Pain Management Role of GPs in Pain Management

- Slides: 25

Pain Management
Role of GPs in Pain Management GPs can: • improve assessment and treatment of pain • offer early intervention and treatment • prevent chronic pain. Pain Management
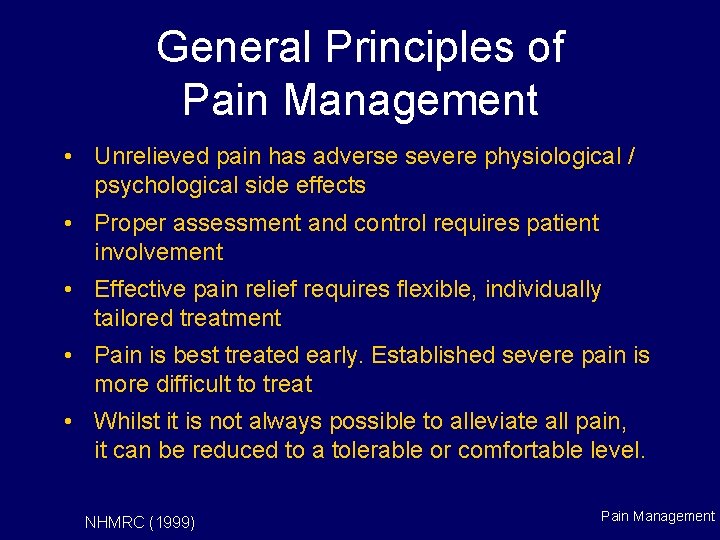
General Principles of Pain Management • Unrelieved pain has adverse severe physiological / psychological side effects • Proper assessment and control requires patient involvement • Effective pain relief requires flexible, individually tailored treatment • Pain is best treated early. Established severe pain is more difficult to treat • Whilst it is not always possible to alleviate all pain, it can be reduced to a tolerable or comfortable level. NHMRC (1999) Pain Management
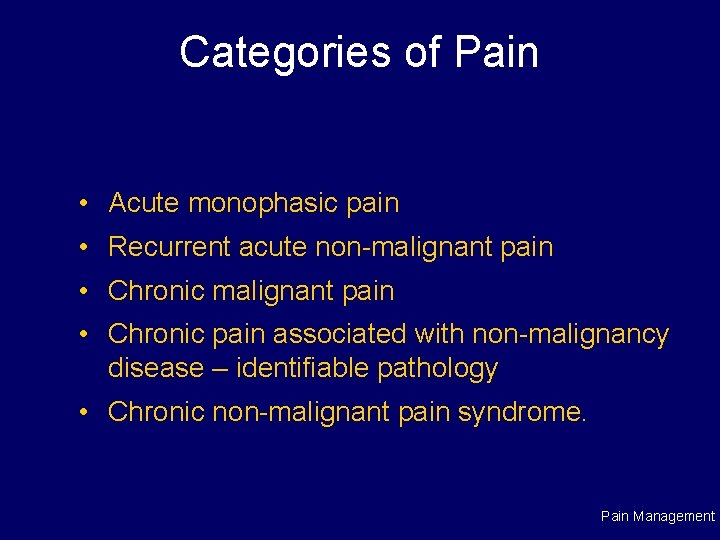
Categories of Pain • Acute monophasic pain • Recurrent acute non-malignant pain • Chronic pain associated with non-malignancy disease – identifiable pathology • Chronic non-malignant pain syndrome. Pain Management
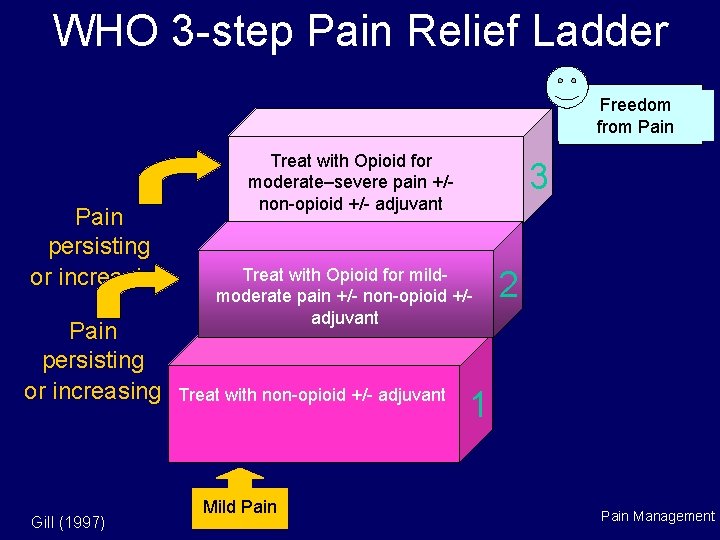
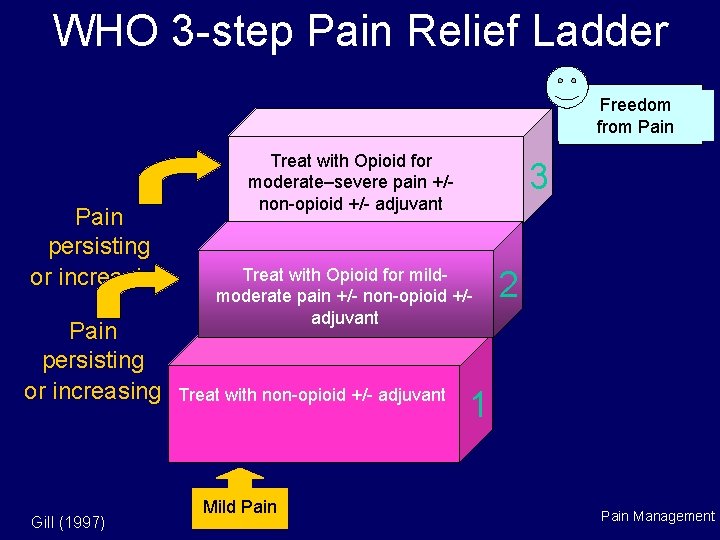
WHO 3 -step Pain Relief Ladder Freedom from Pain persisting or increasing Gill (1997) Treat with Opioid for moderate–severe pain +/non-opioid +/- adjuvant 3 Treat with Opioid for mildmoderate pain +/- non-opioid +/adjuvant Treat with non-opioid +/- adjuvant Mild Pain 2 1 Pain Management
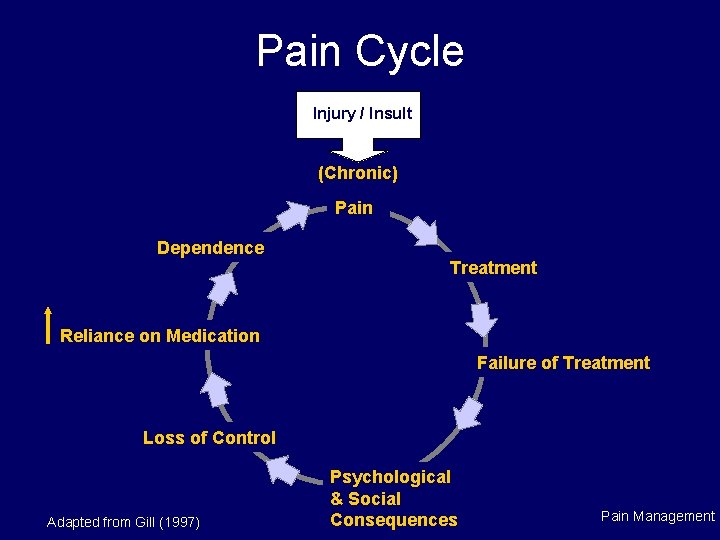
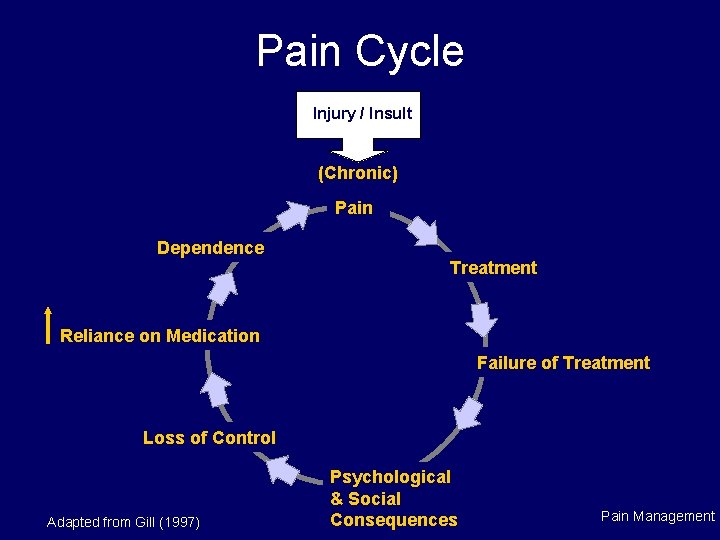
Pain Cycle Injury / Insult (Chronic) Pain Dependence Treatment Reliance on Medication Failure of Treatment Loss of Control Adapted from Gill (1997) Psychological & Social Consequences Pain Management
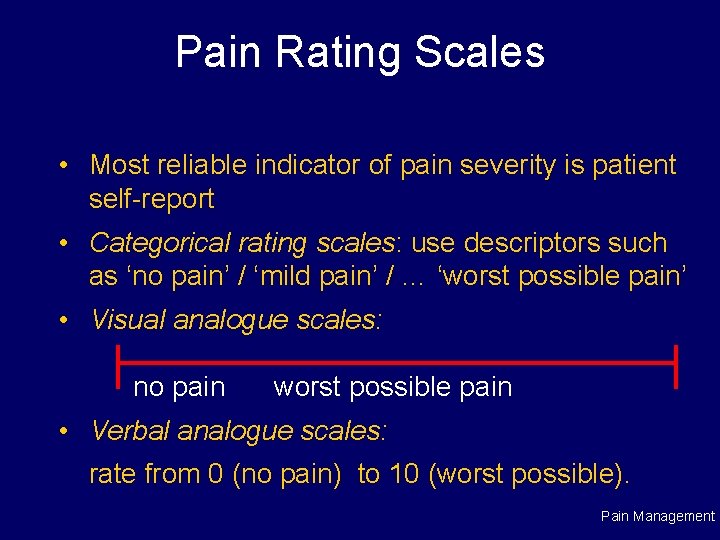
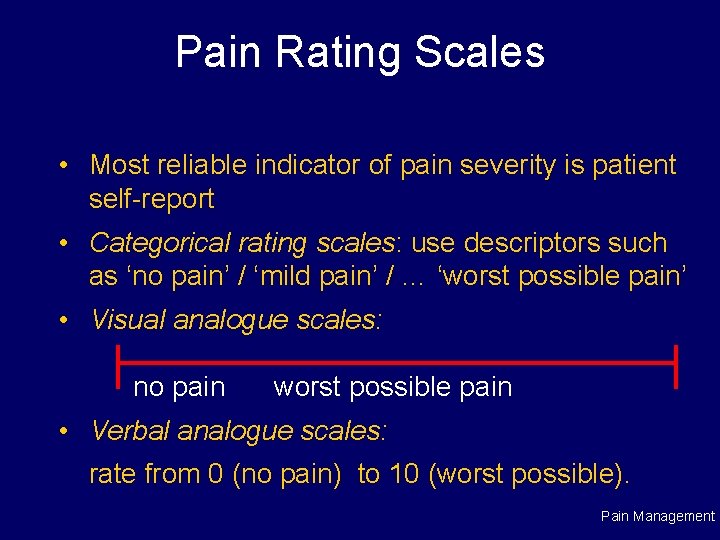
Pain Rating Scales • Most reliable indicator of pain severity is patient self-report • Categorical rating scales: use descriptors such as ‘no pain’ / ‘mild pain’ / … ‘worst possible pain’ • Visual analogue scales: no pain worst possible pain • Verbal analogue scales: rate from 0 (no pain) to 10 (worst possible). Pain Management
The GP–Patient Relationship Successful management depends on: • patient trust & confidence in GP • complete physical and psychosocial history – this is essential so allow adequate time • supportive & clear explanations of the pain issues • ability to discuss strategies openly to reduce potential for ‘self-medicating’ • case management – for consistency in management, commence treatment with consultation between patient and treating staff • trust – avoid placebos at all costs • adequate relief – achieving relief / reducing pain level is paramount. Pain Management
A Shared Care / Team Approach • A team-based, holistic approach tends to be most effective for pain management, involving: – nurses – psychologists & psychiatrists – physiotherapists – pain specialists. Pain Management
Acute Pain Management and High-risk Drug Use Key Principles • Unless patient uses opioids, treat as ‘normal’ patient with pain • ‘First do no harm’ – shortest dose, shortest duration with minimal side effects, with aim to reduce pain to a tolerable level • Maintain clear communication (prevent anxiety, reassure patient) • Do not withhold analgesia unless medically indicated • Avoid Pethidine • Allow adequate time for assessment – impossible in Pain Management 10 minute consultation.
Acute Pain Management: People who Inject Opioids Consider: • tolerance to opioid analgesics – e. g. , if already on regular prescribed opioid medication (iatrogenic dependence), on methadone, opioid-dependent, or regularly taking liver enzyme-inducing drugs • real and perceived legal constraints for prescribers • potential adverse interactions with other CNS depressants • difficulties / misunderstandings which arise in communications between clinicians and patients. Pain Management
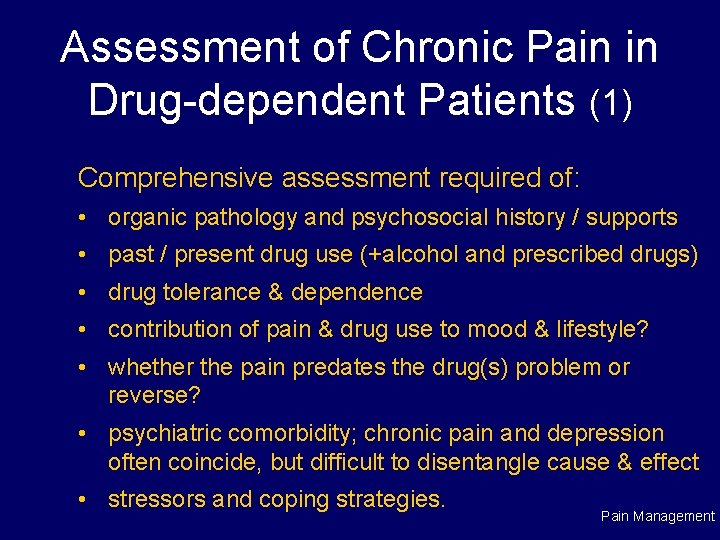
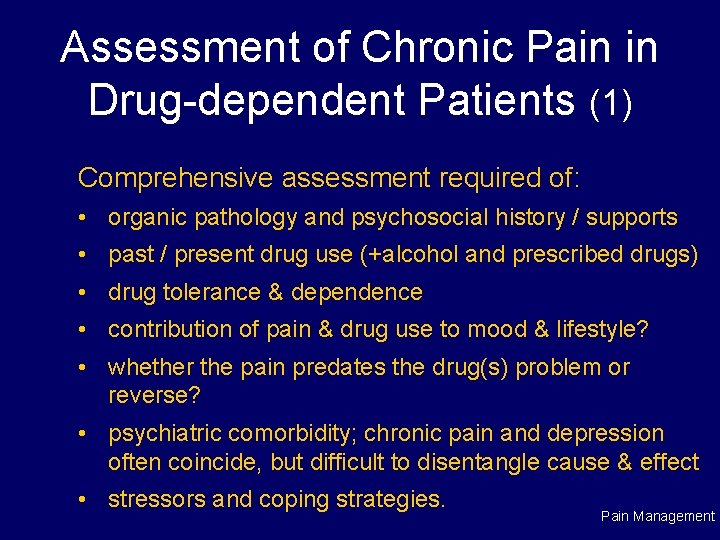
Assessment of Chronic Pain in Drug-dependent Patients (1) Comprehensive assessment required of: • organic pathology and psychosocial history / supports • past / present drug use (+alcohol and prescribed drugs) • drug tolerance & dependence • contribution of pain & drug use to mood & lifestyle? • whether the pain predates the drug(s) problem or reverse? • psychiatric comorbidity; chronic pain and depression often coincide, but difficult to disentangle cause & effect • stressors and coping strategies. Pain Management
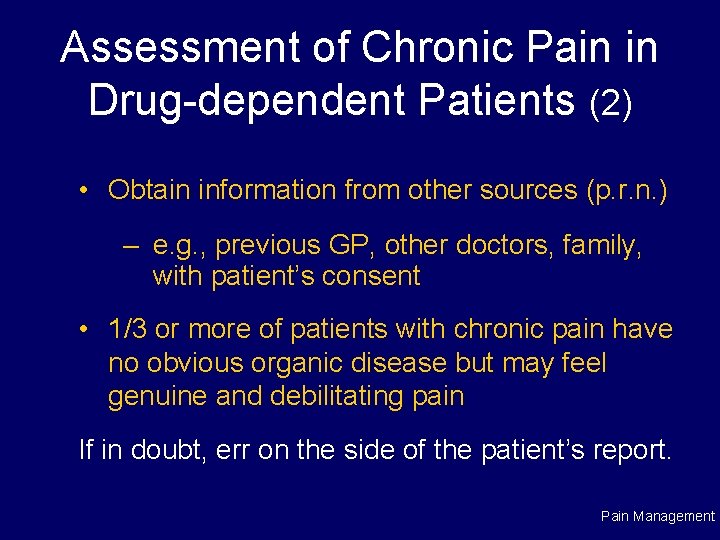
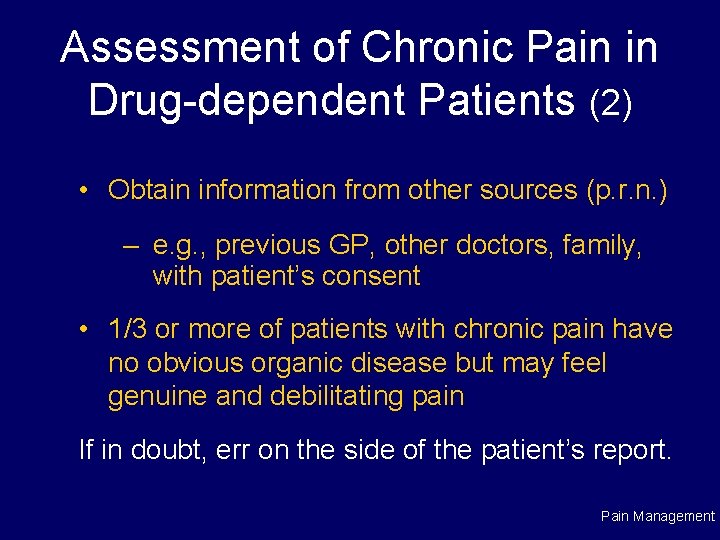
Assessment of Chronic Pain in Drug-dependent Patients (2) • Obtain information from other sources (p. r. n. ) – e. g. , previous GP, other doctors, family, with patient’s consent • 1/3 or more of patients with chronic pain have no obvious organic disease but may feel genuine and debilitating pain If in doubt, err on the side of the patient’s report. Pain Management
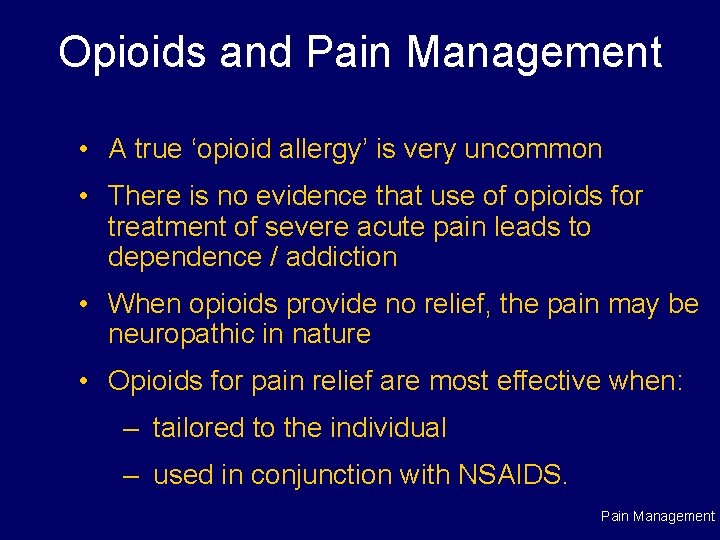
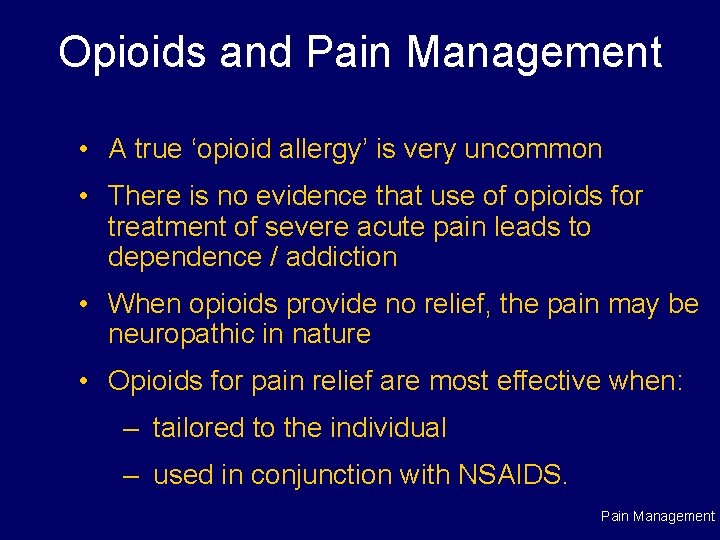
Opioids and Pain Management • A true ‘opioid allergy’ is very uncommon • There is no evidence that use of opioids for treatment of severe acute pain leads to dependence / addiction • When opioids provide no relief, the pain may be neuropathic in nature • Opioids for pain relief are most effective when: – tailored to the individual – used in conjunction with NSAIDS. Pain Management
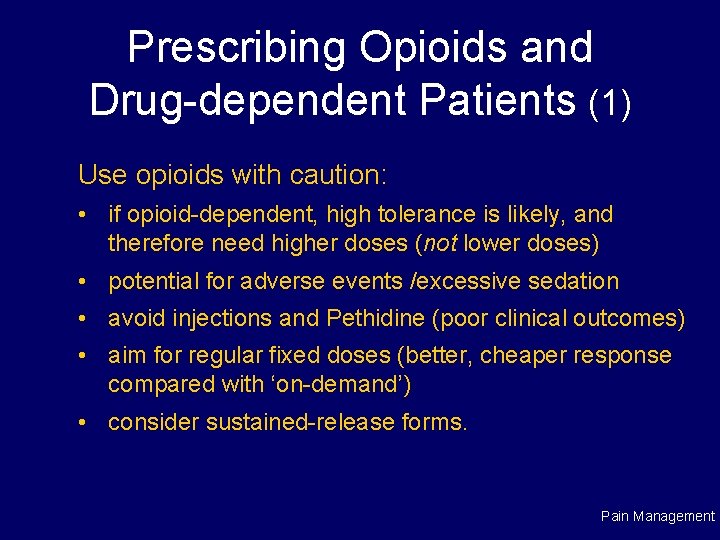
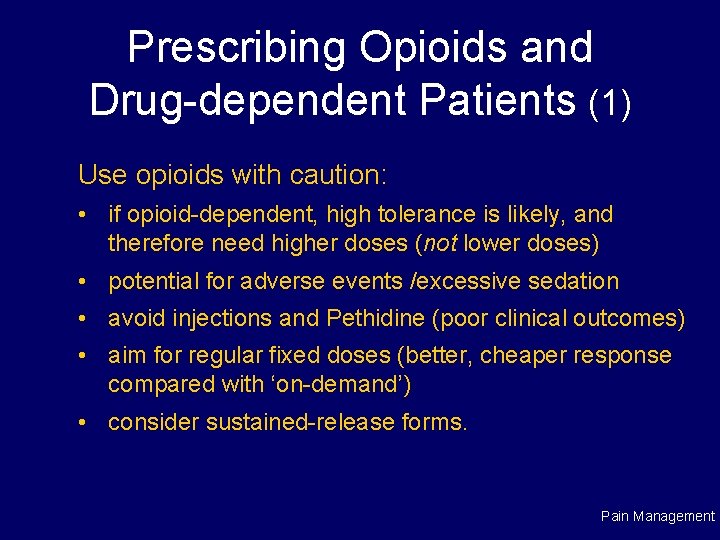
Prescribing Opioids and Drug-dependent Patients (1) Use opioids with caution: • if opioid-dependent, high tolerance is likely, and therefore need higher doses (not lower doses) • potential for adverse events /excessive sedation • avoid injections and Pethidine (poor clinical outcomes) • aim for regular fixed doses (better, cheaper response compared with ‘on-demand’) • consider sustained-release forms. Pain Management
Prescribing Opioids and Drug-dependent Patients (2) • Controversy re prescribing methadone for the opioiddependent • Separate prescribing for dependence from pain management issues (e. g. , via shared care) so that: – patients are not confused about dose, types & purpose of prescribed drugs – drug doses can be adjusted to accommodate the separate problems – staff fears of malingering can be allayed • Analgesics are just part of an effective management plan for chronic pain. Pain Management
Chronic Pain and Iatrogenic Dependence Definition: • dependence on medication following a period of medically-initiated pain management • true extent of the problem is difficult to gauge • treatment: dose tapering or methadone • prevention: – close supervision and monitoring of pain patients – review medication frequently – encourage alternative (non-drug) treatments to complement medication. Pain Management
Chronic Pain Patients and Risk of Drug Dependence Risk indicators may include: • personal / family history of high-risk patterns, problems or therapy (including receiving MMT) • demonstrating abnormal illness behaviour, low frustration tolerance, premorbid personality problems, or poor coping skills • history of childhood abuse • patients who describe euphoric effect from prescribed opiates • current stressors • complex compensable patients • young patients with obscure pathology. Pain Management
Chronic Pain Patients and Suspected Drug Dependence The following signs should alert you: • tolerance to prescribed opiates +/- BZDs and; – intoxication, deterioration in function, pain-associated distress • requesting scripts early • withdrawal symptoms and signs medication(s) not being taken • increased use of alcohol (increases sedation) • requesting opiate-based analgesics (rather than NSAIDS) • preoccupation with obtaining opioids despite analgesia • evidence of ‘doctor shopping’, visits to E. D. , hoarding supplies. Pain Management
Non-drug Complementary Strategies (1) • Medications – Other analgesics, antidepressants, anxiolytics, tranquillisers and hypnotics, muscle relaxants, antispasmodics, antihistamines, corticosteriods, local anaesthetics etc. • Lifestyle adjustment – exercise – ergonomic work stations / change in tasks / roles – relaxation / meditation • Physiotherapy / hydrotherapy / radiotherapy • Supportive counselling/CBT. Pain Management
Non-drug Complementary Strategies (2) • Cognitive therapy – changing beliefs / expectations, blocking negative thinking • Behaviour therapy – goal setting / problem-solving – self-reinforcement – diversion techniques • Stimulation to relieve pain – Transcutaneous Electrical Nerve Stimulation (TENS) – acupuncture – vibration / massage. Pain Management
Pain Relief is the Overriding Consideration • For the very elderly • The terminally ill with a short life expectancy Concerns of exacerbating drug dependence in these situations are secondary Pain Management
10 Tips for Managing Patients with Chronic Pain (1) 1. Define pain syndrome and treat cause (where evident) 2. Ensure Mx by single practitioner 3. Validate and accept patient’s pain experience 4. Establish clear, honest, open relationship 5. Make, and agree on, a clear treatment contract (cont…) Pain Management
10 Tips for Managing Patients with Chronic Pain cont. (2) 6. Educate and inform about your approach to pain Mx 7. Treat comorbidity with shared care team 8. Encourage alternatives to pharmacotherapy 9. Medication Mx – one doctor, close monitoring 10. Monitor progress, compliance and symptoms and maintain vigilance for evidence of dependence. Pain Management
Strategies for Managing Aberrant Behaviour • Re-assess medication, expectations, underlying cause • Consider changing drugs / interval between supply • Reinforce discussions / contract • Consider urine testing / warn of consequences of continued behaviour • Wean or cease opioid use • Notify health department / joint management with drug treatment agency • Consider very frequent medication supply / MMT. Pain Management
 Gps gps gps
Gps gps gps Gps gps gps
Gps gps gps Lewis mad pain and martian pain
Lewis mad pain and martian pain Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Period vs pregnancy symptoms
Period vs pregnancy symptoms Azure web role worker role example
Azure web role worker role example Role making role taking beispiele
Role making role taking beispiele Role conflict occurs when fulfilling the role expectations
Role conflict occurs when fulfilling the role expectations Gps stands for
Gps stands for Fuel monitoring system for vehicles
Fuel monitoring system for vehicles Mit app inventor sensors
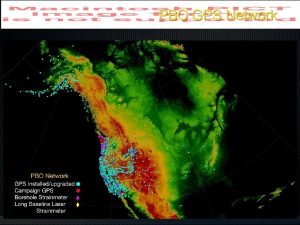
Mit app inventor sensors Understanding mobility based on gps data
Understanding mobility based on gps data Trimble gps rental
Trimble gps rental An/psn-13 defense advanced gps receiver
An/psn-13 defense advanced gps receiver Trimble gps site calibration procedure
Trimble gps site calibration procedure Gpsgaleb
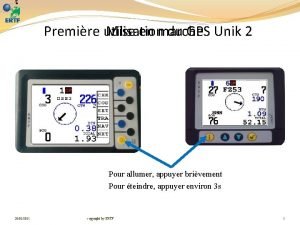
Gpsgaleb Ertf gps
Ertf gps Plgr gps
Plgr gps Rtk gps farming
Rtk gps farming Penjelasan tentang gps
Penjelasan tentang gps Gps glonas
Gps glonas Contigo gps fleet tracker
Contigo gps fleet tracker Marie venner consulting
Marie venner consulting What is gps triangulation
What is gps triangulation Trex gps
Trex gps Gpslockbox
Gpslockbox