Nutrition Support Therapy 2 Parenteral Nutrition Rationale Knowledge


- Slides: 23
Nutrition Support Therapy 2 Parenteral Nutrition
Rationale: • Knowledge of Parenteral Nutrition support is essential to fight complications in situations of inadequate oral intale Learning outcomes: • Understand the indications of TPN • Learn the routes of TPN • Acknowledge the related complications
Definition & Indication Parenteral nutrition (PN) is the intravenous provision of nutrients, without using the gastrointestinal (GI) system. It should be considered for patients with: • malnutrition or inadequate or unsafe oral and/or enteral nutritional intake r • GI functionality insufficient to support an adequate degree of digestion and absorption of nutrients, due to ileus, dysmotility, fistulae, surgical resection, etc. • prolonged GI system failure (>5 days) or intestinal failure which is predicted to last for >5 days. • PN may also be chosen in patients who cannot tolerate enteral feeding (EF) or when EF is unsafe or impractical.
Routes of parenteral nutritional administration? Peripheral parenteral nutrition • Peripheral PN (PPN) is usually reserved for patients requiring short-term nutrition support (up to 2 weeks) who are not markedly hypermetabolic or fluidrestricted and have adequate peripheral venous access. • PPN usually cannot provide adequate calories and protein in patients who are volume restricted, but can be helpful for several days until GI function returns or central access is obtained. Other contraindications to PPN include significant malnutrition, large nutrient or electrolyte needs, and/or renal or liver compromise.
Central Parenteral Nutrition (CPN) • Central PN which is also known as total parenteral nutrition is indicated in patients requiring long-term therapy or a concentrated formula. • Proper selection of venous access depends on nutrient requirements and length of therapy. For short-term CPN a temporary percutaneous non-tunneled CVC may be used in the acute setting via the subclavian or jugular vein (CICC). A peripherally inserted central catheter (PICC) may also be used if CPN is needed for weeks and not long-term. A tunneled catheter such as a Hickman®, Broviac® or Groshong® or implanted port may also be used for longterm access.


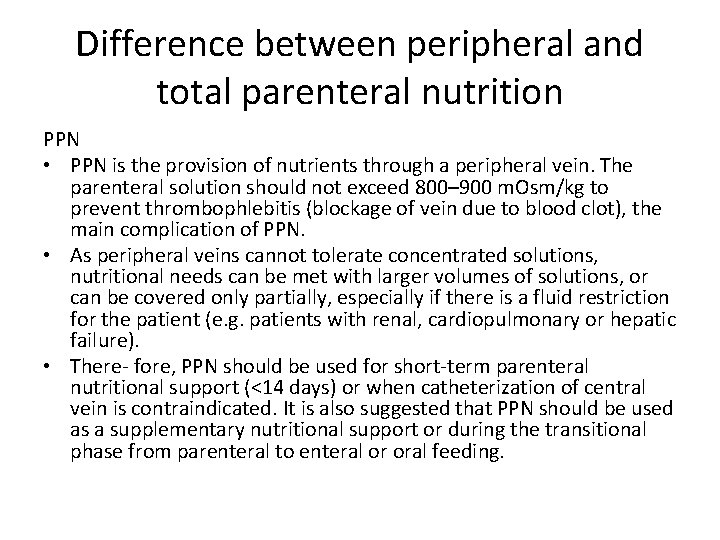
Difference between peripheral and total parenteral nutrition PPN • PPN is the provision of nutrients through a peripheral vein. The parenteral solution should not exceed 800– 900 m. Osm/kg to prevent thrombophlebitis (blockage of vein due to blood clot), the main complication of PPN. • As peripheral veins cannot tolerate concentrated solutions, nutritional needs can be met with larger volumes of solutions, or can be covered only partially, especially if there is a fluid restriction for the patient (e. g. patients with renal, cardiopulmonary or hepatic failure). • There- fore, PPN should be used for short-term parenteral nutritional support (<14 days) or when catheterization of central vein is contraindicated. It is also suggested that PPN should be used as a supplementary nutritional support or during the transitional phase from parenteral to enteral or oral feeding.
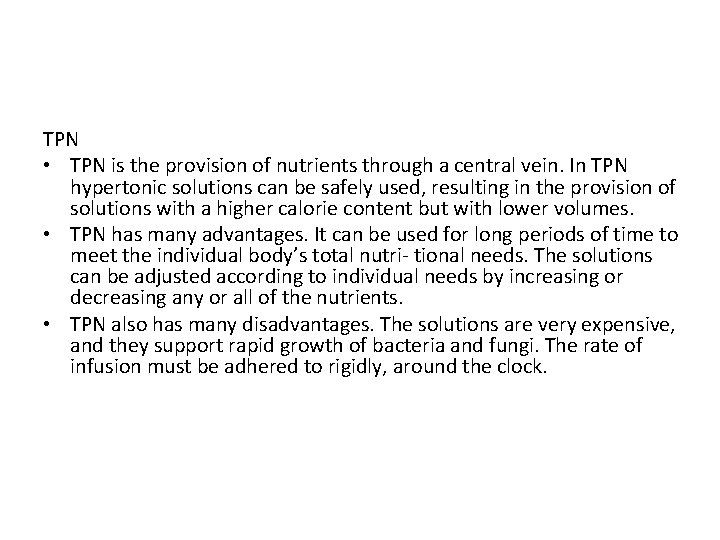
TPN • TPN is the provision of nutrients through a central vein. In TPN hypertonic solutions can be safely used, resulting in the provision of solutions with a higher calorie content but with lower volumes. • TPN has many advantages. It can be used for long periods of time to meet the individual body’s total nutri- tional needs. The solutions can be adjusted according to individual needs by increasing or decreasing any or all of the nutrients. • TPN also has many disadvantages. The solutions are very expensive, and they support rapid growth of bacteria and fungi. The rate of infusion must be adhered to rigidly, around the clock.
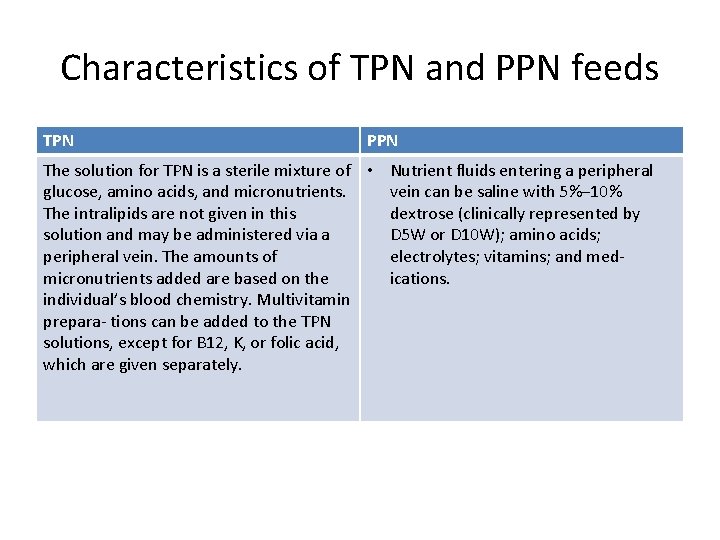
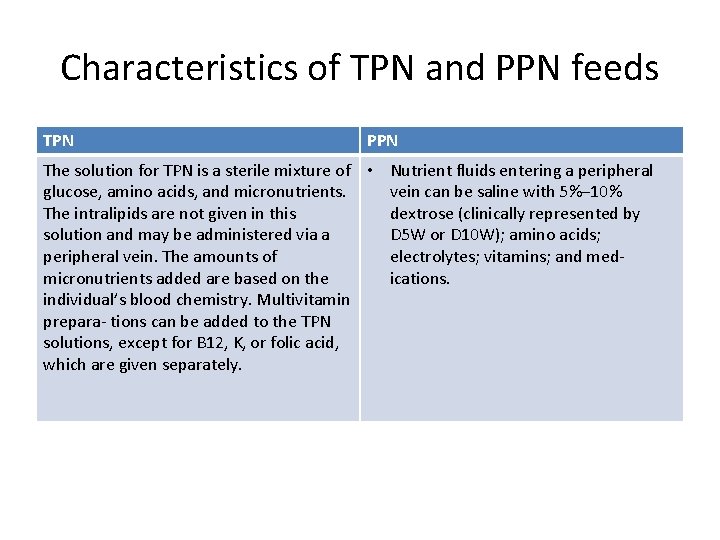
Characteristics of TPN and PPN feeds TPN PPN The solution for TPN is a sterile mixture of • Nutrient fluids entering a peripheral glucose, amino acids, and micronutrients. vein can be saline with 5%– 10% The intralipids are not given in this dextrose (clinically represented by solution and may be administered via a D 5 W or D 10 W); amino acids; peripheral vein. The amounts of electrolytes; vitamins; and medmicronutrients added are based on the ications. individual’s blood chemistry. Multivitamin prepara- tions can be added to the TPN solutions, except for B 12, K, or folic acid, which are given separately.
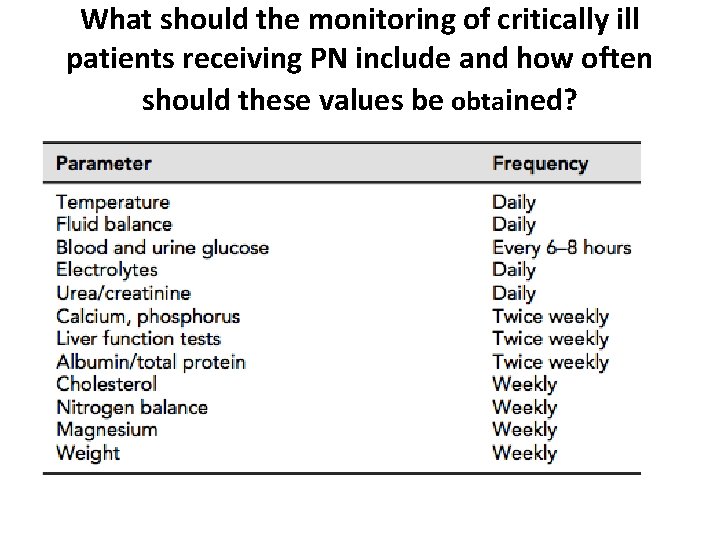
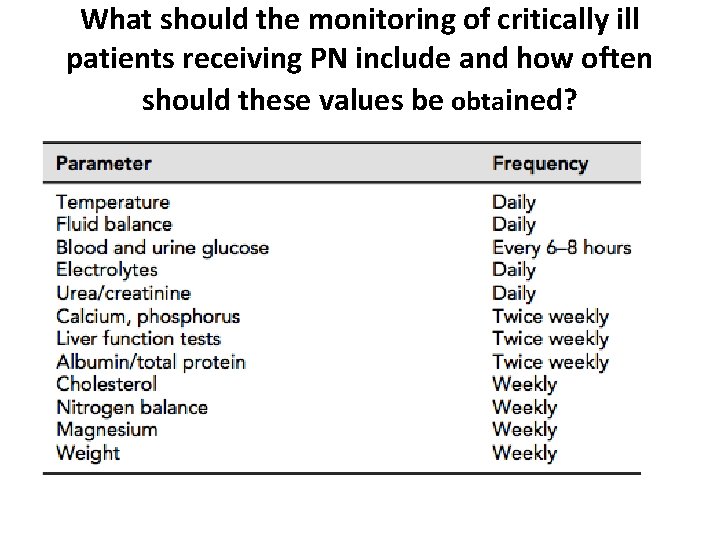
What should the monitoring of critically ill patients receiving PN include and how often should these values be obtained?
How can the nutritional needs of critically ill patients be calculated? Energy: • For the majority of patients, the provision of 20– 30 kcal/kg seems to be adequate, while for severely malnourished patients or those at risk of refeeding syndrome lower levels of energy intake should be chosen. Protein: • Typically, the provision of 1. 0 g/kg of protein (corresponding in 0. 15 g nitrogen from amino acids) is sufficient for most patients. • The primary function of amino acids in PN solutions is to maintain or improve nitrogen balance and promote maintenance of lean body mass. • In situations of severe metabolic stress requirements could be higher (i. e. 1. 0– 1. 5 g/kg), while in patients with renal or hepatic failure lower protein intakes are advised.
Carbohydrates: • Carbohydrates are provided as an energy substrate and are supplied as dextrose monohydrate in concentrations ranging from 2. 5 to 70 percent. A 10 percent solution yields 100 g of carbohydrate per liter of solution. Higher dextrose concentrations, usually greater than 10 percent, are used when central access is available as thrombophlebitis may occur in a peripheral vein • Metabolic stress is characterized by insulin resistance, hyperglycemia, and impaired glucose oxidation. When glucose oxidation rates are exceeded, fat synthesis will occur, which may generate excessive CO 2. This may contribute to CO 2 retention in patients with respiratory disease. It can also contribute to hepatic steatosis or fat deposition in the liver. • Therefore, dextrose infusion should be limited to 7 mg/kg per minute in stable hospitalized patients and greater than 4 mg/kg per minute in the critically ill.
Lipids: • Intravenous fat emulsions (IVFE) supply lipids, which are a source of essential fatty acids (EFAs) and a concentrated source of calories. In addition, the use of IVFE may aid in blood glucose control in the hyperglycemic patient. • IVFE are available in 10 and 20 percent concentrations for infusion • They are composed of aqueous suspensions of soybean or safflower oil, with egg yolk phospholipid as the emulsifier. Patients who are allergic to eggs should not be given IVFE and can be given safflower or sunflower oil topically or enterally. • The high levels of linoleic acid in soy-based lipids produces proinflammatory and immunosup- pressive effects, particularly at high doses and at faster infusion rates. A maximum dose of 1 g of lipid per kg per day should be infused to avoid hepatic effects such a steatosis, cholestasis, and/or parenteral nutrition related liver disease. which can be seen in long -term PN patients. Daily infusion of lipid should therefore be avoided in long-term PN-dependent patients.
Fluids: • Fluids should be about 30– 35 ml/kg per day, adding possible fluid losses owing to drains fistulae, etc. All sources of fluids should be calculated to avoid the excessive provision of fluid. • Daily fluid requirements can be estimated from the sum of fluid losses including urine, GI and insensible losses, minus the fluid gains, such as other IV fluids and/or oral intake. • Weighing the patient daily is the best means of assessing net gain or loss of fluid. Rapid weight gain or loss (more than 4 pounds (1. 8 kg) in 1 week) generally represents fluid changes and not tissue synthesis. • Vital signs, such as blood pressure and heart rate, and physi- cal examination changes (e. g. , edema, ascites, and skin turgor) also offer evidence of fluid status.
Electrolytes: • Electrolytes are routinely added to PN solutions in amounts sufficient to provide for daily needs. Electrolyte requirements will vary depending on the patient’s current electrolyte, renal, and fluid status, as well as their underlying disease process. • Sodium is a major extracellular cation and functions in the maintenance of osmotic pressure and in acid–base balance. The usual dose is 1 to 2 m. Eq/kg per day. Requirements may be increased when there are excess losses from urine, ostomies, or fistulas or decreased in renal, cardiac, or hepatic failure. • Potassium is the major cation of intracellular fluid. The normal dose is 1 m. Eq/kg per day. Hypokalemia may result from diuretics, amphotericin B, nasogastric suction, or vomiting. Other medications such as cyclosporine and tacrolimus may cause hyperkalemia. • Calcium is an extracellular cation that is essential for normal muscle contraction, nerve function, blood coagulation, and bone mineralization. The usual dose is 10 to 15 m. Eq/day. Sixty percent of serum calcium is bound to protein, primarily albumin. Therefore, in the presence of a low serum albumin level, a low serum calcium level needs to be adjusted for hypoalbuminemia. • Magnesium functions in enzyme reactions such as glycolysis and in all reactions involving adenosine triphosphate (ATP). Magnesium is often depleted in patients with protein calorie mal- nutrition and prolonged IV fluid therapy.
main complications of parenteral nutrition • PN is associated with complications related to intravenous access. The establishment and maintenance of PN access may lead to: • trauma on the central line placement, e. g. carotid puncture or pneumothorax • thrombophlebitis, especially when PN is provided peripherally • catheter occlusion and thromboembolism • air embolism • infection of sepsis at the catheter site.
Refeeding syndrome • Refeeding syndrome may occur when starting PN in a patient after a period of prolonged starvation resulting in fluid retention and hyperglycemia in addition to severe imbalances of serum phosphorus, potassium, and magnesium. • Once PN begins, increased cellular uptake of electrolytes may cause extremely low serum levels. This dramatic shift can lead to generalized fatigue, lethargy, muscle weakness, edema, cardiac dysfunction, and potentially death. • The risk of refeeding syndrome can be minimized by initially providing the patient a low-dextrose PN solution for the first several days while closely monitoring phosphorus, potassium, magnesium, glucose, and fluid status • .
Non-Infectious Catheter Complications • Heparin-induced thrombocytopenia (HIT) is a severe immunemediated adverse reaction that occurs by intravascular platelet aggregation that can develop into arterial and venous thrombus. • Catheter occlusions can also occur and are classified as either a complete or incomplete occlusion. In a complete occlusion, fluid cannot be instilled and blood cannot be aspirated out, whereas an incomplete occlusion, fluid can be infused yet blood cannot be aspirated • A venous thrombus can occur if the catheter tip is malpostitioned • An air embolism is a rare yet potentially fatal complication where either during or after insertion, there is catheter breakage or a disconnection of caps. • Catheter dislodgement can occur with any CVC and move out of central circulation in which case the catheter should be replaced
Septic (Infectious) Complications • During CPN infusion, if there is a sudden change in the patient’s usual temperature, in combination with new onset shaking chills, leukocytosis, or unexplained hyperglycemia, the CVC should be viewed as the possible source of infection. • This is known as a catheter-related blood stream infection (CRBSI). CRBSI is a clinical definition, used when diagnosing and treating patients, that requires specific laboratory testing that more thoroughly identifies the catheter as the source of the infection.
METABOLIC COMPLICATIONS Hyperglycemia • Hyperglycemia is the most common adverse effect of PN and has been associated with increased morbidity and mortality in hospitalized patients. Close monitoring of blood sugars along with aggressive treatment reduces hyperglycemia and improves outcomes. Capillary blood glucose levels should be monitored every 6 hours until adequately controlled. Blood sugars in hospitalized patients receiving nutrition support should be maintained between 140 and 180 mg/d. L. • PN-associated hyperglycemia may be treated by insulin drip, shortor long-acting insulin administered subcutaneously, insulin added to the PN or a combination of these methods. In some instances, it may be necessary to reduce dextrose calories and replace with lipid calories to aid in blood glucose control.
Hypoglycemia: • It is defined as a blood glucose concentration of less than 70 mg/d. L, may occur if an excessive amount of insulin is added to the PN solution or after abrupt discontinuation of high- dextrose PN infusion. • To avoid hypoglycemia, insulin should be added in increments to the PN solution and blood sugars monitored frequently until the appropriate dose is determined.
Dehydration and fluid overload: • They are potential complications when PN is the primary source of fluid. • Fluid overload or edema may be seen in patients with renal failure, liver failure, congestive heart failure, and hypoalbuminemia. • Excessive PN volume can significantly exacerbate fluid retention states. Under these circumstances, a concentrated PN solution may be used. • Fluid status should be evaluated daily to determine if the patient is dehydrated or at risk for fluid overload. Monitor intake, output, and body weight records daily. • The physical examination should note the presence of edema, rales, ascites, distended neck veins, and other signs of fluid retention.
 Outpatient parenteral antimicrobial therapy (opat)
Outpatient parenteral antimicrobial therapy (opat) Rationale of periodontal therapy
Rationale of periodontal therapy How to calculate tpn calories
How to calculate tpn calories Tpn tapering guidelines
Tpn tapering guidelines Complication of parenteral nutrition
Complication of parenteral nutrition Types of parenteral nutrition
Types of parenteral nutrition Rxkinetics tpn
Rxkinetics tpn Complication of parenteral nutrition
Complication of parenteral nutrition Total parenteral nutrition cost
Total parenteral nutrition cost Small bowel obstruction parenteral nutrition
Small bowel obstruction parenteral nutrition Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Nutrition fundamentals of nursing
Nutrition fundamentals of nursing Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Chapter 28 nutritional support and iv therapy
Chapter 28 nutritional support and iv therapy Abbott feeding pump error codes
Abbott feeding pump error codes Product formulation statement
Product formulation statement Child nutrition knowledge center
Child nutrition knowledge center Example of major points
Example of major points Knowledge management decision support
Knowledge management decision support