OVERVIEW OF THYROID DISORDERS IN CHILDREN Marielisa Rincon



- Slides: 52
OVERVIEW OF THYROID DISORDERS IN CHILDREN Marielisa Rincon, MD
Learning Objectives n n Review of anatomy, embryology and physiology of the hypothalamic-pituitarythyroid axis Recognize, evaluate and initiate treatment of the following conditions: q q Congenital hypothyroidism Acquired hypothyroidism Hyperthyroidism Thyroid nodules

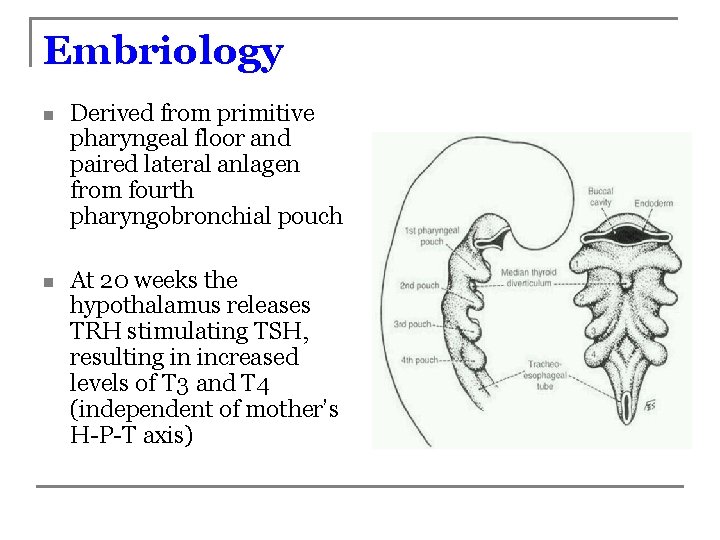
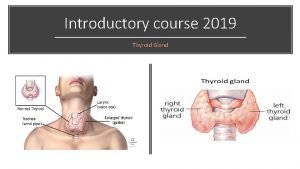
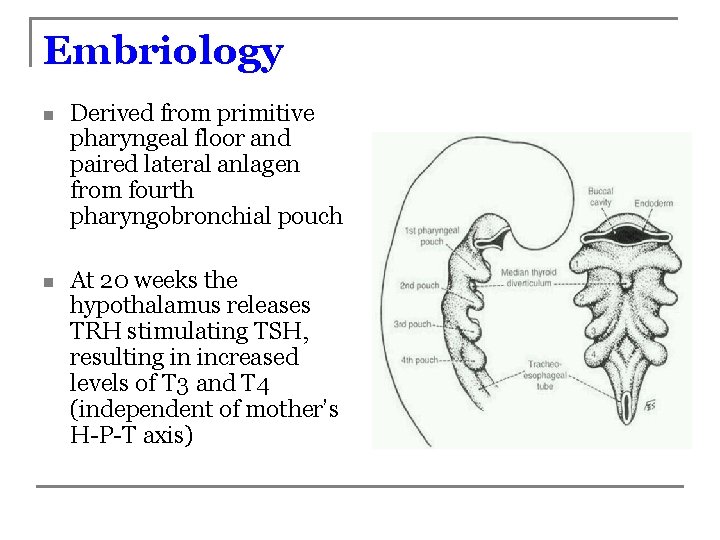
Embriology n Derived from primitive pharyngeal floor and paired lateral anlagen from fourth pharyngobronchial pouch n At 20 weeks the hypothalamus releases TRH stimulating TSH, resulting in increased levels of T 3 and T 4 (independent of mother’s H-P-T axis)
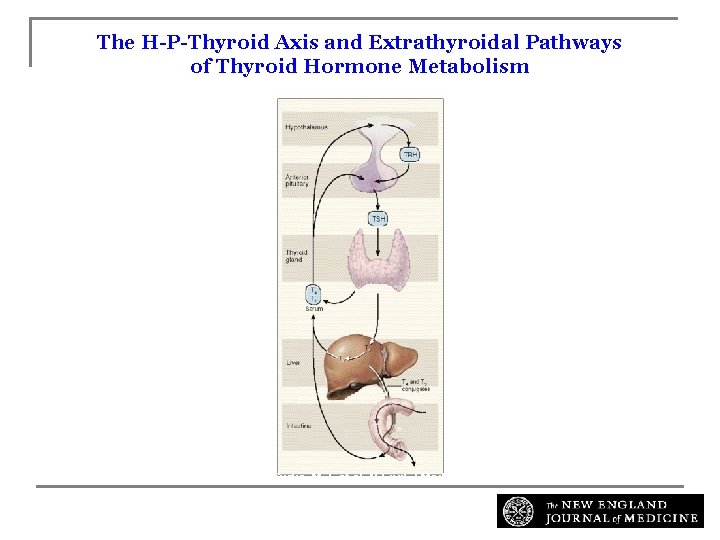
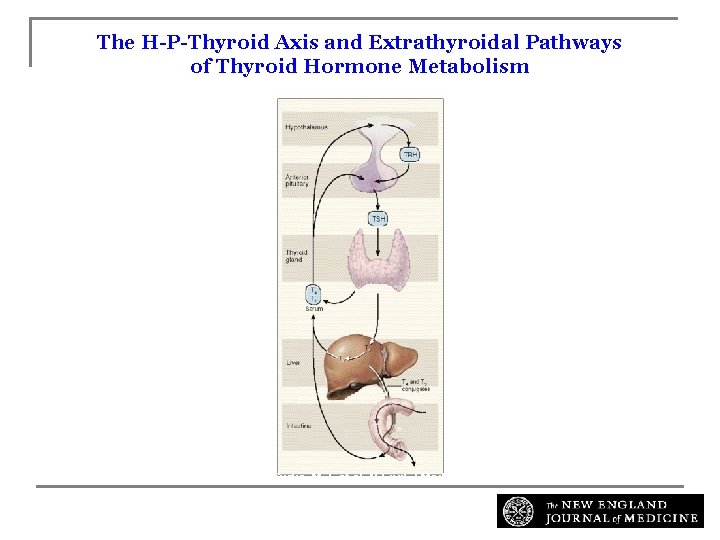
The H-P-Thyroid Axis and Extrathyroidal Pathways of Thyroid Hormone Metabolism Surks, M. I. et al. N Engl J Med 1995; 333: 1688 -1694

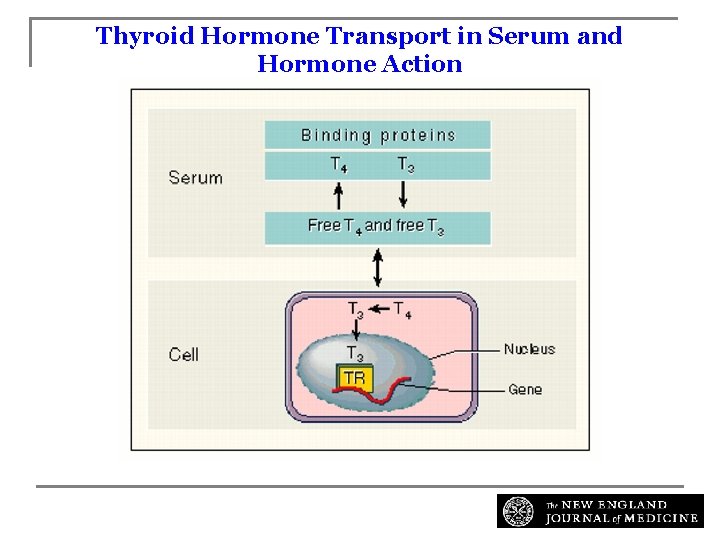
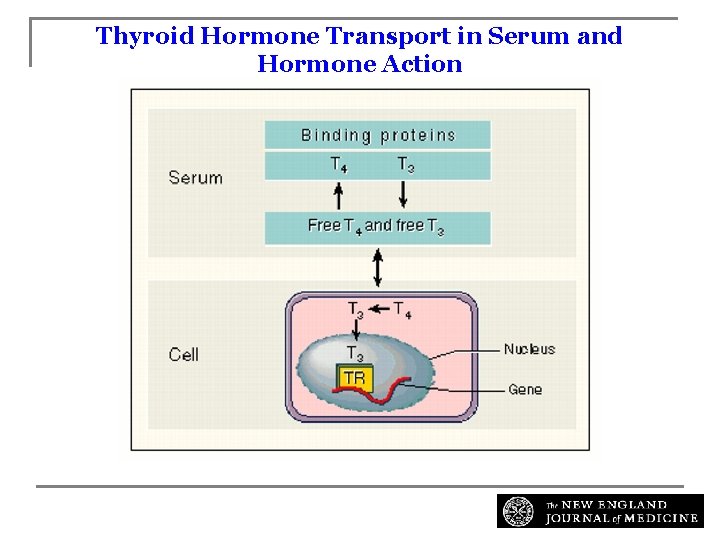
Thyroid Hormone Transport in Serum and Hormone Action Surks, M. I. et al. N Engl J Med 1995; 333: 1688 -1694
Effects of thyroid hormones n CNS: migration, maturation and myelinization n Growth: Growth factors n Thermogenic effects n Metabolic effects include potentiation of hormone synthesis, glucose transport and stimulation of adrenergic receptor binding
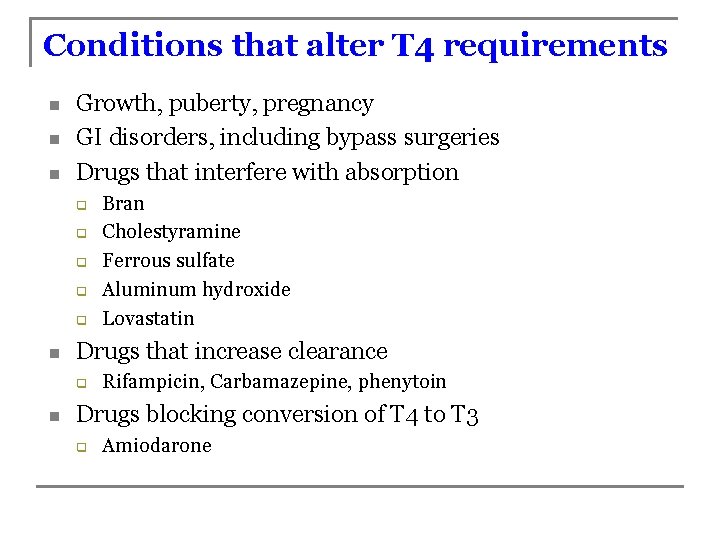
Conditions that alter T 4 requirements n n n Growth, puberty, pregnancy GI disorders, including bypass surgeries Drugs that interfere with absorption q q q n Drugs that increase clearance q n Bran Cholestyramine Ferrous sulfate Aluminum hydroxide Lovastatin Rifampicin, Carbamazepine, phenytoin Drugs blocking conversion of T 4 to T 3 q Amiodarone
Congenital Hypothyroidism
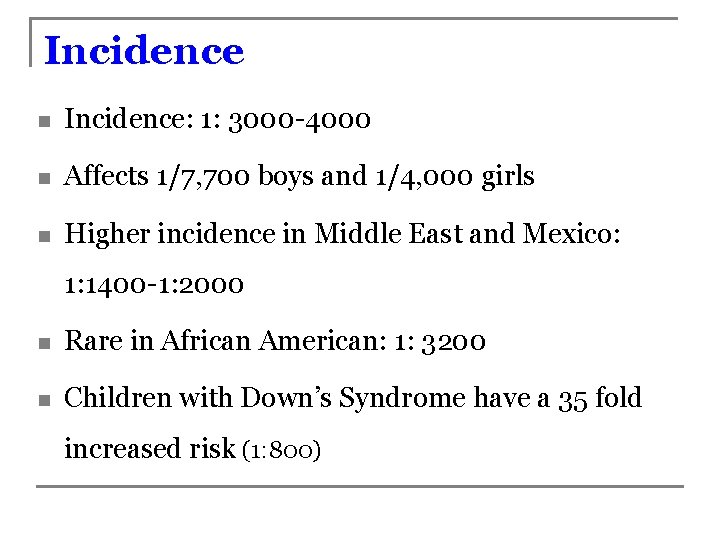
Incidence n Incidence: 1: 3000 -4000 n Affects 1/7, 700 boys and 1/4, 000 girls n Higher incidence in Middle East and Mexico: 1: 1400 -1: 2000 n Rare in African American: 1: 3200 n Children with Down’s Syndrome have a 35 fold increased risk (1: 800)
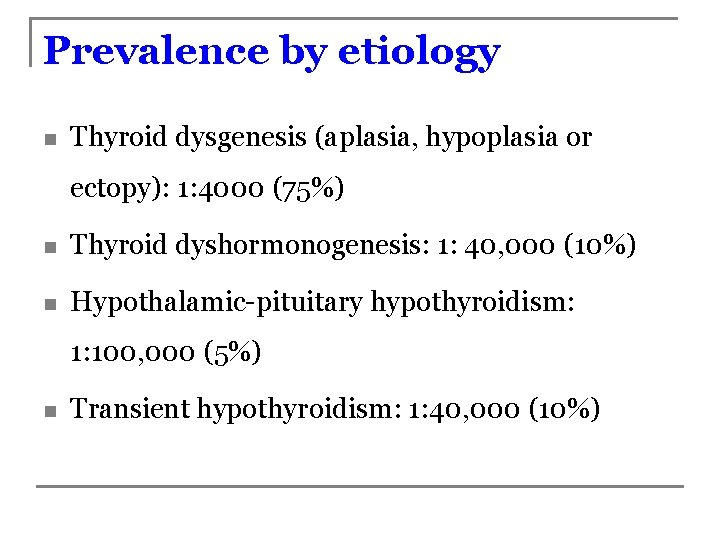
Prevalence by etiology n Thyroid dysgenesis (aplasia, hypoplasia or ectopy): 1: 4000 (75%) n Thyroid dyshormonogenesis: 1: 40, 000 (10%) n Hypothalamic-pituitary hypothyroidism: 1: 100, 000 (5%) n Transient hypothyroidism: 1: 40, 000 (10%)
Transient causes n Iodine deficiency n Maternal blocking antibodies n Maternal or neonatal drug exposure n q Excess iodine (Wolff-Chaikoff effect) q Other drugs (corticosteroids and dopamine) Dyshormonogenesis
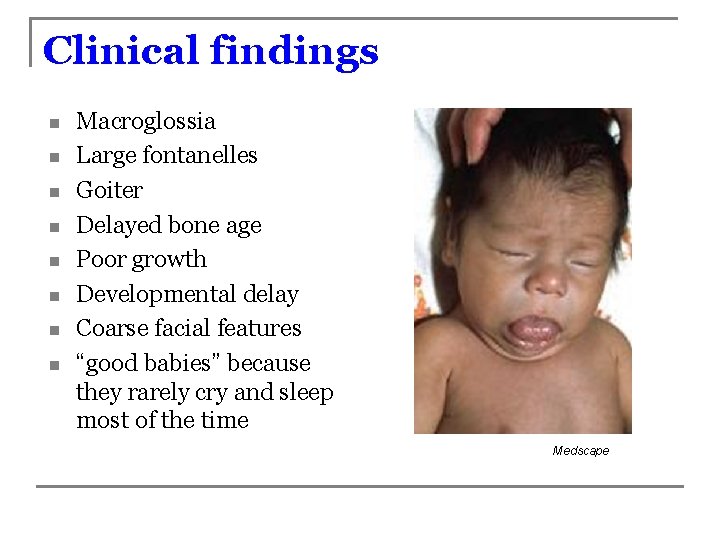
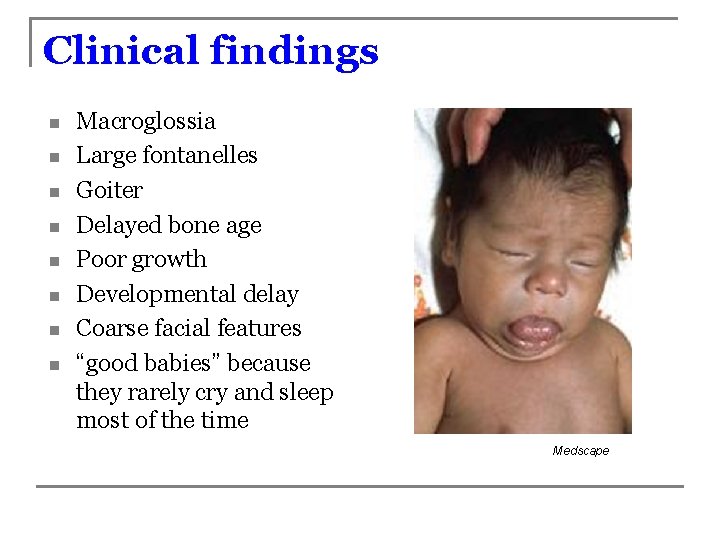
Clinical findings n n n n Macroglossia Large fontanelles Goiter Delayed bone age Poor growth Developmental delay Coarse facial features “good babies” because they rarely cry and sleep most of the time Medscape
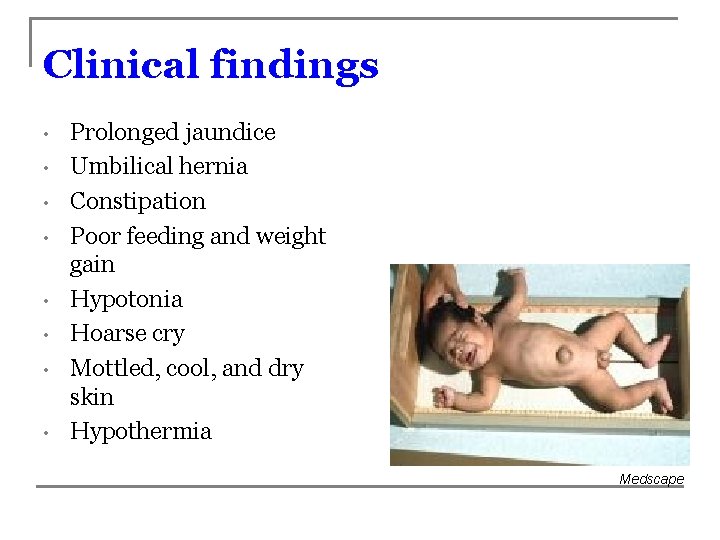
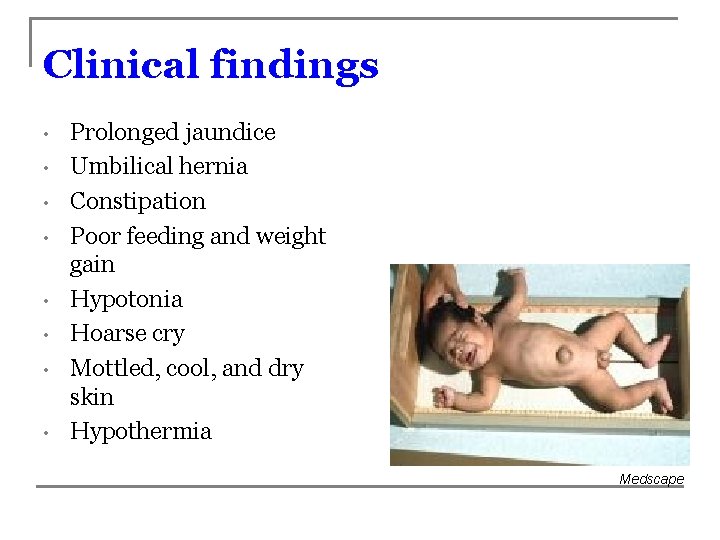
Clinical findings • • Prolonged jaundice Umbilical hernia Constipation Poor feeding and weight gain Hypotonia Hoarse cry Mottled, cool, and dry skin Hypothermia Medscape
Why don’t all infants with hypothyroidism demonstrate these features? q q Although the placenta is impermeable to TSH, small amounts of maternal T 3 and T 4 can pass to fetus A compensatory increase in maternal thyroid hormone transfer and increase in deiodinase activity can protect the fetus
Associated conditions § § Cardiac conditions including sick sinus syndrome, PDA, ASD, PS, and TA have been associated in 12% of kids with congenital hypothyroidism. CH due to impaired hormone synthesis could be associated with deafness (Pendred syndrome)
NB Screening in Kansas n n n Starting July 1, 2008, Kansas newborns are screened for the core panel of 29 conditions recommended for inclusion in all state screening programs by the American College of Medical Genetics. The state laboratory utilizes tandem mass technology (MS/MS) The Kansas program: q Screening - About 40, 000 KS births/initial tests each year with about 2, 000 needing retest
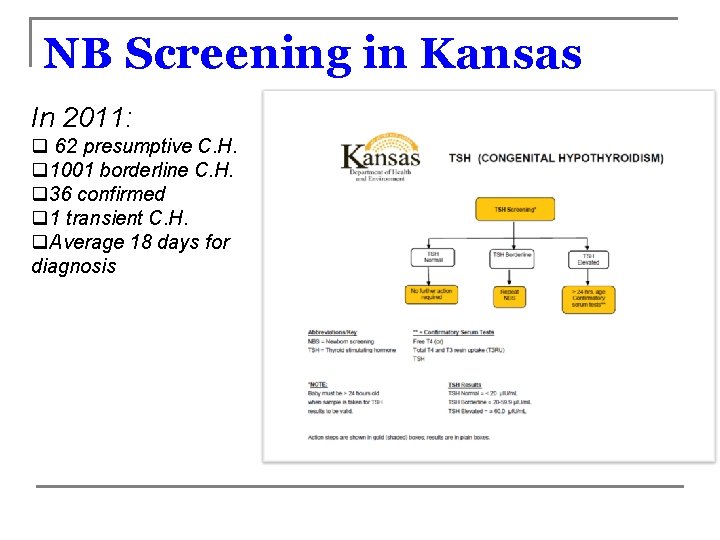
NB Screening in Kansas In 2011: q 62 presumptive C. H. q 1001 borderline C. H. q 36 confirmed q 1 transient C. H. q. Average 18 days for diagnosis
NB Screening for CH Pitfalls: q q q Early samples inconclusive due to TSH surge at birth Only TSH in Kansas: screening identifies primary CH n Does not identify children with secondary hypothyroidism (low T 4, normal TSH) Some (VLBW) infants with CH display delayed TSH rise PCP Responsibilities for Follow-up: n n n Specimens Within Normal Limits (WNL)—to inform parent/guardian of the results Unsatisfactory Specimens—to repeat specimen Process for Presumptive Positive for Disease—to obtain further testing q confirmatory blood sample for (free)T 4 and TSH by venipuncture
Implications for treatment n Children with positive screening and borderline levels of TSH and free T 4 should be treated until 3 years of age n At that time, thyroid hormone replacement can be discontinued and additional diagnostic studies performed n It is essential that any infant or child who manifests symptoms consistent with hypothyroidism be retested by the PCP regardless of the results of the newborn screen
Treatment n L-thyroxin (Synthroid): q q n 10 -15 mcg/kg/day; or 50 mcg daily for two weeks, then 10 mcg/kg/day Precautions: q q Never mix with milk or juice in the bottle Tablets have better bioavailability (do not prescribe “compounds”) Soy can interfere with absorption Any time of day, though some people prefer mornings

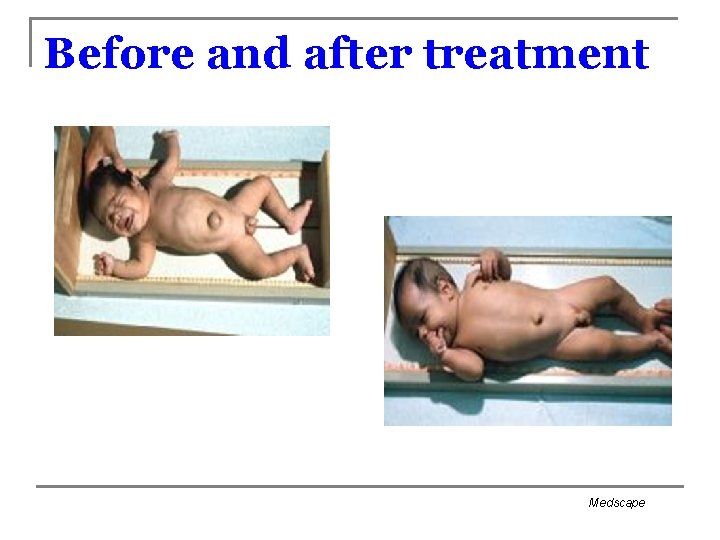
Before and after treatment Medscape
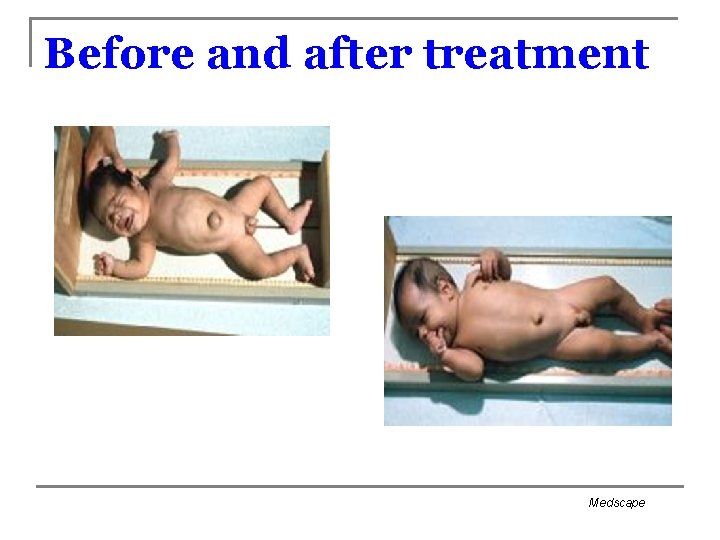
Before and after treatment Medscape
Monitoring treatment n Signs and symptoms q q q n n Developmental milestones Laboratory test: q q q n Growth, especially length/height Dentition Excess treatment : Diarrhea, weight loss , sleep disturbances, craniosynostosis TSH and free T 4 in primary hypothyroidism Free T 4 in secondary hypothyroidism Do levels 4 -6 weeks after introduction of treatment or change in dose Monitor child every 2 -3 months during first 2 years of life
Acquired Juvenile Hypothyroidism
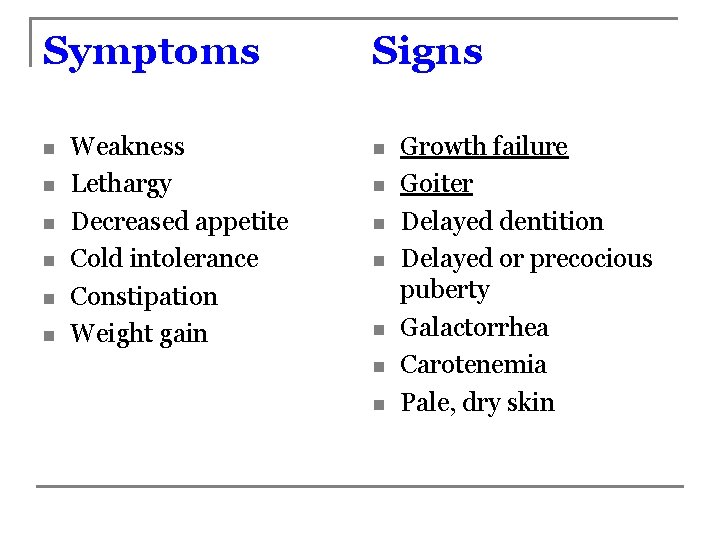
Symptoms n n n Weakness Lethargy Decreased appetite Cold intolerance Constipation Weight gain Signs n n n n Growth failure Goiter Delayed dentition Delayed or precocious puberty Galactorrhea Carotenemia Pale, dry skin
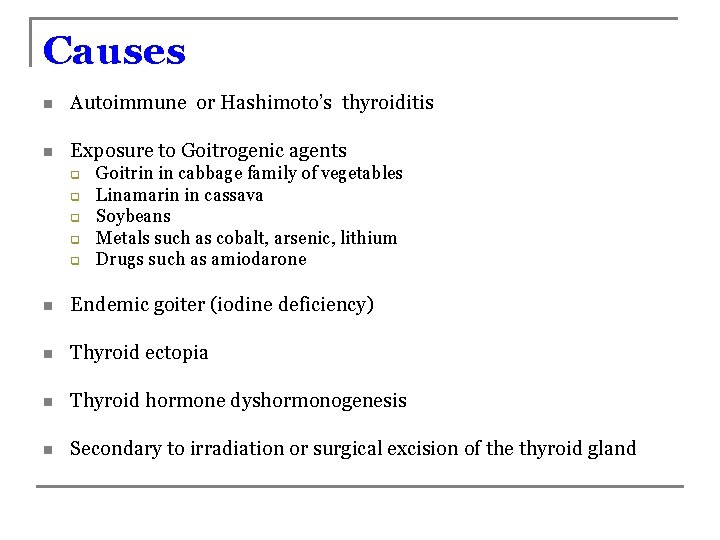
Causes n Autoimmune or Hashimoto’s thyroiditis n Exposure to Goitrogenic agents q q q Goitrin in cabbage family of vegetables Linamarin in cassava Soybeans Metals such as cobalt, arsenic, lithium Drugs such as amiodarone n Endemic goiter (iodine deficiency) n Thyroid ectopia n Thyroid hormone dyshormonogenesis n Secondary to irradiation or surgical excision of the thyroid gland
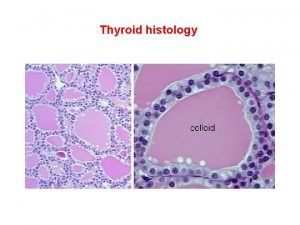
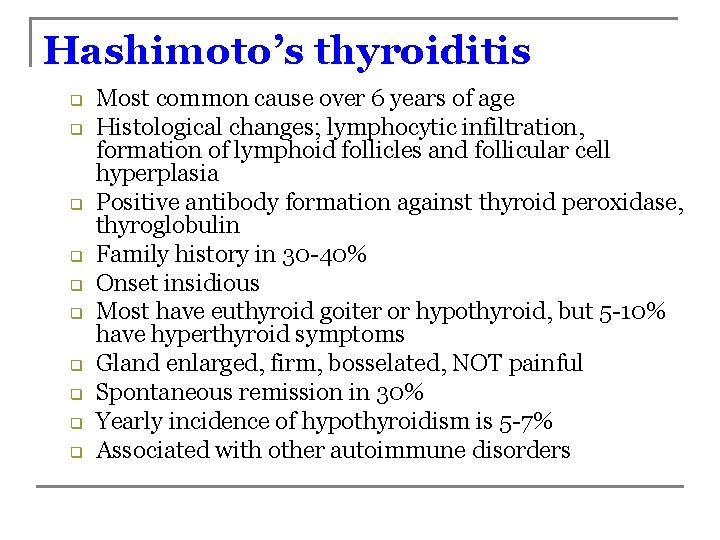
Hashimoto’s thyroiditis q q q q q Most common cause over 6 years of age Histological changes; lymphocytic infiltration, formation of lymphoid follicles and follicular cell hyperplasia Positive antibody formation against thyroid peroxidase, thyroglobulin Family history in 30 -40% Onset insidious Most have euthyroid goiter or hypothyroid, but 5 -10% have hyperthyroid symptoms Gland enlarged, firm, bosselated, NOT painful Spontaneous remission in 30% Yearly incidence of hypothyroidism is 5 -7% Associated with other autoimmune disorders
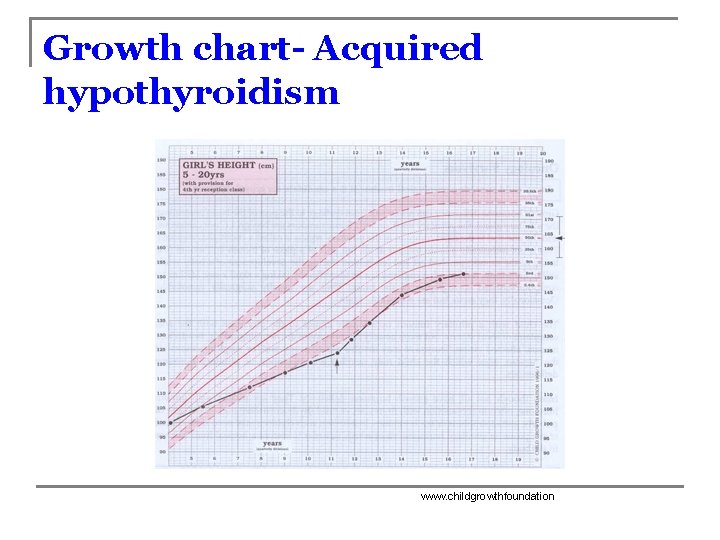
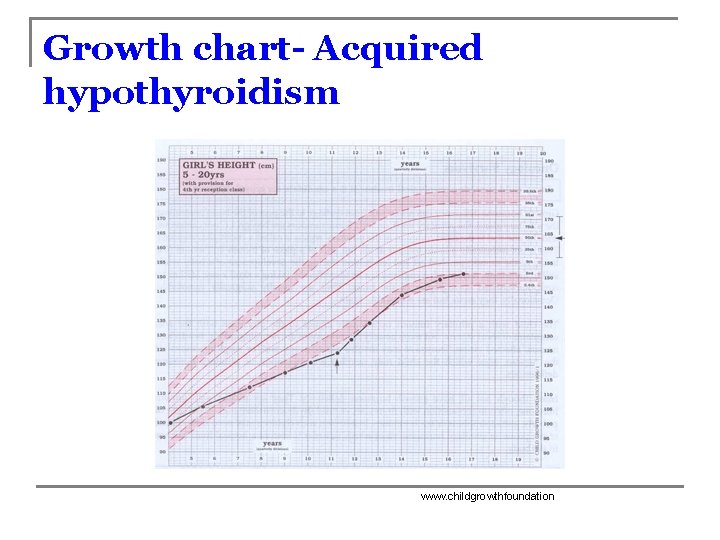
Growth chart- Acquired hypothyroidism www. childgrowthfoundation
Evaluation n HPI-poor growth PE-goiter Laboratory data: q q q Free T 4 TSH Microsomal antibodies (not needed for treatment)
Hypothyroidism and obesity “Moderately elevated TSH and T 3 levels in obese children are a frequent finding, and in the majority of the obese children these increases cannot be explained by autoimmune thyroiditis, iodine deficiency or hypothyroidism. Serum T 4 concentrations are usually normal. TSH and T 3 levels in the upper normal range fully normalized after weight reduction in obese children. ”
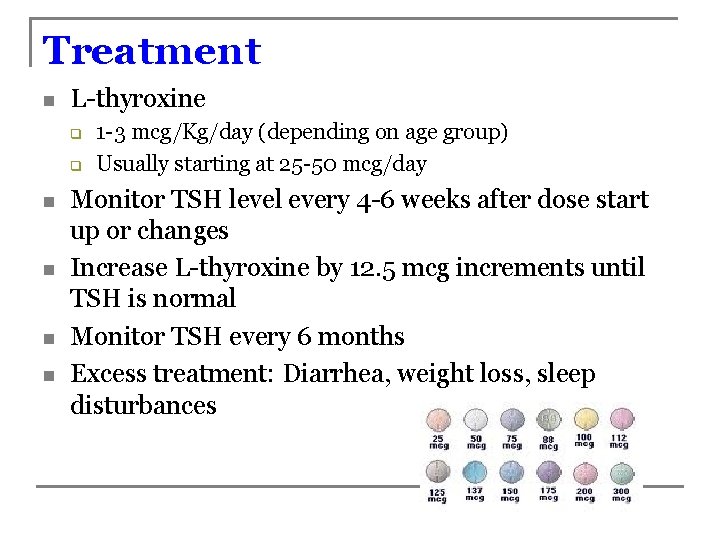
Treatment n L-thyroxine q q n n 1 -3 mcg/Kg/day (depending on age group) Usually starting at 25 -50 mcg/day Monitor TSH level every 4 -6 weeks after dose start up or changes Increase L-thyroxine by 12. 5 mcg increments until TSH is normal Monitor TSH every 6 months Excess treatment: Diarrhea, weight loss, sleep disturbances
Euthyroid Sick syndrome q q Present during acute or chronic severe illness, surgery, trauma or malnutrition Secondary to decrease activity of 5’-deiodinase enzyme, so there is accumulation of reverse T 3 and decreased T 3 There is poor response of TSH to low T 4 and T 3 Biochemical evaluation: n n T 4: low T 3: low r. T 3: High TSH: Normal r. T 3 www. google. com/url? sa=i&rc
Hyperthyroidism
Signs and symptoms of hyperthyroidism n n n n n Nervousness Increased sweating Heat intolerance Palpitations Fatigue Weight loss Tachycardia Goiter Increased pulse pressure n n Dyspnea Weakness Increased appetite Eye complaints q n n n Proptosis Swelling of legs Diarrhea Tremors
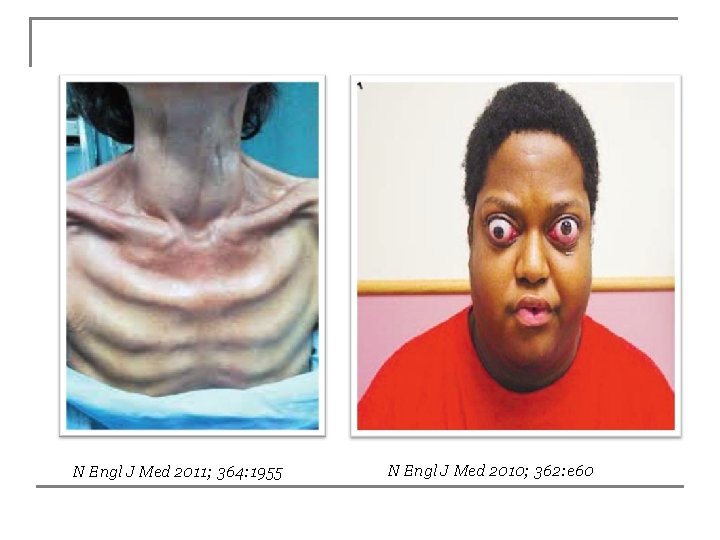
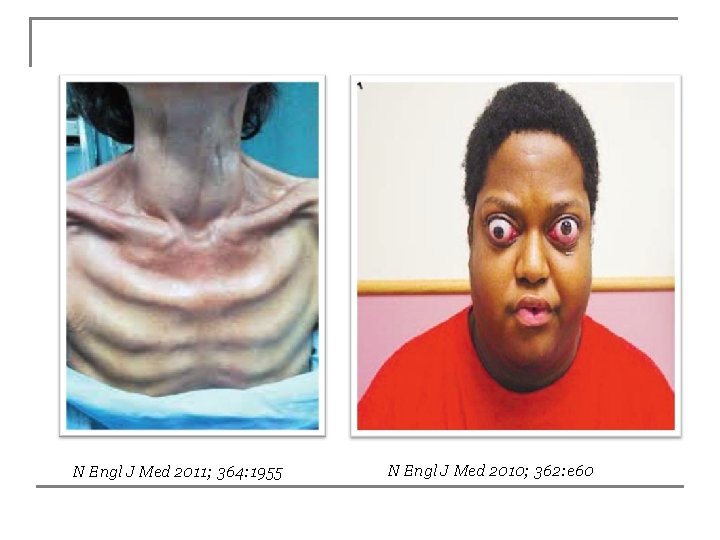
N Engl J Med 2011; 364: 1955 N Engl J Med 2010; 362: e 60
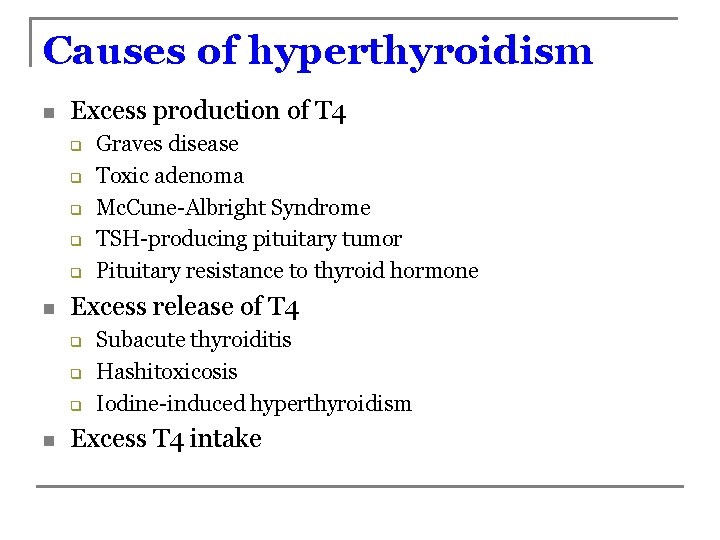
Causes of hyperthyroidism n Excess production of T 4 q q q n Excess release of T 4 q q q n Graves disease Toxic adenoma Mc. Cune-Albright Syndrome TSH-producing pituitary tumor Pituitary resistance to thyroid hormone Subacute thyroiditis Hashitoxicosis Iodine-induced hyperthyroidism Excess T 4 intake
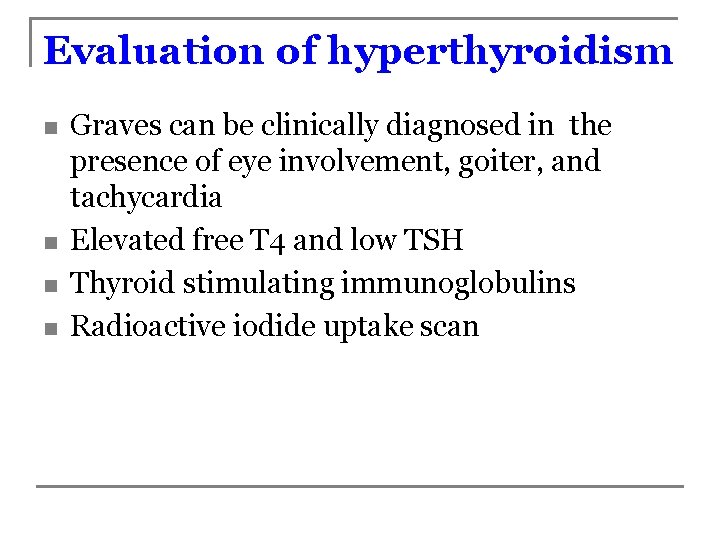
Evaluation of hyperthyroidism n n Graves can be clinically diagnosed in the presence of eye involvement, goiter, and tachycardia Elevated free T 4 and low TSH Thyroid stimulating immunoglobulins Radioactive iodide uptake scan
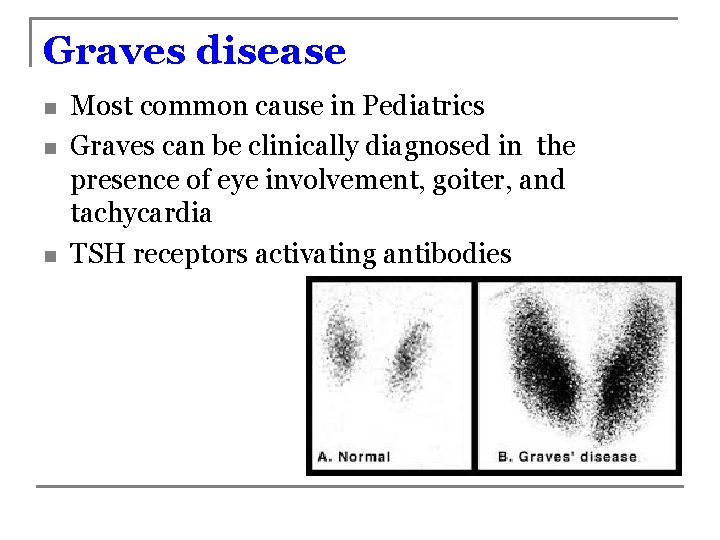
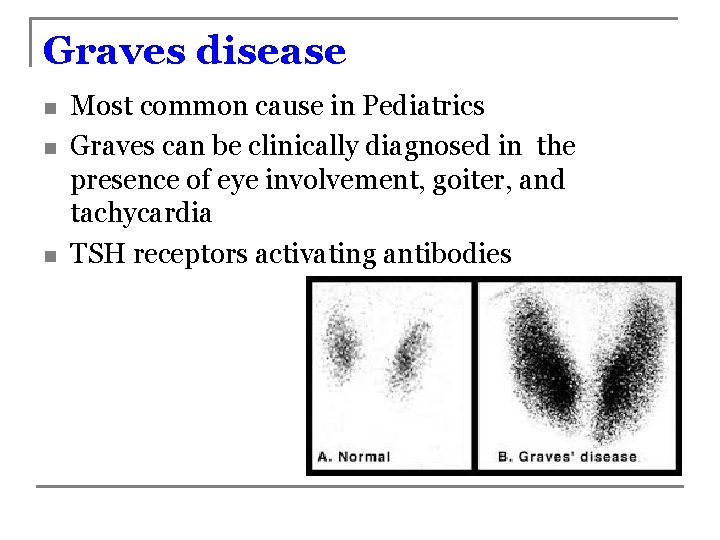
Graves disease n n n Most common cause in Pediatrics Graves can be clinically diagnosed in the presence of eye involvement, goiter, and tachycardia TSH receptors activating antibodies
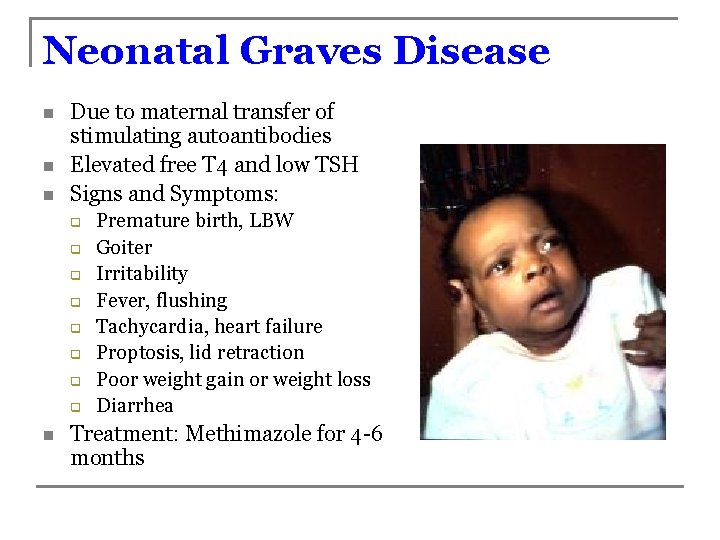
Neonatal Graves Disease n n n Due to maternal transfer of stimulating autoantibodies Elevated free T 4 and low TSH Signs and Symptoms: q q q q n Premature birth, LBW Goiter Irritability Fever, flushing Tachycardia, heart failure Proptosis, lid retraction Poor weight gain or weight loss Diarrhea Treatment: Methimazole for 4 -6 months
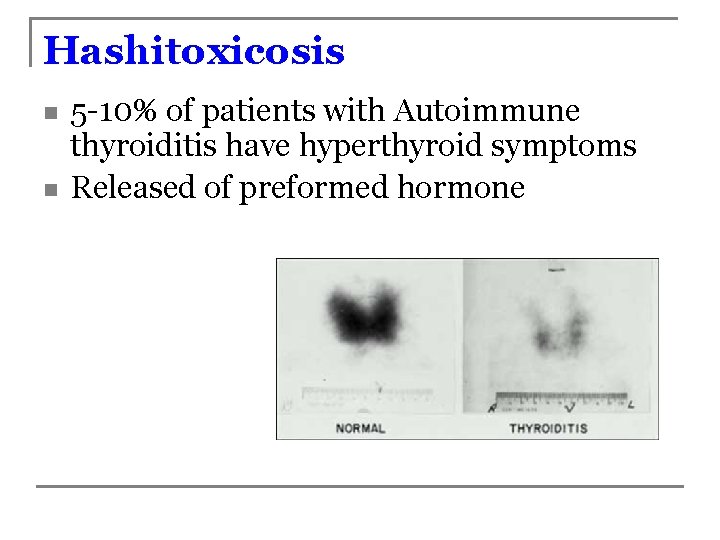
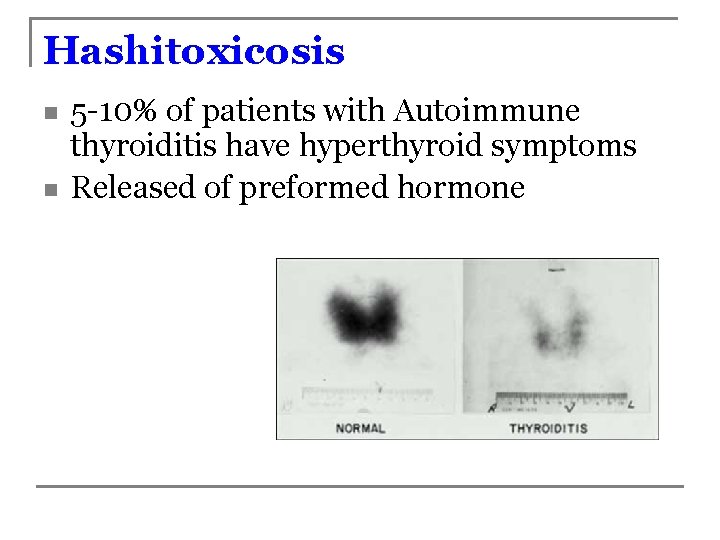
Hashitoxicosis n n 5 -10% of patients with Autoimmune thyroiditis have hyperthyroid symptoms Released of preformed hormone
Subacute Thyroiditis n n Etiology: Postviral syndrome Physical exam: q Painful swelling of thyroid q Hyperthyroidism Laboratory data: q High T 4, low TSH, high ESR, absent TSI q Low radioactive uptake scan Treatment: q Beta blockers, aspirin or glucocorticoids q Antithyroid drugs DO NOT WORK
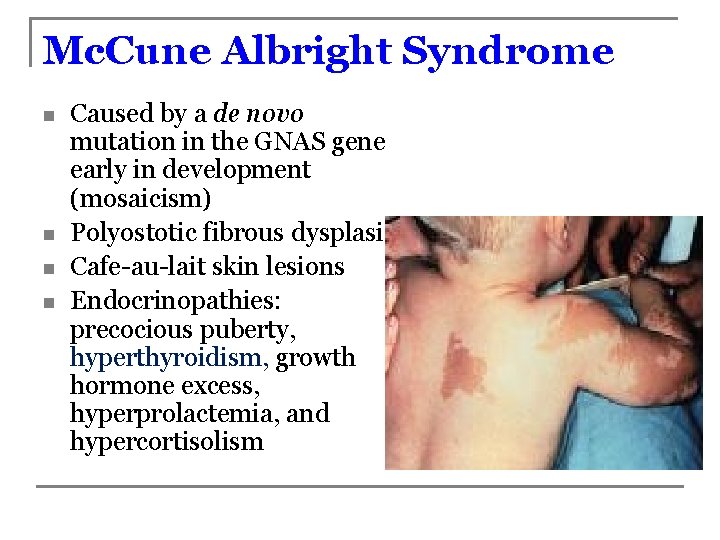
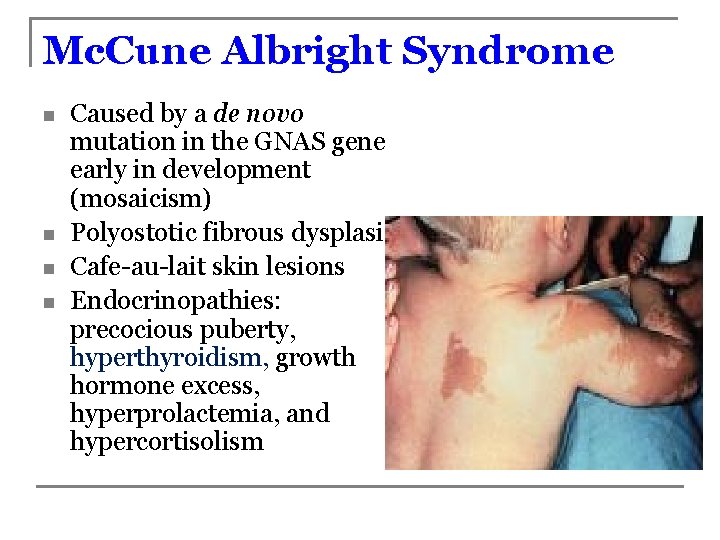
Mc. Cune Albright Syndrome n n Caused by a de novo mutation in the GNAS gene early in development (mosaicism) Polyostotic fibrous dysplasia Cafe-au-lait skin lesions Endocrinopathies: precocious puberty, hyperthyroidism, growth hormone excess, hyperprolactemia, and hypercortisolism
Treatment options n Antithyroid agents q q n n Propylthiouracil (PTU) only for thyroid storm Methimazole 0. 5 -1 mg/Kg QD-TID Both have side effects: (5%) rash, nausea, headache, pruritus, alopecia, arthralgia/arthritis, agranulocytosis, hepatic toxicity, lupus-like syndrome, myalgia, etc. 45 -50% of Graves patients will enter remission within 3 years I 131 radioactive ablation Thyroidectomy
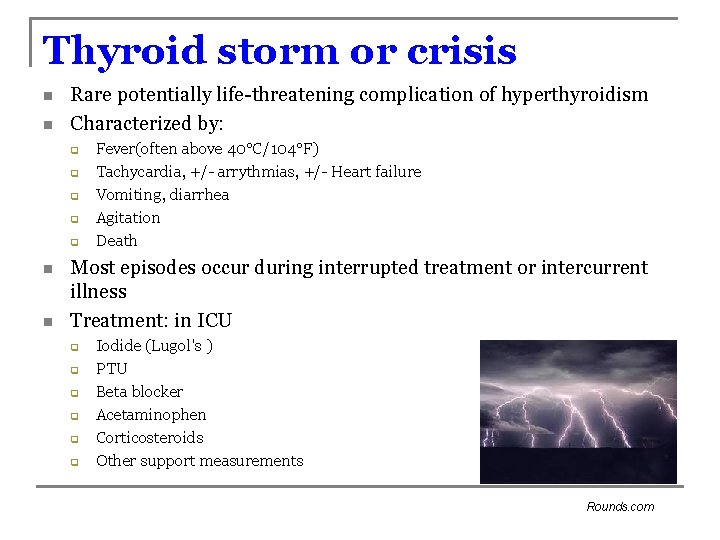
Thyroid storm or crisis n n Rare potentially life-threatening complication of hyperthyroidism Characterized by: q q q n n Fever(often above 40°C/104°F) Tachycardia, +/- arrythmias, +/- Heart failure Vomiting, diarrhea Agitation Death Most episodes occur during interrupted treatment or intercurrent illness Treatment: in ICU q q q Iodide (Lugol's ) PTU Beta blocker Acetaminophen Corticosteroids Other support measurements Rounds. com
Thyroid Nodule
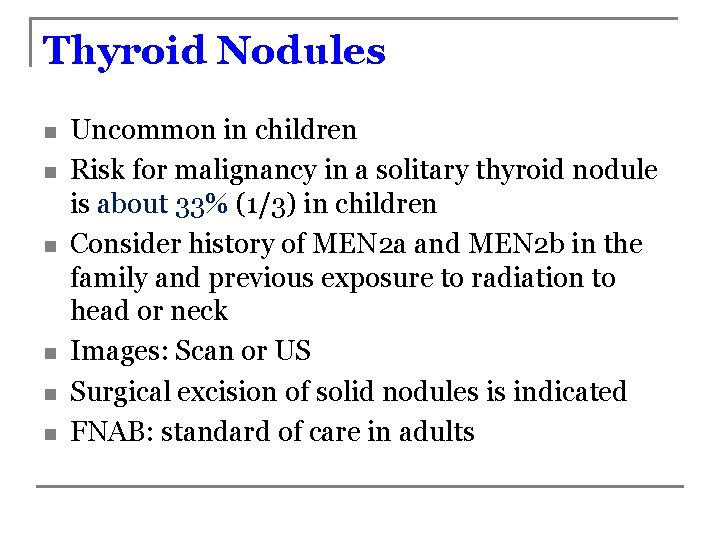
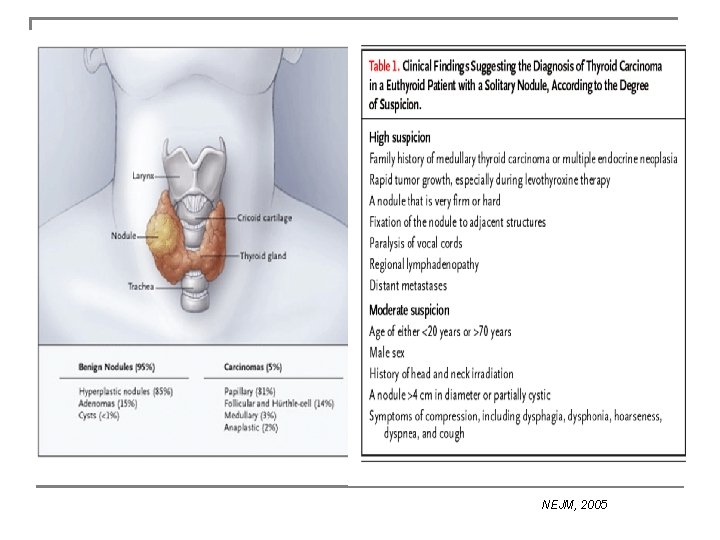
Thyroid Nodules n n n Uncommon in children Risk for malignancy in a solitary thyroid nodule is about 33% (1/3) in children Consider history of MEN 2 a and MEN 2 b in the family and previous exposure to radiation to head or neck Images: Scan or US Surgical excision of solid nodules is indicated FNAB: standard of care in adults
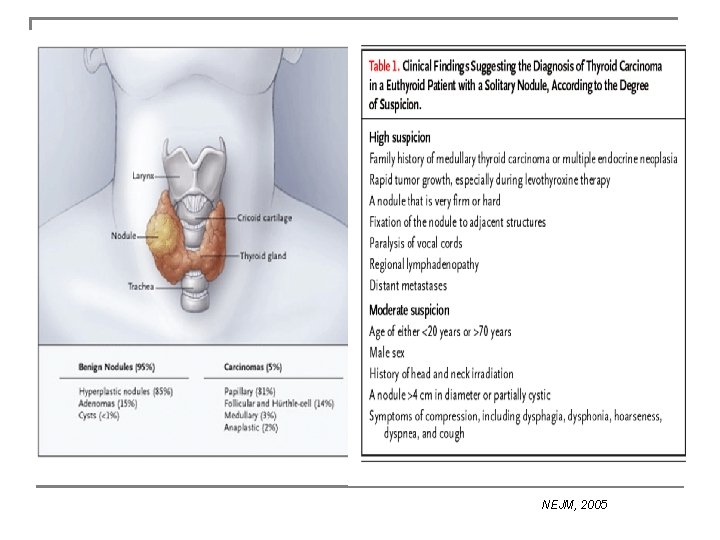
NEJM, 2005
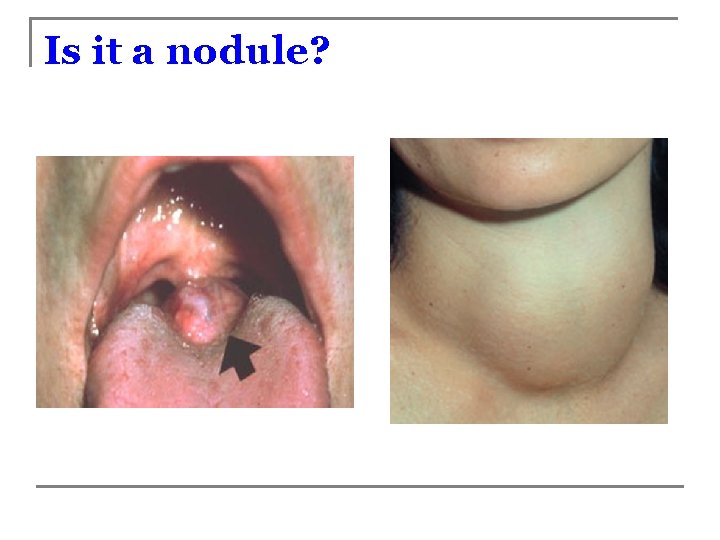
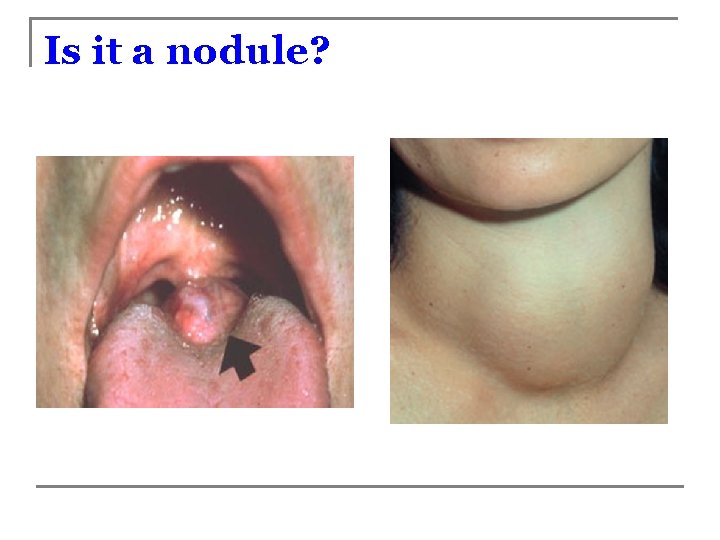
Is it a nodule?
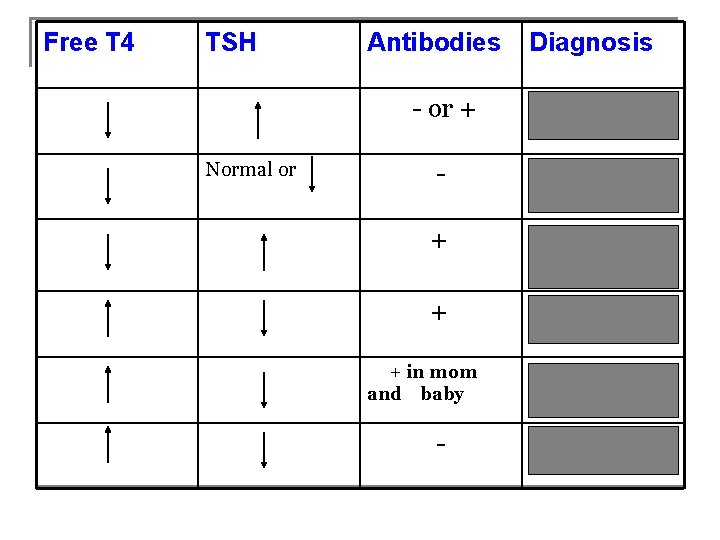
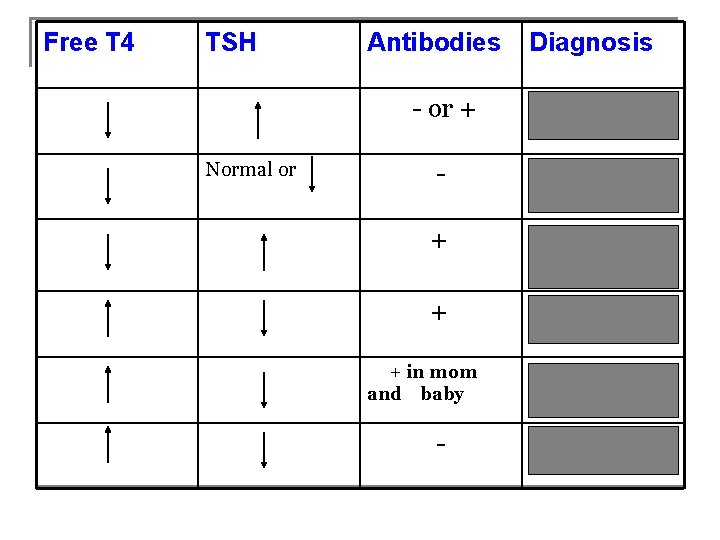
Free T 4 TSH Normal or Antibodies Diagnosis - or + Primary Hypothyroidism - Sick thyroid syndrome, Secondary hypothyroidism + Acquired hypothyroidism (Hashimoto’s) + Hyperthyroidism, Graves disease + in mom and baby - Neonatal Graves disease Subacute thyroiditis
Any questions?
 Resumen del libro del buen amor
Resumen del libro del buen amor Rincón de juegos tranquilos
Rincón de juegos tranquilos Rincon development
Rincon development La mujer necia destruye su hogar
La mujer necia destruye su hogar Sheyla fanory caicedo rincón
Sheyla fanory caicedo rincón El rincon del vago
El rincon del vago Neoplasam
Neoplasam Histological structure of parathyroid gland
Histological structure of parathyroid gland Ata thyroid
Ata thyroid Thyroid eye disease
Thyroid eye disease Site:slidetodoc.com
Site:slidetodoc.com Thyroid hormone secretion
Thyroid hormone secretion Four oval masses on posterior thyroid gland
Four oval masses on posterior thyroid gland Thyroid grading system
Thyroid grading system Parathyroid gland chief cell
Parathyroid gland chief cell Thyrotoxicosis mnemonic
Thyrotoxicosis mnemonic Thyroid pathology
Thyroid pathology Thyroid stimulating hormone
Thyroid stimulating hormone Thyroid liver
Thyroid liver Chapman points omm
Chapman points omm American thyroid association guidelines pregnancy 2017
American thyroid association guidelines pregnancy 2017 Thyroid nodule
Thyroid nodule Quadrangular membrane larynx
Quadrangular membrane larynx Thyroid ultrasonography
Thyroid ultrasonography Armour thyroid dosering
Armour thyroid dosering Lymph node
Lymph node Thyroid anatomy
Thyroid anatomy Thyroglobulin
Thyroglobulin Innervation of parathyroid gland
Innervation of parathyroid gland Shrsies
Shrsies Vulvar dystrophy thyroid
Vulvar dystrophy thyroid Myxödem
Myxödem Acog thyroid pregnancy
Acog thyroid pregnancy Nursing management of thyroid cancer
Nursing management of thyroid cancer Symptoms of thyroid
Symptoms of thyroid Recurrent laryngeal nerve
Recurrent laryngeal nerve Cupping for thyroid
Cupping for thyroid Pituitary gland thyroid
Pituitary gland thyroid Urethritis
Urethritis Goiter
Goiter Colloid thyroid histology
Colloid thyroid histology Burlington medical lead aprons
Burlington medical lead aprons Thyroid peroxidase
Thyroid peroxidase Thyroid functions
Thyroid functions Nodular goiter
Nodular goiter Follicular adenoma
Follicular adenoma Primary hyperthyroidism
Primary hyperthyroidism Pictures of thyroid eye disease
Pictures of thyroid eye disease Thyroid storm pathophysiology
Thyroid storm pathophysiology Thyroid eye disease
Thyroid eye disease Pharyngeal pouch and cleft
Pharyngeal pouch and cleft Principal cells location
Principal cells location Thyroid diverticulum
Thyroid diverticulum