Thyroid pharmacology THYROID GLAND Location 12 to 20

- Slides: 42
Thyroid pharmacology
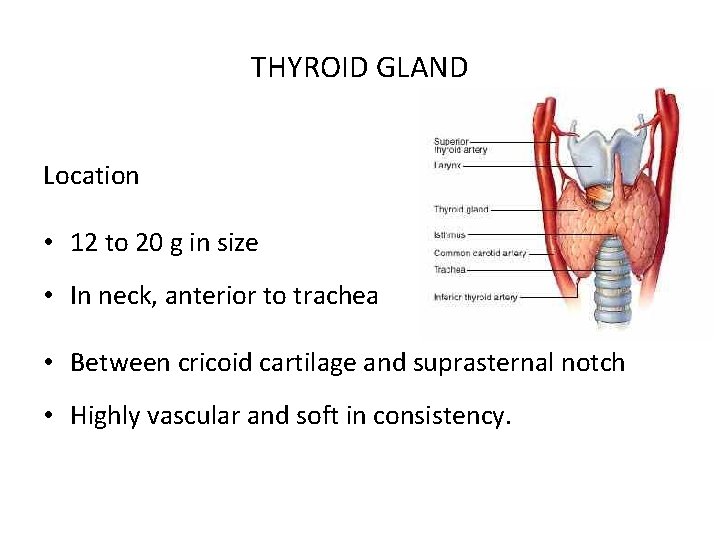
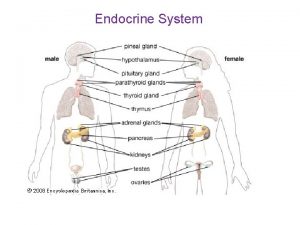
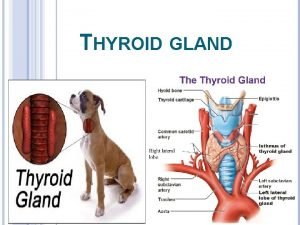
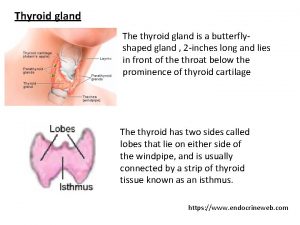
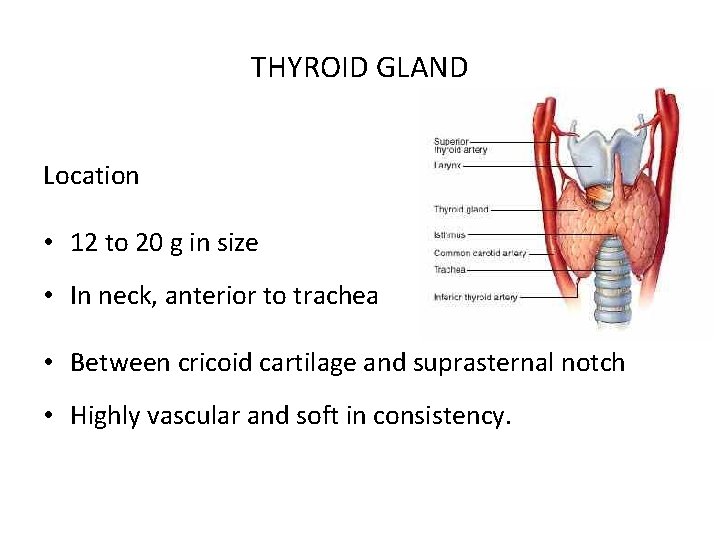
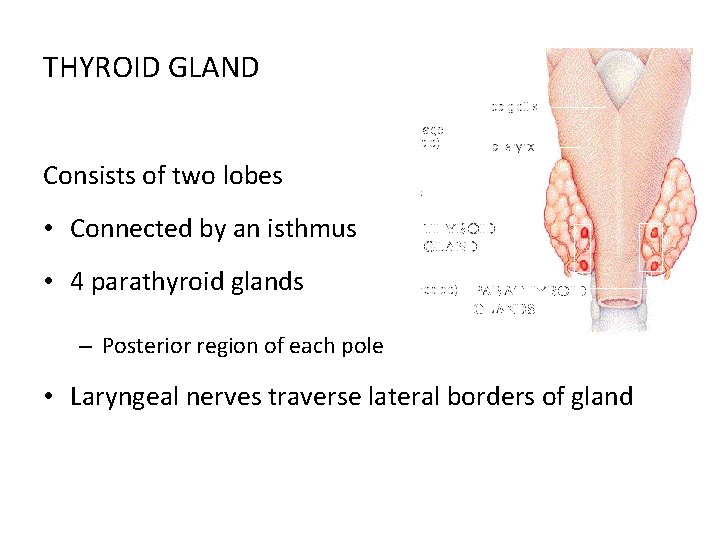
THYROID GLAND Location • 12 to 20 g in size • In neck, anterior to trachea • Between cricoid cartilage and suprasternal notch • Highly vascular and soft in consistency.
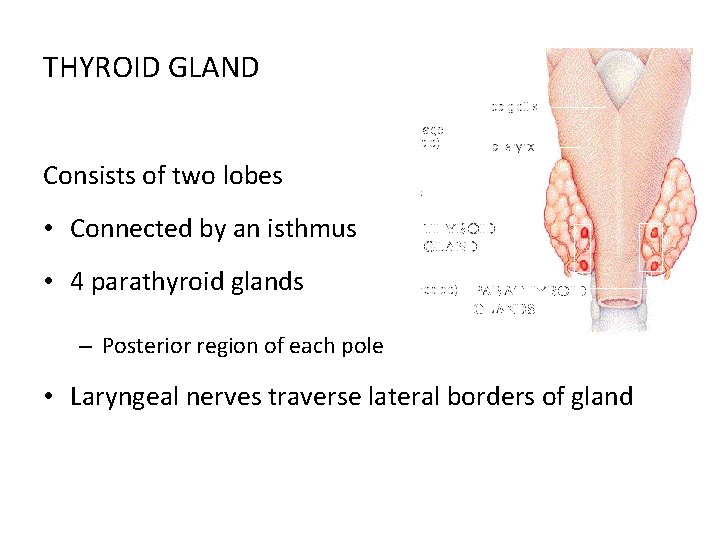
THYROID GLAND Consists of two lobes • Connected by an isthmus • 4 parathyroid glands – Posterior region of each pole • Laryngeal nerves traverse lateral borders of gland
Secretions Produces two related hormones • Thyroxine (T 4) • Triiodothyronine (T 3)
Action Play a critical role in • Cell differentiation during development • Help to maintain thermogenic and metabolic homeostasis in adult. • Act through nuclear hormone receptors to modulate gene expression
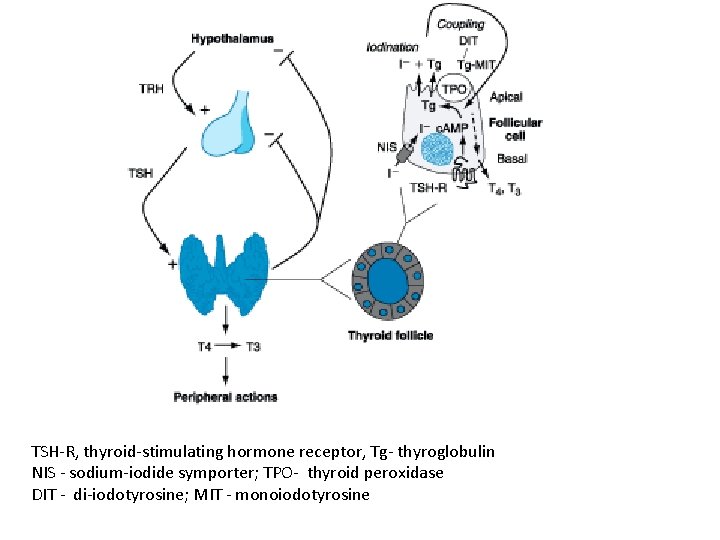
Regulation of thyroid hormone synthesis T 4 and T 3 feed back to inhibit • Hypothalamic production of thyrotropin-releasing hormone (TRH) • Pituitary production of thyroid-stimulating hormone (TSH)
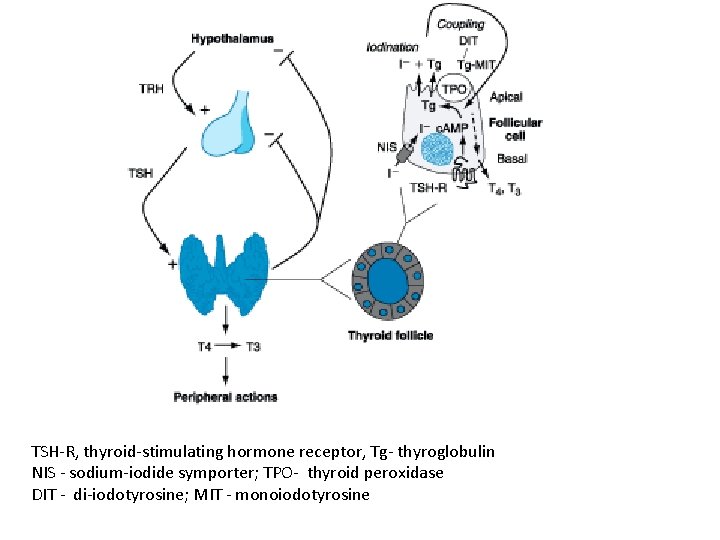
TSH-R, thyroid-stimulating hormone receptor, Tg- thyroglobulin NIS - sodium-iodide symporter; TPO- thyroid peroxidase DIT - di-iodotyrosine; MIT - monoiodotyrosine
Thyroid Hormone Synthesis Thyroid hormones are derived from thyroglobulin • Large iodinated glycoprotein After secretion into the thyroid follicle • Tg is iodinated on selected tyrosine residues that are subsequently coupled via an ether linkage • Reuptake of Tg into thyroid follicular cell allows proteolysis and the release of T 4 and T 3.
Iodine Metabolism and Transport • Iodide uptake is a critical first step in thyroid hormone synthesis • Ingested iodine is bound to serum proteins (particularly albumin) • Unbound iodine is excreted in urine • Iodine extracts from circulation in a highly efficient manner – 10 to 25% of radioactive tracer (e. g. , 123 I) is taken up by the normal thyroid gland over 24 h; this value can rise to 70 to 90% in Graves' disease.
Na+/I- symporter (NIS) • Mediate Iodide uptake • Expressed at basolateral membrane of thyroid follicular cells. • Expressed – Most highly in thyroid gland – Low levels in salivary glands, lactating breast, placenta • Low I 2 levels increase amount of NIS & stimulate uptake • High I 2 levels suppress NIS expression & uptake
Selective expression of NIS in thyroid allows – Treatment of hyperthyroidism – Isotopic scanning – Abolition of thyroid cancer with radioisotopes of iodine Without significant effects on other organs Mutation of the NIS gene is a rare cause of congenital hypothyroidism
Oranification • Iodide enters thyroid • Trapped and transported to apical membrane of thyroid follicular cells • Oxidized in an organification reaction (Tyroid Per. Oxidase & H 2 O 2 )

Coupling Reactive iodine atom is added to selected tyrosyl residues within Tyroglobulin Iodotyrosines in Tg are then coupled via an ether linkage in a reaction Catalyzed by TPO Either T 4 or T 3 can be produced by this reaction • Depending on number of iodine atoms present in iodotyrosines.
Storage, Release • After coupling, Tg is taken back into thyroid cell • It is processed in lysosomes to release T 4 and T 3 • Uncoupled mono- and diiodotyrosines (MIT, DIT) are deiodinated by enzyme dehalogenase • Recycling any iodide that is not converted into thyroid hormones
Factors Influence Synthesis and Release TSH is the dominant hormonal regulator of thyroid gland growth and function Variety of growth factors, most produced locally in thyroid gland, also influence synthesis • • • Insulin-like growth factor I (IGF-I Epidermal growth factor Transforming growth factor β (TGF- β) Endothelins Various cytokines.
• Disorders of thyroid hormone synthesis – Rare causes of congenital hypothyroidism • Majority of disorders due to recessive mutations in TPO or Tg • Defects also identified in – TSH-R – NIS – Pendrin anion transporter • Transports I 2 from cytoplasm to follicle lumen – H 2 O 2 generation – Dehalogenase
• Biosynthetic defect of thyroid hormone • Inadequate amounts of hormone • Increased TSH synthesis • Goiter
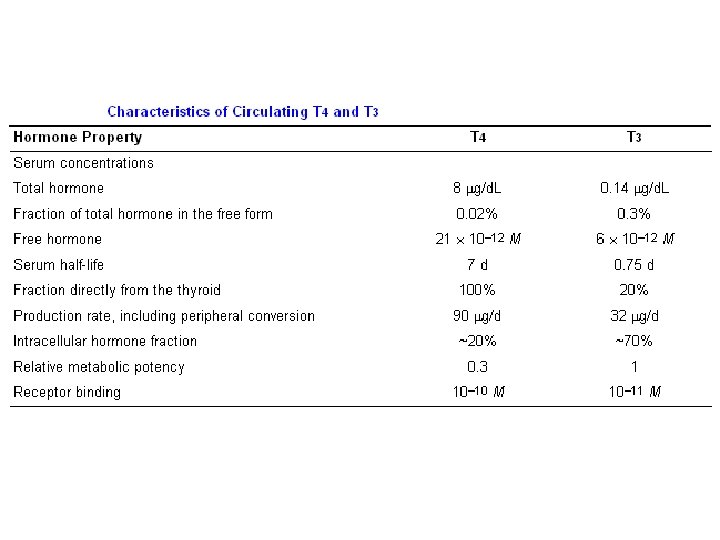
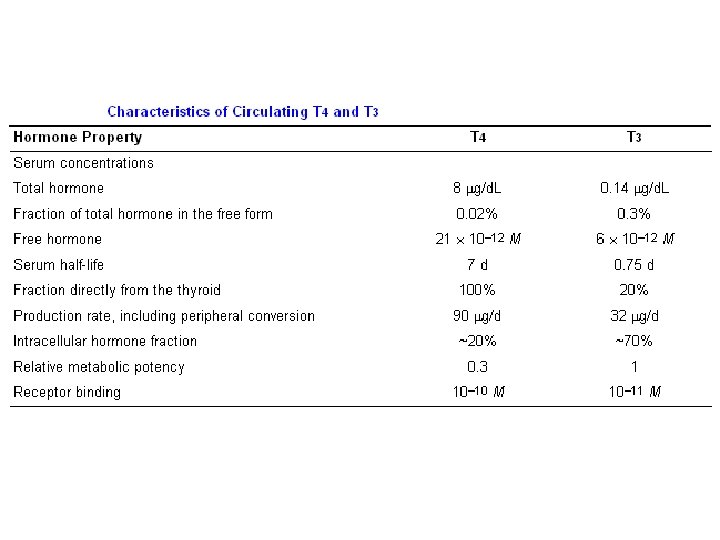
Transport And Metabolism • T 4 is secreted from the thyroid gland in at least 20 fold excess over T 3 Both circulate bound to plasma proteins • Thyroxine-binding globulin (TBG) • Transthyretin (TTR), formerly known as thyroxinebinding prealbumin (TBPA) • Albumin
Functions of serum-binding proteins • Increase pool of circulating hormone • Delay hormone clearance • Modulate hormone delivery to selected tissue sites
Con. of TBG is relatively low (1 to 2 mg/d. L) • High affinity for thyroid hormones (T 4 > T 3), it carries about 80% of bound hormones Albumin has relatively low affinity for thyroid hormones (high plasma con ~3. 5 g/d. L) • It binds up to 10% of T 4 and 30% of T 3. TTR carries about 10% of T 4 but little T 3.
• ≈ 99. 98% of T 4 and 99. 7% of T 3 are protein-bound • T 3 is less tightly bound than T 4 • Amount of free T 3 > free T 4 Unbound (free) cons • T 4 ~2 ´ 10 -11 M • T 3 ~6 ´ 10 -12 M
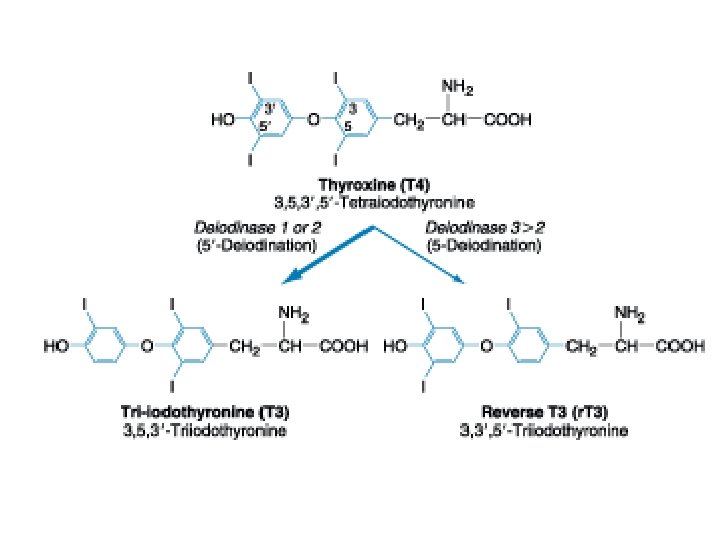
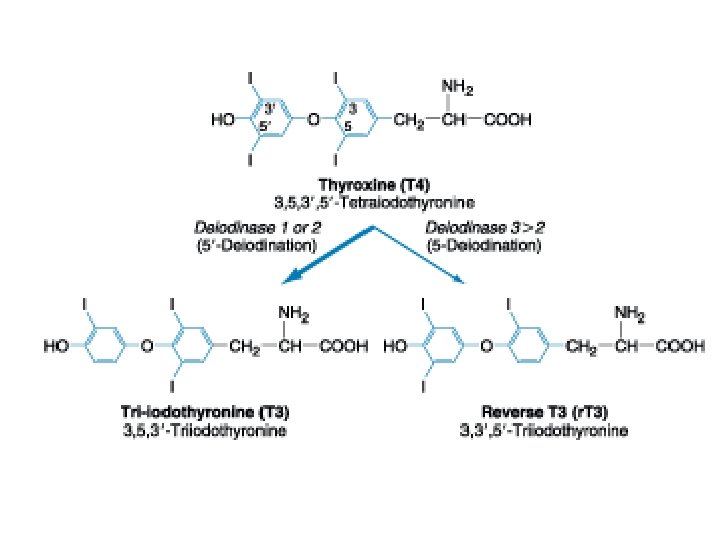
Deiodinases • In many respects, T 4 may be thought of as a precursor for more potent T 3 • T 4 is converted to T 3 by the deiodinase enzymes Type I deiodinase • Located primarily in thyroid, liver, kidney • Has a relatively low affinity for T 4 Type II deiodinase • Higher affinity for T 4 • Found primarily in pituitary gland, brain, brown fat, thyroid gland
T 4 - T 3 conversion may be impaired by • Fasting • Acute trauma • Oral contraseptive agents • Propylthiouracil • Propranolol • Amiodarone • Glucocorticoids
THYROID HORMONE ACTION • Act by binding to nuclear receptors, termed thyroid hormone receptors (TRs) ά and β • Both ά and β are expressed in most tissues • Both receptors are variably spliced to form unique isoforms
Thyroid hormone receptors ά Highly expressed in – – – Brain Kidney Gonads Muscle Heart • TR ά 2 isoform contains a unique carboxy terminus that prevents thyroid hormone binding • It may function to block actions of other TR isoforms
Thyroid hormone receptors β Highly expressed in – Pituitary – Liver TR β 2 isoform • Has a unique amino terminus • Selectively expressed in hypothalamus & pituitary • Play a role in feedback control of thyroid axis
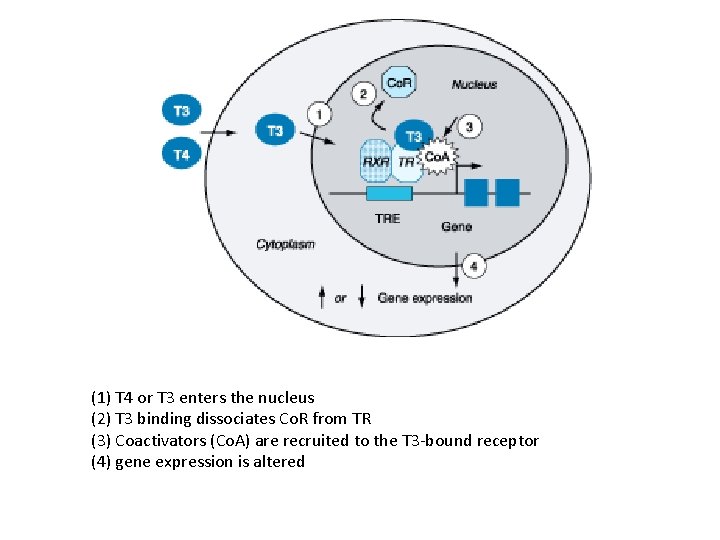
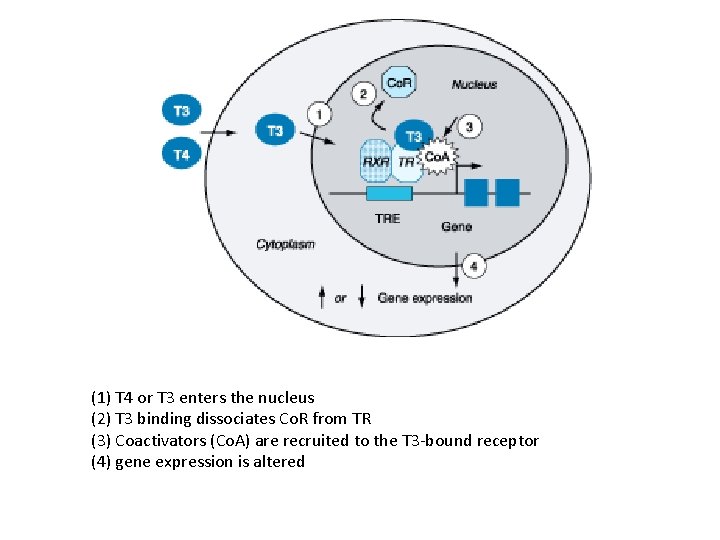
(1) T 4 or T 3 enters the nucleus (2) T 3 binding dissociates Co. R from TR (3) Coactivators (Co. A) are recruited to the T 3 -bound receptor (4) gene expression is altered
Thyroid Hormone Resistance (RTH) An autosomal dominant disorder characterized by • Elevated free thyroid hormone levels • Inappropriately normal or elevated TSH • Individuals with RTH (in general) do not exhibit signs and symptoms that are typical of hypothyroidism • Apparently hormone resistance is compensated by increased levels of thyroid hormone
HYPOTHYROIDISM • Worldwide most common cause of hypothyroidism - Iodine deficiency Other causes • Autoimmune disease (Hashimoto's thyroiditis) • Iatrogenic causes (treatment of hyperthyroidism)
Treatment • T 4 - 10 to 15 ug/kg/ day • Dose adjusted by close monitoring of TSH levels • T 4 requirements- relatively great during first year of life • High circulating T 4 level is usually needed to normalize TSH • Early treatment with T 4 results in normal IQ levels
Hyperthyroidism • Excessive thyroid function Thyrotoxicosis • State of thyroid hormone excess Major etiologies of thyrotoxicosis • Hyperthyroidism caused by Graves' disease • Toxic multinodular goiter • Toxic adenomas
Treatment Hyperthyroidism of Graves' disease is treated by reducing thyroid hormone synthesis • Antithyroid drugs • Reducing the amount of thyroid tissue with radioiodine (131 I) • Subtotal thyroidectomy No single approach is optimal and that patients may require multiple treatments to achieve remission. Antithyroid drugs are the predominant therapy in many centers in Europe and Japan Radioiodine is more often the first line of treatment in North America
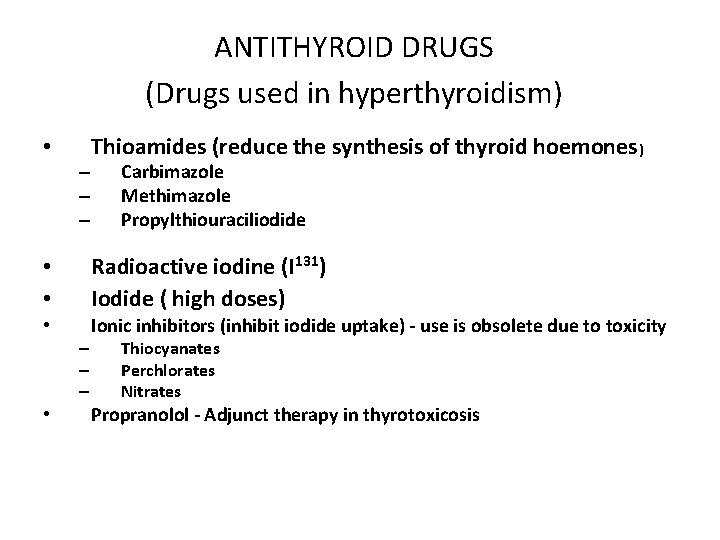
ANTITHYROID DRUGS (Drugs used in hyperthyroidism) • – – – Thioamides (reduce the synthesis of thyroid hoemones) Carbimazole Methimazole Propylthiouraciliodide • • Radioactive iodine (I 131) Iodide ( high doses) • Ionic inhibitors (inhibit iodide uptake) - use is obsolete due to toxicity – – – • Thiocyanates Perchlorates Nitrates Propranolol - Adjunct therapy in thyrotoxicosis
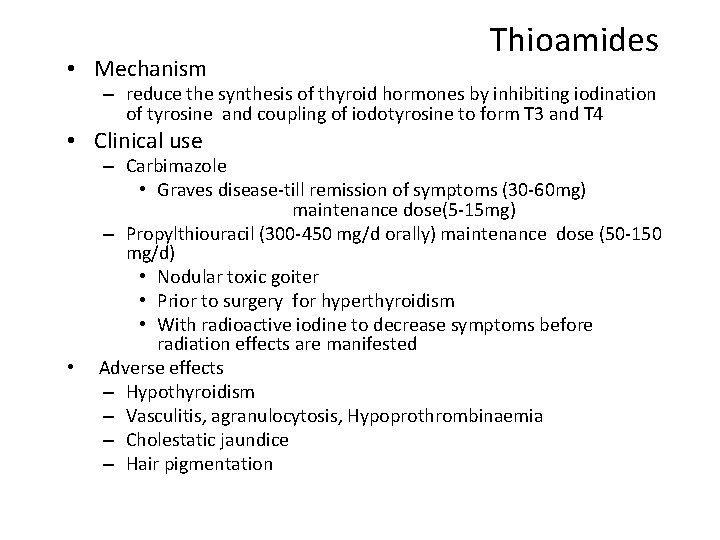
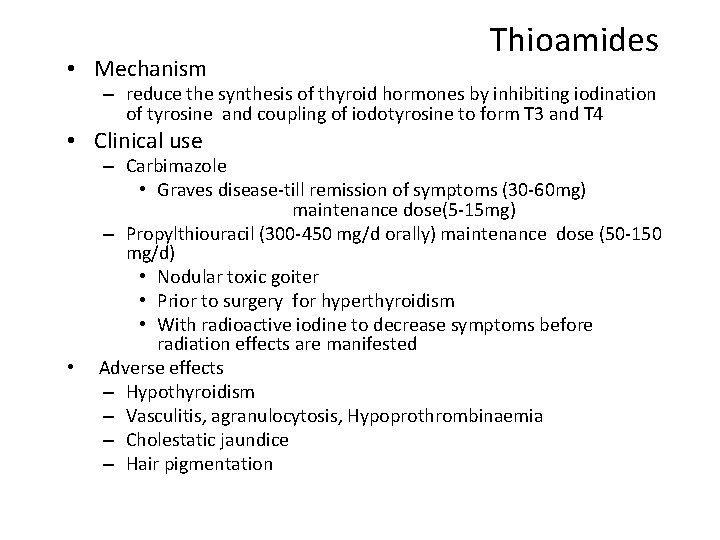
• Mechanism Thioamides – reduce the synthesis of thyroid hormones by inhibiting iodination of tyrosine and coupling of iodotyrosine to form T 3 and T 4 • Clinical use • – Carbimazole • Graves disease-till remission of symptoms (30 -60 mg) maintenance dose(5 -15 mg) – Propylthiouracil (300 -450 mg/d orally) maintenance dose (50 -150 mg/d) • Nodular toxic goiter • Prior to surgery for hyperthyroidism • With radioactive iodine to decrease symptoms before radiation effects are manifested Adverse effects – Hypothyroidism – Vasculitis, agranulocytosis, Hypoprothrombinaemia – Cholestatic jaundice – Hair pigmentation
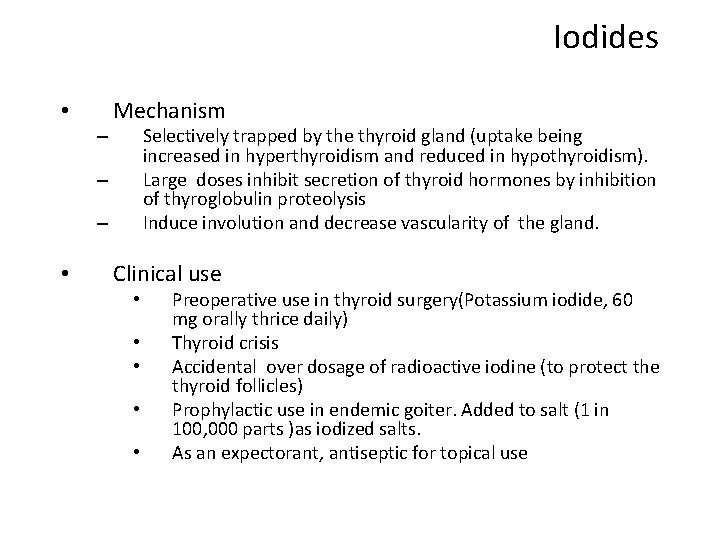
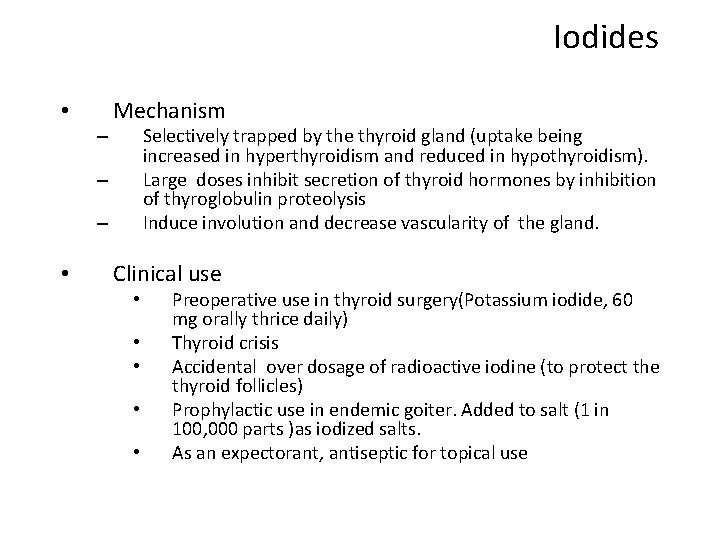
Iodides • – Mechanism Selectively trapped by the thyroid gland (uptake being increased in hyperthyroidism and reduced in hypothyroidism). Large doses inhibit secretion of thyroid hormones by inhibition of thyroglobulin proteolysis Induce involution and decrease vascularity of the gland. – – • Clinical use • • • Preoperative use in thyroid surgery(Potassium iodide, 60 mg orally thrice daily) Thyroid crisis Accidental over dosage of radioactive iodine (to protect the thyroid follicles) Prophylactic use in endemic goiter. Added to salt (1 in 100, 000 parts )as iodized salts. As an expectorant, antiseptic for topical use
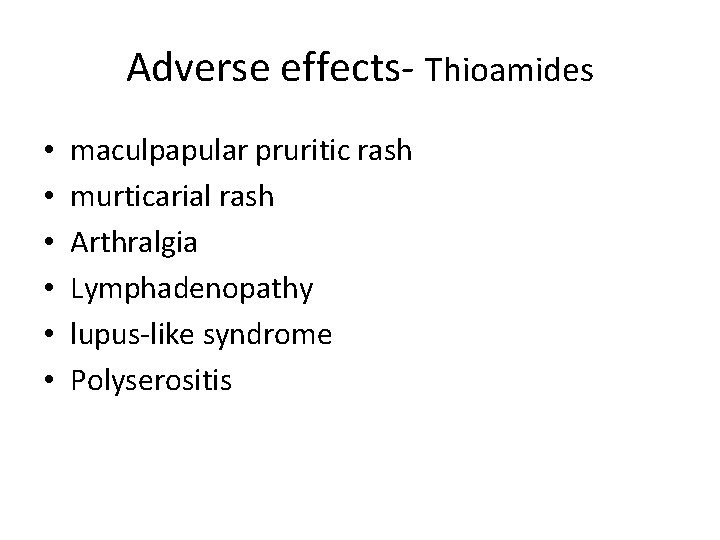
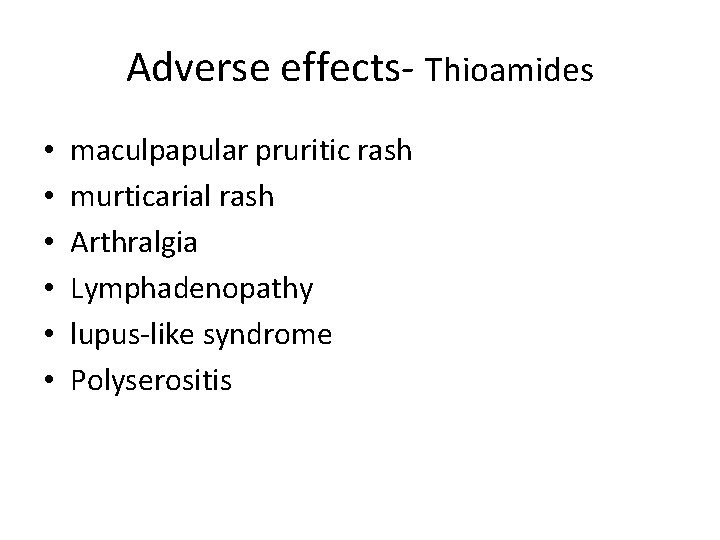
Adverse effects- Thioamides • • • maculpapular pruritic rash murticarial rash Arthralgia Lymphadenopathy lupus-like syndrome Polyserositis
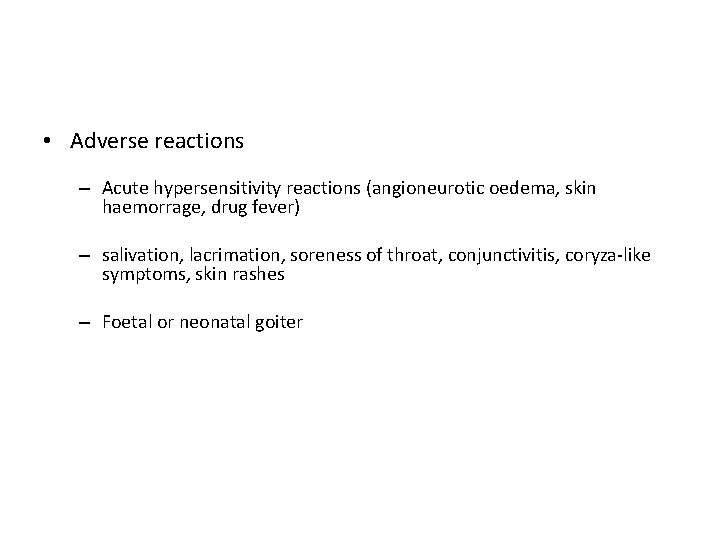
• Adverse reactions – Acute hypersensitivity reactions (angioneurotic oedema, skin haemorrage, drug fever) – salivation, lacrimation, soreness of throat, conjunctivitis, coryza-like symptoms, skin rashes – Foetal or neonatal goiter
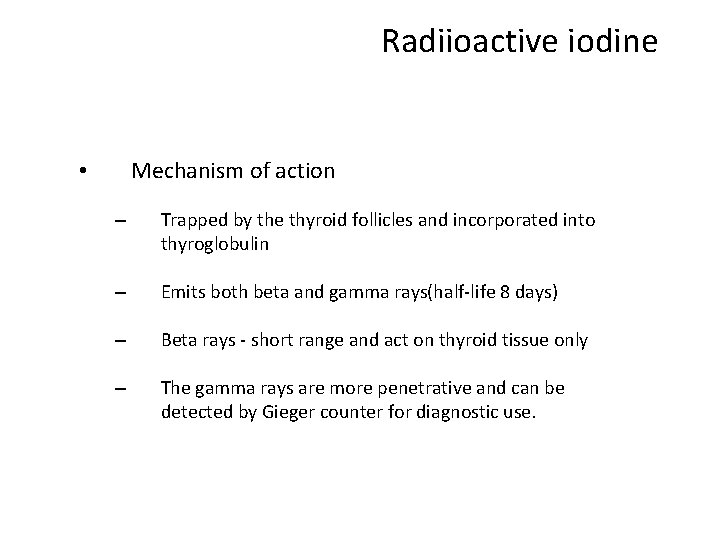
Radiioactive iodine Mechanism of action • – Trapped by the thyroid follicles and incorporated into thyroglobulin – Emits both beta and gamma rays(half-life 8 days) – Beta rays - short range and act on thyroid tissue only – The gamma rays are more penetrative and can be detected by Gieger counter for diagnostic use.
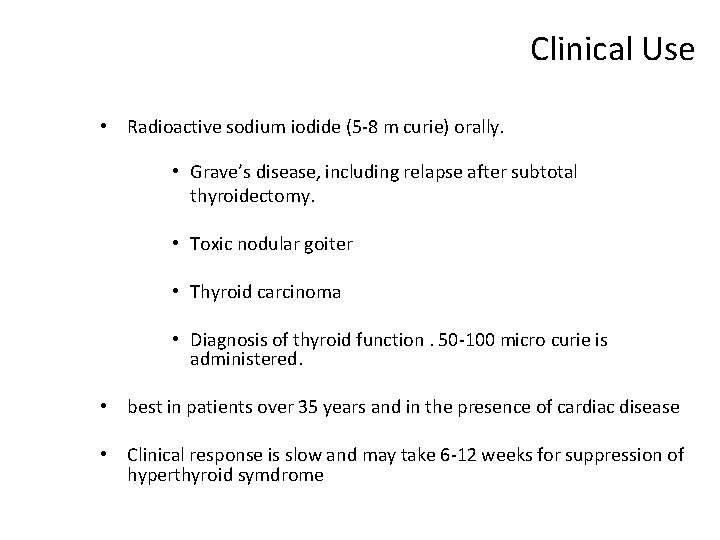
Clinical Use • Radioactive sodium iodide (5 -8 m curie) orally. • Grave’s disease, including relapse after subtotal thyroidectomy. • Toxic nodular goiter • Thyroid carcinoma • Diagnosis of thyroid function. 50 -100 micro curie is administered. • best in patients over 35 years and in the presence of cardiac disease • Clinical response is slow and may take 6 -12 weeks for suppression of hyperthyroid symdrome
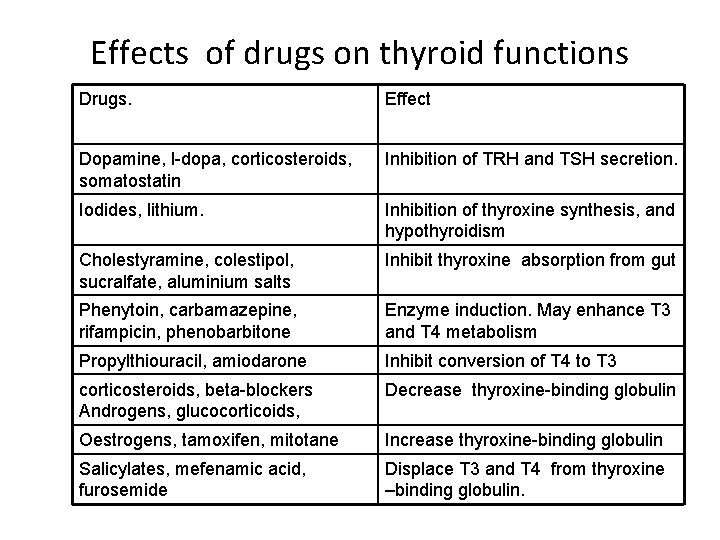
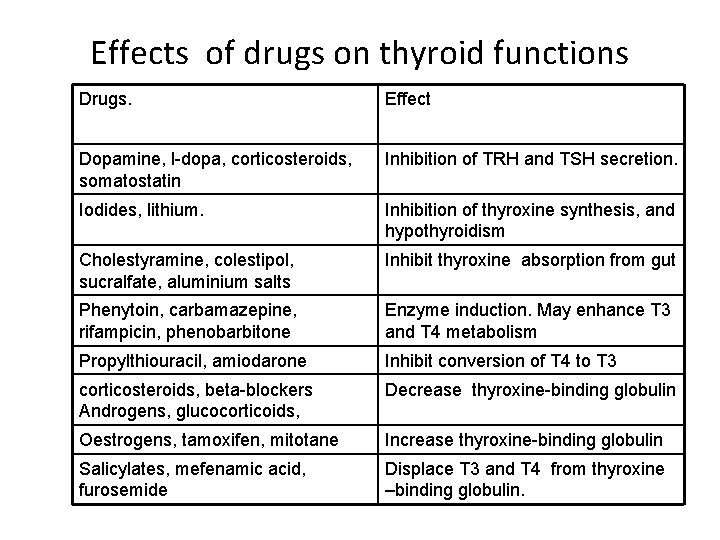
Effects of drugs on thyroid functions Drugs. Effect Dopamine, l-dopa, corticosteroids, somatostatin Inhibition of TRH and TSH secretion. Iodides, lithium. Inhibition of thyroxine synthesis, and hypothyroidism Cholestyramine, colestipol, sucralfate, aluminium salts Inhibit thyroxine absorption from gut Phenytoin, carbamazepine, rifampicin, phenobarbitone Enzyme induction. May enhance T 3 and T 4 metabolism Propylthiouracil, amiodarone Inhibit conversion of T 4 to T 3 corticosteroids, beta-blockers Androgens, glucocorticoids, Decrease thyroxine-binding globulin Oestrogens, tamoxifen, mitotane Increase thyroxine-binding globulin Salicylates, mefenamic acid, furosemide Displace T 3 and T 4 from thyroxine –binding globulin.
 Thyoid gland
Thyoid gland Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual Follicular cells of thyroid gland
Follicular cells of thyroid gland Tonsils
Tonsils Berry's ligament thyroid
Berry's ligament thyroid Low thyroid symptoms
Low thyroid symptoms Parafollicular
Parafollicular Pheochromocytoma
Pheochromocytoma Oxyphil
Oxyphil Parathyroid gland supplied by
Parathyroid gland supplied by Four oval masses on posterior thyroid gland
Four oval masses on posterior thyroid gland Hypothyroidism dwarfism
Hypothyroidism dwarfism Papillary thyroid carcinoma gross
Papillary thyroid carcinoma gross How to check thyroid at home
How to check thyroid at home Hashitoxicosis
Hashitoxicosis Principal cells location
Principal cells location Parathyroid gland chief cell
Parathyroid gland chief cell Nodular goiter
Nodular goiter Admisteration
Admisteration Baş beyinin hissələri
Baş beyinin hissələri Thymus gland location
Thymus gland location Parathyroid gland location
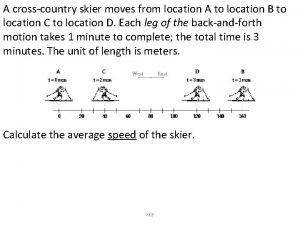
Parathyroid gland location A cross country skier moves from location a
A cross country skier moves from location a What is location planning in operations management
What is location planning in operations management What is ion trapping in pharmacology
What is ion trapping in pharmacology Absolute bioavailability
Absolute bioavailability What is ion trapping in pharmacology
What is ion trapping in pharmacology Objectives of pharmacology
Objectives of pharmacology Clinical pharmacology residency
Clinical pharmacology residency Toxicology and applied pharmacology
Toxicology and applied pharmacology Lomotib
Lomotib Basic principles of pharmacology
Basic principles of pharmacology What is bioavailability
What is bioavailability Formula of maintenance dose
Formula of maintenance dose Receptors in pharmacology
Receptors in pharmacology Essential drug concept in pharmacology
Essential drug concept in pharmacology Pharmacology and venipuncture in radiology pdf
Pharmacology and venipuncture in radiology pdf Clinical pharmacology
Clinical pharmacology Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Adrenal drugs pharmacology
Adrenal drugs pharmacology Slidetodoc.com
Slidetodoc.com Factors affecting drug metabolism
Factors affecting drug metabolism What is pharmacology
What is pharmacology