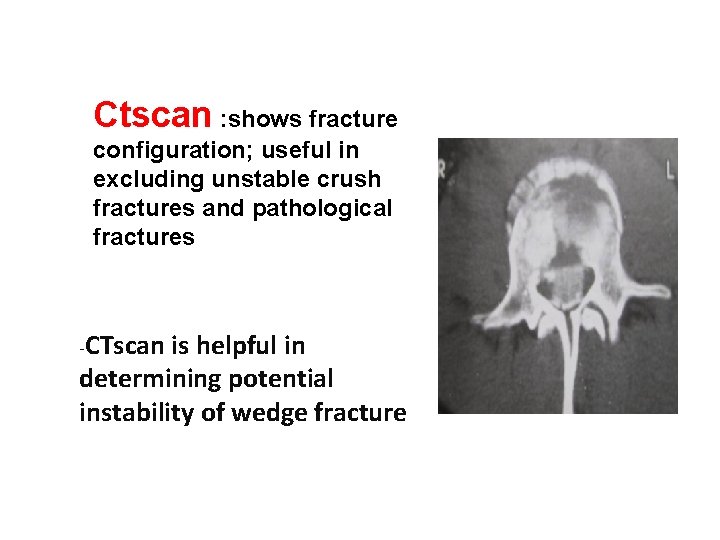
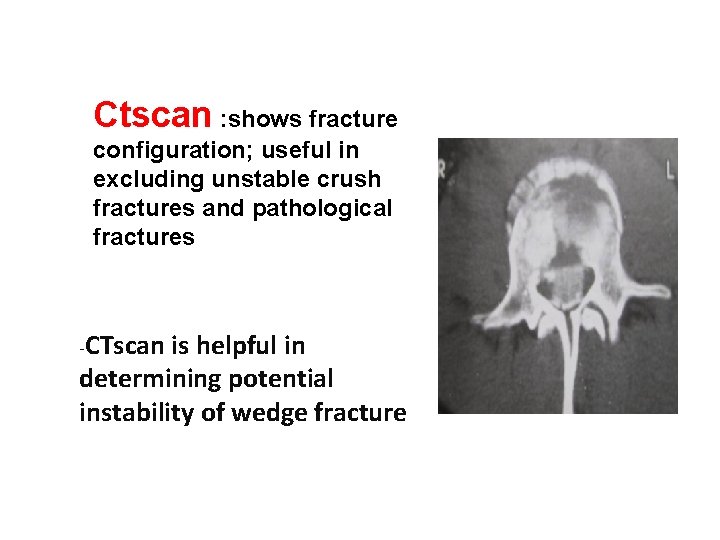
Ctscan : shows fracture configuration; useful in excluding unstable crush fractures and pathological fractures -CTscan is helpful in determining potential instability of wedge fracture

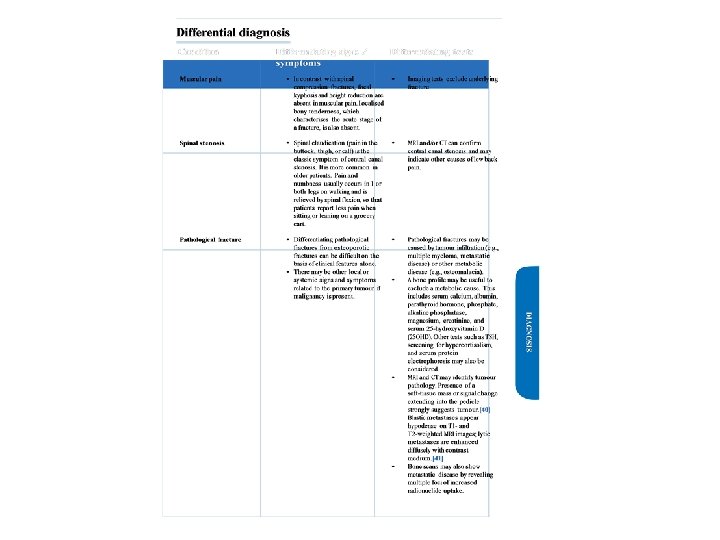
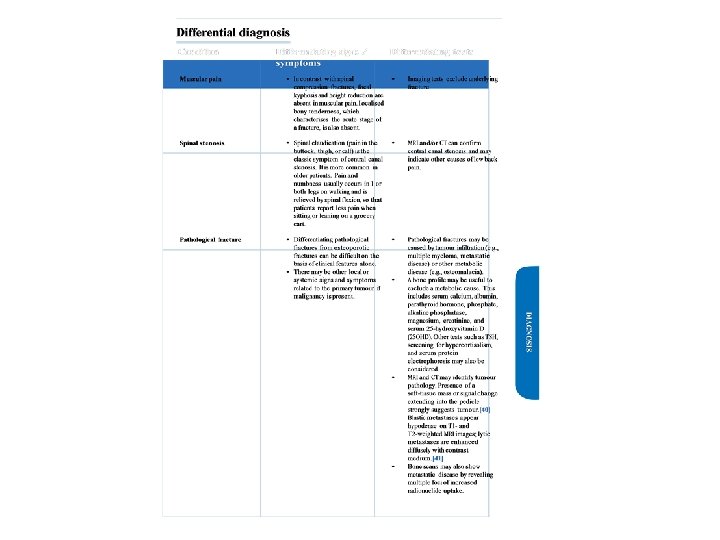
-confirm diagnosis : -certain clues and more than investigation: MRI and CTSCan considered when further diagnostic information is indicated by result of XR and lab test -OVCF in not older patient(<55 yrs malignancy) -OVCF in higher than T 4 is unusual -febrile patient and weightloss and sweeting ….
Pathologic vertebral fracure: - 0 steoporotic VCF - metastatic VCF - another VCF Metastatic VCF treatment: (Palliative Tx) Radiotherapy : - radiosensentive (high: lymphoma, myeloma, seminoma- moderate: Breast, prostate CA) - can not tolerate surgery -poor survival prognosis ( < 3 month) - no cord compression - no acute or progressive neurologic deterioration - pain and neurologic improvement in 70% patient -If surgery is need , optimally radiotherapy perform after surgical stabilization due to decrease of radiotherapy complication. (infection , wound dehiscence). - Medication for pain control.
our managment in OVCF: short term treatment (pain control, activity modification…) long term treatment ( underlying osteoporosis) -- early treatment composed non operative +radiographic follow up --surgical treatment in unstable Fx - incapaciating pain-significant deformityneurologic involvmennt
§First line therapy for relief of acute pain due to VCF is oral analgesic. § The choice of initial agent depend on the severity of the pain. § Acetaminaphon 2 gr, ibuprofen 400 qid, naproxen 500 bd are sufficient for mild pain §Moderate pain is not response to oral analgesic § Opioids(tramadol, tapandadol) and/or calcitonin are options that inadequte analgesia or pain is moderate. §sever pain is acute pain(0 -4 week)from VCF require oral opioids at the outset §. If pain is sever or incapacitating , hospital admission parenteral opioids for 3 to 7 days and then convert to oral formulation and discharge
Nasal calcitonin: • indication is mild to moderate pain is not response to oral analgesia • is not a first line agent because more expesive than NSAIDS. • Use in acute phase is only antipain effect. • is not fist line agent for treatment of osteoporosis. • dose is 200 unit (one spary) daily for 2 -4 weeks • nasal calcitonin is more effective intramuscular preperation. • Only used until the pain is better (not longer than 6 months)
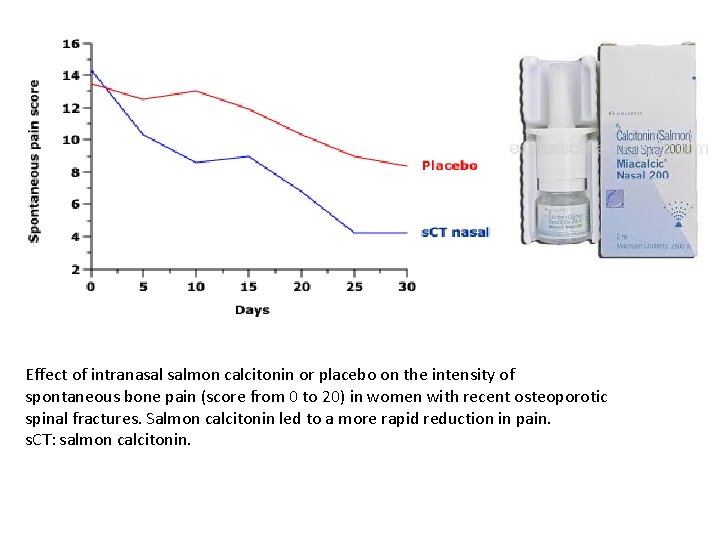
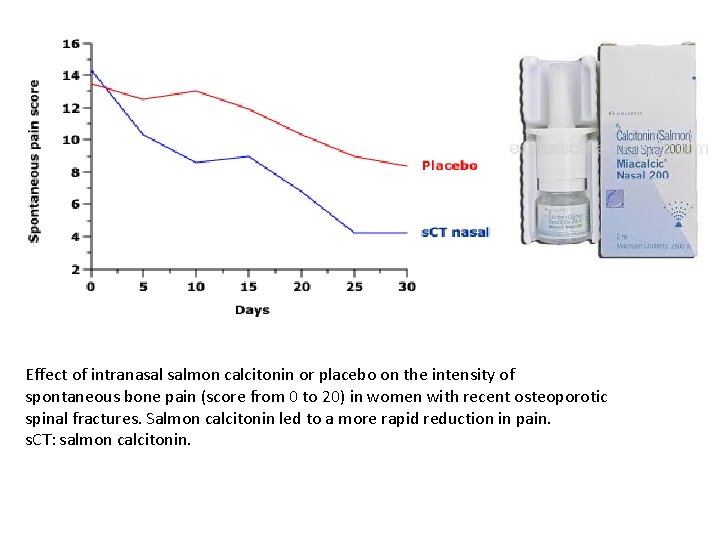
Effect of intranasal salmon calcitonin or placebo on the intensity of spontaneous bone pain (score from 0 to 20) in women with recent osteoporotic spinal fractures. Salmon calcitonin led to a more rapid reduction in pain. s. CT: salmon calcitonin.
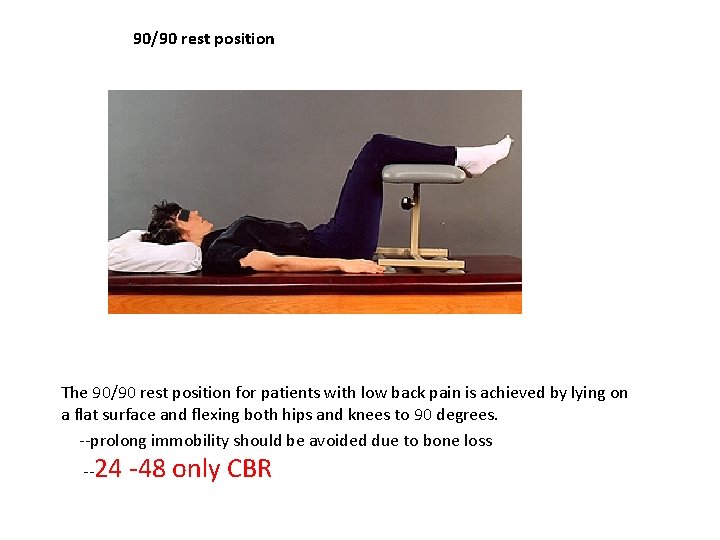
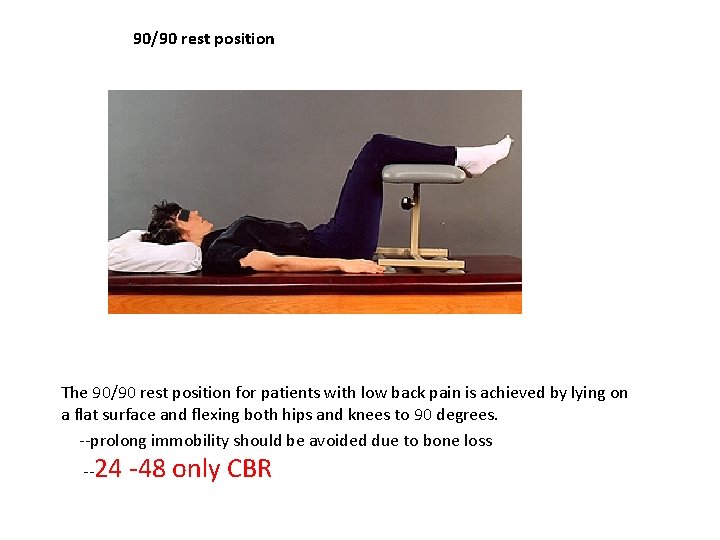
90/90 rest position The 90/90 rest position for patients with low back pain is achieved by lying on a flat surface and flexing both hips and knees to 90 degrees. --prolong immobility should be avoided due to bone loss --24 -48 only CBR
Walking aids : After short period of bed rest mobilization encourged walking aids help compensate for loss of sagittal balance and impaired proprioception -decrease fall risk
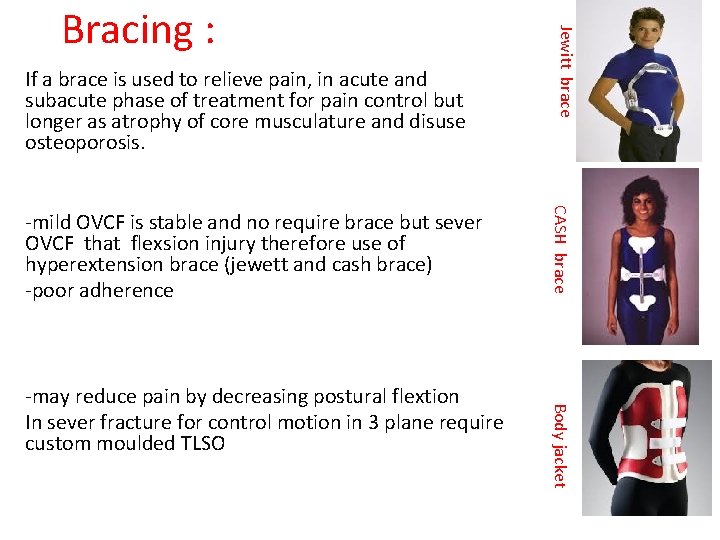
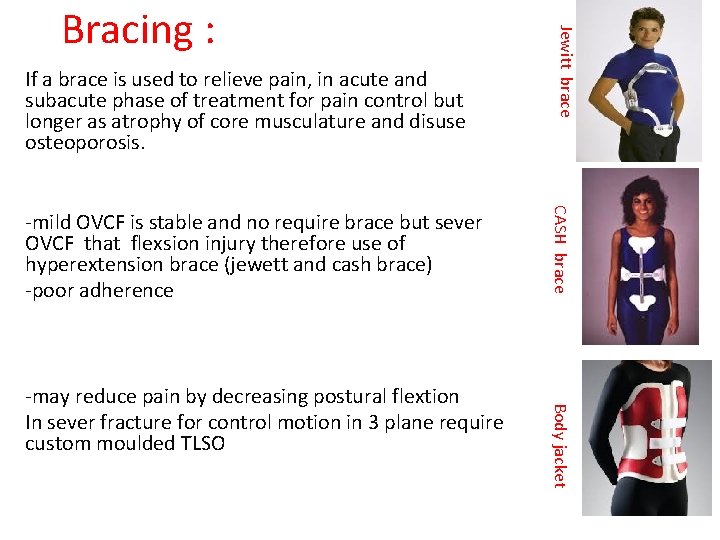
If a brace is used to relieve pain, in acute and subacute phase of treatment for pain control but longer as atrophy of core musculature and disuse osteoporosis. Body jacket -may reduce pain by decreasing postural flextion In sever fracture for control motion in 3 plane require custom moulded TLSO CASH brace -mild OVCF is stable and no require brace but sever OVCF that flexsion injury therefore use of hyperextension brace (jewett and cash brace) -poor adherence Jewitt brace Bracing :
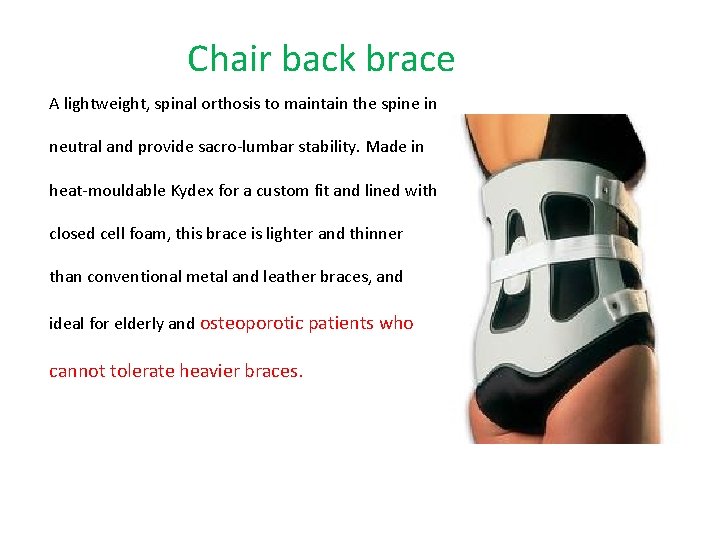
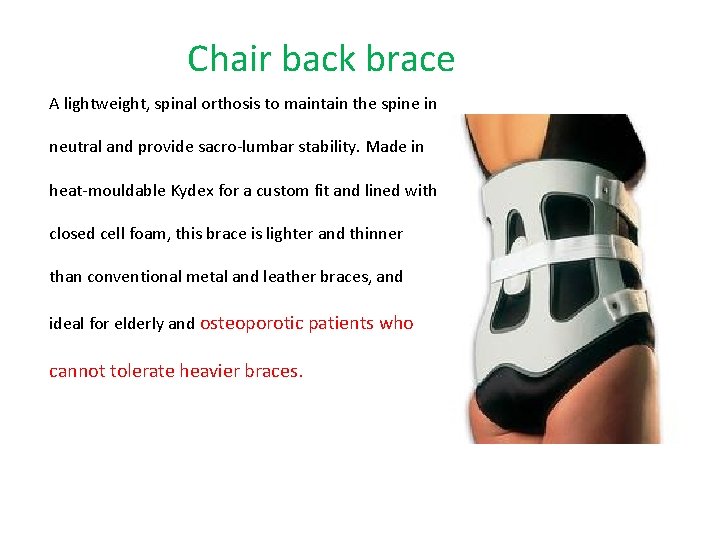
Chair back brace A lightweight, spinal orthosis to maintain the spine in neutral and provide sacro-lumbar stability. Made in heat-mouldable Kydex for a custom fit and lined with closed cell foam, this brace is lighter and thinner than conventional metal and leather braces, and ideal for elderly and osteoporotic patients who cannot tolerate heavier braces.
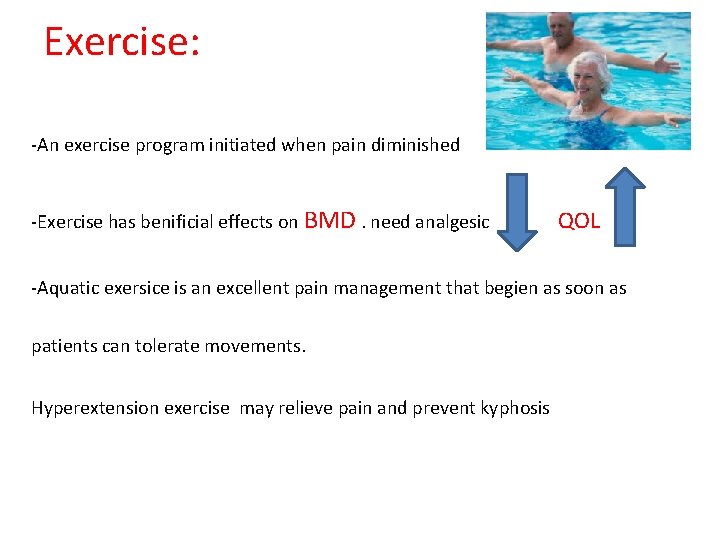
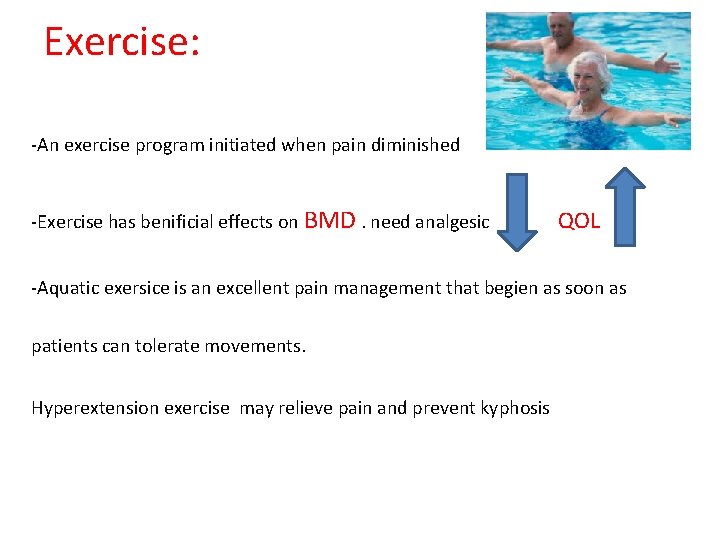
Exercise: -An exercise program initiated when pain diminished -Exercise has benificial effects on BMD. need analgesic QOL -Aquatic exersice is an excellent pain management that begien as soon as patients can tolerate movements. Hyperextension exercise may relieve pain and prevent kyphosis
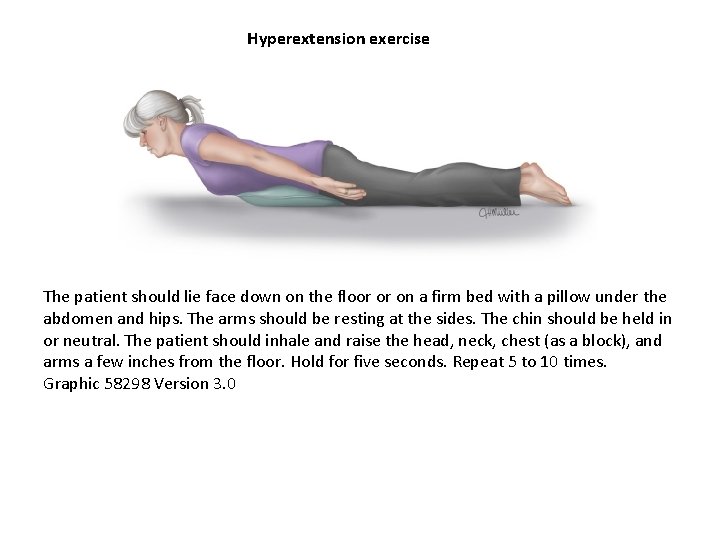
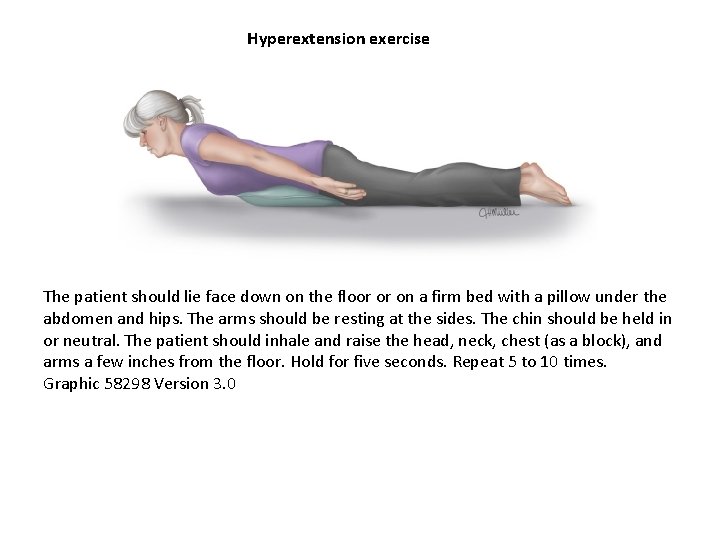
Hyperextension exercise The patient should lie face down on the floor or on a firm bed with a pillow under the abdomen and hips. The arms should be resting at the sides. The chin should be held in or neutral. The patient should inhale and raise the head, neck, chest (as a block), and arms a few inches from the floor. Hold for five seconds. Repeat 5 to 10 times. Graphic 58298 Version 3. 0
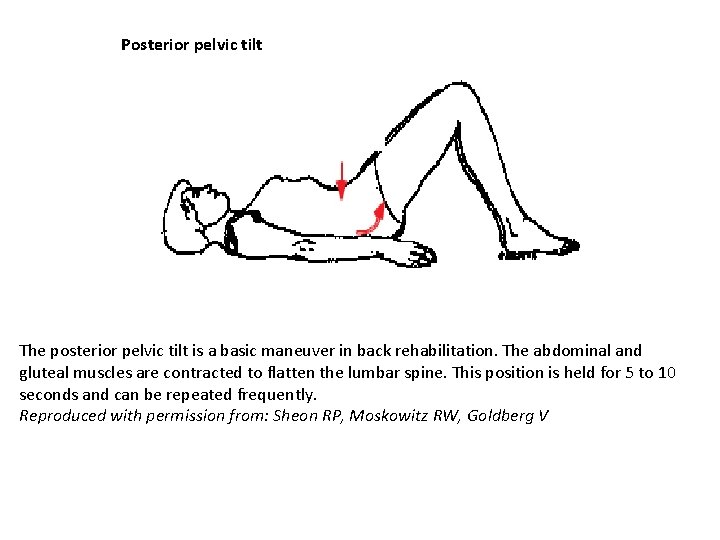
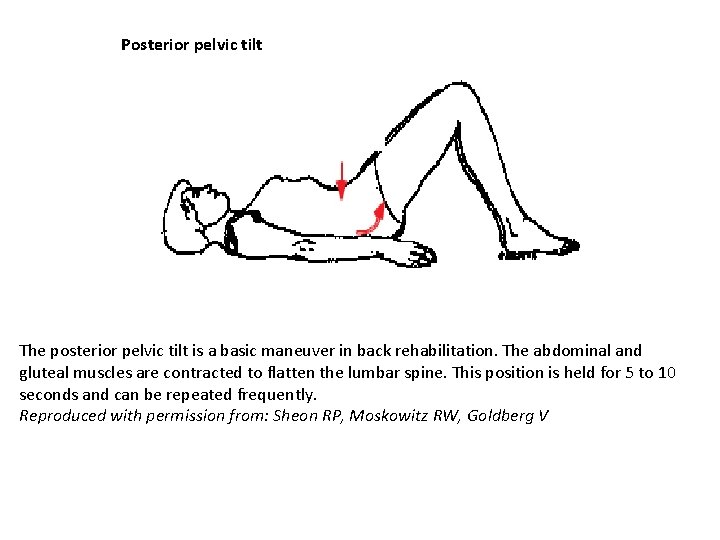
Posterior pelvic tilt The posterior pelvic tilt is a basic maneuver in back rehabilitation. The abdominal and gluteal muscles are contracted to flatten the lumbar spine. This position is held for 5 to 10 seconds and can be repeated frequently. Reproduced with permission from: Sheon RP, Moskowitz RW, Goldberg V
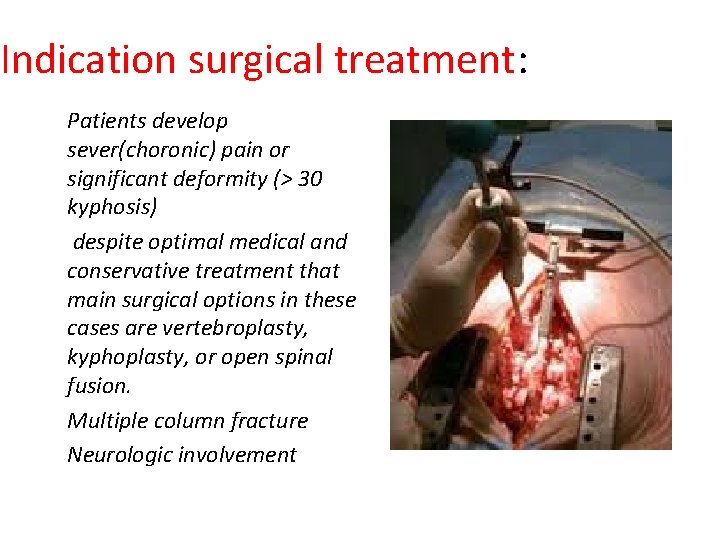
Indication surgical treatment: Patients develop sever(choronic) pain or significant deformity (> 30 kyphosis) despite optimal medical and conservative treatment that main surgical options in these cases are vertebroplasty, kyphoplasty, or open spinal fusion. Multiple column fracture Neurologic involvement
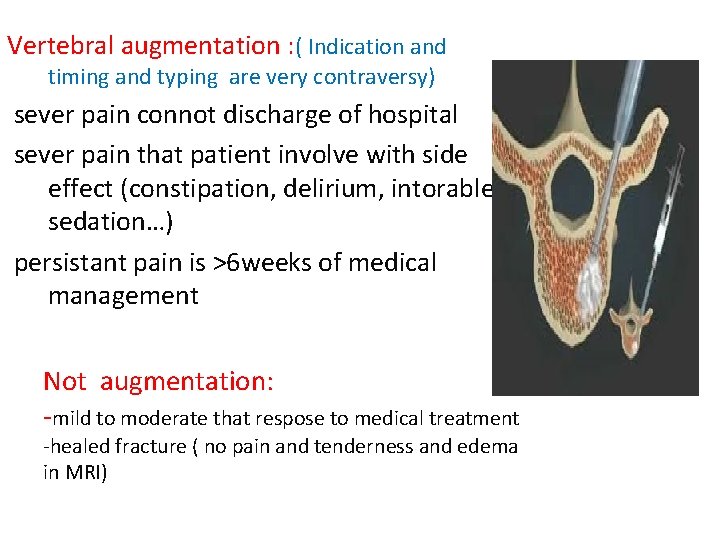
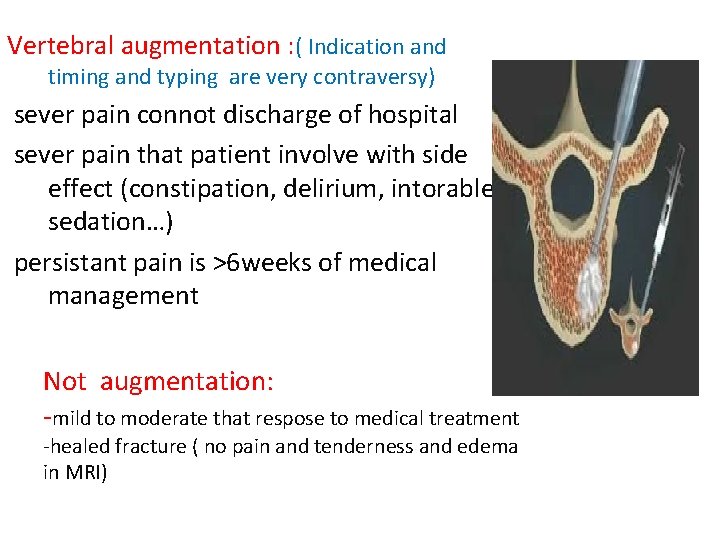
Vertebral augmentation : ( Indication and timing and typing are very contraversy) sever pain connot discharge of hospital sever pain that patient involve with side effect (constipation, delirium, intorable sedation…) persistant pain is >6 weeks of medical management Not augmentation: -mild to moderate that respose to medical treatment -healed fracture ( no pain and tenderness and edema in MRI)
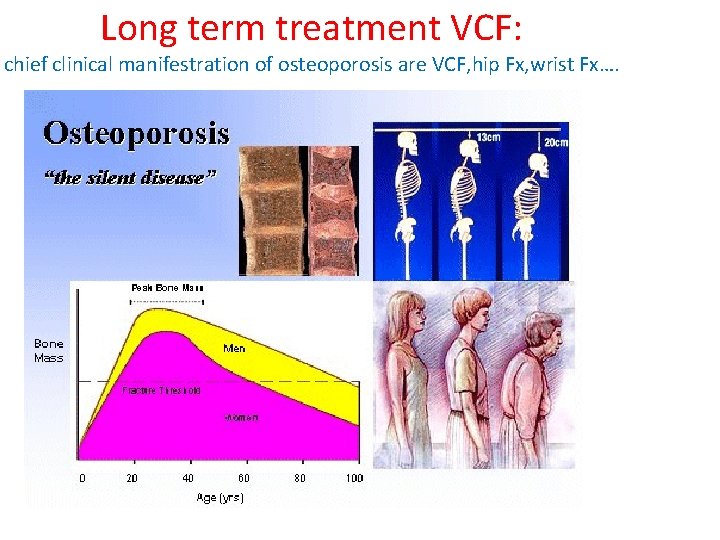
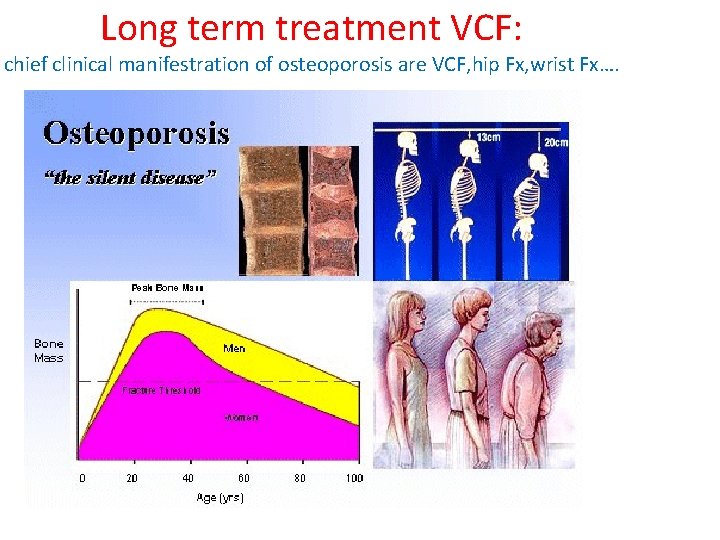
Long term treatment VCF: chief clinical manifestration of osteoporosis are VCF, hip Fx, wrist Fx….
Failure To Diagnose and Treat • Studies show failure to diagnosis and treat osteoporosis in older patients who have suffered a fracture • In study of 4 Midwestern health systems: – 1/8 – 1/4 of hip fracture pts received BMD testing – < ¼ were given calcium/D supplements – < 1/10 treated with antiresorptive medications US Department of Health and Human Services: Bone Health and Osteoporosis: A Report of the Surgeon General, Office of the Surgeon General, 2004.
Lab tests : usually is normal BUT? ? ? initial evaluation with lab tests to diagnose secondry causes : ( CBC , ca, ph , Alb , total protein , cr , LFT ( Alkp , ESR ) , 25 -hydroxy vitamin D, in men serum testestrone) if there is abnormality , we require additional lab tests
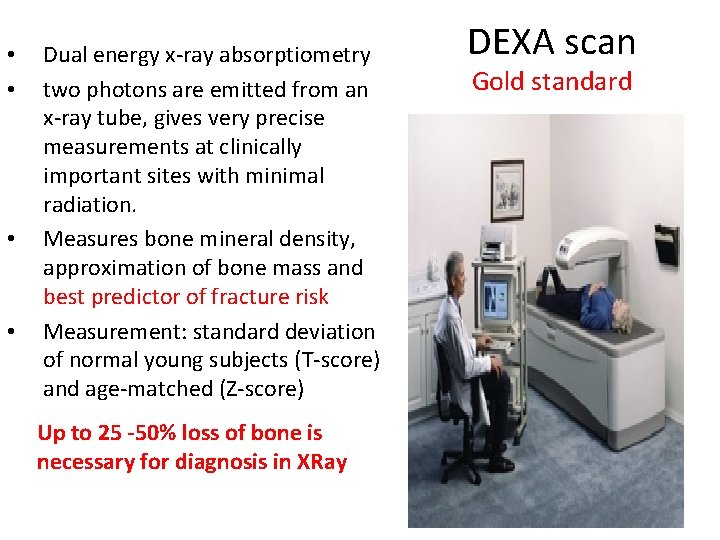
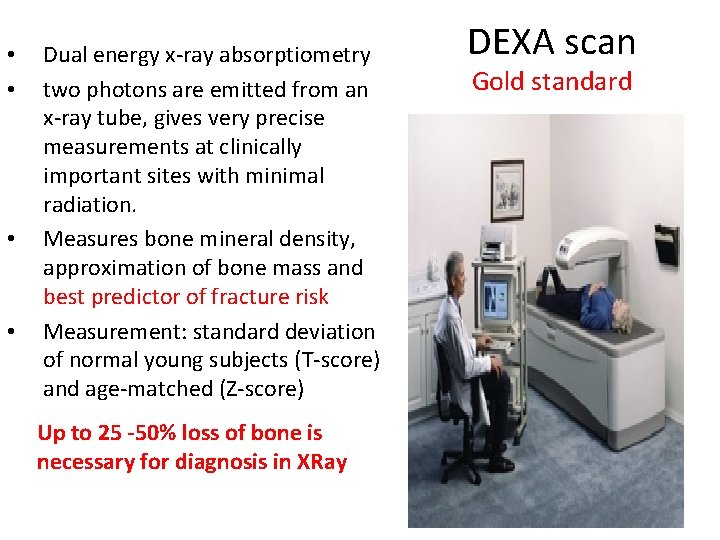
• • Dual energy x-ray absorptiometry two photons are emitted from an x-ray tube, gives very precise measurements at clinically important sites with minimal radiation. Measures bone mineral density, approximation of bone mass and best predictor of fracture risk Measurement: standard deviation of normal young subjects (T-score) and age-matched (Z-score) DEXA scan Gold standard Up to 25 -50% loss of bone is necessary for diagnosis in XRay 33
DEXA scan: uses • To detect those at risk for bone fracture (those with low bone density) • To confirm diagnosis of osteoporosis in those with fracture • To determine rate of bone loss • To determine response to therapy • Prior to spine surgery in old patient 34

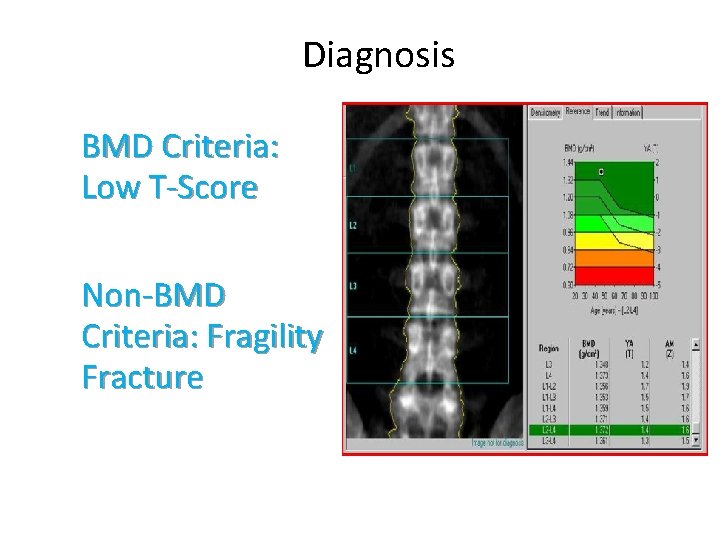
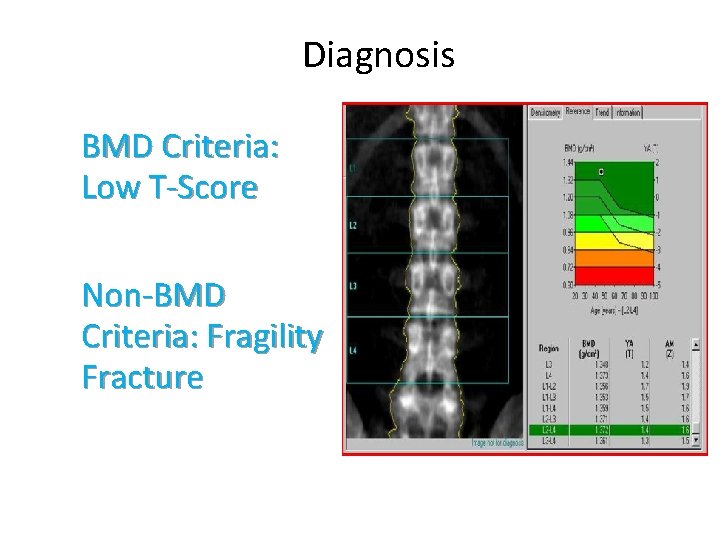
Diagnosis BMD Criteria: Low T-Score Non-BMD Criteria: Fragility Fracture
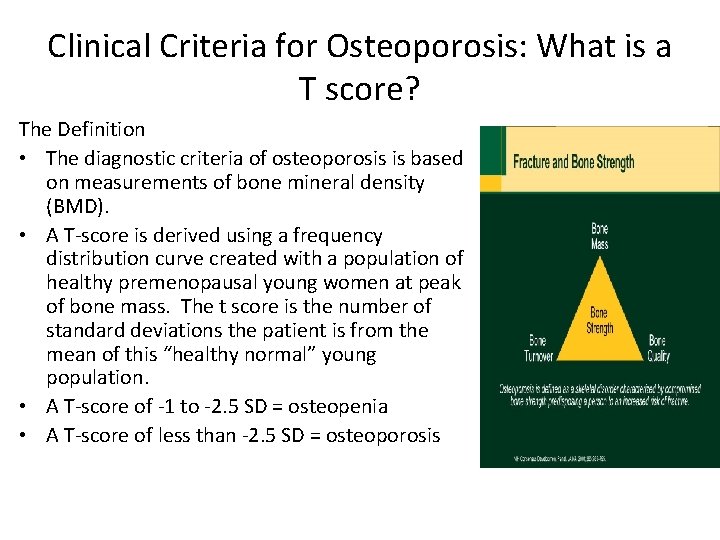
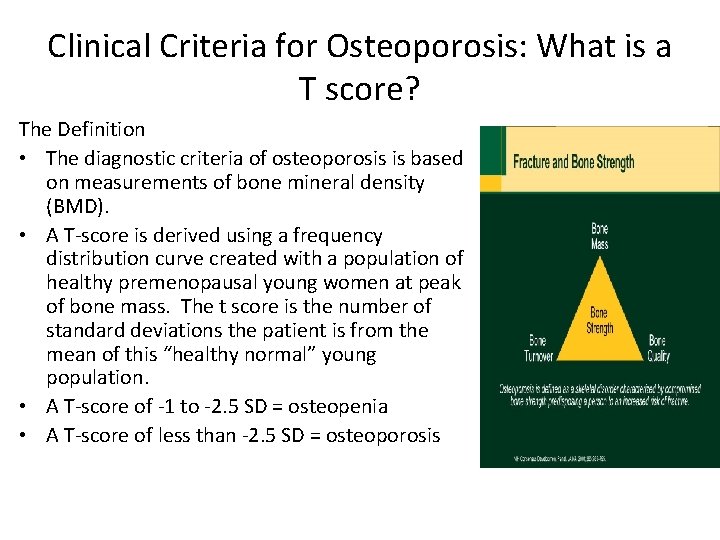
Clinical Criteria for Osteoporosis: What is a T score? The Definition • The diagnostic criteria of osteoporosis is based on measurements of bone mineral density (BMD). • A T-score is derived using a frequency distribution curve created with a population of healthy premenopausal young women at peak of bone mass. The t score is the number of standard deviations the patient is from the mean of this “healthy normal” young population. • A T-score of -1 to -2. 5 SD = osteopenia • A T-score of less than -2. 5 SD = osteoporosis
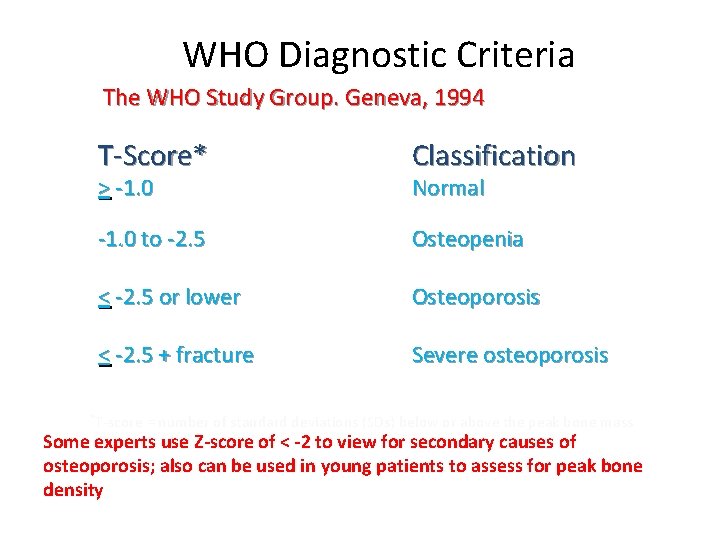
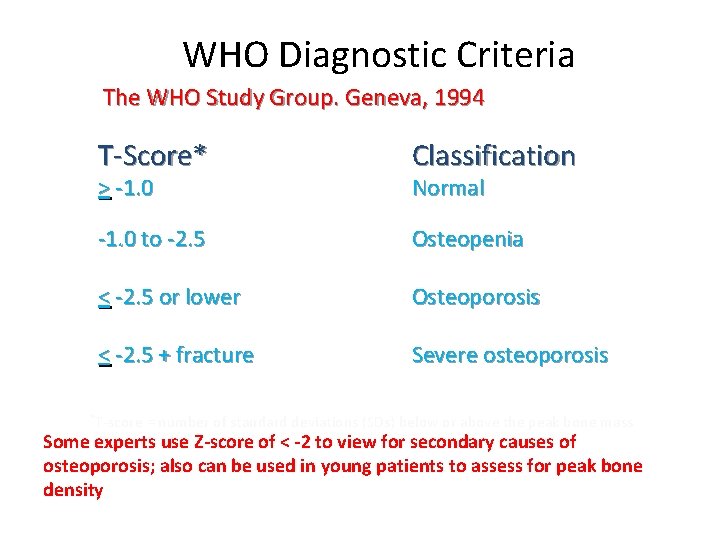
WHO Diagnostic Criteria The WHO Study Group. Geneva, 1994 T-Score* Classification -1. 0 to -2. 5 Osteopenia < -2. 5 or lower Osteoporosis < -2. 5 + fracture Severe osteoporosis > -1. 0 Normal *T-score = number of standard deviations (SDs) below or above the peak bone mass in young adults. Some experts use Z-score of < -2 to view for secondary causes of osteoporosis; also can be used in young patients to assess for peak bone density
§-causes for secodery osteoporosis : osteomalecia Hyperthyroidism, hyperparathyroidism granolomatous desease hematologic desease infectious disease metastatic cancer scheuermann disease hypogonadism malabsorption hypercalciuria
first treatment is prevention : • Adequate nutrition, particularly calcium and vitamin D • Calcium: 1000 – 1200 mg daily (diet plus supplementation) • Vitamin D: goal level of around 30 -50 (most 1000 units daily) • Weight bearing exercise • Discourage smoking • Discourage alcohol abuse • Reduction of risks for falling: consider OT evaluation for home hazards, minimize sedating medications. • decrease caffeine intake • Sunlight exposure • excersice 40

Risk factor: Older age >50 in woman -65 in men Previous OVCF Low body weight Low bone mass Smoking White or asian race Post menopause Alchol Corticosteroid use Hyperthiroidism Vit D deficiency Renal disease Liver dsisease RA and autoimmiune connective disease

Pharmacological therapy : Decrease Resorption ► Bisphonates ► Estrogen ► Raloxifene Calcitonin Enhance Formation ► Parathyroid Hormone ► ► Anderogens
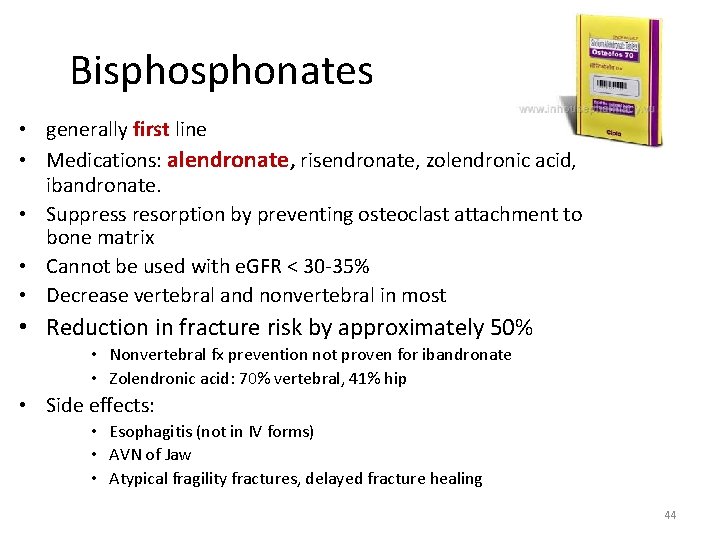
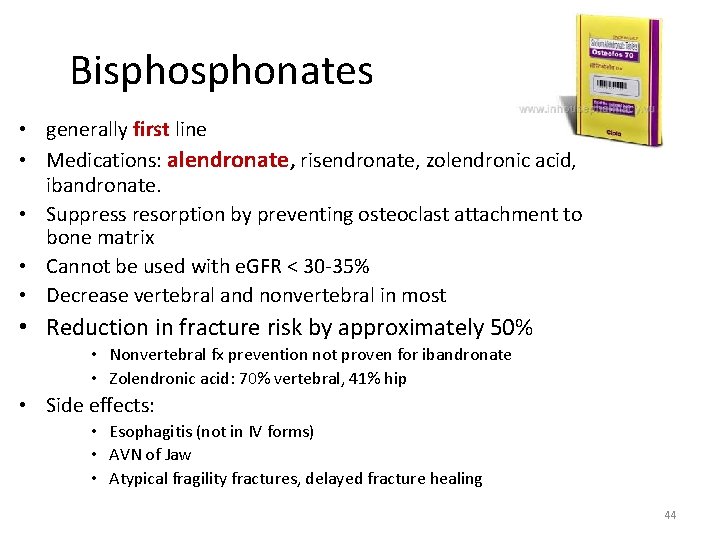
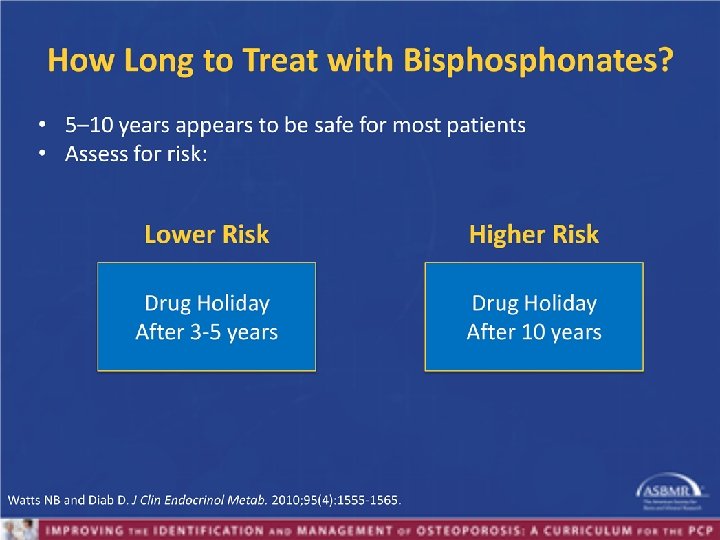
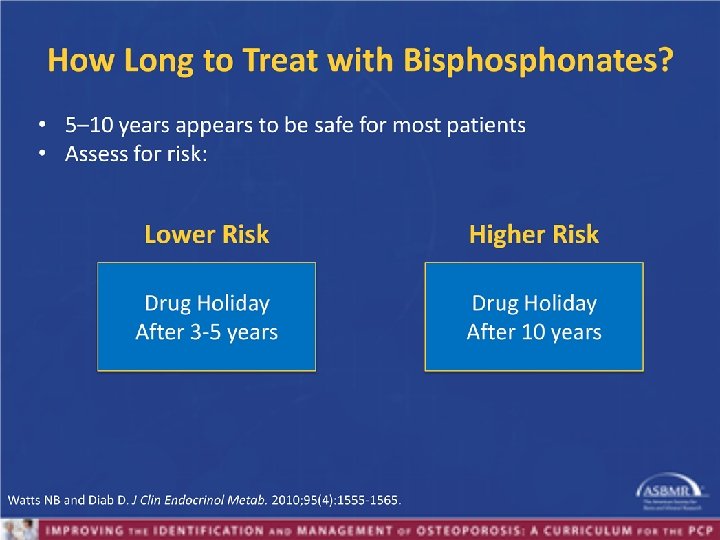
Bisphonates • generally first line • Medications: alendronate, risendronate, zolendronic acid, ibandronate. • Suppress resorption by preventing osteoclast attachment to bone matrix • Cannot be used with e. GFR < 30 -35% • Decrease vertebral and nonvertebral in most • Reduction in fracture risk by approximately 50% • Nonvertebral fx prevention not proven for ibandronate • Zolendronic acid: 70% vertebral, 41% hip • Side effects: • Esophagitis (not in IV forms) • AVN of Jaw • Atypical fragility fractures, delayed fracture healing 44
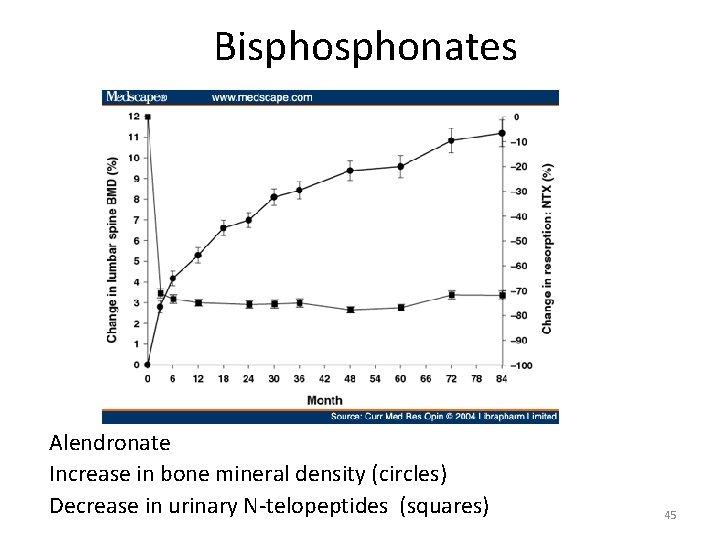
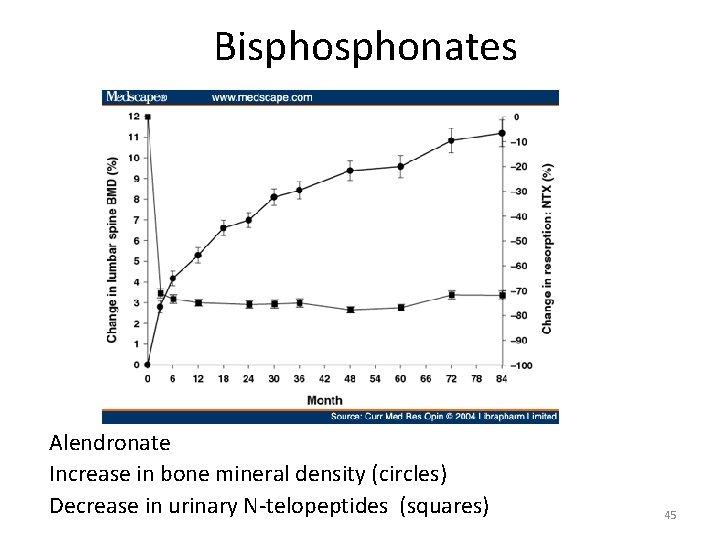
Bisphonates Alendronate Increase in bone mineral density (circles) Decrease in urinary N-telopeptides (squares) 45
Teriparitide (Forteo) Stimulates bone remodeling by increasing bone formation. Moderate to severe osteoporosis: �Reduction of fractures: � Vertebral : 65% � Nonvertebral 53% �High doses in rats caused osteosarcoma but no cases of osteosarcoma seen in >200, 000 patients who received the drug �Should not be given for more than 2 years �Side effects: mild hypercalcemia (10. 5 -11) �Expensive and subcutaneous administration. �Should not be given to patients with: � Hypercalcemia � Multiple Myeloma, bone mets, skeletal tumor �Children/teenagers with growing bones 46

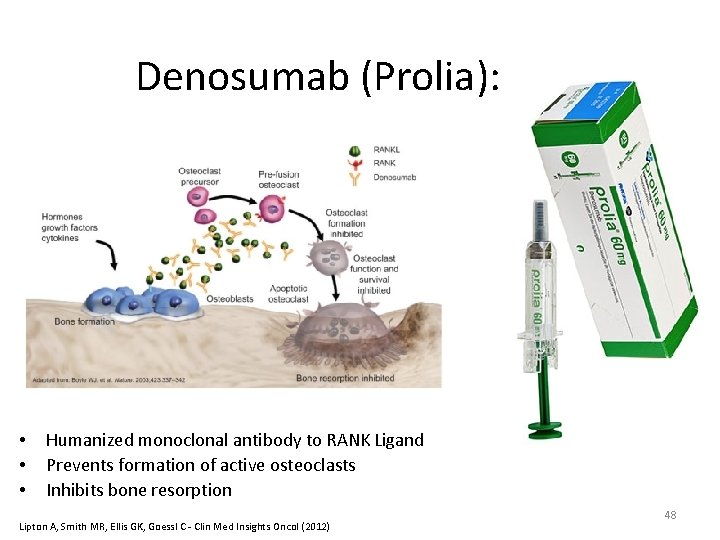
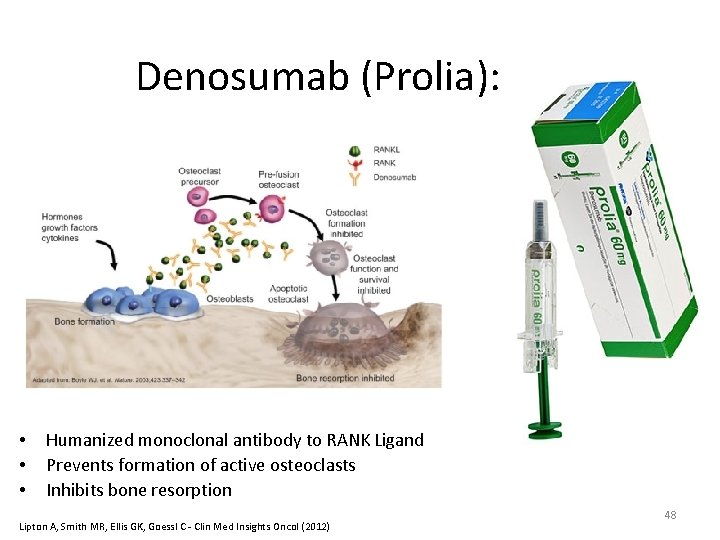
Denosumab (Prolia): • • • Humanized monoclonal antibody to RANK Ligand Prevents formation of active osteoclasts Inhibits bone resorption Lipton A, Smith MR, Ellis GK, Goessl C - Clin Med Insights Oncol (2012) 48

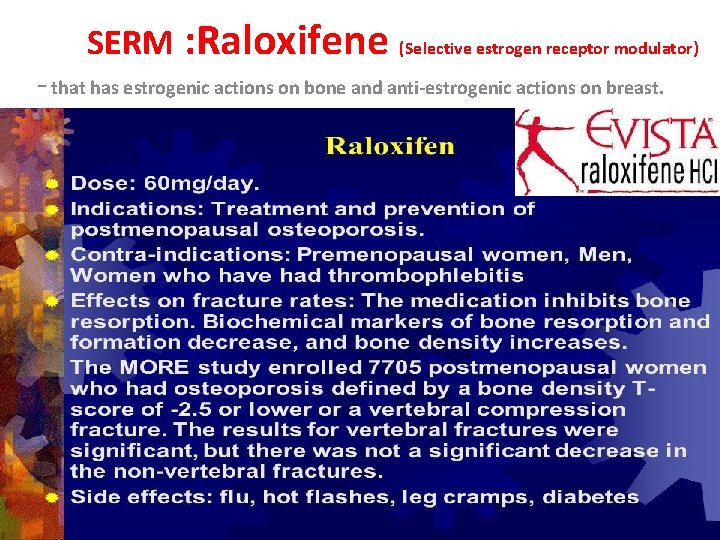
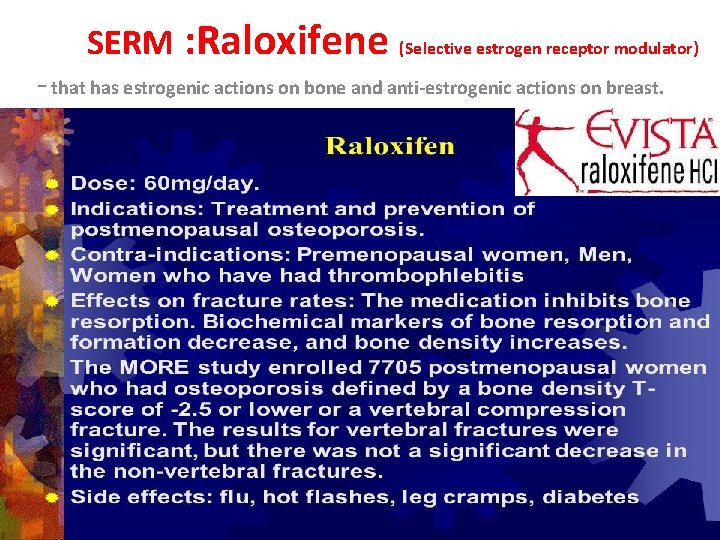
SERM : Raloxifene (Selective estrogen receptor modulator) - that has estrogenic actions on bone and anti-estrogenic actions on breast.
Hormone Replacement Therapy: rise and fall • Estrogens +/- progesterones • HRT was once considered to be the primary therapy of osteoporosis prevention/treatment • Blocks cytokine signaling to the osteoclast • Women’s Health Initiative trial: 34% reduction of hip fracture and vertebral fractures, but increased risk for breast cancer, cardiovascular disease, thrombosis… • Currently, HRT is not used to treat or prevent osteoporosis alone (often used for other indications such as severe postmenopausal symptoms. 51
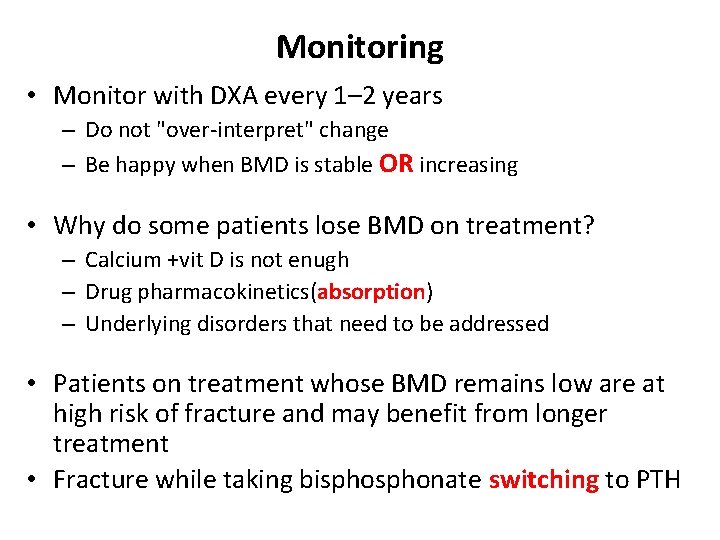
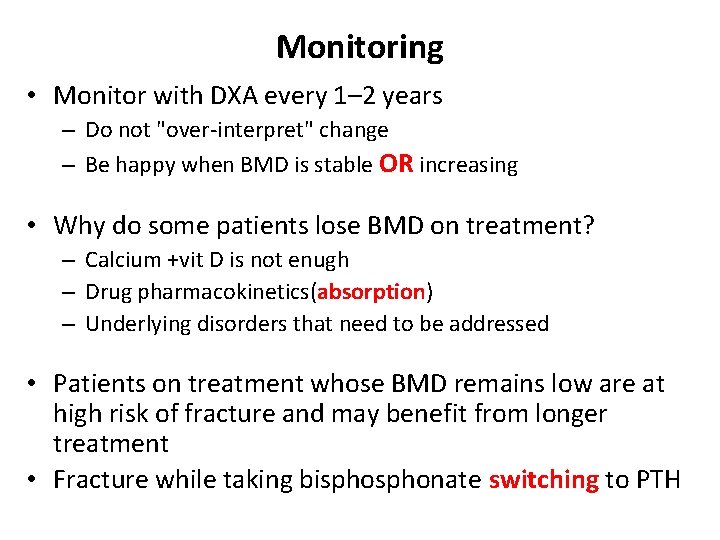
Monitoring • Monitor with DXA every 1– 2 years – Do not "over-interpret" change – Be happy when BMD is stable OR increasing • Why do some patients lose BMD on treatment? – Calcium +vit D is not enugh – Drug pharmacokinetics(absorption) – Underlying disorders that need to be addressed • Patients on treatment whose BMD remains low are at high risk of fracture and may benefit from longer treatment • Fracture while taking bisphonate switching to PTH
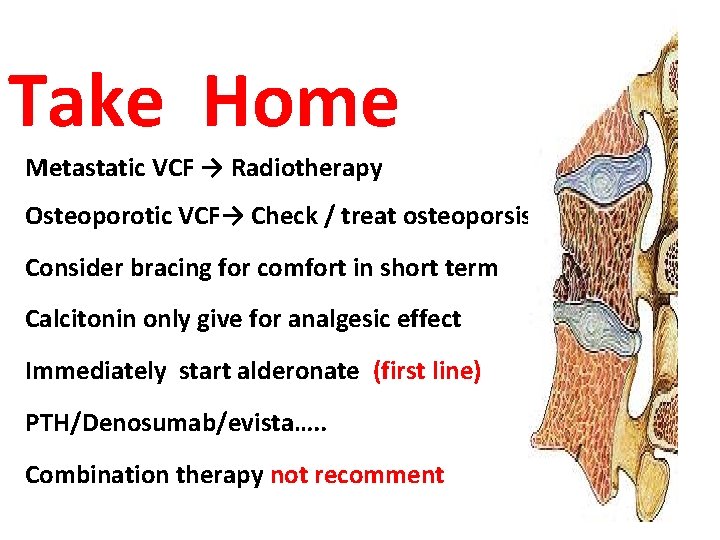
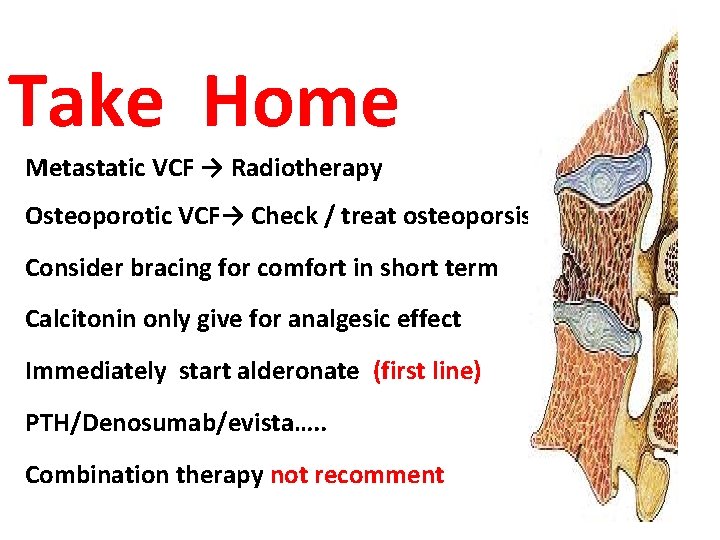
Take Home Metastatic VCF → Radiotherapy Osteoporotic VCF→ Check / treat osteoporsis Consider bracing for comfort in short term Calcitonin only give for analgesic effect Immediately start alderonate (first line) PTH/Denosumab/evista…. . Combination therapy not recomment
World Osteoporosis Day • 20 october

T T R A TH O F U O Y K AN N O I T N E